Congestive heart failure pathophysiology: Difference between revisions
| Line 14: | Line 14: | ||
*[[Dyspnea]] and [[orthopnea]] occur due to interstitial edema at lower pressures. | *[[Dyspnea]] and [[orthopnea]] occur due to interstitial edema at lower pressures. | ||
*Hypoperfusion at rest is suggested by cool extremities, altered mentation, and declining renal function. | *Hypoperfusion at rest is suggested by cool extremities, altered mentation, and declining renal function. | ||
*[[Atrial fibrillation]] is a major target of therapy. It occurs in 20% of patients with [[congestive heart failure]]. | *[[Atrial fibrillation]] is a major target of therapy. It occurs in 20% of patients with [[congestive heart failure]]. | ||
Revision as of 21:00, 1 April 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Saleh El Dassouki, M.D [3], Atif Mohammad, MD
Overview
Heart failure may result from an abnormality of any one of the anatomical structures of the heart; the pericardium, the myocardium, the endocardium, valvular heart disease or disorders of the great vessels. Heart failure was once thought to be secondary to a depressed left ventricular ejection fraction. However, studies have shown that approximately 50% of patients who are diagnosed with heart failure have a normal ejection fraction (diastolic dysfunction). Patients may be broadly classified as having heart failure with depressed left ventricular ejection fraction (systolic dysfunction) or normal/preserved ejection fraction (diastolic dysfunction). Systolic and diastolic dysfunction commonly occur in conjunction with each other.
Pathophysiology
- Cardiac output can be maintained if LV dilation occurs and stroke volume is preserved even though the LVEF is low.
- As LV dilation occurs, functional mitral regurgitation (MR) may develop despite an anatomically normal mitral valve.
- The ejection fraction is usually below 35% in symptomatic patients.
- Rales usually develop if the pulmonary capillary wedge pressure is >25 mm Hg. Rales may not be present in the patient with chronic heart failure. Rales may develop at even lower pressures if LV function deteriorates suddenly.
- Dyspnea and orthopnea occur due to interstitial edema at lower pressures.
- Hypoperfusion at rest is suggested by cool extremities, altered mentation, and declining renal function.
- Atrial fibrillation is a major target of therapy. It occurs in 20% of patients with congestive heart failure.
Pathology
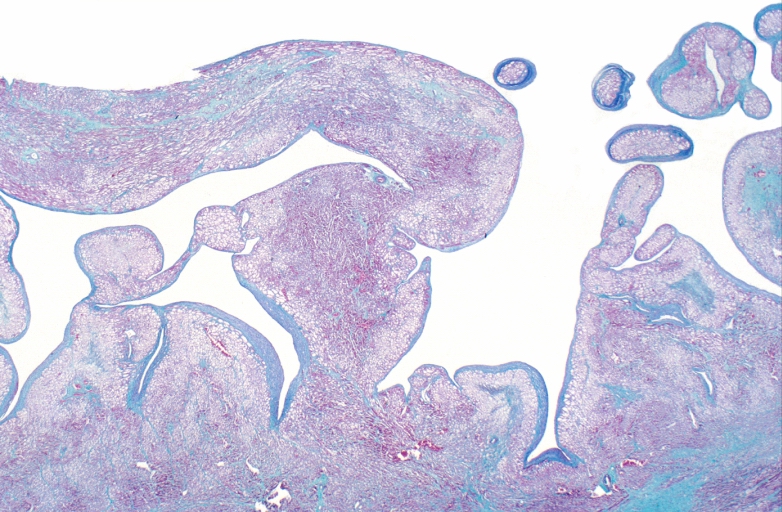
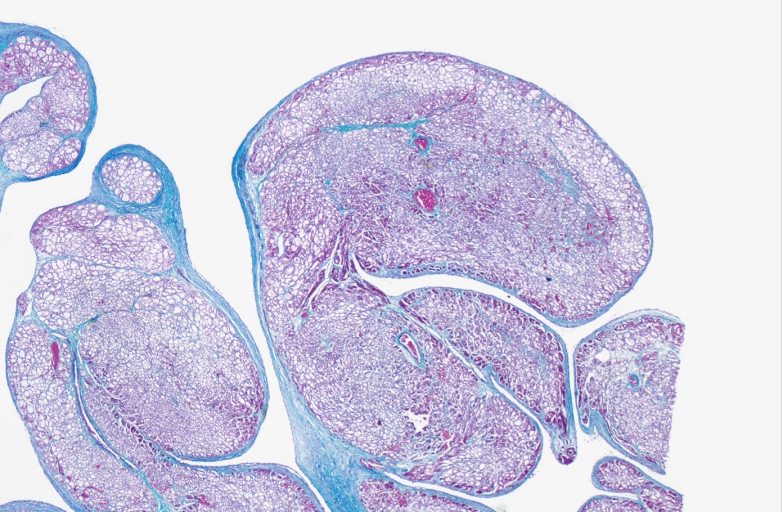
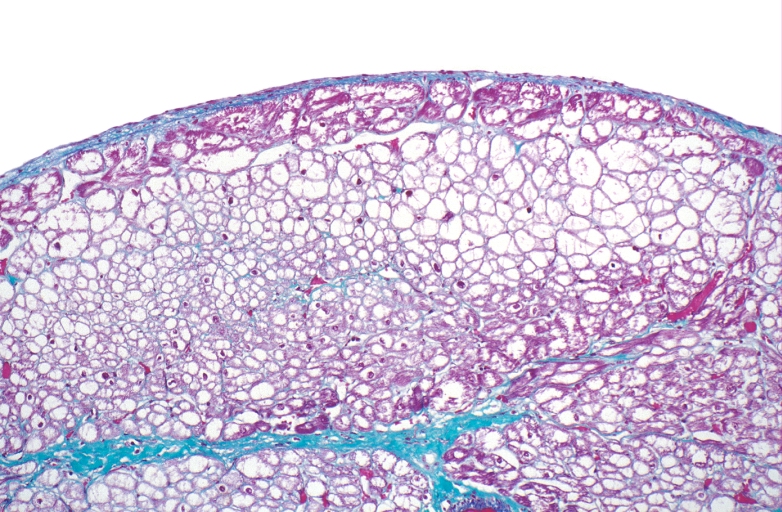
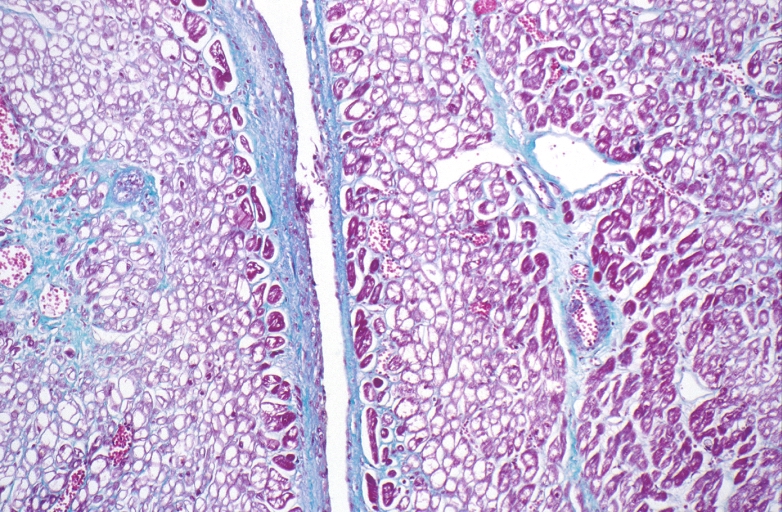
Microscopic Pathology
-
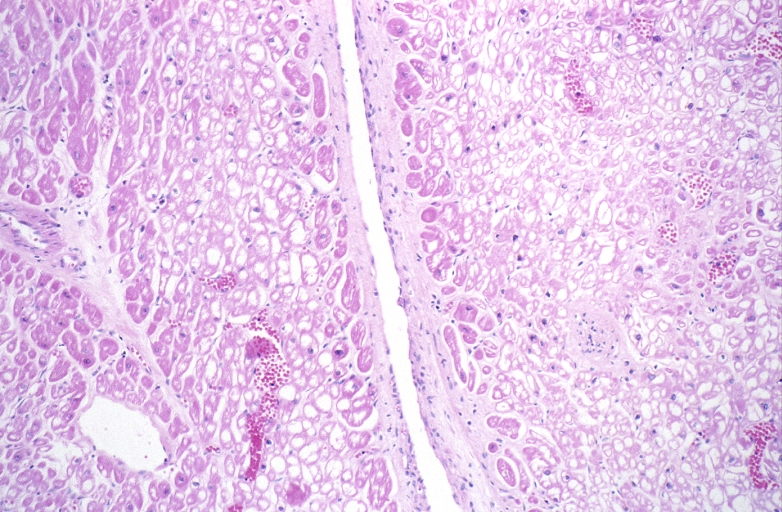
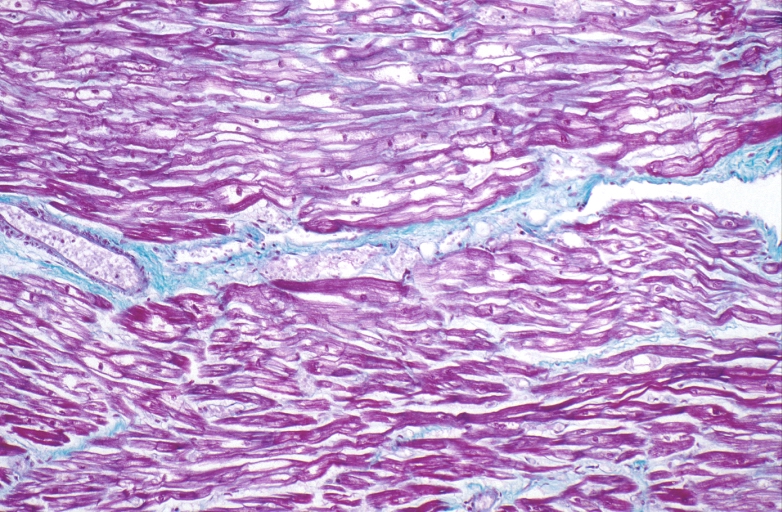
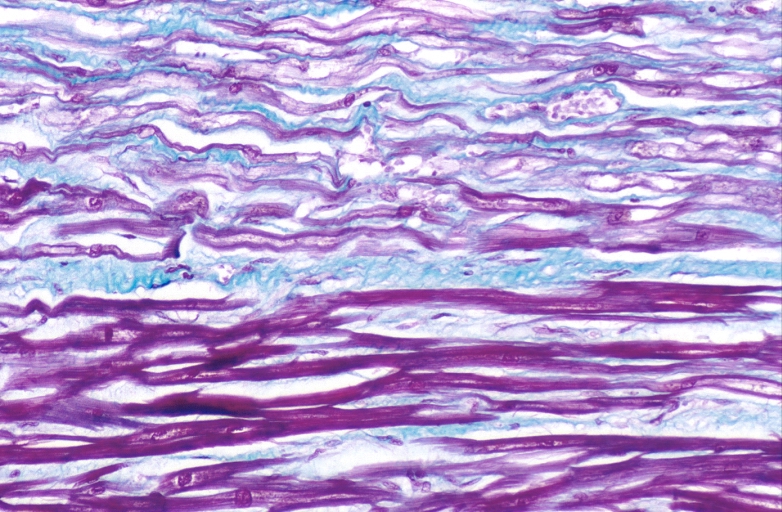
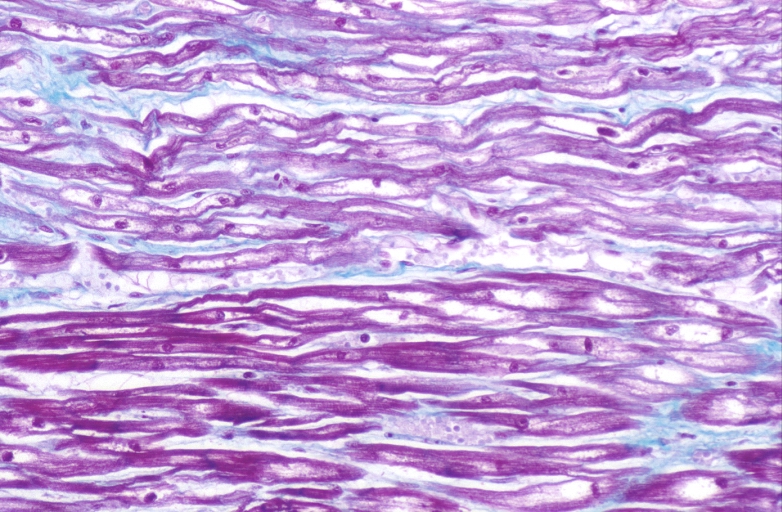
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
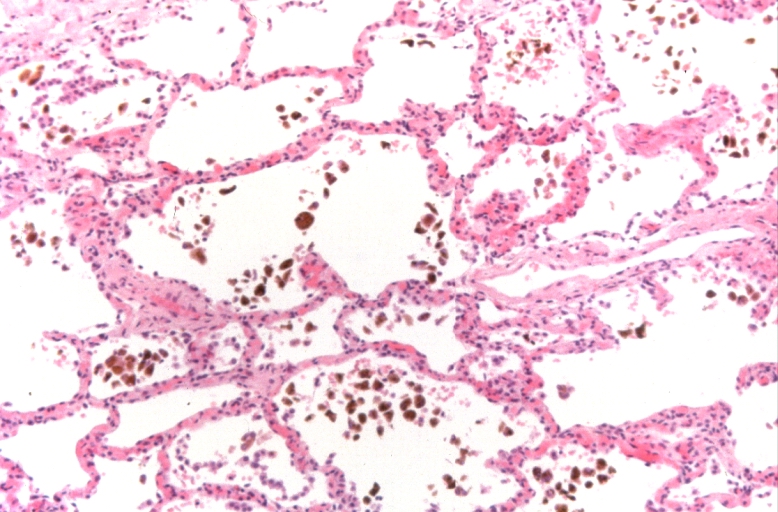
Lung, congestion, heart failure cells (hemosiderin laden macrophages)
-
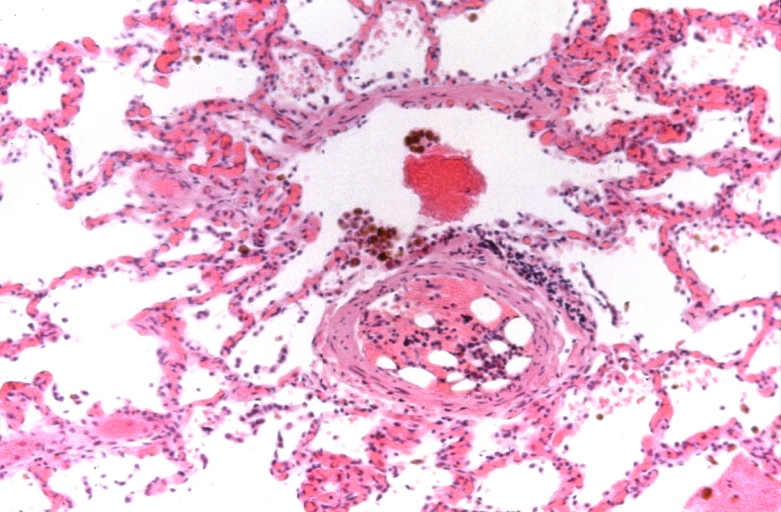
Lung, Congestive Heart Failure, bone marrow embolus
-
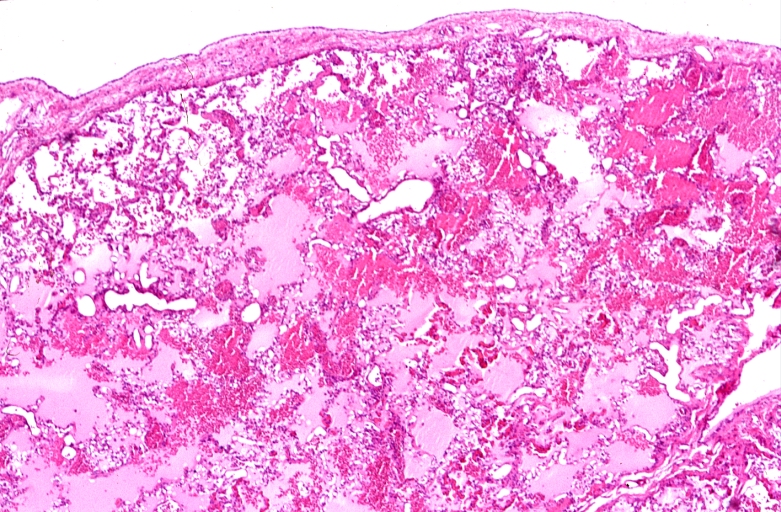
Lung, pulmonary edema in patient with congestive heart failure due to heart transplant rejection
-
HEART: Congestive heart failure, hydropic change
-
HEART Congestive heart failure, hydropic change
-
Spleen, congestion, congestive heart failure