Methicillin-resistant staphylococcus aureus
| Methicillin-resistant Staphylococcus aureus | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
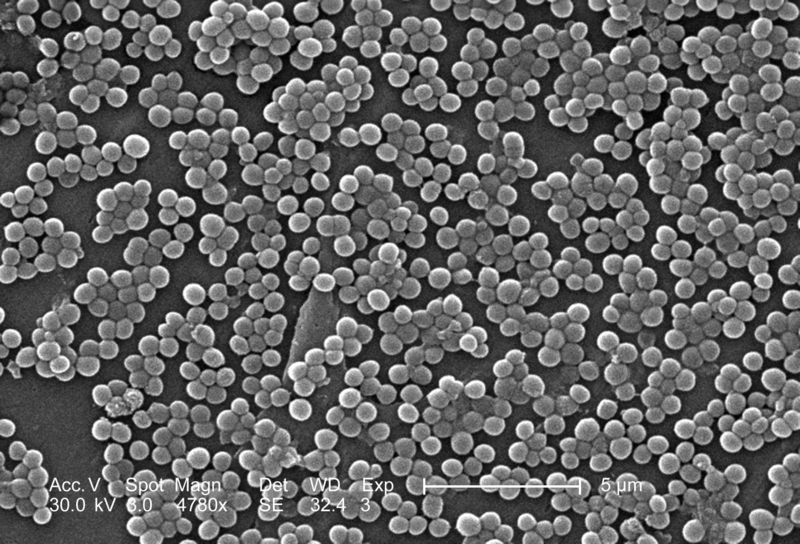 Electron micrograph of MRSA
| ||||||||||||||||
| Scientific classification | ||||||||||||||||
| ||||||||||||||||
| Binomial name | ||||||||||||||||
| Staphylococcus aureus Rosenbach 1884 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: MRSA
Overview
Methicillin-resistant Staphylococcus aureus is an isolate of the bacterium Staphylococcus aureus characterized by antibiotic resistance to all penicillins, including methicillin and other narrow-spectrum β-lactamase-resistant penicillin antibiotics.[1] MRSA was discovered for the first time in 1961 in the United Kingdom, but it is now widespread in the hospital setting. MRSA is commonly termed a superbug.
MRSA may also be known as oxacillin-resistant Staphylococcus aureus (ORSA) and multiple-resistant Staphylococcus aureus. Strains of S. aureus that are non-resistant to methicillin are sometimes called methicillin-susceptible Staphylococcus aureus (MSSA) if an explicit distinction must be made.
Although MRSA has traditionally been seen as a hospital-associated infection, community-acquired MRSA strains have appeared in recent years, notably in the U.S. and Australia.[2] The abbreviations CA-MRSA (community-acquired MRSA) and HA-MRSA (hospital-acquired MRSA) are now commonly seen in medical literature.
Pathophysiology
S. aureus most commonly colonizes the anterior nares (the nostrils), although the respiratory tract, open wounds, intravenous catheters, and urinary tract are also potential sites for infection. Healthy individuals may carry MRSA asymptomatically for periods ranging from a few weeks to many years. Patients with compromised immune systems are at significantly greater risk of symptomatic secondary infection.
Microbiology
Staphylococcus aureus became methicillin resistant by acquiring a mecA gene, usually carried on a larger piece of DNA called a staphylococcal cassette chromosome SCCmec. Expression of mecA yields PBP2a, a penicillin-binding protein with reduced affinity for β-lactam antibiotic binding.[3] Penicillin-binding proteins are necessary for correct synthesis of the bacterial cell wall, and when they are blocked by penicillin, the cell wall is incorrectly formed and the cell is liable to lyse. PBP2a allows the bacterium to synthesize cell wall normally in the presence of methicillin.
Some strains of S. aureus over-express β-lactamase and are resistant to oxacillin and, rarely, methicillin, despite being mecA negative. Beta-lactamase is an enzyme that cleaves the penicillin molecule at its cyclic ring, and second-generation penicillins like methicillin were specifically designed to resist beta-lactamase activity.
Recent outbreaks of CA-MRSA appear to be caused by isolates that also carry genes for Panton-Valentine leukocidin (PVL),[4] a toxin that is known to cause lysis of white blood cells. It has been shown that PVL contributes to severe hemolytic and necrotic pneumonia in children,[5] but its role in severe skin and soft-tissue infection is currently debated. [6]
Strains
In the UK, the most common strains of MRSA are EMRSA15 and EMRSA16.[7] EMRSA16 is the best described epidemiologically; it originated in Kettering, England, and the full genomic sequence of this strain has been published.[8] EMRSA16 has been found to be identical to the ST36:USA200 strain, which circulates in the United Stated, and to carry the SCCmec type II, enterotoxin A and toxic shock syndrome toxin 1 genes.[9] Under the new international typing system, this strain is now called MRSA252. The entire genome sequence of this strain has been published. It is not entirely certain why this strain has become so successful, whereas previous strains have failed to persist. One explanation is the characteristic pattern of antibiotic susceptibility. Both the EMRSA15 and EMRSA16 strains are resistant to erythromycin and ciprofloxacin. It is known that Staphylococcus aureus can survive intracellularly,[10] and these are precisely the antibiotics that best penetrate intracellularly; it may be that these strains of S. aureus are therefore able to exploit an intracellular niche.
In the United States, most cases of CA-MRSA are caused by a CC8 strain designated ST8:USA300, which carries mec type IV, Panton-Valentine leukocidin, and enterotoxins Q and K.[9] Other community-associated strains of MRSA are ST8:USA500 and ST59:USA1000.
Epidemiology and Demographics
Worldwide, an estimated 2 billion people carry some form of S. aureus; of these, up to 53 million (2.7% of carriers) are thought to carry MRSA.[11] In the United States, 95 million carry S. aureus in their noses; of these, 2.5 million (2.6% of carriers) carry MRSA.[12] A population review conducted in three U.S. communities showed the annual incidence of CA-MRSA during 2001–2002 to be 18–25.7/100,000; most CA-MRSA isolates were associated with clinically relevant infections, and 23% of patients required hospitalization.[13]
Because cystic fibrosis patients are often treated with multiple antibiotics in hospital settings, they are often colonized with MRSA, potentially increasing the rate of life-threatening MRSA pneumonia in this group. The risk of cross-colonization has led to the increased use of isolation protocols among these patients. In a hospital setting, patients who have received fluoroquinolones are more likely to become colonized with MRSA;[14] this is probably because many circulating strains of MRSA are fluoroquinolone resistant, which means that MRSA is able to colonize patients whose normal skin flora have been cleared of non-resistant S. aureus by fluoroquinolones.
In the United States, there have been increasing numbers of reports of outbreaks of MRSA colonization and infection through skin contact in locker rooms and gymnasiums, even among healthy populations. MRSA is also becoming a problem in pediatric settings, [15] including hospital nurseries.[16] A 2007 study found that 4.6% of patients in U.S. health care facilities were infected or colonized with MRSA. [17]
MRSA causes as many as 20% of Staphylococcus aureus infections in populations that use intravenous drugs. These out-of-hospital strains, or CA-MRSA, are more easily treated, though more virulent, than HA-MRSA. CA-MRSA apparently did not evolve de novo in the community but represents a hybrid between MRSA that spread from the hospital environment and strains that were once easily treatable in the community. Most of the hybrid strains also acquired a factor that increases their virulence, resulting in the development of deep tissue infections from minor scrapes and cuts, as well as many cases of fatal pneumonia.[18]
As of early 2005, the number of deaths in the United Kingdom attributed to MRSA has been estimated by various sources to lie in the area of 3,000 per year.[19] Staphylococcus bacteria account for almost half of all UK hospital infections. The issue of MRSA infections in hospitals has recently been a major political issue in the UK, playing a significant role in the debates over health policy in the United Kingdom general election held in 2005.
During the summer of 2005, researchers in The Netherlands discovered that three pig farmers or their families were infected by MRSA bacteria that were also found on their pigs.[20] Researchers from Radboud University Nijmegen are now investigating the extent of the MRSA bacteria in pigs and whether it will become characterized among the zoonoses.
It was recently observed that MRSA can replicate inside of Acanthamoeba, increasing MRSA numbers 1,000-fold. [21] Because Acanthamoeba can form cysts that are easily picked up by air currents, these organisms can spread MRSA via airborne routes. Whether control of Acanthamoeba in the clinical environment will also help to control MRSA remains an area for research.
Morbidity and Mortality
It has been difficult to quantify the degree of morbidity and mortality attributable to MRSA. A nationwide study in 2005 showed that patients with S. aureus infection, on average, had three times the length of hospital stay (14.3 vs. 4.5 days), incurred three times the total cost ($48,824 vs $14,141), and experienced five times the risk of in-hospital death (11.2% vs 2.3%) than inpatients without this infection.[22] In a meta-analysis of 31 studies, Cosgrove et al,[23] concluded that MRSA bacteremia is associated with increased mortality as compared with MSSA bacteremia (odds ratio = 1.93; 95% CI = 1.54±2.42; P[24] In addition, Wyllie et al. report a death rate of 34% within 30 days among patients infected with MRSA, a rate similar to the death rate of 27% seen among MSSA-infected patients.[25]
It has been argued that the observed increased mortality among MRSA-infected patients may be the result of the increased underlying morbidity of these patients. Several studies, however, including one by Blot and colleagues, that have adjusted for underlying disease still found MRSA bacteremia to have a higher attributable mortality than MSSA bacteremia.[26]
Screening
According to Betsy McCaughey, founder of the Committee to Reduce Infection Deaths, MRSA can be detected in asymptomatic patients by a blood test. Combined with extra sanitary measures for those in contact with infected patients, screening patients admitted to hospitals has been found to be effective in minimizing the spread of MRSA in hospitals in Denmark, Finland, and the Netherlands.[27]
In the United States, the Centers for Disease Control and Prevention issued guidelines on 19 October 2006, citing the need for additional research, but declined to recommend such screening.[28][29]
History and Symptoms
Many people who are symptomatic present with pus-filled boils and occasionally with rashes.
Treatment
CA-MRSA often results in abscess formation that requires incision and drainage. Before the spread of MRSA into the community, abscesses were not considered contagious because it was assumed that infection required violation of skin integrity and the introduction of staphylococci from normal skin colonization. However, newly emerging CA-MRSA is transmissible (similar, but with very important differences) from hospital-acquired MRSA. CA-MRSA is less likely than other forms of MRSA to cause cellulitis.
Both CA-MRSA and HA-MRSA are resistant to traditional anti-staphylococcal beta-lactam antibiotics such as cephalexin. CA-MRSA has a greater spectrum of antimicrobial susceptibility, including to sulfa drugs, tetracyclines, and clindamycin. HA-MRSA is resistant even to these antibiotics and often is susceptible only to vancomycin. Newer drugs, such as linezolid (belonging to the newer oxazolidinones class), may be effective against both CA-MRSA and HA-MRSA.
Vancomycin and teicoplanin are glycopeptide antibiotics used to treat MRSA infections.[30] Teicoplanin is a structural congener of vancomycin that has a similar activity spectrum but a longer half-life (t½).[31] Because the oral absorption of vancomycin and teicoplanin is very low, these agents must be administered intravenously to control systemic infections.[32] Treatment of MRSA infection with vancomyin can be complicated due to its inconvenient route of administration. Moreover, many clinicians believe that the efficacy of vancomycin against MRSA is inferior to that of anti-staphylococcal beta-lactam antibiotics against MSSA.[33][34]
Several newly disovered strains of MRSA show antibiotic resistance even to vancomycin and teicoplanin. These new evolutions of the MRSA bacterium have dubbed vancomycin intermediate-resistant Staphylococcus aureus (VISA).[35][36] Linezolid, quinupristin/dalfopristin, daptomycin, and tigecycline are used to treat more severe infections that do not respond to glycopeptides such as vancomycin.[37] MRSA infections can be treated with oral agents, including linezolid, rifampicin+fusidic acid, rifampicin+fluoroquinolone, pristinamycin, co-trimoxazole (trimethoprim-sulfamethoxazole), doxycycline or minocycline, and clindamycin.[38]
On 18 May 2006, a team of researchers from Merck Pharmaceuticals reported in Nature that they had discovered an entirely new type of antibiotic, called platensimycin, and had demonstrated its successful use against MRSA.[39][40]
An entirely different and promising approach is phage therapy (e.g., at the Tbilisi Institute in Georgia), which has a reported efficacy against up to 95% of tested Staphylococcus isolates.[41]
It has been reported that use of maggots to treat an MRSA infection has been successful. Studies in diabetic patients reported significantly shorter treatment times than those achieved with standard treatments.[42] [43] [44]
Prevention
Alcohol has proven to be an effective topical sanitizer against MRSA. Quaternary ammonium can be used in conjunction with alcohol to increase the duration of the sanitizing action. The prevention of nosocomial infections involve routine and terminal cleaning. Nonflammable alcohol vapor in CO2 NAV-CO2 systems have an advantage as they do not attack metals or plastics used in medical environments, and do not contribute to antibacterial resistance.
Because MRSA can survive on surfaces and fabrics, including privacy curtains or garments worn by care providers, the need for complete surface sanitation is necessary to eliminate MRSA in areas where patients are recovering from invasive procedures. Vaporized sanitizers reach areas missed by traditional cleaning methods, particularly in ICU and ER units. Ambulances, police vehicles, artificial turf surfaces, and sports equipment are also areas where MRSA can be found.
At the end of August 2004, after a successful pilot scheme to tackle MRSA, the UK National Health Service announced its Clean Your Hands campaign. Wards will be required to ensure that alcohol-based hand rubs are placed near all beds so that staff can hand wash more regularly. It is thought that if this cuts infection by just 1% the plan will pay for itself many times over. Health care workers are reportedly largely neglecting the simple, yet effective, practice of hand-washing, despite the Centers for Disease Control and Prevention (CDC)'s report that hand-washing alone would save the lives of roughly 30,000 patients per year in the US, not from MRSA alone, but from all nosocomial infections.
Mathematical models describe one way in which a loss of infection control can occur after measures for screening and isolation seem to be effective for years, as happened in the UK. In the "search and destroy" strategy that was employed by all UK hospitals until the mid 1990s, all patients with MRSA were immediately isolated, and all staff were screened for MRSA and were prevented from working until they had completed a course of eradication therapy that was proven to work. Loss of control occurs because colonised patients are discharged back into the community and then readmitted: when the number of colonised patients in the community reaches a certain threshold, the "search and destroy" strategy is overwhelmed.[45] One of the few countries not to have been overwhelmed by MRSA is the Netherlands: an important part of the success of the Dutch strategy may have been to attempt eradication of carriage upon discharge from hospital.[46] However, the number of MRSA infected people in the Netherlands is currently rising, because of numerous infections in pig farms. The MRSA strain is carried from pig to human. Very recently, the Dutch food association has discovered strains of the MRSA bacterium on pork meat. These strains were able to infect humans. For countries that have been overwhelmed by MRSA (such as the U.S. and UK), the Dutch model suggests that a co-ordinated re-instatement of search and destroy measures can still bring MRSA under control,[46] but given the enormous investment in facilities that would be required others have suggested that for all practical purposes the point of no return has already been passed.[47]
Related Chapters
- Methicillin resistant staphylococcus aureus infections
- Drug resistance
- Drug resistant diseases
References
- ↑ Foster T (1996). Staphylococcus. In: Barron's Medical Microbiology (Barron S et al, eds.) (4th ed. ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1.
- ↑ Okuma K, Iwakawa K, Turnidge J; et al. (2002). "Dissemination of new methicillin-resistant Staphylococcus aureus clones in the community". J Clin Microbiol. 40 (11): 4289–94. PMID 12409412.
- ↑ Guignard B, Entenza JM, Moreillon P (2005). "Beta-lactams against methicillin-resistant Staphylococcus aureus". Curr Opin Pharmacol. 5 (5): 479–89. PMID 16095969.
- ↑ Miller L, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer A, Tang A, Phung T, Spellberg B (2005). "Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles". N Engl J Med. 352 (14): 1445–53. PMID 15814880.
- ↑ Labandeira-Rey M, Couzon F, Boisset S, Brown EL, Bes M, Benito Y, Barbu EM, Vazquez V, Hook M, Etienne J, Vandenesch F, Bowden MG. (2007). "Staphylococcus aureus Panton-Valentine leukocidin causes necrotizing pneumonia". Science. 315 (5815): 1130–3.
- ↑ Voyich JM, Otto M, Mathema B, Braughton KR, Whitney AR, Welty D, Long RD, Dorward DW, Gardner DJ, Lina G, Kreiswirth BN, DeLeo FR (2006). "Is Panton-Valentine leukocidin the major virulence determinant in community-associated methicillin-resistant Staphylococcus aureus disease?". J Infect Dis. 194 (12): 1761–70.
- ↑ Johnson AP, Aucken HM, Cavendish S; et al. (2001). "Dominance of EMRSA-15 and -16 among MRSA causing nosocomial bacteraemia in the UK: analysis of isolates from the European Antimicrobial Resistance Surveillance System (EARSS)". J Antimicrob Chemother. 48 (1): 143–4. PMID 11418528.
- ↑ Holden MTG, Feil EJ, Lindsay JA; et al. (2004). "Complete genomes of two clinical Staphylococcus aureus strains: Evidence for the rapid evolution of virulence and drug resistance". Proc Natl Acad Sci U S A. 101: 9786–91. doi:10.1073/pnas.0402521101. PMID 15213324. Unknown parameter
|issues=ignored (help) - ↑ 9.0 9.1 Diep B, Carleton H, Chang R, Sensabaugh G, Perdreau-Remington F (2006). "Roles of 34 virulence genes in the evolution of hospital- and community-associated strains of methicillin-resistant Staphylococcus aureus". J Infect Dis. 193 (11): 1495–503. PMID 16652276.
- ↑ von Eiff C, Becker K, Metze D; et al. (2001). "Intracellular persistence of Staphylococcus aureus small-colony variants within keratinocytes: a cause for antibiotic treatment failure in a patient with Darier's disease". Clin Infect Dis. 32 (11): 1643–7. PMID 11340539.
- ↑ MRSA Infections - [keepkidshealthy.com]
- ↑ Graham P, Lin S, Larson E (2006). "A U.S. population-based survey of Staphylococcus aureus colonization". Ann Intern Med. 144 (5): 318–25. PMID 16520472.
- ↑ Jernigan JA, Arnold K, Heilpern K, Kainer M, Woods C, Hughes JM (2006-05-12). "Methicillin-resistant Staphylococcus aureus as community pathogen". Symposium on Community-acquired Methicillin-resistant Staphylococcus aureus (Atlanta, Georgia, USA). Cited in Emerg Infect Dis. Centers for Disease Control and Prevention. Retrieved 2007-01-27.
- ↑ Charbonneau P, Parienti J, Thibon P, Ramakers M, Daubin C, du Cheyron D, Lebouvier G, Le Coutour X, Leclercq R (2006). "Fluoroquinolone use and methicillin-resistant Staphylococcus aureus isolation rates in hospitalized patients: a quasi experimental study". Clin Infect Dis. 42 (6): 778–84. PMID 16477553.
- ↑ MRSA: the problem reaches paediatrics - Archives of Disease in Childhood
- ↑ Community-associated Methicillin-resistant Staphylococcus aureus in Hospital Nursery and Maternity Units - CDC
- ↑ Association for Professionals in Infection Control & Epidemiology (2007-06-25). "National Prevalence Study of Methicillin-Resistant Staphylococcus aureus (MRSA) in U.S. Healthcare Facilities". Retrieved 2007-07-14.
- ↑ Community-acquired meticillin-resistant Staphylococcusaureus: an emerging threat - The Lancet
- ↑ Johnson AP, Pearson A, Duckworth G (2005). "Surveillance and epidemiology of MRSA bacteraemia in the UK". J Antimicrob Chemother. 56 (3): 455–62. PMID 16046464.
- ↑ Voss A, Loeffen F, Bakker J, Klaassen C, Wulf M (2005). "Methicillin-resistant Staphylococcus aureus in pig farming". Emerg Infect Dis. 11 (12): 1965–6. PMID 16485492.
- ↑ Single Cell Amoeba Increases MRSA Numbers One Thousand Fold
- ↑ Noskin GA, Rubin RJ,Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, Lapetina E, Gemmen E (2005). "The Burden of Staphylococcus aureus Infections on Hospitals in the United States: An Analysis of the 2000 and 2001 Nationwide Inpatient Sample Database". Arch Intern Med. 165: 1756–1761. PMID 16087824.
- ↑ Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y (2005). "The impact of Methicillin Resistance in Staphylococcus aureus Bacteremia on Patient Outcomes: Mortality, Length of Stay, and Hospital Charges". Infection Control and Hospital Epidemiology. 26: 166–174.
- ↑ Hardy KJ, Hawkey PM, Gao F, Oppenheim BA (2004). "Methicillin resistant Staphylococcus aureus in the critically ill". British Journal of Anaesthesia. 92: 121–30.
- ↑ Wyllie D, Crook D, Peto T (2006). "Mortality after Staphylococcus aureus bacteraemia in two hospitals in Oxfordshire, 1997-2003: cohort study". BMJ. 333 (7562): 281. PMID 16798756.
- ↑ Blot S, Vandewoude K, Hoste E, Colardyn F (2002). "Outcome and attributable mortality in critically Ill patients with bacteremia involving methicillin-susceptible and methicillin-resistant Staphylococcus aureus". Arch Intern Med. 162 (19): 2229–35. PMID 12390067.
- ↑ McCaughey B, Unnecessary Deaths: The Human and Financial Costs of Hospital Infections (PDF) (2nd. ed.), retrieved 2007-08-05
- ↑ "To Catch a Deadly Germ," New York Times opinion
- ↑ CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- ↑ Schentag JJ, Hyatt JM, Carr JR, Paladino JA, Birmingham MC, Zimmer GS, Cumbo TJ (1998). "Genesis of methicillin-resistant Staphylococcus aureus (MRSA), how treatment of MRSA infections has selected for vancomycin-resistant Enterococcus faecium, and the importance of antibiotic management and infection control". Clin. Infect. Dis. 26 (5): 1204–14. PMID 9597254.
- ↑ Rybak MJ, Lerner SA, Levine DP, Albrecht LM, McNeil PL, Thompson GA, Kenny MT, Yuh L (1991). "Teicoplanin pharmacokinetics in intravenous drug abusers being treated for bacterial endocarditis". Antimicrob. Agents Chemother. 35 (4): 696–700. PMID 1829880.
- ↑ Janknegt R (1997). "The treatment of staphylococcal infections with special reference to pharmacokinetic, pharmacodynamic and pharmacoeconomic considerations". Pharmacy world & science : PWS. 19 (3): 133–41. PMID 9259029.
- ↑ Chang FY, Peacock JE Jr, Musher DM; et al. (2003). "Staphylococcus aureus bacteremia: recurrence and the impact of antibiotic treatment in a prospective multicenter study". Medicine (Baltimore). 82 (5): 333–9. PMID 14530782.
- ↑ Siegman-Igra Y, Reich P, Orni-Wasserlauf R, Schwartz D, Giladi M. (2005). "The role of vancomycin in the persistence or recurrence of Staphylococcus aureus bacteraemia". Scand J Infect Dis. 37 (8): 572–578. PMID 16138425.
- ↑ Sieradzki K, Tomasz A (1997). "Inhibition of cell wall turnover and autolysis by vancomycin in a highly vancomycin-resistant mutant of Staphylococcus aureus". J. Bacteriol. 179 (8): 2557–66. PMID 9098053.
- ↑ Schito GC (2006). "The importance of the development of antibiotic resistance in Staphylococcus aureus". Clin Microbiol Infect. 12 Suppl 1: 3–8. PMID 16445718} Check
|pmid=value (help). - ↑ Mongkolrattanothai K, Boyle S, Kahana MD, Daum RS (2003). "Severe Staphylococcus aureus infections caused by clonally related community-acquired methicillin-susceptible and methicillin-resistant isolates". Clin. Infect. Dis. 37 (8): 1050–8. PMID 14523769.
- ↑ Birmingham MC, Rayner CR, Meagher AK, Flavin SM, Batts DH, Schentag JJ (2003). "Linezolid for the treatment of multidrug-resistant, gram-positive infections: experience from a compassionate-use program". Clin. Infect. Dis. 36 (2): 159–68. PMID 12522747.
- ↑ Bayston R, Ashraf W, Smith T (2007). "Triclosan resistance in methicillin-resistant Staphylococcus aureus expressed as small colony variants: a novel mode of evasion of susceptibility to antiseptics". J. Antimicrob. Chemother. 59 (5): 848–53. PMID 17337510.
- ↑ Wang J (2006). "Platensimycin is a selective FabF inhibitor with potent antibiotic properties". Nature (441): 358–361. PMID 16710421} Check
|pmid=value (help). Unknown parameter|month=ignored (help) - ↑ Matsuzaki S, Yasuda M, Nishikawa H, Kuroda M, Ujihara T, Shuin T, Shen Y, Jin Z, Fujimoto S, Nasimuzzaman MD, Wakiguchi H, Sugihara S, Sugiura T, Koda S, Muraoka A, Imai S (2003). "Experimental protection of mice against lethal Staphylococcus aureus infection by novel bacteriophage phi MR11". J. Infect. Dis. 187 (4): 613–24. PMID 12599078.
- ↑ Bowling FL, Salgami EV, Boulton AJ (2007). "Larval therapy: a novel treatment in eliminating methicillin-resistant Staphylococcus aureus from diabetic foot ulcers". Diabetes Care. 30 (2): 370–371. PMID 17259512.
- ↑ "Maggots help cure MRSA patients". BBC News. 2007-05-02.
- ↑ "Maggots rid patients of MRSA". EurekAlert!/AAAS. 2007-05-03.
- ↑ Cooper BS, Medley GF, Stone SP; et al. (2004). "Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes". 101 (27): 10223–8. PMID 15220470. Unknown parameter
|.journal=ignored (help) - ↑ 46.0 46.1 Bootsma MC, Diekmann O, Bonten MJ (2006). "Controlling methicillin-resistant Staphylococcus aureus: quantifying the effects of interventions and rapid diagnostic testing". Proc Natl Acad Sci USA. 103 (14): 5620–5. PMID 16565219.
- ↑ Paul J (2006). "Surveillance and management of all types of Staphylococcus aureus bacteraemia". BMJ. 333 (7562): 269–70. PMID 16888291.
Further reading
- Carson CF, Cookson BD, Farrelly HD, Riley TV (1995). "Susceptibility of methicillin-resistant Staphylococcus aureus to the essential oil of Melaleuca alternifolia". J. Antimicrob. Chemother. 35 (3): 421–4. PMID 7782258.
- Edwards-Jones V, Buck R, Shawcross SG, Dawson MM, Dunn K (2004). "The effect of essential oils on methicillin-resistant Staphylococcus aureus using a dressing model". Burns : journal of the International Society for Burn Injuries. 30 (8): 772–7. doi:10.1016/j.burns.2004.06.006. PMID 15555788.
Resources
- CDC Article on Hospital Acquired MRSA
- CDC Article on Community Acquired MRSA
- CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- The Independent - PVL: New strain of superbug targets the young, and its latest victim is an NHS nurse - 18/12/06
- BURDEN of Resistance and Disease in European Nations - An EU-Project to estimate the financial burden of antibiotic resistance in European Hospitals
- MRSA and Families Network an Irish support group for people and families that have been affected by MRSA and raising awareness of the infection. They have many branches of the network nationwide.
- MRSA Action UK a charity that aims "to raise public awareness and to influence Government and healthcare providers in the fight to prevent MRSA and all healthcare associated infections"
- Deadly Superbugs, a Reader's Digest article on Community Acquired MRSA
- MRSA Watch provides an index of 4000 articles on MRSA covering every aspect of it's diagnosis and treatment."
- Bacterial Infections Including MRSA Superbug