Mast cell

|
WikiDoc Resources for Mast cell |
|
Articles |
|---|
|
Most recent articles on Mast cell |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Mast cell at Clinical Trials.gov Clinical Trials on Mast cell at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Mast cell
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Mast cell Discussion groups on Mast cell Directions to Hospitals Treating Mast cell Risk calculators and risk factors for Mast cell
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Mast cell |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
A mast cell (or mastocyte) is a resident cell of several types of tissues and contains many granules rich in histamine and heparin. Although best known for their role in allergy and anaphylaxis, mast cells play an important protective role as well, being intimately involved in wound healing and defense against pathogens.[1]
Origin and classification
Mast cells were first described by Paul Ehrlich in his 1878 doctoral thesis on the basis of their unique staining characteristics and large granules. These granules also led him to the mistaken belief that they existed to nourish the surrounding tissue, and he named them "mastzellen," a german term, meaning "feeding-cells."[2] Nowadays, they are considered part of the immune system. Mast cells are very similar to basophil granulocytes (a class of white blood cells) in blood; the similarities between mast cells and basophils has led many to speculate that mast cells are basophils that have "homed in" on tissues. However, current evidence suggests that they are generated by different precursor cells in the bone marrow. Nevertheless, both mast cells and basophils are thought to originate from bone marrow precursors expressing the CD34 molecule. The basophil leaves the bone marrow already mature while the mast cell circulates in an immature form, only maturing once in a tissue site. The tissue site an immature mast cell chooses to settle in probably determines its precise characteristics.[1]

Two types of mast cells are recognized, those from connective tissue and a distinct set of mucosal mast cells. The activities of the latter are dependent on T-cells.
Mast cells are present in most tissues in the vicinity of blood vessels, and are especially prominent near the boundaries between the outside world and the internal milieu, such as the skin, mucosa of the lungs and digestive tract, as well as in the mouth, conjunctiva and nose.[1]
Physiology
Mast cells play a key role in the inflammatory process. When activated, a mast cell rapidly releases its characteristic granules and various hormonal mediators into the interstitium. Mast cells can be stimulated to degranulate by direct injury (e.g physical or chemical), cross-linking of IgE receptors, or by activated complement proteins.[1]
Mast cells express a high-affinity receptor (FcεRI) for the Fc region of Immunoglobulin E (IgE), the least-abundant member of the antibodies. This receptor is of such high affinity that binding of IgE molecules is essentially irreversible. As a result, mast cells are coated with IgE. IgE is produced by B-cells (the antibody-producing cells of the immune system). IgE molecules, like all antibodies, are specific to one particular antigen.[1]
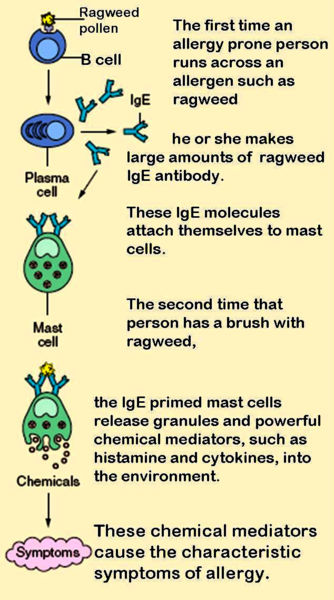
In allergic reactions, mast cells remain inactive until an allergen binds to IgE already in association with the cell (see above). Allergens are generally proteins or polysaccharides. The allergen binds to the Fab part of the IgE molecules on the mast cell surface. It appears that binding of two or more IgE molecules (this is called crosslinking) is required to activate the mast cell; the steric changes lead to a slight disturbance to the cell membrane structure, causing a complex sequence of reactions inside the cell that lead to its activation. Although this reaction is most well understood in terms of allergy, it appears to have evolved as a defense system against intestinal worm infestations (tapeworms, etc).[1]
The molecules thus released into the intercellular environment include:[1]
- preformed mediators (from the granules):
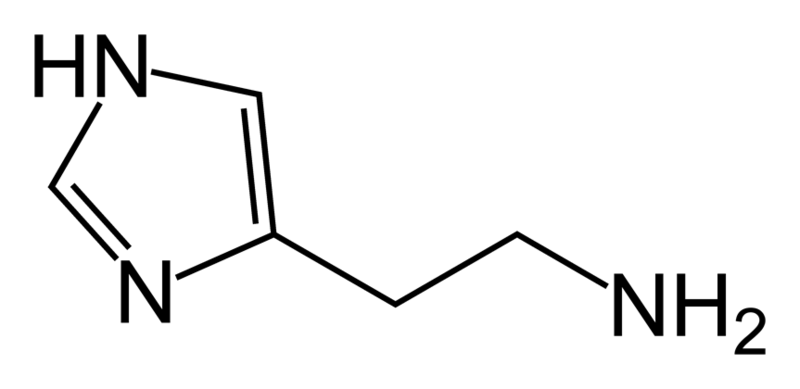
- histamine (2-5 pg/cell)
- proteoglycans, mainly heparin (active as anticoagulant)
- serine proteases
- newly formed lipid mediators (eicosanoids):
- cytokines
Histamine dilates post capillary venules, activates the endothelium, and increases blood vessel permeability. This leads to local edema (swelling), warmth, redness, and the attraction of other inflammatory cells to the site of release. It also irritates nerve endings (leading to itching or pain). Cutaneous signs of histamine release are the "flare and wheal"-reaction. The bump and redness immediately following a mosquito bite are a good example of this reaction, which occurs seconds after challenge of the mast cell by an allergen.[1]
The other physiologic activities of mast cells are much less well-understood. Several lines of evidence suggest that mast cells may have a fairly fundamental role in innate immunity -- they are capable of elaborating a vast array of important cytokines and other inflammatory mediators, they express multiple "pattern recognition receptors" thought to be involved in recognizing broad classes of pathogens, and mice without mast cells seem to be much more susceptible to a variety of infections.
Mast cell granules carry a variety of bioactive chemicals. These granules have been found to be transferred to adjacent cells of the immune system and neurons via transgranulation via their pseudopodia.[3]
Role in disease
Allergic disease
Many forms of cutaneous and mucosal allergy are mediated for a large part by mast cells; they play a central role in asthma, eczema, itch (from various causes) and allergic rhinitis and allergic conjunctivitis. Antihistamine drugs act by blocking the action of histamine on nerve endings. Cromoglicate-based drugs (sodium cromoglicate, nedocromil) block a calcium channel essential for mast cell degranulation, stabilizing the cell and preventing release of histamine and related mediators. Leukotriene antagonists (such as montelukast and zafirlukast) block the action of leukotriene mediators, and are being used increasingly in allergic diseases.[1]
Anaphylaxis
In anaphylaxis (a severe systemic reaction to allergens, such as nuts, bee stings or drugs), body-wide degranulation of mast cells leads to vasodilation and, if severe, symptoms of life-threatening shock.
Autoimmunity
Mast cells are implicated in the pathology associated with the autoimmune disorders rheumatoid arthritis, bullous pemphigoid, and multiple sclerosis. They have been shown to be involved in the recruitment of inflammatory cells to the joints (e.g. rheumatoid arthritis) and skin (e.g. bullous pemphigoid) and this activity is dependent on antibodies and complement components.
Mast cell disorders
Mastocytosis is a rare condition featuring proliferation of mast cells. It exists in a cutaneous and systemic form, with the former being limited to the skin and the latter involving multiple organs.[1] Mast cell tumors are often seen in dogs and cats.[4]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Prussin C, Metcalfe DD (2003). "IgE, mast cells, basophils, and eosinophils". J Allergy Clin Immunol. 111 (2 Suppl): S486–94. PMID 12592295.
- ↑ Ehrlich P. Beiträge zur Theorie und Praxis der histologischen Färbung. Dissertation at Leipzig University, 1878.
- ↑ Wilhelm M, Silver R, Silverman AJ (2005). "Central nervous system neurons acquire mast cell products via transgranulation". Eur J Neurosci. 22 (9): 2238–48. doi:10.1111/j.1460-9568.2005.04429.x. PMID 16262662.
- ↑ "Cutaneous Mast Cell Tumors". The Merck Veterinary Manual. 2006.
External links
- Mast+cells at the US National Library of Medicine Medical Subject Headings (MeSH)
ca:Mastòcit da:Mastcelle de:Mastzelle ko:비만 세포 he:תא פיטום mk:Мастоцит nl:Mestcel fi:Syöttösolu sv:Mastcell sr:мастоцит