Ovarian Sarcoma: Difference between revisions
| (33 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Ovarian carcinosarcoma, which is also known as a malignant mixed mullerian tumor (MMMT) of the ovary, is a rare, aggressive cancer of the ovary with two distinct characteristic cancer types i.e carcinoma and sarcoma. | Ovarian carcinosarcoma, which is also known as a [[malignant]] [[mixed mullerian tumor]] (MMMT) of the [[ovary]], is a rare, aggressive [[cancer]] of the [[ovary]] with two distinct characteristic [[cancer]] types i.e [[carcinoma]] and [[sarcoma]]. Primary ovarian sarcomas occur as pure sarcomas or [[Mixed mullerian tumor|mixed mullerian tumors]] (MMTs). Ovarian sarcoma is one of the least common [[Gynecologic Malignancies|gynecologic malignanc]]<nowiki/>y, constituting approximately 1% of all [[Ovarian malignancy|ovarian malignancies]]. [[Prognosis]] is generally poor, and the 5-year [[survival rate]] of [[patients]] with ovarian sarcoma is approximately 28.2%. Most of the [[women]] are [[asymptomatic]], when present, [[symptoms]] may include, [[pain]] in the [[abdomen]] or [[pelvic]] area, [[bloating]] or [[swelling]] of the [[abdomen]], quickly feeling full when [[eating]], other [[digestive]] problems. An elevated concentration of [[CA-125]] in [[serum]] is seen in some [[patients]] of ovarian sarcoma. [[Biopsy]] is the study of choice. Findings on [[MRI]] suggestive of ovarian sarcoma include the following. [[Surgery]] is the mainstay of treatment for ovarian sarcoma.Among all [[Chemotherapy regimens|chemotherapeutic regimens]] that are being used to treat ovarian sarcoma, they are divided into two groups like [[platinum]] containing regimens and non-platinum regimens. [[Cisplatin]], [[carboplatin]] are commonly used. | ||
==Historical Perspective== | ==Historical Perspective== | ||
There is limited information available about the historical perspective of ovarian sarcoma | |||
==Classification== | ==Classification== | ||
*There is no established system for the classification of ovarian | *There is no established system for the [[classification]] of ovarian sarcoma.<ref name="HarrisDelap2003">{{cite journal|last1=Harris|first1=M A|last2=Delap|first2=L M|last3=Sengupta|first3=P S|last4=Wilkinson|first4=P M|last5=Welch|first5=R S|last6=Swindell|first6=R|last7=Shanks|first7=J H|last8=Wilson|first8=G|last9=Slade|first9=R J|last10=Reynolds|first10=K|last11=Jayson|first11=G C|title=Carcinosarcoma of the ovary|journal=British Journal of Cancer|volume=88|issue=5|year=2003|pages=654–657|issn=0007-0920|doi=10.1038/sj.bjc.6600770}}</ref><ref name="pmid27418786">{{cite journal| author=Makris GM, Siristatidis C, Battista MJ, Chrelias C| title=Ovarian carcinosarcoma: a case report, diagnosis, treatment and literature review. | journal=Hippokratia | year= 2015 | volume= 19 | issue= 3 | pages= 256-9 | pmid=27418786 | doi= | pmc=4938474 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27418786 }} </ref><ref name="pmid21420726">{{cite journal| author=Rauh-Hain JA, Growdon WB, Rodriguez N, Goodman AK, Boruta DM, Schorge JO et al.| title=Carcinosarcoma of the ovary: a case-control study. | journal=Gynecol Oncol | year= 2011 | volume= 121 | issue= 3 | pages= 477-81 | pmid=21420726 | doi=10.1016/j.ygyno.2011.02.023 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21420726 }} </ref> | ||
*Primary ovarian sarcomas occur as pure sarcomas or mixed | *Primary ovarian sarcomas occur as pure sarcomas or [[mixed mullerian tumor]]<nowiki/>s (MMTs). | ||
*Pure sarcomas are comprised of a single malignant mesenchymal element and are further categorized as: | *Pure sarcomas are comprised of a single [[malignant]] [[mesenchymal]] element and are further categorized as: | ||
**Stromal cell sarcomas | **Stromal cell sarcomas | ||
**Fibrosarcomas | **[[Fibrosarcoma|Fibrosarcomas]] | ||
**Leiomyosarcomas | **[[Leiomyosarcoma|Leiomyosarcomas]] | ||
**Neurofibrosarcomas | **[[Neurofibrosarcoma|Neurofibrosarcomas]] | ||
**Rhabdomyosarcomas | **[[Rhabdomyosarcoma|Rhabdomyosarcomas]] | ||
** | **[[Chondrosarcoma]]<nowiki/>s | ||
**Angiosarcomas | **[[Angiosarcoma|Angiosarcomas]] | ||
**Liposarcomas | **[[Liposarcoma|Liposarcomas]] | ||
*On the other hand mixed mullerian tumors(MMTs) are defined by the presence of both carcinomatous and sarcomatous elements and are more common than pure sarcomas. | *On the other hand [[Mixed mullerian tumor|mixed mullerian tumors]](MMTs) are defined by the presence of both carcinomatous and sarcomatous elements and are more common than pure sarcomas. | ||
*Ovarian MMTs can be further classified as homologous or heterologous on the basis of the tissue components present. | *Ovarian MMTs can be further classified as homologous or heterologous on the basis of the tissue components present. | ||
*Homologous tumors contain elements that are native to the ovary whereas heterologous tumors contain elements that normally are not present in the ovary. | *Homologous tumors contain elements that are native to the ovary whereas heterologous tumors contain elements that normally are not present in the ovary. | ||
| Line 43: | Line 34: | ||
==Pathophysiology== | ==Pathophysiology== | ||
*The exact pathogenesis of ovarian sarcoma is not fully understood | *The exact [[pathogenesis]] of ovarian sarcoma is not fully understood<ref name="pmid25371706">{{cite journal| author=Vargas AN| title=Natural history of ovarian cancer. | journal=Ecancermedicalscience | year= 2014 | volume= 8 | issue= | pages= 465 | pmid=25371706 | doi=10.3332/ecancer.2014.465 | pmc=4176445 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25371706 }} </ref><ref name="pmid21420726">{{cite journal| author=Rauh-Hain JA, Growdon WB, Rodriguez N, Goodman AK, Boruta DM, Schorge JO et al.| title=Carcinosarcoma of the ovary: a case-control study. | journal=Gynecol Oncol | year= 2011 | volume= 121 | issue= 3 | pages= 477-81 | pmid=21420726 | doi=10.1016/j.ygyno.2011.02.023 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21420726 }} </ref> | ||
*Clonal loss of the wild-type BRCA2 allele as well as the same somatic mutation of the TP53 gene was evident in histologic components | *Clonal loss of the wild-type [[BRCA2]] [[allele]] as well as the same [[somatic mutation]] of the [[TP53]] [[gene]] was evident in [[histologic]] components | ||
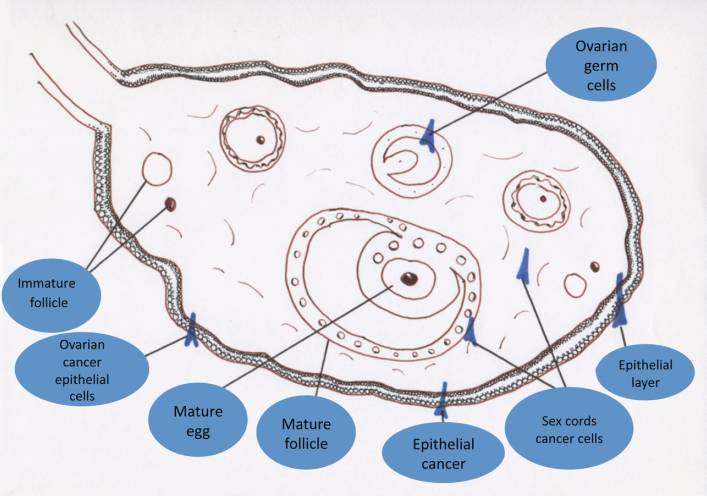
[[File:Tileshop.jpg|400px|thumb|none|Types of ovarian cancer according to origin,Vargas AN. Natural history of ovarian cancer. Ecancermedicalscience. 2014;8:465. Published 2014 Sep 25. doi:10.3332/ecancer.2014.465,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4176445/]] | |||
==Causes== | ==Causes== | ||
The exact [[causes]] of ovarian sarcoma have not been identified. | |||
==Differentiating ovarian sarcoma from Other Diseases== | |||
On the basis of age of onset, [[vaginal discharge]], and constitutional symptoms, ovarian cancer must be differentiated from [[tubo-ovarian abscess]], [[ectopic pregnancy]], [[hydrosalpinx]], [[salpingitis]], [[fallopian tube]] [[carcinoma]], [[uterine leiomyoma]], [[choriocarcinoma]], [[leiomyosarcoma]], [[pregnancy]], [[Appendix|appendiceal]] [[abscess]], [[Appendiceal cancer|appendiceal neoplasm]], [[diverticular abscess]], [[colorectal cancer]], [[pelvic kidney]], advanced [[bladder cancer]], and [[retroperitoneal]] [[sarcoma]]. | |||
[ | |||
{| | {| | ||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |- style="background: #4479BA; color: #FFFFFF; text-align: center;" | ||
| Line 87: | Line 69: | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CT scan/US | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CT scan/US | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |MRI | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |MRI | ||
|- | |||
! colspan="14" style="background: #7d7d7d; color: #FFFFFF; text-align: center;" |Gynecologic | |||
|- | |||
| rowspan="14" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ovary|Ovarian]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ovarian cyst|Follicular cysts]]<br><ref name="pmid20505067">{{cite journal |vauthors=Levine D, Brown DL, Andreotti RF, Benacerraf B, Benson CB, Brewster WR, Coleman B, Depriest P, Doubilet PM, Goldstein SR, Hamper UM, Hecht JL, Horrow M, Hur HC, Marnach M, Patel MD, Platt LD, Puscheck E, Smith-Bindman R |title=Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement |journal=Radiology |volume=256 |issue=3 |pages=943–54 |date=September 2010 |pmid=20505067 |doi=10.1148/radiol.10100213 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Women]] in [[Reproductive system|reproductive]] age (15 -45 y/o) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High level of [[estrogen]] +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see a >3 cm simple [[cyst]] with no internal echo and with posterior acoustic enhancement | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* simple [[cyst]] with no internal echo or septa | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History]]/<br>[[imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[hyperestrogenism]] and [[endometrial hyperplasia]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ovarian cyst|Theca lutein cysts]]<br><ref name="pmid2455880">{{cite journal |vauthors=Montz FJ, Schlaerth JB, Morrow CP |title=The natural history of theca lutein cysts |journal=Obstet Gynecol |volume=72 |issue=2 |pages=247–51 |date=August 1988 |pmid=2455880 |doi= |url=}}</ref><ref name="Southam1962">{{cite journal|last1=Southam|first1=Anna L.|title=Massive Ovarian Hyperstimulation with Clomiphene Citrate|journal=JAMA: The Journal of the American Medical Association|volume=181|issue=5|year=1962|pages=443|issn=0098-7484|doi=10.1001/jama.1962.03050310083018b}}</ref><ref name="NguyenReid1986">{{cite journal|last1=Nguyen|first1=K T|last2=Reid|first2=R L|last3=Sauerbrei|first3=E|title=Antenatal sonographic detection of a fetal theca lutein cyst: a clue to maternal diabetes mellitus.|journal=Journal of Ultrasound in Medicine|volume=5|issue=11|year=1986|pages=665–667|issn=02784297|doi=10.7863/jum.1986.5.11.665}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Women]] in [[reproductive]] age (15 -45 y/o) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Depends on the underlying [[etiology]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see bilaterally enlarged [[ovaries]] with multiple [[cysts]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Multiple bilateral [[cysts]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Theca interna cell [[Hyperplasia]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History]]/<br>[[imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[Hydatidiform mole|hydatidiform moles]], [[choriocarcinoma]], [[diabetes mellitus]] and [[clomiphene]] intake ([[ovulation]] induction) | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Serous cystadenoma/carcinoma<br><ref name="JungLee20022">{{cite journal|last1=Jung|first1=Seung Eun|last2=Lee|first2=Jae Mun|last3=Rha|first3=Sung Eun|last4=Byun|first4=Jae Young|last5=Jung|first5=Jung Im|last6=Hahn|first6=Seong Tai|title=CT and MR Imaging of Ovarian Tumors with Emphasis on Differential Diagnosis|journal=RadioGraphics|volume=22|issue=6|year=2002|pages=1305–1325|issn=0271-5333|doi=10.1148/rg.226025033}}</ref><ref name="ImaiKiyozuka1990">{{cite journal|last1=Imai|first1=Shunsuke|last2=Kiyozuka|first2=Yasuhiko|last3=Maeda|first3=Hiroko|last4=Noda|first4=Tuneo|last5=Hosick|first5=Howard L.|title=Establishment and Characterization of a Human Ovarian Serous Cystadenocarcinoma Cell Line That Produces the Tumor Markers CA-125 and Tissue Polypeptide Antigen|journal=Oncology|volume=47|issue=2|year=1990|pages=177–184|issn=0030-2414|doi=10.1159/000226813}}</ref><ref name="pmid15087669">{{cite journal |vauthors=Malpica A, Deavers MT, Lu K, Bodurka DC, Atkinson EN, Gershenson DM, Silva EG |title=Grading ovarian serous carcinoma using a two-tier system |journal=Am. J. Surg. Pathol. |volume=28 |issue=4 |pages=496–504 |date=April 2004 |pmid=15087669 |doi= |url=}}</ref><ref name="pmid22405464">{{cite journal |vauthors=Li J, Fadare O, Xiang L, Kong B, Zheng W |title=Ovarian serous carcinoma: recent concepts on its origin and carcinogenesis |journal=J Hematol Oncol |volume=5 |issue= |pages=8 |date=March 2012 |pmid=22405464 |doi=10.1186/1756-8722-5-8 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Serous cystadenoma/carcinoma<br><ref name="JungLee20022">{{cite journal|last1=Jung|first1=Seung Eun|last2=Lee|first2=Jae Mun|last3=Rha|first3=Sung Eun|last4=Byun|first4=Jae Young|last5=Jung|first5=Jung Im|last6=Hahn|first6=Seong Tai|title=CT and MR Imaging of Ovarian Tumors with Emphasis on Differential Diagnosis|journal=RadioGraphics|volume=22|issue=6|year=2002|pages=1305–1325|issn=0271-5333|doi=10.1148/rg.226025033}}</ref><ref name="ImaiKiyozuka1990">{{cite journal|last1=Imai|first1=Shunsuke|last2=Kiyozuka|first2=Yasuhiko|last3=Maeda|first3=Hiroko|last4=Noda|first4=Tuneo|last5=Hosick|first5=Howard L.|title=Establishment and Characterization of a Human Ovarian Serous Cystadenocarcinoma Cell Line That Produces the Tumor Markers CA-125 and Tissue Polypeptide Antigen|journal=Oncology|volume=47|issue=2|year=1990|pages=177–184|issn=0030-2414|doi=10.1159/000226813}}</ref><ref name="pmid15087669">{{cite journal |vauthors=Malpica A, Deavers MT, Lu K, Bodurka DC, Atkinson EN, Gershenson DM, Silva EG |title=Grading ovarian serous carcinoma using a two-tier system |journal=Am. J. Surg. Pathol. |volume=28 |issue=4 |pages=496–504 |date=April 2004 |pmid=15087669 |doi= |url=}}</ref><ref name="pmid22405464">{{cite journal |vauthors=Li J, Fadare O, Xiang L, Kong B, Zheng W |title=Ovarian serous carcinoma: recent concepts on its origin and carcinogenesis |journal=J Hematol Oncol |volume=5 |issue= |pages=8 |date=March 2012 |pmid=22405464 |doi=10.1186/1756-8722-5-8 |url=}}</ref> | ||
| Line 195: | Line 223: | ||
* May content [[thyroid]] [[tissue]] and cause [[hyperthyroidism]] | * May content [[thyroid]] [[tissue]] and cause [[hyperthyroidism]] | ||
* In plane [[radiography]] we may see [[calcification]] due to the presence of [[tooth]] in the [[tumor]] | * In plane [[radiography]] we may see [[calcification]] due to the presence of [[tooth]] in the [[tumor]] | ||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Dysgerminoma]]<br><ref name="DganiShoham(Schwartz)1988">{{cite journal|last1=Dgani|first1=R.|last2=Shoham(Schwartz)|first2=Z.|last3=Czernobilsky|first3=B.|last4=Kaftori|first4=A.|last5=Borenstein|first5=R.|last6=Lancet|first6=M.|title=Lactic dehydrogenase, alkaline phosphatase and human chorionic gonadotropin in a pure ovarian dysgerminoma|journal=Gynecologic Oncology|volume=30|issue=1|year=1988|pages=44–50|issn=00908258|doi=10.1016/0090-8258(88)90044-3}}</ref><ref name="pmid8188914">{{cite journal |vauthors=Tanaka YO, Kurosaki Y, Nishida M, Michishita N, Kuramoto K, Itai Y, Kubo T |title=Ovarian dysgerminoma: MR and CT appearance |journal=J Comput Assist Tomogr |volume=18 |issue=3 |pages=443–8 |date=1994 |pmid=8188914 |doi= |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* in the second to third decade of life | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High level of [[HCG]] and [[LDH]] | |||
* [[Hypercalcemia]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Multilobulated solid [[Mass|masses]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We may see [[ovarian]] [[mass]] with septation which are hyperintense on T1 and hypo or isointense on T2 [[imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Sheets fried egg appearance [[Cell (biology)|cells]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Same as [[male]] [[seminoma]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Yolk sac tumor]]<br><ref name="Yang2000">{{cite journal|last1=Yang|first1=Grace C.H.|title=Fine-needle aspiration cytology of Schiller-Duval bodies of yolk-sac tumor|journal=Diagnostic Cytopathology|volume=23|issue=4|year=2000|pages=228–232|issn=8755-1039|doi=10.1002/1097-0339(200010)23:4<228::AID-DC2>3.0.CO;2-M}}</ref><ref name="LevitinHaller1996">{{cite journal|last1=Levitin|first1=A|last2=Haller|first2=K D|last3=Cohen|first3=H L|last4=Zinn|first4=D L|last5=O'Connor|first5=M T|title=Endodermal sinus tumor of the ovary: imaging evaluation.|journal=American Journal of Roentgenology|volume=167|issue=3|year=1996|pages=791–793|issn=0361-803X|doi=10.2214/ajr.167.3.8751702}}</ref><ref name="TalermanHaije1974">{{cite journal|last1=Talerman|first1=A.|last2=Haije|first2=W. G.|title=Alpha-fetoprotein and germ cell tumors: A possible role of yolk sac tumor in production of alpha-fetoprotein|journal=Cancer|volume=34|issue=5|year=1974|pages=1722–1726|issn=0008-543X|doi=10.1002/1097-0142(197411)34:5<1722::AID-CNCR2820340521>3.0.CO;2-F}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Young [[children]] | |||
* [[Male]] [[infants]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High levels of [[AFP]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see a combination of echogenic and hypoechoic components | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Ovarian mass]] with [[hemorrhagic]] areas | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Yellow appearance | |||
* [[Hemorrhagic]] | |||
* Schiller-Duval bodies ([[glomeruli]] like structures) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* The other name is [[Ovarian cyst|ovarian]] [[endodermal sinus tumor]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Fibroma]]<br><ref name="pmid13148256">{{cite journal |vauthors=MEIGS JV |title=Fibroma of the ovary with ascites and hydrothorax; Meigs' syndrome |journal=Am. J. Obstet. Gynecol. |volume=67 |issue=5 |pages=962–85 |date=May 1954 |pmid=13148256 |doi= |url=}}</ref><ref name="SivanesaratnamDutta1990">{{cite journal|last1=Sivanesaratnam|first1=V.|last2=Dutta|first2=R.|last3=Jayalakshmi|first3=P.|title=Ovarian fibroma - clinical and histopathological characteristics|journal=International Journal of Gynecology & Obstetrics|volume=33|issue=3|year=1990|pages=243–247|issn=00207292|doi=10.1016/0020-7292(90)90009-A}}</ref><ref name="AbadCazorla1999">{{cite journal|last1=Abad|first1=Antonio|last2=Cazorla|first2=Eduardo|last3=Ruiz|first3=Fernando|last4=Aznar|first4=Ismael|last5=Asins|first5=Enrique|last6=Llixiona|first6=Joaquin|title=Meigs' syndrome with elevated CA125: case report and review of the literature|journal=European Journal of Obstetrics & Gynecology and Reproductive Biology|volume=82|issue=1|year=1999|pages=97–99|issn=03012115|doi=10.1016/S0301-2115(98)00174-2}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* >50 y/o | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Pulling sensation in the [[groin]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High levels of [[CA-125]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[CT scan]] we may see a unilateral [[mass]] with poor contrast enhancement | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Low signal intensity on T1 and T2 | |||
* We may see scattered hyperintense areas due to [[edema]] or [[cystic]] [[degeneration]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Spindle-shaped [[fibroblast]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may cause [[Meigs syndrome]] ([[ovarian fibroma]], [[ascites]], and [[hydrothorax]]) | |||
* It may cause [[ovarian torsion]] | |||
* It may cause [[pleural effusion]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Thecoma]]<br><ref name="YaghoobianPinck1983">{{cite journal|last1=Yaghoobian|first1=Jahanguir|last2=Pinck|first2=Robert L.|title=Ultrasound findings in thecoma of the ovary|journal=Journal of Clinical Ultrasound|volume=11|issue=2|year=1983|pages=91–93|issn=00912751|doi=10.1002/jcu.1870110207}}</ref><ref name="LiZhang2012">{{cite journal|last1=Li|first1=Xinchun|last2=Zhang|first2=Weidong|last3=Zhu|first3=Guangbin|last4=Sun|first4=Congpeng|last5=Liu|first5=Qingyu|last6=Shen|first6=Yuechun|title=Imaging Features and Pathologic Characteristics of Ovarian Thecoma|journal=Journal of Computer Assisted Tomography|volume=36|issue=1|year=2012|pages=46–53|issn=0363-8715|doi=10.1097/RCT.0b013e31823f6186}}</ref><ref name="ProctorGreeley1951">{{cite journal|last1=Proctor|first1=Francis E.|last2=Greeley|first2=Joseph P.|last3=Rathmell|first3=Thomas K.|title=Malignant thecoma of the ovary|journal=American Journal of Obstetrics and Gynecology|volume=62|issue=1|year=1951|pages=185–192|issn=00029378|doi=10.1016/0002-9378(51)91109-X}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* >50 y/o | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Postmenopausal bleeding]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High level of [[estrogen]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see non-specific [[ovarian]] [[mass]] | |||
* We may see evidence of [[endometrial hyperplasia]] due to increased level of [[estrogen]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Hyperintense on T2 | |||
* T1 intensity depends on the amount of [[fibrous tissue]] ([[fibrous tissue]] lead to hypointensity) | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Lipid-laden [[Stromal cell|stromal cells]] with pale, vaculolated [[cytoplasm]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We may see [[endometrial cancer]] as e result of hyper-[[Estrogen|estrogenism]] | |||
* We may see [[ovarian]] fibrothecoma (mixture of [[fibroma]] and [[thecoma]]) | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Granulosa cell tumour|Granulosa cell tumor]]<br><ref name="pmid17945423">{{cite journal |vauthors=Pectasides D, Pectasides E, Psyrri A |title=Granulosa cell tumor of the ovary |journal=Cancer Treat. Rev. |volume=34 |issue=1 |pages=1–12 |date=February 2008 |pmid=17945423 |doi=10.1016/j.ctrv.2007.08.007 |url=}}</ref><ref name="StenwigHazekamp1979">{{cite journal|last1=Stenwig|first1=Jan Trygve|last2=Hazekamp|first2=Johan The.|last3=Beecham|first3=Jackson B.|title=Granulosa cell tumors of the ovary. A clinicopathological study of 118 cases with long-term follow-up|journal=Gynecologic Oncology|volume=7|issue=2|year=1979|pages=136–152|issn=00908258|doi=10.1016/0090-8258(79)90090-8}}</ref><ref name="pmid9386298">{{cite journal |vauthors=Morikawa K, Hatabu H, Togashi K, Kataoka ML, Mori T, Konishi J |title=Granulosa cell tumor of the ovary: MR findings |journal=J Comput Assist Tomogr |volume=21 |issue=6 |pages=1001–4 |date=1997 |pmid=9386298 |doi= |url=}}</ref><ref name="pmid10227493">{{cite journal |vauthors=Ko SF, Wan YL, Ng SH, Lee TY, Lin JW, Chen WJ, Kung FT, Tsai CC |title=Adult ovarian granulosa cell tumors: spectrum of sonographic and CT findings with pathologic correlation |journal=AJR Am J Roentgenol |volume=172 |issue=5 |pages=1227–33 |date=May 1999 |pmid=10227493 |doi=10.2214/ajr.172.5.10227493 |url=}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Granulosa cell tumour|Granulosa cell tumor]]<br><ref name="pmid17945423">{{cite journal |vauthors=Pectasides D, Pectasides E, Psyrri A |title=Granulosa cell tumor of the ovary |journal=Cancer Treat. Rev. |volume=34 |issue=1 |pages=1–12 |date=February 2008 |pmid=17945423 |doi=10.1016/j.ctrv.2007.08.007 |url=}}</ref><ref name="StenwigHazekamp1979">{{cite journal|last1=Stenwig|first1=Jan Trygve|last2=Hazekamp|first2=Johan The.|last3=Beecham|first3=Jackson B.|title=Granulosa cell tumors of the ovary. A clinicopathological study of 118 cases with long-term follow-up|journal=Gynecologic Oncology|volume=7|issue=2|year=1979|pages=136–152|issn=00908258|doi=10.1016/0090-8258(79)90090-8}}</ref><ref name="pmid9386298">{{cite journal |vauthors=Morikawa K, Hatabu H, Togashi K, Kataoka ML, Mori T, Konishi J |title=Granulosa cell tumor of the ovary: MR findings |journal=J Comput Assist Tomogr |volume=21 |issue=6 |pages=1001–4 |date=1997 |pmid=9386298 |doi= |url=}}</ref><ref name="pmid10227493">{{cite journal |vauthors=Ko SF, Wan YL, Ng SH, Lee TY, Lin JW, Chen WJ, Kung FT, Tsai CC |title=Adult ovarian granulosa cell tumors: spectrum of sonographic and CT findings with pathologic correlation |journal=AJR Am J Roentgenol |volume=172 |issue=5 |pages=1227–33 |date=May 1999 |pmid=10227493 |doi=10.2214/ajr.172.5.10227493 |url=}}</ref> | ||
| Line 244: | Line 375: | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
* It may cause [[virilization]] [[Symptom|symptoms]] and [[amenorrhea]] | * It may cause [[virilization]] [[Symptom|symptoms]] and [[amenorrhea]] | ||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brenner tumor]]<br><ref name="ShevchukFenoglio1980">{{cite journal|last1=Shevchuk|first1=Maria M.|last2=Fenoglio|first2=Cecilia M.|last3=Richart|first3=Ralph M.|title=Histogenesis of brenner tumors, I: Histology and ultrastructure|journal=Cancer|volume=46|issue=12|year=1980|pages=2607–2616|issn=0008-543X|doi=10.1002/1097-0142(19801215)46:12<2607::AID-CNCR2820461213>3.0.CO;2-Q}}</ref><ref name="OutwaterSiegelman1998">{{cite journal|last1=Outwater|first1=Eric K|last2=Siegelman|first2=Evan S|last3=Kim|first3=Bohyun|last4=Chiowanich|first4=Peerapod|last5=Blasbalg|first5=Roberto|last6=Kilger|first6=Alex|title=Ovarian Brenner tumors: MR imaging characteristics|journal=Magnetic Resonance Imaging|volume=16|issue=10|year=1998|pages=1147–1153|issn=0730725X|doi=10.1016/S0730-725X(98)00136-2}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* >55 y/o | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
:* In [[Ultrasound|US]] we may see hypoechoic solid [[Mass-to-charge ratio|mass]] and [[calcification]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Hypointense on T2 because of [[fibrous]] content | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Yellow/pale appearance | |||
* [[Transitional cell]] [[tumor]] (resembles [[Urinary bladder|bladder]]) | |||
* Coffee bean [[nuclei]] on [[H&E stain|H&E]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Most of the times it's an accidental finding | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Krukenberg tumor|Krukenberg tumor]]<br><ref name="pmid8626898">{{cite journal |vauthors=Kim SH, Kim WH, Park KJ, Lee JK, Kim JS |title=CT and MR findings of Krukenberg tumors: comparison with primary ovarian tumors |journal=J Comput Assist Tomogr |volume=20 |issue=3 |pages=393–8 |date=1996 |pmid=8626898 |doi= |url=}}</ref><ref name="pmid17076540">{{cite journal |vauthors=Al-Agha OM, Nicastri AD |title=An in-depth look at Krukenberg tumor: an overview |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=11 |pages=1725–30 |date=November 2006 |pmid=17076540 |doi=10.1043/1543-2165(2006)130[1725:AILAKT]2.0.CO;2 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* >55 y/o | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
Based on underlying [[malignancy]] | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In case of [[Metastasis|metastatic]] [[Gastrointestinal cancer|GI cancers]] we may see [[iron deficiency anemia]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Mostly bilateral, complex ovarian [[lesion]] | |||
* In [[CT scan]] we may see evidence of concurrent [[malignancy]] in other [[organs]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Mostly bilateral, complex [[Ovary|ovarian]] [[lesion]] with solid components | |||
* Internal hyperintensity on T1 and T2 weighted [[Mri|MR]] [[images]] because of [[Mucin 17|mucin]] | |||
* Evidence of concurrent [[malignancy]] in other [[organs]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Mucin]]-secreting [[signet cell]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]]/<br>[[biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* The most common [[primary tumor]] is in [[Colon (anatomy)|colon]], [[stomach]], [[breast]], [[lung]], and contralateral [[ovary]] | |||
* Based on underlying [[malignancy]] it may cause [[pleural effusion]] | |||
|- | |- | ||
| rowspan="5" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Fallopian tube|Tubal]] | | rowspan="5" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Fallopian tube|Tubal]] | ||
| Line 270: | Line 448: | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
*The most common [[Risk factor|risk factors]] are previous [[PID]], [[diabetes mellitus]], [[intrauterine device]] and [[History and Physical examination|history]] of [[Uterus|uterine]] [[surgery]] | *The most common [[Risk factor|risk factors]] are previous [[PID]], [[diabetes mellitus]], [[intrauterine device]] and [[History and Physical examination|history]] of [[Uterus|uterine]] [[surgery]] | ||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Ectopic pregnancy]]<br><ref name="Barnhart2009">{{cite journal|last1=Barnhart|first1=Kurt T.|title=Ectopic Pregnancy|journal=New England Journal of Medicine|volume=361|issue=4|year=2009|pages=379–387|issn=0028-4793|doi=10.1056/NEJMcp0810384}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Women]] in [[reproductive]] age (15 -45 y/o) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High level of [[HCG|BhCG]] | |||
* [[Progesterone]] level ≤5 ng/ml | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see empty [[uterine cavity]], [[Fallopian tube|tubal]] ring sign, ring of fire sign ([[Doppler]]), extra-[[uterine]] [[Fetus|fetal]] [[heart rate]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History]]/<br>[[imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Any [[women]] in [[reproductive]] age presenting with [[abdominal pain]] or [[amenorrhea]] should be screened for [[ectopic pregnancy]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hydrosalpinx]]<br><ref name="KimRha2009">{{cite journal|last1=Kim|first1=Mi Young|last2=Rha|first2=Sung Eun|last3=Oh|first3=Soon Nam|last4=Jung|first4=Seung Eun|last5=Lee|first5=Young Joon|last6=Kim|first6=You Sung|last7=Byun|first7=Jae Young|last8=Lee|first8=Ahwon|last9=Kim|first9=Mee-Ran|title=MR Imaging Findings of Hydrosalpinx: A Comprehensive Review|journal=RadioGraphics|volume=29|issue=2|year=2009|pages=495–507|issn=0271-5333|doi=10.1148/rg.292085070}}</ref><ref name="pmid7938766">{{cite journal |vauthors=Atri M, Nazarnia S, Bret PM, Aldis AE, Kintzen G, Reinhold C |title=Endovaginal sonographic appearance of benign ovarian masses |journal=Radiographics |volume=14 |issue=4 |pages=747–60; discussion 761–2 |date=July 1994 |pmid=7938766 |doi=10.1148/radiographics.14.4.7938766 |url=}}</ref><ref name="ChanellesDucarme2011">{{cite journal|last1=Chanelles|first1=Olivier|last2=Ducarme|first2=Guillaume|last3=Sifer|first3=Christophe|last4=Hugues|first4=Jean-Noel|last5=Touboul|first5=Cyril|last6=Poncelet|first6=Christophe|title=Hydrosalpinx and infertility: what about conservative surgical management?|journal=European Journal of Obstetrics & Gynecology and Reproductive Biology|volume=159|issue=1|year=2011|pages=122–126|issn=03012115|doi=10.1016/j.ejogrb.2011.07.004}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see [[Fallopian tube|tubal]] longitudinal folds thickening (cogwheel appearance) | |||
* In [[CT scan]] we may see tubular [[Adnexa|adnexal]] [[lesion]] with [[fluid]] attenuation | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Dilated [[Fallopian tube]] with [[fluid]] signal intensity | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with [[endometriosis]] (haematosalpinx), [[ovulation]] induction, [[pelvic inflammatory disease]], post-[[hysterectomy]], [[tubal ligation]], and tubal [[malignancy]] | |||
* It may cause [[infertility]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Salpingitis]]<br><ref name="pmid7976247">{{cite journal |vauthors=Czerwenka K, Heuss F, Hosmann J, Manavi M, Jelincic D, Kubista E |title=Salpingitis caused by Chlamydia trachomatis and its significance for infertility |journal=Acta Obstet Gynecol Scand |volume=73 |issue=9 |pages=711–5 |date=October 1994 |pmid=7976247 |doi= |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Women]] of [[reproductive]] age | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | – | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Leukocytosis (patient information)|Leukocytosis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see , [[Edema|edematous]] and thickened endosalpingeal folds | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History/<br>physical<br>exam]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It may cause [[infertility]] | |||
|- | |- | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Fallopian tube cancer|Fallopian tube carcinoma]]<br><ref name="NiloffKlug1984">{{cite journal|last1=Niloff|first1=Jonathan M.|last2=Klug|first2=Thomas L.|last3=Schaetzl|first3=Elena|last4=Zurawski|first4=Vincent R.|last5=Knapp|first5=Robert C.|last6=Bast|first6=Robert C.|title=Elevation of serum CA125 in carcinomas of the fallopian tube, endometrium, and endocervix|journal=American Journal of Obstetrics and Gynecology|volume=148|issue=8|year=1984|pages=1057–1058|issn=00029378|doi=10.1016/S0002-9378(84)90444-7}}</ref> | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Fallopian tube cancer|Fallopian tube carcinoma]]<br><ref name="NiloffKlug1984">{{cite journal|last1=Niloff|first1=Jonathan M.|last2=Klug|first2=Thomas L.|last3=Schaetzl|first3=Elena|last4=Zurawski|first4=Vincent R.|last5=Knapp|first5=Robert C.|last6=Bast|first6=Robert C.|title=Elevation of serum CA125 in carcinomas of the fallopian tube, endometrium, and endocervix|journal=American Journal of Obstetrics and Gynecology|volume=148|issue=8|year=1984|pages=1057–1058|issn=00029378|doi=10.1016/S0002-9378(84)90444-7}}</ref> | ||
| Line 375: | Line 619: | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
* In case of rapid [[uterine]] growth in post [[Menopause|menopausal]] [[women]] we may suspect [[uterine sarcoma]] | * In case of rapid [[uterine]] growth in post [[Menopause|menopausal]] [[women]] we may suspect [[uterine sarcoma]] | ||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Pregnancy]]<br><ref name="CacctatoreTttttnen1990">{{cite journal|last1=Cacctatore|first1=Bruno|last2=Tttttnen|first2=Atla|last3=Stenman|first3=Ulf-Hakan|last4=Ylostalo|first4=Pekka|title=Normal early pregnancy: serum hCG levels and vaginal ultrasonography findings|journal=BJOG: An International Journal of Obstetrics and Gynaecology|volume=97|issue=10|year=1990|pages=899–903|issn=1470-0328|doi=10.1111/j.1471-0528.1990.tb02444.x}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Women]] in [[reproductive]] age (15 -45 y/o) | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/− | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* High level of [[HCG|BhCG]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[Ultrasound|US]] we may see [[gestational sac]], [[yolk sac]], double bleb sign and [[fetal]] pore | |||
* In [[CT scan]] we may see [[cystic]] structure filled with fluid, curvilinear enhancing structure ([[placenta]]) and [[fetal]] pore | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Cystic]] structure filled with fluid | |||
* Curvilinear enhancing structure ([[placenta]]) | |||
* [[Fetal]] pore | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[History and Physical examination|History]]/<br>[[laboratory]]<br>findings | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* We do not perform [[CT scan]] and [[MRI]] in [[pregnancy]] but We may unintentionally image the [[pregnancy]] with [[CT scan]] and [[MRI]]. | |||
|- | |||
! colspan="14" style="background: #7d7d7d; color: #FFFFFF; text-align: center;" |Non-gynecologic | |||
|- | |||
| rowspan="4" style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Gastrointestinal tract|GIT]] | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Appendix|Appendiceal]] [[abscess]]<br><ref name="pmid16037513">{{cite journal |vauthors=Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C |title=CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings |journal=AJR Am J Roentgenol |volume=185 |issue=2 |pages=406–17 |date=August 2005 |pmid=16037513 |doi=10.2214/ajr.185.2.01850406 |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | – | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Leukocytosis]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Fluid collection in the [[appendicular]] region | |||
| | * [[appendicolith]] may be visualized. | ||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Fluid collection in the [[appendicular]] region | |||
* [[appendicolith]] may be visualized. | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* NA | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Imaging]]/<br>[[History and Physical examination|history]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* The most common [[complication]] of [[acute appendicitis]] | |||
* It may cause pleural effusion | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Appendix cancer|Appendiceal neoplasm]]<br><ref name="WHO">Chapter 5: Tumours of the Appendix - IARC. https://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb2/bb2-chap5.pdf Accessed on January 15, 2019</ref><ref name="GoedeCaplin2003">{{cite journal|last1=Goede|first1=A. C.|last2=Caplin|first2=M. E.|last3=Winslet|first3=M. C.|title=Carcinoid tumour of the appendix|journal=British Journal of Surgery|volume=90|issue=11|year=2003|pages=1317–1322|issn=0007-1323|doi=10.1002/bjs.4375}}</ref><ref name="Pablo CarmignaniHampton2004">{{cite journal|last1=Pablo Carmignani|first1=C.|last2=Hampton|first2=Regina|last3=E. Sugarbaker|first3=Christina|last4=Chang|first4=David|last5=H. Sugarbaker|first5=Paul|title=Utility of CEA and CA 19-9 tumor markers in diagnosis and prognostic assessment of mucinous epithelial cancers of the appendix|journal=Journal of Surgical Oncology|volume=87|issue=4|year=2004|pages=162–166|issn=0022-4790|doi=10.1002/jso.20107}}</ref><ref name="pmid20587792">{{cite journal |vauthors=Limsui D, Vierkant RA, Tillmans LS, Wang AH, Weisenberger DJ, Laird PW, Lynch CF, Anderson KE, French AJ, Haile RW, Harnack LJ, Potter JD, Slager SL, Smyrk TC, Thibodeau SN, Cerhan JR, Limburg PJ |title=Cigarette smoking and colorectal cancer risk by molecularly defined subtypes |journal=J. Natl. Cancer Inst. |volume=102 |issue=14 |pages=1012–22 |date=July 2010 |pmid=20587792 |pmc=2915616 |doi=10.1093/jnci/djq201 |url=}}</ref><ref name="pmid2886072">{{cite journal |vauthors=Duh QY, Hybarger CP, Geist R, Gamsu G, Goodman PC, Gooding GA, Clark OH |title=Carcinoids associated with multiple endocrine neoplasia syndromes |journal=Am. J. Surg. |volume=154 |issue=1 |pages=142–8 |date=July 1987 |pmid=2886072 |doi= |url=}}</ref> | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* 60-70 y/o for [[adenocarcinoma]], | |||
* 30-50 y/o for [[Carcinoid cancer|carcinoid]] tumors | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | – | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | – | |||
| style="background: #F5F5F5; padding: 5px; text-align: center;" | +/– | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[adenocarcinoma]] type we may have high levels of [[CEA]] and [[CA 19-9]] | |||
* In [[Carcinoid cancer|carcinoid]] type we may see high levels of [[chromogranin A]], [[5-HIAA]] and Ki67 | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* In [[CT scan]] we may see: | |||
** [[Soft tissue]] thickening and Cystic lesion with Internal septation | |||
** Wall irregularity | |||
** [[Calcification]] | |||
** Peri-[[Appendix|appendiceal]] fat stranding | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Soft tissue mass in the [[appendix]] | |||
* We may see invasion to other structures | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* Gray/yellowi color | |||
* Cystic structures with angiolymphatic invasion | |||
[ | * | ||
| style="background: #F5F5F5; padding: 5px;" | | |||
* [[Biopsy]] | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
* It is associated with: | |||
** [[MEN1 syndrome]] | |||
** [[Ulcerative colitis]] | |||
** [[Neurofibromatosis type 1]] | |||
** [[HNPCC]] | |||
** [[Smoking]] | |||
* It may cause pleural effusion | |||
|} | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*Ovarian sarcoma is one of the least common gynecologic malignancy, constituting approximately 1% of all ovarian malignancies.<ref name="HarrisDelap2003">{{cite journal|last1=Harris|first1=M A|last2=Delap|first2=L M|last3=Sengupta|first3=P S|last4=Wilkinson|first4=P M|last5=Welch|first5=R S|last6=Swindell|first6=R|last7=Shanks|first7=J H|last8=Wilson|first8=G|last9=Slade|first9=R J|last10=Reynolds|first10=K|last11=Jayson|first11=G C|title=Carcinosarcoma of the ovary|journal=British Journal of Cancer|volume=88|issue=5|year=2003|pages=654–657|issn=0007-0920|doi=10.1038/sj.bjc.6600770}}</ref><ref name="FerlaySoerjomataram2015">{{cite journal|last1=Ferlay|first1=Jacques|last2=Soerjomataram|first2=Isabelle|last3=Dikshit|first3=Rajesh|last4=Eser|first4=Sultan|last5=Mathers|first5=Colin|last6=Rebelo|first6=Marise|last7=Parkin|first7=Donald Maxwell|last8=Forman|first8=David|last9=Bray|first9=Freddie|title=Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012|journal=International Journal of Cancer|volume=136|issue=5|year=2015|pages=E359–E386|issn=00207136|doi=10.1002/ijc.29210}}</ref><ref name="FerlayShin2010">{{cite journal|last1=Ferlay|first1=Jacques|last2=Shin|first2=Hai-Rim|last3=Bray|first3=Freddie|last4=Forman|first4=David|last5=Mathers|first5=Colin|last6=Parkin|first6=Donald Maxwell|title=Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008|journal=International Journal of Cancer|volume=127|issue=12|year=2010|pages=2893–2917|issn=00207136|doi=10.1002/ijc.25516}}</ref><ref name="pmid15761078">{{cite journal| author=Parkin DM, Bray F, Ferlay J, Pisani P| title=Global cancer statistics, 2002. | journal=CA Cancer J Clin | year= 2005 | volume= 55 | issue= 2 | pages= 74-108 | pmid=15761078 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15761078 }} </ref><ref name="pmid1410056">{{cite journal| author=Cresanta JL| title=Epidemiology of cancer in the United States. | journal=Prim Care | year= 1992 | volume= 19 | issue= 3 | pages= 419-41 | pmid=1410056 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1410056 }} </ref><ref name="BrayFerlay2018">{{cite journal|last1=Bray|first1=Freddie|last2=Ferlay|first2=Jacques|last3=Soerjomataram|first3=Isabelle|last4=Siegel|first4=Rebecca L.|last5=Torre|first5=Lindsey A.|last6=Jemal|first6=Ahmedin|title=Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries|journal=CA: A Cancer Journal for Clinicians|volume=68|issue=6|year=2018|pages=394–424|issn=00079235|doi=10.3322/caac.21492}}</ref> | *Ovarian sarcoma is one of the least common [[Gynecologic Malignancies|gynecologic malignancy]], constituting approximately 1% of all ovarian malignancies.<ref name="HarrisDelap2003">{{cite journal|last1=Harris|first1=M A|last2=Delap|first2=L M|last3=Sengupta|first3=P S|last4=Wilkinson|first4=P M|last5=Welch|first5=R S|last6=Swindell|first6=R|last7=Shanks|first7=J H|last8=Wilson|first8=G|last9=Slade|first9=R J|last10=Reynolds|first10=K|last11=Jayson|first11=G C|title=Carcinosarcoma of the ovary|journal=British Journal of Cancer|volume=88|issue=5|year=2003|pages=654–657|issn=0007-0920|doi=10.1038/sj.bjc.6600770}}</ref><ref name="FerlaySoerjomataram2015">{{cite journal|last1=Ferlay|first1=Jacques|last2=Soerjomataram|first2=Isabelle|last3=Dikshit|first3=Rajesh|last4=Eser|first4=Sultan|last5=Mathers|first5=Colin|last6=Rebelo|first6=Marise|last7=Parkin|first7=Donald Maxwell|last8=Forman|first8=David|last9=Bray|first9=Freddie|title=Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012|journal=International Journal of Cancer|volume=136|issue=5|year=2015|pages=E359–E386|issn=00207136|doi=10.1002/ijc.29210}}</ref><ref name="FerlayShin2010">{{cite journal|last1=Ferlay|first1=Jacques|last2=Shin|first2=Hai-Rim|last3=Bray|first3=Freddie|last4=Forman|first4=David|last5=Mathers|first5=Colin|last6=Parkin|first6=Donald Maxwell|title=Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008|journal=International Journal of Cancer|volume=127|issue=12|year=2010|pages=2893–2917|issn=00207136|doi=10.1002/ijc.25516}}</ref><ref name="pmid15761078">{{cite journal| author=Parkin DM, Bray F, Ferlay J, Pisani P| title=Global cancer statistics, 2002. | journal=CA Cancer J Clin | year= 2005 | volume= 55 | issue= 2 | pages= 74-108 | pmid=15761078 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15761078 }} </ref><ref name="pmid1410056">{{cite journal| author=Cresanta JL| title=Epidemiology of cancer in the United States. | journal=Prim Care | year= 1992 | volume= 19 | issue= 3 | pages= 419-41 | pmid=1410056 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1410056 }} </ref><ref name="BrayFerlay2018">{{cite journal|last1=Bray|first1=Freddie|last2=Ferlay|first2=Jacques|last3=Soerjomataram|first3=Isabelle|last4=Siegel|first4=Rebecca L.|last5=Torre|first5=Lindsey A.|last6=Jemal|first6=Ahmedin|title=Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries|journal=CA: A Cancer Journal for Clinicians|volume=68|issue=6|year=2018|pages=394–424|issn=00079235|doi=10.3322/caac.21492}}</ref> | ||
*In 2012, approximately 239,000 women were diagnosed with ovarian cancer worldwide, and 152,000 died of the disease. | *In 2012, approximately 239,000 [[women]] were [[Diagnose|diagnosed]] with [[ovarian cancer]] worldwide, and 152,000 died of the [[disease]]. | ||
*Patients of all age groups may develop sarcoma of the ovary both postmenopausal and premenopausal women. | *[[Patients]] of all [[age]] groups may develop [[sarcoma]] of the [[ovary]] both [[postmenopausal]] and [[premenopausal]] [[women]]. | ||
*The incidence of ovarian Sarcoma increases with age; the median age at diagnosis is 50-60 years. | *The [[incidence]] of ovarian Sarcoma increases with [[age]]; the median [[age]] at [[diagnosis]] is 50-60 years. | ||
*There is no racial predilection to ovarian Sarcoma | *There is no [[racial]] predilection to ovarian Sarcoma | ||
==Risk Factors== | ==Risk Factors== | ||
There are no established risk factors for | There are no established risk factors for ovarian sarcoma | ||
==Screening== | ==Screening== | ||
| Line 410: | Line 727: | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
*Ovarian carcinosarcomas follow a distinct natural history compared to other more common epithelial carcinomas<ref name="pmid15099970">Barnholtz-Sloan JS, Morris R, Malone JM, Munkarah AR (2004) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=15099970 Survival of women diagnosed with malignant, mixed mullerian tumors of the ovary (OMMMT).] ''Gynecol Oncol'' 93 (2):506-12. [http://dx.doi.org/10.1016/j.ygyno.2004.02.016 DOI:10.1016/j.ygyno.2004.02.016] PMID: [https://pubmed.gov/15099970 15099970]</ref><ref name="pmid21420726">Rauh-Hain JA, Growdon WB, Rodriguez N, Goodman AK, Boruta DM, Schorge JO et al. (2011) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=21420726 Carcinosarcoma of the ovary: a case-control study.] ''Gynecol Oncol'' 121 (3):477-81. [http://dx.doi.org/10.1016/j.ygyno.2011.02.023 DOI:10.1016/j.ygyno.2011.02.023] PMID: [https://pubmed.gov/21420726 21420726]</ref><ref name="pmid9576296">Sood AK, Sorosky JI, Gelder MS, Buller RE, Anderson B, Wilkinson EJ et al. (1998) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=9576296 Primary ovarian sarcoma: analysis of prognostic variables and the role of surgical cytoreduction.] ''Cancer'' 82 (9):1731-7. PMID: [https://pubmed.gov/9576296 9576296]</ref><ref name="pmid27761279">Cicin İ, Özatlı T, Türkmen E, Özturk T, Özçelik M, Çabuk D et al. (2016) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=27761279 Predictive and Prognostic Factors in Ovarian and Uterine Carcinosarcomas.] ''Balkan Med J'' 33 (5):517-524. [http://dx.doi.org/10.5152/balkanmedj.2016.151268 DOI:10.5152/balkanmedj.2016.151268] PMID: [https://pubmed.gov/27761279 27761279]</ref> | |||
*Ovarian carcinosarcomas are aggressive neoplasms with a predilection towards early dissemination. | |||
*Prognostic factors for this tumor type remain unclear because of its rarity. | *Prognostic factors for this tumor type remain unclear because of its rarity. | ||
*Prognosis is generally poor, and the 5-year survival rate of patients with ovarian sarcoma is approximately 28.2%. | *Prognosis is generally poor, and the 5-year survival rate of patients with ovarian sarcoma is approximately 28.2%. | ||
| Line 420: | Line 734: | ||
==Diagnostic Study of Choice== | ==Diagnostic Study of Choice== | ||
*There are no established criteria for the diagnosis of ovarian sarcoma | |||
*Biopsy is the study of choice | |||
There are no established criteria for the diagnosis of | |||
==History and Symptoms== | ==History and Symptoms== | ||
| Line 461: | Line 765: | ||
==Electrocardiogram== | ==Electrocardiogram== | ||
There are no ECG findings associated with | There are no ECG findings associated with ovarian sarcoma. | ||
==X-ray== | ==X-ray== | ||
| Line 474: | Line 774: | ||
==CT scan== | ==CT scan== | ||
*CT scan may be helpful in the diagnosis of ovarian sarcoma . Findings on CT scan suggestive of ovarian sarcoma include:<ref name="pmid26587944">{{cite journal| author=Miccò M, Sala E, Lakhman Y, Hricak H, Vargas HA| title=Imaging Features of Uncommon Gynecologic Cancers. | journal=AJR Am J Roentgenol | year= 2015 | volume= 205 | issue= 6 | pages= 1346-59 | pmid=26587944 | doi=10.2214/AJR.14.12695 | pmc=5502476 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26587944 }} </ref><ref name="pmid21419327">{{cite journal| author=Bell DJ, Pannu HK| title=Radiological assessment of gynecologic malignancies. | journal=Obstet Gynecol Clin North Am | year= 2011 | volume= 38 | issue= 1 | pages= 45-68, vii | pmid=21419327 | doi=10.1016/j.ogc.2011.02.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21419327 }} </ref><ref name="pmid10472090">{{cite journal| author=Forstner R, Graf A| title=[Diagnostic imaging in staging of gynecologic carcinomas]. | journal=Radiologe | year= 1999 | volume= 39 | issue= 7 | pages= 610-8 | pmid=10472090 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10472090 }} </ref> | |||
==MRI== | ==MRI== | ||
*MRI may be helpful in the diagnosis of ovarian sarcoma. Findings on MRI suggestive of ovarian sarcoma include the following:<ref name="pmid27027614">{{cite journal| author=Manoharan D, Das CJ, Aggarwal A, Gupta AK| title=Diffusion weighted imaging in gynecological malignancies - present and future. | journal=World J Radiol | year= 2016 | volume= 8 | issue= 3 | pages= 288-97 | pmid=27027614 | doi=10.4329/wjr.v8.i3.288 | pmc=4807338 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27027614 }} </ref><ref name="pmid26587944">{{cite journal| author=Miccò M, Sala E, Lakhman Y, Hricak H, Vargas HA| title=Imaging Features of Uncommon Gynecologic Cancers. | journal=AJR Am J Roentgenol | year= 2015 | volume= 205 | issue= 6 | pages= 1346-59 | pmid=26587944 | doi=10.2214/AJR.14.12695 | pmc=5502476 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26587944 }} </ref><ref name="pmid10472090">{{cite journal| author=Forstner R, Graf A| title=[Diagnostic imaging in staging of gynecologic carcinomas]. | journal=Radiologe | year= 1999 | volume= 39 | issue= 7 | pages= 610-8 | pmid=10472090 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10472090 }} </ref><ref name="pmid22037656">{{cite journal| author=Alt CD, Brocker KA, Eichbaum M, Sohn C, Arnegger FU, Kauczor HU et al.| title=Imaging of female pelvic malignancies regarding MRI, CT, and PET/CT: Part 2. | journal=Strahlenther Onkol | year= 2011 | volume= 187 | issue= 11 | pages= 705-14 | pmid=22037656 | doi=10.1007/s00066-011-4002-z | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22037656 }} </ref><ref name="pmid21419327">{{cite journal| author=Bell DJ, Pannu HK| title=Radiological assessment of gynecologic malignancies. | journal=Obstet Gynecol Clin North Am | year= 2011 | volume= 38 | issue= 1 | pages= 45-68, vii | pmid=21419327 | doi=10.1016/j.ogc.2011.02.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21419327 }} </ref> | |||
** | |||
==Other Imaging Findings== | ==Other Imaging Findings== | ||
There are no other imaging findings associated with | There are no other imaging findings associated with ovarian sarcoma | ||
==Other Diagnostic Studies== | ==Other Diagnostic Studies== | ||
Latest revision as of 19:46, 26 August 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Maneesha Nandimandalam, M.B.B.S.[2]
Overview
Ovarian carcinosarcoma, which is also known as a malignant mixed mullerian tumor (MMMT) of the ovary, is a rare, aggressive cancer of the ovary with two distinct characteristic cancer types i.e carcinoma and sarcoma. Primary ovarian sarcomas occur as pure sarcomas or mixed mullerian tumors (MMTs). Ovarian sarcoma is one of the least common gynecologic malignancy, constituting approximately 1% of all ovarian malignancies. Prognosis is generally poor, and the 5-year survival rate of patients with ovarian sarcoma is approximately 28.2%. Most of the women are asymptomatic, when present, symptoms may include, pain in the abdomen or pelvic area, bloating or swelling of the abdomen, quickly feeling full when eating, other digestive problems. An elevated concentration of CA-125 in serum is seen in some patients of ovarian sarcoma. Biopsy is the study of choice. Findings on MRI suggestive of ovarian sarcoma include the following. Surgery is the mainstay of treatment for ovarian sarcoma.Among all chemotherapeutic regimens that are being used to treat ovarian sarcoma, they are divided into two groups like platinum containing regimens and non-platinum regimens. Cisplatin, carboplatin are commonly used.
Historical Perspective
There is limited information available about the historical perspective of ovarian sarcoma
Classification
- There is no established system for the classification of ovarian sarcoma.[1][2][3]
- Primary ovarian sarcomas occur as pure sarcomas or mixed mullerian tumors (MMTs).
- Pure sarcomas are comprised of a single malignant mesenchymal element and are further categorized as:
- Stromal cell sarcomas
- Fibrosarcomas
- Leiomyosarcomas
- Neurofibrosarcomas
- Rhabdomyosarcomas
- Chondrosarcomas
- Angiosarcomas
- Liposarcomas
- On the other hand mixed mullerian tumors(MMTs) are defined by the presence of both carcinomatous and sarcomatous elements and are more common than pure sarcomas.
- Ovarian MMTs can be further classified as homologous or heterologous on the basis of the tissue components present.
- Homologous tumors contain elements that are native to the ovary whereas heterologous tumors contain elements that normally are not present in the ovary.
The staging of [malignancy name] is based on the [staging system].
OR
There is no established system for the staging of [malignancy name].
Pathophysiology
- The exact pathogenesis of ovarian sarcoma is not fully understood[4][3]
- Clonal loss of the wild-type BRCA2 allele as well as the same somatic mutation of the TP53 gene was evident in histologic components
Causes
The exact causes of ovarian sarcoma have not been identified.
Differentiating ovarian sarcoma from Other Diseases
On the basis of age of onset, vaginal discharge, and constitutional symptoms, ovarian cancer must be differentiated from tubo-ovarian abscess, ectopic pregnancy, hydrosalpinx, salpingitis, fallopian tube carcinoma, uterine leiomyoma, choriocarcinoma, leiomyosarcoma, pregnancy, appendiceal abscess, appendiceal neoplasm, diverticular abscess, colorectal cancer, pelvic kidney, advanced bladder cancer, and retroperitoneal sarcoma.
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard | Additional findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age of onset | Symptoms | Physical examination | |||||||||||
| Lab Findings | Imaging | Immunohistopathology | |||||||||||
| pelvic/abdominal pain or pressure | vaginal bleeding/discharge | GI dysturbance | Fever | Tenderness | CT scan/US | MRI | |||||||
| Gynecologic | |||||||||||||
| Ovarian | Follicular cysts [5] |
|
+/– | – | – | – | +/– |
|
|
|
| ||
| Theca lutein cysts [6][7][8] |
|
+/– | – | – | – | +/– |
|
|
|
| |||
| Serous cystadenoma/carcinoma [9][10][11][12] |
|
+/– | – | – | – | +/– |
|
|
| ||||
| Mucinous cystadenoma/carcinoma [13][14][15] |
|
+/– | – | – | – | +/– |
|
|
|
|
| ||
| Endometrioma [16][17][18] |
|
+ | + | +/– | – | + |
|
|
|
| |||
| Teratoma [19][20][21][22]
|
|
+/– | – | – | – | +/– |
|
|
| ||||
| Dysgerminoma [23][24] |
|
+ | +/– | – | – | +/– |
|
|
|
||||
| Yolk sac tumor [25][26][27] |
+ | – | – | – | + |
|
|
|
|
| |||
| Fibroma [28][29][30] |
|
|
– | – | – | +/– |
|
|
|
| |||
| Thecoma [31][32][33] |
|
+/– | – | – | – |
|
|
|
|
| |||
| Granulosa cell tumor [34][35][36][37] |
|
+ | +/– | – | – |
|
| ||||||
| Sertoli-leydig cell tumor [38][39] |
|
+/– | – | – | – | – |
|
|
|
| |||
| Brenner tumor [40][41] |
|
+/– | – | – | – | – | – |
|
|
|
| ||
| Krukenberg tumor [42][43] |
|
+/– | – | +/–
Based on underlying malignancy |
– | – |
|
|
|
| |||
| Tubal | tubo-ovarian abscess [44][45][46][47] |
|
+ | + | – | + | + |
|
|
|
| ||
| Ectopic pregnancy [48] |
|
+ | + | +/– | – | + |
|
|
|
|
| ||
| Hydrosalpinx [49][50][51] |
|
+ | – | – | – | +/– | – |
|
|
| |||
| Salpingitis [52] |
|
+ | + | – | + | + |
|
|
| ||||
| Fallopian tube carcinoma [53] |
|
+ | + | + | – | +/– |
|
|
|
| |||
| Uterine | Leiomyoma [54][55] |
|
+ | + | – | – | +/– |
|
| ||||
| Choriocarcinoma [56][57][58][59] |
|
+ | + | +/– | – | + |
|
|
|
| |||
| Leiomyosarcoma [60][61][62][63][64] |
|
+ | + | – | – | +/– |
|
|
|
| |||
| Pregnancy [65] |
|
+/− | +/− | +/− | – | – |
|
|
|
||||
| Non-gynecologic | |||||||||||||
| GIT | Appendiceal abscess [66] |
|
+ | – | + | +/– | + |
|
|
|
| ||
| Appendiceal neoplasm [67][68][69][70][71] |
|
+ | – | + | – | +/– |
|
|
|
|
| ||
Epidemiology and Demographics
- Ovarian sarcoma is one of the least common gynecologic malignancy, constituting approximately 1% of all ovarian malignancies.[1][72][73][74][75][76]
- In 2012, approximately 239,000 women were diagnosed with ovarian cancer worldwide, and 152,000 died of the disease.
- Patients of all age groups may develop sarcoma of the ovary both postmenopausal and premenopausal women.
- The incidence of ovarian Sarcoma increases with age; the median age at diagnosis is 50-60 years.
- There is no racial predilection to ovarian Sarcoma
Risk Factors
There are no established risk factors for ovarian sarcoma
Screening
There is insufficient evidence to recommend routine screening for ovarian sarcoma.
Natural History, Complications, and Prognosis
- Ovarian carcinosarcomas follow a distinct natural history compared to other more common epithelial carcinomas[77][3][78][79]
- Ovarian carcinosarcomas are aggressive neoplasms with a predilection towards early dissemination.
- Prognostic factors for this tumor type remain unclear because of its rarity.
- Prognosis is generally poor, and the 5-year survival rate of patients with ovarian sarcoma is approximately 28.2%.
- Some possible factors such as age and menopausal status have been proposed.
Diagnostic Study of Choice
- There are no established criteria for the diagnosis of ovarian sarcoma
- Biopsy is the study of choice
History and Symptoms
Most of the women are asymptomatic, when present, symptoms may include:[80][81][82]
- Pain in the abdomen or pelvic area
- Bloating or swelling of the abdomen
- Quickly feeling full when eating
- Other digestive problems
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
- An elevated concentration of CA-125 in serum is seen in some patients of ovarian sarcoma.[83][84][85]
- There are no diagnostic laboratory findings associated with ovarian sarcoma.
Electrocardiogram
There are no ECG findings associated with ovarian sarcoma.
X-ray
There are no x-ray findings associated with ovarian Sarcoma.
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with ovarian Sarcoma.
CT scan
- CT scan may be helpful in the diagnosis of ovarian sarcoma . Findings on CT scan suggestive of ovarian sarcoma include:[86][87][88]
MRI
- MRI may be helpful in the diagnosis of ovarian sarcoma. Findings on MRI suggestive of ovarian sarcoma include the following:[89][86][88][90][87]
Other Imaging Findings
There are no other imaging findings associated with ovarian sarcoma
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no medical treatment for ovarian sarcoma, the mainstay of therapy is surgery and chemotherapy.
Surgery
- Surgery is the mainstay of treatment for ovarian sarcoma.
- The management is similar to that of epithelial carcinoma of ovary, consisting of cytoreductive surgery followed by adjuvant chemotherapy.
Chemotherapy
- Chemotherapy with various regimens has been used in different centers without defined conclusions on efficacy[81][82][91][92][93]
- Multiple chemotherapeutic regimens have been evaluated with modest response rates ranging from 12% to 100%.
- Among all chemotherapeutic regimens that are being used, they are divided into two groups like platinum containing regimens and non-platinum regimens.
- Platinum containing chemotherapy regimens
- Carboplatin and ifosfamide (Carbo-I)
- Carboplatin (Carbo)
- Cyclophosphamide, adriamycin and cisplatin (CAP)
- Carboplatin and cyclophosphamide (Carbo-C)
- Epirubicin, carboplatin and 5FU (E-Carbo-F)
- Epirubicin, cisplatin and 5FU (ECF)
- Taxol and Carboplatin (T-Carbo)
- Other chemotherapy regimens
- Doxorubicin (A)
- Doxorubicin and cyclophosphamide (AC)
- Cyclophosphamide (IV)
- Cyclophosphamide (oral)
- Melphalan
Primary Prevention
There are no established measures for the primary prevention of ovarian sarcoma.
Secondary Prevention
There are no established measures for the secondary prevention of ovarian sarcoma.
References
- ↑ 1.0 1.1 Harris, M A; Delap, L M; Sengupta, P S; Wilkinson, P M; Welch, R S; Swindell, R; Shanks, J H; Wilson, G; Slade, R J; Reynolds, K; Jayson, G C (2003). "Carcinosarcoma of the ovary". British Journal of Cancer. 88 (5): 654–657. doi:10.1038/sj.bjc.6600770. ISSN 0007-0920.
- ↑ Makris GM, Siristatidis C, Battista MJ, Chrelias C (2015). "Ovarian carcinosarcoma: a case report, diagnosis, treatment and literature review". Hippokratia. 19 (3): 256–9. PMC 4938474. PMID 27418786.
- ↑ 3.0 3.1 3.2 Rauh-Hain JA, Growdon WB, Rodriguez N, Goodman AK, Boruta DM, Schorge JO; et al. (2011). "Carcinosarcoma of the ovary: a case-control study". Gynecol Oncol. 121 (3): 477–81. doi:10.1016/j.ygyno.2011.02.023. PMID 21420726.
- ↑ Vargas AN (2014). "Natural history of ovarian cancer". Ecancermedicalscience. 8: 465. doi:10.3332/ecancer.2014.465. PMC 4176445. PMID 25371706.
- ↑ Levine D, Brown DL, Andreotti RF, Benacerraf B, Benson CB, Brewster WR, Coleman B, Depriest P, Doubilet PM, Goldstein SR, Hamper UM, Hecht JL, Horrow M, Hur HC, Marnach M, Patel MD, Platt LD, Puscheck E, Smith-Bindman R (September 2010). "Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement". Radiology. 256 (3): 943–54. doi:10.1148/radiol.10100213. PMID 20505067.
- ↑ Montz FJ, Schlaerth JB, Morrow CP (August 1988). "The natural history of theca lutein cysts". Obstet Gynecol. 72 (2): 247–51. PMID 2455880.
- ↑ Southam, Anna L. (1962). "Massive Ovarian Hyperstimulation with Clomiphene Citrate". JAMA: The Journal of the American Medical Association. 181 (5): 443. doi:10.1001/jama.1962.03050310083018b. ISSN 0098-7484.
- ↑ Nguyen, K T; Reid, R L; Sauerbrei, E (1986). "Antenatal sonographic detection of a fetal theca lutein cyst: a clue to maternal diabetes mellitus". Journal of Ultrasound in Medicine. 5 (11): 665–667. doi:10.7863/jum.1986.5.11.665. ISSN 0278-4297.
- ↑ Jung, Seung Eun; Lee, Jae Mun; Rha, Sung Eun; Byun, Jae Young; Jung, Jung Im; Hahn, Seong Tai (2002). "CT and MR Imaging of Ovarian Tumors with Emphasis on Differential Diagnosis". RadioGraphics. 22 (6): 1305–1325. doi:10.1148/rg.226025033. ISSN 0271-5333.
- ↑ Imai, Shunsuke; Kiyozuka, Yasuhiko; Maeda, Hiroko; Noda, Tuneo; Hosick, Howard L. (1990). "Establishment and Characterization of a Human Ovarian Serous Cystadenocarcinoma Cell Line That Produces the Tumor Markers CA-125 and Tissue Polypeptide Antigen". Oncology. 47 (2): 177–184. doi:10.1159/000226813. ISSN 0030-2414.
- ↑ Malpica A, Deavers MT, Lu K, Bodurka DC, Atkinson EN, Gershenson DM, Silva EG (April 2004). "Grading ovarian serous carcinoma using a two-tier system". Am. J. Surg. Pathol. 28 (4): 496–504. PMID 15087669.
- ↑ Li J, Fadare O, Xiang L, Kong B, Zheng W (March 2012). "Ovarian serous carcinoma: recent concepts on its origin and carcinogenesis". J Hematol Oncol. 5: 8. doi:10.1186/1756-8722-5-8. PMID 22405464.
- ↑ Hoerl HD, Hart WR (December 1998). "Primary ovarian mucinous cystadenocarcinomas: a clinicopathologic study of 49 cases with long-term follow-up". Am. J. Surg. Pathol. 22 (12): 1449–62. PMID 9850171.
- ↑ Lee KR, Scully RE (November 2000). "Mucinous tumors of the ovary: a clinicopathologic study of 196 borderline tumors (of intestinal type) and carcinomas, including an evaluation of 11 cases with 'pseudomyxoma peritonei'". Am. J. Surg. Pathol. 24 (11): 1447–64. PMID 11075847.
- ↑ Jung, Seung Eun; Lee, Jae Mun; Rha, Sung Eun; Byun, Jae Young; Jung, Jung Im; Hahn, Seong Tai (2002). "CT and MR Imaging of Ovarian Tumors with Emphasis on Differential Diagnosis". RadioGraphics. 22 (6): 1305–1325. doi:10.1148/rg.226025033. ISSN 0271-5333.
- ↑ Mol BW, Bayram N, Lijmer JG, Wiegerinck MA, Bongers MY, van der Veen F, Bossuyt PM (December 1998). "The performance of CA-125 measurement in the detection of endometriosis: a meta-analysis". Fertil. Steril. 70 (6): 1101–8. PMID 9848302.
- ↑ Kinkel, Karen; Frei, Kathrin A.; Balleyguier, Corinne; Chapron, Charles (2005). "Diagnosis of endometriosis with imaging: a review". European Radiology. 16 (2): 285–298. doi:10.1007/s00330-005-2882-y. ISSN 0938-7994.
- ↑ de Ziegler, Dominique; Borghese, Bruno; Chapron, Charles (2010). "Endometriosis and infertility: pathophysiology and management". The Lancet. 376 (9742): 730–738. doi:10.1016/S0140-6736(10)60490-4. ISSN 0140-6736.
- ↑ Kawai, Michiyasu; Kano, Takeo; Kikkawa, Fumitaka; Morikawa, Yoshimitsu; Oguchi, Hidenori; Nakashima, Nobuo; Ishizuka, Takao; Kuzuya, Kazuo; Ohta, Masahiro; Arii, Yoshitaro; Tomoda, Yutaka (1992). "Seven tumor markers in benign and malignant germ cell tumors of the ovary". Gynecologic Oncology. 45 (3): 248–253. doi:10.1016/0090-8258(92)90299-X. ISSN 0090-8258.
- ↑ Dunzendorfer, Thomas; deLAS MORENAS, ANTONIO; Kalir, Tamara; Levin, Robert M. (1999). "Struma Ovarii and Hyperthyroidism". Thyroid. 9 (5): 499–502. doi:10.1089/thy.1999.9.499. ISSN 1050-7256.
- ↑ Outwater, Eric K.; Siegelman, Evan S.; Hunt, Jennifer L. (2001). "Ovarian Teratomas: Tumor Types and Imaging Characteristics". RadioGraphics. 21 (2): 475–490. doi:10.1148/radiographics.21.2.g01mr09475. ISSN 0271-5333.
- ↑ Saba, Luca; Guerriero, Stefano; Sulcis, Rosa; Virgilio, Bruna; Melis, GianBenedetto; Mallarini, Giorgio (2009). "Mature and immature ovarian teratomas: CT, US and MR imaging characteristics". European Journal of Radiology. 72 (3): 454–463. doi:10.1016/j.ejrad.2008.07.044. ISSN 0720-048X.
- ↑ Dgani, R.; Shoham(Schwartz), Z.; Czernobilsky, B.; Kaftori, A.; Borenstein, R.; Lancet, M. (1988). "Lactic dehydrogenase, alkaline phosphatase and human chorionic gonadotropin in a pure ovarian dysgerminoma". Gynecologic Oncology. 30 (1): 44–50. doi:10.1016/0090-8258(88)90044-3. ISSN 0090-8258.
- ↑ Tanaka YO, Kurosaki Y, Nishida M, Michishita N, Kuramoto K, Itai Y, Kubo T (1994). "Ovarian dysgerminoma: MR and CT appearance". J Comput Assist Tomogr. 18 (3): 443–8. PMID 8188914.
- ↑ Yang, Grace C.H. (2000). "Fine-needle aspiration cytology of Schiller-Duval bodies of yolk-sac tumor". Diagnostic Cytopathology. 23 (4): 228–232. doi:10.1002/1097-0339(200010)23:4<228::AID-DC2>3.0.CO;2-M. ISSN 8755-1039.
- ↑ Levitin, A; Haller, K D; Cohen, H L; Zinn, D L; O'Connor, M T (1996). "Endodermal sinus tumor of the ovary: imaging evaluation". American Journal of Roentgenology. 167 (3): 791–793. doi:10.2214/ajr.167.3.8751702. ISSN 0361-803X.
- ↑ Talerman, A.; Haije, W. G. (1974). "Alpha-fetoprotein and germ cell tumors: A possible role of yolk sac tumor in production of alpha-fetoprotein". Cancer. 34 (5): 1722–1726. doi:10.1002/1097-0142(197411)34:5<1722::AID-CNCR2820340521>3.0.CO;2-F. ISSN 0008-543X.
- ↑ MEIGS JV (May 1954). "Fibroma of the ovary with ascites and hydrothorax; Meigs' syndrome". Am. J. Obstet. Gynecol. 67 (5): 962–85. PMID 13148256.
- ↑ Sivanesaratnam, V.; Dutta, R.; Jayalakshmi, P. (1990). "Ovarian fibroma - clinical and histopathological characteristics". International Journal of Gynecology & Obstetrics. 33 (3): 243–247. doi:10.1016/0020-7292(90)90009-A. ISSN 0020-7292.
- ↑ Abad, Antonio; Cazorla, Eduardo; Ruiz, Fernando; Aznar, Ismael; Asins, Enrique; Llixiona, Joaquin (1999). "Meigs' syndrome with elevated CA125: case report and review of the literature". European Journal of Obstetrics & Gynecology and Reproductive Biology. 82 (1): 97–99. doi:10.1016/S0301-2115(98)00174-2. ISSN 0301-2115.
- ↑ Yaghoobian, Jahanguir; Pinck, Robert L. (1983). "Ultrasound findings in thecoma of the ovary". Journal of Clinical Ultrasound. 11 (2): 91–93. doi:10.1002/jcu.1870110207. ISSN 0091-2751.
- ↑ Li, Xinchun; Zhang, Weidong; Zhu, Guangbin; Sun, Congpeng; Liu, Qingyu; Shen, Yuechun (2012). "Imaging Features and Pathologic Characteristics of Ovarian Thecoma". Journal of Computer Assisted Tomography. 36 (1): 46–53. doi:10.1097/RCT.0b013e31823f6186. ISSN 0363-8715.
- ↑ Proctor, Francis E.; Greeley, Joseph P.; Rathmell, Thomas K. (1951). "Malignant thecoma of the ovary". American Journal of Obstetrics and Gynecology. 62 (1): 185–192. doi:10.1016/0002-9378(51)91109-X. ISSN 0002-9378.
- ↑ Pectasides D, Pectasides E, Psyrri A (February 2008). "Granulosa cell tumor of the ovary". Cancer Treat. Rev. 34 (1): 1–12. doi:10.1016/j.ctrv.2007.08.007. PMID 17945423.
- ↑ Stenwig, Jan Trygve; Hazekamp, Johan The.; Beecham, Jackson B. (1979). "Granulosa cell tumors of the ovary. A clinicopathological study of 118 cases with long-term follow-up". Gynecologic Oncology. 7 (2): 136–152. doi:10.1016/0090-8258(79)90090-8. ISSN 0090-8258.
- ↑ Morikawa K, Hatabu H, Togashi K, Kataoka ML, Mori T, Konishi J (1997). "Granulosa cell tumor of the ovary: MR findings". J Comput Assist Tomogr. 21 (6): 1001–4. PMID 9386298.
- ↑ Ko SF, Wan YL, Ng SH, Lee TY, Lin JW, Chen WJ, Kung FT, Tsai CC (May 1999). "Adult ovarian granulosa cell tumors: spectrum of sonographic and CT findings with pathologic correlation". AJR Am J Roentgenol. 172 (5): 1227–33. doi:10.2214/ajr.172.5.10227493. PMID 10227493.
- ↑ Lantzsch, T.; Stoerer, S.; Lawrenz, K.; Buchmann, J.; Strauss, H.-G.; Koelbl, H. (2001). "Sertoli-Leydig cell tumor". Archives of Gynecology and Obstetrics. 264 (4): 206–208. doi:10.1007/s004040000114. ISSN 0932-0067.
- ↑ Jung, Seung Eun; Rha, Sung Eun; Lee, Jae Mun; Park, Soo Youn; Oh, Soon Nam; Cho, Kyoung Sik; Lee, Eun Ju; Byun, Jae Young; Hahn, Seong Tai (2005). "CT and MRI Findings of Sex Cord–Stromal Tumor of the Ovary". American Journal of Roentgenology. 185 (1): 207–215. doi:10.2214/ajr.185.1.01850207. ISSN 0361-803X.
- ↑ Shevchuk, Maria M.; Fenoglio, Cecilia M.; Richart, Ralph M. (1980). "Histogenesis of brenner tumors, I: Histology and ultrastructure". Cancer. 46 (12): 2607–2616. doi:10.1002/1097-0142(19801215)46:12<2607::AID-CNCR2820461213>3.0.CO;2-Q. ISSN 0008-543X.
- ↑ Outwater, Eric K; Siegelman, Evan S; Kim, Bohyun; Chiowanich, Peerapod; Blasbalg, Roberto; Kilger, Alex (1998). "Ovarian Brenner tumors: MR imaging characteristics". Magnetic Resonance Imaging. 16 (10): 1147–1153. doi:10.1016/S0730-725X(98)00136-2. ISSN 0730-725X.
- ↑ Kim SH, Kim WH, Park KJ, Lee JK, Kim JS (1996). "CT and MR findings of Krukenberg tumors: comparison with primary ovarian tumors". J Comput Assist Tomogr. 20 (3): 393–8. PMID 8626898.
- ↑ Al-Agha OM, Nicastri AD (November 2006). "An in-depth look at Krukenberg tumor: an overview". Arch. Pathol. Lab. Med. 130 (11): 1725–30. doi:10.1043/1543-2165(2006)130[1725:AILAKT]2.0.CO;2. PMID 17076540.
- ↑ Landers, D. V.; Sweet, R. L. (1983). "Tubo-ovarian Abscess: Contemporary Approach to Management". Clinical Infectious Diseases. 5 (5): 876–884. doi:10.1093/clinids/5.5.876. ISSN 1058-4838.
- ↑ Stewart Taylor, E.; McMillan, James H.; Greer, Benjamin E.; Droegemueller, William; Thompson, Horace E. (1975). "The intrauterine device and tubo-ovarian abscess". American Journal of Obstetrics and Gynecology. 123 (4): 338–348. doi:10.1016/S0002-9378(16)33434-2. ISSN 0002-9378.
- ↑ Ha, H. K.; Lim, G. Y.; Cha, E. S.; Lee, H. G.; Ro, H. J.; Kim, H. S.; Kim, H. H.; Joo, S. W.; Jee, M. K. (1995). "MR Imaging of Tubo-Ovarian Abscess". Acta Radiologica. 36 (5): 510–514. doi:10.1080/02841859509173418. ISSN 0284-1851.
- ↑ Varras M, Polyzos D, Perouli E, Noti P, Pantazis I, Akrivis C (2003). "Tubo-ovarian abscesses: spectrum of sonographic findings with surgical and pathological correlations". Clin Exp Obstet Gynecol. 30 (2–3): 117–21. PMID 12854857. Vancouver style error: initials (help)
- ↑ Barnhart, Kurt T. (2009). "Ectopic Pregnancy". New England Journal of Medicine. 361 (4): 379–387. doi:10.1056/NEJMcp0810384. ISSN 0028-4793.
- ↑ Kim, Mi Young; Rha, Sung Eun; Oh, Soon Nam; Jung, Seung Eun; Lee, Young Joon; Kim, You Sung; Byun, Jae Young; Lee, Ahwon; Kim, Mee-Ran (2009). "MR Imaging Findings of Hydrosalpinx: A Comprehensive Review". RadioGraphics. 29 (2): 495–507. doi:10.1148/rg.292085070. ISSN 0271-5333.
- ↑ Atri M, Nazarnia S, Bret PM, Aldis AE, Kintzen G, Reinhold C (July 1994). "Endovaginal sonographic appearance of benign ovarian masses". Radiographics. 14 (4): 747–60, discussion 761–2. doi:10.1148/radiographics.14.4.7938766. PMID 7938766.
- ↑ Chanelles, Olivier; Ducarme, Guillaume; Sifer, Christophe; Hugues, Jean-Noel; Touboul, Cyril; Poncelet, Christophe (2011). "Hydrosalpinx and infertility: what about conservative surgical management?". European Journal of Obstetrics & Gynecology and Reproductive Biology. 159 (1): 122–126. doi:10.1016/j.ejogrb.2011.07.004. ISSN 0301-2115.
- ↑ Czerwenka K, Heuss F, Hosmann J, Manavi M, Jelincic D, Kubista E (October 1994). "Salpingitis caused by Chlamydia trachomatis and its significance for infertility". Acta Obstet Gynecol Scand. 73 (9): 711–5. PMID 7976247.
- ↑ Niloff, Jonathan M.; Klug, Thomas L.; Schaetzl, Elena; Zurawski, Vincent R.; Knapp, Robert C.; Bast, Robert C. (1984). "Elevation of serum CA125 in carcinomas of the fallopian tube, endometrium, and endocervix". American Journal of Obstetrics and Gynecology. 148 (8): 1057–1058. doi:10.1016/S0002-9378(84)90444-7. ISSN 0002-9378.
- ↑ Bulletti, Carlo; De Ziegler, Dominique; Polli, Valeria; Flamigni, Carlo (1999). "The role of leiomyomas in infertility". The Journal of the American Association of Gynecologic Laparoscopists. 6 (4): 441–445. doi:10.1016/S1074-3804(99)80008-5. ISSN 1074-3804.
- ↑ Murase, Eiko; Siegelman, Evan S.; Outwater, Eric K.; Perez-Jaffe, Liza A.; Tureck, Richard W. (1999). "Uterine Leiomyomas: Histopathologic Features, MR Imaging Findings, Differential Diagnosis, and Treatment". RadioGraphics. 19 (5): 1179–1197. doi:10.1148/radiographics.19.5.g99se131179. ISSN 0271-5333.
- ↑ Seckl, Michael J; Fisher, Rosemary A; Salerno, Giovanni; Rees, Helene; Paradinas, Fernando J; Foskett, Marianne; Newlands, Edward S (2000). "Choriocarcinoma and partial hydatidiform moles". The Lancet. 356 (9223): 36–39. doi:10.1016/S0140-6736(00)02432-6. ISSN 0140-6736.
- ↑ Nishikawa, Yoshiki; Kaseki, Shigeaki; Tomoda, Yutaka; Ishizuka, Takao; Asai, Yasumasa; Suzuki, Toshio; Ushijima, Hiroshi (1985). "Histopathologic classification of uterine choriocarcinoma". Cancer. 55 (5): 1044–1051. doi:10.1002/1097-0142(19850301)55:5<1044::AID-CNCR2820550520>3.0.CO;2-7. ISSN 0008-543X.
- ↑ Libshitz HI, Baber CE, Hammond CB (April 1977). "The pulmonary metastases of choriocarcinoma". Obstet Gynecol. 49 (4): 412–6. PMID 558566.
- ↑ Diouf A, Cissé ML, Laïco A, Ndiaye D, Moreau JC, Diadhiou F (May 2005). "[Sonographic features of gestational choriocarcinoma]". J Radiol (in French). 86 (5 Pt 1): 469–73. PMID 16114202.
- ↑ Seki, K.; Hoshihara, T.; Nagata, I. (1992). "Leiomyosarcoma of the Uterus: Ultrasonography and Serum Lactate Dehydrogenase Level". Gynecologic and Obstetric Investigation. 33 (2): 114–118. doi:10.1159/000294861. ISSN 1423-002X.
- ↑ Juang CM, Yen MS, Horng HC, Twu NF, Yu HC, Hsu WL (2006). "Potential role of preoperative serum CA125 for the differential diagnosis between uterine leiomyoma and uterine leiomyosarcoma". Eur. J. Gynaecol. Oncol. 27 (4): 370–4. PMID 17009628.
- ↑ Pattani, Sita J.; Kier, Ruben; Deal, Robert; Luchansky, Edward (1995). "MRI of uterine leiomyosarcoma". Magnetic Resonance Imaging. 13 (2): 331–333. doi:10.1016/0730-725X(95)93813-5. ISSN 0730-725X.
- ↑ McLeod, A J; Zornoza, J; Shirkhoda, A (1984). "Leiomyosarcoma: computed tomographic findings". Radiology. 152 (1): 133–136. doi:10.1148/radiology.152.1.6729102. ISSN 0033-8419.
- ↑ Robboy, Stanley J.; Bentley, Rex C.; Butnor, Kelly; Anderson, Malcolm C. (2000). "Pathology and Pathophysiology of Uterine Smooth-Muscle Tumors". Environmental Health Perspectives. 108: 779. doi:10.2307/3454306. ISSN 0091-6765.
- ↑ Cacctatore, Bruno; Tttttnen, Atla; Stenman, Ulf-Hakan; Ylostalo, Pekka (1990). "Normal early pregnancy: serum hCG levels and vaginal ultrasonography findings". BJOG: An International Journal of Obstetrics and Gynaecology. 97 (10): 899–903. doi:10.1111/j.1471-0528.1990.tb02444.x. ISSN 1470-0328.
- ↑ Pinto Leite N, Pereira JM, Cunha R, Pinto P, Sirlin C (August 2005). "CT evaluation of appendicitis and its complications: imaging techniques and key diagnostic findings". AJR Am J Roentgenol. 185 (2): 406–17. doi:10.2214/ajr.185.2.01850406. PMID 16037513.
- ↑ Chapter 5: Tumours of the Appendix - IARC. https://www.iarc.fr/en/publications/pdfs-online/pat-gen/bb2/bb2-chap5.pdf Accessed on January 15, 2019
- ↑ Goede, A. C.; Caplin, M. E.; Winslet, M. C. (2003). "Carcinoid tumour of the appendix". British Journal of Surgery. 90 (11): 1317–1322. doi:10.1002/bjs.4375. ISSN 0007-1323.
- ↑ Pablo Carmignani, C.; Hampton, Regina; E. Sugarbaker, Christina; Chang, David; H. Sugarbaker, Paul (2004). "Utility of CEA and CA 19-9 tumor markers in diagnosis and prognostic assessment of mucinous epithelial cancers of the appendix". Journal of Surgical Oncology. 87 (4): 162–166. doi:10.1002/jso.20107. ISSN 0022-4790.
- ↑ Limsui D, Vierkant RA, Tillmans LS, Wang AH, Weisenberger DJ, Laird PW, Lynch CF, Anderson KE, French AJ, Haile RW, Harnack LJ, Potter JD, Slager SL, Smyrk TC, Thibodeau SN, Cerhan JR, Limburg PJ (July 2010). "Cigarette smoking and colorectal cancer risk by molecularly defined subtypes". J. Natl. Cancer Inst. 102 (14): 1012–22. doi:10.1093/jnci/djq201. PMC 2915616. PMID 20587792.
- ↑ Duh QY, Hybarger CP, Geist R, Gamsu G, Goodman PC, Gooding GA, Clark OH (July 1987). "Carcinoids associated with multiple endocrine neoplasia syndromes". Am. J. Surg. 154 (1): 142–8. PMID 2886072.
- ↑ Ferlay, Jacques; Soerjomataram, Isabelle; Dikshit, Rajesh; Eser, Sultan; Mathers, Colin; Rebelo, Marise; Parkin, Donald Maxwell; Forman, David; Bray, Freddie (2015). "Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012". International Journal of Cancer. 136 (5): E359–E386. doi:10.1002/ijc.29210. ISSN 0020-7136.
- ↑ Ferlay, Jacques; Shin, Hai-Rim; Bray, Freddie; Forman, David; Mathers, Colin; Parkin, Donald Maxwell (2010). "Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008". International Journal of Cancer. 127 (12): 2893–2917. doi:10.1002/ijc.25516. ISSN 0020-7136.
- ↑ Parkin DM, Bray F, Ferlay J, Pisani P (2005). "Global cancer statistics, 2002". CA Cancer J Clin. 55 (2): 74–108. PMID 15761078.
- ↑ Cresanta JL (1992). "Epidemiology of cancer in the United States". Prim Care. 19 (3): 419–41. PMID 1410056.
- ↑ Bray, Freddie; Ferlay, Jacques; Soerjomataram, Isabelle; Siegel, Rebecca L.; Torre, Lindsey A.; Jemal, Ahmedin (2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". CA: A Cancer Journal for Clinicians. 68 (6): 394–424. doi:10.3322/caac.21492. ISSN 0007-9235.
- ↑ Barnholtz-Sloan JS, Morris R, Malone JM, Munkarah AR (2004) Survival of women diagnosed with malignant, mixed mullerian tumors of the ovary (OMMMT). Gynecol Oncol 93 (2):506-12. DOI:10.1016/j.ygyno.2004.02.016 PMID: 15099970
- ↑ Sood AK, Sorosky JI, Gelder MS, Buller RE, Anderson B, Wilkinson EJ et al. (1998) Primary ovarian sarcoma: analysis of prognostic variables and the role of surgical cytoreduction. Cancer 82 (9):1731-7. PMID: 9576296
- ↑ Cicin İ, Özatlı T, Türkmen E, Özturk T, Özçelik M, Çabuk D et al. (2016) Predictive and Prognostic Factors in Ovarian and Uterine Carcinosarcomas. Balkan Med J 33 (5):517-524. DOI:10.5152/balkanmedj.2016.151268 PMID: 27761279
- ↑ Dai Y, Shen K, Lang JH, Huang HF, Pan LY, Wu M; et al. (2011). "Primary sarcoma of the ovary: clinicopathological characteristics, prognostic factors and evaluation of therapy". Chin Med J (Engl). 124 (9): 1316–21. PMID 21740740.
- ↑ 81.0 81.1 del Carmen MG, Birrer M, Schorge JO (2012). "Carcinosarcoma of the ovary: a review of the literature". Gynecol Oncol. 125 (1): 271–7. doi:10.1016/j.ygyno.2011.12.418. PMID 22155675.
- ↑ 82.0 82.1 Kim HJ, Lee HM, Kim MK, Lee YK, Lee IH, Lee KH; et al. (2017). "Prognostic assessment of sarcomatous histologic subtypes of ovarian carcinosarcoma". Obstet Gynecol Sci. 60 (4): 350–356. doi:10.5468/ogs.2017.60.4.350. PMC 5547082. PMID 28791266.
- ↑ Shakuntala P, Umadevi K, Usha A, Abhilasha N, Bafna U (2012). "Primary ovarian adenosarcoma with elevated Ca-125 levels and normal ascitic fluid cytology: a case report and review of literature". Ecancermedicalscience. 6: 284. doi:10.3332/ecancer.2012.284. PMC 3530409. PMID 23304240.
- ↑ Mogensen O, Mogensen B, Jakobsen A (1990). "Tumour-associated trypsin inhibitor (TATI) and cancer antigen 125 (CA 125) in mucinous ovarian tumours". Br J Cancer. 61 (2): 327–9. doi:10.1038/bjc.1990.64. PMC 1971406. PMID 2310684.
- ↑ Van Gorp T, Cadron I, Despierre E, Daemen A, Leunen K, Amant F; et al. (2011). "HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the Risk of Ovarian Malignancy Algorithm". Br J Cancer. 104 (5): 863–70. doi:10.1038/sj.bjc.6606092. PMC 3048204. PMID 21304524.
- ↑ 86.0 86.1 Miccò M, Sala E, Lakhman Y, Hricak H, Vargas HA (2015). "Imaging Features of Uncommon Gynecologic Cancers". AJR Am J Roentgenol. 205 (6): 1346–59. doi:10.2214/AJR.14.12695. PMC 5502476. PMID 26587944.
- ↑ 87.0 87.1 Bell DJ, Pannu HK (2011). "Radiological assessment of gynecologic malignancies". Obstet Gynecol Clin North Am. 38 (1): 45–68, vii. doi:10.1016/j.ogc.2011.02.003. PMID 21419327.
- ↑ 88.0 88.1 Forstner R, Graf A (1999). "[Diagnostic imaging in staging of gynecologic carcinomas]". Radiologe. 39 (7): 610–8. PMID 10472090.
- ↑ Manoharan D, Das CJ, Aggarwal A, Gupta AK (2016). "Diffusion weighted imaging in gynecological malignancies - present and future". World J Radiol. 8 (3): 288–97. doi:10.4329/wjr.v8.i3.288. PMC 4807338. PMID 27027614.
- ↑ Alt CD, Brocker KA, Eichbaum M, Sohn C, Arnegger FU, Kauczor HU; et al. (2011). "Imaging of female pelvic malignancies regarding MRI, CT, and PET/CT: Part 2". Strahlenther Onkol. 187 (11): 705–14. doi:10.1007/s00066-011-4002-z. PMID 22037656.
- ↑ Brown E, Stewart M, Rye T, Al-Nafussi A, Williams AR, Bradburn M; et al. (2004). "Carcinosarcoma of the ovary: 19 years of prospective data from a single center". Cancer. 100 (10): 2148–53. doi:10.1002/cncr.20256. PMID 15139057.
- ↑ Harris MA, Delap LM, Sengupta PS, Wilkinson PM, Welch RS, Swindell R; et al. (2003). "Carcinosarcoma of the ovary". Br J Cancer. 88 (5): 654–7. doi:10.1038/sj.bjc.6600770. PMC 2376340. PMID 12618869.
- ↑ Cicin I, Saip P, Eralp Y, Selam M, Topuz S, Ozluk Y; et al. (2008). "Ovarian carcinosarcomas: clinicopathological prognostic factors and evaluation of chemotherapy regimens containing platinum". Gynecol Oncol. 108 (1): 136–40. doi:10.1016/j.ygyno.2007.09.003. PMID 17936342.