Congestive heart failure pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Saleh El Dassouki, M.D [3], Atif Mohammad, MD
Overview
Heart failure may result from an abnormality of any one of the anatomical structures of the heart; the pericardium, the myocardium, the endocardium, valvular heart disease or disorders of the great vessels. Heart failure was once thought to be secondary to a depressed left ventricular ejection fraction. However, studies have shown that approximately 50% of patients who are diagnosed with heart failure have a normal ejection fraction (diastolic dysfunction). Patients may be broadly classified as having heart failure with depressed left ventricular ejection fraction (systolic dysfunction) or normal/preserved ejection fraction (diastolic dysfunction). Systolic and diastolic dysfunction commonly occur in conjunction with each other.
Pathophysiology
- Left ventricular systolic dysfunction is associated with a reduction in stroke volume, the amount of blood the heart ejects with each heart beat.
- The reduction in stroke volume leads to a reduction in cardiac output which is the stroke volume multiplied by the heart rate.
- The reduction in cardiac output can be compensated for in several ways:
- Dilation of the left ventricle to increase the stroke volume and
- Increase in heart rate
- Dilation of the left ventricle increases volume and increases contractility up to a point (see Frank-Starling law of the heart). As further LV dilation occurs, however, functional mitral regurgitation (MR) may develop despite an anatomically normal mitral valve.
- Left ventriular enlargment and lack of forward cardiac output can lead to left atrial enlargement. Left atrial dilation may lead to atrial fibrillation which occurs in 20% of patients with congestive heart failure. Atrial fibrillation diminishes left ventricular filling through the loss of the atrial kick (the atrial contraction) and due to an increase in the heart rate which reduces the time available for the left ventricle to fill.
- The reduction in forward cardiac output leads to a rise in the pulmonary capillary wedge pressure. Rales usually develop if the pulmonary capillary wedge pressure is >25 mm Hg. Rales may not be present in the patient with chronic heart failure. Rales may develop at even lower pressures if LV function deteriorates suddenly.
- Dyspnea and orthopnea occur due to interstitial edema within the lungsat lower pressures.
- The reduction in forward cardiac output leads to hypoperfusion at rest which is suggested by cool extremities, altered mentation, and declining renal function.
Pathology
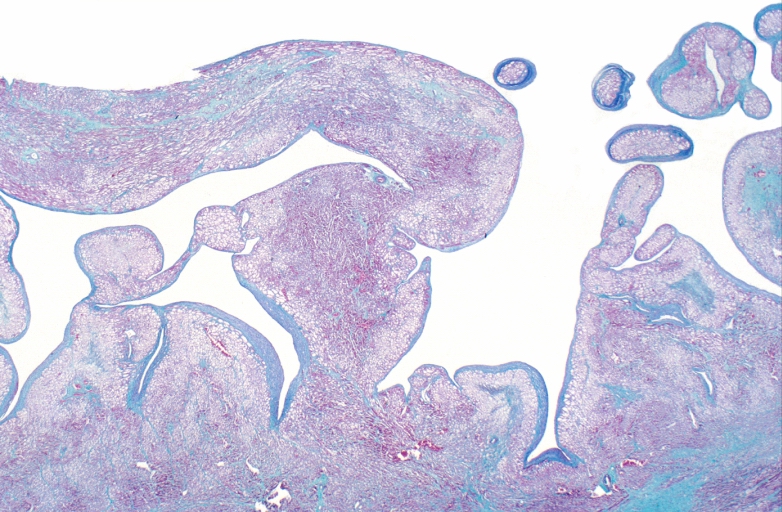
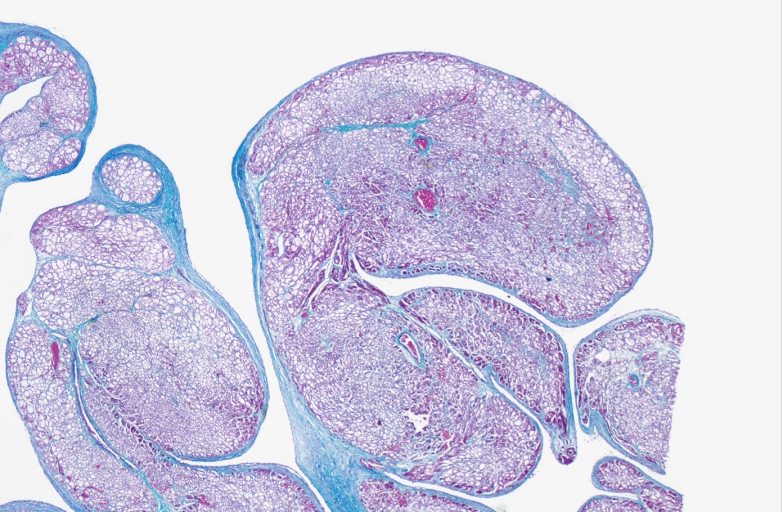
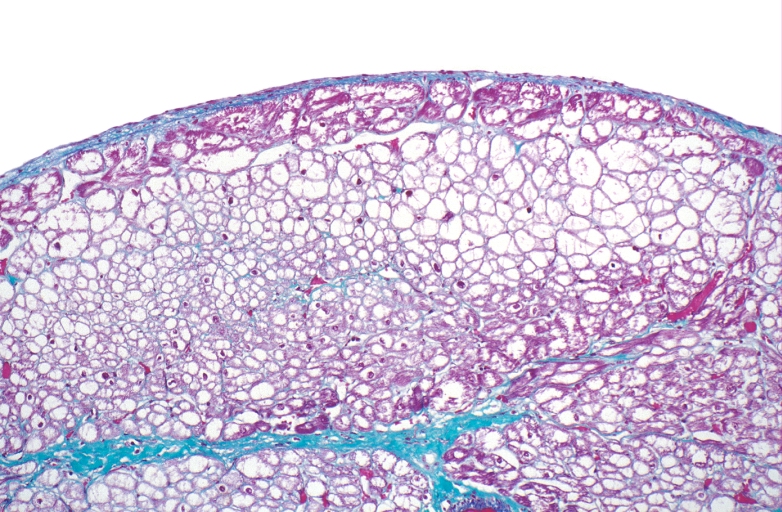
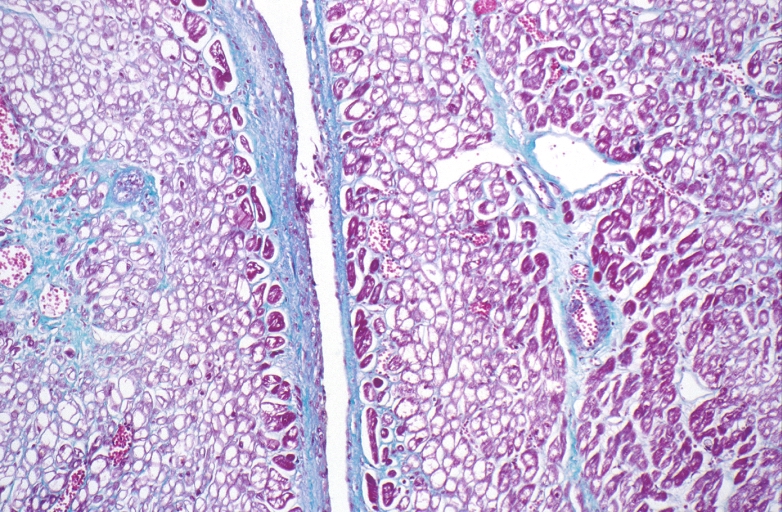
Microscopic Pathology
-
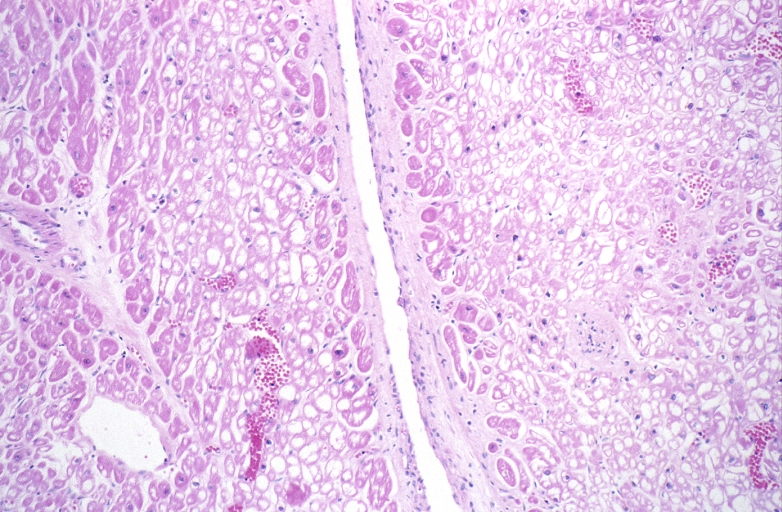
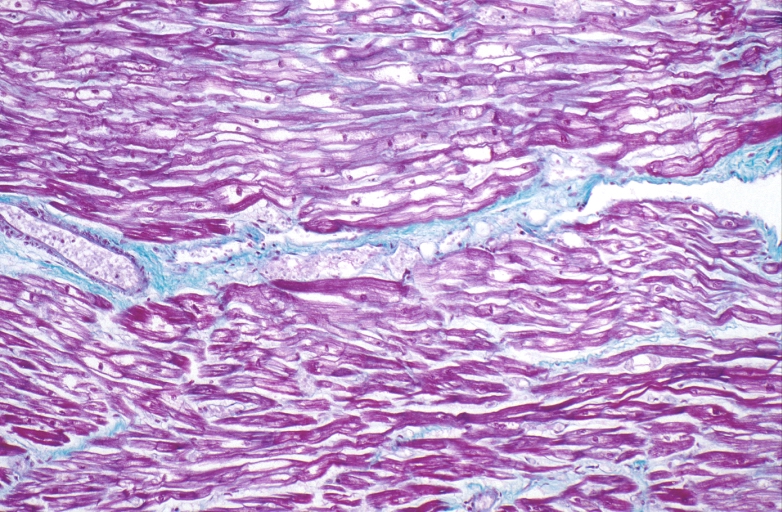
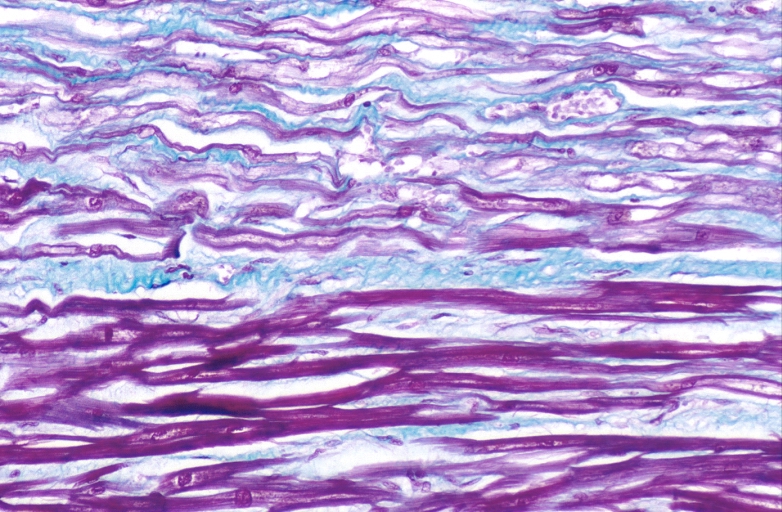
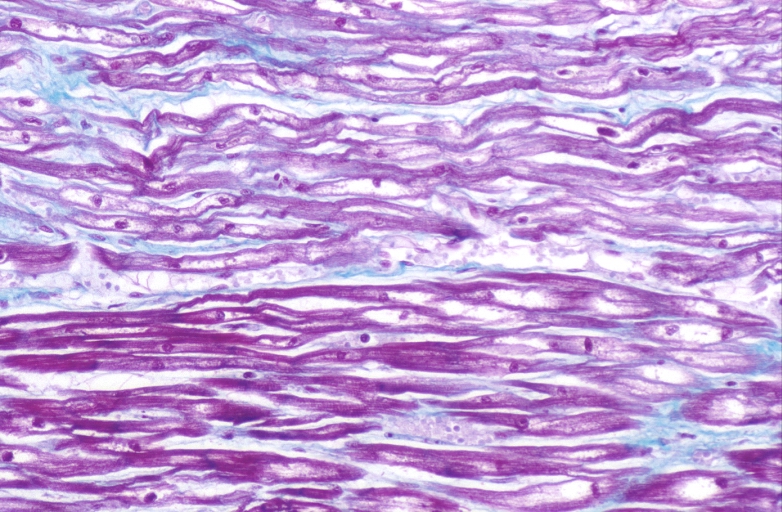
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
HEART: Congestive heart failure, hydropic change
-
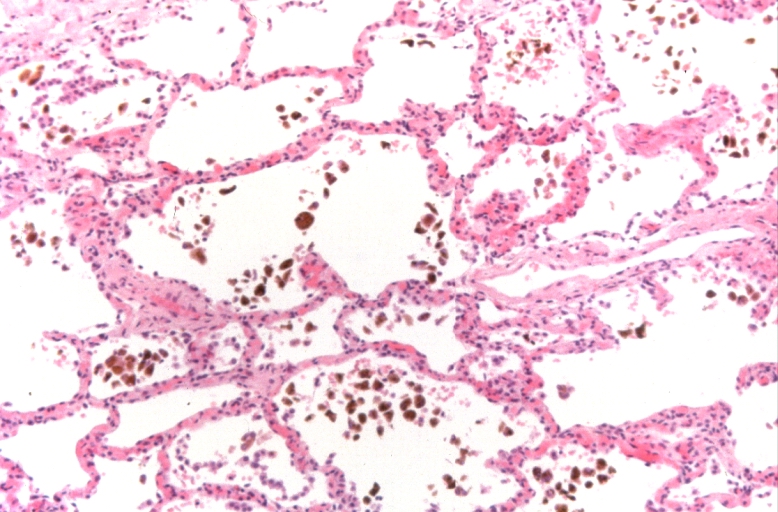
Lung, congestion, heart failure cells (hemosiderin laden macrophages)
-
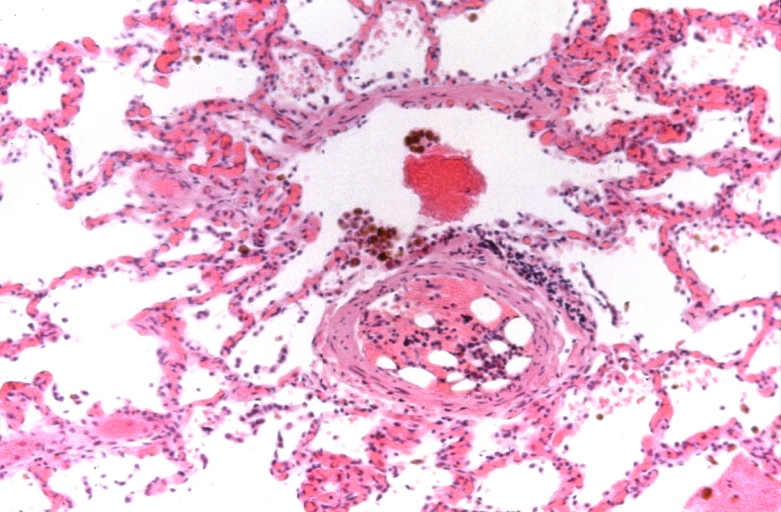
Lung, Congestive Heart Failure, bone marrow embolus
-
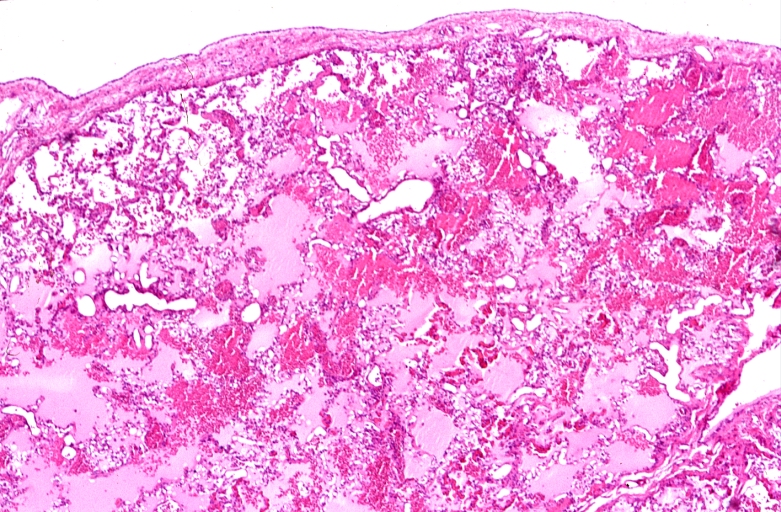
Lung, pulmonary edema in patient with congestive heart failure due to heart transplant rejection
-
HEART: Congestive heart failure, hydropic change
-
HEART Congestive heart failure, hydropic change
-
Spleen, congestion, congestive heart failure