Squamous cell carcinoma of the skin: Difference between revisions
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
==[[Squamous cell carcinoma screening|Screening]]== | ==[[Squamous cell carcinoma screening|Screening]]== | ||
==[[Squamous cell carcinoma causes of squamous cell carcinoma|Causes of Squamous cell carcinoma]]== | ==[[Squamous cell carcinoma causes of squamous cell carcinoma|Causes of Squamous cell carcinoma]]== | ||
Revision as of 21:37, 11 June 2012
For patient information click here
Template:DiseaseDisorder infobox
|
Squamous cell carcinoma of the skin Microchapters |
|
Differentiating Squamous cell carcinoma of the skin from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Squamous cell carcinoma of the skin On the Web |
|
American Roentgen Ray Society Images of Squamous cell carcinoma of the skin |
|
Directions to Hospitals Treating Squamous cell carcinoma of the skin |
|
Risk calculators and risk factors for Squamous cell carcinoma of the skin |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Govindavarjhulla, M.B.B.S. [2], Raviteja Guddeti, M.B.B.S. [3]
Overview
Historical Aspects
Pathophysiology
Epidemiology and Demographics
Risk Factors
Screening
Causes of Squamous cell carcinoma
Related conditions
- Erythroplasia of Queyrat
- Keratoacanthoma is a low-grade malignancy of the skin. It originates in the pilo-sebaceous glands, and is similar in clinical presentation and microscopic analysis to squamous cell carcinoma, except that it contains a central keratin plug. Statistically, it is less likely to become invasive than squamous cell carcinoma.
- Bowen's disease is a sunlight-induced skin disease, and is considered to be an early form of squamous cell carcinoma.
- Marjolin's ulcer is a type of squamous cell carcinoma that arises from a non-healing ulcer or burn wound.
- Melanoma
- Basal Cell Carcinoma
Terminology
A carcinoma can be characterized as either in situ (confined to the original site) or invasive.
Clinical features
Approximately 200,000 cases of cutaneous squamous cell carcinoma occur in the US per year resulting in ~2000 deaths (Miller and Weinstock, 1994). Excessive ultraviolet radiation exposure, immunosuppression, human papilloma virus infection, certain chronic dermatoses, and topical arsenic exposure are all risk factors for developing squamous cell carcinoma (Schwartz and Stoll, 1999). Solid organ transplant recipients commonly develop squamous cell carcinoma in the setting of immunosuppression and in some instances develop several hundred separate primary tumors over the span of a several years (Jensen et al., 1999).
Most squamous cell carcinomas arise on the sun-damaged skin of the head and neck, with fewer lesions arising on the extremities and occasional tumors occurring on the trunk. Early lesions frequently present as a red, scaly spots. Later lesions may form nodules or firm plaques, either of which can ulcerate ( http://tray.dermatology.uiowa.edu). Diagnosis is established by biopsy and histopathological confirmation. Complete excision is curative in the vast majority of cases. Occasionally squamous cell carcinoma will invade along the perineural layer of peripheral nerves and will extend well beyond the clinically apparent mass. Local recurrence is more common in these instances and when present on the head, direct intracranial extension may occur. Metastases to draining lymph nodes occurs in a minority of cases and disseminated disease is the cause of most squamous cell carcinoma-related deaths. Higher rates of metastasis (~15%) are observed with primary lesions of the lips or ears (Rowe et al., 1992). Radiation therapy is helpful in some cases of locally recurrent disease in which complete resection is difficult to achieve and in cases of limited metastatic disease.
Pathology
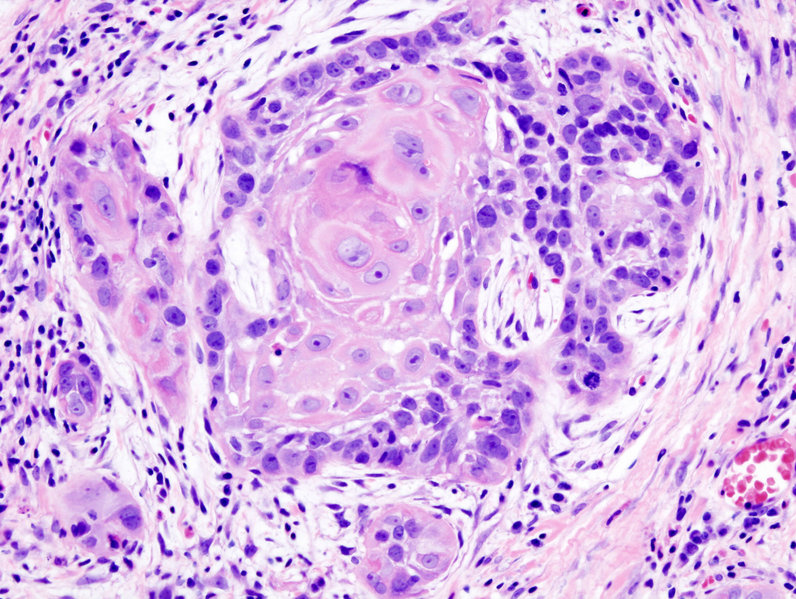
The development of squamous cell carcinoma is frequently a multistep process. Early lesions tend to be either actinic keratoses, with atypia of the basal keratinocytic layer of the epidermis or squamous cell carcinoma in situ, in which keratinocytic atypia spans the full thickness epidermis.
These precursors are frequently present adjacent to invasive squamous cell carcinomas which invade the dermis as nests, islands, or cords squamous cells with or occasionally as individual cells. Several grading schemes have been developed for squamous cell carcinoma and incorporate the extent of keratinization (a form of differentiation) and nuclear atypia (Broders, 1932). A widely used scheme divides tumors into well, moderately, or poorly differentiated.
Although poorly differentiated tumors tend to behave more aggressively, well-differentiated tumors can also give rise to metastasis and result in death. Several histologic variants of squamous cell carcinoma have been documented, including verrucous, spindle cell and pseudovascular.
Frequently an actinic keratosis or squamous cell carcinoma overlies the invasive component and the two are focally contiguous. Occasionally squamous tumors arise rapidly, have a crater-form morphology and spontaneously regress. These tumors are known as keratoacanthomas. Some craterform squamous lesions do not regress, but continue to invade and grow and represent invasive squamous cell carcinomas.
Signs & Symptoms
- The lesion caused by SCC is often asymptomatic
- Ulcer or reddish skin plaque that is slow growing
- Intermittent bleeding from the tumor, especially on the lip
- The clinical appearance is highly variable
- Usually the tumor presents as an ulcerated lesion with hard, raised edges
- The tumor may be in the form of a hard plaque or a papule, often with an opalescent quality, with telangiectasia
- The tumor can lie below the level of the surrounding skin, and eventually ulcerates and invades the underlying tissue
- The tumor commonly presents on sun-exposed areas (e.g. back of the hand, scalp, lip, and superior surface of pinna)
- On the lip, the tumor forms a small ulcer, which fails to heal and bleeds intermittently
- Evidence of chronic skin photodamage, such as multiple actinic keratoses (solar keratoses)
- The tumor grows relatively slowly
- Unlike basal cell carcinoma (BCC), squamous cell carcinoma (SCC) has a substantial risk of metastasis
- Risk of metastasis is higher in SCC arising in scars, on the lower lips or mucosa, and occurring in immunosupressed patients. About *one-third of lingual and mucosal tumors metastasize before diagnosis (these are often related to tobacco and alcohol use)
Diagnosis
Diagnosis is via a biopsy. For the skin, look under skin biopsy.
The pathological appearance of a squamous cell cancer varies with the depth of the biopsy. For that reason, a biopsy including the subcutanous tissue and basalar epithelium, to the surface is necessary for correct diagnosis. The performance of a shave biopsy (see skin biopsy) might not acquire enough information for a diagnosis. An excision biopsy is ideal, but not practical in most cases. An incisional or punch biopsy is preferred. A shave biopsy is least ideal, especially if only the superficial portion is acquired.
Physical Examination
Skin
Squamous cell carcinoma of the skin is often caused by long term exposure to the sun. To be diagnosed, a biopsy is done where a sample is taken and examined under a microscope by a Pathologist. If it is found to be cancerous, a surgery is done to remove it.
Squamous cell carcinomas account for about 20% of non-melanoma skin cancers, (with basal cell carcinomas accounting for about 80%), and are clinically more significant because of their ability to metastasize. Squamous cell carcinoma is usually developed in the epithelial layer of the skin and sometimes in various mucous membranes of the body.
Squamous cell carcinoma is the second most common cancer of the skin (after basal cell carcinoma but more common than melanoma). It usually occurs in areas exposed to the sun, and can generally be treated by excision or mohs surgery only.
Sunlight exposure and immunosuppression are risk factors for SCC of the skin with chronic sun exposure being the strongest environmental risk factor.[1] The risk of metastasis is low, but is much higher than basal cell carcinoma.
Squamous cell cancers of the lip and ears have high metastatic and recurrence rate (20 to 50%)[2]. Squamous cell cancers of the skin in individuals on immunotherapy or having lymphoproliferative disorders (leukemias) are much more aggressive, regardless of their location.[3]
Australian scientist Ian Frazer who developed the cervical cancer vaccine, says that animal tests have been effective in preventing squamous cell carcinoma in animals, and there may be a human vaccine against this kind of skin cancer within the decade.[4]
Ear Nose and Throat
-
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Squamous cell carcinoma in oral cavity.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
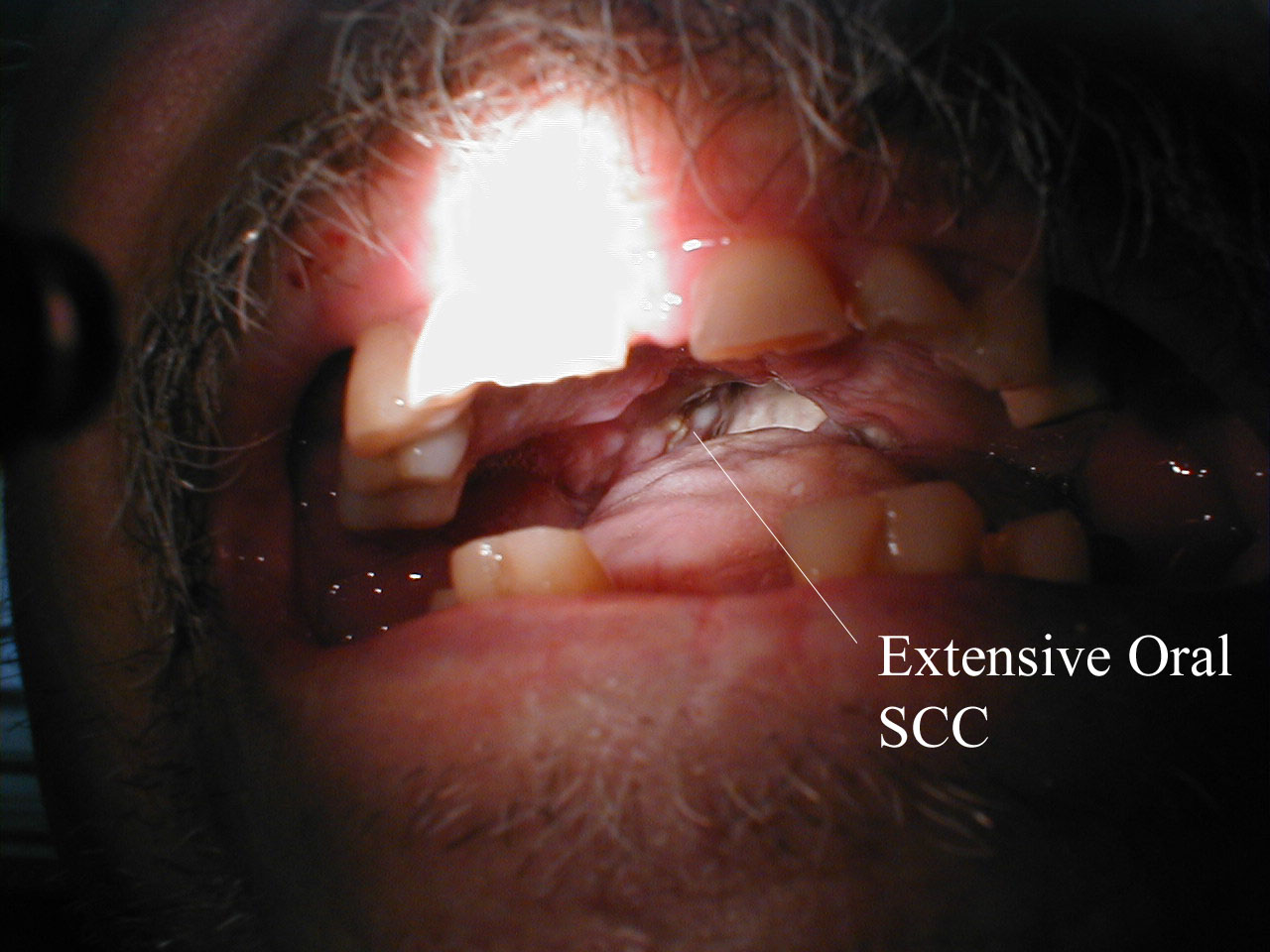
-
Squamous Cell Cancer of the Mouth: Irregular, necrotic appearing tissue on the inside of the mouth due to extensive squamous cell cancer. Patient has limited ability to open his mouth (aka trismus) as a result of the infiltrating cancer.
-
Squamous Cell Cancer, Base of Tongue: Note white area with swelling, right base of tongue.
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
-
Squamous Cell Cancer of the Mouth: Cancer that began along the lower gum line has spread to left submandibular lymph nodes.
Esophagus
Esophageal cancer may be due to either squamous cell carcinoma (ESCC) or adenocarcinoma (EAC). SCCs tend to occur closer to the mouth, while adenocarcinomas occur closer to the stomach. Dysphagia (difficulty swallowing, solids worse than liquids) and odynophagia are common initial symptoms. If the disease is localized, esophagectomy may offer the possibility of a cure. If the disease has spread, chemotherapy and radiotherapy are commonly used.
Penis
When squamous cell carcinoma in situ (Bowen's disease) is found on the penis, it is called erythroplasia of Queyrat[10]. This type of cancer respond very well to an experimental agent called Aldara.
Prostate
When associated with the prostate, squamous cell carcinoma is very aggressive in nature. It is difficult to detect as there is no increase in prostate specific antigen levels seen; meaning that the cancer is often diagnosed at an advanced stage.
Lung
When associated with the lung, it often causes ectopic production of parathyroid hormone-related protein (PTHrP), resulting in hypercalcemia.
-
Biopsy of a highly differentiated squamous cell carcinoma of the mouth. Haematoxylin & eosin stain.
-
Photograph of a squamous cell carcinoma. Tumour is on the left, obstructing the bronchus (lung). Beyond the tumour the bronchus is inflammed and contains mucus
Vagina and cervix
Vaginal squamous cell carcinoma spreads slowly and usually stays near the vagina, but may spread to the lungs and liver. This is the most common type of vaginal cancer.
Cervix: Squamous cell carcinoma
<youtube v=zB47nE-i8dQ/>
<youtube v=J3kULzKGzws/>
Experimental treatments
In 2007, Australian biopharmaceutical company Clinuvel Pharmaceuticals Limited began clinical trials with a melanocyte-stimulating hormone called melanotan (known by the International Nonproprietary Name afamelanotide, formerly CUV1647)[11] to provide photoprotection for organ transplant patients against squamous cell carcinoma of the skin and actinic keratosis.[12][13]
While Mohs surgery is frequently utilized and often considered the treatment of choice for squamous cell carcinoma of the skin, physicians have utilized the method for the treatment of squamous cell carcinoma of the mouth, throat, and neck.[14]
Aldara (Imiquimod) has been used with great success for squamous cell carcinoma in situ of the skin and the penis. After treatment, the skin resembles normal skin without the usual scarring and morbidity associated with standard excision. Imiquimod is not FDA approved for any squamous cell carcinoma.
References
- ↑
- ↑ http://www.aad.org/public/publications/pamphlets/sun_squamous.html
- ↑ http://www.skincarephysicians.com/skincancernet/squamous_cell_carcinoma.html
- ↑ Cosmos Online - Skin cancer vaccine within reach (http://www.cosmosmagazine.com/news/2327/skin-cancer-vaccine-within-reach)
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ http://www.ghorayeb.com
- ↑ http://www.ghorayeb.com
- ↑ http://www.ghorayeb.com
- ↑ http://www.emedicine.com/derm/TOPIC144.HTM
- ↑ "World Health Organisation assigns CUV1647 generic name" (PDF). Clinuvel. 2008. Retrieved 2008-06-17.
- ↑ Clinuvel » Investors » FAQs
- ↑ PharmaAsia - Clinuvel’s Drug Begins Global Phase II Skin Cancer Trials
- ↑ Gross, K.G., et al. Mohs Surgery, Fundamentals and Techniques. 1999, Mosby.
External links
- Information on Squamous Cell Carcinoma from The Skin Cancer Foundation
- Article by Stephen D Hess, MD, PhD
- DermNet NZ: Squamous cell carcinoma
- Squamous cell carcinoma in transplant recipients
Template:Tumors of bone, cartilage, skin, connective, and soft tissue Template:Respiratory and intrathoracic neoplasia Template:Genital neoplasia Template:Epithelial neoplasms
de:Plattenepithelkarzinom he:קרצינומת תאי קשקש nl:Plaveiselcelcarcinoom



![Squamous cell skin cancer.[5]](/images/1/17/Squamous_cell_skin_cancer.jpg)
![A large squamous cell carcinoma of the tongue[6]](/images/e/e9/Squamous_cell_carcinoma.jpg)
![This patient had two adjacent cancers. The flat black lesion below the antitragus is a malignant melanoma. The white elevated keratotic lesion is a squamous cell carcinoma [7].](/images/f/f4/AuricleMelanoma_SqCC.jpg)



![Recurrent squamous cell carcinoma of the auricle (far left) excised with a stellate incision across the antihelix[8].](/images/c/c8/Auriclesqccastellateexcision.jpg)
![The final result of the excision[9].](/images/c/cc/Auricle003.jpg)