Epiglottitis pathophysiology: Difference between revisions
(Created page with "__NOTOC__ {{Epiglottitis}} Please help WikiDoc by adding content here. It's easy! Click here to learn about editing. ==References== {{Reflist|...") |
m (Bot: Removing from Primary care) |
||
| (57 intermediate revisions by 5 users not shown) | |||
| Line 2: | Line 2: | ||
{{Epiglottitis}} | {{Epiglottitis}} | ||
{{CMG}} {{AE}} {{PTD}} | |||
==Overview== | |||
Understading the pathogenesis of [[epiglottitis]] involves a good knowlegde of the causative organisms. | |||
The only known reservoirs for [[H. influenzae]] in humans include, [[respiratory tract]], [[conjunctival]] and genital surfaces.<ref name="pmid18622812" /> [[Pathogenicity]] of H. [[influenza]] is as a result of imbalance between the [[virulent]] factors of the organism and the host [[immune system]]. This [[immunity]] is enhanced when children are vaccinated with the purified polyribosylribitol phosphate (PRP). [[H. influenzae type B|H. influenza]] type b capsule is [[antiphagocytic]]. Serum anit-purified polyribosylribitol phosphate (anti-PRP) [[antibody]] is important in the [[complement]] dependent [[phagocytosis]] and lyses of the [[bacteria]]. <ref name="abc" /> [[IgA]] [[antibody]] accords the [[mucosa]] surface protection again attachment of the [[organism]]. The strategies deployed by a [[microbe]] to assist its survival and [[proliferation]], may or may not lead to disease process. [[Epiglottitis]] caused by [[H. influenzae|H. influenza]] may therefore be considered as an accidental consequence of the microbial factors that permit its survival.<ref name="pmid18622813" /> Acute [[epiglottitis]] [[pathogenesis]] is well exemplified by [[H. influenzae type B|H. influenza]]<nowiki/>e, with the ability to colonize [[mucosal]] surfaces and to spread contiguously or invade [[epithelial]] cells. It commonly disseminates within the [[bloodstream]], or localizes to selected [[tissues]] among these is the [[epiglottis]]. [[Microbial]] [[invasion]] of the [[bloodstream]] around the [[epiglottis]] leads to [[inflammatory]] response and tissue [[edema]] most apparent at the [[lingual]] surface of the [[epiglottis]] compared with the [[laryngeal]] surface. The [[extravasation]] of fluid leads to remarkable tissue [[swelling]] that may lead to [[respiratory]] obstruction and the other symptoms of [[epiglottitis]].<ref name="pmid22113103" /> The pathogenesis of [[necrotizing]] [[epiglottitis]] involves the infection with [[Cytomegalovirus|CMV]] or [[Epstein Barr virus|EBV]] usually in [[immunocompromised]] people. Affected patients are usually [[neutropenic]] and lymphopenic at presentation. [[Cytomegalovirus|CMV]] and [[Epstein Barr virus|EBV]] modulate the host's [[immune]] defense facilitating [[immune]] evasion and thereby predisposing the patient to superimposed infections. | |||
The causative organism of [[necrotizing]] epiglottitis is unclear.<ref name="pmid19106777" /> | |||
==Pathophysiology== | |||
===Pathogenesis=== | |||
====Infectious epiglottitis==== | |||
Infectious epiglottitis is a soft tissue swelling of epiglottis,<ref name="pmid20513048">{{cite journal| author=Shah RK, Stocks C| title=Epiglottitis in the United States: national trends, variances, prognosis, and management. | journal=Laryngoscope | year= 2010 | volume= 120 | issue= 6 | pages= 1256-62 | pmid=20513048 | doi=10.1002/lary.20921 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20513048 }}</ref> and the surrounding structures example; plica aryepiglottica, [[arytenoids]], sinus [[piriformis]] and [[Vestibular fold|vestibular]] folds.<ref name="pmid6967138">{{cite journal| author=Ossoff RH, Wolff AP, Ballenger JJ| title=Acute epiglottitis in adults: experience with fifteen cases. | journal=Laryngoscope | year= 1980 | volume= 90 | issue= 7 Pt 1 | pages= 1155-61 | pmid=6967138 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6967138 }}</ref> | |||
Understading the pathogenesis of [[epiglottitis]] involves a good knowlegde of the causative organisms. | |||
The only known reservoirs for [[H. influenzae]] in humans include:<ref name="pmid18622812">{{cite journal| author=Moxon ER, Wilson R| title=The role of Haemophilus influenzae in the pathogenesis of pneumonia. | journal=Rev Infect Dis | year= 1991 | volume= 13 Suppl 6 | issue= | pages= S518-27 | pmid=1862281 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1862281 }}</ref> | |||
*[[Respiratory]] tract | |||
*[[Conjunctival]] | |||
*Genital surfaces. | |||
Healthy people are normal carriers of the organism. [[Pathogenicity]] of H. [[influenza]] is as a result of imbalance between the [[virulent]] factors of the organism and the host immune system. | |||
This immunity is enhanced when children are vaccinated with the purified polyribosylribitol phosphate (PRP). H. influenza type b capsule is antiphagocytic. Serum anit-purified polyribosylribitol phosphate (anti-PRP) antibody is important in the [[complement]] dependent [[phagocytosis]] and lyses of the bacteria.<Ref name= abc > Robbins JBH. influenza type b disease and immunity in humans, Ann intern medicine78:259, 1973</ref> IgA antibody accords the mucosa surface protection again attachement of the organism. | |||
The strategies deployed by a microbe to assist its survival and proliferation, may or may not lead to disease process. Epiglottitis caused by [[H. influenzae|H. influenza]] may therefore be considered as an accidental consequence of the microbial factors that permit its survival.<ref name="pmid18622813">{{cite journal| author=Moxon ER, Wilson R| title=The role of Haemophilus influenzae in the pathogenesis of pneumonia. | journal=Rev Infect Dis | year= 1991 | volume= 13 Suppl 6 | issue= | pages= S518-27 | pmid=1862281 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1862281 }}</ref> | |||
Acute epiglottis pathogenesis is well exemplified by [[H. influenzae type B|H. influenza]]<nowiki/>e, with the ability to colonize mucosal surfaces and to spread contiguously or invade epithelial cells, to disseminate within the bloodstream, and to localize to selected tissues among these is the epiglottis. The [[H. influenzae|H. influenza]] like other infectious agents cause epiglottis mostly via invasion of the bloodstream by the help of its [[virulence factors]]. These include:<ref name="pmid1862281">{{cite journal| author=Moxon ER, Wilson R| title=The role of Haemophilus influenzae in the pathogenesis of pneumonia. | journal=Rev Infect Dis | year= 1991 | volume= 13 Suppl 6 | issue= | pages= S518-27 | pmid=1862281 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1862281 }}</ref> | |||
*Capsular [[Polysaccharide encapsulated bacteria|polysaccharide]] | |||
*[[Lipopolysaccharide]] | |||
*Outer-membrane proteins | |||
*[[Pilus]] proteins | |||
*IgA proteases | |||
*[[Histamine]] | |||
*Factors affecting cilial | |||
The tissues surrounding the epiglottis have rich blood and [[lymphatic]] supply. Microbial invasion of the [[bloodstream]] around the [[epiglottis]] lead to [[inflammatory]] response and tissue edema most apparent at the [[lingual]] surface of the [[epiglottis]] compared to the [[laryngeal]] surface. The [[extravasation]] of fluid leads to remarkable tissue swelling that may lead to respiratory obstruction and the other symptoms of [[epiglottitis]].<ref name="pmid22113103">{{cite journal| author=Sato S, Kuratomi Y, Inokuchi A| title=Pathological characteristics of the epiglottis relevant to acute epiglottitis. | journal=Auris Nasus Larynx | year= 2012 | volume= 39 | issue= 5 | pages= 507-11 | pmid=22113103 | doi=10.1016/j.anl.2011.10.015 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22113103 }}</ref> | |||
====Necrotizing epiglotitis==== | |||
The pathogenesis of [[necrotizing]] epiglottitis involves the infection with [[Cytomegalovirus|CMV]] or [[Epstein Barr virus|EBV]] usually in [[immunocompromised]] people. Affected patients are usually [[neutropenic]] and lymphopenic at presentation. [[Cytomegalovirus|CMV]] and [[Epstein Barr virus|EBV]] modulate the host's immune defense facilitating immune evasion and thereby predisposing the patient to a superimposed infections. | |||
The causative organism of [[necrotizing]] epiglottitis is unclear.<ref name="pmid19106777">{{cite journal| author=Tebruegge M, Connell T, Kong K, Marks M, Curtis N| title=Necrotizing epiglottitis in an infant: an unusual first presentation of human immunodeficiency virus infection. | journal=Pediatr Infect Dis J | year= 2009 | volume= 28 | issue= 2 | pages= 164-6 | pmid=19106777 | doi=10.1097/INF.0b013e318187a869 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19106777 }} </ref> | |||
===Gross pathology=== | |||
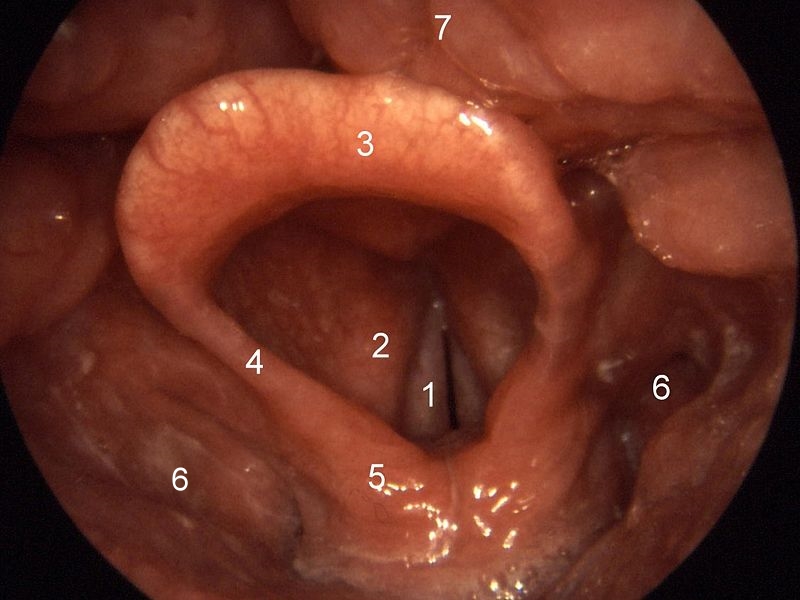
On gross pathology the epiglottis and the surrounding structures appear erythematous and swollen as shown below.<ref name="pmid24052580">{{cite journal| author=Charles R, Fadden M, Brook J| title=Acute epiglottitis. | journal=BMJ | year= 2013 | volume= 347 | issue= | pages= f5235 | pmid=24052580 | doi=10.1136/bmj.f5235 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24052580 }} </ref><ref name="pmid7497775">{{cite journal| author=Mayo-Smith MF, Spinale JW, Donskey CJ, Yukawa M, Li RH, Schiffman FJ| title=Acute epiglottitis. An 18-year experience in Rhode Island. | journal=Chest | year= 1995 | volume= 108 | issue= 6 | pages= 1640-7 | pmid=7497775 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7497775 }}</ref><ref name="pmid6967138">{{cite journal| author=Ossoff RH, Wolff AP, Ballenger JJ| title=Acute epiglottitis in adults: experience with fifteen cases. | journal=Laryngoscope | year= 1980 | volume= 90 | issue= 7 Pt 1 | pages= 1155-61 | pmid=6967138 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6967138 }}</ref> | |||
[[Image:Epiglottis.jpg|thumb|left|400px|1-True vocal cords, 2-False vocal cords, 3-Epiglottis, | |||
4-Plica aryepiglottica, 5-Arytenoids, 6-Pyriform sinuses, | |||
7-Base of tongue - Von I, Welleschik, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=2468726]] <br style="clear:left;" /> | |||
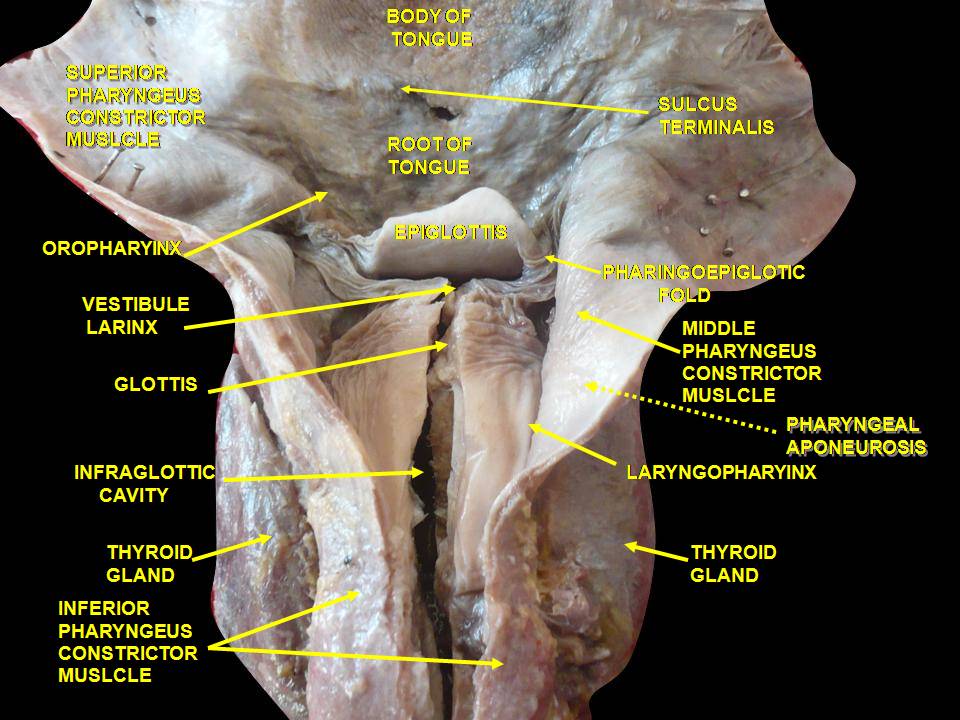
The dissected anatomy of the epiglottis is shown below: <ref name= abdw> https://commons.wikimedia.org/wiki/File:Slide1kuku.JPG </ref> | |||
[[Image:Slide1kuku.JPG|500px|thumb|center|By Anatomist90 - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=25667785]] | |||
===Microscopic pathology=== | |||
The potential space between the [[mucosal]] [[epithelium]] of the [[epiglottis]] and the [[Epiglottic cartilage|epiglottic]] cartilage consists of adipose tissue, fibrous tissue and glands. This space becomes occupied with extravasated fluid resulting from the [[inflammatory]] process. Nuetrophilic [[chemotaxis]] as well as other [[inflammatory]] molecules are responsible for the tissue response to the [[infectious]] agents. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | [[Category:Emergency medicine]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | |||
[[Category:Pediatrics]] | |||
[[Category:Pulmonology]] | [[Category:Pulmonology]] | ||
Latest revision as of 21:36, 29 July 2020
|
Epiglottitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Epiglottitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Epiglottitis pathophysiology |
|
Risk calculators and risk factors for Epiglottitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Prince Tano Djan, BSc, MBChB [2]
Overview
Understading the pathogenesis of epiglottitis involves a good knowlegde of the causative organisms. The only known reservoirs for H. influenzae in humans include, respiratory tract, conjunctival and genital surfaces.[1] Pathogenicity of H. influenza is as a result of imbalance between the virulent factors of the organism and the host immune system. This immunity is enhanced when children are vaccinated with the purified polyribosylribitol phosphate (PRP). H. influenza type b capsule is antiphagocytic. Serum anit-purified polyribosylribitol phosphate (anti-PRP) antibody is important in the complement dependent phagocytosis and lyses of the bacteria. [2] IgA antibody accords the mucosa surface protection again attachment of the organism. The strategies deployed by a microbe to assist its survival and proliferation, may or may not lead to disease process. Epiglottitis caused by H. influenza may therefore be considered as an accidental consequence of the microbial factors that permit its survival.[3] Acute epiglottitis pathogenesis is well exemplified by H. influenzae, with the ability to colonize mucosal surfaces and to spread contiguously or invade epithelial cells. It commonly disseminates within the bloodstream, or localizes to selected tissues among these is the epiglottis. Microbial invasion of the bloodstream around the epiglottis leads to inflammatory response and tissue edema most apparent at the lingual surface of the epiglottis compared with the laryngeal surface. The extravasation of fluid leads to remarkable tissue swelling that may lead to respiratory obstruction and the other symptoms of epiglottitis.[4] The pathogenesis of necrotizing epiglottitis involves the infection with CMV or EBV usually in immunocompromised people. Affected patients are usually neutropenic and lymphopenic at presentation. CMV and EBV modulate the host's immune defense facilitating immune evasion and thereby predisposing the patient to superimposed infections. The causative organism of necrotizing epiglottitis is unclear.[5]
Pathophysiology
Pathogenesis
Infectious epiglottitis
Infectious epiglottitis is a soft tissue swelling of epiglottis,[6] and the surrounding structures example; plica aryepiglottica, arytenoids, sinus piriformis and vestibular folds.[7] Understading the pathogenesis of epiglottitis involves a good knowlegde of the causative organisms. The only known reservoirs for H. influenzae in humans include:[1]
- Respiratory tract
- Conjunctival
- Genital surfaces.
Healthy people are normal carriers of the organism. Pathogenicity of H. influenza is as a result of imbalance between the virulent factors of the organism and the host immune system.
This immunity is enhanced when children are vaccinated with the purified polyribosylribitol phosphate (PRP). H. influenza type b capsule is antiphagocytic. Serum anit-purified polyribosylribitol phosphate (anti-PRP) antibody is important in the complement dependent phagocytosis and lyses of the bacteria.[2] IgA antibody accords the mucosa surface protection again attachement of the organism.
The strategies deployed by a microbe to assist its survival and proliferation, may or may not lead to disease process. Epiglottitis caused by H. influenza may therefore be considered as an accidental consequence of the microbial factors that permit its survival.[3]
Acute epiglottis pathogenesis is well exemplified by H. influenzae, with the ability to colonize mucosal surfaces and to spread contiguously or invade epithelial cells, to disseminate within the bloodstream, and to localize to selected tissues among these is the epiglottis. The H. influenza like other infectious agents cause epiglottis mostly via invasion of the bloodstream by the help of its virulence factors. These include:[8]
- Capsular polysaccharide
- Lipopolysaccharide
- Outer-membrane proteins
- Pilus proteins
- IgA proteases
- Histamine
- Factors affecting cilial
The tissues surrounding the epiglottis have rich blood and lymphatic supply. Microbial invasion of the bloodstream around the epiglottis lead to inflammatory response and tissue edema most apparent at the lingual surface of the epiglottis compared to the laryngeal surface. The extravasation of fluid leads to remarkable tissue swelling that may lead to respiratory obstruction and the other symptoms of epiglottitis.[4]
Necrotizing epiglotitis
The pathogenesis of necrotizing epiglottitis involves the infection with CMV or EBV usually in immunocompromised people. Affected patients are usually neutropenic and lymphopenic at presentation. CMV and EBV modulate the host's immune defense facilitating immune evasion and thereby predisposing the patient to a superimposed infections. The causative organism of necrotizing epiglottitis is unclear.[5]
Gross pathology
On gross pathology the epiglottis and the surrounding structures appear erythematous and swollen as shown below.[9][10][7]
The dissected anatomy of the epiglottis is shown below: [11]
Microscopic pathology
The potential space between the mucosal epithelium of the epiglottis and the epiglottic cartilage consists of adipose tissue, fibrous tissue and glands. This space becomes occupied with extravasated fluid resulting from the inflammatory process. Nuetrophilic chemotaxis as well as other inflammatory molecules are responsible for the tissue response to the infectious agents.
References
- ↑ 1.0 1.1 Moxon ER, Wilson R (1991). "The role of Haemophilus influenzae in the pathogenesis of pneumonia". Rev Infect Dis. 13 Suppl 6: S518–27. PMID 1862281.
- ↑ 2.0 2.1 Robbins JBH. influenza type b disease and immunity in humans, Ann intern medicine78:259, 1973
- ↑ 3.0 3.1 Moxon ER, Wilson R (1991). "The role of Haemophilus influenzae in the pathogenesis of pneumonia". Rev Infect Dis. 13 Suppl 6: S518–27. PMID 1862281.
- ↑ 4.0 4.1 Sato S, Kuratomi Y, Inokuchi A (2012). "Pathological characteristics of the epiglottis relevant to acute epiglottitis". Auris Nasus Larynx. 39 (5): 507–11. doi:10.1016/j.anl.2011.10.015. PMID 22113103.
- ↑ 5.0 5.1 Tebruegge M, Connell T, Kong K, Marks M, Curtis N (2009). "Necrotizing epiglottitis in an infant: an unusual first presentation of human immunodeficiency virus infection". Pediatr Infect Dis J. 28 (2): 164–6. doi:10.1097/INF.0b013e318187a869. PMID 19106777.
- ↑ Shah RK, Stocks C (2010). "Epiglottitis in the United States: national trends, variances, prognosis, and management". Laryngoscope. 120 (6): 1256–62. doi:10.1002/lary.20921. PMID 20513048.
- ↑ 7.0 7.1 Ossoff RH, Wolff AP, Ballenger JJ (1980). "Acute epiglottitis in adults: experience with fifteen cases". Laryngoscope. 90 (7 Pt 1): 1155–61. PMID 6967138.
- ↑ Moxon ER, Wilson R (1991). "The role of Haemophilus influenzae in the pathogenesis of pneumonia". Rev Infect Dis. 13 Suppl 6: S518–27. PMID 1862281.
- ↑ Charles R, Fadden M, Brook J (2013). "Acute epiglottitis". BMJ. 347: f5235. doi:10.1136/bmj.f5235. PMID 24052580.
- ↑ Mayo-Smith MF, Spinale JW, Donskey CJ, Yukawa M, Li RH, Schiffman FJ (1995). "Acute epiglottitis. An 18-year experience in Rhode Island". Chest. 108 (6): 1640–7. PMID 7497775.
- ↑ https://commons.wikimedia.org/wiki/File:Slide1kuku.JPG