Colitis: Difference between revisions
Mohamed riad (talk | contribs) No edit summary |
|||
| (70 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Colitis}} | ||
{{CMG}}; {{AE}} {{MUT}}; {{MK}}; {{Ochuko}}; {{Rim}}; {{QS}} | |||
{{CMG}}; {{AE}}{{MUT}}; {{MK}}; {{Ochuko}}; {{Rim}}; {{QS}}; {{Mohamed riad}}<br> | |||
{{SK}} Proctocolitis, Proctitis, Enterocolitis. | {{SK}} Colitis, Proctocolitis, Proctitis, Enterocolitis. | ||
==Overview== | ==Overview== | ||
Colitis is the [[inflammation]] of the [[colon (anatomy)|colon]], that can be either acute or chronic. | Colitis is the [[inflammation]] of the [[colon (anatomy)|colon]], that can be either [[acute]] or [[Chronic (medical)|chronic]]. Colitis may be caused by microorganisms such as ''[[Chlamydia trachomatis]]'', ''[[Neisseria gonorrhoeae]]'', ''[[Shigella dysenteriae]]'', [[Herpes Simplex Virus|HSV]], allergy (food protein-induced allergic proctocolitis), drugs ([[NSAIDs]]) and [[radiation]]. Colitis may co-exist with enteritis (inflammation of the small bowel), [[proctitis]] (inflammation of the [[rectum]]) or both. The symptoms of colitis such as [[diarrhea]] especially bloody diarrhea and abdominal pain (which may be mild) are seen in all forms of colitis. Colitis may be [[fulminant]] with a rapid downhill clinical course. In addition to the [[diarrhea]], [[fever]], and [[anemia]] may be reported. The patient with fulminant colitis has severe abdominal pain and presents a clinical picture similar to that of [[septicemia]], where [[Shock (medical)|shock]] is present. Treatment of colitis depends on the [[etiology]]. It may include the elimination of [[cows-milk protein]] or other food allergens from the diet, administration of [[antibiotic]]s and general anti-inflammatory medications such as [[mesalamine]] or its derivatives, [[glucocorticoids|steroids]], or one of a number of other drugs that ameliorate inflammation. The mainstay of therapy for infectious colitis is [[antimicrobial]] therapy. A common antibiotic regimen in treatment of patients with colitis is a combination of [[ceftriaxone]] and [[doxycycline]]. Supportive therapies such as correction of dehydration and [[anemia]], and reducing the intake of [[carbohydrates]], [[lactose]] products, soft drinks, and [[caffeine]] is often done for most patients with colitis. [[Irritable bowel syndrome]] (spastic colitis or spastic colon) has been called colitis, causing confusion despite colitis not being a feature of the disease. Immune mediated colitis is the experimental name in animal studies of [[ulcerative colitis]]. It is a synonym of [[ulcerative colitis]], but it should not be used as a synonym when referring to [[ulcerative colitis]]. | ||
==Classification== | ==Classification== | ||
| Line 13: | Line 14: | ||
{| style="cellpadding=0; cellspacing= 0; width: 600px;" | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 40%" align=center |'''Classes of Colitis''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align=center |'''Disorders''' | | style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 40%" align="center" |'''Classes of Colitis'''|| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF;" align="center" |'''Disorders''' | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''Autoimmune''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Autoimmune'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
*[[Ulcerative colitis]] | *[[Ulcerative colitis]] | ||
*[[Crohn's disease|Crohn's colitis]] | *[[Crohn's disease|Crohn's colitis]] | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''Allergic''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Allergic'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
*[[Food protein-induced proctocolitis ( | *[[Food protein-induced allergic proctocolitis (FPIAP)]] | ||
*[[Food protein-induced enterocolitis syndrome (FPIES)]] | |||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left| '''[[Infectious colitis]]''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''[[Infectious colitis]]'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
* [[Pseudomembranous colitis]] (''[[Clostridium difficile]]'') | *[[Pseudomembranous colitis]] (''[[Clostridium difficile]]'') | ||
* Enterohemorrhagic colitis (''[[Shigella dysenteriae]]'' or [[Shigatoxigenic group of Escherichia coli]] (STEC)) | *Enterohemorrhagic colitis (''[[Shigella dysenteriae]]'' or [[Shigatoxigenic group of Escherichia coli]] (STEC)) | ||
* Protozoan (''[[Entamoeba histolytica]]'') | *Protozoan (''[[Entamoeba histolytica]]'') | ||
* [[Lymphogranuloma venereum|''Chlamydia'' proctocolitis]] | *[[Lymphogranuloma venereum|''Chlamydia'' proctocolitis]] | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''[[Idiopathic]]'''||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''[[Idiopathic]]'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
* [[Lymphocytic colitis]] | *[[Lymphocytic colitis]] | ||
* [[Collagenous colitis]] | *[[Collagenous colitis]] | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left| '''Iatrogenic''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Iatrogenic'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
* [[Diversion colitis]] | *[[Diversion colitis]] | ||
* [[Chemical colitis]] | *[[Chemical colitis]] | ||
* [[Radiation colitis]] | *[[Radiation colitis]] | ||
*[[NSAID-induced colitis]] | |||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left| '''Vascular''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Vascular'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
* [[Ischemic colitis]] | *[[Ischemic colitis]] | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left|'''Drug induced''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Drug induced'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
*[[ | *[[NSAID-induced colitis]] | ||
|- | |- | ||
|style="font-size: 100; padding: 0 5px; background: #B8B8B8" align=left| '''Unclassifiable''' ||style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align=left | | | style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |'''Unclassifiable'''|| style="padding: 0 5px; font-size: 100%; background: #DCDCDC;" align="left" | | ||
* Indeterminate colitis (features of both [[Crohn's disease]] and [[ulcerative colitis]]) | *Indeterminate colitis (features of both [[Crohn's disease]] and [[ulcerative colitis]]) | ||
* Atypical colitis | *Atypical colitis | ||
|} | |} | ||
===Classification by Anatomy=== | ===Classification by Anatomy=== | ||
Colitis may co-exist with inflammation involving other parts of the gastrointestinal tract. It can be classified based on anatomy into | Colitis may co-exist with [[inflammation]] involving other parts of the [[gastrointestinal tract]]. It can be classified based on anatomy into: | ||
*Proctitis: When it involves the rectum | |||
*Colitis: When it involves the inflammation is limited to the colon | *[[Proctitis]]: When it involves the [[rectum]] | ||
*Proctocolitis: When it involves the rectum and colon (usually the distal part of the colon 12cm to 15cm above the anus ([[sigmoid colon]])<ref> 2015 Sexually Transmitted Diseases Treatment Guidelines. Centers for Disease Control and Prevention (2015).http://www.cdc.gov/std/tg2015/proctitis.htm Accessed on August 29, 2016</ref><ref name="pmid17099092">{{cite journal| author=Hamlyn E, Taylor C| title=Sexually transmitted proctitis. | journal=Postgrad Med J | year= 2006 | volume= 82 | issue= 973 | pages= 733-6 | pmid=17099092 | doi=10.1136/pmj.2006.048488 | pmc=2660501 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17099092 }} </ref> | *Colitis: When it involves the inflammation is limited to the [[Colon (anatomy)|colon]] | ||
*Enterocolitis: When it involves the small intestine in addition to the colon | *[[Proctocolitis]]: When it involves the [[rectum]] and [[Colon (anatomy)|colon]] (usually the distal part of the colon 12cm to 15cm above the anus ([[sigmoid colon]])<ref>2015 Sexually Transmitted Diseases Treatment Guidelines. Centers for Disease Control and Prevention (2015).http://www.cdc.gov/std/tg2015/proctitis.htm Accessed on August 29, 2016</ref><ref name="pmid17099092">{{cite journal| author=Hamlyn E, Taylor C| title=Sexually transmitted proctitis. | journal=Postgrad Med J | year= 2006 | volume= 82 | issue= 973 | pages= 733-6 | pmid=17099092 | doi=10.1136/pmj.2006.048488 | pmc=2660501 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17099092 }} </ref> | ||
*[[Enterocolitis]]: When it involves the [[small intestine]] in addition to the [[Colon (anatomy)|colon]] | |||
====Schematic of Anatomical Classification of Colitis==== | ====Schematic of Anatomical Classification of Colitis==== | ||
<div style="float: left">[[Image:Gastro-intestinal tract.png|thumb|200px|'''Affected anatomical areas:<ref name="gitractcolitis"> WikiMedia Commons https://commons.wikimedia.org/wiki/File:Gastro-intestinal_tract.png. Accessed on September 09, 2016</ref>'''<br>*'''Regions 4 to 6:''' Enterocolitis<br>*'''Region 6: '''Colitis<br>*'''Regions 6 to 8:''' Proctocolitis<br>*'''Regions 7 to 8:'''Proctitis]]</div><p style="clear:left"></p> | <div style="float: left">[[Image:Gastro-intestinal tract.png|thumb|200px|'''Affected anatomical areas: By Edelhart Kempeneers - Gray's Anatomy, Public Domain, https://commons.wikimedia.org/w/index.php?curid=534843<ref name="gitractcolitis">WikiMedia Commons https://commons.wikimedia.org/wiki/File:Gastro-intestinal_tract.png. Accessed on September 09, 2016</ref>'''<br>*'''Regions 4 to 6:''' Enterocolitis<br>*'''Region 6: '''Colitis<br>*'''Regions 6 to 8:''' Proctocolitis<br>*'''Regions 7 to 8:'''Proctitis]]</div><p style="clear:left"></p> | ||
===Classification by Age=== | ===Classification by Age=== | ||
*Infantile | |||
* | *'''Infantile''' (first six months of life)<ref name="pmid25976434">{{cite journal| author=Nowak-Węgrzyn A| title=Food protein-induced enterocolitis syndrome and allergic proctocolitis. | journal=Allergy Asthma Proc | year= 2015 | volume= 36 | issue= 3 | pages= 172-84 | pmid=25976434 | doi=10.2500/aap.2015.36.3811 | pmc=4405595 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25976434 }} </ref><ref name="pmid11264489">{{cite journal| author=Pumberger W, Pomberger G, Geissler W| title=Proctocolitis in breast fed infants: a contribution to differential diagnosis of haematochezia in early childhood. | journal=Postgrad Med J | year= 2001 | volume= 77 | issue= 906 | pages= 252-4 | pmid=11264489 | doi= | pmc=1741985 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11264489 }} </ref><ref name="pmid21922029">{{cite journal| author=Alfadda AA, Storr MA, Shaffer EA| title=Eosinophilic colitis: epidemiology, clinical features, and current management. | journal=Therap Adv Gastroenterol | year= 2011 | volume= 4 | issue= 5 | pages= 301-9 | pmid=21922029 | doi=10.1177/1756283X10392443 | pmc=3165205 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21922029 }} </ref> | ||
*'''Adult''' | |||
===Classification by duration of symptoms=== | ===Classification by duration of symptoms=== | ||
*'''Acute:''' Less than three months.<ref name="pmid24686268">{{cite journal| author=Hauer-Jensen M, Denham JW, Andreyev HJ| title=Radiation enteropathy--pathogenesis, treatment and prevention. | journal=Nat Rev Gastroenterol Hepatol | year= 2014 | volume= 11 | issue= 8 | pages= 470-9 | pmid=24686268 | doi=10.1038/nrgastro.2014.46 | pmc=4346191 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24686268 }} </ref> | |||
*'''Chronic:''' Longer than three months. Often months to years.<ref name="pmid24686268">{{cite journal| author=Hauer-Jensen M, Denham JW, Andreyev HJ| title=Radiation enteropathy--pathogenesis, treatment and prevention. | journal=Nat Rev Gastroenterol Hepatol | year= 2014 | volume= 11 | issue= 8 | pages= 470-9 | pmid=24686268 | doi=10.1038/nrgastro.2014.46 | pmc=4346191 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24686268 }} </ref> | |||
* | |||
== | ==Differential Diagnosis== | ||
The differential diagnosis of colitis can be classified into two categories according to age group. A work up for colitis must include the following differentials: | |||
===Differential diagnosis in Infants=== | |||
*[[Swallowed maternal blood syndrome]] | |||
*[[Anorectal fissure]] | |||
*[[Necrotizing enterocolitis]] especially in preterm babies | |||
*[[Vitamin K dependent hemorrhage]] | |||
*Other coagulopathies: (hereditary such as coagulation factor deficiency or acquired such as [[disseminated intravascular coagulopathy]]) | |||
*[[Intussusception]] | |||
*Upper Gastrointestinal Infections | |||
*[[Enteritis]] | |||
*[[Meckel diverticulum]] | |||
*[[Intestinal duplication cysts]] | |||
*Vascular malformations | |||
*Inflammatory bowel disease(early onset) | |||
*[[Hirschsprung disease]] complicated by [[enterocolitis]] | |||
*[[Volvulus]] | |||
*Gastro-duodenal ulcers | |||
*Gastrointestinal duplication cyst | |||
*[[Liver disease]] with clotting factor deficiency | |||
*Lymphonodular hyperplasia | |||
===Differential diagnosis in Adults=== | |||
* | *[[Colorectal cancer|Colorectal malignancy]] | ||
*[[Crohn's disease]] | |||
*[[Behçet's disease|Behcet's disease]] | |||
*[[Arteriovenous malformation]] | |||
*[[Diverticulosis]] | |||
*Enteritis | |||
*[[Coagulopathy]] | |||
*[[Systemic lupus erythematosus]](SLE) | |||
*Cytomegalovirus colitis | |||
=== | ===Differentiating Between Different Types of Colitis=== | ||
The symptoms of colitis such as [[diarrhea]] especially [[bloody diarrhea]] and [[abdominal pain]] are seen are seen in all forms of colitis. The table below differentiates among the common causes of colitis:<ref name="pmid14702426">{{cite journal| author=Thielman NM, Guerrant RL| title=Clinical practice. Acute infectious diarrhea. | journal=N Engl J Med | year= 2004 | volume= 350 | issue= 1 | pages= 38-47 | pmid=14702426 | doi=10.1056/NEJMcp031534 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14702426 }} </ref><ref name="pmid15537721">{{cite journal| author=Khan AM, Faruque AS, Hossain MS, Sattar S, Fuchs GJ, Salam MA| title=Plesiomonas shigelloides-associated diarrhoea in Bangladeshi children: a hospital-based surveillance study. | journal=J Trop Pediatr | year= 2004 | volume= 50 | issue= 6 | pages= 354-6 | pmid=15537721 | doi=10.1093/tropej/50.6.354 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15537721 }} </ref> | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="2" |Diseases | |||
! colspan="4" |History and Symptoms | |||
! colspan="4" |Physical Examination | |||
! colspan="4" |Laboratory findings | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!Diarrhea | |||
!Rectal bleeding | |||
: | !Abdominal pain | ||
!Atopy | |||
: | !Dehydration | ||
!Fever | |||
!Hypotension | |||
!Malnutrition | |||
!Blood in stool (frank or occult) | |||
!Microorganism in stool | |||
!Pseudomembranes on endoscopy | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Allergic Colitis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Chemical colitis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Infectious colitis | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | +++ | |||
| style="background: #F5F5F5; padding: 5px;" | +++ | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Radiation colitis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Ischemic colitis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Drug-induced colitis | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | ++ | |||
| style="background: #F5F5F5; padding: 5px;" | | |||
| style="background: #F5F5F5; padding: 5px;" | + | |||
|} | |||
==Causes== | ==Causes== | ||
===Common Causes=== | ===Common Causes=== | ||
Common causes of | Common causes of proctocolitis include infectious agents such as ''[[Chlamydia trachomatis]]'' (which causes lymphogranuloma venereum), ''[[Neisseria gonorrhoeae]]'', ''[[Herpes Simplex Virus|HSV]]'', ''[[Shigella dysenteriae]]'' and ''[[Campylobacter|Campylobacter species]]''. It can also be allergic (e.g. food protein-induced proctocolitis), idiopathic (e.g. [[microscopic colitis]]), vascular (e.g. [[ischemic colitis]]), or autoimmune (e.g. [[inflammatory bowel disease]]). | ||
===Causes by Organ System=== | ===Causes by Organ System=== | ||
{|style="width:80%; height:100px" border="1" | {| style="width:80%; height:100px" border="1" | ||
| | | style="width:25%" bgcolor="LightSteelBlue" ; border="1" |'''Cardiovascular''' | ||
| | | style="width:75%" bgcolor="Beige" ; border="1" |[[EVAR]], [[vasculitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Chemical / poisoning''' | |'''Chemical / poisoning''' | ||
|bgcolor="Beige"| [[Chemical colitis]] from Glutaraldehyde, Coffee enema, Hydrogen peroxide, [[lanthanum]] | | bgcolor="Beige" |[[Chemical colitis]] from Glutaraldehyde, Coffee enema, Hydrogen peroxide, [[lanthanum]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Dental''' | |'''Dental''' | ||
|bgcolor="Beige"|[[Dental braces]] | | bgcolor="Beige" |[[Dental braces]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Dermatologic''' | |'''Dermatologic''' | ||
|bgcolor="Beige"|[[Albinism]], [[Behcet disease]], [[scleroderma]], [[vasculitis]] | | bgcolor="Beige" |[[Albinism]], [[Behcet disease]], [[scleroderma]], [[vasculitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Drug Side Effect''' | |'''Drug Side Effect''' | ||
|bgcolor="Beige"| [[Alosetron]], [[ampicillin Oral]], [[auranofin]], [[azithromycin]], [[aztreonam Injection]], [[cefaclor]], [[cefadroxil]], [[cefamandole Nafate Injection]], [[cefazolin Sodium Injection]], [[cefepime Injection]], [[cefepime]], [[cefoperazone Sodium Injection]], [[cefotaxime Sodium Injection]], [[cefotetan Disodium Injection]], [[cefoxitin Sodium Injection]], [[cefpodoxime]], [[ceftazidime Injection]], [[ceftazidime]], [[ceftizoxime Sodium Injection]], [[ceftriaxone Sodium Injection]], [[cefuroxime Sodium Injection]], [[cephalexin]], [[cephalosporin]], [[cephradine Oral]], [[cidofovir]], [[cilansetron]], [[clindamycin]], [[co-amoxiclav]], [[corticosteroid]], [[darifenacin]], [[desogestrel and ethinyl estradiol]], [[dicloxacillin]], [[dirithromycin]], [[enoxacin]], [[ertapenem]], [[erythromycin and Sulfisoxazole]], [[flucytosine]], [[glycopyrrolate]], [[hyoscyamine]], [[idelalisib]], [[imipenem and Cilastatin Sodium Injection]], [[ipilimumab]], [[ixabepilone]], [[levofloxacin Oral]], [[lincomycin hydrochloride]], [[linezolid]], [[lomefloxacin]], [[loracarbef]], [[methotrexate]], [[miconazole Injection]], [[moxifloxacin]], [[nafcillin Sodium Injection]], [[nivolumab]], [[norfloxacin]], [[ofloxacin injection]], [[oxacillin Sodium Injection]], [[oxcarbazepine]], [[oxybutynin]], [[peginterferon alfa-2a]], [[penicillin]], [[pergolide]], [[piperacillin sodium injection]], [[pramipexole]], [[prednisolone]], [[procyclidine]], [[propantheline]], [[pseudoephedrine]], [[quinolone]], [[ramosetron]], [[reserpine]], [[solifenacin]], [[sparfloxacin]], [[tegaserod]] | | bgcolor="Beige" |[[Alosetron]], [[ampicillin Oral]], [[auranofin]], [[azithromycin]], [[aztreonam Injection]], [[cefaclor]], [[cefadroxil]], [[cefamandole Nafate Injection]], [[cefazolin Sodium Injection]], [[cefepime Injection]], [[cefepime]], [[cefoperazone Sodium Injection]], [[cefotaxime Sodium Injection]], [[cefotetan Disodium Injection]], [[cefoxitin Sodium Injection]], [[cefpodoxime]], [[ceftazidime Injection]], [[ceftazidime]], [[ceftizoxime Sodium Injection]], [[ceftriaxone Sodium Injection]], [[cefuroxime Sodium Injection]], [[cephalexin]], [[cephalosporin]], [[cephradine Oral]], [[cidofovir]], [[cilansetron]], [[clindamycin]], [[co-amoxiclav]], [[corticosteroid]], [[darifenacin]], [[desogestrel and ethinyl estradiol]], [[dicloxacillin]], [[dirithromycin]], [[enoxacin]], [[ertapenem]], [[erythromycin and Sulfisoxazole]], [[flucytosine]], [[glycopyrrolate]], [[hyoscyamine]], [[idelalisib]], [[imipenem and Cilastatin Sodium Injection]], [[ipilimumab]], [[ixabepilone]], [[levofloxacin Oral]], [[lincomycin hydrochloride]], [[linezolid]], [[lomefloxacin]], [[loracarbef]], [[methotrexate]], [[miconazole Injection]], [[moxifloxacin]], [[nafcillin Sodium Injection]], [[nivolumab]], [[norfloxacin]], [[ofloxacin injection]], [[oxacillin Sodium Injection]], [[oxcarbazepine]], [[oxybutynin]], [[peginterferon alfa-2a]], [[penicillin]], [[pergolide]], [[piperacillin sodium injection]], [[pramipexole]], [[prednisolone]], [[procyclidine]], [[propantheline]], [[pseudoephedrine]], [[quinolone]], [[ramosetron]], [[reserpine]], [[solifenacin]], [[sparfloxacin]], [[tegaserod]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Ear Nose Throat''' | |'''Ear Nose Throat''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Endocrine''' | |'''Endocrine''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Environmental''' | |'''Environmental''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Gastroenterologic''' | |'''Gastroenterologic''' | ||
|bgcolor="Beige"| [[Aganglionic megacolon]], [[alpha 1-antitrypsin deficiency]], [[autistic enterocolitis]], [[bacterial gastroenteritis]], [[polyp|cap polyposis]], [[chemical colitis]], [[colitis ulcerosa]], [[collagenous colitis]], [[colonic ischemia]], [[Crohn's disease]], [[diversion colitis]], [[diverticulosis]], [[Gerson diet]], [[infectious colitis]], [[inflammatory bowel disease]], [[intestinal ischemia]], [[irritable bowel syndrome]], [[ischemic colitis]], [[lymphocytic colitis]], [[microscopic colitis]], [[multiple organ dysfunction syndrome]], [[primary sclerosing cholangitis]], [[protein losing enteropathy]], [[pseudomembranous colitis]], [[radiation colitis]], [[radiation proctitis]], [[solitary rectal ulcer syndrome]], [[toxic megacolon]], [[typhlitis]], [[ulcerative colitis]] | | bgcolor="Beige" |[[Aganglionic megacolon]], [[alpha 1-antitrypsin deficiency]], [[autistic enterocolitis]], [[bacterial gastroenteritis]], [[polyp|cap polyposis]], [[chemical colitis]], [[colitis ulcerosa]], [[collagenous colitis]], [[colonic ischemia]], [[Crohn's disease]], [[diversion colitis]], [[diverticulosis]], [[Gerson diet]], [[infectious colitis]], [[inflammatory bowel disease]], [[intestinal ischemia]], [[irritable bowel syndrome]], [[ischemic colitis]], [[lymphocytic colitis]], [[microscopic colitis]], [[multiple organ dysfunction syndrome]], [[primary sclerosing cholangitis]], [[protein losing enteropathy]], [[pseudomembranous colitis]], [[radiation colitis]], [[radiation proctitis]], [[solitary rectal ulcer syndrome]], [[toxic megacolon]], [[typhlitis]], [[ulcerative colitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Genetic''' | |'''Genetic''' | ||
|bgcolor="Beige"| [[Albinism]], [[alpha 1-antitrypsin deficiency]] | | bgcolor="Beige" |[[Albinism]], [[alpha 1-antitrypsin deficiency]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Hematologic''' | |'''Hematologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Iatrogenic''' | |'''Iatrogenic''' | ||
|bgcolor="Beige"| [[Diversion colitis]], [[EVAR]], [[radiation colitis]], [[radiation proctitis]] | | bgcolor="Beige" |[[Diversion colitis]], [[EVAR]], [[radiation colitis]], [[radiation proctitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Infectious Disease''' | |'''Infectious Disease''' | ||
|bgcolor="Beige"| [[Bacillary dysentery]], [[bacterial gastroenteritis]], [[balantidium coli]], [[campylobacter jejuni]], [[chlamydia trachomatis]], [[clostridium difficile]], [[cryptosporidiosis]], [[cytomegalovirus]], [[entamoeba histolytica]], [[escherichia coli O157:H7]], [[giardiasis]], [[infectious colitis]], [[isosporiasis]], [[neisseria gonorrhoeae]], [[neonatal necrotizing enterocolitis]], [[pigbel]], [[salmonella]], [[schistosoma]], [[sepsis]], [[shigella]], [[strongyloides stercoralis]], [[syphilis]], [[treponema pallidum]], [[yersinia enterocolitica]] | | bgcolor="Beige" |[[Bacillary dysentery]], [[bacterial gastroenteritis]], [[balantidium coli]], [[campylobacter jejuni]], [[chlamydia trachomatis]], [[clostridium difficile]], [[cryptosporidiosis]], [[cytomegalovirus]], [[entamoeba histolytica]], [[escherichia coli O157:H7]], [[giardiasis]], [[infectious colitis]], [[isosporiasis]], [[neisseria gonorrhoeae]], [[neonatal necrotizing enterocolitis]], [[pigbel]], [[salmonella]], [[schistosoma]], [[sepsis]], [[shigella]], [[strongyloides stercoralis]], [[syphilis]], [[treponema pallidum]], [[yersinia enterocolitica]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Musculoskeletal / Ortho''' | |'''Musculoskeletal / Ortho''' | ||
|bgcolor="Beige"| [[Ankylosing Spondylitis]] | | bgcolor="Beige" |[[Ankylosing Spondylitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Neurologic''' | |'''Neurologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Nutritional / Metabolic''' | |'''Nutritional / Metabolic''' | ||
|bgcolor="Beige"| [[Gerson diet]], [[lysinuric protein intolerance]], [[milk allergy]], [[pigbel]], [[soy protein]] | | bgcolor="Beige" |[[Gerson diet]], [[lysinuric protein intolerance]], [[milk allergy]], [[pigbel]], [[soy protein]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Obstetric/Gynecologic''' | |'''Obstetric/Gynecologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Oncologic''' | |'''Oncologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Opthalmologic''' | |'''Opthalmologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Overdose / Toxicity''' | |'''Overdose / Toxicity''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Psychiatric''' | |'''Psychiatric''' | ||
|bgcolor="Beige"| [[Autistic enterocolitis]] | | bgcolor="Beige" |[[Autistic enterocolitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Pulmonary''' | |'''Pulmonary''' | ||
|bgcolor="Beige"|[[Multiple organ dysfunction syndrome]] | | bgcolor="Beige" |[[Multiple organ dysfunction syndrome]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Renal / Electrolyte''' | |'''Renal / Electrolyte''' | ||
|bgcolor="Beige"|[[Multiple organ dysfunction syndrome]] | | bgcolor="Beige" |[[Multiple organ dysfunction syndrome]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Rheum / Immune / Allergy''' | |'''Rheum / Immune / Allergy''' | ||
|bgcolor="Beige"| [[Ankylosing spondylitis]], [[Behcet disease]], [[common variable immunodeficiency]], [[allergic colitis]] (Food protein-induced colitis), [[scleroderma]], [[vasculitis]], [[Ulcerative colitis]] | | bgcolor="Beige" |[[Ankylosing spondylitis]], [[Behcet disease]], [[common variable immunodeficiency]], [[allergic colitis]] (Food protein-induced colitis), [[scleroderma]], [[vasculitis]], [[Ulcerative colitis]] | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Sexual''' | |'''Sexual''' | ||
|bgcolor="Beige"| Typical [[STI]] such as ''[[Chlamydia trachomatis]]'', ''[[Neisseria gonorrheae]]'', ''[[Treponema pallidum]]'', ''[[Herpes Simplex Virus|HSV]]'', ''[[Cytomegalovirus|CMV]]'', Unusual [[STI]] ''[[Shigella dysenteriae]]'' | | bgcolor="Beige" |Typical [[STI]] such as ''[[Chlamydia trachomatis]]'', ''[[Neisseria gonorrheae]]'', ''[[Treponema pallidum]]'', ''[[Herpes Simplex Virus|HSV]]'', ''[[Cytomegalovirus|CMV]]'', Unusual [[STI]] ''[[Shigella dysenteriae]]''. Proctitis is more common among individuals who have receptive anal exposures (oral-anal, digital-anal, or genital-anal). Genital [[HSV]] and [[Chlamydia]] [[proctitis]] occur predominantly in individuals with HIV infection. [[Neisseria meningitidis]] causes [[proctitis]] among men who have sex with men and individuals with [[HIV infection]].<ref name="pmid28221124">{{cite journal| author=Gutierrez-Fernandez J, Medina V, Hidalgo-Tenorio C, Abad R| title=Two Cases of Neisseria meningitidis Proctitis in HIV-Positive Men Who Have Sex with Men.<nowiki><ref name="pmid24687130"></nowiki>{{cite journal| author=Pallawela SN, Sullivan AK, Macdonald N, French P, White J, Dean G | display-authors=etal| title=Clinical predictors of rectal lymphogranuloma venereum infection: results from a multicentre case-control study in the U.K. | journal=Sex Transm Infect | year= 2014 | volume= 90 | issue= 4 | pages= 269-74 | pmid=24687130 | doi=10.1136/sextrans-2013-051401 | pmc=4033117 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24687130 }} </ref><ref name="pmid28221124">{{cite journal| author=Gutierrez-Fernandez J, Medina V, Hidalgo-Tenorio C, Abad R| title=Two Cases of Neisseria meningitidis Proctitis in HIV-Positive Men Who Have Sex with Men. | journal=Emerg Infect Dis | year= 2017 | volume= 23 | issue= 3 | pages= 542-543 | pmid=28221124 | doi=10.3201/eid2303.161039 | pmc=5382739 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28221124 }} </ref> | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Trauma''' | |'''Trauma''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Urologic''' | |'''Urologic''' | ||
|bgcolor="Beige"| No underlying causes | | bgcolor="Beige" |No underlying causes | ||
|- | |- | ||
|-bgcolor="LightSteelBlue" | |- bgcolor="LightSteelBlue" | ||
| '''Miscellaneous''' | |'''Miscellaneous''' | ||
|bgcolor="Beige"| Microscopic colitis | | bgcolor="Beige" |Microscopic colitis | ||
|- | |- | ||
|} | |} | ||
===Causes in Alphabetical Order=== | ===Causes in Alphabetical Order=== | ||
{{columns-list | {{columns-list| | ||
*[[Aganglionic megacolon]] | *[[Aganglionic megacolon]] | ||
*[[Albinism]] <ref name="pmid19833565">{{cite journal| author=Mohan P, Ramakrishnan MK, Revathy S, Jayanthi V| title=Granulomatous colitis in oculocutaneous albinism. | journal=Dig Liver Dis | year= 2011 | volume= 43 | issue= 1 | pages= e1 | pmid=19833565 | doi=10.1016/j.dld.2009.09.006 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19833565 }} </ref> | *[[Albinism]] <ref name="pmid19833565">{{cite journal| author=Mohan P, Ramakrishnan MK, Revathy S, Jayanthi V| title=Granulomatous colitis in oculocutaneous albinism. | journal=Dig Liver Dis | year= 2011 | volume= 43 | issue= 1 | pages= e1 | pmid=19833565 | doi=10.1016/j.dld.2009.09.006 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19833565 }} </ref> | ||
| Line 453: | Line 468: | ||
===Life Threatening Causes=== | ===Life Threatening Causes=== | ||
Example include toxic megacolon | Example include [[toxic megacolon]], [[ischemic colitis]], [[infectious colitis]] such as [[escherichia coli O157:H7]] and [[shigella]]. | ||
==Screening== | ==Screening== | ||
There is insufficient evidence to recommend routine screening of sexual partners of patients with sexually transmitted enteric pathogens. | |||
==Diagnosis== | |||
== | ===History and Symptoms=== | ||
* | *Symptoms of [[proctitis]] include [[anorectal pain]], [[tenesmus]], or [[rectal]] [[discharge]]. | ||
*Symptoms of [[proctocolitis]] include fatigue, weight loss, [[anorectal pain]], [[tenesmus]], [[rectal]] [[discharge]], [[diarrhea]] or [[abdominal cramps]]. | |||
=== | ===Laboratory Findings=== | ||
Laboratory findings consistent with the diagnosis of proctitis include: | |||
*[[Stool examination]]: Detection of [[blood]] or fecal [[polymorphonuclear leukocytes]] using gram-stained smear of any [[anorectal]] [[exudate]] from anoscopic or anal examination. | |||
*[[Microbiology]] [[workup]]: [[Nucleic acid test|NAAT]] of [[rectal]] lesions for HSV, [[Nucleic acid test|NAAT]] for [[Neisseria gonorrhoeae|Neisseria gonorrhea]], [[syphilis serology]], [[Nucleic acid test|NAAT]] for [[Chlamydia trachomatis]], and [[Nucleic acid test|NAAT]] for [[Mycoplasma genitalium infection|Mycoplasma genitalium]] in case of persistence of symptoms after receiving the recommended treatment. [[CMV]] and other [[Opportunistic infection|opportunistic infections]] may be evaluated in [[Immunosuppression|immunosuppressed]] individuals as [[HIV AIDS|HIV/AIDS]]. | |||
*An elevated [[erythrocyte sedimentation rate]] ([[Erythrocyte sedimentation rate|ESR]]) is one typical finding in the acute exacerbation of [[proctocolitis]]. | |||
=== | ===Other Imaging Findings=== | ||
== | ====Colonoscopy==== | ||
= | [[Anoscopy]] or [[sigmoidoscopy]] may be helpful in the diagnosis of [[proctocolitis]]. Findings on an sigmoidoscopy suggestive of proctocolitis include [[inflammation]] of the colonic mucosa extending to 12 cm above the [[anus]] and [[rectal]] [[Ulcer|ulcers]].<br /> | ||
== | ==Treatment== | ||
=== | ===Medical Therapy=== | ||
Acute [[proctocolitis]] among individuals with receptive anal exposure is often [[sexually-transmitted]]. [[Empiric therapy|Empiric]] [[antibiotic]] treatment should be started while awaiting for the results of laboratory tests for | |||
=== | patients presenting with anorectal [[exudate]] on anoscopy or positive [[Gram staining|Gram]]-stained [[Smear test|smear]] of [[anorectal]] exudate or secretions [[polymorphonuclear leukocytes]] or if anoscopy or Gram stain is not available.<ref name="pmid24275725">{{cite journal| author=Bissessor M, Fairley CK, Read T, Denham I, Bradshaw C, Chen M| title=The etiology of infectious proctitis in men who have sex with men differs according to HIV status. | journal=Sex Transm Dis | year= 2013 | volume= 40 | issue= 10 | pages= 768-70 | pmid=24275725 | doi=10.1097/OLQ.0000000000000022 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24275725 }}</ref> | ||
=== | ====Recommended Regimen for Acute Proctitis==== | ||
'''[[Ceftriaxone]]''' 500 mg IM in a single dose | |||
plus | |||
'''[[Doxycycline]]''' 100 mg orally 2 times/day for 7 days | |||
* | *[[Doxycycline]] course is continued to 100 mg orally 2 times/day for 21 days in case of [[Perianal abscess|perianal]] or [[mucosal]] [[Ulcer|ulcers]], [[Dysentery|bloody]] [[discharge]], or [[tenesmus]] and a positive [[rectal]] [[chlamydia]] test. | ||
*For individuals weighing ≥150 kg, 1 g of [[ceftriaxone]] is given. | |||
* | *Patients presenting with [[mucosal]] or [[Perianal abscess|perianal]] ulcers or [[bloody diarrhea]] with positive [[Nucleic acid test|NAAT]] for [[chlamydia]] should receive [[Empiric therapy|empiric]] therapy for [[Lymphogranuloma venereum|Lymphogranuloma Venereum]] (LGV) with a prolonged course of [[doxycycline]] 100 mg orally 2 times/day for 3 weeks.<ref name="pmid25394161">{{cite journal| author=Mohrmann G, Noah C, Sabranski M, Sahly H, Stellbrink HJ| title=Ongoing epidemic of lymphogranuloma venereum in HIV-positive men who have sex with men: how symptoms should guide treatment. | journal=J Int AIDS Soc | year= 2014 | volume= 17 | issue= 4 Suppl 3 | pages= 19657 | pmid=25394161 | doi=10.7448/IAS.17.4.19657 | pmc=4225278 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25394161 }}</ref> | ||
*Patients presenting with [[painful]] [[Perianal abscess|perianal]] [[Ulcer|ulcers]] or [[mucosal]] [[Ulcer|ulcers]] on anoscopy should also receive [[Empiric therapy|empiric]] treatment for [[genital herpes]]. | |||
*[[Herpes Genitalis|Herpes]] [[proctocolitis]] and [[Lymphogranuloma venereum|LGV]] occur predominantly among [[HIV AIDS|HIV/AIDS]] patients; hence [[Empiric therapy|empiric]] treatment in those patients should cover [[Herpes simplex|genital herpes]] and [[Lymphogranuloma venereum|LGV]]. | |||
===Surgery=== | ===Surgery=== | ||
Surgical intervention is not recommended for the management of [[proctocolitis]]. | |||
== | ==Primary Prevention== | ||
As [[proctocolitis]] can be a sexually transmitted disease, effective measures for the primary prevention of [[proctocolitis]] include: | |||
*[[Counseling]] on safe sex practices | |||
* [[ | *Avoiding contact with feces during [[sexual intercourse]] | ||
* [[ | *Hand washing after handing objects or materials that have been in contact with the [[Anal-oral contact|anal]] area (i.e., sex toys or barriers) and after touching the anal area. | ||
== | ==Secondary Prevention== | ||
Effective measures for the secondary prevention of [[proctocolitis]] include: | |||
*Abstinence from sexual activity until the patient and their partners are successfully treated (i.e., completion of a 7-day regimen and resolution of symptoms) | |||
*Sexual partners with individuals treated for [[Chlamydia infection|chlamydia]] or [[gonorrhea]] <60 days before the onset of symptoms should receive evaluation and empiric treatment of the causative infection | |||
*Testing for other sexually-transmitted diseases | |||
*In case of [[proctocolitis]] caused by [[Chlamydia infection|chlamydia]] or [[Neisseria gonorrhoeae|Neisseria gonorrhea]], retesting for the causative organism is recommended 3 months after completion of treatment. | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[Category:Crowdiagnosis]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category: | [[Category:Up-To-Date]] | ||
Latest revision as of 22:21, 14 August 2021
|
Colitis Microchapters |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: M.Umer Tariq [2]; Maham Khan [3]; Ogheneochuko Ajari, MB.BS, MS [4]; Rim Halaby, M.D. [5]; Qasim Salau, M.B.B.S., FMCPaed [6]; Mohamed Riad, M.D.[7]
Synonyms and keywords: Colitis, Proctocolitis, Proctitis, Enterocolitis.
Overview
Colitis is the inflammation of the colon, that can be either acute or chronic. Colitis may be caused by microorganisms such as Chlamydia trachomatis, Neisseria gonorrhoeae, Shigella dysenteriae, HSV, allergy (food protein-induced allergic proctocolitis), drugs (NSAIDs) and radiation. Colitis may co-exist with enteritis (inflammation of the small bowel), proctitis (inflammation of the rectum) or both. The symptoms of colitis such as diarrhea especially bloody diarrhea and abdominal pain (which may be mild) are seen in all forms of colitis. Colitis may be fulminant with a rapid downhill clinical course. In addition to the diarrhea, fever, and anemia may be reported. The patient with fulminant colitis has severe abdominal pain and presents a clinical picture similar to that of septicemia, where shock is present. Treatment of colitis depends on the etiology. It may include the elimination of cows-milk protein or other food allergens from the diet, administration of antibiotics and general anti-inflammatory medications such as mesalamine or its derivatives, steroids, or one of a number of other drugs that ameliorate inflammation. The mainstay of therapy for infectious colitis is antimicrobial therapy. A common antibiotic regimen in treatment of patients with colitis is a combination of ceftriaxone and doxycycline. Supportive therapies such as correction of dehydration and anemia, and reducing the intake of carbohydrates, lactose products, soft drinks, and caffeine is often done for most patients with colitis. Irritable bowel syndrome (spastic colitis or spastic colon) has been called colitis, causing confusion despite colitis not being a feature of the disease. Immune mediated colitis is the experimental name in animal studies of ulcerative colitis. It is a synonym of ulcerative colitis, but it should not be used as a synonym when referring to ulcerative colitis.
Classification
There is no established classification system for colitis. However, it may be classified based on etiology, age and duration of symptom.
Classification by etiology
| Classes of Colitis | Disorders |
| Autoimmune | |
| Allergic | |
| Infectious colitis |
|
| Idiopathic | |
| Iatrogenic | |
| Vascular | |
| Drug induced | |
| Unclassifiable |
|
Classification by Anatomy
Colitis may co-exist with inflammation involving other parts of the gastrointestinal tract. It can be classified based on anatomy into:
- Proctitis: When it involves the rectum
- Colitis: When it involves the inflammation is limited to the colon
- Proctocolitis: When it involves the rectum and colon (usually the distal part of the colon 12cm to 15cm above the anus (sigmoid colon)[1][2]
- Enterocolitis: When it involves the small intestine in addition to the colon
Schematic of Anatomical Classification of Colitis
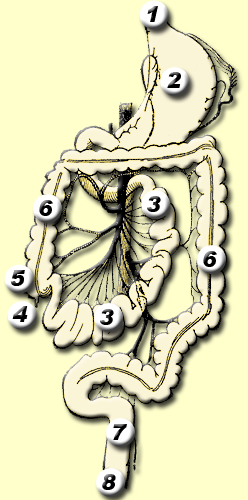
*Regions 4 to 6: Enterocolitis
*Region 6: Colitis
*Regions 6 to 8: Proctocolitis
*Regions 7 to 8:Proctitis
Classification by Age
Classification by duration of symptoms
Differential Diagnosis
The differential diagnosis of colitis can be classified into two categories according to age group. A work up for colitis must include the following differentials:
Differential diagnosis in Infants
- Swallowed maternal blood syndrome
- Anorectal fissure
- Necrotizing enterocolitis especially in preterm babies
- Vitamin K dependent hemorrhage
- Other coagulopathies: (hereditary such as coagulation factor deficiency or acquired such as disseminated intravascular coagulopathy)
- Intussusception
- Upper Gastrointestinal Infections
- Enteritis
- Meckel diverticulum
- Intestinal duplication cysts
- Vascular malformations
- Inflammatory bowel disease(early onset)
- Hirschsprung disease complicated by enterocolitis
- Volvulus
- Gastro-duodenal ulcers
- Gastrointestinal duplication cyst
- Liver disease with clotting factor deficiency
- Lymphonodular hyperplasia
Differential diagnosis in Adults
- Colorectal malignancy
- Crohn's disease
- Behcet's disease
- Arteriovenous malformation
- Diverticulosis
- Enteritis
- Coagulopathy
- Systemic lupus erythematosus(SLE)
- Cytomegalovirus colitis
Differentiating Between Different Types of Colitis
The symptoms of colitis such as diarrhea especially bloody diarrhea and abdominal pain are seen are seen in all forms of colitis. The table below differentiates among the common causes of colitis:[8][9]
| Diseases | History and Symptoms | Physical Examination | Laboratory findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diarrhea | Rectal bleeding | Abdominal pain | Atopy | Dehydration | Fever | Hypotension | Malnutrition | Blood in stool (frank or occult) | Microorganism in stool | Pseudomembranes on endoscopy | ||
| Allergic Colitis | + | ++ | + | ++ | ++ | |||||||
| Chemical colitis | + | ++ | ++ | + | + | ++ | + | |||||
| Infectious colitis | ++ | ++ | ++ | +++ | +++ | ++ | + | ++ | ++ | + | ||
| Radiation colitis | + | ++ | + | + | + | ++ | ||||||
| Ischemic colitis | + | + | ++ | + | + | + | + | ++ | ||||
| Drug-induced colitis | + | + | ++ | + | ++ | + | ||||||
Causes
Common Causes
Common causes of proctocolitis include infectious agents such as Chlamydia trachomatis (which causes lymphogranuloma venereum), Neisseria gonorrhoeae, HSV, Shigella dysenteriae and Campylobacter species. It can also be allergic (e.g. food protein-induced proctocolitis), idiopathic (e.g. microscopic colitis), vascular (e.g. ischemic colitis), or autoimmune (e.g. inflammatory bowel disease).
Causes by Organ System
Causes in Alphabetical Order
- Aganglionic megacolon
- Albinism [11]
- Alosetron
- Alpha 1-antitrypsin deficiency
- Ampicillin Oral
- Ankylosing spondylitis
- Auranofin
- Autistic enterocolitis
- Azithromycin
- Aztreonam Injection
- Bacillary dysentery
- Bacterial gastroenteritis
- Balantidium coli
- Behcet disease
- Campylobacter jejuni
- Cap polyposis
- Cefaclor
- Cefadroxil
- Cefamandole Nafate Injection
- Cefazolin Sodium Injection
- Cefepime
- Cefepime Injection
- Cefoperazone Sodium Injection
- Cefotaxime Sodium Injection
- Cefotetan Disodium Injection
- Cefoxitin Sodium Injection
- Cefpodoxime
- Ceftazidime
- Ceftazidime Injection
- Ceftizoxime Sodium Injection
- Ceftriaxone Sodium Injection
- Cefuroxime Sodium Injection
- Cephalexin
- Cephalosporin
- Cephradine Oral
- Chemical colitis
- Chlamydia trachomatis
- Cidofovir
- Cilansetron
- Clindamycin
- Clostridium difficile [12]
- Co-amoxiclav
- Colitis ulcerosa
- Collagenous colitis
- Colonic ischemia
- Common variable immunodeficiency
- Corticosteroid
- Crohn's disease
- Cryptosporidiosis
- Cytomegalovirus
- Darifenacin
- Dental braces
- Desogestrel and Ethinyl Estradiol
- Dicloxacillin
- Dirithromycin
- Diversion colitis
- Diverticulosis
- Enoxacin
- Entamoeba histolytica
- Ertapenem
- Erythromycin and Sulfisoxazole
- Escherichia coli O157:H7
- EVAR
- Flucytosine
- Gerson diet
- Giardiasis
- Glycopyrrolate
- Hyoscyamine
- Idelalisib
- Imipenem and Cilastatin Sodium Injection
- Infectious colitis
- Inflammatory bowel disease
- Intestinal ischemia
- Ipilimumab
- Irritable bowel syndrome
- Ischemic colitis
- Isosporiasis
- Ixabepilone
- Lanthanum
- Levofloxacin Oral
- Lincomycin hydrochloride
- Linezolid
- Lomefloxacin
- Loracarbef
- Lymphocytic colitis
- Lysinuric protein intolerance
- Methotrexate
- Miconazole Injection
- Microscopic colitis
- Milk allergy
- Moxifloxacin
- Multiple organ dysfunction syndrome
- Nafcillin Sodium Injection
- Neisseria gonorrhoeae
- Neonatal necrotizing enterocolitis
- Nivolumab
- Norfloxacin
- Ofloxacin injection
- Oxacillin Sodium Injection
- Oxcarbazepine
- Oxybutynin
- Peginterferon alfa-2a
- Penicillin
- Pergolide
- Pigbel
- Piperacillin sodium injection
- Pramipexole
- Prednisolone
- Primary sclerosing cholangitis
- Procyclidine
- Propantheline
- Protein losing enteropathy
- Pseudoephedrine
- Pseudomembranous colitis
- Quinolone
- Radiation colitis
- Radiation proctitis
- Ramosetron
- Reserpine
- Salmonella
- Schistosoma
- Scleroderma
- Sepsis
- Shigella
- Solifenacin
- Solitary rectal ulcer syndrome
- Soy protein
- Sparfloxacin
- Strongyloides stercoralis
- Syphilis
- Tegaserod
- Toxic megacolon
- Treponema pallidum
- Typhlitis
- Ulcerative colitis
- Vasculitis
- Yersinia enterocolitica
Life Threatening Causes
Example include toxic megacolon, ischemic colitis, infectious colitis such as escherichia coli O157:H7 and shigella.
Screening
There is insufficient evidence to recommend routine screening of sexual partners of patients with sexually transmitted enteric pathogens.
Diagnosis
History and Symptoms
- Symptoms of proctitis include anorectal pain, tenesmus, or rectal discharge.
- Symptoms of proctocolitis include fatigue, weight loss, anorectal pain, tenesmus, rectal discharge, diarrhea or abdominal cramps.
Laboratory Findings
Laboratory findings consistent with the diagnosis of proctitis include:
- Stool examination: Detection of blood or fecal polymorphonuclear leukocytes using gram-stained smear of any anorectal exudate from anoscopic or anal examination.
- Microbiology workup: NAAT of rectal lesions for HSV, NAAT for Neisseria gonorrhea, syphilis serology, NAAT for Chlamydia trachomatis, and NAAT for Mycoplasma genitalium in case of persistence of symptoms after receiving the recommended treatment. CMV and other opportunistic infections may be evaluated in immunosuppressed individuals as HIV/AIDS.
- An elevated erythrocyte sedimentation rate (ESR) is one typical finding in the acute exacerbation of proctocolitis.
Other Imaging Findings
Colonoscopy
Anoscopy or sigmoidoscopy may be helpful in the diagnosis of proctocolitis. Findings on an sigmoidoscopy suggestive of proctocolitis include inflammation of the colonic mucosa extending to 12 cm above the anus and rectal ulcers.
Treatment
Medical Therapy
Acute proctocolitis among individuals with receptive anal exposure is often sexually-transmitted. Empiric antibiotic treatment should be started while awaiting for the results of laboratory tests for
patients presenting with anorectal exudate on anoscopy or positive Gram-stained smear of anorectal exudate or secretions polymorphonuclear leukocytes or if anoscopy or Gram stain is not available.[13]
Recommended Regimen for Acute Proctitis
Ceftriaxone 500 mg IM in a single dose
plus
Doxycycline 100 mg orally 2 times/day for 7 days
- Doxycycline course is continued to 100 mg orally 2 times/day for 21 days in case of perianal or mucosal ulcers, bloody discharge, or tenesmus and a positive rectal chlamydia test.
- For individuals weighing ≥150 kg, 1 g of ceftriaxone is given.
- Patients presenting with mucosal or perianal ulcers or bloody diarrhea with positive NAAT for chlamydia should receive empiric therapy for Lymphogranuloma Venereum (LGV) with a prolonged course of doxycycline 100 mg orally 2 times/day for 3 weeks.[14]
- Patients presenting with painful perianal ulcers or mucosal ulcers on anoscopy should also receive empiric treatment for genital herpes.
- Herpes proctocolitis and LGV occur predominantly among HIV/AIDS patients; hence empiric treatment in those patients should cover genital herpes and LGV.
Surgery
Surgical intervention is not recommended for the management of proctocolitis.
Primary Prevention
As proctocolitis can be a sexually transmitted disease, effective measures for the primary prevention of proctocolitis include:
- Counseling on safe sex practices
- Avoiding contact with feces during sexual intercourse
- Hand washing after handing objects or materials that have been in contact with the anal area (i.e., sex toys or barriers) and after touching the anal area.
Secondary Prevention
Effective measures for the secondary prevention of proctocolitis include:
- Abstinence from sexual activity until the patient and their partners are successfully treated (i.e., completion of a 7-day regimen and resolution of symptoms)
- Sexual partners with individuals treated for chlamydia or gonorrhea <60 days before the onset of symptoms should receive evaluation and empiric treatment of the causative infection
- Testing for other sexually-transmitted diseases
- In case of proctocolitis caused by chlamydia or Neisseria gonorrhea, retesting for the causative organism is recommended 3 months after completion of treatment.
References
- ↑ 2015 Sexually Transmitted Diseases Treatment Guidelines. Centers for Disease Control and Prevention (2015).http://www.cdc.gov/std/tg2015/proctitis.htm Accessed on August 29, 2016
- ↑ Hamlyn E, Taylor C (2006). "Sexually transmitted proctitis". Postgrad Med J. 82 (973): 733–6. doi:10.1136/pmj.2006.048488. PMC 2660501. PMID 17099092.
- ↑ WikiMedia Commons https://commons.wikimedia.org/wiki/File:Gastro-intestinal_tract.png. Accessed on September 09, 2016
- ↑ Nowak-Węgrzyn A (2015). "Food protein-induced enterocolitis syndrome and allergic proctocolitis". Allergy Asthma Proc. 36 (3): 172–84. doi:10.2500/aap.2015.36.3811. PMC 4405595. PMID 25976434.
- ↑ Pumberger W, Pomberger G, Geissler W (2001). "Proctocolitis in breast fed infants: a contribution to differential diagnosis of haematochezia in early childhood". Postgrad Med J. 77 (906): 252–4. PMC 1741985. PMID 11264489.
- ↑ Alfadda AA, Storr MA, Shaffer EA (2011). "Eosinophilic colitis: epidemiology, clinical features, and current management". Therap Adv Gastroenterol. 4 (5): 301–9. doi:10.1177/1756283X10392443. PMC 3165205. PMID 21922029.
- ↑ 7.0 7.1 Hauer-Jensen M, Denham JW, Andreyev HJ (2014). "Radiation enteropathy--pathogenesis, treatment and prevention". Nat Rev Gastroenterol Hepatol. 11 (8): 470–9. doi:10.1038/nrgastro.2014.46. PMC 4346191. PMID 24686268.
- ↑ Thielman NM, Guerrant RL (2004). "Clinical practice. Acute infectious diarrhea". N Engl J Med. 350 (1): 38–47. doi:10.1056/NEJMcp031534. PMID 14702426.
- ↑ Khan AM, Faruque AS, Hossain MS, Sattar S, Fuchs GJ, Salam MA (2004). "Plesiomonas shigelloides-associated diarrhoea in Bangladeshi children: a hospital-based surveillance study". J Trop Pediatr. 50 (6): 354–6. doi:10.1093/tropej/50.6.354. PMID 15537721.
- ↑ 10.0 10.1 {{cite journal| author=Gutierrez-Fernandez J, Medina V, Hidalgo-Tenorio C, Abad R| title=Two Cases of Neisseria meningitidis Proctitis in HIV-Positive Men Who Have Sex with Men.<ref name="pmid24687130">Pallawela SN, Sullivan AK, Macdonald N, French P, White J, Dean G; et al. (2014). "Clinical predictors of rectal lymphogranuloma venereum infection: results from a multicentre case-control study in the U.K." Sex Transm Infect. 90 (4): 269–74. doi:10.1136/sextrans-2013-051401. PMC 4033117. PMID 24687130.
- ↑ Mohan P, Ramakrishnan MK, Revathy S, Jayanthi V (2011). "Granulomatous colitis in oculocutaneous albinism". Dig Liver Dis. 43 (1): e1. doi:10.1016/j.dld.2009.09.006. PMID 19833565.
- ↑ Gié O, Clerc D, Giulieri S, Demartines N (2014). "[Clostridial colitis: diagnosis and strategies for management]". Rev Med Suisse. 10 (434): 1309–13. PMID 25073304.
- ↑ Bissessor M, Fairley CK, Read T, Denham I, Bradshaw C, Chen M (2013). "The etiology of infectious proctitis in men who have sex with men differs according to HIV status". Sex Transm Dis. 40 (10): 768–70. doi:10.1097/OLQ.0000000000000022. PMID 24275725.
- ↑ Mohrmann G, Noah C, Sabranski M, Sahly H, Stellbrink HJ (2014). "Ongoing epidemic of lymphogranuloma venereum in HIV-positive men who have sex with men: how symptoms should guide treatment". J Int AIDS Soc. 17 (4 Suppl 3): 19657. doi:10.7448/IAS.17.4.19657. PMC 4225278. PMID 25394161.