Retropharyngeal abscess: Difference between revisions
Ahmed Younes (talk | contribs) |
Ahmed Younes (talk | contribs) |
||
| Line 193: | Line 193: | ||
|Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; [[ampicillin]]-[[sulbactam]] or [[clindamycin]]. | |Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; [[ampicillin]]-[[sulbactam]] or [[clindamycin]]. | ||
|} | |} | ||
Retropharyngeal abscess must be differentiated from other causes of dysphagia and fever. | |||
{| class="wikitable" | |||
!Variable | |||
! | |||
![[Croup]] | |||
![[Epiglottitis]] | |||
![[Pharyngitis]] | |||
![[Tracheitis|Bacterial tracheitis]] | |||
![[Tonsilitis]] | |||
![[Retropharyngeal abscess]] | |||
![[Subglottic stenosis]] | |||
|- | |||
| rowspan="4" |Presentation | |||
|[[Cough]] | |||
|✔ | |||
|<small>—</small> | |||
| rowspan="4" |[[Sore throat]], pain on swallowing, [[fever]], [[headache]], [[Abdominal pain|abdominal]] pain, [[nausea]] and [[vomiting]] | |||
| rowspan="4" |Barking [[cough]], [[stridor]], | |||
[[fever]], [[chest pain]], | |||
[[ear pain]], [[difficulty breathing]], [[headache]], [[dizziness]]. | |||
| rowspan="4" |[[Sore throat]], pain on swallowing, [[fever]], [[headache]], [[cough]] | |||
| rowspan="4" |[[Neck pain]], [[stiff neck]], [[torticollis]] | |||
[[fever]], [[malaise]], [[stridor]], and barking [[cough]] | |||
| rowspan="4" |Depends on severity. May have respiratory distress at birth, exercise-induced [[dyspnea]], intermittent [[wheezing]]. Inspiratory [[stridor]]. <ref name="pmid26132943">{{cite journal| author=Nussbaumer-Ochsner Y, Thurnheer R| title=IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis. | journal=N Engl J Med | year= 2015 | volume= 373 | issue= 1 | pages= 73 | pmid=26132943 | doi=10.1056/NEJMicm1404785 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26132943 }}</ref> | |||
|- | |||
|[[Stridor]] | |||
|✔ | |||
|✔ | |||
|- | |||
|[[Drooling]] | |||
|<small>—</small> | |||
|✔ | |||
|- | |||
| colspan="2" |Others are [[Hoarseness]], [[Difficulty breathing]], symptoms of the [[common cold]], [[Runny nose]], [[Fever]] | |||
|[[Difficulty breathing|Other symptoms include difficulty breathing]], [[Difficulty swallowing|fever, chills, difficulty swallowing]], [[hoarseness]] of voice | |||
|- | |||
|Causes | |||
| colspan="2" |[[Parainfluenza virus]] | |||
|[[Hemolysis|H. influenza type b, beta-hemolytic]] [[streptococci]], ''[[Staphylococcus aureus]],'' [[fungi]] and [[viruses]]. | |||
|[[Group A beta-hemolytic streptococci|Group A beta-hemolytic streptococcus]]. | |||
|[[Staphylococcus aureus]] | |||
|Most common cause is viral including [[adenovirus]], [[rhinovirus]], [[influenza]], [[coronavirus]], and [[respiratory syncytial virus]]. Second most common causes are bacterial; ''[[Group A streptococcal infection|Group A streptococcal bacteria]]'',<ref name="pmid3601520">{{cite journal |author=Putto A |title=Febrile exudative tonsillitis: viral or streptococcal? |journal=[[Pediatrics]] |volume=80 |issue=1 |pages=6–12 |year=1987 |pmid=3601520 |doi= |issn=}}</ref> | |||
|Polymicrobial infection. Mostly; [[Streptococcus pyogenes]], [[Staphylococcus aureus]] and respiratory anaerobes (example; Fusobacteria, [[Prevotella species|Prevotella]], and Veillonella species)<ref name="pmid23520072">{{cite journal| author=Cheng J, Elden L| title=Children with deep space neck infections: our experience with 178 children. | journal=Otolaryngol Head Neck Surg | year= 2013 | volume= 148 | issue= 6 | pages= 1037-42 | pmid=23520072 | doi=10.1177/0194599813482292 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23520072 }} </ref><ref name="pmid22481424">{{cite journal| author=Abdel-Haq N, Quezada M, Asmar BI| title=Retropharyngeal abscess in children: the rising incidence of methicillin-resistant Staphylococcus aureus. | journal=Pediatr Infect Dis J | year= 2012 | volume= 31 | issue= 7 | pages= 696-9 | pmid=22481424 | doi=10.1097/INF.0b013e318256fff0 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22481424 }} </ref><ref name="pmid18948832">{{cite journal| author=Inman JC, Rowe M, Ghostine M, Fleck T| title=Pediatric neck abscesses: changing organisms and empiric therapies. | journal=Laryngoscope | year= 2008 | volume= 118 | issue= 12 | pages= 2111-4 | pmid=18948832 | doi=10.1097/MLG.0b013e318182a4fb | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18948832 }} </ref><ref name="pmid15573356">{{cite journal| author=Brook I| title=Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=J Oral Maxillofac Surg | year= 2004 | volume= 62 | issue= 12 | pages= 1545-50 | pmid=15573356 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15573356 }} </ref><ref name="pmid18427007">{{cite journal| author=Wright CT, Stocks RM, Armstrong DL, Arnold SR, Gould HJ| title=Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess. | journal=Arch Otolaryngol Head Neck Surg | year= 2008 | volume= 134 | issue= 4 | pages= 408-13 | pmid=18427007 | doi=10.1001/archotol.134.4.408 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18427007 }} </ref><ref name="pmid2235179">{{cite journal| author=Asmar BI| title=Bacteriology of retropharyngeal abscess in children. | journal=Pediatr Infect Dis J | year= 1990 | volume= 9 | issue= 8 | pages= 595-7 | pmid=2235179 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2235179 }} </ref> | |||
|Congenital, trauma | |||
|- | |||
|Physical exams findings | |||
| colspan="2" |Suprasternal and [[intercostal]] [[Indrawing|indrawing,]]<ref name="pmid19445760">{{cite journal |vauthors=Johnson D |title=Croup |journal=BMJ Clin Evid |volume=2009 |issue= |pages= |year=2009 |pmid=19445760 |pmc=2907784 |doi= |url=}}</ref> Inspiratory [[stridor]]<ref name="Cherry2008">{{cite journal|last1=Cherry|first1=James D.|title=Croup|journal=New England Journal of Medicine|volume=358|issue=4|year=2008|pages=384–391|issn=0028-4793|doi=10.1056/NEJMcp072022}}</ref>, expiratory [[wheezing]],<ref name="Cherry2008">{{cite journal|last1=Cherry|first1=James D.|title=Croup|journal=New England Journal of Medicine|volume=358|issue=4|year=2008|pages=384–391|issn=0028-4793|doi=10.1056/NEJMcp072022}}</ref> [[Sternal]] wall retractions<ref name="pmid194457602">{{cite journal |vauthors=Johnson D |title=Croup |journal=BMJ Clin Evid |volume=2009 |issue= |pages= |year=2009 |pmid=19445760 |pmc=2907784 |doi= |url=}}</ref> | |||
|[[Cyanosis]], [[Cervical]] [[lymphadenopathy]], Inflammed [[epiglottis]] | |||
|Inflammed [[pharynx]] with or without [[exudate]] | |||
|Subglottic narrowing with purulent secretions in the trachea<ref name="pmid6869336">{{cite journal| author=Liston SL, Gehrz RC, Siegel LG, Tilelli J| title=Bacterial tracheitis. | journal=Am J Dis Child | year= 1983 | volume= 137 | issue= 8 | pages= 764-7 | pmid=6869336 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6869336 }} </ref><ref name="pmid7271556">{{cite journal| author=Liston SL, Gehrz RC, Jarvis CW| title=Bacterial tracheitis. | journal=Arch Otolaryngol | year= 1981 | volume= 107 | issue= 9 | pages= 561-4 | pmid=7271556 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7271556 }} </ref> | |||
|[[Fever]], especially 100°F or higher.<ref name="Tonsillitis">Tonsillitis. Medline Plus. https://www.nlm.nih.gov/medlineplus/ency/article/001043.htm. Accessed May 2nd, 2016.</ref><ref name="urlTonsillitis - NHS Choices">{{cite web |url=http://www.nhs.uk/Conditions/Tonsillitis/Pages/Introduction.aspx |title=Tonsillitis - NHS Choices |format= |work= |accessdate=}}</ref>[[Erythema]], [[edema]] and [[Exudate]] of the [[tonsils]].<ref name="pmid25587367">{{cite journal |vauthors=Stelter K |title=Tonsillitis and sore throat in children |journal=GMS Curr Top Otorhinolaryngol Head Neck Surg |volume=13 |issue= |pages=Doc07 |year=2014 |pmid=25587367 |pmc=4273168 |doi=10.3205/cto000110 |url=}}</ref> cervical [[lymphadenopathy]], [[Dysphonia]].<ref name="urlTonsillitis - Symptoms - NHS Choices">{{cite web |url=http://www.nhs.uk/Conditions/Tonsillitis/Pages/Symptoms.aspx |title=Tonsillitis - Symptoms - NHS Choices |format= |work= |accessdate=}}</ref> | |||
|Child may be unable to open the mouth widely. May have enlarged | |||
[[cervical]] [[lymph nodes]] and neck mass. | |||
|Signs of respiratory distress, intermittent [[wheezing]]. Inspiratory [[stridor]]. <ref name="pmid26132943" /> | |||
|- | |||
|Age commonly affected | |||
| colspan="2" |Mainly 6 months and 3 years old | |||
rarely, adolescents and adults<ref name="pmid8769531">{{cite journal| author=Tong MC, Chu MC, Leighton SE, van Hasselt CA| title=Adult croup. | journal=Chest | year= 1996 | volume= 109 | issue= 6 | pages= 1659-62 | pmid=8769531 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8769531 }}</ref> | |||
|Used to be mostly found in | |||
pediatric age group between 3 to 5 years, | |||
however, recent trend favors adults | |||
as most commonly affected individuals<ref name="pmid270310102">{{cite journal| author=Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED| title=Epiglottitis: It Hasn't Gone Away. | journal=Anesthesiology | year= 2016 | volume= 124 | issue= 6 | pages= 1404-7 | pmid=27031010 | doi=10.1097/ALN.0000000000001125 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27031010 }}</ref> | |||
with a mean age of 44.94 years. | |||
|Mostly in children and young adults, | |||
with 50% of cases identified | |||
between the ages of 5 to 24 years.<ref>{{cite book | last = Bennett | first = John | title = Mandell, Douglas, and Bennett's principles and practice of infectious diseases | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2015 | isbn = 978-1455748013 }}</ref> | |||
|Mostly during the first six years of life | |||
|Primarily affects children | |||
between 5 and 15 years old.<ref name="Oroface">{{cite book |last1=Sharav |first1=Yair |last2=Benoliel |first2=Rafael |date=2008 |title=Orofacial Pain and Headache |url= |location= |publisher=Elsevier |page= |isbn=0723434123}}</ref> | |||
|Mostly between 2-4 years, but can occur in other age groups.<ref name="pmid12777558">{{cite journal| author=Craig FW, Schunk JE| title=Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. | journal=Pediatrics | year= 2003 | volume= 111 | issue= 6 Pt 1 | pages= 1394-8 | pmid=12777558 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12777558 }}</ref><ref name="pmid1876473">{{cite journal| author=Coulthard M, Isaacs D| title=Neonatal retropharyngeal abscess. | journal=Pediatr Infect Dis J | year= 1991 | volume= 10 | issue= 7 | pages= 547-9 | pmid=1876473 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1876473 }}</ref> | |||
|May be congenital congenital or acquired. Mean age in acquired is 54.1 years<ref name="pmid28007041">{{cite journal| author=Nicolli EA, Carey RM, Farquhar D, Haft S, Alfonso KP, Mirza N| title=Risk factors for adult acquired subglottic stenosis. | journal=J Laryngol Otol | year= 2017 | volume= 131 | issue= 3 | pages= 264-267 | pmid=28007041 | doi=10.1017/S0022215116009798 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28007041 }}</ref> | |||
|- | |||
|Imaging finding | |||
| colspan="2" |[[Steeple sign]] on neck X-ray | |||
|[[Thumbprint sign]] on neck x-ray | |||
|<small>—</small> | |||
|Lateral neck xray shows intraluminal membranes and tracheal wall irregularity. | |||
|Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.<ref name="pmid26527518">{{cite journal| author=Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H et al.| title=Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy. | journal=Auris Nasus Larynx | year= 2016 | volume= 43 | issue= 2 | pages= 182-6 | pmid=26527518 | doi=10.1016/j.anl.2015.09.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26527518 }} </ref><ref name="pmid25946659">{{cite journal| author=Nogan S, Jandali D, Cipolla M, DeSilva B| title=The use of ultrasound imaging in evaluation of peritonsillar infections. | journal=Laryngoscope | year= 2015 | volume= 125 | issue= 11 | pages= 2604-7 | pmid=25946659 | doi=10.1002/lary.25313 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25946659 }} </ref><ref name="pmid25945805">{{cite journal| author=Fordham MT, Rock AN, Bandarkar A, Preciado D, Levy M, Cohen J et al.| title=Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess. | journal=Laryngoscope | year= 2015 | volume= 125 | issue= 12 | pages= 2799-804 | pmid=25945805 | doi=10.1002/lary.25354 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25945805 }} </ref> | |||
|On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen<ref name="pmid15667676">{{cite journal| author=Philpott CM, Selvadurai D, Banerjee AR| title=Paediatric retropharyngeal abscess. | journal=J Laryngol Otol | year= 2004 | volume= 118 | issue= 12 | pages= 919-26 | pmid=15667676 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15667676 }}</ref><ref name="pmid12761699">{{cite journal| author=Vural C, Gungor A, Comerci S| title=Accuracy of computerized tomography in deep neck infections in the pediatric population. | journal=Am J Otolaryngol | year= 2003 | volume= 24 | issue= 3 | pages= 143-8 | pmid=12761699 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12761699 }}</ref> | |||
|Bronchoscopy reveals subglottic stenosis. Computed tomography may reveal a concentric stenotic tracheal segment.<ref name="pmid261329432">{{cite journal| author=Nussbaumer-Ochsner Y, Thurnheer R| title=IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis. | journal=N Engl J Med | year= 2015 | volume= 373 | issue= 1 | pages= 73 | pmid=26132943 | doi=10.1056/NEJMicm1404785 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26132943 }}</ref> | |||
|- | |||
|Treatment | |||
| colspan="2" |[[Dexamethasone]] and nebulised [[epenephrine|epinephrine]] | |||
|Airway maintenance, p[[Parenteral|arenteral]] [[Cefotaxime]] or [[Ceftriaxone]] in combination with [[Vancomycin]]. Adjuvant therapy includes [[corticosteroids]] and racemic [[Epinephrine]].<ref name="pmid15983574">{{cite journal| author=Nickas BJ| title=A 60-year-old man with stridor, drooling, and "tripoding" following a nasal polypectomy. | journal=J Emerg Nurs | year= 2005 | volume= 31 | issue= 3 | pages= 234-5; quiz 321 | pmid=15983574 | doi=10.1016/j.jen.2004.10.015 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15983574 }}</ref><ref name="pmid12557859">{{cite journal| author=Wick F, Ballmer PE, Haller A| title=Acute epiglottis in adults. | journal=Swiss Med Wkly | year= 2002 | volume= 132 | issue= 37-38 | pages= 541-7 | pmid=12557859 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12557859 }}</ref> | |||
|[[Antimicrobial]] therapy mainly [[penicillin]]-based and [[analgesics]]. | |||
|Airway maintenance and antibiotics | |||
|[[Antimicrobial]] therapy mainly [[penicillin]]-based and [[analgesics]] with [[tonsilectomy]] in selected cases. | |||
|Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. | |||
|Endoscopic balloon dilation for patients with low-grade subglottic stenosis,<ref name="pmid27095722">{{cite journal| author=Cui PC, Luo JS, Zhao DQ, Guo ZH, Ma RN| title=[Management of subglottic stenosis in children with endoscopic balloon dilation]. | journal=Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi | year= 2016 | volume= 51 | issue= 4 | pages= 286-8 | pmid=27095722 | doi=10.3760/cma.j.issn.1673-0860.2016.04.009 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27095722 }}</ref> glucocorticoid injections, and resection.<ref name="pmid261329433">{{cite journal| author=Nussbaumer-Ochsner Y, Thurnheer R| title=IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis. | journal=N Engl J Med | year= 2015 | volume= 373 | issue= 1 | pages= 73 | pmid=26132943 | doi=10.1056/NEJMicm1404785 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26132943 }}</ref> | |||
|} | |||
==Diagnosis== | ==Diagnosis== | ||
Revision as of 21:13, 27 September 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Vishal Devarkonda, M.B.B.S[2]
Overview
Retropharyngeal space is a deep space in neck extending from the base of skull to the posterior mediastinum. Microorganisms can be introduced into this space either through lymphatic or direct or traumatic spread leading to cellulitis. Cellulitis may progress to form phlegmon, which in-turn progress to form mature abscess. Most common causes of retropharyngeal abscess are polymicrobial infections, beta-hemolytic streptococcus, Streptococcus pyogenes (group A streptococcus [GAS]), Staphylococcus aureus (including methicillin-resistant S. aureus [[[Methicillin resistant staphylococcus aureus infections|MRSA]]]), and respiratory anaerobes. Retropharyngeal abscess commonly affects children, median age being 4 years for children. Common complications of retropharyngeal abscess are life-threatening descending necrotizing mediastinitis, sepsis, internal jugular vein thrombophlebitis, and mediastinitis. Patients with retropharyngeal abscess may present with pain in neck, fever, sore throat, and mass in neck . Diagnosis of retropharyngeal abscess is based on clinical presentation supported by radio-graphic imaging. Management predominantly consists of empiric intravenous antibiotics or combination of surgical drainage and intravenous antibiotics.
Historical Perspective
- The exact origins of the disease is not clearly known. The term abscess is derived from latin term abscessus(meaning: act of going away)
- In 1926, Guthrie described a case of retropharyngeal abscess in childhood.[1]
- In 1946, Davidson described a case of retropharyngeal abscess in adults.[2]
Classification
There is no established classification system for retropharyngeal abscess.
Pathophysiology
The pathophysiology of retropharyngeal abscess can be discussed in following headings:[3][4][5][6][7][8][9][10][11][12]
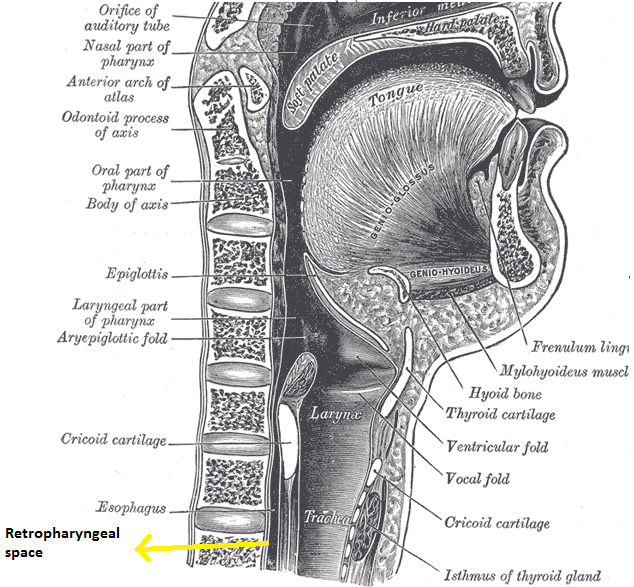
Anatomy of retropharyngeal space
Retropharyngeal space is a deep space of neck extending from the base of skull to the posterior mediastinum. Space is bordered anteriorly by middle layer of deep cervical fascia(buccopharyngeal fascia), posteriorly by deep layer of deep cervical fascia, laterally by carotid sheath containing carotid artery and jugular vein.
Transmission
Transmission of microorganisms into the retropharyngeal space could be through trauma or direct spread or lymphatic spread.
| Mode of transmission of infection to retropharyngeal space | |
|---|---|
| Lymphatic spread | Retropharyngeal space consists two pair of lymph nodes, which drains nasopharynx, adenoids, posterior para-nasal sinuses, middle ear, and eustachian tube. Draining lymph nodes may get inflamed/infected following an upper respiratory tract infection. Lymph node may undergo liquefaction necrosis, which my progress into retropharyngeal cellulitis, which left untreated can progress to abscess formation. However by age 4 years, these lymph nodes undergo spontaneous atrophy. |
| Direct spread/ Trauma | Adults
In adults, retropharyngeal space can be contaminated by direct trauma(eg, penetrating foreign trauma, endoscopy, dental procedures) or extension of local infection such as odontogenic infection, ludwig's angina, osteomyelitis of cervical spine. Children In children, retropharyngeal space can be contaminated by direct trauma to oropharynx(swallowing a foreign body or running and falling with an object in mouth). |
Immune response
Introduction of infections into retropharyngeal space either through lymphatic or direct or traumatic spread may lead to suppurative adenitis of retropharyngeal lymph nodes or cellulitis of retropharyngeal space. Cellulitis may progress to form phlegmon, which in-turn progress to form mature abscess.
Causes
Polymicrobial infection is often responsible for retropharyngeal abscess. The other organisms involved in causing retropharyngeal abscess include:[3][4][13][14][15][16][17]
Most common causes
- Poly-microbial infections
- Beta-hemolytic streptococcus
- Streptococcus pyogenes (group A streptococcus [GAS])
- Staphylococcus aureus (including methicillin-resistant S. aureus [MRSA])
- Prevotella
- Veillonella
Less common causes
- Haemophilus Influenzae
- Haemophilus parainfluenzae
- Neisseria species
- Bacteroides
- Fusobacterium
- Salmonella
- Mycobacterium
- Bartonella henselae
- Porphyromonas species
Epidemiology and Demographics
There are no comprehensive studies studying the epidemiology and demographics of retropharyngeal abscess worldwide.
Incidence
In United states, incidence of retropharyngeal abscess in kids under age 20 years is 4.10 per 100,000 population for year 2012.[18]
Case Fatality Rate
Case fatality rate for retropharyngeal abscess varies from study to study, it ranges from low of zero case fatalities(after reviewing the data from 1321 pediatric admissions with retropharyngeal abscess in year 2003) to high of 2.6% case fatalities(234 adults with deep space neck infections in adults).[19]
Age
Retropharyngeal abscess commonly affects children, with median age being 4 years for children.[20]
Gender
Retropharyngeal abscess is more commonly affects in males than in females. The gender ratio is approximately 1.63.[21]
Race
In year 2015, a comprehensive study analysed 6233 patients admitted to US hospitals with retropharyngeal abscess from year 2003 to 2012 and reported that for year 2012, 49.5% of the admitted patients were white, 19.2% were black, 21.9 % were hispanic and 9.5% were other race.[22]
Screening
There are no established screening guidelines to screen patients for retropharyngeal abscess.
Natural History, Complications, and Prognosis
Natural history
If left untreated or appropriate medial or surgical interventions are delayed, patients with retropharyngeal abscess may develop life threatening complications which include mediastinitis, sepsis and internal jugular vein thrombophlebitis.[3][4][5][6]
Complications
Complications of retropharyngeal abscess include:[23][24][25]
- Epidural abscess
- Mediastinitis
- Carotid artery aneurysm or erosion
- Internal jugular vein thrombophlebitis
- Septic pulmonary embolism
- Cranial nerve dysfunction (IX–XII)
- Cavernous sinus thrombosis
- Aspiration pneumonia
- Life-threatening descending necrotizing mediastinitis
- Sepsis
Prognosis
The prognosis of retropharyngeal abscess is good when detected early and appropriately treated. Relapse may occur in 1 to 5 percent of cases.[26][27]
Differentiating retropharyngeal abscess from other diseases
Differential diagnosis
Retropharyngeal abscess must be differentiated from other upper respiratory diseases and conditions that may cause throat pain and airway obstruction as shown in the table below:
| Disease/Variable | Presentation | Causes | Physical exams findings | Age commonly affected | Imaging finding | Treatment |
|---|---|---|---|---|---|---|
| Peritonsillar abscess | Severe sore throat, otalgia fever, a "hot potato" or muffled voice, drooling, and trismus[28] | Aerobic and anaerobic | Contralateral deflection of the uvula,
the tonsil is displaced inferiorly and medially, tender submandibular and anterior cervical lymph nodes, tonsillar hypertrophy with likely peritonsillar edema. |
The highest occurrence is in adults between 20 to 40 years of age.[28] | On ultrasound peritonsillar abscess appears as focal irregularly marginated hypoechoic area.[33][34][35][36][33][34] | Ampicillin-sulbactam, Clindamycin, Vancomycin or Linezolid |
| Croup | Has cough and stridor but no drooling. Others are Hoarseness, Difficulty breathing, symptoms of the common cold, Runny nose, Fever | Parainfluenza virus | Suprasternal and intercostal indrawing,[37] Inspiratory stridor[38], expiratory wheezing,[38] Sternal wall retractions[39] | Mainly 6 months and 3 years old
rarely, adolescents and adults[40] |
Steeple sign on neck X-ray | Dexamethasone and nebulised epinephrine |
| Epiglottitis | Stridor and drooling but no cough. Other symptoms include difficulty breathing, fever, chills, difficulty swallowing, hoarseness of voice | H. influenza type b, | Cyanosis, Cervical lymphadenopathy, Inflamed epiglottis | Used to be mostly found in
pediatric age group between 3 to 5 years, however, recent trend favors adults as most commonly affected individuals[41] with a mean age of 44.94 years |
Thumbprint sign on neck x-ray | Airway maintenance, parenteral Cefotaxime or Ceftriaxone in combination with Vancomycin. Adjuvant therapy includes corticosteroids and racemic Epinephrine.[42][43] |
| Pharyngitis | Sore throat, pain on swallowing, fever, headache, abdominal pain, nausea and vomiting | Group A beta-hemolytic | Inflamed pharynx with or without exudate | Mostly in children and young adults,
with 50% of cases identified between the ages of 5 to 24 years.[44] |
_ | Antimicrobial therapy mainly penicillin-based and analgesics. |
| Tonsilitis | Sore throat, pain on swallowing, fever, headache, and cough | Most common cause is
viral including adenovirus, coronavirus, and Second most common causes are bacterial; |
Fever, especially 100°F or higher.[46][47]Erythema, edema and exudate of the tonsils,[48] cervical lymphadenopathy, and Dysphonia.[49] | Primarily affects children
between 5 and 15 years old.[50] |
Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.[51][52][53] | Antimicrobial therapy mainly penicillin-based and analgesics with tonsilectomy in selected cases. |
| Retropharyngeal abscess | Neck pain, stiff neck, torticollis, fever, malaise, stridor, and barking cough | Polymicrobial infection.
Mostly; Streptococcus pyogenes, Staphylococcus aureus and respiratory anaerobes (example; Fusobacteria, Prevotella, |
Child may be unable to open the mouth widely. May have enlarged cervical lymph nodes and neck mass. | Mostly between 2-4 years, but can occur in other age groups.[59][60] | On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen[61][62] | Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. |
Retropharyngeal abscess must be differentiated from other causes of dysphagia and fever.
| Variable | Croup | Epiglottitis | Pharyngitis | Bacterial tracheitis | Tonsilitis | Retropharyngeal abscess | Subglottic stenosis | |
|---|---|---|---|---|---|---|---|---|
| Presentation | Cough | ✔ | — | Sore throat, pain on swallowing, fever, headache, abdominal pain, nausea and vomiting | Barking cough, stridor, | Sore throat, pain on swallowing, fever, headache, cough | Neck pain, stiff neck, torticollis | Depends on severity. May have respiratory distress at birth, exercise-induced dyspnea, intermittent wheezing. Inspiratory stridor. [63] |
| Stridor | ✔ | ✔ | ||||||
| Drooling | — | ✔ | ||||||
| Others are Hoarseness, Difficulty breathing, symptoms of the common cold, Runny nose, Fever | Other symptoms include difficulty breathing, fever, chills, difficulty swallowing, hoarseness of voice | |||||||
| Causes | Parainfluenza virus | H. influenza type b, beta-hemolytic streptococci, Staphylococcus aureus, fungi and viruses. | Group A beta-hemolytic streptococcus. | Staphylococcus aureus | Most common cause is viral including adenovirus, rhinovirus, influenza, coronavirus, and respiratory syncytial virus. Second most common causes are bacterial; Group A streptococcal bacteria,[64] | Polymicrobial infection. Mostly; Streptococcus pyogenes, Staphylococcus aureus and respiratory anaerobes (example; Fusobacteria, Prevotella, and Veillonella species)[17][16][15][14][13][3] | Congenital, trauma | |
| Physical exams findings | Suprasternal and intercostal indrawing,[65] Inspiratory stridor[66], expiratory wheezing,[66] Sternal wall retractions[67] | Cyanosis, Cervical lymphadenopathy, Inflammed epiglottis | Inflammed pharynx with or without exudate | Subglottic narrowing with purulent secretions in the trachea[68][69] | Fever, especially 100°F or higher.[70][71]Erythema, edema and Exudate of the tonsils.[72] cervical lymphadenopathy, Dysphonia.[73] | Child may be unable to open the mouth widely. May have enlarged
cervical lymph nodes and neck mass. |
Signs of respiratory distress, intermittent wheezing. Inspiratory stridor. [63] | |
| Age commonly affected | Mainly 6 months and 3 years old
rarely, adolescents and adults[74] |
Used to be mostly found in
pediatric age group between 3 to 5 years, however, recent trend favors adults as most commonly affected individuals[75] with a mean age of 44.94 years. |
Mostly in children and young adults,
with 50% of cases identified between the ages of 5 to 24 years.[76] |
Mostly during the first six years of life | Primarily affects children
between 5 and 15 years old.[77] |
Mostly between 2-4 years, but can occur in other age groups.[24][78] | May be congenital congenital or acquired. Mean age in acquired is 54.1 years[79] | |
| Imaging finding | Steeple sign on neck X-ray | Thumbprint sign on neck x-ray | — | Lateral neck xray shows intraluminal membranes and tracheal wall irregularity. | Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.[80][81][82] | On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen[7][83] | Bronchoscopy reveals subglottic stenosis. Computed tomography may reveal a concentric stenotic tracheal segment.[84] | |
| Treatment | Dexamethasone and nebulised epinephrine | Airway maintenance, parenteral Cefotaxime or Ceftriaxone in combination with Vancomycin. Adjuvant therapy includes corticosteroids and racemic Epinephrine.[85][86] | Antimicrobial therapy mainly penicillin-based and analgesics. | Airway maintenance and antibiotics | Antimicrobial therapy mainly penicillin-based and analgesics with tonsilectomy in selected cases. | Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. | Endoscopic balloon dilation for patients with low-grade subglottic stenosis,[87] glucocorticoid injections, and resection.[88] | |
Diagnosis
Diagnosis is based on clinical presentation supported by radio-graphic imaging:[89][4][13][78][90][91][92][93]
History and symptoms
Patients with retropharyngeal abscess may present with:
- Pain in neck
- Fever
- Sore throat
- Mass in neck
- Respiratory distress(stridor)
- Difficulty swallowing (dysphagia)
- Pain with swallowing (odynophagia)
- Unwillingness to move the neck(torticollis)
- Change in voice
- reduced opening of the jaws(Trismus)
- Chest pain
Physical examination
Role of physical examination in diagnosing retropharyngeal abscess is limited, as most of the patients aren't able to open the mouth widely.
Patients with suspected retropharyngeal abscess should be examined in a head-down position(trendelenburg) position. It is recommended to perform examination in an operation room as it permits to place an artificial airway, if necessary. A midline or unilateral swelling of the posterior pharyngeal wall may be appreciated.
Appearance of the Patient
- They are usually acutely-ill looking.
Vital Signs
- High temperature
HEENT
Neck
- Tenderness of anterior neck
- Tender submandibular and anterior cervical lymph nodes
- Tender anterior cervical lymphadenopathy
- Palpable neck mass
Laboratory findings
Laboratory findings may show non-specific leukocytosis.
Imaging
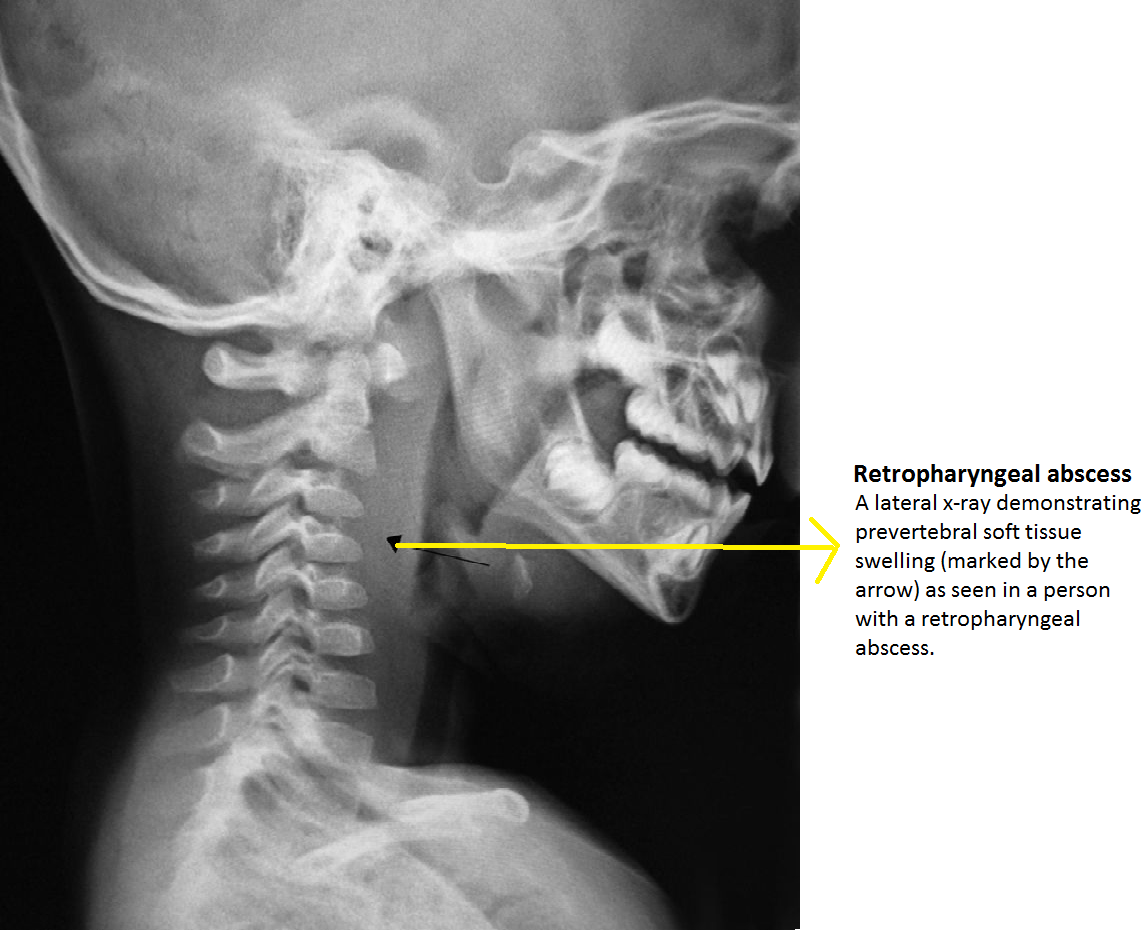
Diagnosis of retropharyngeal abscess should be ultimately supported by radio-graphic imaging. In suspected patients, an initial lateral and anterio-posterior X-ray of neck should be ordered, which is usually followed with CT scan of the neck with IV contrast. CT scan not only helps in diagnosing the retropharyngeal abscess but also helps in identifying the position of carotid artery and internal jugular vein in relation to infectious process.
Plain X-ray
Lateral neck X ray demonstrate thickening of soft tissue with possible gas-fluid levels in pre-vertebral cervical space.
Pathological widening of retropharyngeal space should be considered, if it is greater than 22 mm at C6 in adults and 7 mm at C2 or 14 mm at C6 in children.
Other X ray findings include:
- Reversal of normal cervical lordosis
- Radiopaque foreign body
- Soft-tissue mass
CT scan
Patients with retropharyngeal abscess, abscess may appear as
- Mass impinging on the posterior pharyngeal wall
- Complete rim enhancement with scalloping is indicative of an abscess
- Low density core, soft tissue swelling, obliterated fat planes are other common CT scan findings associated with retropharyngeal abscess
Management
There are no comprehensive randomized controlled studies evaluating the management of retropharyngeal infections. Patients should be ideally hospitalized in a setting where intubation or tracheotomy are easily accessible, in case if there is any respiratory compromise. Management predominantly consists of empiric intravenous antibiotics or combination of surgical drainage and intravenous antibiotics. During hospitalization patient should be regularly monitored for airway patency, hydration status, and potential complications.
Management of retropharyngeal abscess in children and adults follows:[94][4][83][95][95][96][97][98]
Children
Combination of surgical drainage and intravenous antibiotics
Widely accepted indications for surgical drainage of abscess include: airway compromise, or failure to response after 24-24 hrs administration of empiric anti microbial therapy, or CT scan showing large (>3 cm2) hypodense area(indicative of mature abscess) or life-threatening complications. Drainage fluid should be sent for culture and sensitivity, for choosing appropriate antibiotics for further management.
Medical therapy
Trail of antimicrobial therapy for initial 24 to 48 hours without surgical drainage should be considered in patients who do not have airway compromise, CT scan showing cross-sectional hypodense area between <2 to 3 cm2 and no life-threatening complications.
Empiric intravenous antibiotic include:
- Ampicillin-sulbactam (50 mg/kg 6 h IV) or Clindamycin (15 mg/kg per dose [maximum single dose 900 mg]every 8 h IV).
- In patients with moderate or severe disease who do not respond to empiric therapy, additional intravenous Vancomycin (40 to 60 mg/kg per day divided in three to four doses; maximum daily dose 2 to 4 g or Linezolid (<12 years: 30 mg/kg per day divided in three doses; ≥12 years: 20 mg/kg per day in two doses; maximum daily dose 1200 mg) should be considered to optimize the coverage against Gram-positive cocci.
- Once the patients is afebrile and shows signs of clinical improvement, a 14 day oral antimicrobial therapy with either Amoxicillin-clavulanate (45 mg/kg per dose 12 h oral) or Clindamycin (13 mg/kg 8 h oral) should be prescribed.
- Antimicrobial therapy should be adequately supplemented with analgesics, antipyretics and intravenous fluids.
Adults
Combination of surgical drainage and intravenous antibiotics
Widely accepted indications for surgical drainage of abscess include: airway compromise or failure to response after 24-24 hrs administration of empiric antimicrobial therapy or CT scan showing large volume abscess or life-threatening complication. Drainage fluid should be sent for culture and sensitivity, for choosing appropriate antibiotics for further management.
Medical therapy
Trail of antimicrobial therapy for initial 24 to 48 hours without surgical drainage should be considered in patients who do not have airway compromise, CT scan showing small volume abscess, and no life-threatening complications.
| Antibiotics regimen coverage for deep neck space infections[99] | |
|---|---|
| Antibiotics regimen | Coverage rate (%) |
| Ceftriaxone, clindamycin | 76.40% |
| Ceftriaxone, metronidazole | 70.79% |
| Cefuroxime, clindamycin | 61.80% |
| Penicillin G, metronidazole | 16.85% |
| Penicillin, gentamicin, clindamycin | 67.42% |
Preferred medical therapies
Preferred regimen
Ampicillin-sulbactam 3 g/6h IV
Alternative regimens
- Penicillin G 2 to 4 MU/6h IV every four to six hours plus metronidazole 500 mg/6h IV OR
- Clindamycin 600 mg/6h IV OR
- Ceftriaxone 1 g/24 h plus metronidazole 500 mg/6 h IV OR
- Ciprofloxacin 400 mg/12 h IV plus clindamycin 600 mg/6h IV
In patients with moderate or severe disease or having MRSA risk factors(higher incidence of MRSA in hospital and community, IV drug abuse or co-morbid conditions like diabetes mellitus, living in crowed places) or who do not respond to empiric therapy, additional intravenous vancomycin (15 to 20 mg/kg/12 h IV) or linezolid (600 mg/12 h IV) should be considered to optimize the coverage against gram-positive cocci.
Antimicrobial therapy should be adequately supplemented with analgesics, antipyretics and intravenous fluids.
Duration
Once the patients is afebrile and shows signs of clinical improvement IV antibiotics can be replaced with oral antibiotics. Oral antibiotics should be continued for 2-3 weeks after discharge to prevent recurrence or complications.
Discharge instructions
Patients should be asked to report to the health care provider if they notice any new onset of enlarging mass, difficulty in breathing, worsening pain, fever and any stiffness in neck.
Prevention
Primary Prevention
There are no established primary preventive measures for preventing retropharyngeal abscess.
Secondary prevention
There are no established secondary prevention measures, but early detection and appropriate medical and surgical intervention can help in early recovery and prevention of complications.
References
- ↑ Guthrie D (1926). "Acute Retropharyngeal Abscess in Childhood". Br Med J. 2 (3441): 1174–5. PMC 2524315. PMID 20772906.
- ↑ DAVIDSON M (1949). "Abscesses of the retropharyngeal spaces in adults". Laryngoscope. 59 (10): 1146–70. PMID 15406726.
- ↑ 3.0 3.1 3.2 3.3 Asmar BI (1990). "Bacteriology of retropharyngeal abscess in children". Pediatr Infect Dis J. 9 (8): 595–7. PMID 2235179.
- ↑ 4.0 4.1 4.2 4.3 4.4 McClay JE, Murray AD, Booth T (2003). "Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography". Arch Otolaryngol Head Neck Surg. 129 (11): 1207–12. doi:10.1001/archotol.129.11.1207. PMID 14623752.
- ↑ 5.0 5.1 Ungkanont K, Yellon RF, Weissman JL, Casselbrant ML, González-Valdepeña H, Bluestone CD (1995). "Head and neck space infections in infants and children". Otolaryngol Head Neck Surg. 112 (3): 375–82. PMID 7870436.
- ↑ 6.0 6.1 Page NC, Bauer EM, Lieu JE (2008). "Clinical features and treatment of retropharyngeal abscess in children". Otolaryngol Head Neck Surg. 138 (3): 300–6. doi:10.1016/j.otohns.2007.11.033. PMID 18312875.
- ↑ 7.0 7.1 Philpott CM, Selvadurai D, Banerjee AR (2004). "Paediatric retropharyngeal abscess". J Laryngol Otol. 118 (12): 919–26. PMID 15667676.
- ↑ Poluri A, Singh B, Sperling N, Har-El G, Lucente FE (2000). "Retropharyngeal abscess secondary to penetrating foreign bodies". J Craniomaxillofac Surg. 28 (4): 243–6. doi:10.1054/jcms.2000.0151. PMID 11110158.
- ↑ Sethi DS, Chew CT (1991). "Retropharyngeal abscess--the foreign body connection". Ann Acad Med Singapore. 20 (5): 581–8. PMID 1781639.
- ↑ Singh B, Kantu M, Har-El G, Lucente FE (1997). "Complications associated with 327 foreign bodies of the pharynx, larynx, and esophagus". Ann Otol Rhinol Laryngol. 106 (4): 301–4. doi:10.1177/000348949710600407. PMID 9109720.
- ↑ Morrison JE, Pashley NR (1988). "Retropharyngeal abscesses in children: a 10-year review". Pediatr Emerg Care. 4 (1): 9–11. PMID 3283710.
- ↑ Gaglani MJ, Edwards MS (1995). "Clinical indicators of childhood retropharyngeal abscess". Am J Emerg Med. 13 (3): 333–6. doi:10.1016/0735-6757(95)90214-7. PMID 7755832.
- ↑ 13.0 13.1 13.2 Wright CT, Stocks RM, Armstrong DL, Arnold SR, Gould HJ (2008). "Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess". Arch Otolaryngol Head Neck Surg. 134 (4): 408–13. doi:10.1001/archotol.134.4.408. PMID 18427007.
- ↑ 14.0 14.1 Brook I (2004). "Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses". J Oral Maxillofac Surg. 62 (12): 1545–50. PMID 15573356.
- ↑ 15.0 15.1 Inman JC, Rowe M, Ghostine M, Fleck T (2008). "Pediatric neck abscesses: changing organisms and empiric therapies". Laryngoscope. 118 (12): 2111–4. doi:10.1097/MLG.0b013e318182a4fb. PMID 18948832.
- ↑ 16.0 16.1 Abdel-Haq N, Quezada M, Asmar BI (2012). "Retropharyngeal abscess in children: the rising incidence of methicillin-resistant Staphylococcus aureus". Pediatr Infect Dis J. 31 (7): 696–9. doi:10.1097/INF.0b013e318256fff0. PMID 22481424.
- ↑ 17.0 17.1 Cheng J, Elden L (2013). "Children with deep space neck infections: our experience with 178 children". Otolaryngol Head Neck Surg. 148 (6): 1037–42. doi:10.1177/0194599813482292. PMID 23520072.
- ↑ Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM; et al. (2016). "Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012". J Pediatric Infect Dis Soc. 5 (3): 259–68. doi:10.1093/jpids/piv010. PMID 26407249.
- ↑ Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM; et al. (2016). "Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012". J Pediatric Infect Dis Soc. 5 (3): 259–68. doi:10.1093/jpids/piv010. PMID 26407249.
- ↑ Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM; et al. (2016). "Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012". J Pediatric Infect Dis Soc. 5 (3): 259–68. doi:10.1093/jpids/piv010. PMID 26407249.
- ↑ Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM; et al. (2016). "Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012". J Pediatric Infect Dis Soc. 5 (3): 259–68. doi:10.1093/jpids/piv010. PMID 26407249.
- ↑ Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM; et al. (2016). "Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012". J Pediatric Infect Dis Soc. 5 (3): 259–68. doi:10.1093/jpids/piv010. PMID 26407249.
- ↑ Page NC, Bauer EM, Lieu JE (2008). "Clinical features and treatment of retropharyngeal abscess in children". Otolaryngol Head Neck Surg. 138 (3): 300–6. doi:10.1016/j.otohns.2007.11.033. PMID 18312875.
- ↑ 24.0 24.1 Craig FW, Schunk JE (2003). "Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management". Pediatrics. 111 (6 Pt 1): 1394–8. PMID 12777558.
- ↑ Goldenberg D, Golz A, Joachims HZ (1997). "Retropharyngeal abscess: a clinical review". J Laryngol Otol. 111 (6): 546–50. PMID 9231089.
- ↑ Thompson JW, Cohen SR, Reddix P (1988). "Retropharyngeal abscess in children: a retrospective and historical analysis". Laryngoscope. 98 (6 Pt 1): 589–92. doi:10.1288/00005537-198806000-00001. PMID 3374231.
- ↑ Coulthard M, Isaacs D (1991). "Retropharyngeal abscess". Arch Dis Child. 66 (10): 1227–30. PMC 1793510. PMID 1953008.
- ↑ 28.0 28.1
- ↑ 29.0 29.1
- ↑
- ↑
- ↑
- ↑ 33.0 33.1
- ↑ 34.0 34.1
- ↑
- ↑
- ↑
- ↑ 38.0 38.1
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑ 63.0 63.1 Nussbaumer-Ochsner Y, Thurnheer R (2015). "IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis". N Engl J Med. 373 (1): 73. doi:10.1056/NEJMicm1404785. PMID 26132943.
- ↑ Putto A (1987). "Febrile exudative tonsillitis: viral or streptococcal?". Pediatrics. 80 (1): 6–12. PMID 3601520.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ 66.0 66.1 Cherry, James D. (2008). "Croup". New England Journal of Medicine. 358 (4): 384–391. doi:10.1056/NEJMcp072022. ISSN 0028-4793.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ Liston SL, Gehrz RC, Siegel LG, Tilelli J (1983). "Bacterial tracheitis". Am J Dis Child. 137 (8): 764–7. PMID 6869336.
- ↑ Liston SL, Gehrz RC, Jarvis CW (1981). "Bacterial tracheitis". Arch Otolaryngol. 107 (9): 561–4. PMID 7271556.
- ↑ Tonsillitis. Medline Plus. https://www.nlm.nih.gov/medlineplus/ency/article/001043.htm. Accessed May 2nd, 2016.
- ↑ "Tonsillitis - NHS Choices".
- ↑ Stelter K (2014). "Tonsillitis and sore throat in children". GMS Curr Top Otorhinolaryngol Head Neck Surg. 13: Doc07. doi:10.3205/cto000110. PMC 4273168. PMID 25587367.
- ↑ "Tonsillitis - Symptoms - NHS Choices".
- ↑ Tong MC, Chu MC, Leighton SE, van Hasselt CA (1996). "Adult croup". Chest. 109 (6): 1659–62. PMID 8769531.
- ↑ Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED (2016). "Epiglottitis: It Hasn't Gone Away". Anesthesiology. 124 (6): 1404–7. doi:10.1097/ALN.0000000000001125. PMID 27031010.
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Sharav, Yair; Benoliel, Rafael (2008). Orofacial Pain and Headache. Elsevier. ISBN 0723434123.
- ↑ 78.0 78.1 Coulthard M, Isaacs D (1991). "Neonatal retropharyngeal abscess". Pediatr Infect Dis J. 10 (7): 547–9. PMID 1876473.
- ↑ Nicolli EA, Carey RM, Farquhar D, Haft S, Alfonso KP, Mirza N (2017). "Risk factors for adult acquired subglottic stenosis". J Laryngol Otol. 131 (3): 264–267. doi:10.1017/S0022215116009798. PMID 28007041.
- ↑ Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H; et al. (2016). "Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy". Auris Nasus Larynx. 43 (2): 182–6. doi:10.1016/j.anl.2015.09.014. PMID 26527518.
- ↑ Nogan S, Jandali D, Cipolla M, DeSilva B (2015). "The use of ultrasound imaging in evaluation of peritonsillar infections". Laryngoscope. 125 (11): 2604–7. doi:10.1002/lary.25313. PMID 25946659.
- ↑ Fordham MT, Rock AN, Bandarkar A, Preciado D, Levy M, Cohen J; et al. (2015). "Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess". Laryngoscope. 125 (12): 2799–804. doi:10.1002/lary.25354. PMID 25945805.
- ↑ 83.0 83.1 Vural C, Gungor A, Comerci S (2003). "Accuracy of computerized tomography in deep neck infections in the pediatric population". Am J Otolaryngol. 24 (3): 143–8. PMID 12761699.
- ↑ Nussbaumer-Ochsner Y, Thurnheer R (2015). "IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis". N Engl J Med. 373 (1): 73. doi:10.1056/NEJMicm1404785. PMID 26132943.
- ↑ Nickas BJ (2005). "A 60-year-old man with stridor, drooling, and "tripoding" following a nasal polypectomy". J Emerg Nurs. 31 (3): 234–5, quiz 321. doi:10.1016/j.jen.2004.10.015. PMID 15983574.
- ↑ Wick F, Ballmer PE, Haller A (2002). "Acute epiglottis in adults". Swiss Med Wkly. 132 (37–38): 541–7. PMID 12557859.
- ↑ Cui PC, Luo JS, Zhao DQ, Guo ZH, Ma RN (2016). "[Management of subglottic stenosis in children with endoscopic balloon dilation]". Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 51 (4): 286–8. doi:10.3760/cma.j.issn.1673-0860.2016.04.009. PMID 27095722.
- ↑ Nussbaumer-Ochsner Y, Thurnheer R (2015). "IMAGES IN CLINICAL MEDICINE. Subglottic Stenosis". N Engl J Med. 373 (1): 73. doi:10.1056/NEJMicm1404785. PMID 26132943.
- ↑ Page NC, Bauer EM, Lieu JE (2008). "Clinical features and treatment of retropharyngeal abscess in children". Otolaryngol Head Neck Surg. 138 (3): 300–6. doi:10.1016/j.otohns.2007.11.033. PMID 18312875.
- ↑ Sztajnbok J, Grassi MS, Katayama DM, Troster EJ (1999). "Descending suppurative mediastinitis: nonsurgical approach to this unusual complication of retropharyngeal abscesses in childhood". Pediatr Emerg Care. 15 (5): 341–3. PMID 10532666.
- ↑ Lazor JB, Cunningham MJ, Eavey RD, Weber AL (1994). "Comparison of computed tomography and surgical findings in deep neck infections". Otolaryngol Head Neck Surg. 111 (6): 746–50. doi:10.1177/019459989411100608. PMID 7991254.
- ↑ Kirse DJ, Roberson DW (2001). "Surgical management of retropharyngeal space infections in children". Laryngoscope. 111 (8): 1413–22. doi:10.1097/00005537-200108000-00018. PMID 11568578.
- ↑ Daya H, Lo S, Papsin BC, Zachariasova A, Murray H, Pirie J; et al. (2005). "Retropharyngeal and parapharyngeal infections in children: the Toronto experience". Int J Pediatr Otorhinolaryngol. 69 (1): 81–6. doi:10.1016/j.ijporl.2004.08.010. PMID 15627452.
- ↑ Harkani A, Hassani R, Ziad T, Aderdour L, Nouri H, Rochdi Y; et al. (2011). "Retropharyngeal abscess in adults: five case reports and review of the literature". ScientificWorldJournal. 11: 1623–9. doi:10.1100/2011/915163. PMC 3201680. PMID 22125422.
- ↑ 95.0 95.1 Stein MT, Trauner D (1982). "The child with a stiff neck". Clin Pediatr (Phila). 21 (9): 559–63. doi:10.1177/000992288202100908. PMID 7105615.
- ↑ Broughton RA (1992). "Nonsurgical management of deep neck infections in children". Pediatr Infect Dis J. 11 (1): 14–8. PMID 1549402.
- ↑ Saluja S, Brietzke SE, Egan KK, Klavon S, Robson CD, Waltzman ML; et al. (2013). "A prospective study of 113 deep neck infections managed using a clinical practice guideline". Laryngoscope. 123 (12): 3211–8. doi:10.1002/lary.24168. PMID 23918509.
- ↑ Waggie Z, Hatherill M, Millar A, France H, Van Der Merwe A, Argent A (2002). "Retropharyngeal abscess complicated by carotid artery rupture". Pediatr Crit Care Med. 3 (3): 303–304. doi:10.1097/01.PCC.0000019791.40189.F6. PMID 12780973.
- ↑ Yang SW, Lee MH, See LC, Huang SH, Chen TM, Chen TA (2008). "Deep neck abscess: an analysis of microbial etiology and the effectiveness of antibiotics". Infect Drug Resist. 1: 1–8. PMC 3108716. PMID 21694873.