Celiac disease pathophysiology
| https://https://www.youtube.com/watch?v=nXzBApAx5lY%7C350}} |
|
Celiac disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Celiac disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Celiac disease pathophysiology |
|
Risk calculators and risk factors for Celiac disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ;Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
Celiac disease is caused by a reaction to gliadin, a gluten protein found in wheat (and similar proteins of the tribe Triticeae which includes other cultivars such as barley and rye). Upon exposure to gliadin, the enzyme tissue transglutaminase modifies the protein, and the immune system cross-reacts with the bowel tissue, causing an inflammatory reaction. That leads to flattening of the lining of the small intestine, which interferes with the absorption of nutrients. The only effective treatment is a lifelong gluten-free diet.
Gluten may cause symptoms in people without celiac disease.[1][2]
Pathophysiology
Coeliac disease appears to be polyfactorial, both in that more than one abnormal factor can cause the disease and also more than one factor is necessary for the disease to manifest in a patient. Gluten triggers autoimmunity and results in the inflammation in the gastrointestinal mucosa.
- Gluten is mainly found in wheat. Gluten consists of storage proteins that remain after starch is washed from wheat-flour dough.
- These storage proteins have different solubilities in alcohol–water solutions and are usually separated into two fractions:
- Gliadins
- Glutenins
- Gluten proteins are grouped into four main types (ω5-, ω1,2-, α/β-, γ-gliadins).
- Several gliadin epitopes are immunogenic and also have direct toxic effects
Wheat
Wheat varieties or subspecies containing gluten such as spelt, Kamut®, and the rye/wheat hybrid triticale may also trigger the symptoms of celiac disease.[3]
Barley and rye
Barley and rye also induce symptoms of celiac disease. A small minority of coeliac patients also react to oats.[3][4][5]
- Prolamines are storage proteins with a similar aminoacid composition to the gliadin fractions of wheat. Prolines have been identified in barley (hordeins) and rye (secalines), and and are related closely to the properties of wheat cereal that affect people with celiac disease
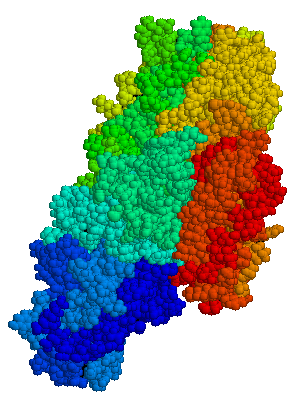
Pathogenesis
Gluten in wheat, rye, and barley may trigger the autoimmunity to develop celiac disease.[6]
- Gluten peptides cross the epithelium into the lamina propria.
- Gluten is deamidated by tissue transglutaminase.
- After the deamination presented by DQ2+ or DQ8+ antigen-presenting cells to pathogenic CD4+ T cells.
- The CD4+ T cells triggers the T-helper-cell type 1 response.
- The Type 1 response of T-helper cells results in the infiltration of inflammatory cells in the lapina propria and epithelium.
- This inflammatory process leads to crypt hyperplasia, and villous atrophy.
Tissue transglutaminase
Anti-transglutaminase antibodies to the enzyme tissue transglutaminase (tTG) are found in an overwhelming majority of cases. Tissue transglutaminase modifies gluten peptides into a form that may stimulate the immune system more effectively.[7]
- Endomysial component of antibodies (EMA) to tTG are believed to be directed toward cell surface transglutaminase.[8]
- It is suggested that the gliadin may be more responsible for the primary manifestations of coeliac disease whereas tTG is a bigger factor in secondary effects such as allergic responses and secondary autoimmune diseases.[9]
- Stored biopsies from suspected celiac patients have revealed that autoantibody deposits in the subclinical gastrointestinal mucosal lining celiacs are detected prior to clinical disease. These deposits are also found in patients who present with other autoimmune diseases, anemia or malabsorption phenomena at an increased rate over the normal population.[10]
VP7 protien
- In a large percentage of coeliac patients the anti-tTG antibodies also recognize a rotavirus protein called VP7. These antibodies stimulate monocytes proliferation and rotavirus infection might explain some early steps in the cascade of immune cell proliferation.[11] Indeed, earlier studies of rotavirus damage in the gut showed this causes a villous atrophy.[12]
- This suggests that viral proteins may take part in the initial flattening and stimulate self-crossreactive anti-VP7 production. Antibodies to VP7 may also slow healing until the gliadin mediated tTG presentation provides a second source of crossreactive antibodies.
Villous atrophy
- The inflammatory process, mediated by T cells, leads to disruption of the structure and function of the small bowel's mucosal lining.
- Alternative causes of this tissue damage have been proposed and involve the release of interleukin 15 and activation of the innate immune system by a shorter gluten peptide (p31–43/49). This would trigger killing of enterocytes by lymphocytes in the epithelium.
- The villous atrophy seen on biopsy may also be due to unrelated causes, such as tropical sprue, giardiasis and radiation enteritis. While positive serology and typical biopsy are highly suggestive of coeliac disease, lack of response to diet may require these alternative diagnoses to be considered.
Genetics
HLA and non HLA genes are involved in the pathogenesis of celiac disease[6].[13]
- HLA genes are a part of the MHC class II antigen-presenting receptor (also called the human leukocyte antigen) system and distinguishes cells between self and non-self for the purposes of the immune system. There are 7 HLA DQ variants (DQ2 and DQ4 through 9).
- DQ2 and DQ8 are associated with celiac disease. The gene is located on the short arm of the sixth chromosome, and as a result of the linkage this locus has been labeled CELIAC1.
- Over 95% of celiac patients have an isoform of DQ2 (encoded by DQA1*05 and DQB1*02 genes) and DQ8 (encoded by the haplotype DQA1*03:DQB1*0302), which is inherited in families. The reason these genes produce an increase in the risk of celiac disease is that the receptors formed by these genes bind to gliadin peptides more tightly than other forms of the antigen-presenting receptor. Therefore, these forms of the receptor are more likely to activate T lymphocytes and initiate the autoimmune process.
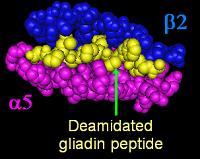
- Most celiac patients bear a two-gene HLA-DQ haplotype referred to as DQ2.5 haplotype. This haplotype is composed of 2 adjacent gene alleles, DQA1*0501 and DQB1*0201, which encode the two subunits, DQ α5 and DQ β2. In most individuals, the DQ2.5 isoform is encoded by one of two chromosomes 6 inherited from parents. Most celiacs inherit only one copy of the DQ2.5 haplotype, while some inherit it from both parents; the latter are especially at risk for coeliac disease, as well as being more susceptible to severe complications.[15]
- Some individuals inherit DQ2.5 from one parent and portions of the haplotype (DQB1*02 or DQA1*05) from the other parent, increasing risk. Less commonly, some individuals inherit the DQA1*05 allele from one parent and the DQB1*02 from the other parent, called a trans-haplotype association, and these individuals are at similar risk for coeliac disease as those with a single DQ2.5 bearing chromosome 6, but in this instance disease tends not to be familial.[16]
- In addition to the CELIAC1 locus, CELIAC2 (5q31-q33 - IBD5 locus), CELIAC3 (2q33 -CTLA4 locus), CELIAC4 (19p13.1 - MYOIXB locus), have been linked to coeliac disease. The CTLA4 and myosin IXB and gene have been found to be linked to coeliac disease and other autoimmune diseases.[17][18] Two additional loci on chromosome 4, 4q27 (IL2 or IL21 locus) and 4q14, have been found to be linked to coeliac disease.[19][20]
Associated Conditions
Celiac disease is associated with other autoimmune diseases which include:[21][22][23] [24][25]
- Type 1 diabetes mellitus
- IgA deficiency
- IgA nephropathy
- Insulin dependent diabetes mellitus (IDDM)
- Sjogren’s syndrome
- Juvenile idiopathic arthritis
- Juvenile rheumatoid arthritis
Gross Pathology
Microscopic Pathology
The classic pathology changes of coeliac disease in the small bowel are categorized by the "Marsh classification":[26]
- Marsh stage 0: normal mucosa
- Marsh stage 1: increased number of intra-epithelial lymphocytes, usually exceeding 20 per 100 enterocytes
- Marsh stage 2: proliferation of the crypts of Lieberkuhn
- Marsh stage 3: partial or complete villous atrophy
- Marsh stage 4: hypoplasia of the small bowel architecture
References
- ↑ Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD; et al. (2011). "Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial". Am J Gastroenterol. 106 (3): 508–14. doi:10.1038/ajg.2010.487. PMID 21224837.
- ↑ Carroccio A, Mansueto P, Iacono G, Soresi M, D'Alcamo A, Cavataio F; et al. (2012). "Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity". Am J Gastroenterol. 107 (12): 1898–906. doi:10.1038/ajg.2012.236. PMID 22825366.
- ↑ 3.0 3.1 "Grain toxicity" (RTF). The CELIAC list. Retrieved 2006-08-27.
- ↑ Lundin K, Nilsen E, Scott H, Løberg E, Gjøen A, Bratlie J, Skar V, Mendez E, Løvik A, Kett K (2003). "Oats induced villous atrophy in coeliac disease". Gut. 52 (11): 1649–52. PMID 14570737.
- ↑ Størsrud S, Olsson M, Arvidsson Lenner R, Nilsson L, Nilsson O, Kilander A (2003). "Adult coeliac patients do tolerate large amounts of oats". Eur J Clin Nutr. 57 (1): 163–9. PMID 12548312.
- ↑ 6.0 6.1 Di Sabatino A, Corazza GR (2009). "Coeliac disease". Lancet. 373 (9673): 1480–93. doi:10.1016/S0140-6736(09)60254-3. PMID 19394538.
- ↑ Dieterich W, Ehnis T, Bauer M, Donner P, Volta U, Riecken E, Schuppan D (1997). "Identification of tissue transglutaminase as the autoantigen of celiac disease". Nat Med. 3 (7): 797–801. PMID 9212111.
- ↑ Salmi T, Collin P, Korponay-Szabó I, Laurila K, Partanen J, Huhtala H, Király R, Lorand L, Reunala T, Mäki M, Kaukinen K (2006). "Endomysial antibody-negative coeliac disease: clinical characteristics and intestinal autoantibody deposits". Gut. 55 (12): 1746–53. PMID 16571636.
- ↑ Londei M, Ciacci C, Ricciardelli I, Vacca L, Quaratino S, and Maiuri L. (2005). "Gliadin as a stimulator of innate responses in celiac disease". Mol Immunol. 42 (8): 913–918. PMID 15829281.
- ↑ Kaukinen K, Peraaho M, Collin P, Partanen J, Woolley N, Kaartinen T, Nuuntinen T, Halttunen T, Maki M, Korponay-Szabo I (2005). "Small-bowel mucosal transglutaminase 2-specific IgA deposits in coeliac disease without villous atrophy: A Prospective and randomized clinical study". Scand J Gastroenterology. 40: 564–572. PMID 16036509.
- ↑ Zanoni G, Navone R, Lunardi C, Tridente G, Bason C, Sivori S, Beri R, Dolcino M, Valletta E, Corrocher R, Puccetti A (2006). "In celiac disease, a subset of autoantibodies against transglutaminase binds toll-like receptor 4 and induces activation of monocytes". PLoS Med. 3 (9): e358. PMID 16984219.
- ↑ Salim A, Phillips A, Farthing M (1990). "Pathogenesis of gut virus infection". Baillieres Clin Gastroenterol. 4 (3): 593–607. PMID 1962725.
- ↑ Hadithi M, von Blomberg BM, Crusius JB; et al. (2007). "Accuracy of serologic tests and HLA-DQ typing for diagnosing celiac disease". Ann. Intern. Med. 147 (5): 294–302. PMID 17785484.
- ↑ Kim C, Quarsten H, Bergseng E, Khosla C, Sollid L (2004). "Structural basis for HLA-DQ2-mediated presentation of gluten epitopes in celiac disease". Proc Natl Acad Sci U S A. 101 (12): 4175–9. PMID 15020763.
- ↑ Jores RD, Frau F, Cucca F; et al. (2007). "HLA-DQB1*0201 homozygosis predisposes to severe intestinal damage in celiac disease". Scand. J. Gastroenterol. 42 (1): 48–53. doi:10.1080/00365520600789859. PMID 17190762.
- ↑ Karell K, Louka AS, Moodie SJ; et al. (2003). "HLA types in celiac disease patients not carrying the DQA1*05-DQB1*02 (DQ2) heterodimer: results from the European Genetics Cluster on Celiac Disease". Hum. Immunol. 64 (4): 469–77. PMID 12651074.
- ↑ Zhernakova A, Eerligh P, Barrera P; et al. (2005). "CTLA4 is differentially associated with autoimmune diseases in the Dutch population". Hum. Genet. 118 (1): 58–66. doi:10.1007/s00439-005-0006-z. PMID 16025348.
- ↑ Sánchez E, Alizadeh BZ, Valdigem G; et al. (2007). "MYO9B gene polymorphisms are associated with autoimmune diseases in Spanish population". Hum. Immunol. 68 (7): 610–5. doi:10.1016/j.humimm.2007.03.006. PMID 17584584.
- ↑ van Heel DA, Franke L, Hunt KA; et al. (2007). "A genome-wide association study for celiac disease identifies risk variants in the region harboring IL2 and IL21". Nat Genet. 39 (7): 827–9. doi:10.1038/ng2058. PMID 17558408.
- ↑ Popat S, Bevan S, Braegger C, Busch A, O'Donoghue D, Falth-Magnusson K, Godkin A, Hogberg L, Holmes G, Hosie K, Howdle P, Jenkins H, Jewell D, Johnston S, Kennedy N, Kumar P, Logan R, Love A, Marsh M, Mulder C, Sjoberg K, Stenhammar L, Walker-Smith J, Houlston R (2002). "Genome screening of coeliac disease". J Med Genet. 39 (5): 328–31. PMID 12011149.
- ↑ Fasano A, Berti I, Gerarduzzi T, Not T, Colletti RB, Drago S, Elitsur Y, Green PH, Guandalini S, Hill ID, Pietzak M, Ventura A, Thorpe M, Kryszak D, Fornaroli F, Wasserman SS, Murray JA, Horvath K (2003). "Prevalence of celiac disease in at-risk and not-at-risk groups in the United States: a large multicenter study". Arch. Intern. Med. 163 (3): 286–92. PMID 12578508.
- ↑ Murray JA (2005). "Celiac disease in patients with an affected member, type 1 diabetes, iron-deficiency, or osteoporosis?". Gastroenterology. 128 (4 Suppl 1): S52–6. PMID 15825127.
- ↑ "Co-occurrence of celiac disease and other autoimmune diseases in celiacs and their first-degree relatives - ScienceDirect".
- ↑ Cataldo F, Marino V, Bottaro G, Greco P, Ventura A (1997). "Celiac disease and selective immunoglobulin A deficiency". J. Pediatr. 131 (2): 306–8. PMID 9290622.
- ↑ "www.omicsonline.org".
- ↑ Marsh MN (1992). "Gluten, major histocompatibility complex, and the small intestine. A molecular and immunobiologic approach to the spectrum of gluten sensitivity ('celiac sprue')". Gastroenterology. 102 (1): 330–54. PMID 1727768. Unknown parameter
|month=ignored (help)