Acromegaly: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
{{GS}} | {{GS}} | ||
{{SI}} | {{SI}} | ||
==Overview== | ==Overview== | ||
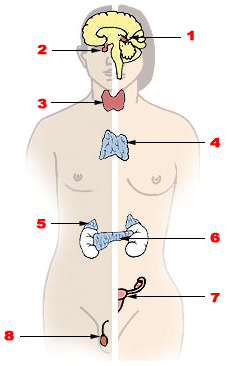
'''Acromegaly''' (from Greek ''akros'' "extreme" or "extremities" and ''megalos'' "large" - extremities enlargement) is a [[hormone|hormonal]] disorder that results when the [[pituitary]] gland produces excess [[human growth hormone|growth hormone]] (hGH). Most commonly it begins when a GH producing tumor derived from a distinct type of cells ([[somatotrophs]]) and called '''[[pituitary adenoma]]'''. | '''Acromegaly''' (from Greek ''akros'' "extreme" or "extremities" and ''megalos'' "large" - extremities enlargement) is a [[hormone|hormonal]] disorder that results when the [[pituitary]] gland produces excess [[human growth hormone|growth hormone]] (hGH). Most commonly it begins when a GH producing tumor derived from a distinct type of cells ([[somatotrophs]]) and called '''[[pituitary adenoma]]'''. | ||
Revision as of 15:18, 18 January 2012
| Acromegaly | |
 | |
|---|---|
| Acromegaly. Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California | |
| ICD-10 | E22.0 |
| ICD-9 | 253.0 |
| OMIM | 102200 |
| DiseasesDB | 114 |
| MedlinePlus | 000321 |
| MeSH | D000172 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
|
WikiDoc Resources for Acromegaly |
|
Articles |
|---|
|
Most recent articles on Acromegaly |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Acromegaly at Clinical Trials.gov Clinical Trials on Acromegaly at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Acromegaly
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Acromegaly Discussion groups on Acromegaly Patient Handouts on Acromegaly Directions to Hospitals Treating Acromegaly Risk calculators and risk factors for Acromegaly
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Acromegaly |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Overview
Acromegaly (from Greek akros "extreme" or "extremities" and megalos "large" - extremities enlargement) is a hormonal disorder that results when the pituitary gland produces excess growth hormone (hGH). Most commonly it begins when a GH producing tumor derived from a distinct type of cells (somatotrophs) and called pituitary adenoma.
Acromegaly most commonly affects middle-aged adults and can result in serious illness and premature death. Because of its insidious pathogenesis and slow progression, the disease is hard to diagnose in the early stages and is frequently missed for many years.
Symptoms
Features that result from high level of hGH or expanding tumor include:
- Soft tissue swelling of the hands and feet
- Brow and lower jaw protrusion
- Enlarging hands
- Enlarging feet
- Arthritis and carpal tunnel syndrome
- Teeth spacing increase
- Macroglossia [enlarged tongue]
- Heart failure
- Kidney failure
- Compression of the optic chiasm leading to loss of vision in the outer visual fields (typically bitemporal hemianopia)
- Headache
- Diabetes mellitus
- Hypertension
- Enlarging heart
- Increased palmar sweating and sebum production over the face (seborrhea) are clinical indicators of active growth hormone (GH) producing pituitary tumours. These symptoms can also be used to monitor the activity of the tumour after surgery although biochemical monitoring is confirmatory.
Causes
Pituitary adenoma
In over 90 percent of acromegaly patients, the overproduction of GH is caused by a benign tumor of the pituitary gland, called an adenoma. These tumors produce excess GH and, as they expand, compress surrounding brain tissues, such as the optic nerves. This expansion causes the headaches and visual disturbances that are often symptoms of acromegaly. In addition, compression of the surrounding normal pituitary tissue can alter production of other hormones, leading to changes in menstruation and breast discharge in women and impotence in men because of reduced testosterone production.
There is a marked variation in rates of GH production and the aggressiveness of the tumor. Some adenomas grow slowly and symptoms of GH excess are often not noticed for many years. Other adenomas grow rapidly and invade surrounding brain areas or the sinuses, which are located near the pituitary. In general, younger patients tend to have more aggressive tumors.
Most pituitary tumors arise spontaneously and are not genetically inherited. Many pituitary tumors arise from a genetic alteration in a single pituitary cell which leads to increased cell division and tumor formation. This genetic change, or mutation, is not present at birth, but is acquired during life. The mutation occurs in a gene that regulates the transmission of chemical signals within pituitary cells; it permanently switches on the signal that tells the cell to divide and secrete GH. The events within the cell that cause disordered pituitary cell growth and GH oversecretion currently are the subject of intensive research.
Other tumors
In a few patients, acromegaly is caused not by pituitary tumors but by tumors of the pancreas, lungs, and adrenal glands. These tumors also lead to an excess of GH, either because they produce GH themselves or, more frequently, because they produce GHRH, the hormone that stimulates the pituitary to make GH. In these patients, the excess GHRH can be measured in the blood and establishes that the cause of the acromegaly is not due to a pituitary defect. When these non-pituitary tumors are surgically removed, GH levels fall and the symptoms of acromegaly improve.
In patients with GHRH-producing, non-pituitary tumors, the pituitary still may be enlarged and may be mistaken for a tumor. Therefore, it is important that physicians carefully analyze all "pituitary tumors" removed from patients with acromegaly in order not to overlook the possibility that a tumor elsewhere in the body is causing the disorder.
Diagnosis
If acromegaly is suspected, medical imaging and medical laboratory investigations are generally used together to confirm or rule out the presence of this condition.
(Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
-
Facial changes secondary to elevated growth hormone levels. Note in particular prominent supra-orbital ridge, jaw, and generally enlarged facial features.
-
Markedly enlarged hand resulting from excess growth hormone. For reference purposes, the comparison hand is size 6 1/2.
-
Facial changes secondary to elevated growth hormone levels. Note in particular prominent supra-orbital ridge, jaw, and generally enlarged facial features.
Hormonal
IGF1 provides the most sensitive and useful lab test for the diagnosis of acromegaly. A single value of the Growth hormone (GH) is not useful in view of its pulsatality (levels in the blood vary greatly even in healthy individuals). GH levels taken 2 hours after a 75 or 100 gram glucose tolerance test are helpful in the diagnosis: GH levels are suppressed below 1 μg/L in normal people, and levels higher than this cutoff are confirmatory of acromegaly.
Other pituitary hormones have to be assessed to address the secretory effects of the tumour as well as the mass effect of the tumor on the normal pituitary gland. They include TSH (thyroid stimulating hormone), gonadotropic hormones (FSH,LH), ACTH (adrenocorticotropic hormone), prolactin.
Radiological
An MRI of the brain focussing on the sella turcica after gadolinium administration allows for clear delineation of the pituitary and the hypothalamus and the location of the tumour.
Treatment
The goals of treatment are to reduce GH production to normal levels, to relieve the pressure that the growing pituitary tumor exerts on the surrounding brain areas, to preserve normal pituitary function, and to reverse or ameliorate the symptoms of acromegaly. Currently, treatment options include surgical removal of the tumor, drug therapy, and radiation therapy of the pituitary.
Surgery
Surgery is a rapid and effective treatment, of which there are two alternative methods. The first method, a procedure known as Endonasal Transphenoidal surgery, involves the surgeon reaching the pituitary through an incision in the nasal cavity wall. The wall is reached by passing through the nostrils with microsurgical instruments. The second method is Transphenoidal surgery during which an incision is made into the gum beneath the upper lip. Further incisions are made to cut through the septum to reach the nasal cavity, where the pituitary is located. Endonasal Transphenoidal surgery is a less invasive procedure with a shorter recovery time than the older method of Transphenoidal surgery, and the likelihood of removing the entire tumor is greater with reduced side-effects. Consequently, Endosnasal Transphenoidal surgery is often used as a first option, with Transphenoidal and other treatments, such as, medicinal therapy or radiostatic neurosurgery being used to reduce the remaining adverse effects of the remaining tumor.
These procedures normally relieve the pressure on the surrounding brain regions and lead to a lowering of GH levels. If the surgery is successful, facial appearance and soft tissue swelling improve within a few days. Surgery is most successful in patients with blood GH levels below 40 ng/ml before the operation and with pituitary tumors no larger than 10 mm in diameter. Success depends on the skill and experience of the surgeon. The success rate also depends on what level of GH is defined as a cure. The best measure of surgical success is normalization of GH and IGF-1 levels. Ideally, GH should be less than 2 ng/ml after an oral glucose load. A review of GH levels in 1,360 patients worldwide immediately after surgery revealed that 60 percent had random GH levels below 5 ng/ml. Complications of surgery may include cerebrospinal fluid leaks, meningitis, or damage to the surrounding normal pituitary tissue, requiring lifelong pituitary hormone replacement.
Even when surgery is successful and hormone levels return to normal, patients must be carefully monitored for years for possible recurrence. More commonly, hormone levels may improve, but not return completely to normal. These patients may then require additional treatment, usually with medications.
Drug therapy
Two medications currently are used to treat acromegaly. These drugs reduce both GH secretion and tumor size. Medical therapy is sometimes used to shrink large tumors before surgery. Bromocriptine (Parlodel) in divided doses of about 20 mg daily reduces GH secretion from some pituitary tumors. Side effects include gastrointestinal upset, nausea, vomiting, light-headedness when standing, and nasal congestion. These side effects can be reduced or eliminated if medication is started at a very low dose at bedtime, taken with food, and gradually increased to the full therapeutic dose. Because bromocriptine can be taken orally, it is an attractive choice as primary drug or in combination with other treatments. However, bromocriptine lowers GH and IGF-1 levels and reduces tumor size in less than half of patients with acromegaly. Some patients report improvement in their symptoms although their GH and IGF-1 levels still are elevated.
The second medication used to treat acromegaly is octreotide (Sandostatin) and lanreotide (Somatulin). Both are synthetic forms of a brain hormone, somatostatin, that stops GH production. The long-acting forms of these drugs must be injected every 2 to 4 weeks for effective treatment. Most patients with acromegaly respond to this medication. In many patients, GH levels fall within one hour and headaches improve within minutes after the injection. Several studies have shown that octreotide and lanreotide are effective for long-term treatment. Octreotide and lanreotide have also been used successfully to treat patients with acromegaly caused by non-pituitary tumors.
Because octreotide inhibits gastrointestinal and pancreatic function, long-term use causes digestive problems such as loose stools, nausea, and gas in one third of patients. In addition, approximately 25 percent of patients develop gallstones, which are usually asymptomatic. In rare cases, octreotide treatment can cause diabetes. On the other hand, scientists have found that in some acromegaly patients who already have diabetes, octreotide can reduce the need for insulin and improve blood sugar control.
The latest development in the medical treatment of acromegaly is the use of growth hormone receptor antagonists. The only available member of this family is pegvisomant (Somavert). By blocking the action of the endogenous growth hormone molecules, this compound is able to control disease activity of acromegaly in virtually all patients. Pegvisomant has to be administered subcutaneously by daily injections. Combinations of long-acting somatostatin analogues and weekly injections of pegvisomant seem to be equally effective as daily injections of pegvisomant.
Radiation therapy
Radiation therapy has been used both as a primary treatment and combined with surgery or drugs. It is usually reserved for patients who have tumor remaining after surgery. These patients often also receive medication to lower GH levels. Radiation therapy is given in divided doses over four to six weeks. This treatment lowers GH levels by about 50 percent over 2 to 5 years. Patients monitored for more than 5 years show significant further improvement. Radiation therapy causes a gradual loss of production of other pituitary hormones with time. Loss of vision and brain injury, which have been reported, are very rare complications of radiation treatments.
No single treatment is effective for all patients. Treatment should be individualized depending on patient characteristics, such as age and tumor size. If the tumor has not yet invaded surrounding brain tissues, removal of the pituitary adenoma by an experienced neurosurgeon is usually the first choice. After surgery, a patient must be monitored for a long time for increasing GH levels. If surgery does not normalize hormone levels or a relapse occurs, a doctor will usually begin additional drug therapy. The first choice should be bromocriptine because it is easy to administer; octreotide is the second alternative. With both medications, long-term therapy is necessary because their withdrawal can lead to rising GH levels and tumor re-expansion. Radiation therapy is generally used for patients whose tumors are not completely removed by surgery; for patients who are not good candidates for surgery because of other health problems; and for patients who do not respond adequately to surgery and medication.
Pituitary gigantism in children
This condition of growth hormone excess is rare in children and is referred to as pituitary gigantism, because the excessive growth hormone produces excessive growth of bones and the child can achieve excessive height. As an affected child becomes an adult, many of the adult problems can gradually develop. The distinction between gigantism (occurring in children) and acromegaly (occurring in adults) can be made by the occurrence of the adenoma in relation to the closure of the epiphyses. If elevated growth hormone levels occur before the closure of the epiphyses (i.e. in prepubertal children), then gigantism ensues. If it occurs after the closure of the epiphyses (i.e., in adults) then acromegaly ensues.
See also
External links
- acromegaly.org A satellite site of the Pituitary Network Association
- Acromegaly and Gigantism (a very comprehensive article)
- Acromegaly and Gigantism (Image of a patient with macroglossia - enlargement of the tongue)
- Acromegaly at eMedicine
References
Source
bg:Акромегалия cs:Akromegalie de:Akromegalie gl:Acromegalia it:Acromegalia he:אקרומגליה nl:Acromegalie no:Akromegali sq:Akromegalia sk:Akromegália sr:Акромегалија fi:Akromegalia sv:Akromegali uk:Акромегалія

