Congestive heart failure pathophysiology: Difference between revisions
| Line 20: | Line 20: | ||
* In heart failure, there is a failure of blood to move forward (forward failure) and a tendency of blood to move back ward (backward failure). | * In heart failure, there is a failure of blood to move forward (forward failure) and a tendency of blood to move back ward (backward failure). | ||
* Normally, with respect to the left side of the heart, blood flows from the lungs, into the [[pulmonary veins]], into the [[left atrium]], through the [[mitral valve]], and finally into the [[left ventricle]]. When the [[left ventricle]] cannot be normally filled during diastole, blood will back up into the [[left atrium]] and, eventually, into the lungs. The result is a higher than normal pressure of blood within the vessels of the lung. As a result of hydrostatic forces, this high pressure leads to leaking of fluid (i.e. [[transudate]]) from the lung's blood vessels into the air-spaces ([[alveoli]]) of the lungs. The result is [[pulmonary edema]], a condition characterized by difficulty breathing, inadequate [[oxygenation]] of blood, and, if severe and untreated, death. | * Normally, with respect to the left side of the heart, blood flows from the lungs, into the [[pulmonary veins]], into the [[left atrium]], through the [[mitral valve]], and finally into the [[left ventricle]]. When the [[left ventricle]] cannot be normally filled during diastole, blood will back up into the [[left atrium]] and, eventually, into the lungs. The result is a higher than normal pressure of blood within the vessels of the lung. As a result of hydrostatic forces, this high pressure leads to leaking of fluid (i.e. [[transudate]]) from the lung's blood vessels into the air-spaces ([[alveoli]]) of the lungs. The result is [[pulmonary edema]], a condition characterized by difficulty breathing, inadequate [[oxygenation]] of blood, and, if severe and untreated, death. | ||
===Compensatory Mechanisms=== | |||
*Left ventricular systolic dysfunction is associated with a reduction in [[stroke volume]], the amount of blood the heart ejects with each heart beat. | *Left ventricular systolic dysfunction is associated with a reduction in [[stroke volume]], the amount of blood the heart ejects with each heart beat. | ||
* The reduction in [[stroke volume]] leads to a reduction in [[cardiac output]] which is the [[stroke volume]] multiplied by the [[heart rate]]. | * The reduction in [[stroke volume]] leads to a reduction in [[cardiac output]] which is the [[stroke volume]] multiplied by the [[heart rate]]. | ||
| Line 27: | Line 28: | ||
*Dilation of the left ventricle increases volume and increases contractility up to a point (see [[Frank-Starling law of the heart]]). As further LV dilation occurs, however, contractility drops, and functional [[mitral regurgitation]] ([[MR]]) may develop despite an anatomically normal [[mitral valve]]. | *Dilation of the left ventricle increases volume and increases contractility up to a point (see [[Frank-Starling law of the heart]]). As further LV dilation occurs, however, contractility drops, and functional [[mitral regurgitation]] ([[MR]]) may develop despite an anatomically normal [[mitral valve]]. | ||
* Left ventricular enlargement and lack of forward cardiac output can lead to [[left atrial enlargement]]. [[Left atrial dilation]] may lead to [[atrial fibrillation]] which occurs in 20% of patients with [[congestive heart failure]]. Atrial fibrillation diminishes left ventricular filling through the loss of the [[atrial kick]] (the atrial contraction) and due to an increase in the [[heart rate]] which reduces the time available for the left ventricle to fill. | * Left ventricular enlargement and lack of forward cardiac output can lead to [[left atrial enlargement]]. [[Left atrial dilation]] may lead to [[atrial fibrillation]] which occurs in 20% of patients with [[congestive heart failure]]. Atrial fibrillation diminishes left ventricular filling through the loss of the [[atrial kick]] (the atrial contraction) and due to an increase in the [[heart rate]] which reduces the time available for the left ventricle to fill. | ||
===Pulmonary Edema=== | |||
* The reduction in forward cardiac output leads to a rise in the [[pulmonary capillary wedge pressure]]. [[Rales]] usually develop if the [[pulmonary capillary wedge pressure]] is >25 mm Hg. [[Rales]] may not be present in the patient with chronic heart failure. [[Rales]] may develop at even lower pressures if LV function deteriorates suddenly. | * The reduction in forward cardiac output leads to a rise in the [[pulmonary capillary wedge pressure]]. [[Rales]] usually develop if the [[pulmonary capillary wedge pressure]] is >25 mm Hg. [[Rales]] may not be present in the patient with chronic heart failure. [[Rales]] may develop at even lower pressures if LV function deteriorates suddenly. | ||
*[[Dyspnea]] and [[orthopnea]] occur due to interstitial edema within the lungs at lower pressures. | *[[Dyspnea]] and [[orthopnea]] occur due to interstitial edema within the lungs at lower pressures. | ||
*The reduction in forward cardiac output leads to [[hypoperfusion]] at rest which is suggested by [[cool extremities]] | ===End Organ Hypoperfusion=== | ||
*The reduction in forward cardiac output leads to [[hypoperfusion]] at rest which is suggested by :*[[cool extremities]] | |||
:*[[confusion]] and altered mentation | |||
:*Impaired renal perfusion and declining renal function | |||
==Pathology== | ==Pathology== | ||
Revision as of 11:59, 2 April 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Saleh El Dassouki, M.D [3], Atif Mohammad, MD
Overview
Underlying Anatomic Abnormalities
Heart failure may result from an abnormality of any one of the anatomical structures of the heart:
- Pericardium
- Myocardium
- Endocardium
- Valvular heart disease or
- Disorders of the great vessels (e.g. pulmonary hypertension)
Systolic versus Diastolic Dysfunction
Heart failure was once thought to be secondary to a depressed left ventricular ejection fraction. However, studies have shown that approximately 50% of patients who are diagnosed with heart failure have a normal ejection fraction (diastolic dysfunction). Patients may be broadly classified as having heart failure with depressed left ventricular ejection fraction (systolic dysfunction) or normal/preserved ejection fraction (diastolic dysfunction). Systolic and diastolic dysfunction commonly occur in conjunction with each other.
Pathophysiology
- In heart failure, there is a failure of blood to move forward (forward failure) and a tendency of blood to move back ward (backward failure).
- Normally, with respect to the left side of the heart, blood flows from the lungs, into the pulmonary veins, into the left atrium, through the mitral valve, and finally into the left ventricle. When the left ventricle cannot be normally filled during diastole, blood will back up into the left atrium and, eventually, into the lungs. The result is a higher than normal pressure of blood within the vessels of the lung. As a result of hydrostatic forces, this high pressure leads to leaking of fluid (i.e. transudate) from the lung's blood vessels into the air-spaces (alveoli) of the lungs. The result is pulmonary edema, a condition characterized by difficulty breathing, inadequate oxygenation of blood, and, if severe and untreated, death.
Compensatory Mechanisms
- Left ventricular systolic dysfunction is associated with a reduction in stroke volume, the amount of blood the heart ejects with each heart beat.
- The reduction in stroke volume leads to a reduction in cardiac output which is the stroke volume multiplied by the heart rate.
- There are two compensatory mechanisms to preserve forward cardiac output (the product of stroke volume and heart rate):
- Dilation of the left ventricle to increase the stroke volume and
- Increase in heart rate
- Dilation of the left ventricle increases volume and increases contractility up to a point (see Frank-Starling law of the heart). As further LV dilation occurs, however, contractility drops, and functional mitral regurgitation (MR) may develop despite an anatomically normal mitral valve.
- Left ventricular enlargement and lack of forward cardiac output can lead to left atrial enlargement. Left atrial dilation may lead to atrial fibrillation which occurs in 20% of patients with congestive heart failure. Atrial fibrillation diminishes left ventricular filling through the loss of the atrial kick (the atrial contraction) and due to an increase in the heart rate which reduces the time available for the left ventricle to fill.
Pulmonary Edema
- The reduction in forward cardiac output leads to a rise in the pulmonary capillary wedge pressure. Rales usually develop if the pulmonary capillary wedge pressure is >25 mm Hg. Rales may not be present in the patient with chronic heart failure. Rales may develop at even lower pressures if LV function deteriorates suddenly.
- Dyspnea and orthopnea occur due to interstitial edema within the lungs at lower pressures.
End Organ Hypoperfusion
- The reduction in forward cardiac output leads to hypoperfusion at rest which is suggested by :*cool extremities
- confusion and altered mentation
- Impaired renal perfusion and declining renal function
Pathology
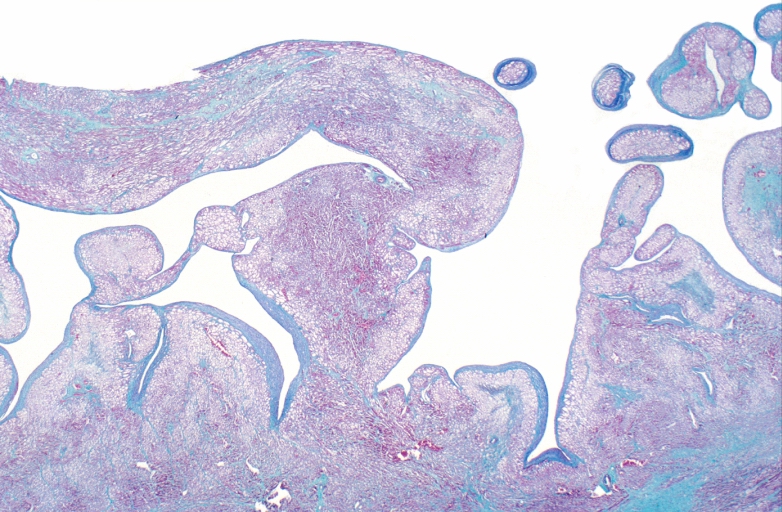
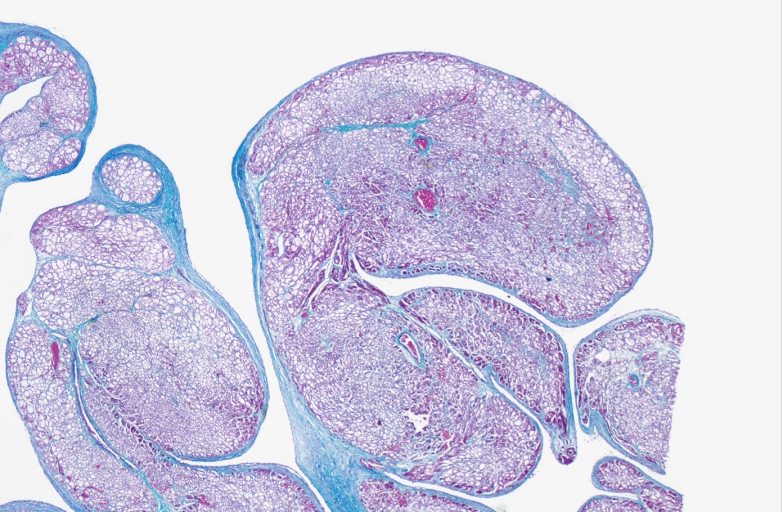
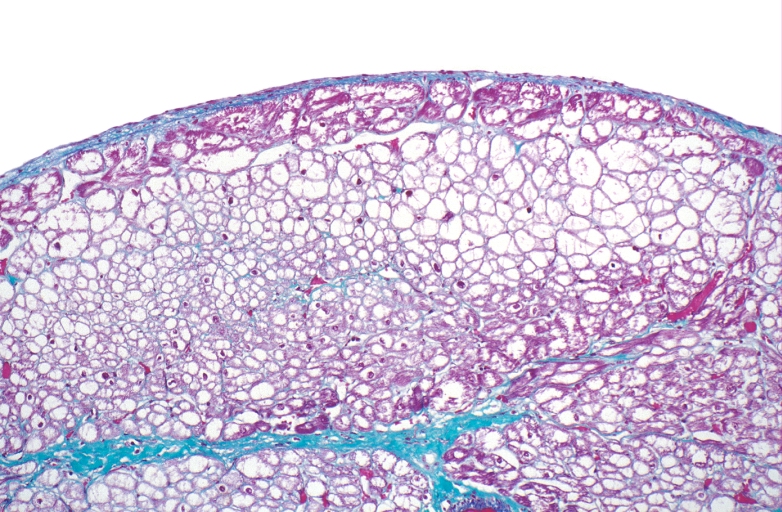
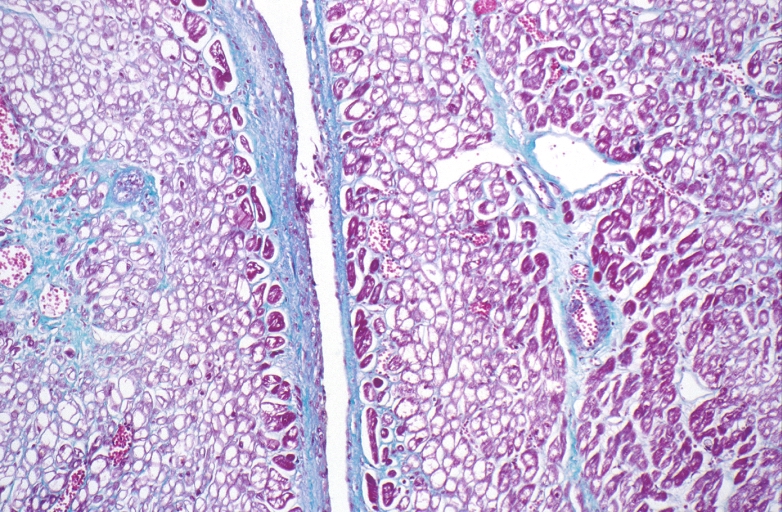
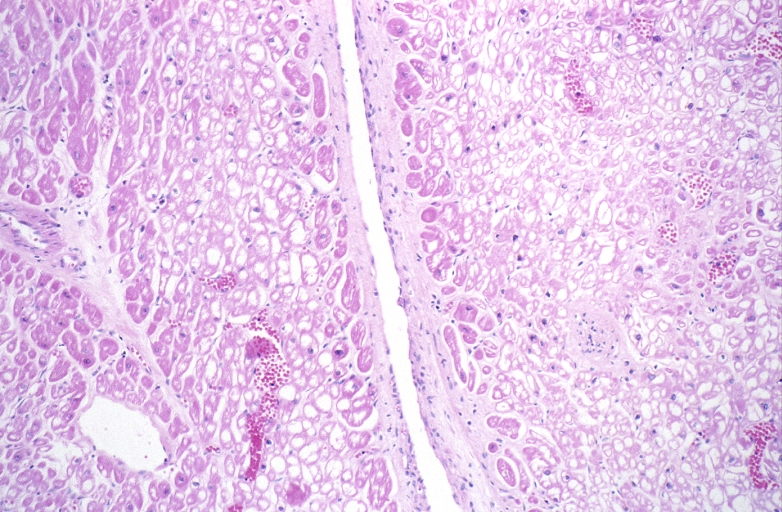
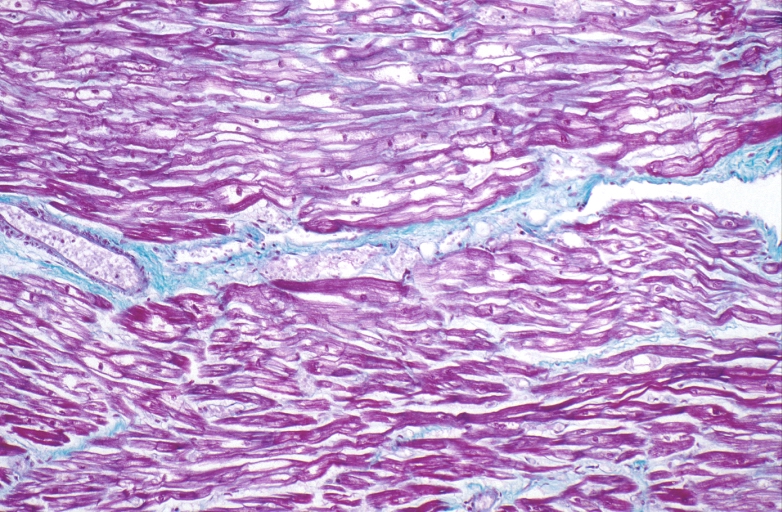
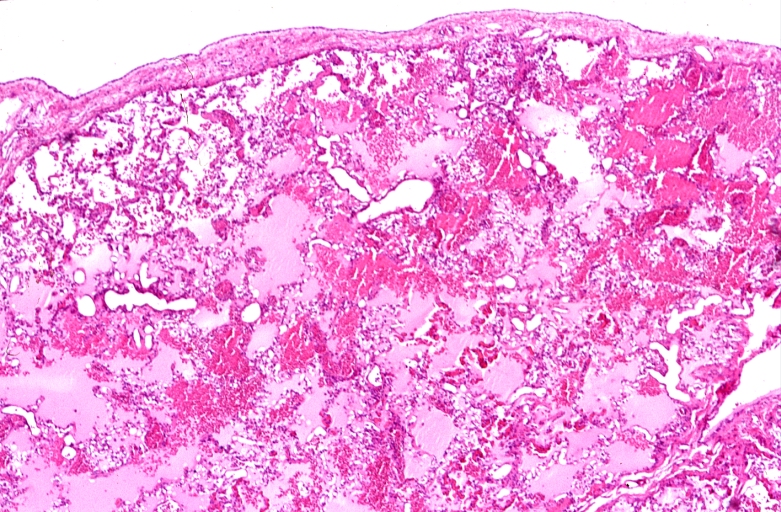
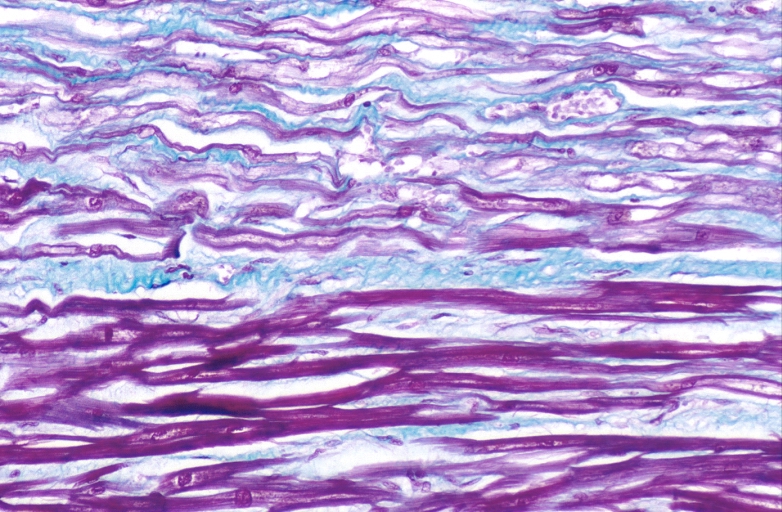
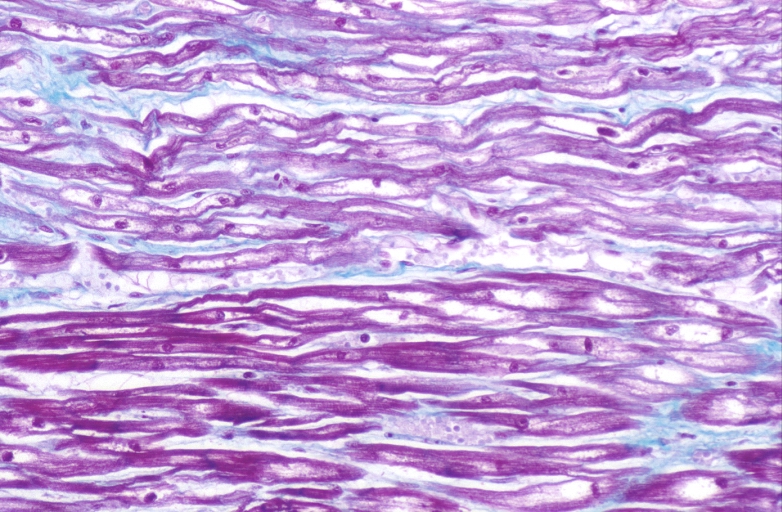
Microscopic Pathology
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
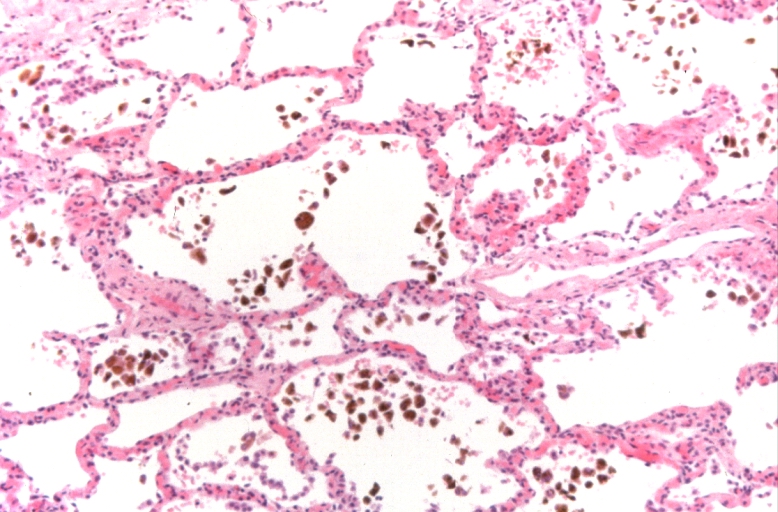
-
Lung, congestion, heart failure cells (hemosiderin laden macrophages)
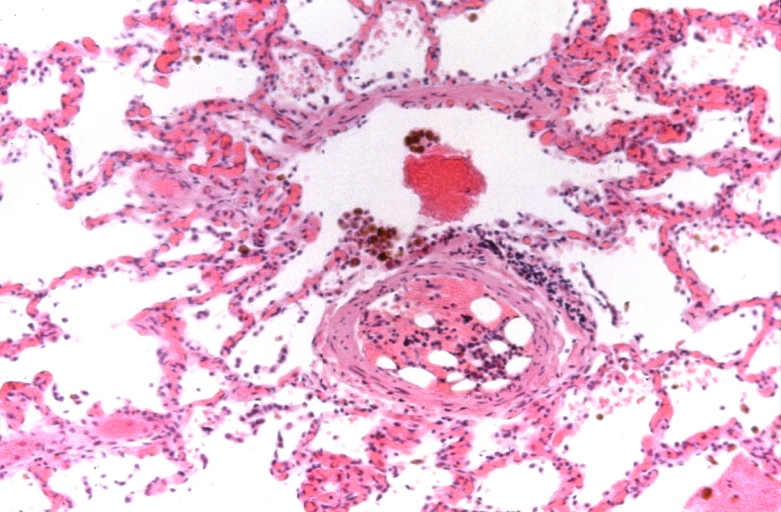
-
Lung, Congestive Heart Failure, bone marrow embolus
-
Lung, pulmonary edema in patient with congestive heart failure due to heart transplant rejection
-
HEART: Congestive heart failure, hydropic change
-
HEART Congestive heart failure, hydropic change
-
Spleen, congestion, congestive heart failure