|
|
| (17 intermediate revisions by 11 users not shown) |
| Line 1: |
Line 1: |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | | __NOTOC__ |
| {{DiseaseDisorder infobox |
| | '''For patient information, click [[{{PAGENAME}} (patient information)|here]]''' |
| Name = Herpes zoster |
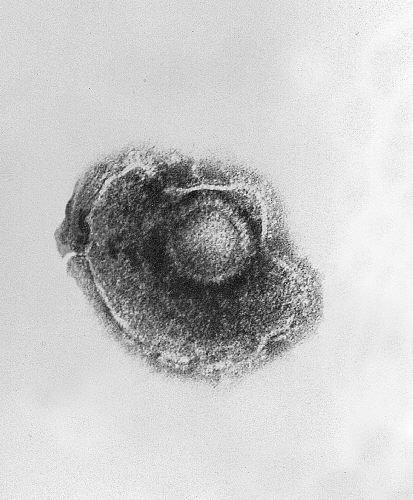
| | [[Image:Chickenpox-virus.jpg|thumb|right|[[Electron microscope|Electron micrograph]] of [[Varicella zoster virus]]. Approx. 150.000-fold magnification.]] |
| ICD10 = {{ICD10|B|02||b|00}} |
| | {{Herpes zoster}} |
| ICD9 = {{ICD9|053}} |
| | {{CMG}}; L. Katie Morrison, MD; |
| ICDO = |
| | {{AE}} {{CZ}}, {{JH}}{{AAA}}. |
| Image = Herpes zoster neck.jpg |
| |
| Caption = Herpes zoster blisters on the neck and shoulder |
| |
| OMIM = |
| |
| MedlinePlus = 000858 |
| |
| eMedicineSubj = |
| |
| eMedicineTopic = |
| |
| eMedicine_mult = { |
| |
| DiseasesDB = 29119 |
| |
| }}
| |
| {{SI}}
| |
| '''Editor-in-Chief:''' {{CMG}}; L. Katie Morrison, MD; '''Associate Editor(s)-In-Chief:''' {{CZ}}
| |
| | |
| ==Overview==
| |
| '''Herpes zoster''' (or simply '''zoster'''), commonly known as '''shingles''', is a [[viral disease]] characterized by a painful skin rash with [[blister]]s in a limited area on one side of the body, often in a stripe. The initial infection with [[varicella zoster virus]] (VZV) causes the acute (short-lived) illness [[chickenpox]], and generally occurs in children and young people. Once an episode of chickenpox has resolved, the virus is not eliminated from the body but can go on to cause shingles—an illness with very different symptoms—often many years after the initial infection.
| |
|
| |
| Varicella zoster virus can become latent in the [[neuron|nerve cell bodies]] and less frequently in [[Satellite cells|non-neuronal satellite cells]] of [[Dorsal root ganglion|dorsal root]], [[Cranial nerves|cranial nerve]] or [[autonomic]] [[ganglion]],<ref name="pmid12676845">{{cite journal| journal=BMJ| year=2003| volume=326| issue=7392| pages=748| doi=10.1136/bmj.326.7392.748| author=Johnson, RW & Dworkin, RH| title=Clinical review: Treatment of herpes zoster and postherpetic neuralgia | pmid=12676845 | url=http://www.bmj.com/cgi/content/full/326/7392/748}}</ref> without causing any [[symptoms]].<ref name="pmid12211045">{{cite journal |author=Kennedy PG |title=Varicella-zoster virus latency in human ganglia |journal=Rev. Med. Virol. |volume=12 |issue=5 |pages=327–34 |year=2002 |pmid=12211045 |doi=10.1002/rmv.362}}</ref><ref name="pmid12491156">{{cite journal| author=Kennedy PG| title=Key issues in varicella-zoster virus latency| journal=J. Neurovirol| volume=8 Suppl 2| pages=80–4| year=2002| pmid=12491156| doi=10.1080/13550280290101058}}</ref> In an [[Immunodeficiency|immunocompromised]] individual, perhaps years or decades after a chickenpox infection, the virus may break out of nerve cell bodies and travel down nerve [[axon]]s to cause viral infection of the skin in the region of the nerve. The virus may spread from one or more ganglia along nerves of an affected [[Segmentation (biology)|segment]] and infect the corresponding [[Dermatomic area|dermatome]] (an area of skin supplied by one spinal nerve) causing a painful rash.<ref name="pmid1666443">{{cite journal |author=Peterslund NA |title=Herpesvirus infection: an overview of the clinical manifestations |journal=Scand J Infect Dis Suppl |volume=80 |issue= |pages=15–20 |year=1991 |pmid=1666443 |doi= |issn= }}</ref><ref name="pmid14583142"/> Although the rash usually heals within two to four weeks, some sufferers experience residual nerve pain for months or years, a condition called [[postherpetic neuralgia]]. Exactly how the virus remains latent in the body, and subsequently re-activates is not understood.<ref name="pmid12676845">{{cite journal| journal=BMJ| year=2003| volume=326| issue=7392| pages=748| doi=10.1136/bmj.326.7392.748| author=Johnson, RW & Dworkin, RH| title=Clinical review: Treatment of herpes zoster and postherpetic neuralgia | pmid=12676845 | url=http://www.bmj.com/cgi/content/full/326/7392/748}}</ref>
| |
| | |
| Throughout the world the [[Incidence (epidemiology)|incidence rate]] of herpes zoster every year ranges from 1.2 to 3.4 cases per 1,000 healthy individuals, increasing to 3.9–11.8 per year per 1,000 individuals among those older than 65 years.<ref name="pmid17143845">{{cite journal
| |
| | author=Dworkin RH, Johnson RW, Breuer J ''et al.''| title=Recommendations for the management of herpes zoster| journal=Clin. Infect. Dis| volume=44 Suppl 1| pages=S1–26| year=2007| pmid=17143845| doi=10.1086/510206| url=http://www.journals.uchicago.edu/doi/full/10.1086/510206}}</ref><ref name="pmid7618983"/><ref name="pmid17939895"/> [[Antiviral drug]] treatment can reduce the severity and duration of herpes zoster, if a seven to ten day course of these drugs is started within 72 hours of the appearance of the characteristic rash.<ref name="pmid17143845">{{cite journal
| |
| | author=Dworkin RH, Johnson RW, Breuer J ''et al.''| title=Recommendations for the management of herpes zoster| journal=Clin. Infect. Dis| volume=44 Suppl 1| pages=S1–26| year=2007| pmid=17143845| doi=10.1086/510206| url=http://www.journals.uchicago.edu/doi/full/10.1086/510206}}</ref><ref name="pmid18241179">{{cite journal |author=Cunningham AL, Breuer J, Dwyer DE, Gronow DW, Helme RD, Litt JC, Levin MJ, Macintyre CR |title=The prevention and management of herpes zoster |journal=Med. J. Aust. |volume=188 |issue=3 |pages=171–6 |year=2008 |pmid=18241179 |doi=}}</ref> <ref>{{cite journal|author=Weaver BA|title=The burden of herpes zoster and postherpetic neuralgia in the United States|journal=J Am Osteopath Assoc.|date=2007|volume=107|issue=3 Suppl 1|pages=S2-7|pmid= 17488884}}</ref>
| |
| <ref>{{cite web|url=http://www3.niaid.nih.gov/healthscience/healthtopics/shingles/ |title=National Institute of Allergy and Infectious Diseases Shingles Index|accessdate=2007-05-17|format=HTML}}</ref> <ref name="Zamula">{{cite web|url=http://www.fda.gov/FDAC/features/2001/301_pox.html|title=Shingles:An Unwelcome Encore|last=Zamula|first=Evelyn|date=2005|publisher=United States Food and Drug Administration|accessdate=2007-04-10}}</ref> <ref name="Stankus">{{cite journal|last=Stankus|first=SJ|coauthors=Dlugopolski, M & Packer, D|date=2000|journal=American Family Physician|volume=61|issue=8|pages=2437-2447|title=Management of Herpes Zoster (Shingles) and Postherpetic Neuralgia|id=PMID 10794584 |url=http://www.aafp.org/afp/20000415/2437.html|accessdate=2007-04-08}}</ref><ref>{{cite web|url=http://www.cdc.gov/nip/diseases/shingles/faqs-disease-shingles.htm|title=Shingles (Herpes Zoster)|date=2006|publisher=[[Centers for Disease Control]]|accessdate=2007-05-30}}</ref>
| |
| | |
| ==Nomenclature==
| |
| | |
| Multiple names are used to refer to same virus, creating some confusion. Varicella virus, zoster virus, human herpes 3 (HHV-3), and Varicella Zoster Virus (VZV) all refer to the same viral pathogen. The disease caused by this pathogen is called chickenpox or Varicella disease during the initial infection. A reactivation of the infection is commonly called [[shingles]], herpes zoster or simply zoster.
| |
| | |
| ==Morphology==
| |
| | |
| VZV is closely related to the [[herpes simplex virus]]es (HSV), sharing much [[genome]] homology. The known envelope glycoproteins (gB, gC, gE, gH, gI, gK, gL) correspond with those in HSV, however there is no equivalent of HSV gD. VZV virons are spherical and 150-200 nm in diameter. Their [[lipid]] envelope encloses the nucleocapsid of 162 capsomeres arranged in a hexagonal form. Its [[DNA]] is a single, linear, double-stranded molecule, 125,000 nt long.
| |
| | |
| The virus is very susceptible to [[disinfectant]]s, notably [[sodium hypochlorite]]. Within the body it can be treated by a number of drugs and therapeutic agents including [[aciclovir]], [[zoster-immune globulin]] (ZIG), and [[vidarabine]].
| |
| | |
| ==Human disease==
| |
| Primary VZV infection results in [[chickenpox]] (varicella), which may rarely result in complications including VZV [[encephalitis]] or [[pneumonia]]. Even when clinical symptoms of varicella have resolved, VZV remains dormant in the [[nervous system]] of the host in the [[trigeminal nerve|trigeminal]] and [[dorsal root ganglion|dorsal root ganglia]]. In about 10-20% of cases, VZV reactivates later in life producing a disease known as [[herpes zoster]] or shingles. Serious complications of shingles include post-herpetic neuralgia, zoster multiplex, myelitis, herpes ophthalmicus, or zoster sine herpete.
| |
| | |
| ==History==
| |
|
| |
|
| Herpes zoster has a long recorded history, although historical accounts fail to distinguish the blistering caused by VZV and those caused by smallpox,<ref>Weinberg JM (2007). "Herpes zoster: epidemiology, natural history, and common complications". J Am Acad Dermatol 57 (6 Suppl): S130–5. doi:10.1016/j.jaad.2007.08.046. PMID 18021864</ref> [[ergotism]], and [[erysipelas]]. It was only in the late eighteenth century that [[William Heberden]] established a way to differentiate between herpes zoster and smallpox,<ref name="Weller">{{cite book|author=Weller TH|date=2000|title=Chapter 1. Historical perspective in: Varicella-Zoster Virus: Virology and Clinical Management (Arvin AM & Gershon AA, editors)|publisher=Cambridge University Press|isbn=0521660246}}</ref> and only in the late nineteenth century that herpes zoster was differentiated from [[erysipelas]]. The first indications that chickenpox and herpes zoster were caused by the same virus were noticed at the beginning of the 20th century. Physicians began to report that cases of herpes zoster were often followed by chickenpox in the younger people who lived with the shingles patients. The idea of an association between the two diseases gained strength when it was shown that lymph from a sufferer of herpes zoster could induce chickenpox in young volunteers. This was finally proved by the first isolation of the virus in cell cultures, by the Nobel laureate Thomas H. Weller in 1953.<ref name="pmid13064265">{{cite journal |author=Weller TH |title=Serial propagation in vitro of agents producing inclusion bodies derived from varicella and herpes zoster |journal=Proc. Soc. Exp. Biol. Med. |volume=83 |issue=2 |pages=340–6 |year=1953 |pmid=13064265}}</ref>
| | ==[[Herpes zoster overview|Overview]]== |
|
| |
|
| Until the 1940s, the disease was considered benign, and that serious complications were thought to be very rare.<ref name="Holt1936">{{cite book|author=Holt LE & McIntosh R|title=Holt's Diseases of Infancy and Childhood|date=1936|publisher=D Appleton Century Company|pages=931–3}}</ref> However, by 1942, it was recognized that herpes zoster was a more serious disease in adults than in children and that it increased in frequency with advancing age. Further studies during the 1950s on immunosuppressed individuals showed that the disease was not as benign as once thought, and the search for various therapeutic and preventive measures began.<ref name="Weller"/> By the mid-1960s, several studies identified the gradual reduction in cellular immunity in old age, observing that in a cohort of 1,000 people who lived to the age of 85, approximately 500 would have one attack of herpes zoster and 10 would have two attacks.<ref name="pmid14267505">{{cite journal|author=Hope-Simpson RE|date=1965|title=The nature of herpes zoster; a long-term study and a new hypothesis|journal=Proc R Soc Med| volume=58| pages=9–20| pmid=14267505| url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1898279}}</ref>
| | ==[[Herpes zoster historical perspective|Historical Perspective]]== |
|
| |
|
| ==Epidemiology== | | ==[[Herpes zoster pathophysiology|Pathophysiology]]== |
|
| |
|
| Before introduction of varicella vaccine in the United States in 1995, varicella was endemic, with virtually all persons being infected by adulthood. Since implementation of the varicella vaccination program, incidence has declined in all age groups, with the greatest decline among children aged 1-4 years. Data from passive and active surveillance have indicated a decline in varicella cases of 70%-84% from 1995 through 2001 (1-3). The downward trend in varicella has continued in the United States through 2005 with an approximately 90% decline in incidence from 1995 in active surveillance sites with high vaccine coverage (CDC, unpublished data).
| | ==[[Herpes zoster causes|Causes]]== |
|
| |
|
| Varicella zoster virus has a high level of [[infectivity]] and is prevalent worldwide,<ref>{{cite journal |author=Apisarnthanarak A, Kitphati R, Tawatsupha P, Thongphubeth K, Apisarnthanarak P, Mundy LM |title=Outbreak of varicella-zoster virus infection among Thai healthcare workers |journal=Infect Control Hosp Epidemiol |volume=28 |issue=4 |pages=430-4 |year=2007 |pmid=17385149 |doi=10.1086/512639}}</ref> and has a very stable prevalence from generation to generation.<ref name="pmid11289797">{{cite journal |author=Abendroth A, Arvin AM |title=Immune evasion as a pathogenic mechanism of varicella zoster virus |journal=Semin. Immunol. |volume=13 |issue=1 |pages=27–39 |year=2001 |pmid=11289797 |doi=10.1006/smim.2001.0293}}</ref> VZV is a benign disease in a healthy child in developed countries. However, varicella can be lethal to individuals who are infected later in life or who have low immunity. The number of people in this high-risk group has increased, due to the HIV epidemic and the increase in immunosuppressive therapies. Infections of varicella in institutions such as hospitals are also a significant problem, especially in hospitals that care for these high-risk populations.<ref name="Weller">{{cite book|author=Weller TH|title=Varicella-herpes zoster virus. In: Viral Infections of Humans: Epidemiology and Control. Evans AS, Kaslow RA, eds.|publisher=Plenum Press|date=1997|pages=865-892|isbn=978-0306448553}}</ref>
| | ==[[Herpes zoster differential diagnosis|Differentiating Herpes zoster from other Diseases]]== |
|
| |
|
| In general, herpes zoster has no seasonal incidence and does not occur in epidemics.<ref>Thomas SL, Hall AJ (2004). "What does epidemiology tell us about risk factors for herpes zoster?". Lancet Infect Dis 4 (1): 26–33. doi:10.1016/S1473-3099(03)00857-0. PMID 14720565</ref> In temperate zones chickenpox is a disease of children, with most cases occurring during the winter and spring, most likely due to school contact; there is no evidence for regular epidemics. In the tropics chickenpox typically occurs among older people. <ref>Wharton M (1996). "The epidemiology of varicella-zoster virus infections". Infect Dis Clin North Am 10 (3): 571–81. PMID 8856352</ref> Incidence is highest in people who are over age 55, as well as in [[Immunosuppression|immunocompromised]] patients regardless of age group, and in individuals undergoing [[Stress (medicine)|psychological stress]]. Non-whites may be at lower risk; it is unclear whether the risk is increased in females. Other potential risk factors include [[Physical trauma|mechanical trauma]], genetic susceptibility, and exposure to [[immunotoxin]]s. <ref>Thomas SL, Hall AJ (2004). "What does epidemiology tell us about risk factors for herpes zoster?". Lancet Infect Dis 4 (1): 26–33. doi:10.1016/S1473-3099(03)00857-0. PMID 14720565</ref>
| | ==[[Herpes zoster epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| The incidence rate of herpes zoster ranges from 1.2 to 3.4 per 1,000 person-years among healthy individuals, increasing to 3.9–11.8 per 1,000 person‐years among those older than 65 years. <ref>Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845</ref> Similar incidence rates have been observed worldwide.<ref name="pmid17939895">{{cite journal| author=Araújo LQ, Macintyre CR, Vujacich C| title=Epidemiology and burden of herpes zoster and post-herpetic neuralgia in Australia, Asia and South America| journal=Herpes| volume=14| issue=Suppl 2| pages=40A–4A| year=2007| pmid=17939895| url=http://www.ihmf.org/journal/download/5%20-%20Herpes%2014.2%20suppl%20Araujo.pdf| format=PDF}}</ref> <ref>Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845</ref> Herpes zoster develops in an estimated 500,000 Americans each year.<ref name="pmid16050886">{{cite journal |author=Insinga RP |title=The incidence of herpes zoster in a United States administrative database |journal=J Gen Intern Med |volume=20 |issue=6 |pages=748–753 |year=2005 |pmid=16050886 |doi=10.1111/j.1525-1497.2005.0150.x |url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16050886 }}</ref> Multiple studies and surveillance data demonstrate no consistent trends in incidence in the U.S. since the chickenpox vaccination program began in 1995.<ref>{{cite journal |journal= MMWR Recomm Rep |date=2007 |volume=56 |issue=RR-4 |pages=1–40 |title= Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP) |author= Marin M, Güris D, Chaves SS, Schmid S, Seward JF |pmid=17585291 |url=http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5604a1.htm}}</ref> It is likely that incidence rate will change in the future, due to the aging of the population, changes in therapy for malignant and autoimmune diseases, and changes in chickenpox vaccination rates; a wide adoption of zoster vaccination could dramatically reduce the incidence rate.<ref>Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845</ref>
| | ==[[Herpes zoster risk factors|Risk Factors]]== |
|
| |
|
| In one study, it was estimated that 26% of patients who contract herpes zoster eventually present with complications. Postherpetic neuralgia arises in approximately 20% of patients.<ref name="pmid17939894">{{cite journal |author= Volpi A |title= Severe complications of herpes zoster |journal=Herpes |volume=14 |issue= Suppl 2 |pages=35A–9A |year=2007 |pmid=17939894 |url=http://www.ihmf.org/journal/download/4%20-%20Herpes%2014.2%20suppl%20Volpi.pdf |format=PDF}}</ref> A study of 1994 California data found hospitalization rates of 2.1 per 100,000 person-years, rising to 9.3 per 100,000 person-years for ages 60 and up.<ref>{{cite journal |journal=Pediatr Infect Dis J |date=2001 |volume=20 |issue=7 |pages=641-5 |title= Incidence and hospitalization rates of varicella and herpes zoster before varicella vaccine introduction: a baseline assessment of the shifting epidemiology of varicella disease |author= Coplan P, Black S, Rojas C |pmid=11465834}}</ref> An earlier Connecticut study found a higher hospitalization rate; the difference may be due to the prevalence of [[HIV]] in the earlier study, or to the introduction of antivirals in California before 1994.<ref>{{cite journal |journal= J Am Osteopath Assoc |date=2007 |volume=107 |issue=3 Suppl |pages=S2–7 |title= The burden of herpes zoster and postherpetic neuralgia in the United States |author= Weaver BA |pmid=17488884 |url=http://www.jaoa.org/cgi/content/full/107/suppl_1/S2}}</ref>
| | ==[[Herpes zoster screening|Screening]]== |
|
| |
|
| ==Pathophysiology== | | ==[[Herpes zoster natural history|Natural History, Complications and Prognosis]]== |
| [[Image:A Course of Shingles diagram.png|left|Progression of herpes zoster. A cluster of small bumps (1) turns into blisters (2). The blisters fill with [[lymph]], break open (3), crust over (4), and finally disappear. [[Postherpetic neuralgia]] can sometimes occur due to nerve damage (5),|thumb|250px]]
| |
| | |
| The causative agent for herpes zoster is [[varicella zoster virus]] (VZV), a double-stranded [[DNA virus]] related to the [[Herpes simplex virus]] group. Most people are infected with this virus as children, and suffer from an episode of chickenpox. The immune system eventually eliminates the virus from most locations, but it remains dormant (or [[viral latency|latent]]) in the [[ganglion|ganglia]] adjacent to the spinal cord (called the dorsal root ganglion) or the ganglion semilunare (ganglion Gasseri) in the base of the skull.<ref name="pmid17945155">{{cite journal|author=Steiner I, Kennedy PG, Pachner AR|title=The neurotropic herpes viruses: herpes simplex and varicella-zoster|journal=Lancet Neurol|volume=6|issue=11|pages=1015–28|year=2007|pmid=17945155|doi=10.1016/S1474-4422(07)70267-3}}</ref> However, repeated attacks of herpes zoster are rare,<ref name="Stankus">{{cite journal|last=Stankus|first=SJ|coauthors=Dlugopolski, M & Packer, D|date=2000|journal=American Family Physician|volume=61|issue=8|pages=2437-2447|title=Management of Herpes Zoster (Shingles) and Postherpetic Neuralgia|id=PMID 10794584 |url=http://www.aafp.org/afp/20000415/2437.html|accessdate=2007-04-08}}</ref> and it is extremely rare for patients to suffer more than three recurrences.<ref name="pmid17945155">{{cite journal|author=Steiner I, Kennedy PG, Pachner AR|title=The neurotropic herpes viruses: herpes simplex and varicella-zoster|journal=Lancet Neurol|volume=6|issue=11|pages=1015–28|year=2007|pmid=17945155|doi=10.1016/S1474-4422(07)70267-3}}</ref>
| |
| | |
| Herpes zoster occurs only in people who have had chickenpox, and although it can occur at any age, the majority of sufferers are more than 50 years old.<ref name="pmid18021864">{{cite journal| author=Weinberg JM| title=Herpes zoster: epidemiology, natural history, and common complications| journal=J Am Acad Dermatol| volume=57| issue=6 Suppl| pages=S130–5| year=2007| pmid=18021864| doi=10.1016/j.jaad.2007.08.046}}</ref> The disease results from the virus reactivating in a single sensory ganglion.<ref name="pmid14583142">{{cite journal| author=Gilden DH, Cohrs RJ, Mahalingam R| title=Clinical and molecular pathogenesis of varicella virus infection| journal=Viral Immunol| volume=16| issue=3| pages=243–58| year=2003| pmid=14583142| doi=10.1089/088282403322396073}}</ref> In contrast to [[Herpes simplex virus]], the latency of VZV is poorly understood. The virus has not been recovered from human nerve cells by [[cell culture]] and the location and structure of the viral [[DNA]] is not known. Virus-specific proteins continue to be made by the infected cells during the latent period, so true latency, as opposed to a [[chronic (medical)|chronic]] low-level [[infectious disease|infection]], has not been proven.<ref name="pmid12211045">{{cite journal |author=Kennedy PG |title=Varicella-zoster virus latency in human ganglia |journal=Rev. Med. Virol. |volume=12 |issue=5 |pages=327–34 |year=2002 |pmid=12211045 |doi=10.1002/rmv.362}}</ref><ref name="pmid12491156">{{cite journal| author=Kennedy PG| title=Key issues in varicella-zoster virus latency| journal=J. Neurovirol| volume=8 Suppl 2| pages=80–4| year=2002| pmid=12491156| doi=10.1080/13550280290101058}}</ref> Although VZV has been detected in autopsies of nervous tissue, there are no methods to find dormant virus in the ganglia in living people.
| |
| | |
| Unless the [[immune system]] is compromised, it suppresses reactivation of the virus and prevents herpes zoster. Why this suppression sometimes fails is poorly understood,<ref name="pmid7618983">{{cite journal| author=Donahue JG, Choo PW, Manson JE, Platt R| title=The incidence of herpes zoster| journal=Arch. Intern. Med| volume=155| issue=15| pages=1605–9| year=1995| pmid=7618983| doi=10.1001/archinte.155.15.1605}}</ref> but herpes zoster is more likely to occur in people whose immune system is impaired due to aging, [[immunosuppressive therapy]], psychological stress, or other factors.<ref name="pmid14720565">{{cite journal| author=Thomas SL, Hall AJ| title=What does epidemiology tell us about risk factors for herpes zoster?| journal=Lancet Infect Dis| volume=4| issue=1| pages=26–33| year=2004| doi=10.1016/S1473-3099(03)00857-0| pmid=14720565}}</ref> Upon reactivation, the virus replicates in the nerve cells, and [[virion]]s are shed from the cells and carried down the [[axon]]s to the area of skin served by that ganglion. In the skin, the virus causes local [[inflammation]] and blisters. The short and long-term pain caused by herpes zoster comes from the widespread growth of the virus in the infected nerves, which causes inflammation.<ref name="pmid17631237">{{cite journal |author=Schmader K |title=Herpes zoster and postherpetic neuralgia in older adults |journal=Clin. Geriatr. Med. |volume=23 |issue=3 |pages=615–32, vii–viii |year=2007 |pmid=17631237 |doi=10.1016/j.cger.2007.03.003 |url=http://linkinghub.elsevier.com/retrieve/pii/S0749-0690(07)00021-3}}</ref>
| |
| | |
| The symptoms of herpes zoster cannot be transmitted to another person.<ref name="pmid10825029">{{cite journal| author=Schmader K| title=Herpes zoster in the elderly: issues related to geriatrics| journal=Clin. Infect. Dis| volume=28| issue=4| pages=736–9| year=1999| pmid=10825029| doi=10.1086/515205}}</ref> However, during the blister phase, direct contact with the rash can spread VZV to a person who has no immunity to the virus. This newly-infected individual may then develop chickenpox, but will not immediately develop shingles. Until the rash has developed crusts, a person is extremely contagious. A person is also not infectious before blisters appear, or during postherpetic neuralgia (pain after the rash is gone). The person is no longer contagious after the virus has disappeared.<ref>PMID 10794584</ref>
| |
| | |
| ==Causes==
| |
| | |
| Shingles can only arise in individuals who have been previously exposed to chicken pox (varicella zoster). The disease arises from various events which depress the immune system, such as aging, severe emotional stress, severe illness, immunosuppression or long-term use of [[corticosteroid]]s.<ref name="Mounsey">{{cite journal|title=Herpes zoster and postherpetic neuralgia: prevention and management|author=Mounsey AL, Matthew LG, & Slawson DC|date=2005|journal=American Family Physician|volume=72|issue=6|pages=1075-1080|pmid=16190505|url=http://www.aafp.org/afp/20050915/1075.html|accessdate=2007-06-15}}</ref><ref>{[cite journal|title=What does epidemiology tell us about risk factors for herpes zoster?|author=Thomas SL, Hall AJ|journal= Lancet Infect Dis.|date=2004|volume=4|issue=1|pages=26-33|pmid= 14720565}}</ref> The cellular and immunological events that lead to reactivation are poorly understood.<ref>Donahue JG, Choo PW, Manson JE, Platt R (1995). "The incidence of herpes zoster". Arch. Intern. Med 155 (15): 1605–9. PMID 7618983</ref> There have been recorded cases of outbreaks occurring due to unmanaged stress or other stresses to the skin such as pinching, biting or scratching of more sensitive areas, such as nipples, ears, and underarms.<ref name="Stankus"/>
| |
| | |
| == Risk Factors ==
| |
| | |
| ===Can you get chickenpox if you've been vaccinated?===
| |
| | |
| Yes. About 15%–20% of people who have received one dose of chickenpox vaccine do still get chickenpox if they are exposed, but their disease is usually mild. Vaccinated persons who get chickenpox generally have fewer than 50 spots or bumps, which may resemble bug bites more than typical, fluid-filled chickenpox blisters. In 2006, the Advisory Committee on Immunization Practices (ACIP) voted to recommend routine two-dose varicella vaccination for children. In one study, children who received two doses of the chickenpox vaccine were three times less likely to get chickenpox than individuals who have had only one dose.
| |
| | |
| ===What are the serious complications from chickenpox?===
| |
| | |
| Serious complications from chickenpox include bacterial infections which can involve many sites of the body including the skin, tissues under the skin, bone, lungs (pneumonia), joints, and blood. Other serious complications are due directly to infection with the varicella-zoster virus and include viral pneumonia, bleeding problems, and infection of the brain (encephalitis). Many people are not aware that before a vaccine was available approximately 10,600 persons were hospitalized
| |
| and 100 to 150 died as a result of chickenpox in the U.S. every year.
| |
| | |
| ===Can a healthy person who gets varicella die from the disease?===
| |
| | |
| Yes. Many of the deaths and complications from chickenpox occur in previously healthy children and adults. From 1990 to 1994, before a vaccine was available, about 50 children and 50 adults died from chickenpox every year; most of these persons were healthy or did not have a medical illness (such as cancer) that placed them at higher risk of getting severe chickenpox. Since 1999, states have been encouraged to report chickenpox deaths to CDC. These reports have shown that some deaths from chickenpox continue to occur in healthy, unvaccinated children and adults. Most of the healthy adults who died from chickenpox contracted the disease from their unvaccinated children.
| |
| | |
| ==Signs and symptoms==
| |
| | |
| The earliest symptoms (constituting the [[prodrome]]) of shingles include [[headache]], sensitivity to light, [[fever]], and [[malaise]], all of which may be followed by itching, tingling, and [[Pain and nociception|pain]] within one to seven days. The pain may be extreme in the affected nerve, where the rash will later develop, and can be characterized as stinging, tingling, aching, numbing, or throbbing, and can be pronounced with quick stabs of intensity. During this phase, herpes zoster is frequently misdiagnosed as other diseases with similar symptoms, including [[myocardial infarction|heart attacks]] and [[renal colic]]. Some patients may have these symptoms without developing the characteristic rash. This situation, known as "zoster sine herpete," can delay diagnosis and treatment.<ref name="Stankus"/><ref name="Mounsey"/>
| |
| | |
| The initial phase is followed, in most cases, by development of the characteristic skin rashes of herpes zoster. The rash is visually similar to [[hives]], and follow a distribution near [[dermatome]]s, commonly occurring in a stripe or belt-like pattern. The rash evolves into vesicles or small [[blister]]s filled with [[serous fluid]]. The vesicles are generally painful, and their development is often associated with the occurrence of anxiety and further flu-like symptoms, such as fever, tiredness, and generalized pain. The vesicles eventually become hemorrhagic (filled with blood), and crust over within seven to 10 days. As the crusts fall off, patients are rarely left with scarring and pigmented skin.<ref name="Stankus"/>
| |
| | |
| Shingles cannot be passed from one person to another. However, the virus that causes shingles, VZV, can be spread from a person with active shingles to a person who has no immunity to the virus by direct contact with the rash, while in the blister phase. The person exposed would then develop chicken pox, not shingles. The virus is not spread through airborne transmission, such as sneezing or coughing. Once the rash has developed crusts, the person is no longer contagious. A person is not infectious before blisters appear or with post-herpetic neuralgia (pain after the rash is gone).<ref name="Zamula"/><ref name="Stankus"/>
| |
| | |
| Chicken pox virus can remain dormant for decades, and does so inside the [[ganglion]] of the spinal cord. As the virus is reactivated it spreads down peripheral nerve fibers and produces intense pain. The blisters therefore only affect one area of the body and do not cross the midline. They are most common on the torso, but can also appear on the face, eyes or other parts of the body.<ref name="Zamula"/><ref name="Stankus"/>
| |
| | |
| {| align="center"
| |
| |+ '''Development of the shingles rash'''
| |
| ! Day 1 !! Day 2 !! Day 5 !! Day 6
| |
| |-valign="top"
| |
| | [[Image:ShinglesDay1.JPG|143px|Herpes zoster blisters day 1.]]
| |
| | [[Image:ShinglesDay2 ed.JPG|120px|Herpes zoster blisters day 2.]]
| |
| | [[Image:ShinglesDay5 ed.JPG|145px|Herpes zoster blisters day 5]]
| |
| | [[Image:ShinglesDay6 ed.JPG|149px|Herpes zoster blisters day 6, characteristic purple color.]]
| |
| |}
| |
| | |
| ===What is the chickenpox illness like?===
| |
| | |
| In unvaccinated children, chickenpox most commonly causes an illness that lasts about 5-10 days. Children usually miss 5 or 6 days of school or childcare due to their chickenpox and have symptoms such as high fever, severe itching, an uncomfortable rash, and dehydration or headache. In addition, about 1 in 10 unvaccinated children who get the disease will have a complication from chickenpox serious enough to visit a health-care provider. These complications include infected skin lesions, other infections, dehydration from vomiting or diarrhea, or more serious complications such as pneumonia and encephalitis. In vaccinated children, chickenpox illness is typically mild, producing no symptoms at all other than a few red bumps. However, about 25% to 30% of vaccinated children who get the disease will develop illness as serious as unvaccinated children.
| |
| | |
| Certain groups of people are more likely to have more severe illness with serious complications. These include adults, infants, adolescents, and people whose immune systems have been weakened because of illness or medications such as long-term use of steroids.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| If the rash has appeared, identifying this disease (making a [[differential diagnosis]]) only requires a visual examination, since very few diseases produce a rash in a [[dermatomic area|dermatomal pattern (see map)]]. However, [[herpes simplex virus]] (HSV) can occasionally produce a rash in such a pattern. The [[Tzanck test|Tsanck smear]] is helpful for diagnosing acute infection with a herpes virus, but does not distinguish between HSV and VZV.<ref name="pmid2842739">{{cite journal | author = Oranje AP, Folkers E | title = The Tzanck smear: old, but still of inestimable value. | journal = Pediatr Dermatol | volume = 5 | issue = 2 | pages = 127–9 | year = 1988 | pmid = 2842739}}</ref>
| | [[Herpes zoster history and symptoms|History and Symptoms]] | [[Herpes zoster physical examination|Physical Examination]] | [[Herpes zoster laboratory tests|Laboratory Findings ]] | [[Herpes zoster electrocardiogram|Electrocardiogram]] | [[Herpes zoster chest x ray|Chest X Ray]] | [[Herpes zoster other imaging findings|Other Imaging Findings]] | [[Herpes zoster other diagnostic studies|Other Diagnostic Studies]] |
| | |
| When the rash is absent (early or late in the disease, or in the case of zoster sine herpete), herpes zoster can be difficult to diagnose.<ref name="pmid15334402">{{cite journal| author=Chan J, Bergstrom RT, Lanza DC, Oas JG| title=Lateral sinus thrombosis associated with zoster sine herpete| journal=Am J Otolaryngol| volume=25| issue=5| pages=357–60| year=2004| pmid=15334402}}</ref> Apart from the rash, most symptoms can occur also in other conditions.
| |
| | |
| [[Medical test|Laboratory test]]s are available to diagnose herpes zoster. The most popular test detects VZV-specific [[IgM]] [[antibody]] in blood; this only appears during chickenpox or herpes zoster and not while the virus is dormant.<ref name="pmid8809466">{{cite journal| author=Arvin AM| title=Varicella-zoster virus| journal=Clin. Microbiol. Rev| volume=9| issue=3| pages=361–81| year=1996| pmid=8809466| url=http://cmr.asm.org/cgi/reprint/9/3/361.pdf| format=PDF}}</ref> In larger laboratories, [[lymph]] collected from a blister is tested by the [[polymerase chain reaction]] for VZV DNA, or examined with an [[electron microscope]] for virus particles.<ref name="pmid9515761">{{cite journal|author=Beards G, Graham C, Pillay D| title=Investigation of vesicular rashes for HSV and VZV by PCR| journal=J. Med. Virol| volume=54| issue=3| pages=155–7| year=1998| pmid=9515761}}</ref> | |
| | |
| In a recent study, samples of lesions on the skin, eyes, and lung from 182 patients with presumed herpes simplex or herpes zoster were tested with [[real-time PCR]] or with [[viral culture]]. <ref name="pmid15072752">{{cite journal | author = Stránská R, Schuurman R, de Vos M, van Loon AM. | title = Routine use of a highly automated and internally controlled real-time PCR assay for the diagnosis of herpes simplex and varicella-zoster virus infections. | journal = J Clin Virol. | volume=30 | issue=1| pages=39-44 | year=2003 | pmid=15072752}}</ref>. In this comparison, viral culture detected VZV with only a 14.3% [[sensitivity]], although the test was highly specific ([[specificity]]=100%). By comparison, real-time PCR resulted in 100% sensitivity and specificity. Overall testing for herpes simplex and herpes zoster using PCR showed a 60.4% improvement over viral culture.
| |
| | |
| === Physical Examination ===
| |
| ====Skin====
| |
| | |
| <div align="left">
| |
| <gallery heights="175" widths="175">
| |
| Image:Herpes zoster chest.jpg|Herpes zoster on the chest
| |
| Image:Varicella child-ab.jpg
| |
| Image:varicella zoster.jpg|Varicella zoster
| |
| Image:shingles2.jpg|Shingles
| |
| </gallery>
| |
| </div>
| |
| | |
| (Images shown below courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
| |
| | |
| <div align="left">
| |
| <gallery heights="175" widths="175">
| |
| Image:Skin zoster buttocks1.jpg|Herpes Zoster: Coalesced vesicles resulting from reativation of HZV infection.
| |
| Image:Skin zoster buttocks2.jpg|Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
| |
| Image:Skin zoster buttocks4.jpg|Herpes Zoster: Dermatomally distributed vesicles in patient with HZV infection.
| |
| Image:Skin_zoster_buttocks3.jpg|Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
| |
| </gallery>
| |
| </div>
| |
| | |
| | |
| <div align="left">
| |
| <gallery heights="175" widths="175">
| |
| Image:skin_herpes_zoster.jpg|Herpes Zoster. <br> (Courtesy of Josh Fierer, M.D. and Charlie Goldberg, M.D.)
| |
| Image:c3zoster.jpg|Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
| |
| Image:c3zoster2.jpg|Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| [[Image:Disease varicella3.jpg|thumb|right|Transmission electron micrograph of varicella-zoster virions]] | | [[Herpes zoster medical therapy|Medical Therapy]] | [[Herpes zoster primary prevention|Primary Prevention]] | [[Herpes zoster cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Herpes zoster future or investigational therapies|Future or Investigational Therapies]] |
| [[Image:Chickenpox-virus.jpg|thumb|right|[[Electron microscope|Electron micrograph]] of [[Varicella zoster virus]]. Approx. 150.000-fold magnification.]]
| | ==Case Studies== |
| | | [[Herpes zoster case study one|Case #1]] |
| Currently, there is no cure available for Herpes zoster, nor a treatment to effectively eliminate the virus from the body. However, there are some treatments that can mitigate the length of the disease and alleviate certain side effects.
| | ==Related Chapters== |
| | |
| ===Antiviral drugs===
| |
| | |
| [[Aciclovir|Acyclovir]] (an [[antiviral drug]]) inhibits replication of the viral DNA, and is used both as [[prophylaxis]] (''e.g.'', in patients with [[AIDS]]) and as therapy for herpes zoster. Other antivirals are [[valacyclovir]] and [[famciclovir]]. During the [[Acute (medical)|acute phase]], oral acyclovir should be given. Use of acylovir is most effective in moderating the progress of the symptoms, and in preventing post-herpetic neuralgia, if started within 24 to 72 hours of the onset of symptoms, so medical care should be obtained as soon as the condition is recognized. [[Immunocompromised]] patients may respond best to intravenous acyclovir. In patients who are at high risk for recurrences, an oral dose of acyclovir, taken twice daily, is usually effective.<ref name="Johnson"/> It is also reported that the [[amino acid]] [[lysine]] inhibits the replication of herpes zoster.<ref>{{cite journal|last=Griffith|first=RS|coauthors=Walsh DE, Myrmel KH, Thmpson RW, and Behforooz A|title=Success of L-lysine therapy in frequently recurrent herpes simplex infection. Treatment and prophylaxis|journal=Dermatologica|date=1987|volume=175|issue=4|pages=183-190|id=PMID 3115841}}</ref>
| |
| | |
| ===Other drugs===
| |
| | |
| [[Cimetidine]], a common component of over-the-counter heartburn medication, has been shown to lessen the severity of herpes zoster outbreaks in several different instances.<ref>{{cite journal|author=Kapinska-Mrowiecka M, &Toruwski G | title=Efficacy of cimetidine in treatment of herpes zoster in the first 5 days from the moment of disease manifestation. | journal= Pol Tyg Lek. | year=1996. | pages=338-339 | volume=51 | issue=23-26 | id=PMID 9273526}}</ref><ref>{{cite journal|author=Hayne ST, & Mercer JB|title=Herpes zoster: treatment with cemetidine|journal=Canadian Medical Association Journal|year=1983|pages=1284-1285| volume=129|issue=12|id=PMID 6652595}}</ref><ref>{{cite journal|author=Notmann J, Arieli J, Hart J, Levinsky H, Halbrecht I, & Sendovsky U | title=In vitro cell-mediated immune reactions in herpes zoster patients treated with cimetidine. | journal=Asian Pacific Journal Allergy and Immunology|year=1994|pages=51-58|volume=12|issue=1|id=PMID 7872992}}</ref> This usage is considered an [[off-label use]] of the drug. In addition, cimetidine and [[probenecid]] have been shown to reduce the renal clearance of aciclovir. <ref>{{cite journal|author=De Bony F, Tod M, Bidault R, On NT, Posner J, & Rolan P| title=Multiple interactions of cimetidine and probenecid with valaciclovir and its metabolite acyclovir |journal=Antimicrobial Agents and Chemotherapy|year=2002|pages=458-463|volume=46 |issue=2|id=PMID 11796358}}</ref> The study showed these compounds reduce the rate, but not the extent, at which valaciclovir is converted into aciclovir. Renal clearance of aciclovir was reduced by approximately 24% and 33% respectively. In addition, respective increases in the peak plasma concentration of acyclovir of 8% and 22% were observed. The authors concluded that these effects were "not expected to have clinical consequences regarding the safety of valaciclovir". Due to the tendency of aciclovir to precipitate in renal tubules, combining these drugs should only occur under the supervision of a physician. | |
| | |
| ===Complementary Therapies===
| |
| Digestive Enzymes are available on prescription and in some over the counter preparations. Before the availability of antivirals, oral pancreatic enzyme therapy in shingles was used in some countries and later subjected to clinical and scientific research. A large scale multi-centre clinical study, using an oral preparation of such enzymes, has shown promising results.<ref name="pmid7713467">{{cite journal |author=Billigmann P |title=[Enzyme therapy--an alternative in treatment of herpes zoster. A controlled study of 192 patients] |language=German |journal=Fortschr. Med. |volume=113 |issue=4 |pages=43-8 |year=1995 |pmid=7713467 |doi=}}</ref> <ref name="pmid16813460">{{cite journal |author=Roxas M |title=Herpes zoster and postherpetic neuralgia: diagnosis and therapeutic considerations |journal=Alternative medicine review : a journal of clinical therapeutic |volume=11 |issue=2 |pages=102-13 |year=2006 |pmid=16813460 |doi=}}</ref> The results of another clinical study support the concept that oral enzyme therapy is beneficial in diseases characterized in part by TGF-beta overproduction that included shingles patients. <ref name="pmid11561866">{{cite journal |author=Desser L, Holomanova D, Zavadova E, Pavelka K, Mohr T, Herbacek I |title=Oral therapy with proteolytic enzymes decreases excessive TGF-beta levels in human blood |journal=Cancer Chemother. Pharmacol. |volume=47 Suppl |issue= |pages=S10-5 |year=2001 |pmid=11561866 |doi=}}</ref> TGF-β has also been found to be elevated in instances of VZV infection. <ref name="pmid15547808">{{cite journal |author=Kaygusuz I, Gödekmerdan A, Keleş E, ''et al'' |title=The role of viruses in idiopathic peripheral facial palsy and cellular immune response |journal=American journal of otolaryngology |volume=25 |issue=6 |pages=401-6 |year=2004 |pmid=15547808 |doi=}}</ref> <ref name="pmid11094200">{{cite journal |author=Sato M, Abe T, Tamai M |title=Expression of the Varicella Zoster Virus Thymidine Kinase and Cytokines in Patients with Acute Retinal Necrosis Syndrome |journal= |volume=44 |issue=6 |pages=693 |year=2000 |pmid=11094200 |doi=}}</ref>
| |
| | |
| ==Prognosis==
| |
| The rash and pain usually subside within 3 to 5 weeks. Many patients develop a painful condition called [[postherpetic neuralgia]], which is often difficult to manage. In some patients, herpes zoster can reactivate subclinically, with pain in a dermatomal distribution without [[rash]]. This condition is known as ''zoster sine herpete,'' and may be more complicated, affecting multiple levels of the [[nervous system]] and causing multiple [[cranial]] [[neuropathy|neuropathies]], [[neuritis|polyneuritis]], [[myelitis]], or [[aseptic meningitis]]. Sometimes serious effects including partial [[Bell's palsy|facial paralysis]] (usually temporary), ear damage, or [[encephalitis]] may occur. Shingles on the upper half of the face (the first branch of the [[trigeminal nerve]]) may result in [[eye]] damage and require urgent ophthalmological assessment. Ocular complications occur in approximately one half of patients with involvement of the ophthalmic division of the [[trigeminal nerve]]. These complications include [[mucopurulent]] [[conjunctivitis]], episcleritis, [[keratitis]] and anterior [[uveitis]]. Cranial nerve [[palsy|palsies]] of the third, fourth and sixth [[cranial nerve]]s may occur, affecting [[Extraocular muscles|extraocular motility]].<ref name="Johnson">{{cite journal|journal=BMJ|date=2003|volume=326|issue=7392|pages=748|doi=10.1136/bmj.326.7392.748|author=Johnson, RW & Dworkin, RH|title=Clinical review: Treatment of herpes zoster and postherpetic neuralgia}}</ref>
| |
| | |
| Since shingles is a reactivation of a virus contracted previously—often decades earlier—it cannot be induced by exposure to another person with shingles or [[chicken pox]]. Those with active blisters, however, can spread chicken pox to others who have never had that condition and who have not been vaccinated against it.<ref name="Zamula"/>
| |
| | |
| ===What are the serious complications from chickenpox?=== | |
| | |
| Serious complications from chickenpox include bacterial infections which can involve many sites of the body including the skin, tissues under the skin, bone, lungs (pneumonia), joints, and blood. Other serious complications are due directly to infection with the varicella-zoster virus and include viral pneumonia, bleeding problems, and infection of the brain (encephalitis). Many people are not aware that before a vaccine was available approximately 10,600 persons were hospitalized and 100 to 150 died as a result of chickenpox in the U.S. every year.
| |
| | |
| ==Prevention==
| |
| | |
| [[Zostavax]] is a [[vaccine]] developed by [[Merck & Co.]] which has proven successful in preventing half the cases of herpes zoster in a study of 38,000 people who received the vaccine. <ref>Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD et al. (2005). "A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults". N Engl J Med 253 (22): 2271–84. PMID 15930418</ref> The vaccine also reduced by two-thirds the number of cases of postherpetic neuralgia. <ref>Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD et al. (2005). "A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults". N Engl J Med 253 (22): 2271–84. PMID 15930418</ref> However, prior to the vaccine, it has long been known that adults received natural immune boosting from contact with children infected with [[varicella]]. This helped to suppress the reactivation of herpes zoster.<ref>{{cite journal | author = Brisson M, Gay N, Edmunds W, Andrews N | title = Exposure to varicella boosts immunity to herpes-zoster: implications for mass vaccination against chicken pox. | journal = Vaccine | volume = 20 | issue = 19-20 | pages = 2500-7 | year = 2002 | id = PMID 12057605}}</ref> In Massachusetts, herpes zoster incidence increased 90%, from 2.77/1000 to 5.25/1000 in the period of increasing varicella vaccination 1999-2003.<ref>{{cite journal | last=Yih|first=WK |coauthors =Brooks DR, Lett SM, Jumaan AO, Zhang Z, Clements KM, & Seward JF| title=The incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccination coverage, 1998-2003 | journal=BMC Public Health | volume=5| issue=1 | year=2005 | pages=68-68 | id=PMID 15960856}}</ref> The effectiveness of the varicella vaccine itself is dependent on this exogenous (outside) boosting mechanism. Thus, as natural cases of varicella decline, so has the effectiveness of the vaccine.<ref>{{cite journal | first=GS|last=Goldman| title=Universal varicella vaccination: efficacy trends and effect on herpes zoster | journal=International Journal of Toxicology| volume=24| issue=4 | year=2005 | pages=205-213 | id=PMID 16126614}}</ref> | |
| | |
| The intake of micronutrients, including antioxidant vitamins, A, C, E and vitamin B, as well as fresh fruit, may reduce the risk of developing shingles. In one study, patients who consumed less than one serving of fruit a day had three times the risk as those who consumed over three servings per day. For those aged 60 or more, micronutrient and vegetable intake had a similar lowering of risk.<ref name="pmid16330478">{{cite journal |author=Thomas SL, Wheeler JG, Hall AJ |title=Micronutrient intake and the risk of herpes zoster: a case-control study |journal=International Journal of Epidemiology |volume=35 |issue=2 |pages=307-14 |year=2006 |pmid=16330478 |doi=10.1093/ije/dyi270}}</ref> A recent study evaluated the effects of two types of behavioral intervention, [[Tai Chi Chuan|Tai Chi]] and health education, on healthy adults, who, after 16 weeks of the intervention, were vaccinated with VARIVAX, a live attenuated Oka/Merck Varicella zoster virus vaccine.<ref>{{cite journal|last=Irwin|first=MR|coauthors=Olmstead, R & Oxman, MN|title=Augmenting Immune Responses to Varicella Zoster Virus in Older Adults: A Randomized, Controlled Trial of Tai Chi|date=2007|journal=Journal of the American Geriatrics Society|volume=55|issue=4|pages=511-517|url=http://www.blackwell-synergy.com/doi/abs/10.1111/j.1532-5415.2007.01109.x|doi=10.1111/j.1532-5415.2007.01109.x|accessdate=2007-04-08}}</ref>
| |
| | |
| === Primary Prevention ===
| |
| [[Varicella (Chickenpox) Vaccine]] can prevent this disease. Currently, two doses of vaccine are recommended for children, adolescents, and adults.
| |
| | |
| ===Vaccine===
| |
| A live attenuated VZV Oka/Merck strain [[vaccine]] is available and is marketed under the trade name ''Varivax''. It was developed by [[Merck & Co.|Merck, Sharp & Dohme]] in the 1980s from the Oka strain virus isolated and attenuated by Michiaki Takahashi and colleagues in the 1970s. It was submitted to the U.S. [[Food and Drug Administration]] for approval in 1990 and was approved in 1995. Since then, it has been added to the recommended vaccination schedules for children in Australia, the United States, and many other countries, causing controversy because it is only expected to be effective for about twenty years, leaving adults vulnerable to the most dangerous forms of infection by this virus. The use of varicella virus vaccine live (Varivax) has been limited by practitioner concerns that adults vaccinated as children could develop severe varicella infection complications if immunity provided by the vaccine is not long-lasting. However, clinical data has proved that the vaccine is effective for over 10 years in preventing varicella infection in healthy individuals and when breakthrough infections do occur, illness is typically mild.<ref>Centers for Disease Control and Prevention (CDC). Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1996;45(No.RR-11)</ref>
| |
| | |
| In 2006, the [[FDA]] approved [[Zostavax]] for the prevention of shingles. Zostavax is a more concentrated formulation of the Varivax vaccine, designed to elicit an immune response in the eldery whose immunity to VZV wanes with advancing age. <ref>Poland, Gregory. "The Growing Paradigm of Preventing Disease." Annals of Internal Medicine. 2005;143539-541. </ref>
| |
| | |
| ==References==
| |
| {{Reflist|2}}
| |
| | |
| ==See also== | |
| *[[Progressive outer retinal necrosis]] | | *[[Progressive outer retinal necrosis]] |
|
| |
|
| ==External links== | | ==External Links== |
|
| |
|
| * National Institute of Neurological Disorders and Stroke {{NINDS|shingles}}
| |
| * {{NHS|335}}
| |
| * [http://www.emergency-medicine.info/articles/shingles.html Information about management of Shingles for physicians]
| |
| * [http://www.lib.uiowa.edu/hardin/md/shingles.html Links to pictures of Shingles (Hardin MD)] University of Iowa
| |
| * [http://www.aftershingles.com/index.html After Shingles--Information about Shingles and Post-Herpetic Neuralgia]
| |
| * [http://www.nei.nih.gov/health/cornealdisease/index.asp#f The National Eye Institute (NEI)] | | * [http://www.nei.nih.gov/health/cornealdisease/index.asp#f The National Eye Institute (NEI)] |
| * [http://www.herpies.co.uk Genital Herpies Resource]
| |
| * [http://www.cdc.gov/vaccines/vpd-vac/varicella/in-short-adult.htm Center for Disease Control on Varicella] | | * [http://www.cdc.gov/vaccines/vpd-vac/varicella/in-short-adult.htm Center for Disease Control on Varicella] |
| * [http://wwwn.cdc.gov/travel/yellowBookCh4-Chickenpox.aspx Center for Disease Control on Chickenpox] | | * [http://wwwn.cdc.gov/travel/yellowBookCh4-Chickenpox.aspx Center for Disease Control on Chickenpox] |
| Line 220: |
Line 47: |
| {{Viral diseases}} | | {{Viral diseases}} |
| {{Varicella zoster}} | | {{Varicella zoster}} |
| | | {{WikiDoc Help Menu}} |
| <br>
| | {{WikiDoc Sources}} |
| [[da:Helvedesild]]
| |
| [[de:Herpes Zoster]]
| |
| [[es:Herpes zóster]]
| |
| [[fr:Zona]]
| |
| [[it:Herpes zoster]]
| |
| [[he:שלבקת חוגרת]]
| |
| [[lb:Gürtelrous]]
| |
| [[nl:Gordelroos]]
| |
| [[ja:帯状疱疹]]
| |
| [[no:Helvetesild]]
| |
| [[pt:Herpes-zóster]]
| |
| [[simple:Shingles]]
| |
| [[sl:Pasovec]]
| |
| [[fi:Vyöruusu]]
| |
| [[sv:Bältros]]
| |
| [[th:โรคงูสวัด]]
| |
| [[zh:带状疱疹]]
| |
| | |
|
| |
|
| [[Category:Infectious skin diseases]] | | [[Category:Infectious skin diseases]] |
| [[Category:Viral diseases]] | | [[Category:Viral diseases]] |
| [[Category:Herpesviruses]] | | [[Category:Herpesviruses]] |
| [[Category:Infectious disease]]
| |
| [[Category:Overview complete]]
| |
| [[pl:Półpasiec]]
| |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |
|
| |
|
| |
| == Other ==
| |
|
| |
| [http://thetvtopc.com/Reverse_Cell_Phone_Lookup_Number cell phone lookup]
| |