Esophagitis pathophysiology
|
Esophagitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Esophagitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Esophagitis pathophysiology |
|
Risk calculators and risk factors for Esophagitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
Overview
Eosinophilic esophagitis is an immunoallergic disorder resulting from the interaction between genetics and environmental triggers such as repeated exposure to food and aeroallergens. The eosinophils are absent in an otherwise normal esophagus, the presence of the eosinophils in the esophagus suggests GERD or EoE. The documented cytokine expression profile in the esophageal tissue of EoE patients is that of a TH2 inflammatory response. IL-5 and IL-13 are produced by the type-2 helper T cells (Th2) in response to the antigenic proteins from the food or inhalation. IL-13 further stimulates the epithelial cells of the esophagus to produce large proteins to induce a gene called eotaxin-3, which in turn recruits eosinophils from the peripheral blood into the tissue. IL-5 prolongs the survival of the eosinophils. The activated TH2 response leads to the recruitment and activation of Mast cells degranulate and cause tissue damage and repair. Cytokines produced by TH-1 cells are tumor necrosis factor (TNF)-α, Interferon (IFN)-γ, TNF-α is expressed by the epithelial cells of the esophagus whereas the INF-γ is upregulated by the peripheral T cells. Delayed or type- IV hypersensitivity is the mechanism is involved in the EoE rather than the non-IgE. It is postulated that the EoE-defining endoscopic and histologic manifestations are a culmination of the disease process which, may have debilitating long-term effects including strictures and food impactions in untreated or poorly managed cases of EoE. CD34+ myeloid precursor cells in the bone marrow produce eosinophils and then the eosinophils develop granulation and migrate to vascular spaces. Eosinophils although present in all the layers of the esophagus in patients with EoE, they are predominant in the lamina propria and submucosa of the esophagus. The preformed granule proteins of the eosinophils are ECP- Eosinophil Cationic Protein, MBP- Major Basic Protein, EPO- Eosinophil Peroxidase, EDN- Eosinophil Derived Neurotoxin. Upon the stimulation and the degranulation, the eosinophils release the granule proteins into the tissues. Eosinophils synthesize and release cytokines such as IL-5, IL-13, Transforming growth factor (TGF)-α and -β, Chemokines (eotaxins and RANTES), Lipid mediators such as platelet activating factor (PAF) and leukotriene C4. IL-5, IL-13, and granulocyte-macrophage colony stimulating factor (GM-CSF) can cause the maturation and migration of the eosinophils. Eosinophils cause inflammation in the EoE patients by the following mechanisms Angiogenic molecules from the eosinophils recruits the inflammatory cells and the increase the vascularity. Fibrogenic mediators such as TGF-β1 and matrix metalloproteinase 9 (MMP)-9 causes the airway remodeling. MBP and MMP-9 disrupt the integrity of the epithelial cells of the esophageal through their involvement in smooth muscles, fibroblasts, and cell-adhesion molecules. The above-mentioned processes lead to tissue remodeling eventually causing an overall esophageal dysfunction.Pathophysiology of reflux esophagitis depends on several mechanisms that lead to the retrograde movement of the acidic content of the stomach to the esophagus. These mechanisms include transient lower esophageal sphincter relaxation, hypotensive lower esophageal sphincter, hiatal hernia, and prolongedesophageal acid clearance.
Pathophysiology
Normal physiology of the food motility through the esophagus
- The esophagus is a part of the gastrointestinal tract which is responsible of moving the food from the mouth to the rectum.[1]
- The esophagus has anti-reflux barrier which prevents the return of the acidic contentof the stomach back to the esophagus. The anti-reflux barrier consists of the lower esophageal sphincter (LES) and the related part of the diaphragm.
- The lower esophageal sphincter is contracting smooth muscle at the end of the esophagus responsible for the food passage to the stomach. LES has high pressure tone which helps keeping it a strong barrier between the esophagus and the stomach.

Reflux Esophagitis
- Pathogenesis of GERD depends on various mechanisms that lead to the reflux of the gastric acidic contents into the esophagus.
- Several mechanisms impair the anti-reflux barrier and cause esophageal dysmotility. These mechanisms include the following:[2][3]
- Transient lower esophageal sphincter relaxations
- Hypotensive lower esophageal sphincter
- Hiatus hernia
- Impaired esophageal acid clearance
- Delayed gastric emptying
Transient lower esophageal sphincter relaxations
- Transient lower esophageal sphincter relaxations is considered the main mechanism of GERD development in most of the patients. It occurs alongside a normal LES and more common with obesity. [4]
- Distension of the stomach worsens the case of transient lower esophageal sphincter relaxation. The diaphragm is also affected by the sphincter relaxation leading to diaphragm inhibition. [5]
- Some of the GERD patients have hypotensive lower esophageal sphincter which leads to retrograde movement of the gastric content into the esophagus.
Hiatal hernia
- A hiatal hernia occurs as part of the stomach is dislocated into the chest. This dislocation leads to placement of the LES above the diaphragm impairing the acid clearance.[6]
- Increase the exposure of the lower esophagus due to a hiatal hernia plays a big role in the pathogenesis of GERD.
Impaired mucosal resistance
- The esophagus has pre-epithelial and epithelial defensive mechanisms against the acidic components that can lead to esophageal injury. However, these defensive mechanisms are limited and weak to stand against injury in case of excessive acid exposure.
- In case of an excessive increase of the noxious agents more than the ability of the mucosal defensive mechanism to eliminate them, mucosal injury occurs and GERD develops.
- The gastric acid leads to erosion of the esophageal mucosa and destruction of the intercellular junctions which leads to increase cellular permeability. The increase in the cellular permeability is proved by the dilation of the intercellular spaces and explains the typical symptoms (e.g, heartburn) of GERD.
Eosinophilic Esophagitis
- The pathophysiology of the EoE is as follows:[7][8][9][10][11][12][13][14][15][16]
- Eosinophilic esophagitis is an immunoallergic disorder resulting from the interaction between genetics and environmental triggers such as repeated exposure to food and aeroallergens.
- Patients presenting with EoE have a history of:
- Elevated serum IgE levels
- Response to interventions such as diet restriction
- History of food hypersensitivity
- Eosinophils originate from CD34+ myeloid precursor cells in the bone marrow, mature to a granulated state and migrate to the vascular spaces.
- The eosinophils are absent in an otherwise normal esophagus, the presence of the eosinophils in the esophagus suggests GERD or EoE.
- They tend to be present in all layers of the esophagus in EoE, but predominate in the lamina propria and submucosal regions.
- The documented cytokine expression profile in the esophageal tissue of patients is that of a TH2 inflammatory response.
- IL-5 and IL-13 are produced by the type-2 helper T cells (Th2) in response to the antigenic proteins from the food or inhalation.
- IL-13 further stimulates the epithelial cells of the esophagus to produce large proteins to induce a gene called eotaxin-3, which in turn recruits eosinophils from the peripheral blood into the tissue.
- IL-5 prolongs the survival of the eosinophils.
- The activated TH2 response leads to the recruitment and activation of
- Mast cells degranulate and cause tissue damage and repair.
- Cytokines produced by TH-1 cells are
- TNF-α is expressed by the epithelial cells of the esophagus whereas INF-γ is upregulated by the peripheral T cells.
- Delayed or type- IV hypersensitivity is the mechanism is involved in the EoE.
- It is postulated that the EoE-defining endoscopic and histologic manifestations are a culmination of the disease process which, may have debilitating long-term effects including strictures and food impactions in untreated or poorly managed cases of EoE.
- The preformed granule proteins of the eosinophils are
- ECP- Eosinophil Cationic Protein
- MBP- Major Basic Protein
- EPO- Eosinophil Peroxidase
- EDN- Eosinophil Derived Neurotoxin
- Upon the stimulation and the degranulation, the eosinophils release the granule proteins into the tissues.
- Eosinophils synthesize and release cytokines such as
- IL-5
- IL-13
- Transforming growth factor (TGF)-α and -β
- Chemokines (eotaxins and RANTES)
- Lipid mediators such as platelet activating factor (PAF) and leukotriene C4
- IL-5, IL-13, and granulocyte-macrophage colony stimulating factor (GM-CSF) can cause the maturation and migration of the eosinophils.
- Eosinophils cause inflammation in the EoE patients by the following mechanisms
- Angiogenic molecules from the eosinophils recruits the inflammatory cells and increase the vascularity.
- Fibrogenic mediators such as TGF-β1 and matrix metalloproteinase 9 (MMP)-9 causes the airway remodeling.
- MBP and MMP-9 disrupt the integrity of the epithelial cells of the esophagus through their involvement in the smooth muscles, fibroblasts, and cell-adhesion molecules.
- The above-mentioned processes lead to tissue remodeling eventually, causing an overall esophageal dysfunction.
- TGF-β and eosinophilic granule proteins MBP and EPO are the key eosinophil effector proteins. The importance of eosinophils in mediating tissue fibrosis is supported by evidence in both murine and human models.
- These findings not only highlight the importance of targeting fibrosis reversal in the treatment of EoE, but also underline the importance of eosinophils in tissue remodeling.
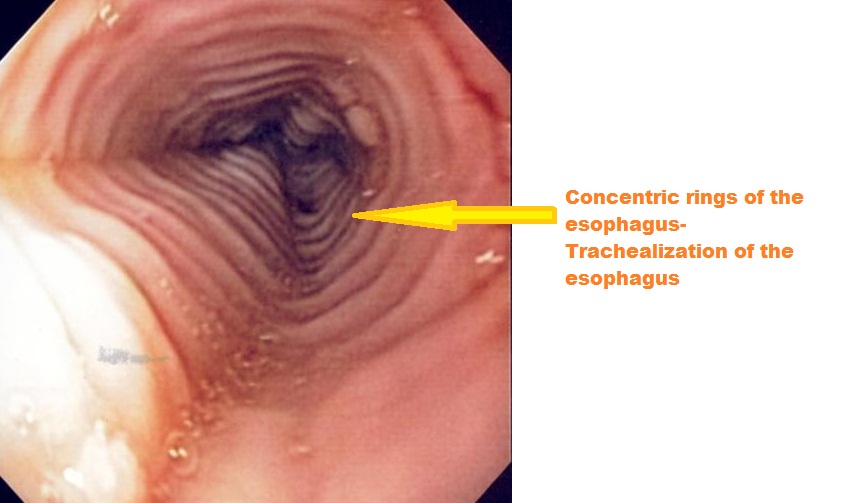
Gross Pathology
- Mucosal biopsies of the esophagus should be obtained in all patients in whom EoE is a clinical possibility regardless of the endoscopic appearance.
- Endoscopic abnormalities in patients with EoE are as follows:[17][18][19][20][21]
- Fixed esophageal ring which is corrugated
- White exudate
- Longitudinal furrows
- Mucosal pallor
- Diffuse esophageal narrowing
- Mucosal fragility leading to esophageal lacerations during the endoscopy
- However, because these endoscopic features have been described in other esophageal disorders, none can be considered pathognomonic for EoE.
-
Endoscopy of the esophagus: Eosinophilic esophagitis
Source: Wikimedia
Histopathology
- Characteristic features are as follows:
- > 20 eosinophils/0.24 mm2.
- Papillae are elongated
- Papillae reach into the top 1/3 of the epithelial layer
- Basal cell hyperplasia; > 3 cells thick or >15% of epithelial thickness
- The most common cause is gastroesophageal reflux disease (GERD). If caused by GERD, the diseases is also called reflux esophagitis.
- Other causes of esophagitis include infections (most commonly candida, herpes simplex and cytomegalovirus). These infections are typically seen in immunocompromised people, such as those with HIV.
- Food allergies have also been known to cause esophagitis
- Chemical injury by alkaline or acid solutions may also cause esophagitis, and is usually seen in children or in adults who attempt suicide.
- Physical injury resulting from radiation therapy or by nasogastric tubes may also be responsible.
Pathological Findings
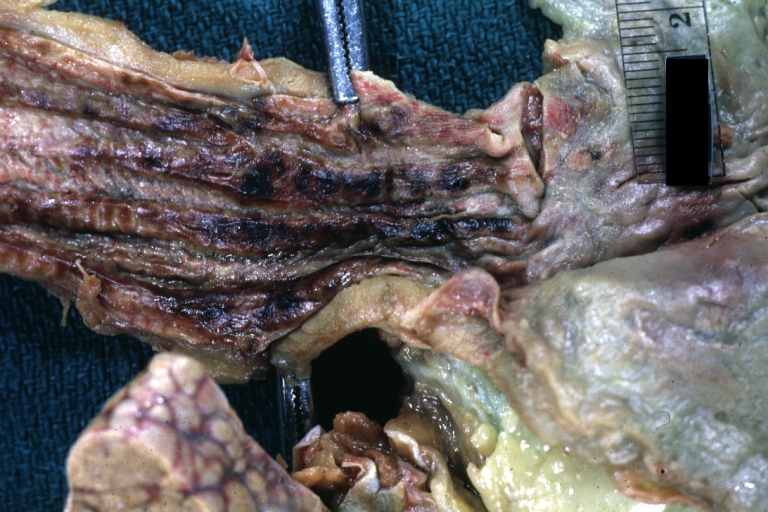
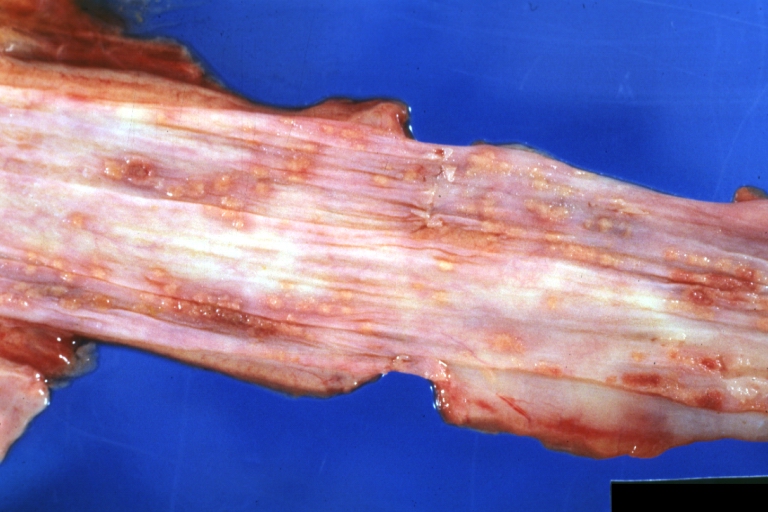
Gross Images
-
Esophagus: Candida: Gross natural color close up of distal esophagus mucosa, an excellent example of candida esophagitis
-
Esophagitis Candida: Gross natural color close-up, an excellent example
-
Esophagitis Candida: Gross natural color excellent close-up photo case of acute myelomonocytic leukemia
-
Necrotizing esophagitis and gastritis, sulfuric acid ingested as suicide attempt
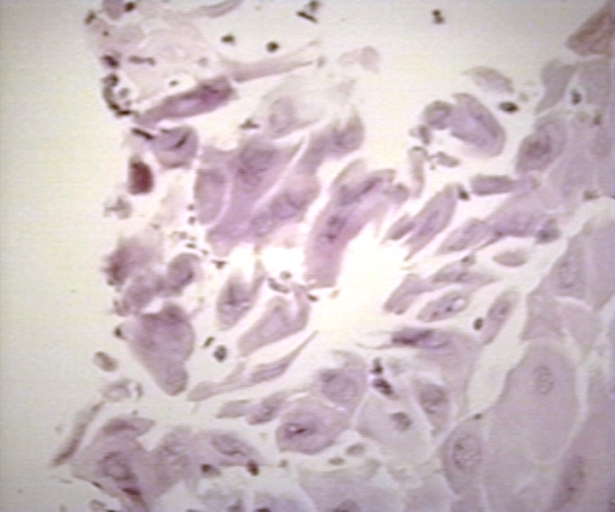
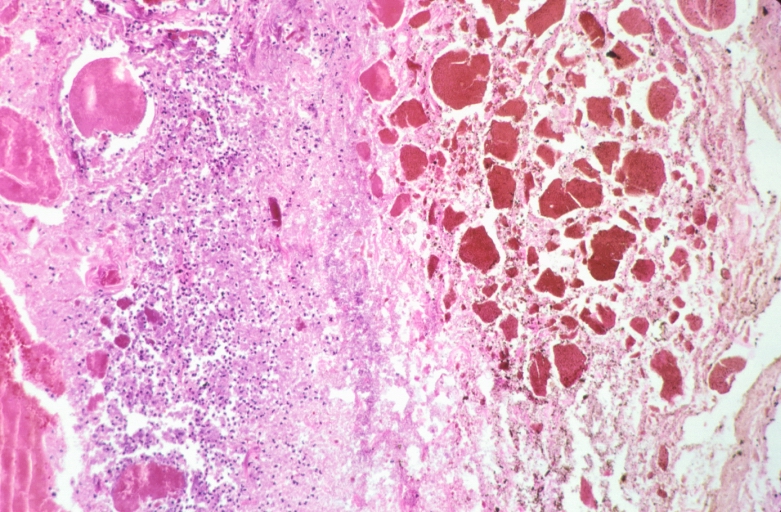
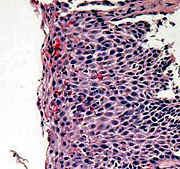
Microscopic Images
-
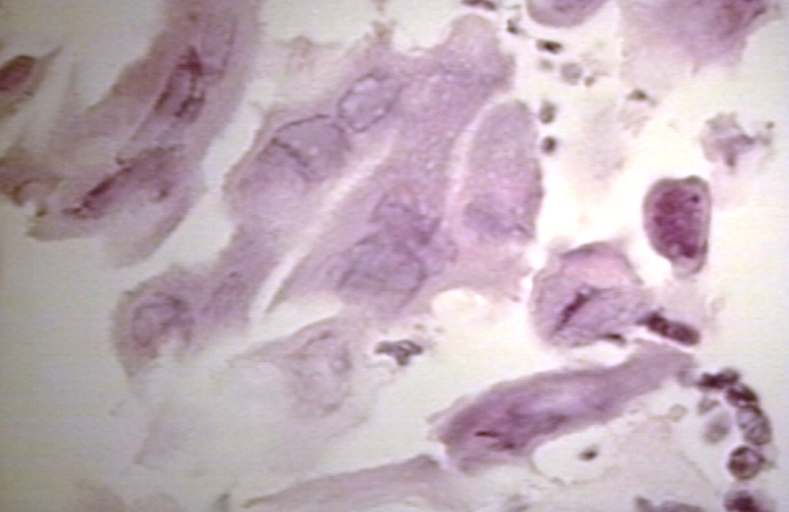
Herpes esophagitis 100 x
-
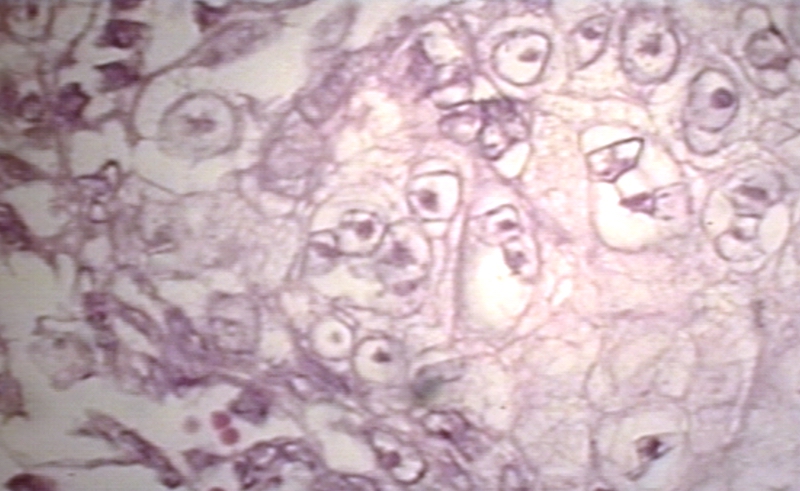
Herpes esophagitis 400 x
-
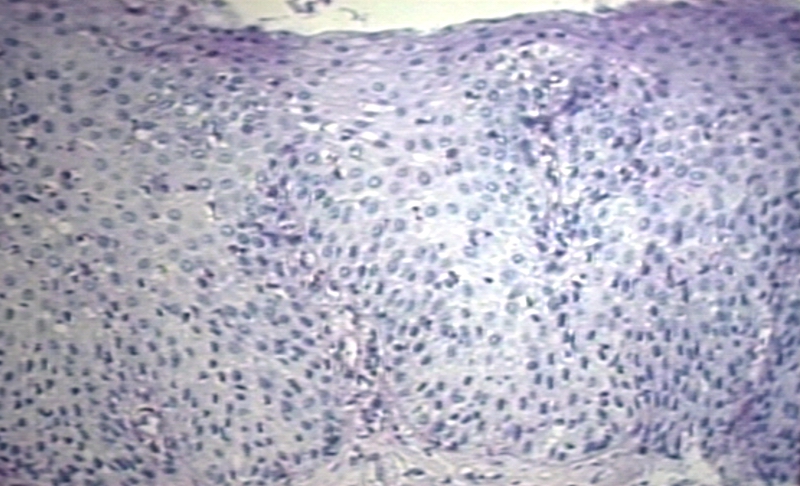
Herpes esophagitis 600 x
-
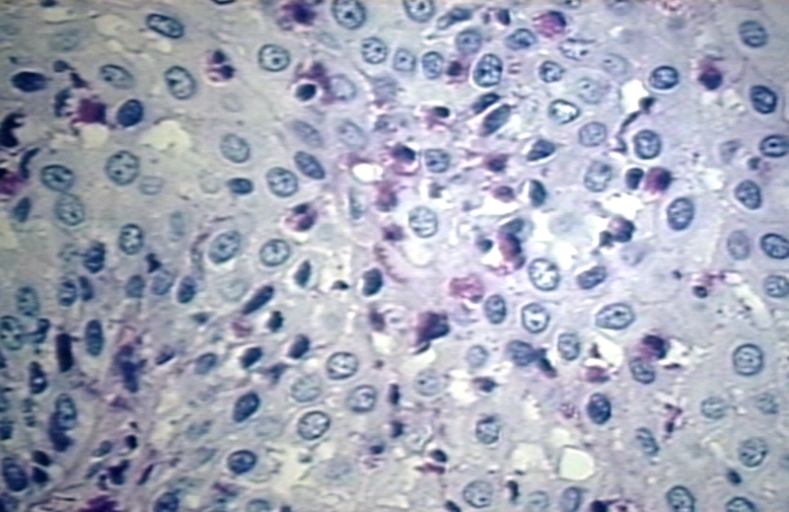
Reflux esophagitis 100 x
-
Reflux esophagitis 400 x
-
Necrotizing esophagitis and gastritis, sulfuric acid ingested as suicide attempt
Histopathological Findings: Herpes Esophagitis
{{#ev:youtube|bJME-CJvHfs}}
References
- ↑ Stein HJ, DeMeester TR (1992). "Outpatient physiologic testing and surgical management of foregut motility disorders". Curr Probl Surg. 29 (7): 413–555. PMID 1606845.
- ↑ Storr M, Meining A, Allescher HD (2000). "Pathophysiology and pharmacological treatment of gastroesophageal reflux disease". Dig Dis. 18 (2): 93–102. doi:10.1159/000016970. PMID 11060472.
- ↑ De Giorgi F, Palmiero M, Esposito I, Mosca F, Cuomo R (2006). "Pathophysiology of gastro-oesophageal reflux disease". Acta Otorhinolaryngol Ital. 26 (5): 241–6. PMC 2639970. PMID 17345925.
- ↑ Fisher BL, Pennathur A, Mutnick JL, Little AG (1999). "Obesity correlates with gastroesophageal reflux". Dig Dis Sci. 44 (11): 2290–4. PMID 10573376.
- ↑ Kahrilas PJ, Shi G, Manka M, Joehl RJ (2000). "Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia". Gastroenterology. 118 (4): 688–95. PMID 10734020.
- ↑ Richter J (1999). "Do we know the cause of reflux disease?". Eur J Gastroenterol Hepatol. 11 Suppl 1: S3–9. PMID 10443906.
- ↑ Malhotra N, Levine J (2014). "Eosinophilic esophagitis: an autoimmune esophageal disorder". Curr Probl Pediatr Adolesc Health Care. 44 (11): 335–40. doi:10.1016/j.cppeds.2014.10.004. PMID 25499460.
- ↑ Martin LJ, Franciosi JP, Collins MH, Abonia JP, Lee JJ, Hommel KA, Varni JW, Grotjan JT, Eby M, He H, Marsolo K, Putnam PE, Garza JM, Kaul A, Wen T, Rothenberg ME (2015). "Pediatric Eosinophilic Esophagitis Symptom Scores (PEESS v2.0) identify histologic and molecular correlates of the key clinical features of disease". J. Allergy Clin. Immunol. 135 (6): 1519–28.e8. doi:10.1016/j.jaci.2015.03.004. PMC 4460579. PMID 26051952.
- ↑ Lucendo AJ, Arias A, Tenias JM (2014). "Relation between eosinophilic esophagitis and oral immunotherapy for food allergy: a systematic review with meta-analysis". Ann. Allergy Asthma Immunol. 113 (6): 624–9. doi:10.1016/j.anai.2014.08.004. PMID 25216976.
- ↑ López-Colombo A (2012). "[Eosinophilic esophagitis]". Rev Gastroenterol Mex (in Spanish; Castilian). 77 Suppl 1: 1–3. doi:10.1016/j.rgmx.2012.07.002. PMID 22939463.
- ↑ Chehade M, Lucendo AJ, Achem SR, Souza RF (2013). "Causes, evaluation, and consequences of eosinophilic esophagitis". Ann. N. Y. Acad. Sci. 1300: 110–8. doi:10.1111/nyas.12243. PMID 24117638.
- ↑ Straumann A (2013). "Eosinophilic esophagitis: a bulk of mysteries". Dig Dis. 31 (1): 6–9. doi:10.1159/000347095. PMID 23797116.
- ↑ Straumann A (2012). "Eosinophilic esophagitis: rapidly emerging disorder". Swiss Med Wkly. 142: w13513. doi:10.4414/smw.2012.13513. PMID 22307811.
- ↑ Schoepfer AM, Simon D, Straumann A (2011). "Eosinophilic oesophagitis: latest intelligence". Clin. Exp. Allergy. 41 (5): 630–9. doi:10.1111/j.1365-2222.2011.03739.x. PMID 21429051.
- ↑ Godat S, Moradpour D, Schoepfer A (2011). "[Eosinophilic esophagitis: update 2011]". Rev Med Suisse (in French). 7 (307): 1678–80, 1682. PMID 21987875.
- ↑ Potter JW, Saeian K, Staff D, Massey BT, Komorowski RA, Shaker R, Hogan WJ (2004). "Eosinophilic esophagitis in adults: an emerging problem with unique esophageal features". Gastrointest. Endosc. 59 (3): 355–61. PMID 14997131.
- ↑ 44</a>)">"Table 3: Proposed classification and grading system for the endoscopic assessment of the esophageal features of eosinophilic esophagitis (<a id=ref-link-section-1 title="" href=/articles/#ref44>44</a>)".
- ↑ "Vertical lines in distal esophageal mucosa (VLEM): a true endoscopic manifestation of esophagitis in children? - PubMed - NCBI".
- ↑ "Fragility of the esophageal mucosa: a pathognomonic endoscopic sign of primary eosinophilic esophagitis? - PubMed - NCBI".
- ↑ "Eosinophilic esophagitis: red on microscopy, white on endoscopy. - PubMed - NCBI".
- ↑ "The prevalence and diagnostic utility of endoscopic features of eosinophilic esophagitis: a meta-analysis. - PubMed - NCBI".