Atomoxetine
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING:
See full prescribing information for complete Boxed Warning.
SUICIDAL IDEATION IN CHILDREN AND ADOLESCENTS
|
Overview
Atomoxetine is a selective norepinephrine reuptake inhibitor that is FDA approved for the treatment of attention-deficit/hyperactivity disorder(ADHD). There is a Black Box Warning for this drug as shown here. Common adverse reactions include nausea, vomiting, fatigue, decreased appetite, abdominal pain, and somnolence.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Attention-Deficit/Hyperactivity Disorder (ADHD)
- Dosing Information
- Acute Treatment
- Atomoxetine should be initiated at a total daily dose of 40 mg and increased after a minimum of 3 days to a target total daily dose of approximately 80 mg administered either as a single daily dose in the morning or as evenly divided doses in the morning and late afternoon/early evening. After 2 to 4 additional weeks, the dose may be increased to a maximum of 100 mg in patients who have not achieved an optimal response. There are no data that support increased effectiveness at higher doses.
- The maximum recommended total daily dose in adults is 100 mg.
- Maintenance/Extended Treatment
- It is generally agreed that pharmacological treatment of ADHD may be needed for extended periods. Patients assigned to Atomoxetine in the maintenance phase were generally continued on the same dose used to achieve a response in the open label phase. The physician who elects to use Atomoxetine for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Atomoxetine in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Atomoxetine in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Attention-Deficit/Hyperactivity Disorder (ADHD)
- The efficacy of Atomoxetine Capsules was established in seven clinical trials in outpatients with ADHD: four 6 to 9-week trials in pediatric patients (ages 6 to 18), two 10-week trial in adults, and one maintenance trial in pediatrics (ages 6 to 15).
- Diagnostic Considerations
- A diagnosis of ADHD (DSM-IV) implies the presence of hyperactive-impulsive or inattentive symptoms that cause impairment and that were present before age 7 years. The symptoms must be persistent, must be more severe than is typically observed in individuals at a comparable level of development, must cause clinically significant impairment, e.g., in social, academic, or occupational functioning, and must be present in 2 or more settings, e.g., school (or work) and at home. The symptoms must not be better accounted for by another mental disorder.
- The specific etiology of ADHD is unknown, and there is no single diagnostic test. Adequate diagnosis requires the use not only of medical but also of special psychological, educational, and social resources. Learning may or may not be impaired. The diagnosis must be based upon a complete history and evaluation of the patient and not solely on the presence of the required number of DSM-IV characteristics.
- For the Inattentive Type, at least 6 of the following symptoms must have persisted for at least 6 months: lack of attention to details/careless mistakes, lack of sustained attention, poor listener, failure to follow through on tasks, poor organization, avoids tasks requiring sustained mental effort, loses things, easily distracted, forgetful. For the Hyperactive-Impulsive Type, at least 6 of the following symptoms must have persisted for at least 6 months: fidgeting/squirming, leaving seat, inappropriate running/climbing, difficulty with quiet activities, “on the go,” excessive talking, blurting answers, can't wait turn, intrusive. For a Combined Type diagnosis, both inattentive and hyperactive-impulsive criteria must be met.
- Need for Comprehensive Treatment Program
- Atomoxetine is indicated as an integral part of a total treatment program for ADHD that may include other measures (psychological, educational, social) for patients with this syndrome. Drug treatment may not be indicated for all patients with this syndrome. Drug treatment is not intended for use in the patient who exhibits symptoms secondary to environmental factors and/or other primary psychiatric disorders, including psychosis. Appropriate educational placement is essential in children and adolescents with this diagnosis and psychosocial intervention is often helpful. When remedial measures alone are insufficient, the decision to prescribe drug treatment medication will depend upon the physician's assessment of the chronicity and severity of the patient's symptoms
- Dosing Information
- Acute Treatment
- Dosing of children and adolescents up to 70 kg body weight
- Atomoxetine should be initiated at a total daily dose of approximately 0.5 mg/kg and increased after a minimum of 3 days to a target total daily dose of approximately 1.2 mg/kg administered either as a single daily dose in the morning or as evenly divided doses in the morning and late afternoon/early evening. No additional benefit has been demonstrated for doses higher than 1.2 mg/kg/day.
- The total daily dose in children and adolescents should not exceed 1.4 mg/kg or 100 mg, whichever is less.
- Dosing of children and adolescents up to 70 kg body weight
- Dosing of children and adolescents over 70 kg body weight
- Atomoxetine should be initiated at a total daily dose of 40 mg and increased after a minimum of 3 days to a target total daily dose of approximately 80 mg administered either as a single daily dose in the morning or as evenly divided doses in the morning and late afternoon/early evening. After 2 to 4 additional weeks, the dose may be increased to a maximum of 100 mg in patients who have not achieved an optimal response. There are no data that support increased effectiveness at higher doses.
- The maximum recommended total daily dose in children and adolescents over 70 kg.
- Dosing of children and adolescents over 70 kg body weight
- Maintenance/Extended Treatment
- It is generally agreed that pharmacological treatment of ADHD may be needed for extended periods. The benefit of maintaining pediatric patients (ages 6-15 years) with ADHD on Atomoxetine after achieving a response in a dose range of 1.2 to 1.8 mg/kg/day was demonstrated in a controlled trial. Patients assigned to Atomoxetine in the maintenance phase were generally continued on the same dose used to achieve a response in the open label phase. The physician who elects to use Atomoxetine for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
- Dosing in Specific Populations
- Dosing adjustment for hepatically impaired patients — For those ADHD patients who have hepatic insufficiency (HI), dosage adjustment is recommended as follows: For patients with moderate HI (Child-Pugh Class B), initial and target doses should be reduced to 50% of the normal dose (for patients without HI). For patients with severe HI (Child-Pugh Class C), initial dose and target doses should be reduced to 25% of normal.
- Dosing adjustment for use with a strong CYP2D6 inhibitor or in patients who are known to be CYP2D6 PMs — In children and adolescents up to 70 kg body weight administered strong CYP2D6 inhibitors, e.g., paroxetine, fluoxetine, and quinidine, or in patients who are known to be CYP2D6 PMs, Atomoxetine should be initiated at 0.5 mg/kg/day and only increased to the usual target dose of 1.2 mg/kg/day if symptoms fail to improve after 4 weeks and the initial dose is well tolerated.
- In children and adolescents over 70 kg body weight and adults administered strong CYP2D6 inhibitors, e.g., paroxetine, fluoxetine, and quinidine, Atomoxetine should be initiated at 40 mg/day and only increased to the usual target dose of 80 mg/day if symptoms fail to improve after 4 weeks and the initial dose is well tolerated.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Atomoxetine in pediatric patients.
Non–Guideline-Supported Use
Nocturnal enuresis
- Dosing Information
- 0.5 mg/kg daily for 3 days, followed by 1 mg/kg/day for the next 3 days and then increased to 1.5 mg/kg/day.
Contraindications
- Hypersensitivity
- Atomoxetine is contraindicated in patients known to be hypersensitive to atomoxetine or other constituents of the product.
- Monoamine Oxidase Inhibitors (MAOI)
- Atomoxetine should not be taken with an MAOI, or within 2 weeks after discontinuing an MAOI. Treatment with an MAOI should not be initiated within 2 weeks after discontinuing Atomoxetine. With other drugs that affect brain monoamine concentrations, there have been reports of serious, sometimes fatal reactions (including hyperthermia, rigidity, myoclonus, autonomic instability with possible rapid fluctuations of vital signs, and mental status changes that include extreme agitation progressing to delirium and coma) when taken in combination with an MAOI. Some cases presented with features resembling neuroleptic malignant syndrome. Such reactions may occur when these drugs are given concurrently or in close proximity.
- Narrow Angle Glaucoma
- In clinical trials, Atomoxetine use was associated with an increased risk of mydriasis and therefore its use is not recommended in patients with narrow angle glaucoma.
- Pheochromocytoma
- Serious reactions, including elevated blood pressure and tachyarrhythmia, have been reported in patients with pheochromocytoma or a history of pheochromocytoma who received Atomoxetine. Therefore, Atomoxetine should not be taken by patients with pheochromocytoma or a history of pheochromocytoma.
- Severe Cardiovascular Disorders
- Atomoxetine should not be used in patients with severe cardiac or vascular disorders whose condition would be expected to deteriorate if they experience increases in blood pressure or heart rate that could be clinically important (for example, 15 to 20 mm Hg in blood pressure or 20 beats per minute in heart rate).
Warnings
|
WARNING:
See full prescribing information for complete Boxed Warning.
SUICIDAL IDEATION IN CHILDREN AND ADOLESCENTS
|
Precautions
- Suicidal Ideation
- Atomoxetine increased the risk of suicidal ideation in short-term studies in children and adolescents with Attention-Deficit/Hyperactivity Disorder (ADHD). Pooled analyses of short-term (6 to 18 weeks) placebo-controlled trials of Atomoxetine in children and adolescents have revealed a greater risk of suicidal ideation early during treatment in those receiving Atomoxetine. There were a total of 12 trials (11 in ADHD and 1 in enuresis) involving over 2200 patients (including 1357 patients receiving Atomoxetine and 851 receiving placebo). The average risk of suicidal ideation in patients receiving Atomoxetine was 0.4% (5/1357 patients), compared to none in placebo-treated patients. There was 1 suicide attempt among these approximately 2200 patients, occurring in a patient treated with Atomoxetine. No suicides occurred in these trials. All reactions occurred in children 12 years of age or younger. All reactions occurred during the first month of treatment. It is unknown whether the risk of suicidal ideation in pediatric patients extends to longer-term use. A similar analysis in adult patients treated with Atomoxetine for either ADHD or major depressive disorder (MDD) did not reveal an increased risk of suicidal ideation or behavior in association with the use of Atomoxetine.
- All pediatric patients being treated with Atomoxetine should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
- The following symptoms have been reported with Atomoxetine: anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania and mania. Although a causal link between the emergence of such symptoms and the emergence of suicidal impulses has not been established, there is a concern that such symptoms may represent precursors to emerging suicidality. Thus, patients being treated with Atomoxetine should be observed for the emergence of such symptoms.
- Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients who are experiencing emergent suicidality or symptoms that might be precursors to emerging suicidality, especially if these symptoms are severe or abrupt in onset, or were not part of the patient's presenting symptoms.
- Families and caregivers of pediatric patients being treated with Atomoxetine should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers.
- Severe Liver Injury
- Postmarketing reports indicate that Atomoxetine can cause severe liver injury. Although no evidence of liver injury was detected in clinical trials of about 6000 patients, there have been rare cases of clinically significant liver injury that were considered probably or possibly related to Atomoxetine use in postmarketing experience. Rare cases of liver failure have also been reported, including a case that resulted in a liver transplant. Because of probable underreporting, it is impossible to provide an accurate estimate of the true incidence of these reactions. Reported cases of liver injury occurred within 120 days of initiation of atomoxetine in the majority of cases and some patients presented with markedly elevated liver enzymes [>20 X upper limit of normal (ULN)], and jaundice with significantly elevated bilirubin levels (>2 X ULN), followed by recovery upon atomoxetine discontinuation. In one patient, liver injury, manifested by elevated hepatic enzymes up to 40 X ULN and jaundice with bilirubin up to 12 X ULN, recurred upon rechallenge, and was followed by recovery upon drug discontinuation, providing evidence that Atomoxetine likely caused the liver injury. Such reactions may occur several months after therapy is started, but laboratory abnormalities may continue to worsen for several weeks after drug is stopped. The patient described above recovered from his liver injury, and did not require a liver transplant.
- Atomoxetine should be discontinued in patients with jaundice or laboratory evidence of liver injury, and should not be restarted. Laboratory testing to determine liver enzyme levels should be done upon the first symptom or sign of liver dysfunction (e.g., pruritus, dark urine, jaundice, right upper quadrant tenderness, or unexplained “flu like” symptoms).
- Serious Cardiovascular Events
- Sudden Death and Pre-existing Structural Cardiac Abnormalities or Other Serious Heart Problems
- Children and Adolescents — Sudden death has been reported in association with atomoxetine treatment at usual doses in children and adolescents with structural cardiac abnormalities or other serious heart problems. Although some serious heart problems alone carry an increased risk of sudden death, atomoxetine generally should not be used in children or adolescents with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, or other serious cardiac problems that may place them at increased vulnerability to the noradrenergic effects of atomoxetine.
- Adults — Sudden deaths, stroke, and myocardial infarction have been reported in adults taking atomoxetine at usual doses for ADHD. Although the role of atomoxetine in these adult cases is also unknown, adults have a greater likelihood than children of having serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, coronary artery disease, or other serious cardiac problems. Consideration should be given to not treating adults with clinically significant cardiac abnormalities.
- Assessing Cardiovascular Status in Patients being Treated with Atomoxetine
- Children, adolescents, or adults who are being considered for treatment with atomoxetine should have a careful history (including assessment for a family history of sudden death or ventricular arrhythmia) and physical exam to assess for the presence of cardiac disease, and should receive further cardiac evaluation if findings suggest such disease (e.g., electrocardiogram and echocardiogram). Patients who develop symptoms such as exertional chest pain, unexplained syncope, or other symptoms suggestive of cardiac disease during atomoxetine treatment should undergo a prompt cardiac evaluation.
- Effects on Blood Pressure and Heart Rate
- Atomoxetine should be used with caution in patients whose underlying medical conditions could be worsened by increases in blood pressure or heart rate such as certain patients with hypertension, tachycardia, or cardiovascular or cerebrovascular disease. It should not be used in patients with severe cardiac or vascular disorders whose condition would be expected to deteriorate if they experienced clinically important increases in blood pressure or heart rate. Pulse and blood pressure should be measured at baseline, following Atomoxetine dose increases, and periodically while on therapy to detect possible clinically important increases.
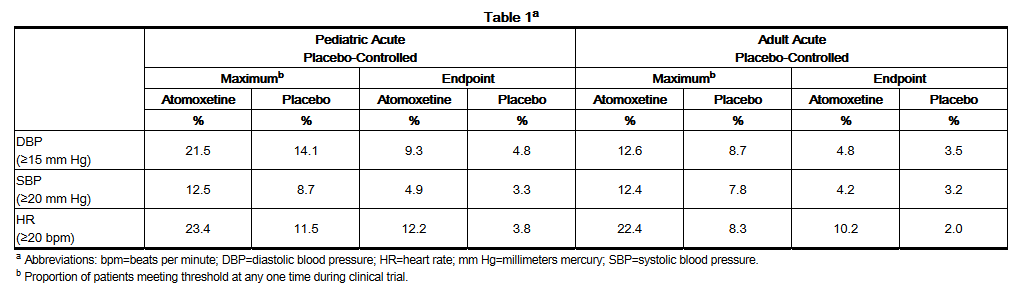
- The following table provides short-term, placebo-controlled clinical trial data for the proportions of patients having an increase in: diastolic blood pressure ≥15 mm Hg; systolic blood pressure ≥20 mm Hg; heart rate greater than or equal to 20 bpm, in both the pediatric and adult populations (see Table 1).
- In placebo-controlled registration studies involving pediatric patients, tachycardia was identified as an adverse event for 0.3% (5/1597) of these Atomoxetine patients compared with 0% (0/934) of placebo patients. The mean heart rate increase in extensive metabolizer (EM) patients was 5.0 beats/minute, and in poor metabolizer (PM) patients 9.4 beats/minute.
- In adult clinical trials where EM/PM status was available, the mean heart rate increase in PM patients was significantly higher than in EM patients (11 beats/minute versus 7.5 beats/minute). The heart rate effects could be clinically important in some PM patients.
- In placebo-controlled registration studies involving adult patients, tachycardia was identified as an adverse event for 1.5% (8/540) of Atomoxetine patients compared with 0.5% (2/402) of placebo patients.
- In adult clinical trials where EM/PM status was available, the mean change from baseline in diastolic blood pressure in PM patients was higher than in EM patients (4.21 versus 2.13 mm Hg) as was the mean change from baseline in systolic blood pressure (PM: 2.75 versus EM: 2.40 mm Hg). The blood pressure effects could be clinically important in some PM patients.
- Orthostatic hypotension and syncope have been reported in patients taking Atomoxetine. In child and adolescent registration studies, 0.2% (12/5596) of Atomoxetine-treated patients experienced orthostatic hypotension and 0.8% (46/5596) experienced syncope. In short-term child and adolescent registration studies, 1.8% (6/340) of Atomoxetine-treated patients experienced orthostatic hypotension compared with 0.5% (1/207) of placebo-treated patients. Syncope was not reported during short-term child and adolescent placebo-controlled ADHD registration studies. Atomoxetine should be used with caution in any condition that may predispose patients to hypotension, or conditions associated with abrupt heart rate or blood pressure changes.
- Emergence of New Psychotic or Manic Symptoms
- Treatment emergent psychotic or manic symptoms, e.g., hallucinations, delusional thinking, or mania in children and adolescents without a prior history of psychotic illness or mania can be caused by atomoxetine at usual doses. If such symptoms occur, consideration should be given to a possible causal role of atomoxetine, and discontinuation of treatment should be considered. In a pooled analysis of multiple short-term, placebo-controlled studies, such symptoms occurred in about 0.2% (4 patients with reactions out of 1939 exposed to atomoxetine for several weeks at usual doses) of atomoxetine-treated patients compared to 0 out of 1056 placebo-treated patients.
- Screening Patients for Bipolar Disorder
- In general, particular care should be taken in treating ADHD in patients with comorbid bipolar disorder because of concern for possible induction of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with Atomoxetine, patients with comorbid depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression.
- Aggressive Behavior or Hostility
- Patients beginning treatment for ADHD should be monitored for the appearance or worsening of aggressive behavior or hostility. Aggressive behavior or hostility is often observed in children and adolescents with ADHD. In pediatric short-term controlled clinical trials, 21/1308 (1.6%) of atomoxetine patients versus 9/806 (1.1%) of placebo-treated patients spontaneously reported treatment emergent hostility-related adverse events (overall risk ratio of 1.33 [95% C.I. 0.67-2.64 – not statistically significant]). In adult placebo-controlled clinical trials, 6/1697 (0.35%) of atomoxetine patients versus 4/1560 (0.26%) of placebo-treated patients spontaneously reported treatment emergent hostility-related adverse events (overall risk ratio of 1.38 [95% C.I. 0.39-4.88 – not statistically significant]). Although this is not conclusive evidence that Atomoxetine causes aggressive behavior or hostility, these behaviors were more frequently observed in clinical trials among children, adolescents, and adults treated with Atomoxetine compared to placebo.
- Allergic Events
- Although uncommon, allergic reactions, including anaphylactic reactions, angioneurotic edema, urticaria, and rash, have been reported in patients taking Atomoxetine.
- Effects on Urine Outflow from the Bladder
- In adult ADHD controlled trials, the rates of urinary retention (1.7%, 9/540) and urinary hesitation (5.6%, 30/540) were increased among atomoxetine subjects compared with placebo subjects (0%, 0/402 ; 0.5%, 2/402, respectively). Two adult atomoxetine subjects and no placebo subjects discontinued from controlled clinical trials because of urinary retention. A complaint of urinary retention or urinary hesitancy should be considered potentially related to atomoxetine.
- Priapism
- Rare postmarketing cases of priapism, defined as painful and nonpainful penile erection lasting more than 4 hours, have been reported for pediatric and adult patients treated with Atomoxetine. The erections resolved in cases in which follow-up information was available, some following discontinuation of Atomoxetine. Prompt medical attention is required in the event of suspected priapism.
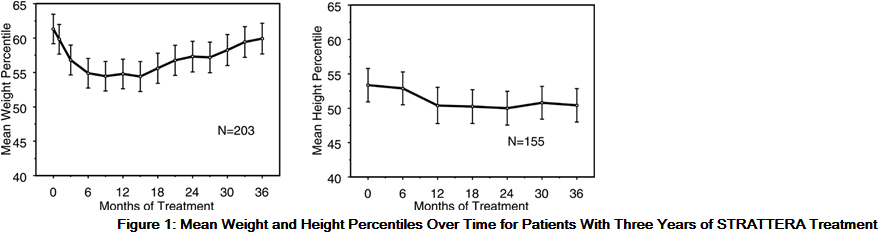
- Effects on Growth
- Data on the long-term effects of Atomoxetine on growth come from open-label studies, and weight and height changes are compared to normative population data. In general, the weight and height gain of pediatric patients treated with Atomoxetine lags behind that predicted by normative population data for about the first 9-12 months of treatment. Subsequently, weight gain rebounds and at about 3 years of treatment, patients treated with Atomoxetine have gained 17.9 kg on average, 0.5 kg more than predicted by their baseline data. After about 12 months, gain in height stabilizes, and at 3 years, patients treated with Atomoxetine have gained 19.4 cm on average, 0.4 cm less than predicted by their baseline data (see Figure 1 below).
- This growth pattern was generally similar regardless of pubertal status at the time of treatment initiation. Patients who were pre-pubertal at the start of treatment (girls ≤8 years old, boys ≤9 years old) gained an average of 2.1 kg and 1.2 cm less than predicted after three years. Patients who were pubertal (girls >8 to ≤13 years old, boys >9 to ≤14 years old) or late pubertal (girls >13 years old, boys >14 years old) had average weight and height gains that were close to or exceeded those predicted after three years of treatment.
- Growth followed a similar pattern in both extensive and poor metabolizers (EMs, PMs). PMs treated for at least two years gained an average of 2.4 kg and 1.1 cm less than predicted, while EMs gained an average of 0.2 kg and 0.4 cm less than predicted.
- In short-term controlled studies (up to 9 weeks), Atomoxetine-treated patients lost an average of 0.4 kg and gained an average of 0.9 cm, compared to a gain of 1.5 kg and 1.1 cm in the placebo-treated patients. In a fixed-dose controlled trial, 1.3%, 7.1%, 19.3%, and 29.1% of patients lost at least 3.5% of their body weight in the placebo, 0.5, 1.2, and 1.8 mg/kg/day dose groups.
- Growth should be monitored during treatment with Atomoxetine.
- Laboratory Tests
- Routine laboratory tests are not required.
- CYP2D6 metabolism — Poor metabolizers (PMs) of CYP2D6 have a 10-fold higher AUC and a 5-fold higher peak concentration to a given dose of Atomoxetine compared with extensive metabolizers (EMs). Approximately 7% of a Caucasian population are PMs. Laboratory tests are available to identify CYP2D6 PMs. The blood levels in PMs are similar to those attained by taking strong inhibitors of CYP2D6. The higher blood levels in PMs lead to a higher rate of some adverse effects of Atomoxetine.
- Concomitant Use of Potent CYP2D6 Inhibitors or Use in patients who are known to be CYP2D6 PMs
- Atomoxetine is primarily metabolized by the CYP2D6 pathway to 4-hydroxyatomoxetine. Dosage adjustment of Atomoxetine may be necessary when coadministered with potent CYP2D6 inhibitors (e.g., paroxetine, fluoxetine, and quinidine) or when administered to CYP2D6 PMs.
Adverse Reactions
Clinical Trials Experience
- Atomoxetine was administered to 5382 children or adolescent patients with ADHD and 1007 adults with ADHD in clinical studies. During the ADHD clinical trials, 1625 children and adolescent patients were treated for longer than 1 year and 2529 children and adolescent patients were treated for over 6 months.
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Child and Adolescent Clinical Trials
- Reasons for discontinuation of treatment due to adverse reactions in child and adolescent clinical trials — In acute child and adolescent placebo-controlled trials, 3.0% (48/1613) of atomoxetine subjects and 1.4% (13/945) placebo subjects discontinued for adverse reactions. For all studies, (including open-label and long-term studies), 6.3% of extensive metabolizer (EM) patients and 11.2% of poor metabolizer (PM) patients discontinued because of an adverse reaction. Among Atomoxetine-treated patients, irritability (0.3%, N=5); somnolence (0.3%, N=5); aggression (0.2%, N=4); nausea (0.2%, N=4); vomiting (0.2%, N=4); abdominal pain (0.2%, N=4); constipation (0.1%, N=2); fatigue (0.1%, N=2); feeling abnormal (0.1%, N=2); and headache (0.1%, N=2) were the reasons for discontinuation reported by more than 1 patient.
- Seizures — Atomoxetine has not been systematically evaluated in pediatric patients with seizure disorder as these patients were excluded from clinical studies during the product's premarket testing. In the clinical development program, seizures were reported in 0.2% (12/5073) of children whose average age was 10 years (range 6 to 16 years). In these clinical trials, the seizure risk among poor metabolizers was 0.3% (1/293) compared to 0.2% (11/4741) for extensive metabolizers.
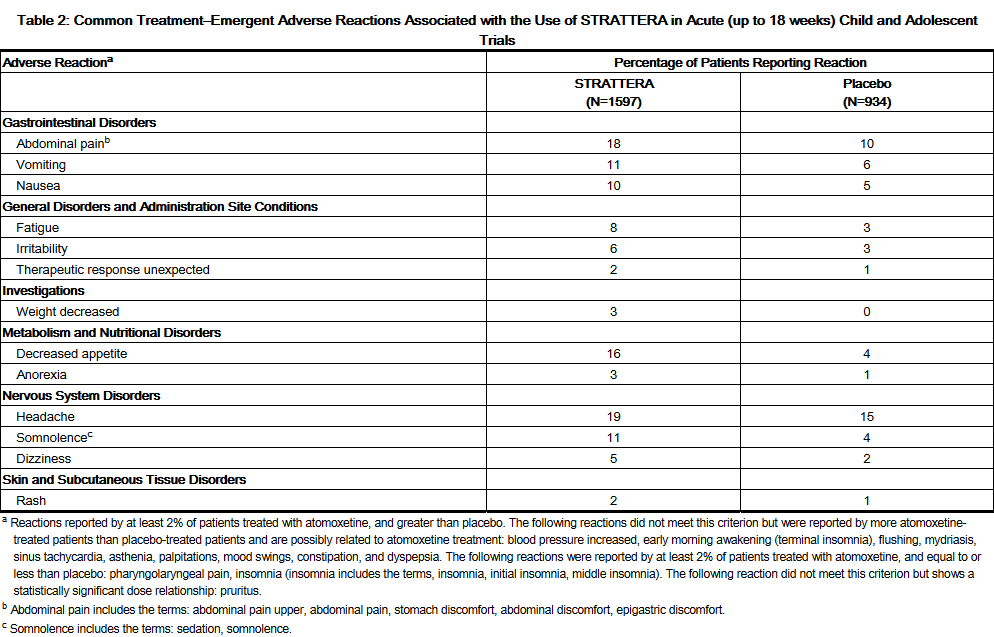
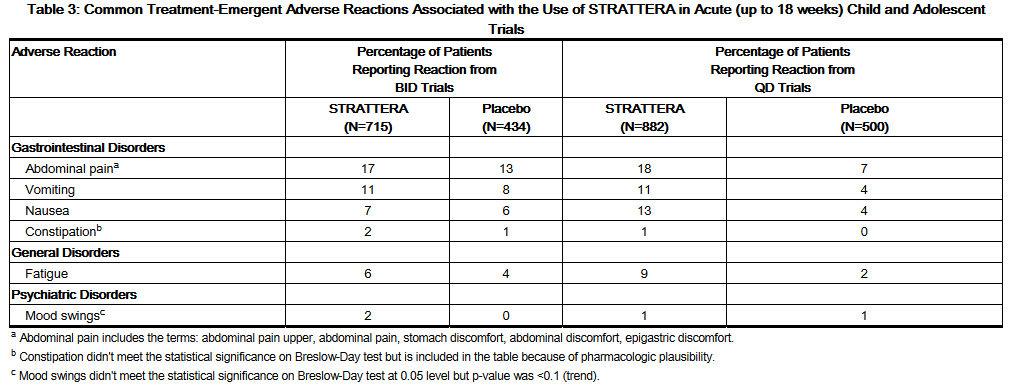
- Commonly observed adverse reactions in acute child and adolescent, placebo-controlled trials — Commonly observed adverse reactions associated with the use of Atomoxetine (incidence of 2% or greater) and not observed at an equivalent incidence among placebo-treated patients (Atomoxetine incidence greater than placebo) are listed in Table 2. Results were similar in the BID and the QD trial except as shown in Table 3, which shows both BID and QD results for selected adverse reactions based on statistically significant Breslow-Day tests. The most commonly observed adverse reactions in patients treated with Atomoxetine (incidence of 5% or greater and at least twice the incidence in placebo patients, for either BID or QD dosing) were: nausea, vomiting, fatigue, decreased appetite, abdominal pain, and somnolence (see Tables 2 and 3).
- Additional data from ADHD clinical trials (controlled and uncontrolled) has shown that approximately 5 to 10% of pediatric patients experienced potentially clinically important changes in heart rate (≥20 beats per min) or blood pressure (≥15 to 20 mm Hg).
- The following adverse reactions occurred in at least 2% of child and adolescent CYP2D6 PM patients and were statistically significantly more frequent in PM patients compared with CYP2D6 EM patients: insomnia (11% of PMs, 6% of EMs); weight decreased (7% of PMs, 4% of EMs); constipation (7% of PMs, 4% of EMs); depression (7% of PMs, 4% of EMs); tremor (5% of PMs, 1% of EMs); excoriation (4% of PMs, 2% of EMs); middle insomnia (3% of PMs, 1% of EMs); conjunctivitis (3% of PMs, 1% of EMs); syncope (3% of PMs, 1% of EMs); early morning awakening (2% of PMs, 1% of EMs); mydriasis (2% of PMs, 1% of EMs); sedation (4% of PMs, 2% of EMs).
- Depression includes the following terms: depression, major depression, depressive symptoms, depressed mood, dysphoria.
Adult Clinical Trials
- Reasons for discontinuation of treatment due to adverse reactions in acute adult placebo-controlled trials — In the acute adult placebo-controlled trials, 11.3% (61/541) atomoxetine subjects and 3.0% (12/405) placebo subjects discontinued for adverse reactions. Among Atomoxetine-treated patients, insomnia (0.9%, N=5); nausea (0.9%, N=5); chest pain (0.6%, N=3); fatigue (0.6%, N=3); anxiety (0.4%, N=2); erectile dysfunction (0.4%, N=2); mood swings (0.4%, N=2); nervousness (0.4%, N=2); palpitations (0.4%, N=2); and urinary retention (0.4%, N=2) were the reasons for discontinuation reported by more than 1 patient.
- Seizures — Atomoxetine has not been systematically evaluated in adult patients with a seizure disorder as these patients were excluded from clinical studies during the product's premarket testing. In the clinical development program, seizures were reported on 0.1% (1/748) of adult patients. In these clinical trials, no poor metabolizers (0/43) reported seizures compared to 0.1% (1/705) for extensive metabolizers.
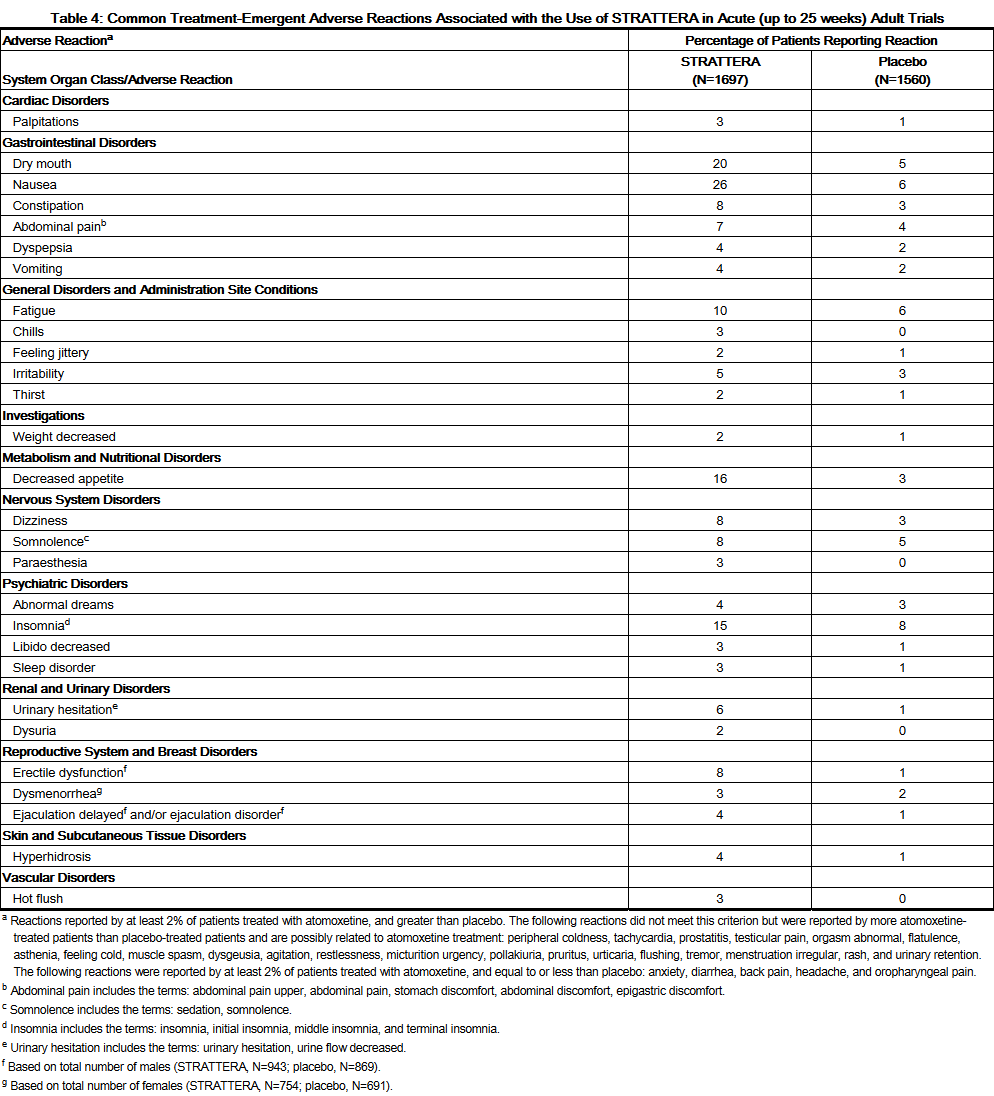
- Commonly observed adverse reactions in acute adult placebo-controlled trials — Commonly observed adverse reactions associated with the use of Atomoxetine (incidence of 2% or greater) and not observed at an equivalent incidence among placebo-treated patients (Atomoxetine incidence greater than placebo) are listed in Table 4. The most commonly observed adverse reactions in patients treated with Atomoxetine (incidence of 5% or greater and at least twice the incidence in placebo patients) were: constipation, dry mouth, nausea, decreased appetite, dizziness, erectile dysfunction, and urinary hesitation (see Table 4).
- Additional data from ADHD clinical trials (controlled and uncontrolled) has shown that approximately 5 to 10% of adult patients experienced potentially clinically important changes in heart rate (≥20 beats per min) or blood pressure (≥15 to 20 mm Hg).
- The following adverse events occurred in at least 2% of adult CYP2D6 poor metaboliser (PM) patients and were statistically significantly more frequent in PM patients compared to CYP2D6 extensive metaboliser (EM) patients: vision blurred (4% of PMs, 1% of EMs); dry mouth (35% of PMs, 17% of EMs); constipation (11% of PMs, 7% of EMs); feeling jittery (5% of PMs, 2% of EMs); decreased appetite (23% of PMs, 15% of EMs); tremor (5% of PMs, 1% of EMs); insomnia (19% of PMs, 11% of EMs); sleep disorder (7% of PMs, 3% of EMs); middle insomnia (5% of PMs, 3% of EMs); terminal insomnia (3% of PMs, 1% of EMs); urinary retention (6% of PMs, 1% of EMs); erectile dysfunction (21% of PMs, 9% of EMs); ejaculation disorder (6% of PMs, 2% of EMs); hyperhidrosis(15% of PMs, 7% of EMs); peripheral coldness (3% of PMs, 1% of EMs).
- Male and female sexual dysfunction — Atomoxetine appears to impair sexual function in some patients. Changes in sexual desire, sexual performance, and sexual satisfaction are not well assessed in most clinical trials because they need special attention and because patients and physicians may be reluctant to discuss them. Accordingly, estimates of the incidence of untoward sexual experience and performance cited in product labeling are likely to underestimate the actual incidence. Table 4 above displays the incidence of sexual side effects reported by at least 2% of adult patients taking Atomoxetine in placebo-controlled trials.
- There are no adequate and well-controlled studies examining sexual dysfunction with Atomoxetine treatment. While it is difficult to know the precise risk of sexual dysfunction associated with the use of Atomoxetine, physicians should routinely inquire about such possible side effects.
Postmarketing Experience
- The following adverse reactions have been identified during post approval use of Atomoxetine. Unless otherwise specified, these adverse reactions have occurred in adults and children and adolescents. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular system
Peripheral vascular effects
General disorders and administration site conditions
Nervous system disorders
Hypoaesthesia; paraesthesia in children and adolescents; sensory disturbances; tics.
Psychiatric disorders
Depression and depressed mood; anxiety, libido changes.
- Seizures
- Seizures have been reported in the postmarketing period. The postmarketing seizure cases include patients with pre-existing seizure disorders and those with identified risk factors for seizures, as well as patients with neither a history of nor identified risk factors for seizures. The exact relationship between Atomoxetine and seizures is difficult to evaluate due to uncertainty about the background risk of seizures in ADHD patients.
Skin and subcutaneous tissue disorders
Urogenital system
Male pelvic pain; urinary hesitation in children and adolescents; urinary retention in children and adolescents.
Drug Interactions
- Monoamine Oxidase Inhibitors
- With other drugs that affect brain monoamine concentrations, there have been reports of serious, sometimes fatal reactions (including hyperthermia, rigidity, myoclonus, autonomic instability with possible rapid fluctuations of vital signs, and mental status changes that include extreme agitation progressing to delirium and coma) when taken in combination with an MAOI. Some cases presented with features resembling neuroleptic malignant syndrome. Such reactions may occur when these drugs are given concurrently or in close proximity.
- Effect of CYP2D6 Inhibitors on Atomoxetine
- In extensive metabolizers (EMs), inhibitors of CYP2D6 (e.g., paroxetine, fluoxetine, and quinidine) increase atomoxetine steady-state plasma concentrations to exposures similar to those observed in poor metabolizers (PMs). In EM individuals treated with paroxetine or fluoxetine, the AUC of atomoxetine is approximately 6- to 8-fold and Css, max is about 3- to 4-fold greater than atomoxetine alone.
- In vitro studies suggest that coadministration of cytochrome P450 inhibitors to PMs will not increase the plasma concentrations of atomoxetine.
- Antihypertensive Drugs and Pressor Agents
- Because of possible effects on blood pressure, Atomoxetine should be used cautiously with antihypertensive drugs and pressor agents (e.g., dopamine, dobutamine) or other drugs that increase blood pressure.
- Albuterol
- Atomoxetine should be administered with caution to patients being treated with systemically-administered (oral or intravenous) albuterol (or other beta2 agonists) because the action of albuterol on the cardiovascular system can be potentiated resulting in increases in heart rate and blood pressure. Albuterol (600 mcg iv over 2 hours) induced increases in heart rate and blood pressure. These effects were potentiated by atomoxetine (60 mg BID for 5 days) and were most marked after the initial coadministration of albuterol and atomoxetine. However, these effects on heart rate and blood pressure were not seen in another study after the coadministration with inhaled dose of albuterol (200-800 mcg) and atomoxetine (80 mg QD for 5 days) in 21 healthy Asian subjects who were excluded for poor metabolizer status.
- Effect of Atomoxetine on P450 Enzymes
- Atomoxetine did not cause clinically important inhibition or induction of cytochrome P450 enzymes, including CYP1A2, CYP3A, CYP2D6, and CYP2C9.
- CYP3A Substrate (e.g., Midazolam) — Coadministration of Atomoxetine (60 mg BID for 12 days) with midazolam, a model compound for CYP3A4 metabolized drugs (single dose of 5 mg), resulted in 15% increase in AUC of midazolam. No dose adjustment is recommended for drugs metabolized by CYP3A.
- CYP2D6 Substrate (e.g., Desipramine) — Coadministration of Atomoxetine (40 or 60 mg BID for 13 days) with desipramine, a model compound for CYP2D6 metabolized drugs (single dose of 50 mg), did not alter the pharmacokinetics of desipramine. No dose adjustment is recommended for drugs metabolized by CYP2D6.
- Alcohol
- Consumption of ethanol with Atomoxetine did not change the intoxicating effects of ethanol.
- Methylphenidate
- Coadministration of methylphenidate with Atomoxetine did not increase cardiovascular effects beyond those seen with methylphenidate alone.
- Drugs Highly Bound to Plasma Protein
- In vitro drug-displacement studies were conducted with atomoxetine and other highly-bound drugs at therapeutic concentrations. Atomoxetine did not affect the binding of warfarin, acetylsalicylic acid, phenytoin, or diazepam to human albumin. Similarly, these compounds did not affect the binding of atomoxetine to human albumin.
- Drugs that Affect Gastric pH
- Drugs that elevate gastric pH (magnesium hydroxide/aluminum hydroxide, omeprazole) had no effect on Atomoxetine bioavailability.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- Pregnant rabbits were treated with up to 100 mg/kg/day of atomoxetine by gavage throughout the period of organogenesis. At this dose, in 1 of 3 studies, a decrease in live fetuses and an increase in early resorptions was observed. Slight increases in the incidences of atypical origin of carotid artery and absent subclavian artery were observed. These findings were observed at doses that caused slight maternal toxicity. The no-effect dose for these findings was 30 mg/kg/day. The 100 mg/kg dose is approximately 23 times the maximum human dose on a mg/m2 basis; plasma levels (AUC) of atomoxetine at this dose in rabbits are estimated to be 3.3 times (extensive metabolizers) or 0.4 times (poor metabolizers) those in humans receiving the maximum human dose.
- Rats were treated with up to approximately 50 mg/kg/day of atomoxetine (approximately 6 times the maximum human dose on a mg/m2 basis) in the diet from 2 weeks (females) or 10 weeks (males) prior to mating through the periods of organogenesis and lactation. In 1 of 2 studies, decreases in pup weight and pup survival were observed. The decreased pup survival was also seen at 25 mg/kg (but not at 13 mg/kg). In a study in which rats were treated with atomoxetine in the diet from 2 weeks (females) or 10 weeks (males) prior to mating throughout the period of organogenesis, a decrease in fetal weight (female only) and an increase in the incidence of incomplete ossification of the vertebral arch in fetuses were observed at 40 mg/kg/day (approximately 5 times the maximum human dose on a mg/m2 basis) but not at 20 mg/kg/day.
- No adverse fetal effects were seen when pregnant rats were treated with up to 150 mg/kg/day (approximately 17 times the maximum human dose on a mg/m2 basis) by gavage throughout the period of organogenesis.
- No adequate and well-controlled studies have been conducted in pregnant women. Atomoxetine should not be used during pregnancy unless the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Atomoxetine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Atomoxetine during labor and delivery.
Nursing Mothers
- Atomoxetine and/or its metabolites were excreted in the milk of rats. It is not known if atomoxetine is excreted in human milk. Caution should be exercised if Atomoxetine is administered to a nursing woman.
Pediatric Use
- Anyone considering the use of Atomoxetine in a child or adolescent must balance the potential risks with the clinical need.
- The pharmacokinetics of atomoxetine in children and adolescents are similar to those in adults. The safety, efficacy, and pharmacokinetics of Atomoxetine in pediatric patients less than 6 years of age have not been evaluated.
- A study was conducted in young rats to evaluate the effects of atomoxetine on growth and neurobehavioral and sexual development. Rats were treated with 1, 10, or 50 mg/kg/day (approximately 0.2, 2, and 8 times, respectively, the maximum human dose on a mg/m2 basis) of atomoxetine given by gavage from the early postnatal period (Day 10 of age) through adulthood. Slight delays in onset of vaginal patency (all doses) and preputial separation (10 and 50 mg/kg), slight decreases in epididymal weight and sperm number (10 and 50 mg/kg), and a slight decrease in corpora lutea (50 mg/kg) were seen, but there were no effects on fertility or reproductive performance. A slight delay in onset of incisor eruption was seen at 50 mg/kg. A slight increase in motor activity was seen on Day 15 (males at 10 and 50 mg/kg and females at 50 mg/kg) and on Day 30 (females at 50 mg/kg) but not on Day 60 of age. There were no effects on learning and memory tests. The significance of these findings to humans is unknown.
Geriatic Use
There is no FDA guidance on the use of Atomoxetine with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Atomoxetine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Atomoxetine with respect to specific racial populations.
Renal Impairment
- EM subjects with end stage renal disease had higher systemic exposure to atomoxetine than healthy subjects (about a 65% increase), but there was no difference when exposure was corrected for mg/kg dose. Atomoxetine can therefore be administered to ADHD patients with end stage renal disease or lesser degrees of renal insufficiency using the normal dosing regimen.
Hepatic Impairment
- Atomoxetine exposure (AUC) is increased, compared with normal subjects, in EM subjects with moderate (Child-Pugh Class B) (2-fold increase) and severe (Child-Pugh Class C) (4-fold increase) hepatic insufficiency. Dosage adjustment is recommended for patients with moderate or severe hepatic insufficiency.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Atomoxetine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Atomoxetine in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Atomoxetine in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Atomoxetine in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- No fatal overdoses occurred in clinical trials. There is limited clinical trial experience with Atomoxetine overdose. During postmarketing, there have been fatalities reported involving a mixed ingestion overdose of Atomoxetine and at least one other drug. There have been no reports of death involving overdose of Atomoxetine alone, including intentional overdoses at amounts up to 1400 mg. In some cases of overdose involving Atomoxetine, seizures have been reported. The most commonly reported symptoms accompanying acute and chronic overdoses of Atomoxetine were gastrointestinal symptoms, somnolence, dizziness, tremor, and abnormal behavior. Hyperactivity and agitation have also been reported. Signs and symptoms consistent with mild to moderate sympathetic nervous system activation (e.g., tachycardia, blood pressure increased, mydriasis, dry mouth) have also been observed. Most events were mild to moderate. Less commonly, there have been reports of QT prolongation and mental changes, including disorientation and hallucinations.
Management
- Consult with a Certified Poison Control Center for up to date guidance and advice. Because atomoxetine is highly protein-bound, dialysis is not likely to be useful in the treatment of overdose.
Chronic Overdose
There is limited information regarding Chronic Overdose of Atomoxetine in the drug label.
Pharmacology
Mechanism of Action
- The precise mechanism by which atomoxetine produces its therapeutic effects in Attention-Deficit/Hyperactivity Disorder (ADHD) is unknown, but is thought to be related to selective inhibition of the pre-synaptic norepinephrine transporter, as determined in ex vivo uptake and neurotransmitter depletion studies.
Structure
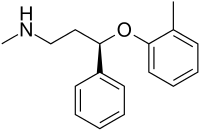
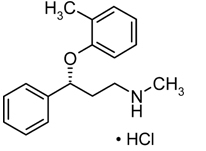
- Atomoxetine® (atomoxetine) is a selective norepinephrine reuptake inhibitor. Atomoxetine HCl is the R(-) isomer as determined by x-ray diffraction. The chemical designation is (-)-N-Methyl-3-phenyl-3-(o-tolyloxy)-propylamine hydrochloride. The molecular formula is C17H21NO•HCl, which corresponds to a molecular weight of 291.82. The chemical structure is:
- Atomoxetine HCl is a white to practically white solid, which has a solubility of 27.8 mg/mL in water.
- Atomoxetine capsules are intended for oral administration only.
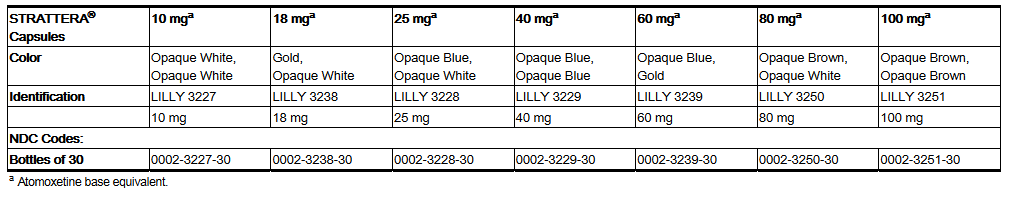
- Each capsule contains atomoxetine HCl equivalent to 10, 18, 25, 40, 60, 80, or 100 mg of atomoxetine. The capsules also contain pregelatinized starch and dimethicone. The capsule shells contain gelatin, sodium lauryl sulfate, and other inactive ingredients. The capsule shells also contain one or more of the following:
- FD&C Blue No. 2, synthetic yellow iron oxide, titanium dioxide, red iron oxide. The capsules are imprinted with edible black ink.
Pharmacodynamics
- An exposure-response analysis encompassing doses of atomoxetine (0.5, 1.2 or 1.8 mg/kg/day) or placebo demonstrated atomoxetine exposure correlates with efficacy as measured by the Attention-Deficit/Hyperactivity Disorder Rating Scale-IV-Parent Version: Investigator administered and scored. The exposure-efficacy relationship was similar to that observed between dose and efficacy with median exposures at the two highest doses resulting in near maximal changes from baseline.
- Cardiac Electrophysiology — The effect of Atomoxetine on QT prolongation was evaluated in a randomized, double-blinded, positive-(moxifloxacin 400 mg) and placebo-controlled, cross-over study in healthy male CYP2D6 poor metabolizers. A total of 120 healthy subjects were administered Atomoxetine (20 mg and 60 mg) twice daily for 7 days. No large changes in QTc interval (i.e., increases >60 msec from baseline, absolute QTc >480 msec) were observed in the study. However, small changes in QTc interval cannot be excluded from the current study, because the study failed to demonstrate assay sensitivity. There was a slight increase in QTc interval with increased atomoxetine concentration.
Pharmacokinetics
- Atomoxetine is well-absorbed after oral administration and is minimally affected by food. It is eliminated primarily by oxidative metabolism through the cytochrome P450 2D6 (CYP2D6) enzymatic pathway and subsequent glucuronidation. Atomoxetine has a half-life of about 5 hours. A fraction of the population (about 7% of Caucasians and 2% of African Americans) are poor metabolizers (PMs) of CYP2D6 metabolized drugs. These individuals have reduced activity in this pathway resulting in 10-fold higher AUCs, 5-fold higher peak plasma concentrations, and slower elimination (plasma half-life of about 24 hours) of atomoxetine compared with people with normal activity [extensive metabolizers (EMs)]. Drugs that inhibit CYP2D6, such as fluoxetine, paroxetine, and quinidine, cause similar increases in exposure.
- The pharmacokinetics of atomoxetine have been evaluated in more than 400 children and adolescents in selected clinical trials, primarily using population pharmacokinetic studies. Single-dose and steady-state individual pharmacokinetic data were also obtained in children, adolescents, and adults. When doses were normalized to a mg/kg basis, similar half-life, Cmax, and AUC values were observed in children, adolescents, and adults. Clearance and volume of distribution after adjustment for body weight were also similar.
- Absorption and distribution — Atomoxetine is rapidly absorbed after oral administration, with absolute bioavailability of about 63% in EMs and 94% in PMs. Maximal plasma concentrations (Cmax) are reached approximately 1 to 2 hours after dosing.
- Atomoxetine can be administered with or without food. Administration of Atomoxetine with a standard high-fat meal in adults did not affect the extent of oral absorption of atomoxetine (AUC), but did decrease the rate of absorption, resulting in a 37% lower Cmax, and delayed Tmax by 3 hours. In clinical trials with children and adolescents, administration of Atomoxetine with food resulted in a 9% lower Cmax.
- The steady-state volume of distribution after intravenous administration is 0.85 L/kg indicating that atomoxetine distributes primarily into total body water. Volume of distribution is similar across the patient weight range after normalizing for body weight.
- At therapeutic concentrations, 98% of atomoxetine in plasma is bound to protein, primarily albumin.
- Metabolism and elimination — Atomoxetine is metabolized primarily through the CYP2D6 enzymatic pathway. People with reduced activity in this pathway (PMs) have higher plasma concentrations of atomoxetine compared with people with normal activity (EMs). For PMs, AUC of atomoxetine is approximately 10-fold and Css, max is about 5-fold greater than EMs. Laboratory tests are available to identify CYP2D6 PMs. Coadministration of Atomoxetine with potent inhibitors of CYP2D6, such as fluoxetine, paroxetine, or quinidine, results in a substantial increase in atomoxetine plasma exposure, and dosing adjustment may be necessary. Atomoxetine did not inhibit or induce the CYP2D6 pathway.
- The major oxidative metabolite formed, regardless of CYP2D6 status, is 4-hydroxyatomoxetine, which is glucuronidated. 4-Hydroxyatomoxetine is equipotent to atomoxetine as an inhibitor of the norepinephrine transporter but circulates in plasma at much lower concentrations (1% of atomoxetine concentration in EMs and 0.1% of atomoxetine concentration in PMs). 4-Hydroxyatomoxetine is primarily formed by CYP2D6, but in PMs, 4-hydroxyatomoxetine is formed at a slower rate by several other cytochrome P450 enzymes. N-Desmethylatomoxetine is formed by CYP2C19 and other cytochrome P450 enzymes, but has substantially less pharmacological activity compared with atomoxetine and circulates in plasma at lower concentrations (5% of atomoxetine concentration in EMs and 45% of atomoxetine concentration in PMs).
- Mean apparent plasma clearance of atomoxetine after oral administration in adult EMs is 0.35 L/hr/kg and the mean half-life is 5.2 hours. Following oral administration of atomoxetine to PMs, mean apparent plasma clearance is 0.03 L/hr/kg and mean half-life is 21.6 hours. For PMs, AUC of atomoxetine is approximately 10-fold and Css, max is about 5-fold greater than EMs. The elimination half-life of 4-hydroxyatomoxetine is similar to that of N-desmethylatomoxetine (6 to 8 hours) in EM subjects, while the half-life of N-desmethylatomoxetine is much longer in PM subjects (34 to 40 hours).
- Atomoxetine is excreted primarily as 4-hydroxyatomoxetine-O-glucuronide, mainly in the urine (greater than 80% of the dose) and to a lesser extent in the feces (less than 17% of the dose). Only a small fraction of the Atomoxetine dose is excreted as unchanged atomoxetine (less than 3% of the dose), indicating extensive biotransformation.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenesis — Atomoxetine HCl was not carcinogenic in rats and mice when given in the diet for 2 years at time-weighted average doses up to 47 and 458 mg/kg/day, respectively. The highest dose used in rats is approximately 8 and 5 times the maximum human dose in children and adults, respectively, on a mg/m2 basis. Plasma levels (AUC) of atomoxetine at this dose in rats are estimated to be 1.8 times (extensive metabolizers) or 0.2 times (poor metabolizers) those in humans receiving the maximum human dose. The highest dose used in mice is approximately 39 and 26 times the maximum human dose in children and adults, respectively, on a mg/m2 basis.
- Mutagenesis — Atomoxetine HCl was negative in a battery of genotoxicity studies that included a reverse point mutation assay (Ames Test), an in vitro mouse lymphoma assay, a chromosomal aberration test in Chinese hamster ovary cells, an unscheduled DNA synthesis test in rat hepatocytes, and an in vivo micronucleus test in mice. However, there was a slight increase in the percentage of Chinese hamster ovary cells with diplochromosomes, suggesting endoreduplication (numerical aberration).
- The metabolite N-desmethylatomoxetine HCl was negative in the Ames Test, mouse lymphoma assay, and unscheduled DNA synthesis test.
- Impairment of fertility — Atomoxetine HCl did not impair fertility in rats when given in the diet at doses of up to 57 mg/kg/day, which is approximately 6 times the maximum human dose on a mg/m2 basis.
Clinical Studies
ADHD studies in Children and Adolescents
- Acute Studies — The effectiveness of Atomoxetine in the treatment of ADHD was established in 4 randomized, double-blind, placebo-controlled studies of pediatric patients (ages 6 to 18). Approximately one-third of the patients met DSM-IV criteria for inattentive subtype and two-thirds met criteria for both inattentive and hyperactive/impulsive subtypes.
- Signs and symptoms of ADHD were evaluated by a comparison of mean change from baseline to endpoint for Atomoxetine- and placebo-treated patients using an intent-to-treat analysis of the primary outcome measure, the investigator administered and scored ADHD Rating Scale-IV-Parent Version (ADHDRS) total score including hyperactive/impulsive and inattentive subscales. Each item on the ADHDRS maps directly to one symptom criterion for ADHD in the DSM-IV.
- In Study 1, an 8-week randomized, double-blind, placebo-controlled, dose-response, acute treatment study of children and adolescents aged 8 to 18 (N=297), patients received either a fixed dose of Atomoxetine (0.5, 1.2, or 1.8 mg/kg/day) or placebo. Atomoxetine was administered as a divided dose in the early morning and late afternoon/early evening. At the 2 higher doses, improvements in ADHD symptoms were statistically significantly superior in Atomoxetine-treated patients compared with placebo-treated patients as measured on the ADHDRS scale. The 1.8 mg/kg/day Atomoxetine dose did not provide any additional benefit over that observed with the 1.2 mg/kg/day dose. The 0.5 mg/kg/day Atomoxetine dose was not superior to placebo.
- In Study 2, a 6-week randomized, double-blind, placebo-controlled, acute treatment study of children and adolescents aged 6 to 16 (N=171), patients received either Atomoxetine or placebo. Atomoxetine was administered as a single dose in the early morning and titrated on a weight-adjusted basis according to clinical response, up to a maximum dose of 1.5 mg/kg/day. The mean final dose of Atomoxetine was approximately 1.3 mg/kg/day. ADHD symptoms were statistically significantly improved on Atomoxetine compared with placebo, as measured on the ADHDRS scale. This study shows that Atomoxetine is effective when administered once daily in the morning.
- In 2 identical, 9-week, acute, randomized, double-blind, placebo-controlled studies of children aged 7 to 13 (Study 3, N=147; Study 4, N=144), Atomoxetine and methylphenidate were compared with placebo. Atomoxetine was administered as a divided dose in the early morning and late afternoon (after school) and titrated on a weight-adjusted basis according to clinical response. The maximum recommended Atomoxetine dose was 2.0 mg/kg/day. The mean final dose of Atomoxetine for both studies was approximately 1.6 mg/kg/day. In both studies, ADHD symptoms statistically significantly improved more on Atomoxetine than on placebo, as measured on the ADHDRS scale.
- Examination of population subsets based on gender and age (<12 and 12 to 17) did not reveal any differential responsiveness on the basis of these subgroupings. There was not sufficient exposure of ethnic groups other than Caucasian to allow exploration of differences in these subgroups.
- Maintenance Study — The effectiveness of Atomoxetine in the maintenance treatment of ADHD was established in an outpatient study of children and adolescents (ages 6-15 years). Patients meeting DSM-IV criteria for ADHD who showed continuous response for about 4 weeks during an initial 10 week open-label treatment phase with Atomoxetine (1.2 to 1.8 mg/kg/day) were randomized to continuation of their current dose of Atomoxetine (N=292) or to placebo (N=124) under double-blind treatment for observation of relapse. Response during the open-label phase was defined as CGI-ADHD-S score ≤2 and a reduction of at least 25% from baseline in ADHDRS-IV-Parent:Inv total score. Patients who were assigned to Atomoxetine and showed continuous response for approximately 8 months during the first double-blind treatment phase were again randomized to continuation of their current dose of Atomoxetine (N=81) or to placebo (N=82) under double-blind treatment for observation of relapse. Relapse during the double-blind phase was defined as CGI-ADHD-S score increases of at least 2 from the end of open-label phase and ADHDRS-IV-Parent:Inv total score returns to ≥90% of study entry score for 2 consecutive visits. In both double-blind phases, patients receiving continued Atomoxetine treatment experienced significantly longer times to relapse than those receiving placebo.
ADHD studies in Adults
- The effectiveness of Atomoxetine in the treatment of ADHD was established in 2 randomized, double-blind, placebo-controlled clinical studies of adult patients, age 18 and older, who met DSM-IV criteria for ADHD.
- Signs and symptoms of ADHD were evaluated using the investigator-administered Conners Adult ADHD Rating Scale Screening Version (CAARS), a 30-item scale. The primary effectiveness measure was the 18-item Total ADHD Symptom score (the sum of the inattentive and hyperactivity/impulsivity subscales from the CAARS) evaluated by a comparison of mean change from baseline to endpoint using an intent-to-treat analysis.
- In 2 identical, 10-week, randomized, double-blind, placebo-controlled acute treatment studies (Study 5, N=280; Study 6, N=256), patients received either Atomoxetine or placebo. Atomoxetine was administered as a divided dose in the early morning and late afternoon/early evening and titrated according to clinical response in a range of 60 to 120 mg/day. The mean final dose of Atomoxetine for both studies was approximately 95 mg/day. In both studies, ADHD symptoms were statistically significantly improved on Atomoxetine, as measured on the ADHD Symptom score from the CAARS scale.
- Examination of population subsets based on gender and age (<42 and ≥42) did not reveal any differential responsiveness on the basis of these subgroupings. There was not sufficient exposure of ethnic groups other than Caucasian to allow exploration of differences in these subgroups.
How Supplied
- Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F).
Storage
There is limited information regarding Atomoxetine Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Atomoxetine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Atomoxetine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
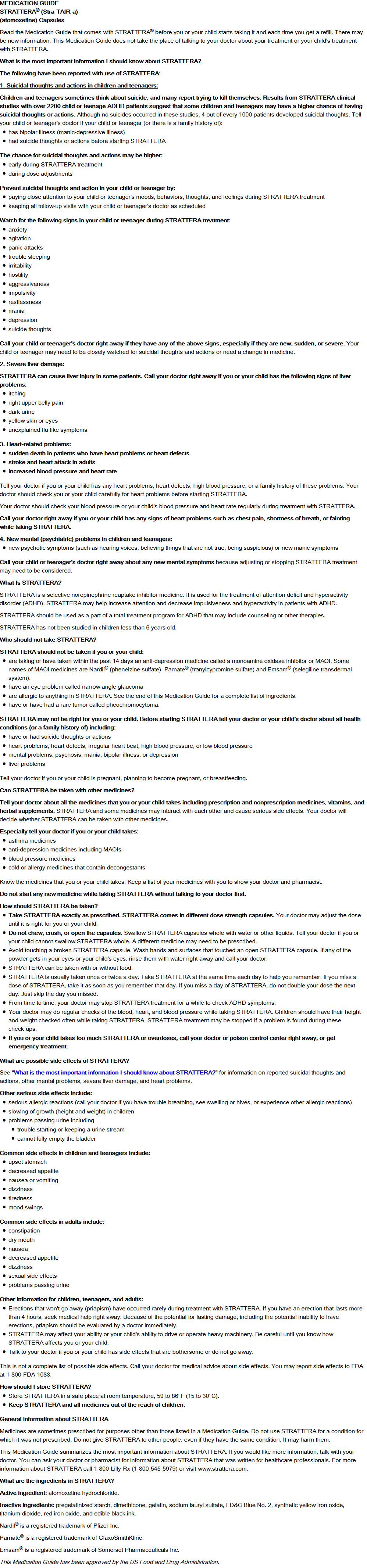
Patient Counseling Information
General Information
- Physicians should instruct their patients to read the Medication Guide before starting therapy with Atomoxetine and to reread it each time the prescription is renewed.
- Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with Atomoxetine and should counsel them in its appropriate use. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have.
- Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking Atomoxetine.
Suicide Risk
- Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, depression, and suicidal ideation, especially early during Atomoxetine treatment and when the dose is adjusted. Families and caregivers of patients should be advised to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Severe Liver Injury
- Patients initiating Atomoxetine should be cautioned that severe liver injury may develop. Patients should be instructed to contact their physician immediately should they develop pruritus, dark urine, jaundice, right upper quadrant tenderness, or unexplained “flu-like” symptoms.
Aggression or Hostility
- Patients should be instructed to call their doctor as soon as possible should they notice an increase in aggression or hostility.
Priapism
- Rare postmarketing cases of priapism, defined as painful and nonpainful penile erection lasting more than 4 hours, have been reported for pediatric and adult patients treated with Atomoxetine. The parents or guardians of pediatric patients taking Atomoxetine and adult patients taking Atomoxetine should be instructed that priapism requires prompt medical attention.
Ocular Irritant
- Atomoxetine is an ocular irritant. Atomoxetine capsules are not intended to be opened. In the event of capsule content coming in contact with the eye, the affected eye should be flushed immediately with water, and medical advice obtained. Hands and any potentially contaminated surfaces should be washed as soon as possible.
Drug-Drug Interaction
- Patients should be instructed to consult a physician if they are taking or plan to take any prescription or over-the-counter medicines, dietary supplements, or herbal remedies.
Pregnancy
- Patients should be instructed to consult a physician if they are nursing, pregnant, or thinking of becoming pregnant while taking Atomoxetine.
Food
- Patients may take Atomoxetine with or without food.
Missed Dose
- If patients miss a dose, they should be instructed to take it as soon as possible, but should not take more than the prescribed total daily amount of Atomoxetine in any 24-hour period.
Interference with Psychomotor Performance
- Patients should be instructed to use caution when driving a car or operating hazardous machinery until they are reasonably certain that their performance is not affected by atomoxetine.
Precautions with Alcohol
- Alcohol-Atomoxetine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- STRATTERA®[4]
Look-Alike Drug Names
There is limited information regarding Atomoxetine Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 1.2 1.3 1.4 "atomoxetine (Rx) - Atomoxetine". Medscape Reference. WebMD. Retrieved 10 November 2013.
- ↑ 2.0 2.1 2.2 2.3 2.4
- ↑ 3.0 3.1 3.2 3.3 3.4 "ATOMOXETINE HYDROCHLORIDE capsule [Mylan Pharmaceuticals Inc.]". DailyMed. Mylan Pharmaceuticals Inc. October 2011. Retrieved 10 November 2013.
- ↑ "STRATTERA(atomoxetine hydrochloride) capsule Atomoxetine (atomoxetine hydrochloride) kit [Eli Lilly and Company ]".
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023227.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3227;10;mg |Pill Dosage=10 mg |Pill Color=White|+sep=; |Pill Shape=Capsule |Pill Size (mm)=16 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023227
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023228.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3228;25;mg |Pill Dosage=25 mg |Pill Color=White;Blue|+sep=; |Pill Shape=Capsule |Pill Size (mm)=16 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023228
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023229.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3229;40;mg |Pill Dosage=40 mg |Pill Color=Blue|+sep=; |Pill Shape=Capsule |Pill Size (mm)=16 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023229
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023238.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3238;18;mg |Pill Dosage=18 mg |Pill Color=White;Yellow|+sep=; |Pill Shape=Capsule |Pill Size (mm)=16 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023238
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023239.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3239;60;mg |Pill Dosage=60 mg |Pill Color=Blue;Yellow|+sep=; |Pill Shape=Capsule |Pill Size (mm)=18 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023239
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023250.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3250;80;mg |Pill Dosage=80 mg |Pill Color=White;Brown|+sep=; |Pill Shape=Capsule |Pill Size (mm)=18 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023250
}}
{{#subobject:
|Page Name=Atomoxetine |Pill Name=Strattera_NDC_00023251.jpg |Drug Name=Strattera |Pill Ingred=Atomoxetine hydrochloride[Atomoxetine]|+sep=; |Pill Imprint=LILLY;3251;100;mg |Pill Dosage=100 mg |Pill Color=Brown|+sep=; |Pill Shape=Capsule |Pill Size (mm)=20 |Pill Scoring=1 |Pill Image= |Drug Author=Eli Lilly and Company |NDC=00023251
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine06.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine07.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine08.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine09.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine10.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine11.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine12.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine13.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine14.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine15.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine16.png
}}
{{#subobject:
|Label Page=Atomoxetine |Label Name=Atomoxetine16(1).png
}}