Hepatocellular carcinoma: Difference between revisions
| Line 17: | Line 17: | ||
==[[Hepatocellular carcinoma overview|Overview]]== | ==[[Hepatocellular carcinoma overview|Overview]]== | ||
== | == [[Hepatocellular carcinoma epidemiology and demographics|Epidemiology & Demographics]] == | ||
==Pathological Images== | ==Pathological Images== | ||
Revision as of 13:53, 23 December 2011
For patient information click here
| Hepatocellular carcinoma | |
 | |
|---|---|
| Hepatocellular Carcinoma, Hepatitis C positive. Tumor growth in portal vein | |
| ICD-10 | C22.0 |
| ICD-9 | 155 |
| ICD-O: | 8170/3 |
| MedlinePlus | 000280 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]
|
Hepatocellular carcinoma Microchapters |
|
Differentiating Hepatocellular carcinoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hepatocellular carcinoma On the Web |
|
American Roentgen Ray Society Images of Hepatocellular carcinoma |
|
Risk calculators and risk factors for Hepatocellular carcinoma |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Epidemiology & Demographics
Pathological Images
-
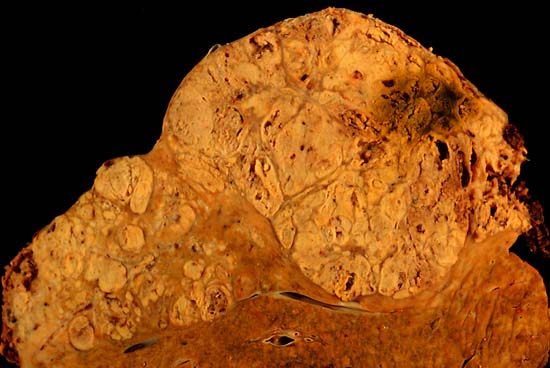
Hepatocelluler carcinoma. The image shows a longitudinal slice taken through the full length of the liver.
(Courtesy of Ed Uthman, MD) -
The tumor is at the top, cirrhotic liver at the bottom, and a fibrous reaction in between. Hepatocellular carcinomas can have a variety of gross patterns, including multinodular / multifocal, such as this one.
(Courtesy of Ed Uthman, MD)
Pathogenesis
Hepatocellular carcinoma, like any other cancer, develops when there is a mutation to the cellular machinery that causes the cell to replicate at a higher rate and/or results in the cell avoiding apoptosis. In particular, chronic infections of Hepatitis B and/or C can aid the development of hepatocellular carcinoma by repeatedly causing the body's own immune system to attack the liver cells, some of which are infected by the virus, others merely bystanders. While this constant cycle of damage followed by repair can lead to mistakes during repair which in turn lead to carcinogenesis, this hypothesis is more applicable, at present, to Hepatitis C. In Hepatitis B, however, the integration of the viral genome into infected cells is the most consistently associated factor in malignancy. Alternatively, repeated consumption of large amounts of ethanol can have a similar effect. The toxin aflatoxin from certain Aspergillus species of fungus is a carcinogen and aids carcinogenesis of hepatocellular cancer by building up in the liver. The combined high prevalence of rates of aflaxtoxin and hepatitis B in countries like China and western Africa has led to relatively high rates of heptatocellular carcinoma in these regions. Other viral hepatitides such as hepatitis A have no potential to become a chronic infection and thus are not related to hepatocellular carcinoma.
Diagnosis, screening and monitoring
Hepatocellular carcinoma (HCC) most commonly appears in a patient with chronic viral hepatitis (hepatitis B or hepatitis C, 20%) or with cirrhosis (about 80%). These patients commonly undergo surveillance with ultrasound due to the cost-effectiveness.
In patients with a higher suspicion of HCC (such as rising alpha-fetoprotein and des-gamma carboxyprothrombin levels), the best method of diagnosis involves a CT scan of the abdomen using intravenous contrast agent and three-phase scanning (before contrast administration, immediately after contrast administration, and again after a delay) to increase the ability of the radiologist to detect small or subtle tumors. It is important to optimize the parameters of the CT examination, because the underlying liver disease that most HCC patients have can make the findings more difficult to appreciate.
On CT, HCC can have three distinct patterns of growth:
- A single large tumor
- Multiple tumors
- Poorly defined tumor with an infiltrative growth pattern
Once imaged, diagnosis is confirmed by percutaneous biopsy and histopathologic analysis.
The key characteristics on CT are hypervascularity in the arterial phase scans, washout or de-enhancement in the portal and delayed phase studies, a pseudocapsule and a mosaic pattern. Both calcifications and intralesional fat may be appreciated.
CT scans use contrast agents, which are typically iodine or barium based. Some patients are allergic to one or both of these contrast agents, most often iodine. Usually the allergic reaction is manageable and not life threating.
An alternative to a CT imaging study would be the MRI.
Pathology
Macroscopically, liver cancer appears as a nodular or infiltrative tumor. The nodular type may be solitary (large mass) or multiple (when developed as a complication of cirrhosis). Tumor nodules are round to oval, grey or green (if the tumor produces bile), well circumscribed but not encapsulated. The diffuse type is poorly circumscribed and infiltrates the portal veins, or the hepatic veins (rarely).
Microscopically, there are four architectural and cytological types (patterns) of hepatocellular carcinoma: fibrolamellar, pseudoglandular (adenoid), pleomorphic (giant cell) and clear cell. In well differentiated forms, tumor cells resemble hepatocytes, form trabeculae, cords and nests, and may contain bile pigment in cytoplasm. In poorly differentiated forms, malignant epithelial cells are discohesive, pleomorphic, anaplastic, giant. The tumor has a scant stroma and central necrosis because of the poor vascularization.1
Staging and prognosis
Important features that guide treatment include: -
- size
- spread (stage)
- involvement of liver vessels
- presence of a tumor capsule
- presence of extrahepatic metastases
- presence of daughter nodules
- vascularity of the tumor
MRI is the best imaging method to detect the presence of a tumor capsule.
Treatment
- Liver transplantation to replace the liver with a cadaver liver or a live donor lobe. Historically low survival rates (20%-36%) recent improvement (61.1%; 1996-2001), likely related to adoption of Milan criteria at US transplantation centers. If the tumor disease has metastasized, the immuno-suppressant post-transplant drugs decrease the chance of survival. NIH
- Surgical resection to remove a tumor to treat small or slow-growing tumors if they are diagnosed early. This treatment offers the best prognosis for long-term survival but unfortunately is possible in only 10-15% of cases. Resection in cirrhotic patients carries high morbidity and mortality. Medicinenet
- Percutaneous ethanol injection (PEI) well tolerated, high RR in small (< 3 cm) solitary tumors; as of 2005, no randomized trial comparing resection to percutaneous treatments; recurrence rates similar to those for postresection.
- Transcatheter arterial chemoembolization (TACE) is usually performed in the treatment of large tumors (larger than 3 cm and less than 4 cm in diameter), most frequently by intraarterially injecting an infusion of antineoplastic agents mixed with iodized oil (such as Lipiodol). As of 2005, multiple trials show objective tumor responses and slowed tumor progression but questionable survival benefit compared to supportive care; greatest benefit seen in patients with preserved liver function, absence of vascular invasion, and smallest tumors.
- Sealed source radiotherapy can be used to destroy the tumor from within (thus minimizing exposure to healthy tissue). TheraSphere is an FDA approved treatment which has been shown in clinical trials to increase survival rate of low-risk patients. This method uses a catheter (inserted by a radiologist) to deposit radioactive particles to the area of interest.
- Radiofrequency ablation (RFA) uses high frequency radio-waves to ablate the tumour.
- Intra-arterial iodine-131–lipiodol administration Efficacy demonstrated in unresectable patients, those with portal vein thrombus. This treatment is also used as adjuvant therapy in resected patients (Lau at et, 1999). It is believed to raise the 3-year survival rate from 46 to 86%. This adjuvant therapy is in phase III clinical trials in Singapore and is available as a standard medical treatment to qualified patients in Hong Kong.
- Combined PEI and TACE can be used for tumors larger than 4 cm in diameter, although some Italian groups have had success with larger tumours using TACE alone.
- High intensity focused ultrasound (HIFU) (not to be confused with normal diagnostic ultrasound) is a new technique which uses much more powerful ultrasound to treat the tumour. Still at a very experimental stage. Most of the work has been done in China. Some early work is being done in Oxford and London in the UK.
- Hormonal therapy Antiestrogen therapy with tamoxifen studied in several trials, mixed results across studies, but generally considered ineffective Octreotide (somatostatin analogue) showed 13-month MS v 4-month MS in untreated patients in a small randomized study; results not reproduced.
- Chemotherapy adjuvant: No randomized trials showing benefit of neoadjuvant or adjuvant systemic therapy in HCC; single trial showed decrease in new tumors in patients receiving oral synthetic retinoid for 12 months after resection/ablation; results not reproduced. Clinical trials have varying results.[1]
- Palliative: Regimens that included doxorubicin, cisplatin, fluorouracil, interferon, epirubicin, or taxol, as single agents or in combination, have not shown any survival benefit (RR, 0%-25%); a few isolated major responses allowed patients to undergo partial hepatectomy; no published results from any randomized trial of systemic chemotherapy.
- Cryosurgery: Cryosurgery is a new technique that can destroy tumors in a variety of sites (brain, breast, kidney, prostate, liver). Cryosurgery is the destruction of abnormal tissue using sub-zero temperatures. The tumor is not removed and the destroyed cancer is left to be reabsorbed by the body. Initial results in properly selected patients with unresectable liver tumors are equivalent to those of resection. Cryosurgery involves the placement of a stainless steel probe into the center of the tumor. Liquid nitrogen is circulated through the end of this device. The tumor and a half inch margin of normal liver are frozen to -190°C for 15 minutes, which is lethal to all tissues. The area is thawed for 10 minutes and then re-frozen to -190°C for another 15 minutes. After the tumor has thawed, the probe is removed, bleeding is controlled, and the procedure is complete. The patient will spend the first post-operative night in the intensive care unit and typically is discharged in 3 - 5 days. Proper selection of patients and attention to detail in performing the cryosurgical procedure are mandatory in order to achieve good results and outcomes. Frequently, cryosurgery is used in conjunction with liver resection as some of the tumors are removed while others are treated with cryosurgery. Patients may also have insertion of a hepatic intra-arterial artery catheter for post-operative chemotherapy. As with liver resection, your surgeon should have experience with cryosurgical techniques in order to provide the best treatment possible.
Abbreviations: HCC, hepatocellular carcinoma; TACE, transarterial embolization/chemoembolization; PFS, progression-free survival; PS, performance status; HBV, hepatitis B virus; PEI, percutaneous ethanol injection; RR, response rate; MS, median survival.
Awareness
The Jade Ribbon Campaign is used for awareness of liver cancer in the Pacific Islands and will be introduced into America someday.
Jade is the official color of liver cancer.
Future directions
Current research includes the search for the genes that are disregulated in HCC,[2] protein markers[3], and other predictive biomarkers.[4][5] As similar research is yielding results in various other malignant diseases, it is hoped that identifying the aberrant genes and the resultant proteins could lead to the identification of pharmacological interventions for HCC.[6]
References
- ↑ [1] American Society of Clinical Oncology, 2005 Annual Meeting, Abstracts on Hepatobiliary Cancer
- ↑ Genetic research in HCC Stanford Asian Liver Center
- ↑ Huntington Medical Research Institute News, May 2005
- ↑ [2] Journal of Clinical Oncology, Special Issue on Molecular Oncology: Receptor-Based Therapy, April 2005
- ↑ Lau W, Leung T, Ho S, Chan M, Machin D, Lau J, Chan A, Yeo W, Mok T, Yu S, Leung N, Johnson P (1999). "Adjuvant intra-arterial iodine-131-labelled lipiodol for resectable hepatocellular carcinoma: a prospective randomised trial". Lancet. 353 (9155): 797–801. PMID 10459961.
- ↑ Thomas M, Zhu A (2005). "Hepatocellular carcinoma: the need for progress". J Clin Oncol. 23 (13): 2892–9. PMID 15860847.
External links
Template:Gastroenterology Template:Tumors Template:Tumor morphology de:Leberzellkarzinom fi:Maksasyöpä hr:Rak jetre hu:Májtumor la:Carcinoma hepatocellulare ko:간암 nl:Leverkanker no:Leverkreft sv:Levercancer