Dermatophytosis pathophysiology
|
Dermatophytosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dermatophytosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Dermatophytosis pathophysiology |
|
Risk calculators and risk factors for Dermatophytosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [2]
Overview
Dermatophytes mode of transmission is direct (or)indirect contact with skin (or) scalp lesions of infected people,animals (or) fomites. Following transmission, the dermatophytes use proteases to adhere to the stratum corneum of the skin. Penetration by dermatophytes is achieved by secreting multiple serine-subtilisins and metallo-endoproteases (fungalysins) formerly called keratinases that are found only in the dermatophytes. Acutely, the host responds to fungal invasion by Type IV delayed type hypersensitivity reaction (also known as "Trichophytin reaction") leading to a cell mediated response. Fungus secreted proteases are one of the most important virulence factors of dermatophytes and are thought to be responsible for evasion from host defense mechanisms. Secreted subtilisin proteases expressed in the dermatophytes could play a role in keratin degradation. Dermatophyte infections of the skin surface (tinea corporis and tinea faciei) mostly present as erythematous, scaly papules that gradually progress to annular or circular red patches or plaques, with central clearing and scaling at the periphery. On microscopic examination of the skin, there may be neutrophils retained in the stratum corneum, parakeratosis, spongiosis and dermal edema.
Pathophysiology
- Dermatophytes survive on the outer layer of skin called stratum corneum.
- Stratum corneum has been known to be not only source of nutrition for the dermatophytes, but also the growing fungal mycelia.[1]
Pathogenesis
After the inoculation in the host skin, suitable conditions favor the infection to progress through the following stages:
Adherence
- Dermatophyte-secreted proteases not only mediate adherence to the host skin but also help in germination of arthroconidia and hyphal growth leading to growth of the fungi in multiple directions.[2][3]
- Fungal arthroconidia attach to keratinocytes via long and sparse microprojections (fibrils).[3]
Penetration
- Penetration by dermatophytes is achieved by secreting multiple serine-subtilisins and metallo-endoproteases (fungalysins) formerly called keratinases that are found only in the dermatophytes.[4]
- Fungal mannans in the dermatophyte cell wall have immunosupressive ability and inhibit the action of T cells. T. rubrum cell wall mannans (TRM) may lead to inhibition of lymphoproliferative response of mononuclear leukocytes. This leads to fungal growth and proliferation on the host skin.
Host response
- Fungal metabolic products diffuse through the stratum basale and stratum spinosum to cause erythema, vesicle or even pustule formation and pruritus.
- Acutely, the host responds to fungal invasion by Type IV delayed type hypersensitivity reaction (also known as "Trichophytin" reaction) leading to a cell mediated response.[5]
- Interferon-α secretion from type 1 T-helper lymphocytes, cytokines like interferon-γ (IFN-γ), IL-8 and macrophages are the effector mechanisms involved in defense against dermatophytes acutely.[6]
- Dermatophyte species have cell wall carbohydrate molecules (β-glucan) that are recognized by the innate immune mechanisms, such as Dectin-1 and Dectin-2, which consequently stimulate toll-like receptor 2 and 4 (TLR-2 and TLR-4). Dectin-1 augments the production of tumor necrosis factor-α and IL-17, IL-6, and IL-10, all of which activate the adaptive immunity.
- IL-8 mediated chemotaxis allows polymorphonuclear leukocytes adhere to opsonized and unopsonized hyphae to inhibit growth of the dermatophyte.[4]
- The dermatophyte antigen is thought to be processed by epidermal Langerhans cells and presented in local lymph nodes to T lymphocytes which proliferate, migrate to the infected site, and produce inflammation.[7]
- The immune response, and especially the level of inflammation, is different for various dermatophyte species, the host species and the pathophysiological status of the host. In general, the zoophilic species cause more inflammatory infections, which may heal spontaneously and result in relative resistance to re-infection. The anthropophilic species usually cause more chronic, less circumscribed infections, which consequently lead to a poor resistance to re-infection.
- Cell-associated as well as secreted factors contribute to the dermatophyte's ability to exaggerate or suppress an inflammatory response.
- Many host factors for example, number and activity of sebaceous glands (due to inhibitory effect of sebum on dermatophytes) in a particular body region, breaks in the integrity of skin barrier, moisturized and macerated skin can promote invasion of dermatophytes.
- Fungus secreted proteases are one of the most important virulence factors of dermatophytes and are thought to be responsible for evasion from host defense mechanisms.[7]
Genetics
- The genomes of the dermatophytes are similar in size, ranging from 22.5 Mb for T. rubrum to 24.1 Mb for T. equinum.
- The LysM domains are implicated in evasion of the host innate immune response (14) by securing fragments of chitin, so that the chitin cannot stimulate the immune response.[8]
- Secreted subtilisin proteases expressed in the dermatophytes could play a role in keratin degradation.[9]
- Dermatophytes have a large number of genes connected to secondary-metabolite production.
- Genes for protein kinases activate mitogen-activated protein kinase (MAPK) pathways and produce cytokines.
- T. equinum infection of epidermal tissue increase the expression of other human genes associated with inflammation, including the tissue remodeling matrix metalloprotease, its regulatory gene Timp1, and the proinflammatory mediator gene COX2.[10]
Gross Pathology
- Dermatophyte infections of the skin surface (tinea corporis and tinea faciei) mostly present as erythematous, scaly papules that gradually progress to annular or circular red patches or plaques, with central clearing and scaling at the periphery.[11]
- Pustules, vesicles, or large blisters may be infrequently seen grossly.
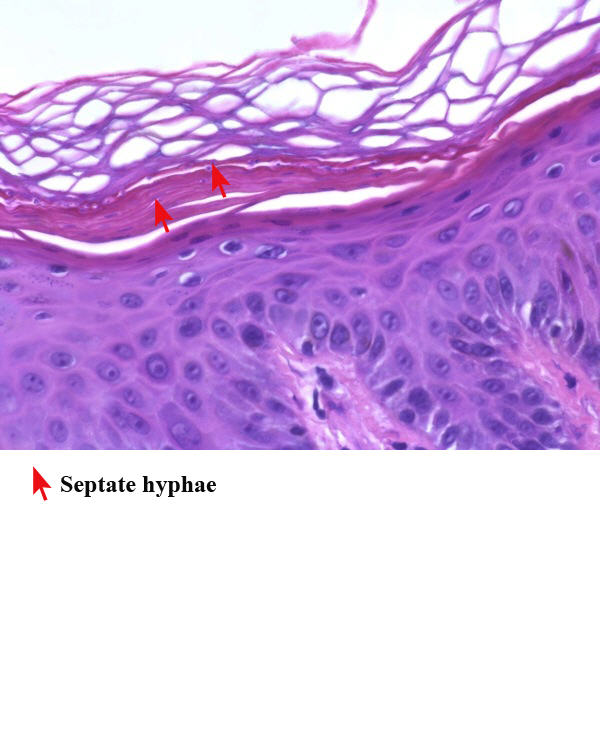
Microscopic Pathology
The following features may be seen on microscopic examination of the skin in dermatophytosis:[12]
- Parakeratosis
- Spongiosis
- Neutrophils in the stratum corneum
- Compact orthokeratosis
- Papillary dermal edema
- Fungal hyphae between 2 zones of cornified cells (called the 'sandwich' sign)
References
- ↑ Samdani AJ (2005). "Dermatophyte growth and degradation of human stratum corneum in vitro (pathogenesis of dermatophytosis)". J Ayub Med Coll Abbottabad. 17 (4): 19–21. PMID 16599028.
- ↑ Aljabre SH, Richardson MD, Scott EM, Rashid A, Shankland GS (1993). "Adherence of arthroconidia and germlings of anthropophilic and zoophilic varieties of Trichophyton mentagrophytes to human corneocytes as an early event in the pathogenesis of dermatophytosis". Clin. Exp. Dermatol. 18 (3): 231–5. PMID 8348716.
- ↑ 3.0 3.1 Vermout S, Tabart J, Baldo A, Mathy A, Losson B, Mignon B (2008). "Pathogenesis of dermatophytosis". Mycopathologia. 166 (5–6): 267–75. doi:10.1007/s11046-008-9104-5. PMID 18478361.
- ↑ 4.0 4.1 Dahl MV (1994). "Dermatophytosis and the immune response". J. Am. Acad. Dermatol. 31 (3 Pt 2): S34–41. PMID 8077506.
- ↑ Almeida SR (2008). "Immunology of dermatophytosis". Mycopathologia. 166 (5–6): 277–83. doi:10.1007/s11046-008-9103-6. PMID 18478362.
- ↑ Brasch J (2009). "Current knowledge of host response in human tinea". Mycoses. 52 (4): 304–12. doi:10.1111/j.1439-0507.2008.01667.x. PMID 19207841.
- ↑ 7.0 7.1 Tainwala R, Sharma Y (2011). "Pathogenesis of dermatophytoses". Indian J Dermatol. 56 (3): 259–61. doi:10.4103/0019-5154.82476. PMC 3132899. PMID 21772583.
- ↑ de Jonge R, Thomma BP (2009). "Fungal LysM effectors: extinguishers of host immunity?". Trends Microbiol. 17 (4): 151–7. doi:10.1016/j.tim.2009.01.002. PMID 19299132.
- ↑ Burmester A, Shelest E, Glöckner G, Heddergott C, Schindler S, Staib P, Heidel A, Felder M, Petzold A, Szafranski K, Feuermann M, Pedruzzi I, Priebe S, Groth M, Winkler R, Li W, Kniemeyer O, Schroeckh V, Hertweck C, Hube B, White TC, Platzer M, Guthke R, Heitman J, Wöstemeyer J, Zipfel PF, Monod M, Brakhage AA (2011). "Comparative and functional genomics provide insights into the pathogenicity of dermatophytic fungi". Genome Biol. 12 (1): R7. doi:10.1186/gb-2011-12-1-r7. PMC 3091305. PMID 21247460.
- ↑ Martinez DA, Oliver BG, Gräser Y, Goldberg JM, Li W, Martinez-Rossi NM, Monod M, Shelest E, Barton RC, Birch E, Brakhage AA, Chen Z, Gurr SJ, Heiman D, Heitman J, Kosti I, Rossi A, Saif S, Samalova M, Saunders CW, Shea T, Summerbell RC, Xu J, Young S, Zeng Q, Birren BW, Cuomo CA, White TC (2012). "Comparative genome analysis of Trichophyton rubrum and related dermatophytes reveals candidate genes involved in infection". MBio. 3 (5): e00259–12. doi:10.1128/mBio.00259-12. PMC 3445971. PMID 22951933.
- ↑ Stein DH (1998). "Tineas--superficial dermatophyte infections". Pediatr Rev. 19 (11): 368–72. PMID 9805462.
- ↑ Stein DH (1998). "Tineas--superficial dermatophyte infections". Pediatr Rev. 19 (11): 368–72. PMID 9805462.
