Fibroma pathophysiology: Difference between revisions
| (93 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Fibroma}} | {{Fibroma}} | ||
{{CMG}}{{AE}}{{Simrat}} | {{CMG}}{{AE}} {{M.N}}, {{Simrat}} | ||
==Overview== | ==Overview== | ||
On gross [[pathology]], [[polypoid]] [[lesion]] which is usually small, are characteristic findings of [[oral fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[fibrous]] [[stroma]], [[collagen]] bundles, prominent [[vessels]], and overlying [[squamous]] [[mucosa]] with [[hyperkeratosis]] and focal [[ulceration]] are characteristic findings of [[oral fibroma]]. On gross [[pathology]], well circumscribed, [[metaphyseal]] [[lesion]], and fragments of white-grey rubbery [[tissue]] are characteristic findings of [[chondromyxoid fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[spindle cells]] or [[Stellate cell|stellate cells]] in a myxoid or chondroid [[stroma]], lobules with hypocellular centers and hypercellular peripheries, [[giant cells]] in a hypercellular periphery, and scattered [[Calcification|calcifications]] are characteristic findings of [[chondromyxoid fibroma]]. On gross [[pathology]], fleshy, [[fibrous]], yellow or tan-brown lesion with variable areas of [[haemorrhage]] are characteristic findings of [[non-ossifying fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[spindle cells]] without [[Cytological|cytologic]] [[atypia]] are arranged in a storiform pattern, scattered [[chronic]] [[inflammatory cells]] and [[benign]] [[giant cells]], [[foam cells]] and [[hemosiderin]] deposition, and [[mitoses]] are characteristic findings of [[non-ossifying fibroma]]. On gross [[pathology]], discrete [[mass]] that is well delineated from surrounding [[bone]], tan-white, rubbery cut surface, firm to gritty and no [[Encapsulation (pharmacology)|encapsulation]] are characteristic findings of [[ossifying fibroma]]. On [[microscopic]] [[histopathological]] analysis, haphazardly distributed lamellated bony [[spicules]] on a background of [[fibrous]] [[stroma]], a zonal architecture with a center of immature [[bone]] surrounded by more mature lamellar [[bone]], and central [[spicules]] of woven bony [[trabeculae]] are lined by a layer of [[osteoblasts]] are characteristic findings of [[ossifying fibroma]].<ref name="librepathology">Fibroma. Libre pathology(2015) http://librepathology.org/wiki/Fibroma Accessed on March 12, 2016</ref><ref name="radio">Fibroma. Radiopedia(2015) http://radiopaedia.org/search?utf8=%E2%9C%93&q=fibroma&scope=all Accessed on March 12, 2016</ref> | On gross [[pathology]], [[polypoid]] [[lesion]] which is usually small, are characteristic findings of [[oral fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[fibrous]] [[stroma]], [[collagen]] bundles, prominent [[vessels]], and overlying [[squamous]] [[mucosa]] with [[hyperkeratosis]] and focal [[ulceration]] are characteristic findings of [[oral fibroma]]. On gross [[pathology]], well circumscribed, [[metaphyseal]] [[lesion]], and fragments of white-grey rubbery [[tissue]] are characteristic findings of [[chondromyxoid fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[spindle cells]] or [[Stellate cell|stellate cells]] in a myxoid or chondroid [[stroma]], lobules with hypocellular centers and hypercellular peripheries, [[giant cells]] in a hypercellular periphery, and scattered [[Calcification|calcifications]] are characteristic findings of [[chondromyxoid fibroma]]. On gross [[pathology]], fleshy, [[fibrous]], yellow or tan-brown lesion with variable areas of [[haemorrhage]] are characteristic findings of [[non-ossifying fibroma]]. On [[microscopic]] [[histopathological]] analysis, [[spindle cells]] without [[Cytological|cytologic]] [[atypia]] are arranged in a storiform pattern, scattered [[chronic]] [[inflammatory cells]] and [[benign]] [[giant cells]], [[foam cells]] and [[hemosiderin]] deposition, and [[mitoses]] are characteristic findings of [[non-ossifying fibroma]]. On gross [[pathology]], discrete [[mass]] that is well delineated from surrounding [[bone]], tan-white, rubbery cut surface, firm to gritty and no [[Encapsulation (pharmacology)|encapsulation]] are characteristic findings of [[ossifying fibroma]]. On [[microscopic]] [[histopathological]] analysis, haphazardly distributed lamellated bony [[spicules]] on a background of [[fibrous]] [[stroma]], a zonal architecture with a center of immature [[bone]] surrounded by more mature lamellar [[bone]], and central [[spicules]] of woven bony [[trabeculae]] are lined by a layer of [[osteoblasts]] are characteristic findings of [[ossifying fibroma]].<ref name="librepathology">Fibroma. Libre pathology(2015) http://librepathology.org/wiki/Fibroma Accessed on March 12, 2016</ref><ref name="radio">Fibroma. Radiopedia(2015) http://radiopaedia.org/search?utf8=%E2%9C%93&q=fibroma&scope=all Accessed on March 12, 2016</ref> | ||
| Line 9: | Line 9: | ||
|+ | |+ | ||
!Type of fibroma | !Type of fibroma | ||
!Location | |||
!Gross pathology | !Gross pathology | ||
!Microscpoic pathology | !Microscpoic pathology | ||
!Genetics | !Genetics and Immunohistochemistry | ||
!Associated conditions | !Associated conditions | ||
|- | |- | ||
|Ovarian Fibroma <ref name="pmid26175813">{{cite journal |vauthors=Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M |title=Large twisted ovarian fibroma in menopausal women: a case report |journal=Pan Afr Med J |volume=20 |issue= |pages=322 |date=2015 |pmid=26175813 |pmc=4491469 |doi=10.11604/pamj.2015.20.322.5998 |url=}}</ref><ref name="pmid27876070">{{cite journal |vauthors=Chen H, Liu Y, Shen LF, Jiang MJ, Yang ZF, Fang GP |title=Ovarian thecoma-fibroma groups: clinical and sonographic features with pathological comparison |journal=J Ovarian Res |volume=9 |issue=1 |pages=81 |date=November 2016 |pmid=27876070 |pmc=5120502 |doi=10.1186/s13048-016-0291-2 |url=}}</ref><ref name="pmid27770806">{{cite journal |vauthors=Matsuda K, Tateishi S, Akazawa Y, Kinoshita A, Yoshida S, Morisaki S, Fukushima A, Matsuwaki T, Yoshiura KI, Nakashima M |title=Rapid growth of mitotically active cellular fibroma of the ovary: a case report and review of the literature |journal=Diagn Pathol |volume=11 |issue=1 |pages=101 |date=October 2016 |pmid=27770806 |doi=10.1186/s13000-016-0554-7 |url=}}</ref><ref name="pmid26437718">{{cite journal |vauthors=Yamada T, Hattori K, Satomi H, Hirose Y, Nakai G, Daimon A, Hayashi A, Terai Y, Ohmichi M, Fukunaga M |title=Mitotically active cellular fibroma of the ovary: a case report and literature review |journal=J Ovarian Res |volume=8 |issue= |pages=65 |date=October 2015 |pmid=26437718 |pmc=4595272 |doi=10.1186/s13048-015-0191-x |url=}}</ref><ref name="pmid25550794">{{cite journal |vauthors=Zong L, Lin M, Fan X |title=Mitotically active cellular fibroma of ovary should be differentiated from fibrosarcoma: a case report and review of literature |journal=Int J Clin Exp Pathol |volume=7 |issue=11 |pages=7578–82 |date=2014 |pmid=25550794 |pmc=4270577 |doi= |url=}}</ref><ref name="pmid27821988">{{cite journal |vauthors=Parwate NS, Patel SM, Arora R, Gupta M |title=Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature |journal=J Obstet Gynaecol India |volume=66 |issue=6 |pages=460–465 |date=December 2016 |pmid=27821988 |pmc=5080219 |doi=10.1007/s13224-015-0717-6 |url=}}</ref><ref name="pmid22691621">{{cite journal |vauthors=Finch T, Pushpanathan C, Brown K, El-Gohary Y |title=Gorlin syndrome presenting with a unilateral ovarian fibroma in a 22-year-old woman: a case report |journal=J Med Case Rep |volume=6 |issue= |pages=148 |date=June 2012 |pmid=22691621 |doi=10.1186/1752-1947-6-148 |url=}}</ref><ref name="pmid24490014">{{cite journal |vauthors=Yazdani S, Alijanpoor A, Sharbatdaran M, Bouzari Z, Abedisamakoosh M, Lakaieandi F, Mohammadpour M |title=Meigs' syndrome with elevated serum CA125 in a case of ovarian fibroma /thecoma |journal=Caspian J Intern Med |volume=5 |issue=1 |pages=43–5 |date=2014 |pmid=24490014 |pmc=3894471 |doi= |url=}}</ref> | |Ovarian Fibroma <ref name="pmid26175813">{{cite journal |vauthors=Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M |title=Large twisted ovarian fibroma in menopausal women: a case report |journal=Pan Afr Med J |volume=20 |issue= |pages=322 |date=2015 |pmid=26175813 |pmc=4491469 |doi=10.11604/pamj.2015.20.322.5998 |url=}}</ref><ref name="pmid27876070">{{cite journal |vauthors=Chen H, Liu Y, Shen LF, Jiang MJ, Yang ZF, Fang GP |title=Ovarian thecoma-fibroma groups: clinical and sonographic features with pathological comparison |journal=J Ovarian Res |volume=9 |issue=1 |pages=81 |date=November 2016 |pmid=27876070 |pmc=5120502 |doi=10.1186/s13048-016-0291-2 |url=}}</ref><ref name="pmid27770806">{{cite journal |vauthors=Matsuda K, Tateishi S, Akazawa Y, Kinoshita A, Yoshida S, Morisaki S, Fukushima A, Matsuwaki T, Yoshiura KI, Nakashima M |title=Rapid growth of mitotically active cellular fibroma of the ovary: a case report and review of the literature |journal=Diagn Pathol |volume=11 |issue=1 |pages=101 |date=October 2016 |pmid=27770806 |doi=10.1186/s13000-016-0554-7 |url=}}</ref><ref name="pmid26437718">{{cite journal |vauthors=Yamada T, Hattori K, Satomi H, Hirose Y, Nakai G, Daimon A, Hayashi A, Terai Y, Ohmichi M, Fukunaga M |title=Mitotically active cellular fibroma of the ovary: a case report and literature review |journal=J Ovarian Res |volume=8 |issue= |pages=65 |date=October 2015 |pmid=26437718 |pmc=4595272 |doi=10.1186/s13048-015-0191-x |url=}}</ref><ref name="pmid25550794">{{cite journal |vauthors=Zong L, Lin M, Fan X |title=Mitotically active cellular fibroma of ovary should be differentiated from fibrosarcoma: a case report and review of literature |journal=Int J Clin Exp Pathol |volume=7 |issue=11 |pages=7578–82 |date=2014 |pmid=25550794 |pmc=4270577 |doi= |url=}}</ref><ref name="pmid27821988">{{cite journal |vauthors=Parwate NS, Patel SM, Arora R, Gupta M |title=Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature |journal=J Obstet Gynaecol India |volume=66 |issue=6 |pages=460–465 |date=December 2016 |pmid=27821988 |pmc=5080219 |doi=10.1007/s13224-015-0717-6 |url=}}</ref><ref name="pmid22691621">{{cite journal |vauthors=Finch T, Pushpanathan C, Brown K, El-Gohary Y |title=Gorlin syndrome presenting with a unilateral ovarian fibroma in a 22-year-old woman: a case report |journal=J Med Case Rep |volume=6 |issue= |pages=148 |date=June 2012 |pmid=22691621 |doi=10.1186/1752-1947-6-148 |url=}}</ref><ref name="pmid24490014">{{cite journal |vauthors=Yazdani S, Alijanpoor A, Sharbatdaran M, Bouzari Z, Abedisamakoosh M, Lakaieandi F, Mohammadpour M |title=Meigs' syndrome with elevated serum CA125 in a case of ovarian fibroma /thecoma |journal=Caspian J Intern Med |volume=5 |issue=1 |pages=43–5 |date=2014 |pmid=24490014 |pmc=3894471 |doi= |url=}}</ref> | ||
| | |||
*[[Ovary]] | |||
| | | | ||
* The [[tumor]] shows [[homogeneous]] and [[solid]] in appearance with a yellowish-white pigment tinge | * The [[tumor]] shows [[homogeneous]] and [[solid]] in appearance with a yellowish-white pigment tinge | ||
| Line 24: | Line 28: | ||
*Absence of significant [[cytological]] [[atypia]] | *Absence of significant [[cytological]] [[atypia]] | ||
| | | | ||
*None | |||
| | | | ||
*[[Ovarian fibromas]] are associated with [[ascites]] in approximately 40% of cases and with [[pleural effusions]] in a small percentage of cases | *[[Ovarian fibromas]] are associated with [[ascites]] in approximately 40% of cases and with [[pleural effusions]] in a small percentage of cases | ||
| Line 29: | Line 34: | ||
*Fibromas are seen in approximately 75% of [[patients]] with [[Nevoid Basal Cell Carcinoma Syndrome|nevoid basal cell carcinoma syndrome]] ([[Gorlin syndrome]]) | *Fibromas are seen in approximately 75% of [[patients]] with [[Nevoid Basal Cell Carcinoma Syndrome|nevoid basal cell carcinoma syndrome]] ([[Gorlin syndrome]]) | ||
|- | |- | ||
|Oral Fibroma | |Oral Fibroma <ref name="pmid26448815">{{cite journal |vauthors=Panta P |title=Traumatic fibroma |journal=Pan Afr Med J |volume=21 |issue= |pages=220 |date=2015 |pmid=26448815 |pmc=4587079 |doi=10.11604/pamj.2015.21.220.7498 |url=}}</ref><ref name="pmid8035060">{{cite journal |vauthors=Christopoulos P, Sklavounou A, Patrikiou A |title=True fibroma of the oral mucosa: a case report |journal=Int J Oral Maxillofac Surg |volume=23 |issue=2 |pages=98–9 |date=April 1994 |pmid=8035060 |doi= |url=}}</ref><ref name="pmid26958126">{{cite journal |vauthors=Krishnan V, Shunmugavelu K |title=A clinical challenging situation of intra oral fibroma mimicking pyogenic granuloma |journal=Pan Afr Med J |volume=22 |issue= |pages=263 |date=2015 |pmid=26958126 |pmc=4765330 |doi=10.11604/pamj.2015.22.263.8080 |url=}}</ref> | ||
| | |||
*[[Buccal mucosa]] | |||
| | | | ||
* A round-to-ovoid [[polypoid]] lesion, smooth-surfaced, and firm [[sessile]] or pedunculated [[Mass (medicine)|mass]] | * A round-to-ovoid [[polypoid]] lesion, smooth-surfaced, and firm [[sessile]] or pedunculated [[Mass (medicine)|mass]] | ||
| Line 37: | Line 44: | ||
* Known for repeated [[trauma]] | * Known for repeated [[trauma]] | ||
| | | | ||
*Histologically similar to fibrous papule | *[[Histologically]] similar to [[fibrous]] [[papule]] | ||
*Fibrous stroma is a key feature | *[[Fibrous]] [[stroma]] is a key feature | ||
*Collagen bundles may be present | *[[Collagen]] bundles may be present | ||
| | | | ||
*None | |||
| | | | ||
* Multiple oral fibromas may be seen in Cowden disease | * Multiple oral fibromas may be seen in [[Cowden disease]] | ||
|- | |- | ||
|Chondromyxoid fibroma | |Chondromyxoid fibroma <ref name="pmid17907440">{{cite journal |vauthors=Takenaga RK, Frassica FJ, McCarthy EF |title=Subperiosteal chondromyxoid fibroma: a report of two cases |journal=Iowa Orthop J |volume=27 |issue= |pages=104–7 |date=2007 |pmid=17907440 |pmc=2150655 |doi= |url=}}</ref><ref name="pmid16547720">{{cite journal |vauthors=Sharma H, Jane MJ, Reid R |title=Chondromyxoid fibroma of the foot and ankle: 40 years' Scottish bone tumour registry experience |journal=Int Orthop |volume=30 |issue=3 |pages=205–9 |date=June 2006 |pmid=16547720 |pmc=2532097 |doi=10.1007/s00264-005-0046-y |url=}}</ref><ref name="pmid19648885">{{cite journal |vauthors=Yasuda T, Nishio J, Sumegi J, Kapels KM, Althof PA, Sawyer JR, Reith JD, Bridge JA |title=Aberrations of 6q13 mapped to the COL12A1 locus in chondromyxoid fibroma |journal=Mod. Pathol. |volume=22 |issue=11 |pages=1499–506 |date=November 2009 |pmid=19648885 |doi=10.1038/modpathol.2009.101 |url=}}</ref><ref name="pmid22043162">{{cite journal |vauthors=Choi YS, Kim BS, Joo JE, Park YK, Lee SH, Song BY |title=A rare case of epiphyseal chondromyxoid fibroma of the proximal tibia |journal=Korean J Radiol |volume=12 |issue=6 |pages=761–4 |date=2011 |pmid=22043162 |pmc=3194784 |doi=10.3348/kjr.2011.12.6.761 |url=}}</ref><ref name="pmid22094389">{{cite journal |vauthors=Gutiérrez-González R, De Reina L, Saab A, Jiménez-Heffernan J, García-Uría J |title=Chondromyxoid fibroma of the lumbar spine: case report and literature review |journal=Eur Spine J |volume=21 Suppl 4 |issue= |pages=S458–62 |date=June 2012 |pmid=22094389 |doi=10.1007/s00586-011-2078-x |url=}}</ref><ref name="pmid19644549">{{cite journal |vauthors=Morris LG, Rihani J, Lebowitz RA, Wang BY |title=Chondromyxoid fibroma of sphenoid sinus with unusual calcifications: case report with literature review |journal=Head Neck Pathol |volume=3 |issue=2 |pages=169–73 |date=June 2009 |pmid=19644549 |doi=10.1007/s12105-009-0121-6 |url=}}</ref><ref name="pmid27274412">{{cite journal |vauthors=Minasian T, Claus C, Hariri OR, Piao Z, Quadri SA, Yuhan R, Leong D, Tashjian V |title=Chondromyxoid fibroma of the sacrum: A case report and literature review |journal=Surg Neurol Int |volume=7 |issue=Suppl 13 |pages=S370–4 |date=2016 |pmid=27274412 |pmc=4879845 |doi=10.4103/2152-7806.182547 |url=}}</ref><ref name="pmid26413029">{{cite journal |vauthors=Kilic D, Findikcioglu A, Tepeoglu M, Vural C |title=Chondromyxoid Fibroma of the Sternum in a 63-Year-Old Woman |journal=Tex Heart Inst J |volume=42 |issue=4 |pages=400–2 |date=August 2015 |pmid=26413029 |pmc=4567104 |doi=10.14503/THIJ-14-4381 |url=}}</ref><ref name="pmid24987604">{{cite journal |vauthors=Fomete B, Adeosun OO, Awelimobor DI, Olayemi L |title=Chondromyxoid fibroma of the mandible: Case report and review of the literature |journal=Ann Maxillofac Surg |volume=4 |issue=1 |pages=78–80 |date=January 2014 |pmid=24987604 |pmc=4073468 |doi=10.4103/2231-0746.133072 |url=}}</ref> | ||
| | |||
* Proximal [[tibia]] [[metaphysis]] | |||
*Distal [[femoral]] [[metaphysis]] | |||
| | | | ||
* Well circumscribed, metaphyseal lesion, and fragments of white-grey rubbery tissue are noted | * Well circumscribed, [[metaphyseal]] lesion, and fragments of white-grey rubbery tissue are noted | ||
| | | | ||
*[[Spindle cells]] or stellate cells in a myxoid or chondroid stroma | *[[Spindle cells]] or [[Stellate cell|stellate cells]] in a myxoid or chondroid [[stroma]] | ||
*Lobules with hypocellular centers and hypercellular peripheries | *Lobules with hypocellular centers and hypercellular peripheries | ||
*Giant cells in the hypercellular periphery | *[[Giant cells]] in the hypercellular periphery | ||
*Scattered calcifications. | *Scattered [[Calcification|calcifications]]. | ||
*No true hyaline cartilage formation is seen | *No true [[hyaline cartilage]] formation is seen | ||
*No mitotic activity is seen | *No [[Mitotic index|mitotic activity]] is seen | ||
| | | | ||
* ''GRM1'' gene fusion or promoter swapping noted | * ''GRM1'' [[gene fusion]] or [[Promoter region|promoter]] swapping noted | ||
* It can be associated with a translocation at t(1;5)(p13;p13) | * It can be associated with a [[translocation]] at t(1;5)(p13;p13) | ||
| | | | ||
*None | |||
|- | |- | ||
|Uterine fibroma <ref name="pmid27974911">{{cite journal |vauthors=Manta L, Suciu N, Toader O, Purcărea RM, Constantin A, Popa F |title=The etiopathogenesis of uterine fibromatosis |journal=J Med Life |volume=9 |issue=1 |pages=39–45 |date=2016 |pmid=27974911 |pmc=5152611 |doi= |url=}}</ref><ref name="pmid25879625">{{cite journal |vauthors=Borahay MA, Al-Hendy A, Kilic GS, Boehning D |title=Signaling Pathways in Leiomyoma: Understanding Pathobiology and Implications for Therapy |journal=Mol. Med. |volume=21 |issue= |pages=242–56 |date=April 2015 |pmid=25879625 |pmc=4503645 |doi=10.2119/molmed.2014.00053 |url=}}</ref><ref name="pmid27454940">{{cite journal |vauthors=Miettinen M, Felisiak-Golabek A, Wasag B, Chmara M, Wang Z, Butzow R, Lasota J |title=Fumarase-deficient Uterine Leiomyomas: An Immunohistochemical, Molecular Genetic, and Clinicopathologic Study of 86 Cases |journal=Am. J. Surg. Pathol. |volume=40 |issue=12 |pages=1661–1669 |date=December 2016 |pmid=27454940 |pmc=5106328 |doi=10.1097/PAS.0000000000000703 |url=}}</ref><ref name="pmid26141720">{{cite journal |vauthors=Commandeur AE, Styer AK, Teixeira JM |title=Epidemiological and genetic clues for molecular mechanisms involved in uterine leiomyoma development and growth |journal=Hum. Reprod. Update |volume=21 |issue=5 |pages=593–615 |date=2015 |pmid=26141720 |pmc=4533663 |doi=10.1093/humupd/dmv030 |url=}}</ref><ref name="pmid12826476">{{cite journal |vauthors=Flake GP, Andersen J, Dixon D |title=Etiology and pathogenesis of uterine leiomyomas: a review |journal=Environ. Health Perspect. |volume=111 |issue=8 |pages=1037–54 |date=June 2003 |pmid=12826476 |pmc=1241553 |doi=10.1289/ehp.5787 |url=}}</ref><ref name="pmid16504804">{{cite journal |vauthors=Lobel MK, Somasundaram P, Morton CC |title=The genetic heterogeneity of uterine leiomyomata |journal=Obstet. Gynecol. Clin. North Am. |volume=33 |issue=1 |pages=13–39 |date=March 2006 |pmid=16504804 |doi=10.1016/j.ogc.2005.12.006 |url=}}</ref><ref name="pmid16564125">{{cite journal |vauthors=Wolańska M, Bańkowski E |title=Transforming growth factor beta and platelet-derived growth factor in human myometrium and in uterine leiomyomas at various stages of tumour growth |journal=Eur. J. Obstet. Gynecol. Reprod. Biol. |volume=130 |issue=2 |pages=238–44 |date=February 2007 |pmid=16564125 |doi=10.1016/j.ejogrb.2006.01.034 |url=}}</ref><ref name="pmid16443507">{{cite journal |vauthors=Baird DD, Kesner JS, Dunson DB |title=Luteinizing hormone in premenopausal women may stimulate uterine leiomyomata development |journal=J. Soc. Gynecol. Investig. |volume=13 |issue=2 |pages=130–5 |date=February 2006 |pmid=16443507 |doi=10.1016/j.jsgi.2005.12.001 |url=}}</ref><ref name="pmid8885057">{{cite journal |vauthors=Andersen J |title=Growth factors and cytokines in uterine leiomyomas |journal=Semin. Reprod. Endocrinol. |volume=14 |issue=3 |pages=269–82 |date=August 1996 |pmid=8885057 |doi=10.1055/s-2007-1016336 |url=}}</ref><ref name="pmid28875276">{{cite journal |vauthors=Laganà AS, Vergara D, Favilli A, La Rosa VL, Tinelli A, Gerli S, Noventa M, Vitagliano A, Triolo O, Rapisarda AMC, Vitale SG |title=Epigenetic and genetic landscape of uterine leiomyomas: a current view over a common gynecological disease |journal=Arch. Gynecol. Obstet. |volume=296 |issue=5 |pages=855–867 |date=November 2017 |pmid=28875276 |doi=10.1007/s00404-017-4515-5 |url=}}</ref><ref name="pmid1323302">{{cite journal |vauthors=Koutsilieris M |title=Pathophysiology of uterine leiomyomas |journal=Biochem. Cell Biol. |volume=70 |issue=5 |pages=273–8 |date=May 1992 |pmid=1323302 |doi= |url=}}</ref> | |Uterine fibroma <ref name="pmid27974911">{{cite journal |vauthors=Manta L, Suciu N, Toader O, Purcărea RM, Constantin A, Popa F |title=The etiopathogenesis of uterine fibromatosis |journal=J Med Life |volume=9 |issue=1 |pages=39–45 |date=2016 |pmid=27974911 |pmc=5152611 |doi= |url=}}</ref><ref name="pmid25879625">{{cite journal |vauthors=Borahay MA, Al-Hendy A, Kilic GS, Boehning D |title=Signaling Pathways in Leiomyoma: Understanding Pathobiology and Implications for Therapy |journal=Mol. Med. |volume=21 |issue= |pages=242–56 |date=April 2015 |pmid=25879625 |pmc=4503645 |doi=10.2119/molmed.2014.00053 |url=}}</ref><ref name="pmid27454940">{{cite journal |vauthors=Miettinen M, Felisiak-Golabek A, Wasag B, Chmara M, Wang Z, Butzow R, Lasota J |title=Fumarase-deficient Uterine Leiomyomas: An Immunohistochemical, Molecular Genetic, and Clinicopathologic Study of 86 Cases |journal=Am. J. Surg. Pathol. |volume=40 |issue=12 |pages=1661–1669 |date=December 2016 |pmid=27454940 |pmc=5106328 |doi=10.1097/PAS.0000000000000703 |url=}}</ref><ref name="pmid26141720">{{cite journal |vauthors=Commandeur AE, Styer AK, Teixeira JM |title=Epidemiological and genetic clues for molecular mechanisms involved in uterine leiomyoma development and growth |journal=Hum. Reprod. Update |volume=21 |issue=5 |pages=593–615 |date=2015 |pmid=26141720 |pmc=4533663 |doi=10.1093/humupd/dmv030 |url=}}</ref><ref name="pmid12826476">{{cite journal |vauthors=Flake GP, Andersen J, Dixon D |title=Etiology and pathogenesis of uterine leiomyomas: a review |journal=Environ. Health Perspect. |volume=111 |issue=8 |pages=1037–54 |date=June 2003 |pmid=12826476 |pmc=1241553 |doi=10.1289/ehp.5787 |url=}}</ref><ref name="pmid16504804">{{cite journal |vauthors=Lobel MK, Somasundaram P, Morton CC |title=The genetic heterogeneity of uterine leiomyomata |journal=Obstet. Gynecol. Clin. North Am. |volume=33 |issue=1 |pages=13–39 |date=March 2006 |pmid=16504804 |doi=10.1016/j.ogc.2005.12.006 |url=}}</ref><ref name="pmid16564125">{{cite journal |vauthors=Wolańska M, Bańkowski E |title=Transforming growth factor beta and platelet-derived growth factor in human myometrium and in uterine leiomyomas at various stages of tumour growth |journal=Eur. J. Obstet. Gynecol. Reprod. Biol. |volume=130 |issue=2 |pages=238–44 |date=February 2007 |pmid=16564125 |doi=10.1016/j.ejogrb.2006.01.034 |url=}}</ref><ref name="pmid16443507">{{cite journal |vauthors=Baird DD, Kesner JS, Dunson DB |title=Luteinizing hormone in premenopausal women may stimulate uterine leiomyomata development |journal=J. Soc. Gynecol. Investig. |volume=13 |issue=2 |pages=130–5 |date=February 2006 |pmid=16443507 |doi=10.1016/j.jsgi.2005.12.001 |url=}}</ref><ref name="pmid8885057">{{cite journal |vauthors=Andersen J |title=Growth factors and cytokines in uterine leiomyomas |journal=Semin. Reprod. Endocrinol. |volume=14 |issue=3 |pages=269–82 |date=August 1996 |pmid=8885057 |doi=10.1055/s-2007-1016336 |url=}}</ref><ref name="pmid28875276">{{cite journal |vauthors=Laganà AS, Vergara D, Favilli A, La Rosa VL, Tinelli A, Gerli S, Noventa M, Vitagliano A, Triolo O, Rapisarda AMC, Vitale SG |title=Epigenetic and genetic landscape of uterine leiomyomas: a current view over a common gynecological disease |journal=Arch. Gynecol. Obstet. |volume=296 |issue=5 |pages=855–867 |date=November 2017 |pmid=28875276 |doi=10.1007/s00404-017-4515-5 |url=}}</ref><ref name="pmid1323302">{{cite journal |vauthors=Koutsilieris M |title=Pathophysiology of uterine leiomyomas |journal=Biochem. Cell Biol. |volume=70 |issue=5 |pages=273–8 |date=May 1992 |pmid=1323302 |doi= |url=}}</ref> | ||
| | |||
* Intra-uterine: | |||
* Intramural [[leiomyoma]] | |||
*Subserosal [[leiomyoma]] | |||
*[[Submucosal]] [[leiomyoma]] | |||
* Extra-uterine: | |||
* [[Broad ligament]] [[leiomyoma]] | |||
*[[Cervical]] [[leiomyoma]] | |||
*[[Parasitic]] [[leiomyoma]] | |||
*Diffuse [[uterine]] [[leiomyomatosis]] | |||
| | | | ||
* Round, well circumscribed (but not encapsulated), [[solid]] [[nodules]] that are white or tan, and show whorled appearance | * Round, well circumscribed (but not encapsulated), [[solid]] [[nodules]] that are white or tan, and show whorled appearance | ||
| Line 73: | Line 96: | ||
* When multiple [[fibroids]] are present they frequently have unrelated [[genetic defects]]. Specific mutations of the ''[[MED12]]'' protein have been noted in 70% of [[fibroids]]. | * When multiple [[fibroids]] are present they frequently have unrelated [[genetic defects]]. Specific mutations of the ''[[MED12]]'' protein have been noted in 70% of [[fibroids]]. | ||
* If a mother had [[fibroids]], risk in the daughter is about three times higher than average. Researchers have found that only a few specific [[genes]] or [[cytogenetic]] deviations are associated with [[Leiomyoma|uterine leiomyomas]]. An association with [[fatty acid synthase]] has been reported. | * If a mother had [[fibroids]], risk in the daughter is about three times higher than average. Researchers have found that only a few specific [[genes]] or [[cytogenetic]] deviations are associated with [[Leiomyoma|uterine leiomyomas]]. An association with [[fatty acid synthase]] has been reported. | ||
*[[CD10]] positive | |||
*[[SMA]] positive | |||
*[[Desmin]] positive | |||
*H-caldesmon positive | |||
*[[p16]] negative | |||
*[[Ki-67]] negative | |||
| | | | ||
* A syndrome (Reed's syndrome) that causes uterine leiomyomata along with cutaneous leiomyomata and [[renal cell cancer]] has been reported. | * A syndrome (Reed's syndrome) that causes uterine leiomyomata along with cutaneous leiomyomata and [[renal cell cancer]] has been reported. | ||
* This is associated with a [[mutation]] in the [[gene]] that produces the [[enzyme]] [[fumarate hydratase]], located on the long arm of [[Chromosome 1|chromosome]] 1 (''1q42.3-43''). Inheritance is [[autosomal dominant]]. | * This is associated with a [[mutation]] in the [[gene]] that produces the [[enzyme]] [[fumarate hydratase]], located on the long arm of [[Chromosome 1|chromosome]] 1 (''1q42.3-43''). Inheritance is [[autosomal dominant]]. | ||
|- | |- | ||
|Ossifying Fibroma | |Ossifying Fibroma <ref name="pmid24678936">{{cite journal |vauthors=Wang TT, Zhang R, Wang L, Chen Y, Dong Q, Li TJ |title=Two cases of multiple ossifying fibromas in the jaws |journal=Diagn Pathol |volume=9 |issue= |pages=75 |date=March 2014 |pmid=24678936 |pmc=3974450 |doi=10.1186/1746-1596-9-75 |url=}}</ref><ref name="pmid27658992">{{cite journal |vauthors=Chen Y, Hu DY, Wang TT, Zhang R, Dong Q, Xu ZX, Wang L, Li TJ |title=CDC73 gene mutations in sporadic ossifying fibroma of the jaws |journal=Diagn Pathol |volume=11 |issue=1 |pages=91 |date=September 2016 |pmid=27658992 |pmc=5034632 |doi=10.1186/s13000-016-0532-0 |url=}}</ref><ref name="pmid24431886">{{cite journal |vauthors=Maria A, Sharma Y, Malik M |title=Juvenile ossifying fibroma of mandible: a case report |journal=J Maxillofac Oral Surg |volume=12 |issue=4 |pages=447–50 |date=December 2013 |pmid=24431886 |doi=10.1007/s12663-010-0122-8 |url=}}</ref><ref name="pmid29373206">{{cite journal |vauthors=Alghonaim Y, ALRashed ALHumaid S, Arafat A |title=Aggressive ossifying fibroma of right ethmoidal sinus: A case report |journal=Int J Surg Case Rep |volume=53 |issue= |pages=513–516 |date=2018 |pmid=29373206 |pmc=6290393 |doi=10.1016/j.ijscr.2017.12.026 |url=}}</ref><ref name="pmid29151945">{{cite journal |vauthors=Liu Y, Shan XF, Guo XS, Xie S, Cai ZG |title=Clinicopathological Characteristics and Prognosis of Ossifying Fibroma in the Jaws of Children: A Retrospective Study |journal=J Cancer |volume=8 |issue=17 |pages=3592–3597 |date=2017 |pmid=29151945 |pmc=5687175 |doi=10.7150/jca.21556 |url=}}</ref><ref name="pmid28381325">{{cite journal |vauthors=Liu JJ, Thompson LD, Janisiewicz AM, Shibuya TY, Keschner DB, Garg R, Lee JT |title=Ossifying fibroma of the maxilla and sinonasal tract: Case series |journal=Allergy Rhinol (Providence) |volume=8 |issue=1 |pages=32–36 |date=March 2017 |pmid=28381325 |pmc=5380450 |doi=10.2500/ar.2017.8.0190 |url=}}</ref><ref name="pmid25738089">{{cite journal |vauthors=Misra SR, Saigal A, Rastogi V, Priyadarshini SR, Pati AR |title=Giant central ossifying fibroma of the maxilla presenting with a pus discharging intra-oral sinus |journal=J Clin Diagn Res |volume=9 |issue=1 |pages=ZD08–11 |date=January 2015 |pmid=25738089 |pmc=4347180 |doi=10.7860/JCDR/2015/11192.5417 |url=}}</ref> | ||
| | |||
*[[Tibia]]: predilection for the cortex of the tibial [[diaphysis]]. | |||
*[[Femur]] | |||
| | | | ||
* Discrete mass that is well delineated from surrounding bone, tan-white, rubbery cut surface, firm to gritty and no encapsulation | * Discrete [[mass]] that is well delineated from surrounding [[bone]], tan-white, rubbery cut surface, firm to gritty and no [[Encapsulation (pharmacology)|encapsulation]] | ||
| | | | ||
* They comprise of haphazardly distributed lamellated bony spicules on a background of fibrous stroma | * They comprise of haphazardly distributed lamellated bony spicules on a background of [[fibrous]] [[stroma]] | ||
* The lesion has a zonal architecture with a center of immature bone surrounded by more mature lamellar bone. | * The lesion has a zonal architecture with a center of immature [[bone]] surrounded by more mature lamellar bone. | ||
* The central spicules of woven bony trabeculae are lined by a layer of osteoblasts. The background is a loose and storiform fibrous tissue. | * The central spicules of woven bony [[trabeculae]] are lined by a layer of [[osteoblasts]]. The background is a loose and storiform [[fibrous tissue]]. | ||
| | | | ||
*[[Ossifying fibromas]] are [[keratin]] positive - isolated cells accepted by some. | |||
*It is [[osteonectin]], [[neurofibromin]], and [[S-100]] protein positive. | |||
| | | | ||
* Clonal chromosomal abnormalities such as trisomies of [[chromosomes]] 7, 8, 12 ,21, and/or 22 | * Clonal [[chromosomal abnormalities]] such as [[trisomies]] of [[chromosomes]] 7, 8, 12 ,21, and/or 22 | ||
* [[Adamantinoma]] | * [[Adamantinoma]] | ||
|- | |- | ||
|Non-ossifying Fibroma | |Non-ossifying Fibroma <ref name="pmid23008139">{{cite journal |vauthors=Bowers LM, Cohen DM, Bhattacharyya I, Pettigrew JC, Stavropoulos MF |title=The non-ossifying fibroma: a case report and review of the literature |journal=Head Neck Pathol |volume=7 |issue=2 |pages=203–10 |date=June 2013 |pmid=23008139 |doi=10.1007/s12105-012-0399-7 |url=}}</ref><ref name="pmid27044378">{{cite journal |vauthors=Herget GW, Mauer D, Krauß T, El Tayeh A, Uhl M, Südkamp NP, Hauschild O |title=Non-ossifying fibroma: natural history with an emphasis on a stage-related growth, fracture risk and the need for follow-up |journal=BMC Musculoskelet Disord |volume=17 |issue= |pages=147 |date=April 2016 |pmid=27044378 |pmc=4820930 |doi=10.1186/s12891-016-1004-0 |url=}}</ref><ref name="pmid29081852">{{cite journal |vauthors=Goldin A, Muzykewicz DA, Dwek J, Mubarak SJ |title=The aetiology of the non-ossifying fibroma of the distal femur and its relationship to the surrounding soft tissues |journal=J Child Orthop |volume=11 |issue=5 |pages=373–379 |date=October 2017 |pmid=29081852 |pmc=5643931 |doi=10.1302/1863-2548.11.170068 |url=}}</ref> | ||
| | |||
*[[Metaphysis]] of distal [[femur]] or proximal [[tibia]] (80%) | |||
*Cortical | |||
| | | | ||
* Fleshy, fibrous, yellow or tan-brown lesion with variable areas of haemorrhage are noted | * Fleshy, [[fibrous]], yellow or tan-brown lesion with variable areas of [[haemorrhage]] are noted | ||
| | | | ||
* [[Spindle cells]] without cytologic atypia are arranged in a storiform pattern. | * [[Spindle cells]] without [[Cytological|cytologic]] [[atypia]] are arranged in a storiform pattern. | ||
* Scattered chronic inflammatory cells and benign giant cells. | * Scattered chronic [[inflammatory cells]] and [[benign]] [[giant cells]]. | ||
* Foam cells and hemosiderin deposition are present. | *[[Foam cells]] and [[hemosiderin]] deposition are present. | ||
* Mitoses are seen but cytologic atypia is absent. | *[[Mitoses]] are seen but [[Cytological|cytologic]] [[atypia]] is absent. | ||
| | | | ||
* Clonal rearrangements in chromosomes 1, 3, 4, 11, and 14 are noted in NOFs (non-ossifying fibroma) of bone | * Clonal rearrangements in [[chromosomes]] 1, 3, 4, 11, and 14 are noted in NOFs (non-ossifying fibroma) of bone | ||
| | | | ||
* Neurofibromatosis-type 1 (NF1) | *[[Neurofibromatosis type I|Neurofibromatosis-type 1]] (NF1) | ||
* [[Fibrous dysplasia]] | * [[Fibrous dysplasia]] | ||
* [[Jaffe-Campanacci syndrome]] | * [[Jaffe-Campanacci syndrome]] | ||
|- | |- | ||
|Desmoplastic Fibroma | |Desmoplastic Fibroma <ref name="pmid19930688">{{cite journal |vauthors=Schneider M, Zimmermann AC, Depprich RA, Kübler NR, Engers R, Naujoks CD, Handschel J |title=Desmoplastic fibroma of the mandible--review of the literature and presentation of a rare case |journal=Head Face Med |volume=5 |issue= |pages=25 |date=November 2009 |pmid=19930688 |doi=10.1186/1746-160X-5-25 |url=}}</ref><ref name="pmid23459513">{{cite journal |vauthors=Nedopil A, Raab P, Rudert M |title=Desmoplastic fibroma: a case report with three years of clinical and radiographic observation and review of the literature |journal=Open Orthop J |volume=8 |issue= |pages=40–6 |date=2013 |pmid=23459513 |doi=10.2174/1874325001307010040 |url=}}</ref><ref name="pmid26622872">{{cite journal |vauthors=Gong YB, Qu LM, Qi X, Liu JG |title=Desmoplastic fibroma in the proximal femur: A case report with long-term follow-up |journal=Oncol Lett |volume=10 |issue=4 |pages=2465–2467 |date=October 2015 |pmid=26622872 |doi=10.3892/ol.2015.3603 |url=}}</ref><ref name="pmid15937674">{{cite journal |vauthors=Daneyemez M, Akay KM, Izci Y |title=Desmoplastic fibroma of the cervical spine |journal=Eur Spine J |volume=14 |issue=8 |pages=799–802 |date=October 2005 |pmid=15937674 |doi=10.1007/s00586-005-0904-8 |url=}}</ref><ref name="pmid25113037">{{cite journal |vauthors=Woods TR, Cohen DM, Islam MN, Rawal Y, Bhattacharyya I |title=Desmoplastic fibroma of the mandible: a series of three cases and review of literature |journal=Head Neck Pathol |volume=9 |issue=2 |pages=196–204 |date=June 2015 |pmid=25113037 |doi=10.1007/s12105-014-0561-5 |url=}}</ref><ref name="pmid23682186">{{cite journal |vauthors=Goyal T, Rastogi S, Tripathy SK |title=Desmoplastic fibroma of ulna: Excision and reconstruction of olecranon with a fibular graft |journal=Indian J Orthop |volume=47 |issue=2 |pages=207–10 |date=March 2013 |pmid=23682186 |pmc=3654474 |doi=10.4103/0019-5413.108928 |url=}}</ref><ref name="pmid26909301">{{cite journal |vauthors=Evans S, Ramasamy A, Jeys L, Grimer R |title=Desmoplastic fibroma of bone: A rare bone tumour |journal=J Bone Oncol |volume=3 |issue=3-4 |pages=77–9 |date=November 2014 |pmid=26909301 |pmc=4723648 |doi=10.1016/j.jbo.2014.08.001 |url=}}</ref> | ||
| | |||
*[[Mandible]] (22%) and the [[metaphysis]] of long bones (56%). | |||
*[[Pelvis]] | |||
| | | | ||
| | | | ||
* Lamellar bone | * Lamellar bone | ||
* Fibrotic marrow space has following features: | * Fibrotic [[marrow]] space has following features: | ||
** Collagen | **[[Collagen]] | ||
** Low cellularity | ** Low cellularity | ||
** Spindle cells without significant atypia | **[[Spindle cells]] without significant [[atypia]] | ||
* On histopathology, desmoplastic fibromas are identical to soft tissue desmoid tumors, with abundant collagenous stroma and little cellularity or pleomorphism. | * On [[histopathology]], desmoplastic fibromas are identical to soft tissue [[Desmoid tumor|desmoid tumors]], with abundant [[collagenous]] [[stroma]] and little cellularity or [[pleomorphism]]. | ||
* The main cell types that are seen include the following: | * The main cell types that are seen include the following: | ||
** [[Fibroblasts]] | ** [[Fibroblasts]] | ||
| Line 120: | Line 160: | ||
** Undifferentiated mesenchymal cells | ** Undifferentiated mesenchymal cells | ||
| | | | ||
*Strong positive for the adhesion protein β-[[Catenin]] | |||
*Weak positive labelling for [[S-100]] | |||
*No positive stain for the proliferation marker [[Ki67]] | |||
| | | | ||
* No associated conditions | * No associated conditions | ||
|- | |- | ||
|Pleural Fibroma | |Pleural Fibroma <ref name="pmid23503999">{{cite journal |vauthors=Aremu AA, Oyedeji OA, Asaleye CM, Adetiloye VA |title=An elusive chest coin in an African child: a pleural fibroma's long, tortuous path to freedom |journal=Pan Afr Med J |volume=14 |issue= |pages=16 |date=2013 |pmid=23503999 |pmc=3597858 |doi=10.11604/pamj.2013.14.16.1874 |url=}}</ref><ref name="pmid25878653">{{cite journal |vauthors=Hassan S, Husain SS, Anwar MA, Saeed S |title=Pleural Fibroma; A meandering path to surgical removal |journal=Pak J Med Sci |volume=31 |issue=1 |pages=236–8 |date=2015 |pmid=25878653 |pmc=4386196 |doi=10.12669/pjms.311.5517 |url=}}</ref><ref name="pmid28660826">{{cite journal |vauthors=Ali JM, Ali A, Van Leuven M, Bartosik WR |title=Giant solitary fibrous tumour of the pleura an unpredictable entity: case series and literature review |journal=Ann R Coll Surg Engl |volume=99 |issue=6 |pages=e165–e171 |date=July 2017 |pmid=28660826 |pmc=5696978 |doi=10.1308/rcsann.2017.0067 |url=}}</ref><ref name="pmid26632548">{{cite journal |vauthors=Supakul R, Sodhi A, Tamashiro CY, Azmi SS, Kadaria D |title=Solitary Fibrous Tumor of the Pleura: A Rare Cause of Pleural Mass |journal=Am J Case Rep |volume=16 |issue= |pages=854–7 |date=December 2015 |pmid=26632548 |pmc=4671454 |doi= |url=}}</ref><ref name="pmid22014289">{{cite journal |vauthors=Guo W, Xiao HL, Jiang YG, Wang RW, Zhao YP, Ma Z, Niu HJ |title=Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review of the literature |journal=World J Surg Oncol |volume=9 |issue= |pages=134 |date=October 2011 |pmid=22014289 |pmc=3214850 |doi=10.1186/1477-7819-9-134 |url=}}</ref><ref name="pmid22833820">{{cite journal |vauthors=Chu X, Zhang L, Xue Z, Ren Z, Sun YE, Wang M, Liu M |title=Solitary fibrous tumor of the pleura: An analysis of forty patients |journal=J Thorac Dis |volume=4 |issue=2 |pages=146–54 |date=April 2012 |pmid=22833820 |doi=10.3978/j.issn.2072-1439.2012.01.05 |url=}}</ref><ref name="pmid20628740">{{cite journal |vauthors=Guo J, Chu X, Sun YE, Zhang L, Zhou N |title=Giant solitary fibrous tumor of the pleura: an analysis of five patients |journal=World J Surg |volume=34 |issue=11 |pages=2553–7 |date=November 2010 |pmid=20628740 |pmc=2949573 |doi=10.1007/s00268-010-0715-x |url=}}</ref><ref name="pmid1792644">{{cite journal |vauthors=Moat NE, Teale JD, Lea RE, Matthews AW |title=Spontaneous hypoglycaemia and pleural fibroma: role of insulin like growth factors |journal=Thorax |volume=46 |issue=12 |pages=932–3 |date=December 1991 |pmid=1792644 |pmc=463503 |doi=10.1136/thx.46.12.932 |url=}}</ref><ref name="pmid1792643">{{cite journal |vauthors=Masson EA, MacFarlane IA, Graham D, Foy P |title=Spontaneous hypoglycaemia due to a pleural fibroma: role of insulin like growth factors |journal=Thorax |volume=46 |issue=12 |pages=930–1 |date=December 1991 |pmid=1792643 |doi=10.1136/thx.46.12.930 |url=}}</ref><ref name="pmid28049955">{{cite journal |vauthors=Vejvodova S, Spidlen V, Mukensnabl P, Krakorova G, Molacek J, Vodicka J |title=Solitary Fibrous Tumor - Less Common Neoplasms of the Pleural Cavity |journal=Ann Thorac Cardiovasc Surg |volume=23 |issue=1 |pages=12–18 |date=February 2017 |pmid=28049955 |pmc=5347482 |doi=10.5761/atcs.oa.16-00108 |url=}}</ref><ref name="pmid23832995">{{cite journal |vauthors=Rahnemai-Azar AA, Rahnemai-Aazr AA, Robinson P, Pham S |title=Solitary fibrous tumour of the pleura masquerading as catecholamine-secreting paraganglioma |journal=BMJ Case Rep |volume=2013 |issue= |pages= |date=July 2013 |pmid=23832995 |pmc=3736364 |doi=10.1136/bcr-2013-009939 |url=}}</ref><ref name="pmid28063145">{{cite journal |vauthors=Ichiki Y, Kakizoe K, Hamatsu T, Matsuyama A, Suehiro T, Tanaka F, Hisaoka M, Sugimachi K |title=Solitary fibrous tumor of the lung: a case report |journal=Surg Case Rep |volume=3 |issue=1 |pages=10 |date=December 2017 |pmid=28063145 |pmc=5218951 |doi=10.1186/s40792-016-0286-7 |url=}}</ref> | ||
| | |||
* 80% of [[pleural fibroma]]<nowiki/>s originate in the [[visceral pleura]], while 20% arise from [[parietal pleura]]. | |||
| | | | ||
| | | | ||
* Composed of irregularly arranged fascicles comprising of spindle cells with collagen separation. | * Composed of irregularly arranged [[fascicles]] comprising of [[spindle cells]] with [[collagen]] separation. | ||
* They originate from submesothelial mesenchymal cells. | * They originate from submesothelial mesenchymal cells. | ||
* Myxoid or cystic degeneration can occur. | * Myxoid or cystic degeneration can occur. | ||
| | | | ||
* Recurrent somatic fusions of the two genes, | * Recurrent [[somatic]] fusions of the two [[genes]], ''[[STAT6]]'', located at chromosomal region ''[[12q13]]'', have been identified in pleural fibromas. | ||
| | | | ||
* Some pleural fibromas are associated with the paraneoplastic Doege–Potter syndrome, which is caused by tumor production of IGF-2. | * Some pleural fibromas are associated with the paraneoplastic Doege–Potter syndrome, which is caused by tumor production of [[IGF-2]]. | ||
* [[Hypoglycaemia]]: 2-4% 6, thought to be due to production of IGF-2 | * [[Hypoglycaemia]]: 2-4% 6, thought to be due to production of IGF-2 | ||
* [[Hypertrophic pulmonary osteoarthropathy]] (HPOA): ~20% 6: thought to be due to abnormal production of hyaluronic acid | * [[Hypertrophic pulmonary osteoarthropathy]] (HPOA): ~20% 6: thought to be due to abnormal production of [[hyaluronic acid]] | ||
|- | |- | ||
|Cardiac Fibroma <ref name="pmid22472419">{{cite journal |vauthors=Torimitsu S, Nemoto T, Wakayama M, Okubo Y, Yokose T, Kitahara K, Ozawa T, Nakayama H, Shinozaki M, Sasai D, Ishiwatari T, Takuma K, Shibuya K |title=Literature survey on epidemiology and pathology of cardiac fibroma |journal=Eur. J. Med. Res. |volume=17 |issue= |pages=5 |date=March 2012 |pmid=22472419 |pmc=3351722 |doi=10.1186/2047-783X-17-5 |url=}}</ref><ref name="pmid25887953">{{cite journal |vauthors=Jha NK, Kiraly L, Tamas C, Talo H, Khan MD, El Badaoui H, Jain A, Hammad A |title=Large cardiac fibroma and teratoma in children- case reports |journal=J Cardiothorac Surg |volume=10 |issue= |pages=38 |date=March 2015 |pmid=25887953 |pmc=4373309 |doi=10.1186/s13019-015-0242-9 |url=}}</ref><ref name="pmid7580366">{{cite journal |vauthors=Busch U, Kampmann C, Meyer R, Sandring KH, Hausdorf G, Konertz W |title=Removal of a giant cardiac fibroma from a 4-year-old child |journal=Tex Heart Inst J |volume=22 |issue=3 |pages=261–4 |date=1995 |pmid=7580366 |pmc=325263 |doi= |url=}}</ref><ref name="pmid16572881">{{cite journal |vauthors=Bossert T, Walther T, Vondrys D, Gummert JF, Kostelka M, Mohr FW |title=Cardiac fibroma as an inherited manifestation of nevoid basal-cell carcinoma syndrome |journal=Tex Heart Inst J |volume=33 |issue=1 |pages=88–90 |date=2006 |pmid=16572881 |pmc=1413607 |doi= |url=}}</ref><ref name="pmid29336396">{{cite journal |vauthors=Heidari A, Sabzi F, Faraji R |title=Right atrial fibroma in an adult patient |journal=Ann Card Anaesth |volume=21 |issue=1 |pages=65–67 |date=2018 |pmid=29336396 |pmc=5791493 |doi=10.4103/aca.ACA_121_17 |url=}}</ref><ref name="pmid18329553">{{cite journal |vauthors=Scanlan D, Radio SJ, Nelson M, Zhou M, Streblow R, Prasad V, Reyes C, Perry D, Fletcher S, Bridge JA |title=Loss of the PTCH1 gene locus in cardiac fibroma |journal=Cardiovasc. Pathol. |volume=17 |issue=2 |pages=93–7 |date=2008 |pmid=18329553 |pmc=2342874 |doi=10.1016/j.carpath.2007.08.001 |url=}}</ref><ref name="pmid27067427">{{cite journal |vauthors=Ying L, Lin R, Gao Z, Qi J, Zhang Z, Gu W |title=Primary cardiac tumors in children: a center's experience |journal=J Cardiothorac Surg |volume=11 |issue=1 |pages=52 |date=April 2016 |pmid=27067427 |doi=10.1186/s13019-016-0448-5 |url=}}</ref> | |Cardiac Fibroma <ref name="pmid22472419">{{cite journal |vauthors=Torimitsu S, Nemoto T, Wakayama M, Okubo Y, Yokose T, Kitahara K, Ozawa T, Nakayama H, Shinozaki M, Sasai D, Ishiwatari T, Takuma K, Shibuya K |title=Literature survey on epidemiology and pathology of cardiac fibroma |journal=Eur. J. Med. Res. |volume=17 |issue= |pages=5 |date=March 2012 |pmid=22472419 |pmc=3351722 |doi=10.1186/2047-783X-17-5 |url=}}</ref><ref name="pmid25887953">{{cite journal |vauthors=Jha NK, Kiraly L, Tamas C, Talo H, Khan MD, El Badaoui H, Jain A, Hammad A |title=Large cardiac fibroma and teratoma in children- case reports |journal=J Cardiothorac Surg |volume=10 |issue= |pages=38 |date=March 2015 |pmid=25887953 |pmc=4373309 |doi=10.1186/s13019-015-0242-9 |url=}}</ref><ref name="pmid7580366">{{cite journal |vauthors=Busch U, Kampmann C, Meyer R, Sandring KH, Hausdorf G, Konertz W |title=Removal of a giant cardiac fibroma from a 4-year-old child |journal=Tex Heart Inst J |volume=22 |issue=3 |pages=261–4 |date=1995 |pmid=7580366 |pmc=325263 |doi= |url=}}</ref><ref name="pmid16572881">{{cite journal |vauthors=Bossert T, Walther T, Vondrys D, Gummert JF, Kostelka M, Mohr FW |title=Cardiac fibroma as an inherited manifestation of nevoid basal-cell carcinoma syndrome |journal=Tex Heart Inst J |volume=33 |issue=1 |pages=88–90 |date=2006 |pmid=16572881 |pmc=1413607 |doi= |url=}}</ref><ref name="pmid29336396">{{cite journal |vauthors=Heidari A, Sabzi F, Faraji R |title=Right atrial fibroma in an adult patient |journal=Ann Card Anaesth |volume=21 |issue=1 |pages=65–67 |date=2018 |pmid=29336396 |pmc=5791493 |doi=10.4103/aca.ACA_121_17 |url=}}</ref><ref name="pmid18329553">{{cite journal |vauthors=Scanlan D, Radio SJ, Nelson M, Zhou M, Streblow R, Prasad V, Reyes C, Perry D, Fletcher S, Bridge JA |title=Loss of the PTCH1 gene locus in cardiac fibroma |journal=Cardiovasc. Pathol. |volume=17 |issue=2 |pages=93–7 |date=2008 |pmid=18329553 |pmc=2342874 |doi=10.1016/j.carpath.2007.08.001 |url=}}</ref><ref name="pmid27067427">{{cite journal |vauthors=Ying L, Lin R, Gao Z, Qi J, Zhang Z, Gu W |title=Primary cardiac tumors in children: a center's experience |journal=J Cardiothorac Surg |volume=11 |issue=1 |pages=52 |date=April 2016 |pmid=27067427 |doi=10.1186/s13019-016-0448-5 |url=}}</ref><ref name="pmid23102388">{{cite journal |vauthors=Yadava OP |title=Cardiac tumours in infancy |journal=Indian Heart J |volume=64 |issue=5 |pages=492–6 |date=2012 |pmid=23102388 |pmc=3861228 |doi=10.1016/j.ihj.2012.05.004 |url=}}</ref><ref name="pmid26457206">{{cite journal |vauthors=Cho SH, Fritz T, Cronin LJ, Cohle SD |title=Primary Cardiac Fibroma in an Adult |journal=Case Rep Cardiol |volume=2015 |issue= |pages=713702 |date=2015 |pmid=26457206 |doi=10.1155/2015/713702 |url=}}</ref><ref name="pmid23847693">{{cite journal |vauthors=Mecchia D, Lavezzi AM, Matturri L |title=Primary Cardiac Fibroma and Cardiac Conduction System Alterations in a Case of Sudden Death of a 4-month-old Infant |journal=Open Cardiovasc Med J |volume=7 |issue= |pages=47–9 |date=2013 |pmid=23847693 |pmc=3706798 |doi=10.2174/1874192401307010047 |url=}}</ref> | ||
| | |||
*[[Ventricular septum]] and left ventricular free wall. | |||
| | | | ||
* Well defined, solitary, intramyocardial lesions with smooth margins and usually large, with a mean diameter of ~5 cm | * Well defined, solitary, intramyocardial lesions with smooth margins and usually large, with a mean diameter of ~5 cm | ||
| | | | ||
* Usually have no foci of cystic change, hemorrhage, or necrosis. Calcification is common | * Usually have no foci of cystic change, [[hemorrhage]], or [[necrosis]]. [[Calcification]] is common | ||
| | | | ||
*None | |||
| | | | ||
* There is an increased prevalence of cardiac fibromas in [[Gorlin syndrome]]. | * There is an increased prevalence of cardiac fibromas in [[Gorlin syndrome]]. | ||
|- | |- | ||
|Renal Medullary Fibroma | |Renal Medullary Fibroma <ref name="pmid24228211">{{cite journal |vauthors=Kumar S, Choudhary GR, Nanjappa B, Bal A |title=Benign medullary fibroma of the kidney: a rare diagnostic dilemma |journal=J Clin Imaging Sci |volume=3 |issue= |pages=43 |date=2013 |pmid=24228211 |pmc=3823390 |doi=10.4103/2156-7514.120776 |url=}}</ref><ref name="pmid11054036">{{cite journal |vauthors=Bircan S, Orhan D, Tulunay O, Safak M |title=Renomedullary interstitial cell tumor |journal=Urol. Int. |volume=65 |issue=3 |pages=163–6 |date=2000 |pmid=11054036 |doi=10.1159/000064864 |url=}}</ref><ref name="pmid24642074">{{cite journal |vauthors=Bazzi WM, Huang H, Al-Ahmadie H, Russo P |title=Clinicopathologic features of renomedullary interstitial cell tumor presenting as the main solid renal mass |journal=Urology |volume=83 |issue=5 |pages=1104–6 |date=May 2014 |pmid=24642074 |doi=10.1016/j.urology.2014.01.008 |url=}}</ref> | ||
| | |||
*[[Renal medulla]] | |||
| | | | ||
* Small, and white well circumscribed nodule in medulla typically less than 3mm are characteristic findings of renal medullary fibroma | * Small, and white well circumscribed [[nodule]] in medulla typically less than 3mm are characteristic findings of renal medullary fibroma | ||
| | | | ||
* Small polygonal/stellate cells | * Small polygonal/stellate cells | ||
* Abundant loose/myxoid stroma | * Abundant loose/myxoid stroma | ||
* Entrapped renal tubules may be present | * Entrapped [[renal tubules]] may be present | ||
| | | | ||
*None | |||
| | | | ||
* No associated conditions | * No associated conditions | ||
|- | |- | ||
|Cemento-ossifying Fibroma | |Cemento-ossifying Fibroma <ref name="pmid28439606">{{cite journal |vauthors=Bala TK, Soni S, Dayal P, Ghosh I |title=Cemento-ossifying fibroma of the mandible. A clinicopathological report |journal=Saudi Med J |volume=38 |issue=5 |pages=541–545 |date=May 2017 |pmid=28439606 |pmc=5447217 |doi=10.15537/smj.2017.5.15643 |url=}}</ref><ref name="pmid21760674">{{cite journal |vauthors=Chatterjee A, Ajmera N, Singh A |title=Peripheral cemento-ossifying fibroma of maxilla |journal=J Indian Soc Periodontol |volume=14 |issue=3 |pages=186–9 |date=July 2010 |pmid=21760674 |pmc=3100863 |doi=10.4103/0972-124X.75915 |url=}}</ref><ref name="pmid24303483">{{cite journal |vauthors=Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H |title=Peripheral cemento-ossifying fibroma: A case report with review of literature |journal=World J Clin Cases |volume=1 |issue=3 |pages=128–33 |date=June 2013 |pmid=24303483 |pmc=3845913 |doi=10.12998/wjcc.v1.i3.128 |url=}}</ref><ref name="pmid21503260">{{cite journal |vauthors=Dalghous A, Alkhabuli JO |title=Cemento-ossifying fibroma occurring in an elderly patient. A case report and a review of literature |journal=Libyan J Med |volume=2 |issue=2 |pages=95–8 |date=June 2007 |pmid=21503260 |pmc=3078280 |doi=10.4176/061220 |url=}}</ref><ref name="pmid22091236">{{cite journal |vauthors=Hekmatnia A, Ghazavi A, Saboori M, Mahzouni P, Tayari N, Hekmatnia F |title=A case report of cemento-ossifying fibroma presenting as a mass of the ethmoid sinus |journal=J Res Med Sci |volume=16 |issue=2 |pages=224–8 |date=February 2011 |pmid=22091236 |pmc=3214308 |doi= |url=}}</ref><ref name="pmid27174452">{{cite journal |vauthors=Katti G, Khan MM, Chaubey SS, Amena M |title=Cemento-ossifying fibroma of the jaw |journal=BMJ Case Rep |volume=2016 |issue= |pages= |date=May 2016 |pmid=27174452 |pmc=4885328 |doi=10.1136/bcr-2015-214327 |url=}}</ref><ref name="pmid22557904">{{cite journal |vauthors=Ram R, Singhal A, Singhal P |title=Cemento-ossifying fibroma |journal=Contemp Clin Dent |volume=3 |issue=1 |pages=83–5 |date=January 2012 |pmid=22557904 |pmc=3341766 |doi=10.4103/0976-237X.94553 |url=}}</ref><ref name="pmid22629060">{{cite journal |vauthors=Sah K, Kale AD, Hallikerimath S, Chandra S |title=Peripheral cemento-ossifying fibroma: Report of a recurrence case |journal=Contemp Clin Dent |volume=3 |issue=Suppl 1 |pages=S23–5 |date=April 2012 |pmid=22629060 |pmc=3354807 |doi=10.4103/0976-237X.95098 |url=}}</ref><ref name="pmid24678226">{{cite journal |vauthors=Naik RM, Guruprasad Y, Sujatha D, Gurudath S, Pai A, Suresh K |title=Giant cemento-ossifying fibroma of the mandible |journal=J Nat Sci Biol Med |volume=5 |issue=1 |pages=190–4 |date=January 2014 |pmid=24678226 |pmc=3961933 |doi=10.4103/0976-9668.127326 |url=}}</ref><ref name="PereiraDiniz2018">{{cite journal|last1=Pereira|first1=Thaís dos Santos Fontes|last2=Diniz|first2=Marina Gonçalves|last3=França|first3=Josiane Alves|last4=Moreira|first4=Rennan Garcias|last5=Menezes|first5=Grazielle Helena Ferreira de|last6=Sousa|first6=Sílvia Ferreira de|last7=Castro|first7=Wagner Henriques de|last8=Gomes|first8=Carolina Cavaliéri|last9=Gomez|first9=Ricardo Santiago|title=The Wnt/β-catenin pathway is deregulated in cemento-ossifying fibromas|journal=Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology|volume=125|issue=2|year=2018|pages=172–178|issn=22124403|doi=10.1016/j.oooo.2017.10.004}}</ref> | ||
| | |||
*[[Maxillary]] [[gingiva]] is involved more often than the [[mandibular]] [[gingiva]] | |||
| | | | ||
* Solid, sessile or pedunculated mass, which is often ulcerated, and generally has a diameter of less than 2 cm are characteristic findings of cemento-ossifying fibroma. | * Solid, [[sessile]] or [[pedunculated]] [[mass]], which is often [[Ulcerated lesion|ulcerated]], and generally has a diameter of less than 2 cm are characteristic findings of cemento-ossifying fibroma. | ||
| | | | ||
* Cemento -ossifying tumors are composed of fibrous tissue, calcified tissue resembling bone and/or cementum. | * Cemento -ossifying tumors are composed of [[fibrous tissue]], calcified tissue resembling [[bone]] and/or [[cementum]]. | ||
* The bone-like component is predominant reminiscent of woven bone and is found in more 'mature' lesions. | * The bone-like component is predominant reminiscent of woven bone and is found in more 'mature' lesions. | ||
* In some instances, this entity has been divided into cementifying fibroma and [[ossifying fibroma]] depending on the relative amounts of the tumor's constituent tissues | * In some instances, this entity has been divided into cementifying fibroma and [[ossifying fibroma]] depending on the relative amounts of the tumor's constituent tissues. | ||
* Surface ulceration is common | * Surface [[ulceration]] is common | ||
| | | | ||
*None | |||
| | | | ||
* No associated conditions | * No associated conditions | ||
|- | |- | ||
|Desmoplastic Fibroblastoma | |Desmoplastic Fibroblastoma <ref name="pmid21221866">{{cite journal |vauthors=de Sousa SF, Caldeira PC, Grossmann Sde M, de Aguiar MC, Mesquita RA |title=Desmoplastic fibroblastoma (collagenous fibroma): a case identified in the buccal mucosa |journal=Head Neck Pathol |volume=5 |issue=2 |pages=175–9 |date=June 2011 |pmid=21221866 |doi=10.1007/s12105-010-0239-6 |url=}}</ref><ref name="pmid26855713">{{cite journal |vauthors=Pereira TD, de Lacerda JC, Porto-Matias MD, de Jesus AO, Gomez RS, Mesquita RA |title=Desmoplastic fibroblastoma (collagenous fibroma) of the oral cavity |journal=J Clin Exp Dent |volume=8 |issue=1 |pages=e89–92 |date=February 2016 |pmid=26855713 |doi=10.4317/jced.52605 |url=}}</ref><ref name="pmid29374633">{{cite journal |vauthors=Grewal R, Natter P, Makary R, Silliman J |title=Desmoplastic fibroblastoma of the left upper arm |journal=BMJ Case Rep |volume=2018 |issue= |pages= |date=January 2018 |pmid=29374633 |doi=10.1136/bcr-2017-221738 |url=}}</ref><ref name="pmid19503798">{{cite journal |vauthors=Osipov V, Carrera GF |title=Collagenous fibroma (desmoplastic fibroblastoma) with vertebral body erosion |journal=Sarcoma |volume=2009 |issue= |pages=682687 |date=2009 |pmid=19503798 |doi=10.1155/2009/682687 |url=}}</ref><ref name="pmid23504494">{{cite journal |vauthors=Nagaraja V, Coleman HG, Morgan GJ |title=Desmoplastic fibroblastoma presenting as a parotid tumour: a case report and review of the literature |journal=Head Neck Pathol |volume=7 |issue=3 |pages=285–90 |date=September 2013 |pmid=23504494 |pmc=3738752 |doi=10.1007/s12105-013-0435-2 |url=}}</ref><ref name="pmid22783503">{{cite journal |vauthors=Kim JH, Oh DY, Kim SW, Lee JH, Ahn ST, Rhie JW |title=Desmoplastic fibroblastoma of the finger tip in an adult |journal=Arch Plast Surg |volume=39 |issue=1 |pages=84–6 |date=January 2012 |pmid=22783503 |pmc=3385291 |doi=10.5999/aps.2012.39.1.84 |url=}}</ref> | ||
| | |||
*[[Shoulder]] region | |||
| | | | ||
| | | | ||
* [[Spindle cells]] or stellate cells without nuclear atypia | * [[Spindle cells]] or [[Stellate cell|stellate cells]] without nuclear [[atypia]] | ||
* Acellular stroma with abundant collagen | * Acellular [[stroma]] with abundant [[collagen]] | ||
* Myxoid areas may be present | * Myxoid areas may be present | ||
* Mitoses is rare | *[[Mitoses]] is rare | ||
| | | | ||
* ''FOSL1'' [[gene]] is involved in the pathogenesis of [[desmoplastic]] fibroblastoma, ''llq 12'' breakpoint described as being characteristic. | * ''[[FOSL1]]'' [[gene]] is involved in the pathogenesis of [[desmoplastic]] fibroblastoma, ''llq 12'' breakpoint described as being characteristic. | ||
* [[Beta-catenin]] -ve | |||
*Positive in desmoid-type fibromatosis | |||
*[[Desmin]] negative | |||
*[[S-100]] negative | |||
*[[CD34]] negative | |||
*[[MSA]] positive | |||
*Alpha-SMA positive | |||
| | | | ||
* No associated conditions | * No associated conditions | ||
|- | |- | ||
|Elastofibroma | |Elastofibroma <ref name="pmid21681661">{{cite journal |vauthors=Darling MR, Kutalowski M, MacPherson DG, Jackson-Boeters L, Wysocki GP |title=Oral elastofibromatous lesions: a review and case series |journal=Head Neck Pathol |volume=5 |issue=3 |pages=254–8 |date=September 2011 |pmid=21681661 |pmc=3173539 |doi=10.1007/s12105-011-0274-y |url=}}</ref><ref name="pmid19578045">{{cite journal |vauthors=Daum O, Ferda J, Curik R, Choc M, Mukensnabl P, Michal M |title=Elastofibromatous changes in tissues from spinal biopsies. A degenerative process afflicting a small but important subset of patients operated for spinal canal compression: report of 18 cases |journal=Int. J. Surg. Pathol. |volume=18 |issue=6 |pages=508–15 |date=December 2010 |pmid=19578045 |doi=10.1177/1066896909339736 |url=}}</ref><ref name="pmid20237986">{{cite journal |vauthors=Tosios KI, Economou I, Vasilopoulos NN, Koutlas IG |title=Elastofibromatous changes and hyperelastosis of the oral mucosa |journal=Head Neck Pathol |volume=4 |issue=1 |pages=31–6 |date=March 2010 |pmid=20237986 |pmc=2825534 |doi=10.1007/s12105-009-0153-y |url=}}</ref><ref name="pmid26890837">{{cite journal |vauthors=Smith HG, Hannay JA, Thway K, Messiou C, Smith MJ, Strauss DC, Hayes AJ |title=Elastofibroma dorsi: The clunking tumour that need not cause alarm |journal=Ann R Coll Surg Engl |volume=98 |issue=3 |pages=208–11 |date=March 2016 |pmid=26890837 |pmc=5226161 |doi=10.1308/rcsann.2016.0064 |url=}}</ref><ref name="pmid19628444">{{cite journal |vauthors=Kourda J, Ayadi-Kaddour A, Merai S, Hantous S, Miled KB, Mezni FE |title=Bilateral elastofibroma dorsi. A case report and review of the literature |journal=Orthop Traumatol Surg Res |volume=95 |issue=5 |pages=383–7 |date=September 2009 |pmid=19628444 |doi=10.1016/j.otsr.2009.05.002 |url=}}</ref><ref name="pmid19900325">{{cite journal |vauthors=Hoven-Gondrie ML, IJpma FF, Havenith MG, van Geldere D |title=[Elastofibroma dorsi: a characteristic, benign, subscapular swelling] |language=Dutch; Flemish |journal=Ned Tijdschr Geneeskd |volume=153 |issue= |pages=A569 |date=2009 |pmid=19900325 |doi= |url=}}</ref><ref name="pmid15063901">{{cite journal |vauthors=Hayes AJ, Alexander N, Clark MA, Thomas JM |title=Elastofibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom |journal=Eur J Surg Oncol |volume=30 |issue=4 |pages=450–3 |date=May 2004 |pmid=15063901 |doi=10.1016/j.ejso.2004.01.006 |url=}}</ref> | ||
| | |||
*[[Subscapular]] region. | |||
| | | | ||
* I'll defined, nonencapsulated, rubbery, firm, white lesion with interspersed fat and with moderate demarcation to surrounding tissue are characteristic findings of [[elastofibroma]]. | * I'll defined, nonencapsulated, rubbery, firm, white lesion with interspersed [[fat]] and with moderate demarcation to surrounding tissue are characteristic findings of [[elastofibroma]]. | ||
* The tumors can be quite large (up to 20 cm), although most are around 5 cm. | * The [[tumors]] can be quite large (up to 20 cm), although most are around 5 cm. | ||
| | | | ||
* Thick bundles of [[collagen]] and elastin | * Thick bundles of [[collagen]] and [[elastin fibers]] are characteristic findings of [[elastofibroma]]. | ||
* Admixture of heavy dense bands of collagenous tissue dissected by fat and abnormal elastic fibers. | * Admixture of heavy dense bands of [[collagenous]] tissue dissected by fat and abnormal [[elastic fibers]]. | ||
* The elastic fibers are coarse, thick, and darkly eosinophilic, often fragmented into globules, creating a "string of pearls" or "pipe cleaner" appearance. Because of degeneration, the elastic fibers will appear as globules with a serrated or "prickled" edge. | * The [[elastic fibers]] are coarse, thick, and darkly [[eosinophilic]], often fragmented into globules, creating a "string of pearls" or "pipe cleaner" appearance. Because of degeneration, the [[elastic fibers]] will appear as globules with a serrated or "prickled" edge. | ||
| | | | ||
* There are alterations of short arm of chromosome 1 | * There are alterations of [[short arm]] of [[chromosome]] 1 | ||
* Multifocality may suggest systemic enzymatic defect, resulting in abnormal elastogenesis | * Multifocality may suggest systemic enzymatic defect, resulting in abnormal [[elastogenesis]] | ||
* The [[elastic fibers]] will be visible on a Weigert or von Gieson elastic stains. | |||
| | | | ||
* No associated conditions | * No associated conditions | ||
|- | |- | ||
|Sclerotic Fibroma | |Sclerotic Fibroma <ref name="pmid20729948">{{cite journal |vauthors=Bhambri A, Del Rosso JQ |title=Solitary sclerotic fibroma |journal=J Clin Aesthet Dermatol |volume=2 |issue=6 |pages=36–8 |date=June 2009 |pmid=20729948 |pmc=2923956 |doi= |url=}}</ref><ref name="pmid18544068">{{cite journal |vauthors=Nakashima K, Yamada N, Adachi K, Yoshida Y, Yamamoto O |title=Solitary sclerotic fibroma of the skin: morphological characterization of the 'plywood-like pattern' |journal=J. Cutan. Pathol. |volume=35 Suppl 1 |issue= |pages=74–9 |date=October 2008 |pmid=18544068 |doi=10.1111/j.1600-0560.2008.01001.x |url=}}</ref><ref name="pmid1430474">{{cite journal |vauthors=Requena L, Gutiérrez J, Sánchez Yus E |title=Multiple sclerotic fibromas of the skin. A cutaneous marker of Cowden's disease |journal=J. Cutan. Pathol. |volume=19 |issue=4 |pages=346–51 |date=August 1992 |pmid=1430474 |doi= |url=}}</ref><ref name="pmid1491554">{{cite journal |vauthors=Mori O, Hachisuka H, Sasai Y |title=Sclerotic fibromas of the skin--reports of two cases and a review of the literature in Japan |journal=Kurume Med J |volume=39 |issue=3 |pages=191–3 |date=1992 |pmid=1491554 |doi= |url=}}</ref><ref name="pmid2258475">{{cite journal |vauthors=Lo WL, Wong CK |title=Solitary sclerotic fibroma |journal=J. Cutan. Pathol. |volume=17 |issue=5 |pages=269–73 |date=October 1990 |pmid=2258475 |doi= |url=}}</ref><ref name="pmid10698210">{{cite journal |vauthors=Hanft VN, Shea CR, McNutt NS, Pullitzer D, Horenstein MG, Prieto VG |title=Expression of CD34 in sclerotic ("plywood") fibromas |journal=Am J Dermatopathol |volume=22 |issue=1 |pages=17–21 |date=February 2000 |pmid=10698210 |doi= |url=}}</ref><ref name="pmid15059222">{{cite journal |vauthors=High WA, Stewart D, Essary LR, Kageyama NP, Hoang MP, Cockerell CJ |title=Sclerotic fibroma-like change in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? |journal=J. Cutan. Pathol. |volume=31 |issue=5 |pages=373–8 |date=May 2004 |pmid=15059222 |doi=10.1111/j.0303-6987.2004.00199.x |url=}}</ref><ref name="pmid8600796">{{cite journal |vauthors=Shitabata PK, Crouch EC, Fitzgibbon JF, Swanson PE, Adesokan PN, Wick MR |title=Cutaneous sclerotic fibroma. Immunohistochemical evidence of a fibroblastic neoplasm with ongoing type I collagen synthesis |journal=Am J Dermatopathol |volume=17 |issue=4 |pages=339–43 |date=August 1995 |pmid=8600796 |doi= |url=}}</ref><ref name="pmid15166503">{{cite journal |vauthors=Alawi F, Freedman PD |title=Sporadic sclerotic fibroma of the oral soft tissues |journal=Am J Dermatopathol |volume=26 |issue=3 |pages=182–7 |date=June 2004 |pmid=15166503 |doi= |url=}}</ref> | ||
| | |||
*[[Skin]], may be solitary or multifocal | |||
| | | | ||
| | | | ||
* Well-delineated but unencapsulated mass of densely collagenized, hypocellular fibrous tissue with a storiform pattern, and prominent clefts between collagen bundles are characteristic findings of elastofibroma. | * Well-delineated but unencapsulated mass of densely collagenized, hypocellular [[fibrous tissue]] with a storiform pattern, and prominent clefts between [[collagen]] bundles are characteristic findings of [[elastofibroma]]. | ||
| | | | ||
*[[CD34]] | |||
*[[Vimentin]] positive | |||
| | | | ||
* [[Cowden syndrome]] | * [[Cowden syndrome]] | ||
| Line 205: | Line 276: | ||
|Giant cell fibroma <ref name="pmid28785965">{{cite journal |vauthors=Upadhyaya JD, Cohen DM, Islam MN, Bhattacharyya I |title=Hybrid Central Odontogenic Fibroma with Giant Cell Granuloma like Lesion: A Report of Three Additional Cases and Review of the Literature |journal=Head Neck Pathol |volume=12 |issue=2 |pages=166–174 |date=June 2018 |pmid=28785965 |pmc=5953869 |doi=10.1007/s12105-017-0845-7 |url=}}</ref><ref name="pmid24511398">{{cite journal |vauthors=Sonalika WG, Sahu A, Deogade SC, Gupta P, Naitam D, Chansoria H, Agarwal J, Katoch S |title=Giant cell fibroma of tongue: understanding the nature of an unusual histopathological entity |journal=Case Rep Dent |volume=2014 |issue= |pages=864512 |date=2014 |pmid=24511398 |pmc=3910466 |doi=10.1155/2014/864512 |url=}}</ref><ref name="pmid20614305">{{cite journal |vauthors=Tosios KI, Gopalakrishnan R, Koutlas IG |title=So-called hybrid central odontogenic fibroma/central giant cell lesion of the jaws. A report on seven additional cases, including an example in a patient with cherubism, and hypotheses on the pathogenesis |journal=Head Neck Pathol |volume=2 |issue=4 |pages=333–8 |date=December 2008 |pmid=20614305 |pmc=2807578 |doi=10.1007/s12105-008-0076-z |url=}}</ref><ref name="pmid23248467">{{cite journal |vauthors=Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B |title=Giant cell fibroma: A clinicopathological study |journal=J Oral Maxillofac Pathol |volume=16 |issue=3 |pages=359–62 |date=September 2012 |pmid=23248467 |pmc=3519210 |doi=10.4103/0973-029X.102485 |url=}}</ref><ref name="pmid27822394">{{cite journal |vauthors=Mello-Moura AC, Santos AM, Bonini GA, Del Conte Zardetto CG, Moura-Netto C, Wanderley MT |title=Giant Cell Fibroma in a Two-Year-Old Child |journal=Case Rep Dent |volume=2016 |issue= |pages=7058356 |date=2016 |pmid=27822394 |pmc=5086372 |doi=10.1155/2016/7058356 |url=}}</ref><ref name="pmid30158768">{{cite journal |vauthors=Hosur MB, Puranik RS, Vanaki SS, Puranik SR, Ingaleshwar PS |title=Clinicopathological profile of central giant cell granulomas: An institutional experience and study of immunohistochemistry expression of p63 in central giant cell granuloma |journal=J Oral Maxillofac Pathol |volume=22 |issue=2 |pages=173–179 |date=2018 |pmid=30158768 |pmc=6097366 |doi=10.4103/jomfp.JOMFP_260_17 |url=}}</ref><ref name="pmid29391720">{{cite journal |vauthors=Kulkarni S, Chandrashekar C, Kudva R, Radhakrishnan R |title=Giant-cell fibroma: Understanding the nature of the melanin-laden cells |journal=J Oral Maxillofac Pathol |volume=21 |issue=3 |pages=429–433 |date=2017 |pmid=29391720 |pmc=5763868 |doi=10.4103/jomfp.JOMFP_209_16 |url=}}</ref><ref name="pmid24551733">{{cite journal |vauthors=Jimson S, Jimson S |title=Giant cell fibroma: a case report with immunohistochemical markers |journal=J Clin Diagn Res |volume=7 |issue=12 |pages=3079–80 |date=December 2013 |pmid=24551733 |pmc=3919395 |doi=10.7860/JCDR/2013/6476.3859 |url=}}</ref> | |Giant cell fibroma <ref name="pmid28785965">{{cite journal |vauthors=Upadhyaya JD, Cohen DM, Islam MN, Bhattacharyya I |title=Hybrid Central Odontogenic Fibroma with Giant Cell Granuloma like Lesion: A Report of Three Additional Cases and Review of the Literature |journal=Head Neck Pathol |volume=12 |issue=2 |pages=166–174 |date=June 2018 |pmid=28785965 |pmc=5953869 |doi=10.1007/s12105-017-0845-7 |url=}}</ref><ref name="pmid24511398">{{cite journal |vauthors=Sonalika WG, Sahu A, Deogade SC, Gupta P, Naitam D, Chansoria H, Agarwal J, Katoch S |title=Giant cell fibroma of tongue: understanding the nature of an unusual histopathological entity |journal=Case Rep Dent |volume=2014 |issue= |pages=864512 |date=2014 |pmid=24511398 |pmc=3910466 |doi=10.1155/2014/864512 |url=}}</ref><ref name="pmid20614305">{{cite journal |vauthors=Tosios KI, Gopalakrishnan R, Koutlas IG |title=So-called hybrid central odontogenic fibroma/central giant cell lesion of the jaws. A report on seven additional cases, including an example in a patient with cherubism, and hypotheses on the pathogenesis |journal=Head Neck Pathol |volume=2 |issue=4 |pages=333–8 |date=December 2008 |pmid=20614305 |pmc=2807578 |doi=10.1007/s12105-008-0076-z |url=}}</ref><ref name="pmid23248467">{{cite journal |vauthors=Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B |title=Giant cell fibroma: A clinicopathological study |journal=J Oral Maxillofac Pathol |volume=16 |issue=3 |pages=359–62 |date=September 2012 |pmid=23248467 |pmc=3519210 |doi=10.4103/0973-029X.102485 |url=}}</ref><ref name="pmid27822394">{{cite journal |vauthors=Mello-Moura AC, Santos AM, Bonini GA, Del Conte Zardetto CG, Moura-Netto C, Wanderley MT |title=Giant Cell Fibroma in a Two-Year-Old Child |journal=Case Rep Dent |volume=2016 |issue= |pages=7058356 |date=2016 |pmid=27822394 |pmc=5086372 |doi=10.1155/2016/7058356 |url=}}</ref><ref name="pmid30158768">{{cite journal |vauthors=Hosur MB, Puranik RS, Vanaki SS, Puranik SR, Ingaleshwar PS |title=Clinicopathological profile of central giant cell granulomas: An institutional experience and study of immunohistochemistry expression of p63 in central giant cell granuloma |journal=J Oral Maxillofac Pathol |volume=22 |issue=2 |pages=173–179 |date=2018 |pmid=30158768 |pmc=6097366 |doi=10.4103/jomfp.JOMFP_260_17 |url=}}</ref><ref name="pmid29391720">{{cite journal |vauthors=Kulkarni S, Chandrashekar C, Kudva R, Radhakrishnan R |title=Giant-cell fibroma: Understanding the nature of the melanin-laden cells |journal=J Oral Maxillofac Pathol |volume=21 |issue=3 |pages=429–433 |date=2017 |pmid=29391720 |pmc=5763868 |doi=10.4103/jomfp.JOMFP_209_16 |url=}}</ref><ref name="pmid24551733">{{cite journal |vauthors=Jimson S, Jimson S |title=Giant cell fibroma: a case report with immunohistochemical markers |journal=J Clin Diagn Res |volume=7 |issue=12 |pages=3079–80 |date=December 2013 |pmid=24551733 |pmc=3919395 |doi=10.7860/JCDR/2013/6476.3859 |url=}}</ref> | ||
| | | | ||
* Sessile or pedunculated nodule that is smaller than 1cm in diameter are characteristic findings of [[giant cell fibroma]]. Often, it has a bosselated or somewhat papillary surface. | *[[Mandibular]] [[gingiva]], followed by the [[maxillary]] [[gingiva]], the [[tongue]], and the [[palate]]. | ||
| | |||
*[[Sessile]] or [[pedunculated]] [[nodule]] that is smaller than 1cm in diameter are characteristic findings of [[giant cell fibroma]]. Often, it has a bosselated or somewhat [[papillary]] surface. | |||
| | | | ||
* An unencapsulated mass of fibrous connective tissue that contains numerous characteristic large, plump, stellate and spindle-shaped fibroblasts, some of which are multinucleated. | * An unencapsulated mass of [[fibrous connective tissue]] that contains numerous characteristic large, plump, [[Stellate cell|stellate]] and spindle-shaped [[fibroblasts]], some of which are multinucleated. | ||
* The surface epithelium is often atrophic and corrugated. | * The surface [[epithelium]] is often [[atrophic]] and corrugated. | ||
| | | | ||
*None | |||
| | | | ||
*No associated conditions | |||
|- | |- | ||
|Peripheral Odontogenic Fibroma <ref name="pmid29333009">{{cite journal |vauthors=Chandna P, Srivastava N, Bansal V, Wadhwan V, Dubey P |title=Peripheral and Central Giant Cell Lesions in Children: Institutional Experience at Subharti Dental College and Hospital |journal=Indian J Med Paediatr Oncol |volume=38 |issue=4 |pages=440–446 |date=2017 |pmid=29333009 |pmc=5759061 |doi=10.4103/ijmpo.ijmpo_17_16 |url=}}</ref><ref name=" | |Peripheral Odontogenic Fibroma <ref name="pmid29333009">{{cite journal |vauthors=Chandna P, Srivastava N, Bansal V, Wadhwan V, Dubey P |title=Peripheral and Central Giant Cell Lesions in Children: Institutional Experience at Subharti Dental College and Hospital |journal=Indian J Med Paediatr Oncol |volume=38 |issue=4 |pages=440–446 |date=2017 |pmid=29333009 |pmc=5759061 |doi=10.4103/ijmpo.ijmpo_17_16 |url=}}</ref><ref name="pmid29354306">{{cite journal |vauthors=Wright JM, Soluk Tekkesin M |title=Odontogenic tumors: where are we in 2017 ? |journal=J Istanb Univ Fac Dent |volume=51 |issue=3 Suppl 1 |pages=S10–S30 |date=2017 |pmid=29354306 |pmc=5750825 |doi=10.17096/jiufd.52886 |url=}}</ref><ref name="pmid24920510">{{cite journal |vauthors=Reddy SV, Medikonda SK, Konda A, Natta S |title=A rare benign odontogenic neoplasm: peripheral odontogenic fibroma |journal=BMJ Case Rep |volume=2014 |issue= |pages= |date=June 2014 |pmid=24920510 |pmc=4069815 |doi=10.1136/bcr-2013-201065 |url=}}</ref><ref name="pmid22028517">{{cite journal |vauthors=Baiju CS, Rohatgi S |title=Peripheral odontogenic fibroma: A case report and review |journal=J Indian Soc Periodontol |volume=15 |issue=3 |pages=273–5 |date=July 2011 |pmid=22028517 |pmc=3200026 |doi=10.4103/0972-124X.85674 |url=}}</ref><ref name="pmid25210375">{{cite journal |vauthors=Sreeja C, Vezhavendan N, Shabana F, Vijayalakshmi D, Devi M, Arunakiry N |title=Recurrent peripheral odontogenic fibroma associated with basal cell budding |journal=J Pharm Bioallied Sci |volume=6 |issue=Suppl 1 |pages=S204–7 |date=July 2014 |pmid=25210375 |pmc=4157271 |doi=10.4103/0975-7406.137470 |url=}}</ref> | ||
|Firm, slowly growing, [[sessile]], and nodular growth of the gingiva are characteristic findings of peripheral odontogenic fibroma. | | | ||
*[[Mandible]] | |||
|Firm, slowly growing, [[sessile]], and [[nodular]] growth of the [[gingiva]] are characteristic findings of peripheral odontogenic fibroma. | |||
| | | | ||
* An unencapsulated mass of interwoven cellular fibrous connective tissue that contains scattered nests or strands of odontogenic epithelium | * An unencapsulated mass of interwoven cellular [[fibrous connective tissue]] that contains scattered nests or strands of [[odontogenic]] [[epithelium]] | ||
* It consists of cellular fibrous connective tissue parenchyma with non neoplastic islands, strands of columnar or cuboidal odontogenic epithelium. | * It consists of [[cellular]] [[fibrous connective tissue]] parenchyma with non neoplastic islands, strands of [[Columnar epithelium|columnar]] or [[Cuboidal epithelia|cuboidal]] [[odontogenic]] [[epithelium]]. | ||
* Myxoid foci, osteoid, cementoid, or dystrophic calcifications are sometimes seen. | * Myxoid foci, osteoid, cementoid, or [[Dystrophic calcification|dystrophic calcifications]] are sometimes seen. | ||
* Generally, the surface is not ulcerated. | * Generally, the surface is not [[Ulcerated lesion|ulcerated]]. | ||
| | | | ||
*None | |||
| | | | ||
*No associated conditions | |||
|} | |||
* | |||
==Gross Pathology and Microscopic Pathology== | |||
{| class="wikitable" | |||
|+ | |||
!Type of fibroma | |||
!Gross image | |||
!Microscopic image | |||
|- | |||
|Ovarian fibroma | |||
|[[File:1200px-Fibroma of the Ovary.jpg|400px|thumb|none|Ed Uthman, MD [CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0)],https://upload.wikimedia.org/wikipedia/commons/0/04/Fibroma_of_the_Ovary.jpg,https://commons.wikimedia.org/wiki/File:Fibroma_of_the_Ovary.jpg]] | |||
|[[File:Ovarian fibroma 1.jpg|300px|thumb|none|Histopathology of ovarian fibroma showing benignspindle cellproliferation,Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M. Large twisted ovarian fibroma in menopausal women: a case report. Pan Afr Med J. 2015;20:322. Published 2015 Apr 6. doi:10.11604/pamj.2015.20.322.5998,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4491469/]] | |||
|- | |||
|Oral fibroma | |||
|[[File:Oral fibroma.jpeg|300px|thumb|center|Fibroma of oral mucosa,Klaus D. Peter, Gummersbach, Germany [CC BY 3.0 de (https://creativecommons.org/licenses/by/3.0/de/deed.en)],https://upload.wikimedia.org/wikipedia/commons/c/c5/Fibroma.jpg,https://commons.wikimedia.org/wiki/File:Fibroma.jpg]] | |||
|[[File:Oral fibroma -- low mag.jpg|300px|thumb|none|Librepath [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)],https://upload.wikimedia.org/wikipedia/commons/d/db/Oral_fibroma_--_low_mag.jpg,https://commons.wikimedia.org/wiki/File:Oral_fibroma_--_low_mag.jpg]] | |||
|- | |- | ||
|Chondromyxoid fibroma | |||
| | | | ||
|[[File:Bone ChondromyxoidFibroma Calcium MP PA.JPG|300px|thumb|none|arahkayb [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)],https://upload.wikimedia.org/wikipedia/commons/a/a6/Bone_ChondromyxoidFibroma_Calcium_MP_PA.JPG,https://commons.wikimedia.org/wiki/File:Bone_ChondromyxoidFibroma_Calcium_MP_PA.JPG]] | |||
|- | |||
|Uterine fibroma | |||
|[[File:Uterine fibroids.jpg|300px|thumb|center|Hic et nunc [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)],https://upload.wikimedia.org/wikipedia/commons/f/f7/Uterine_fibroids.jpg,https://commons.wikimedia.org/wiki/File:Uterine_fibroids.jpg]] | |||
|[[File:Leiomyoma Uterus 40x.jpg|300px|thumb|none|Calicut Medical College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)],https://upload.wikimedia.org/wikipedia/commons/e/ea/Leiomyoma_Uterus_40x.jpg,https://commons.wikimedia.org/wiki/File:Leiomyoma_Uterus_40x.jpg]] | |||
|- | |||
|Ossifying Fibroma | |||
| | | | ||
|[[File:Ossifying fibroma.jpg|300px|thumb|center|Histopathologicaly, this lesion is characterized by spindle cell proliferation packed with globular cementum droplets and round/ovoid fragments of woven bone. These spindle cells appear benign and associated with psammomatoid cementum droplets and some woven bone and consistent with aggressive ossifying fibroma, psammomatous type IV,Alghonaim Y, ALRashed ALHumaid S, Arafat A. Aggressive ossifying fibroma of right ethmoidal sinus: A case report. Int J Surg Case Rep. ;53:513–516. doi:10.1016/j.ijscr.2017.12.026,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290393/]] | |||
|- | |||
|Cardiac fibroma | |||
|[[File:Cardiac fibroma gross.jpg|300px|thumb|center|Jha NK, Kiraly L, Tamas C, et al. Large cardiac fibroma and teratoma in children- case reports. J Cardiothorac Surg. 2015;10:38. Published 2015 Mar 22. doi:10.1186/s13019-015-0242-9,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4373309/]] | |||
|[[File:Cardiac fibroma.jpg|300px|thumb|none|Fibroblast cells in fascicles with abundant collagen fiber,Heidari A, Sabzi F, Faraji R. Right atrial fibroma in an adult patient. Ann Card Anaesth. 2018;21(1):65–67. doi:10.4103/aca.ACA_121_17,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5791493/]] | |||
|- | |||
|Giant cell fibroma | |||
|[[File:Giant cell fibroma.jpg|300px|thumb|center|Pebbly appearance in right retromolar region,Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B. Giant cell fibroma: A clinicopathological study. J Oral Maxillofac Pathol. 2012;16(3):359–362. doi:10.4103/0973-029X.102485,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519210/]] | |||
|[[File:Giant cell fibroma 2.jpg|300px|thumb|none|Artifactual spacing was observed surrounding the giant cells,Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B. Giant cell fibroma: A clinicopathological study. J Oral Maxillofac Pathol. 2012;16(3):359–362. doi:10.4103/0973-029X.102485,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519210/]] | |||
|- | |||
|Peripheral odontogenic fibroma | |||
|[[File:Peripheral odontogenic fibroma.jpg|300px|thumb|center|Baiju CS, Rohatgi S. Peripheral odontogenic fibroma: A case report and review. J Indian Soc Periodontol. 2011;15(3):273–275. doi:10.4103/0972-124X.85674,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200026/]] | |||
|[[File:Peripheral odontogenic fibroma 1.jpg|300px|thumb|none|Baiju CS, Rohatgi S. Peripheral odontogenic fibroma: A case report and review. J Indian Soc Periodontol. 2011;15(3):273–275. doi:10.4103/0972-124X.85674,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200026/]] | |||
|- | |||
|Elastofibroma | |||
|[[File:Elastofibroma1.jpg|300px|thumb|center|The typical location for bilateral elastofibroma dorsi in prone position and with slightly abducted arm,Sarici IS, Basbay E, Mustu M, et al. Bilateral elastofibroma dorsi: A case report. Int J Surg Case Rep. ;5(12):1139–1141. doi:10.1016/j.ijscr.2014.10.032,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275815/]] | |||
|[[File:Elastofibroma.jpg|300px|thumb|none|High Power slide showing elastic fibres (pink areas) which confirms the diagnosis of elastofibroma. (Altered elastic fibres in a collagenous matrix),Pillay Y, Sabarathnam R. Elasto fibroma Dorsi: a case report of bilateral tumours and excision of the symptomatic lesion in a male patient. J Surg Case Rep. 2017;2017(11):rjx206. Published 2017 Nov 7. doi:10.1093/jscr/rjx206,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691368/]] | |||
|- | |||
|Desmoplastic fibroblastoma | |||
| | | | ||
| | |[[File:Desmoplastic fibroblastoma.jpg|300px|thumb|none|Grewal R, Natter P, Makary R, Silliman J. Desmoplastic fibroblastoma of the left upper arm. BMJ Case Rep. 2018;2018:bcr2017221738. Published 2018 Jan 26. doi:10.1136/bcr-2017-221738,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786997/]] | ||
|- | |||
|Renal medullary fibroma | |||
|[[File:Renal medullary fibroma.jpg|300px|thumb|center|Renal medullary fibroma showing a firm grayish yellow calcified tumor (black arrow), renal hilum (white arrow),Kumar S, Choudhary GR, Nanjappa B, Bal A. Benign medullary fibroma of the kidney: a rare diagnostic dilemma. J Clin Imaging Sci. 2013;3:43. Published 2013 Oct 29. doi:10.4103/2156-7514.120776,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3823390/]] | |||
|[[File:Renal medullary fibroma1.jpg|300px|thumb|none|H&E stain showing bland spindle-shaped cells occurring singly within a loose stromal matrix (black arrow) and separated by thick collagen bundles (white arrow),Kumar S, Choudhary GR, Nanjappa B, Bal A. Benign medullary fibroma of the kidney: a rare diagnostic dilemma. J Clin Imaging Sci. 2013;3:43. Published 2013 Oct 29. doi:10.4103/2156-7514.120776,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3823390/]] | |||
|- | |||
|Pleural fibroma | |||
|[[File:Pleural fibroma.jpg|300px|thumb|center|Single multi nodular encapsulated pale white firm piece of tissue,Hassan S, Husain SS, Anwar MA, Saeed S. Pleural Fibroma; A meandering path to surgical removal. Pak J Med Sci. 2015;31(1):236–238. doi:10.12669/pjms.311.5517,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4386196/]] | |||
| | | | ||
|- | |- | ||
| | | | ||
| | | | ||
| Line 235: | Line 363: | ||
|} | |} | ||
== | ==Pathophysiology== | ||
===Physiology=== | |||
The normal physiology of [name of process] can be understood as follows: | |||
=== | ===Pathogenesis=== | ||
*The exact pathogenesis of [disease name] is not completely understood. | |||
OR | |||
*It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3]. | |||
*[Pathogen name] is usually transmitted via the [transmission route] route to the human host. | |||
*Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell. | |||
*[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells]. | |||
*The progression to [disease name] usually involves the [molecular pathway]. | |||
*The pathophysiology of [disease/malignancy] depends on the histological subtype. | |||
== | ==Genetics== | ||
[Disease name] is transmitted in [mode of genetic transmission] pattern. | |||
OR | |||
Genes involved in the pathogenesis of [disease name] include: | |||
*[Gene1] | |||
*[Gene2] | |||
* | *[Gene3] | ||
* | |||
OR | |||
The development of [disease name] is the result of multiple genetic mutations such as: | |||
*[Mutation 1] | |||
* | *[Mutation 2] | ||
*[Mutation 3] | |||
*[ | |||
*[ | |||
==Associated Conditions== | |||
Conditions associated with [disease name] include: | |||
*[Condition 1] | |||
*[Condition 2] | |||
*[Condition 3] | |||
* | |||
* | |||
= | {| class="wikitable" | ||
|+ | |||
== | !Type of fibroma | ||
=== | !Location | ||
!Gross pathology | |||
!Microscpoic pathology | |||
!Genetics and Immunohistochemistry | |||
=== | !Associated conditions | ||
|- | |||
=== | |Ovarian Fibroma <ref name="pmid26175813">{{cite journal |vauthors=Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M |title=Large twisted ovarian fibroma in menopausal women: a case report |journal=Pan Afr Med J |volume=20 |issue= |pages=322 |date=2015 |pmid=26175813 |pmc=4491469 |doi=10.11604/pamj.2015.20.322.5998 |url=}}</ref><ref name="pmid27876070">{{cite journal |vauthors=Chen H, Liu Y, Shen LF, Jiang MJ, Yang ZF, Fang GP |title=Ovarian thecoma-fibroma groups: clinical and sonographic features with pathological comparison |journal=J Ovarian Res |volume=9 |issue=1 |pages=81 |date=November 2016 |pmid=27876070 |pmc=5120502 |doi=10.1186/s13048-016-0291-2 |url=}}</ref><ref name="pmid27770806">{{cite journal |vauthors=Matsuda K, Tateishi S, Akazawa Y, Kinoshita A, Yoshida S, Morisaki S, Fukushima A, Matsuwaki T, Yoshiura KI, Nakashima M |title=Rapid growth of mitotically active cellular fibroma of the ovary: a case report and review of the literature |journal=Diagn Pathol |volume=11 |issue=1 |pages=101 |date=October 2016 |pmid=27770806 |doi=10.1186/s13000-016-0554-7 |url=}}</ref><ref name="pmid26437718">{{cite journal |vauthors=Yamada T, Hattori K, Satomi H, Hirose Y, Nakai G, Daimon A, Hayashi A, Terai Y, Ohmichi M, Fukunaga M |title=Mitotically active cellular fibroma of the ovary: a case report and literature review |journal=J Ovarian Res |volume=8 |issue= |pages=65 |date=October 2015 |pmid=26437718 |pmc=4595272 |doi=10.1186/s13048-015-0191-x |url=}}</ref><ref name="pmid25550794">{{cite journal |vauthors=Zong L, Lin M, Fan X |title=Mitotically active cellular fibroma of ovary should be differentiated from fibrosarcoma: a case report and review of literature |journal=Int J Clin Exp Pathol |volume=7 |issue=11 |pages=7578–82 |date=2014 |pmid=25550794 |pmc=4270577 |doi= |url=}}</ref><ref name="pmid27821988">{{cite journal |vauthors=Parwate NS, Patel SM, Arora R, Gupta M |title=Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature |journal=J Obstet Gynaecol India |volume=66 |issue=6 |pages=460–465 |date=December 2016 |pmid=27821988 |pmc=5080219 |doi=10.1007/s13224-015-0717-6 |url=}}</ref><ref name="pmid22691621">{{cite journal |vauthors=Finch T, Pushpanathan C, Brown K, El-Gohary Y |title=Gorlin syndrome presenting with a unilateral ovarian fibroma in a 22-year-old woman: a case report |journal=J Med Case Rep |volume=6 |issue= |pages=148 |date=June 2012 |pmid=22691621 |doi=10.1186/1752-1947-6-148 |url=}}</ref><ref name="pmid24490014">{{cite journal |vauthors=Yazdani S, Alijanpoor A, Sharbatdaran M, Bouzari Z, Abedisamakoosh M, Lakaieandi F, Mohammadpour M |title=Meigs' syndrome with elevated serum CA125 in a case of ovarian fibroma /thecoma |journal=Caspian J Intern Med |volume=5 |issue=1 |pages=43–5 |date=2014 |pmid=24490014 |pmc=3894471 |doi= |url=}}</ref> | ||
== | | | ||
*[[Ovary]] | |||
=== | | | ||
* The [[tumor]] shows [[homogeneous]] and [[solid]] in appearance with a yellowish-white pigment tinge | |||
* [[Necrosis]] and [[hemorrhage]] may or may not be present | |||
| | |||
*Dense [[cellular]] proliferations of spindle [[fibroblast]]-like [[cells]], which are arranged in a fascicular pattern with ovoid to spindle-shaped [[nuclei]] and a scant [[cytoplasm]] | |||
*[[Tumor cells]] multiply in a trabecular pattern with a [[collagen band]] that is distributed around the [[stroma]] | |||
* | *Absence of significant [[cytological]] [[atypia]] | ||
* | | | ||
* | *None | ||
| | |||
=== | *[[Ovarian fibromas]] are associated with [[ascites]] in approximately 40% of cases and with [[pleural effusions]] in a small percentage of cases | ||
* | *[[Meigs syndrome]]: consists of an ovarian fibroma with [[ascites]] and a [[pleural effusion]] | ||
*Fibromas are seen in approximately 75% of [[patients]] with [[Nevoid Basal Cell Carcinoma Syndrome|nevoid basal cell carcinoma syndrome]] ([[Gorlin syndrome]]) | |||
|- | |||
|Oral Fibroma <ref name="pmid26448815">{{cite journal |vauthors=Panta P |title=Traumatic fibroma |journal=Pan Afr Med J |volume=21 |issue= |pages=220 |date=2015 |pmid=26448815 |pmc=4587079 |doi=10.11604/pamj.2015.21.220.7498 |url=}}</ref><ref name="pmid8035060">{{cite journal |vauthors=Christopoulos P, Sklavounou A, Patrikiou A |title=True fibroma of the oral mucosa: a case report |journal=Int J Oral Maxillofac Surg |volume=23 |issue=2 |pages=98–9 |date=April 1994 |pmid=8035060 |doi= |url=}}</ref><ref name="pmid26958126">{{cite journal |vauthors=Krishnan V, Shunmugavelu K |title=A clinical challenging situation of intra oral fibroma mimicking pyogenic granuloma |journal=Pan Afr Med J |volume=22 |issue= |pages=263 |date=2015 |pmid=26958126 |pmc=4765330 |doi=10.11604/pamj.2015.22.263.8080 |url=}}</ref> | |||
| | |||
*[[Buccal mucosa]] | |||
| | |||
* A round-to-ovoid [[polypoid]] lesion, smooth-surfaced, and firm [[sessile]] or pedunculated [[Mass (medicine)|mass]] | |||
* 1 mm to 2 cm in diameter in size,[[hyperkeratotic]] or [[Ulcerated lesion|ulcerated]] surface | |||
* Known for repeated [[trauma]] | |||
* | | | ||
*[[Histologically]] similar to [[fibrous]] [[papule]] | |||
*[[Fibrous]] [[stroma]] is a key feature | |||
*[[Collagen]] bundles may be present | |||
| | |||
*None | |||
| | |||
* Multiple oral fibromas may be seen in [[Cowden disease]] | |||
|- | |||
|Chondromyxoid fibroma <ref name="pmid17907440">{{cite journal |vauthors=Takenaga RK, Frassica FJ, McCarthy EF |title=Subperiosteal chondromyxoid fibroma: a report of two cases |journal=Iowa Orthop J |volume=27 |issue= |pages=104–7 |date=2007 |pmid=17907440 |pmc=2150655 |doi= |url=}}</ref><ref name="pmid16547720">{{cite journal |vauthors=Sharma H, Jane MJ, Reid R |title=Chondromyxoid fibroma of the foot and ankle: 40 years' Scottish bone tumour registry experience |journal=Int Orthop |volume=30 |issue=3 |pages=205–9 |date=June 2006 |pmid=16547720 |pmc=2532097 |doi=10.1007/s00264-005-0046-y |url=}}</ref><ref name="pmid19648885">{{cite journal |vauthors=Yasuda T, Nishio J, Sumegi J, Kapels KM, Althof PA, Sawyer JR, Reith JD, Bridge JA |title=Aberrations of 6q13 mapped to the COL12A1 locus in chondromyxoid fibroma |journal=Mod. Pathol. |volume=22 |issue=11 |pages=1499–506 |date=November 2009 |pmid=19648885 |doi=10.1038/modpathol.2009.101 |url=}}</ref><ref name="pmid22043162">{{cite journal |vauthors=Choi YS, Kim BS, Joo JE, Park YK, Lee SH, Song BY |title=A rare case of epiphyseal chondromyxoid fibroma of the proximal tibia |journal=Korean J Radiol |volume=12 |issue=6 |pages=761–4 |date=2011 |pmid=22043162 |pmc=3194784 |doi=10.3348/kjr.2011.12.6.761 |url=}}</ref><ref name="pmid22094389">{{cite journal |vauthors=Gutiérrez-González R, De Reina L, Saab A, Jiménez-Heffernan J, García-Uría J |title=Chondromyxoid fibroma of the lumbar spine: case report and literature review |journal=Eur Spine J |volume=21 Suppl 4 |issue= |pages=S458–62 |date=June 2012 |pmid=22094389 |doi=10.1007/s00586-011-2078-x |url=}}</ref><ref name="pmid19644549">{{cite journal |vauthors=Morris LG, Rihani J, Lebowitz RA, Wang BY |title=Chondromyxoid fibroma of sphenoid sinus with unusual calcifications: case report with literature review |journal=Head Neck Pathol |volume=3 |issue=2 |pages=169–73 |date=June 2009 |pmid=19644549 |doi=10.1007/s12105-009-0121-6 |url=}}</ref><ref name="pmid27274412">{{cite journal |vauthors=Minasian T, Claus C, Hariri OR, Piao Z, Quadri SA, Yuhan R, Leong D, Tashjian V |title=Chondromyxoid fibroma of the sacrum: A case report and literature review |journal=Surg Neurol Int |volume=7 |issue=Suppl 13 |pages=S370–4 |date=2016 |pmid=27274412 |pmc=4879845 |doi=10.4103/2152-7806.182547 |url=}}</ref><ref name="pmid26413029">{{cite journal |vauthors=Kilic D, Findikcioglu A, Tepeoglu M, Vural C |title=Chondromyxoid Fibroma of the Sternum in a 63-Year-Old Woman |journal=Tex Heart Inst J |volume=42 |issue=4 |pages=400–2 |date=August 2015 |pmid=26413029 |pmc=4567104 |doi=10.14503/THIJ-14-4381 |url=}}</ref><ref name="pmid24987604">{{cite journal |vauthors=Fomete B, Adeosun OO, Awelimobor DI, Olayemi L |title=Chondromyxoid fibroma of the mandible: Case report and review of the literature |journal=Ann Maxillofac Surg |volume=4 |issue=1 |pages=78–80 |date=January 2014 |pmid=24987604 |pmc=4073468 |doi=10.4103/2231-0746.133072 |url=}}</ref> | |||
*[[ | | | ||
* Proximal [[tibia]] [[metaphysis]] | |||
*Distal [[femoral]] [[metaphysis]] | |||
| | |||
* Well circumscribed, [[metaphyseal]] lesion, and fragments of white-grey rubbery tissue are noted | |||
| | |||
*[[Spindle cells]] or [[Stellate cell|stellate cells]] in a myxoid or chondroid [[stroma]] | |||
*Lobules with hypocellular centers and hypercellular peripheries | |||
*[[Giant cells]] in the hypercellular periphery | |||
*Scattered [[Calcification|calcifications]]. | |||
*No true [[hyaline cartilage]] formation is seen | |||
*No [[Mitotic index|mitotic activity]] is seen | |||
| | |||
* ''GRM1'' [[gene fusion]] or [[Promoter region|promoter]] swapping noted | |||
* | |||
* | |||
* | |||
**[[ | |||
* | |||
* | |||
* It can be associated with a [[translocation]] at t(1;5)(p13;p13) | |||
| | |||
=== | *None | ||
|- | |||
|Uterine fibroma <ref name="pmid27974911">{{cite journal |vauthors=Manta L, Suciu N, Toader O, Purcărea RM, Constantin A, Popa F |title=The etiopathogenesis of uterine fibromatosis |journal=J Med Life |volume=9 |issue=1 |pages=39–45 |date=2016 |pmid=27974911 |pmc=5152611 |doi= |url=}}</ref><ref name="pmid25879625">{{cite journal |vauthors=Borahay MA, Al-Hendy A, Kilic GS, Boehning D |title=Signaling Pathways in Leiomyoma: Understanding Pathobiology and Implications for Therapy |journal=Mol. Med. |volume=21 |issue= |pages=242–56 |date=April 2015 |pmid=25879625 |pmc=4503645 |doi=10.2119/molmed.2014.00053 |url=}}</ref><ref name="pmid27454940">{{cite journal |vauthors=Miettinen M, Felisiak-Golabek A, Wasag B, Chmara M, Wang Z, Butzow R, Lasota J |title=Fumarase-deficient Uterine Leiomyomas: An Immunohistochemical, Molecular Genetic, and Clinicopathologic Study of 86 Cases |journal=Am. J. Surg. Pathol. |volume=40 |issue=12 |pages=1661–1669 |date=December 2016 |pmid=27454940 |pmc=5106328 |doi=10.1097/PAS.0000000000000703 |url=}}</ref><ref name="pmid26141720">{{cite journal |vauthors=Commandeur AE, Styer AK, Teixeira JM |title=Epidemiological and genetic clues for molecular mechanisms involved in uterine leiomyoma development and growth |journal=Hum. Reprod. Update |volume=21 |issue=5 |pages=593–615 |date=2015 |pmid=26141720 |pmc=4533663 |doi=10.1093/humupd/dmv030 |url=}}</ref><ref name="pmid12826476">{{cite journal |vauthors=Flake GP, Andersen J, Dixon D |title=Etiology and pathogenesis of uterine leiomyomas: a review |journal=Environ. Health Perspect. |volume=111 |issue=8 |pages=1037–54 |date=June 2003 |pmid=12826476 |pmc=1241553 |doi=10.1289/ehp.5787 |url=}}</ref><ref name="pmid16504804">{{cite journal |vauthors=Lobel MK, Somasundaram P, Morton CC |title=The genetic heterogeneity of uterine leiomyomata |journal=Obstet. Gynecol. Clin. North Am. |volume=33 |issue=1 |pages=13–39 |date=March 2006 |pmid=16504804 |doi=10.1016/j.ogc.2005.12.006 |url=}}</ref><ref name="pmid16564125">{{cite journal |vauthors=Wolańska M, Bańkowski E |title=Transforming growth factor beta and platelet-derived growth factor in human myometrium and in uterine leiomyomas at various stages of tumour growth |journal=Eur. J. Obstet. Gynecol. Reprod. Biol. |volume=130 |issue=2 |pages=238–44 |date=February 2007 |pmid=16564125 |doi=10.1016/j.ejogrb.2006.01.034 |url=}}</ref><ref name="pmid16443507">{{cite journal |vauthors=Baird DD, Kesner JS, Dunson DB |title=Luteinizing hormone in premenopausal women may stimulate uterine leiomyomata development |journal=J. Soc. Gynecol. Investig. |volume=13 |issue=2 |pages=130–5 |date=February 2006 |pmid=16443507 |doi=10.1016/j.jsgi.2005.12.001 |url=}}</ref><ref name="pmid8885057">{{cite journal |vauthors=Andersen J |title=Growth factors and cytokines in uterine leiomyomas |journal=Semin. Reprod. Endocrinol. |volume=14 |issue=3 |pages=269–82 |date=August 1996 |pmid=8885057 |doi=10.1055/s-2007-1016336 |url=}}</ref><ref name="pmid28875276">{{cite journal |vauthors=Laganà AS, Vergara D, Favilli A, La Rosa VL, Tinelli A, Gerli S, Noventa M, Vitagliano A, Triolo O, Rapisarda AMC, Vitale SG |title=Epigenetic and genetic landscape of uterine leiomyomas: a current view over a common gynecological disease |journal=Arch. Gynecol. Obstet. |volume=296 |issue=5 |pages=855–867 |date=November 2017 |pmid=28875276 |doi=10.1007/s00404-017-4515-5 |url=}}</ref><ref name="pmid1323302">{{cite journal |vauthors=Koutsilieris M |title=Pathophysiology of uterine leiomyomas |journal=Biochem. Cell Biol. |volume=70 |issue=5 |pages=273–8 |date=May 1992 |pmid=1323302 |doi= |url=}}</ref> | |||
| | |||
* Intra-uterine: | |||
* Intramural [[leiomyoma]] | |||
*Subserosal [[leiomyoma]] | |||
*[[Submucosal]] [[leiomyoma]] | |||
=== | |||
* | |||
* | |||
* Extra-uterine: | |||
* | * [[Broad ligament]] [[leiomyoma]] | ||
*When multiple fibroids are present they frequently have unrelated genetic defects. Specific mutations of the ''MED12'' protein have been noted in 70 | *[[Cervical]] [[leiomyoma]] | ||
*If a mother had fibroids, risk in the daughter is about three times higher than average. Researchers have found that only a few specific genes or cytogenetic deviations are associated with [[uterine leiomyomas]]. An association with fatty acid synthase has been reported. | *[[Parasitic]] [[leiomyoma]] | ||
*Diffuse [[uterine]] [[leiomyomatosis]] | |||
| | |||
* Round, well circumscribed (but not encapsulated), [[solid]] [[nodules]] that are white or tan, and show whorled appearance | |||
*CD10 positive | | | ||
*SMA positive | * [[Spindle cells]] arranged in [[fascicles]]. | ||
* Fascicular appearance: Adjacent groups of [[cells]] have their long axis perpendicular to one another. | |||
* Whorled arrangement of [[cells]]. | |||
* These [[cells]] are uniform in size and shape, with scarce [[mitoses]]. | |||
* There are three [[benign]] variants: bizarre (atypical); [[cellular]]; and [[Mitotic|mitotically active]]. | |||
* The appearance of prominent [[nucleoli]] with perinucleolar halos should alert the [[pathologist]] to investigate the possibility of the extremely rare [[hereditary]] [[Leiomyomatosis familial|leiomyomatosis]] and [[renal cell cancer]] (Reed) syndrome. | |||
| | |||
* When multiple [[fibroids]] are present they frequently have unrelated [[genetic defects]]. Specific mutations of the ''[[MED12]]'' protein have been noted in 70% of [[fibroids]]. | |||
* If a mother had [[fibroids]], risk in the daughter is about three times higher than average. Researchers have found that only a few specific [[genes]] or [[cytogenetic]] deviations are associated with [[Leiomyoma|uterine leiomyomas]]. An association with [[fatty acid synthase]] has been reported. | |||
*[[CD10]] positive | |||
*[[SMA]] positive | |||
*[[Desmin]] positive | *[[Desmin]] positive | ||
*H-caldesmon positive | *H-caldesmon positive | ||
*p16 negative | *[[p16]] negative | ||
*Ki-67 negative | *[[Ki-67]] negative | ||
| | |||
[[ | * A syndrome (Reed's syndrome) that causes uterine leiomyomata along with cutaneous leiomyomata and [[renal cell cancer]] has been reported. | ||
* This is associated with a [[mutation]] in the [[gene]] that produces the [[enzyme]] [[fumarate hydratase]], located on the long arm of [[Chromosome 1|chromosome]] 1 (''1q42.3-43''). Inheritance is [[autosomal dominant]]. | |||
|- | |||
|Ossifying Fibroma <ref name="pmid24678936">{{cite journal |vauthors=Wang TT, Zhang R, Wang L, Chen Y, Dong Q, Li TJ |title=Two cases of multiple ossifying fibromas in the jaws |journal=Diagn Pathol |volume=9 |issue= |pages=75 |date=March 2014 |pmid=24678936 |pmc=3974450 |doi=10.1186/1746-1596-9-75 |url=}}</ref><ref name="pmid27658992">{{cite journal |vauthors=Chen Y, Hu DY, Wang TT, Zhang R, Dong Q, Xu ZX, Wang L, Li TJ |title=CDC73 gene mutations in sporadic ossifying fibroma of the jaws |journal=Diagn Pathol |volume=11 |issue=1 |pages=91 |date=September 2016 |pmid=27658992 |pmc=5034632 |doi=10.1186/s13000-016-0532-0 |url=}}</ref><ref name="pmid24431886">{{cite journal |vauthors=Maria A, Sharma Y, Malik M |title=Juvenile ossifying fibroma of mandible: a case report |journal=J Maxillofac Oral Surg |volume=12 |issue=4 |pages=447–50 |date=December 2013 |pmid=24431886 |doi=10.1007/s12663-010-0122-8 |url=}}</ref><ref name="pmid29373206">{{cite journal |vauthors=Alghonaim Y, ALRashed ALHumaid S, Arafat A |title=Aggressive ossifying fibroma of right ethmoidal sinus: A case report |journal=Int J Surg Case Rep |volume=53 |issue= |pages=513–516 |date=2018 |pmid=29373206 |pmc=6290393 |doi=10.1016/j.ijscr.2017.12.026 |url=}}</ref><ref name="pmid29151945">{{cite journal |vauthors=Liu Y, Shan XF, Guo XS, Xie S, Cai ZG |title=Clinicopathological Characteristics and Prognosis of Ossifying Fibroma in the Jaws of Children: A Retrospective Study |journal=J Cancer |volume=8 |issue=17 |pages=3592–3597 |date=2017 |pmid=29151945 |pmc=5687175 |doi=10.7150/jca.21556 |url=}}</ref><ref name="pmid28381325">{{cite journal |vauthors=Liu JJ, Thompson LD, Janisiewicz AM, Shibuya TY, Keschner DB, Garg R, Lee JT |title=Ossifying fibroma of the maxilla and sinonasal tract: Case series |journal=Allergy Rhinol (Providence) |volume=8 |issue=1 |pages=32–36 |date=March 2017 |pmid=28381325 |pmc=5380450 |doi=10.2500/ar.2017.8.0190 |url=}}</ref><ref name="pmid25738089">{{cite journal |vauthors=Misra SR, Saigal A, Rastogi V, Priyadarshini SR, Pati AR |title=Giant central ossifying fibroma of the maxilla presenting with a pus discharging intra-oral sinus |journal=J Clin Diagn Res |volume=9 |issue=1 |pages=ZD08–11 |date=January 2015 |pmid=25738089 |pmc=4347180 |doi=10.7860/JCDR/2015/11192.5417 |url=}}</ref> | |||
| | |||
*[[Tibia]]: predilection for the cortex of the tibial [[diaphysis]]. | |||
*[[Femur]] | |||
| | |||
* Discrete [[mass]] that is well delineated from surrounding [[bone]], tan-white, rubbery cut surface, firm to gritty and no [[Encapsulation (pharmacology)|encapsulation]] | |||
| | |||
* They comprise of haphazardly distributed lamellated bony spicules on a background of [[fibrous]] [[stroma]] | |||
* The lesion has a zonal architecture with a center of immature [[bone]] surrounded by more mature lamellar bone. | |||
* The central spicules of woven bony [[trabeculae]] are lined by a layer of [[osteoblasts]]. The background is a loose and storiform [[fibrous tissue]]. | |||
| | |||
*[[Ossifying fibromas]] are [[keratin]] positive - isolated cells accepted by some. | |||
*It is [[osteonectin]], [[neurofibromin]], and [[S-100]] protein positive. | |||
| | |||
* Clonal [[chromosomal abnormalities]] such as [[trisomies]] of [[chromosomes]] 7, 8, 12 ,21, and/or 22 | |||
* [[Adamantinoma]] | |||
|- | |||
|Non-ossifying Fibroma <ref name="pmid23008139">{{cite journal |vauthors=Bowers LM, Cohen DM, Bhattacharyya I, Pettigrew JC, Stavropoulos MF |title=The non-ossifying fibroma: a case report and review of the literature |journal=Head Neck Pathol |volume=7 |issue=2 |pages=203–10 |date=June 2013 |pmid=23008139 |doi=10.1007/s12105-012-0399-7 |url=}}</ref><ref name="pmid27044378">{{cite journal |vauthors=Herget GW, Mauer D, Krauß T, El Tayeh A, Uhl M, Südkamp NP, Hauschild O |title=Non-ossifying fibroma: natural history with an emphasis on a stage-related growth, fracture risk and the need for follow-up |journal=BMC Musculoskelet Disord |volume=17 |issue= |pages=147 |date=April 2016 |pmid=27044378 |pmc=4820930 |doi=10.1186/s12891-016-1004-0 |url=}}</ref><ref name="pmid29081852">{{cite journal |vauthors=Goldin A, Muzykewicz DA, Dwek J, Mubarak SJ |title=The aetiology of the non-ossifying fibroma of the distal femur and its relationship to the surrounding soft tissues |journal=J Child Orthop |volume=11 |issue=5 |pages=373–379 |date=October 2017 |pmid=29081852 |pmc=5643931 |doi=10.1302/1863-2548.11.170068 |url=}}</ref> | |||
| | |||
*[[Metaphysis]] of distal [[femur]] or proximal [[tibia]] (80%) | |||
*Cortical | |||
| | |||
* Fleshy, [[fibrous]], yellow or tan-brown lesion with variable areas of [[haemorrhage]] are noted | |||
| | |||
* [[Spindle cells]] without [[Cytological|cytologic]] [[atypia]] are arranged in a storiform pattern. | |||
* Scattered chronic [[inflammatory cells]] and [[benign]] [[giant cells]]. | |||
*[[Foam cells]] and [[hemosiderin]] deposition are present. | |||
*[[Mitoses]] are seen but [[Cytological|cytologic]] [[atypia]] is absent. | |||
| | |||
* Clonal rearrangements in [[chromosomes]] 1, 3, 4, 11, and 14 are noted in NOFs (non-ossifying fibroma) of bone | |||
| | |||
*[[Neurofibromatosis type I|Neurofibromatosis-type 1]] (NF1) | |||
* [[Fibrous dysplasia]] | |||
* [[Jaffe-Campanacci syndrome]] | |||
|- | |||
|Desmoplastic Fibroma <ref name="pmid19930688">{{cite journal |vauthors=Schneider M, Zimmermann AC, Depprich RA, Kübler NR, Engers R, Naujoks CD, Handschel J |title=Desmoplastic fibroma of the mandible--review of the literature and presentation of a rare case |journal=Head Face Med |volume=5 |issue= |pages=25 |date=November 2009 |pmid=19930688 |doi=10.1186/1746-160X-5-25 |url=}}</ref><ref name="pmid23459513">{{cite journal |vauthors=Nedopil A, Raab P, Rudert M |title=Desmoplastic fibroma: a case report with three years of clinical and radiographic observation and review of the literature |journal=Open Orthop J |volume=8 |issue= |pages=40–6 |date=2013 |pmid=23459513 |doi=10.2174/1874325001307010040 |url=}}</ref><ref name="pmid26622872">{{cite journal |vauthors=Gong YB, Qu LM, Qi X, Liu JG |title=Desmoplastic fibroma in the proximal femur: A case report with long-term follow-up |journal=Oncol Lett |volume=10 |issue=4 |pages=2465–2467 |date=October 2015 |pmid=26622872 |doi=10.3892/ol.2015.3603 |url=}}</ref><ref name="pmid15937674">{{cite journal |vauthors=Daneyemez M, Akay KM, Izci Y |title=Desmoplastic fibroma of the cervical spine |journal=Eur Spine J |volume=14 |issue=8 |pages=799–802 |date=October 2005 |pmid=15937674 |doi=10.1007/s00586-005-0904-8 |url=}}</ref><ref name="pmid25113037">{{cite journal |vauthors=Woods TR, Cohen DM, Islam MN, Rawal Y, Bhattacharyya I |title=Desmoplastic fibroma of the mandible: a series of three cases and review of literature |journal=Head Neck Pathol |volume=9 |issue=2 |pages=196–204 |date=June 2015 |pmid=25113037 |doi=10.1007/s12105-014-0561-5 |url=}}</ref><ref name="pmid23682186">{{cite journal |vauthors=Goyal T, Rastogi S, Tripathy SK |title=Desmoplastic fibroma of ulna: Excision and reconstruction of olecranon with a fibular graft |journal=Indian J Orthop |volume=47 |issue=2 |pages=207–10 |date=March 2013 |pmid=23682186 |pmc=3654474 |doi=10.4103/0019-5413.108928 |url=}}</ref><ref name="pmid26909301">{{cite journal |vauthors=Evans S, Ramasamy A, Jeys L, Grimer R |title=Desmoplastic fibroma of bone: A rare bone tumour |journal=J Bone Oncol |volume=3 |issue=3-4 |pages=77–9 |date=November 2014 |pmid=26909301 |pmc=4723648 |doi=10.1016/j.jbo.2014.08.001 |url=}}</ref> | |||
| | |||
*[[Mandible]] (22%) and the [[metaphysis]] of long bones (56%). | |||
*[[Pelvis]] | |||
| | |||
| | |||
* Lamellar bone | |||
* Fibrotic [[marrow]] space has following features: | |||
**[[Collagen]] | |||
** Low cellularity | |||
**[[Spindle cells]] without significant [[atypia]] | |||
* On [[histopathology]], desmoplastic fibromas are identical to soft tissue [[Desmoid tumor|desmoid tumors]], with abundant [[collagenous]] [[stroma]] and little cellularity or [[pleomorphism]]. | |||
* The main cell types that are seen include the following: | |||
** [[Fibroblasts]] | |||
** [[Myofibroblasts]] | |||
** Undifferentiated mesenchymal cells | |||
| | |||
*Strong positive for the adhesion protein β-[[Catenin]] | |||
*Weak positive labelling for [[S-100]] | |||
*No positive stain for the proliferation marker [[Ki67]] | |||
| | |||
* No associated conditions | |||
|- | |||
|Pleural Fibroma <ref name="pmid23503999">{{cite journal |vauthors=Aremu AA, Oyedeji OA, Asaleye CM, Adetiloye VA |title=An elusive chest coin in an African child: a pleural fibroma's long, tortuous path to freedom |journal=Pan Afr Med J |volume=14 |issue= |pages=16 |date=2013 |pmid=23503999 |pmc=3597858 |doi=10.11604/pamj.2013.14.16.1874 |url=}}</ref><ref name="pmid25878653">{{cite journal |vauthors=Hassan S, Husain SS, Anwar MA, Saeed S |title=Pleural Fibroma; A meandering path to surgical removal |journal=Pak J Med Sci |volume=31 |issue=1 |pages=236–8 |date=2015 |pmid=25878653 |pmc=4386196 |doi=10.12669/pjms.311.5517 |url=}}</ref><ref name="pmid28660826">{{cite journal |vauthors=Ali JM, Ali A, Van Leuven M, Bartosik WR |title=Giant solitary fibrous tumour of the pleura an unpredictable entity: case series and literature review |journal=Ann R Coll Surg Engl |volume=99 |issue=6 |pages=e165–e171 |date=July 2017 |pmid=28660826 |pmc=5696978 |doi=10.1308/rcsann.2017.0067 |url=}}</ref><ref name="pmid26632548">{{cite journal |vauthors=Supakul R, Sodhi A, Tamashiro CY, Azmi SS, Kadaria D |title=Solitary Fibrous Tumor of the Pleura: A Rare Cause of Pleural Mass |journal=Am J Case Rep |volume=16 |issue= |pages=854–7 |date=December 2015 |pmid=26632548 |pmc=4671454 |doi= |url=}}</ref><ref name="pmid22014289">{{cite journal |vauthors=Guo W, Xiao HL, Jiang YG, Wang RW, Zhao YP, Ma Z, Niu HJ |title=Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review of the literature |journal=World J Surg Oncol |volume=9 |issue= |pages=134 |date=October 2011 |pmid=22014289 |pmc=3214850 |doi=10.1186/1477-7819-9-134 |url=}}</ref><ref name="pmid22833820">{{cite journal |vauthors=Chu X, Zhang L, Xue Z, Ren Z, Sun YE, Wang M, Liu M |title=Solitary fibrous tumor of the pleura: An analysis of forty patients |journal=J Thorac Dis |volume=4 |issue=2 |pages=146–54 |date=April 2012 |pmid=22833820 |doi=10.3978/j.issn.2072-1439.2012.01.05 |url=}}</ref><ref name="pmid20628740">{{cite journal |vauthors=Guo J, Chu X, Sun YE, Zhang L, Zhou N |title=Giant solitary fibrous tumor of the pleura: an analysis of five patients |journal=World J Surg |volume=34 |issue=11 |pages=2553–7 |date=November 2010 |pmid=20628740 |pmc=2949573 |doi=10.1007/s00268-010-0715-x |url=}}</ref><ref name="pmid1792644">{{cite journal |vauthors=Moat NE, Teale JD, Lea RE, Matthews AW |title=Spontaneous hypoglycaemia and pleural fibroma: role of insulin like growth factors |journal=Thorax |volume=46 |issue=12 |pages=932–3 |date=December 1991 |pmid=1792644 |pmc=463503 |doi=10.1136/thx.46.12.932 |url=}}</ref><ref name="pmid1792643">{{cite journal |vauthors=Masson EA, MacFarlane IA, Graham D, Foy P |title=Spontaneous hypoglycaemia due to a pleural fibroma: role of insulin like growth factors |journal=Thorax |volume=46 |issue=12 |pages=930–1 |date=December 1991 |pmid=1792643 |doi=10.1136/thx.46.12.930 |url=}}</ref><ref name="pmid28049955">{{cite journal |vauthors=Vejvodova S, Spidlen V, Mukensnabl P, Krakorova G, Molacek J, Vodicka J |title=Solitary Fibrous Tumor - Less Common Neoplasms of the Pleural Cavity |journal=Ann Thorac Cardiovasc Surg |volume=23 |issue=1 |pages=12–18 |date=February 2017 |pmid=28049955 |pmc=5347482 |doi=10.5761/atcs.oa.16-00108 |url=}}</ref><ref name="pmid23832995">{{cite journal |vauthors=Rahnemai-Azar AA, Rahnemai-Aazr AA, Robinson P, Pham S |title=Solitary fibrous tumour of the pleura masquerading as catecholamine-secreting paraganglioma |journal=BMJ Case Rep |volume=2013 |issue= |pages= |date=July 2013 |pmid=23832995 |pmc=3736364 |doi=10.1136/bcr-2013-009939 |url=}}</ref><ref name="pmid28063145">{{cite journal |vauthors=Ichiki Y, Kakizoe K, Hamatsu T, Matsuyama A, Suehiro T, Tanaka F, Hisaoka M, Sugimachi K |title=Solitary fibrous tumor of the lung: a case report |journal=Surg Case Rep |volume=3 |issue=1 |pages=10 |date=December 2017 |pmid=28063145 |pmc=5218951 |doi=10.1186/s40792-016-0286-7 |url=}}</ref> | |||
| | |||
* 80% of [[pleural fibroma]]<nowiki/>s originate in the [[visceral pleura]], while 20% arise from [[parietal pleura]]. | |||
| | |||
| | |||
* Composed of irregularly arranged [[fascicles]] comprising of [[spindle cells]] with [[collagen]] separation. | |||
* They originate from submesothelial mesenchymal cells. | |||
* Myxoid or cystic degeneration can occur. | |||
| | |||
* Recurrent [[somatic]] fusions of the two [[genes]], ''[[STAT6]]'', located at chromosomal region ''[[12q13]]'', have been identified in pleural fibromas. | |||
| | |||
* Some pleural fibromas are associated with the paraneoplastic Doege–Potter syndrome, which is caused by tumor production of [[IGF-2]]. | |||
* [[Hypoglycaemia]]: 2-4% 6, thought to be due to production of IGF-2 | |||
* [[Hypertrophic pulmonary osteoarthropathy]] (HPOA): ~20% 6: thought to be due to abnormal production of [[hyaluronic acid]] | |||
|- | |||
|Cardiac Fibroma <ref name="pmid22472419">{{cite journal |vauthors=Torimitsu S, Nemoto T, Wakayama M, Okubo Y, Yokose T, Kitahara K, Ozawa T, Nakayama H, Shinozaki M, Sasai D, Ishiwatari T, Takuma K, Shibuya K |title=Literature survey on epidemiology and pathology of cardiac fibroma |journal=Eur. J. Med. Res. |volume=17 |issue= |pages=5 |date=March 2012 |pmid=22472419 |pmc=3351722 |doi=10.1186/2047-783X-17-5 |url=}}</ref><ref name="pmid25887953">{{cite journal |vauthors=Jha NK, Kiraly L, Tamas C, Talo H, Khan MD, El Badaoui H, Jain A, Hammad A |title=Large cardiac fibroma and teratoma in children- case reports |journal=J Cardiothorac Surg |volume=10 |issue= |pages=38 |date=March 2015 |pmid=25887953 |pmc=4373309 |doi=10.1186/s13019-015-0242-9 |url=}}</ref><ref name="pmid7580366">{{cite journal |vauthors=Busch U, Kampmann C, Meyer R, Sandring KH, Hausdorf G, Konertz W |title=Removal of a giant cardiac fibroma from a 4-year-old child |journal=Tex Heart Inst J |volume=22 |issue=3 |pages=261–4 |date=1995 |pmid=7580366 |pmc=325263 |doi= |url=}}</ref><ref name="pmid16572881">{{cite journal |vauthors=Bossert T, Walther T, Vondrys D, Gummert JF, Kostelka M, Mohr FW |title=Cardiac fibroma as an inherited manifestation of nevoid basal-cell carcinoma syndrome |journal=Tex Heart Inst J |volume=33 |issue=1 |pages=88–90 |date=2006 |pmid=16572881 |pmc=1413607 |doi= |url=}}</ref><ref name="pmid29336396">{{cite journal |vauthors=Heidari A, Sabzi F, Faraji R |title=Right atrial fibroma in an adult patient |journal=Ann Card Anaesth |volume=21 |issue=1 |pages=65–67 |date=2018 |pmid=29336396 |pmc=5791493 |doi=10.4103/aca.ACA_121_17 |url=}}</ref><ref name="pmid18329553">{{cite journal |vauthors=Scanlan D, Radio SJ, Nelson M, Zhou M, Streblow R, Prasad V, Reyes C, Perry D, Fletcher S, Bridge JA |title=Loss of the PTCH1 gene locus in cardiac fibroma |journal=Cardiovasc. Pathol. |volume=17 |issue=2 |pages=93–7 |date=2008 |pmid=18329553 |pmc=2342874 |doi=10.1016/j.carpath.2007.08.001 |url=}}</ref><ref name="pmid27067427">{{cite journal |vauthors=Ying L, Lin R, Gao Z, Qi J, Zhang Z, Gu W |title=Primary cardiac tumors in children: a center's experience |journal=J Cardiothorac Surg |volume=11 |issue=1 |pages=52 |date=April 2016 |pmid=27067427 |doi=10.1186/s13019-016-0448-5 |url=}}</ref><ref name="pmid23102388">{{cite journal |vauthors=Yadava OP |title=Cardiac tumours in infancy |journal=Indian Heart J |volume=64 |issue=5 |pages=492–6 |date=2012 |pmid=23102388 |pmc=3861228 |doi=10.1016/j.ihj.2012.05.004 |url=}}</ref><ref name="pmid26457206">{{cite journal |vauthors=Cho SH, Fritz T, Cronin LJ, Cohle SD |title=Primary Cardiac Fibroma in an Adult |journal=Case Rep Cardiol |volume=2015 |issue= |pages=713702 |date=2015 |pmid=26457206 |doi=10.1155/2015/713702 |url=}}</ref><ref name="pmid23847693">{{cite journal |vauthors=Mecchia D, Lavezzi AM, Matturri L |title=Primary Cardiac Fibroma and Cardiac Conduction System Alterations in a Case of Sudden Death of a 4-month-old Infant |journal=Open Cardiovasc Med J |volume=7 |issue= |pages=47–9 |date=2013 |pmid=23847693 |pmc=3706798 |doi=10.2174/1874192401307010047 |url=}}</ref> | |||
| | |||
*[[Ventricular septum]] and left ventricular free wall. | |||
| | |||
* Well defined, solitary, intramyocardial lesions with smooth margins and usually large, with a mean diameter of ~5 cm | |||
| | |||
* Usually have no foci of cystic change, [[hemorrhage]], or [[necrosis]]. [[Calcification]] is common | |||
| | |||
*None | |||
| | |||
* There is an increased prevalence of cardiac fibromas in [[Gorlin syndrome]]. | |||
|- | |||
|Renal Medullary Fibroma <ref name="pmid24228211">{{cite journal |vauthors=Kumar S, Choudhary GR, Nanjappa B, Bal A |title=Benign medullary fibroma of the kidney: a rare diagnostic dilemma |journal=J Clin Imaging Sci |volume=3 |issue= |pages=43 |date=2013 |pmid=24228211 |pmc=3823390 |doi=10.4103/2156-7514.120776 |url=}}</ref><ref name="pmid11054036">{{cite journal |vauthors=Bircan S, Orhan D, Tulunay O, Safak M |title=Renomedullary interstitial cell tumor |journal=Urol. Int. |volume=65 |issue=3 |pages=163–6 |date=2000 |pmid=11054036 |doi=10.1159/000064864 |url=}}</ref><ref name="pmid24642074">{{cite journal |vauthors=Bazzi WM, Huang H, Al-Ahmadie H, Russo P |title=Clinicopathologic features of renomedullary interstitial cell tumor presenting as the main solid renal mass |journal=Urology |volume=83 |issue=5 |pages=1104–6 |date=May 2014 |pmid=24642074 |doi=10.1016/j.urology.2014.01.008 |url=}}</ref> | |||
| | |||
*[[Renal medulla]] | |||
| | |||
* Small, and white well circumscribed [[nodule]] in medulla typically less than 3mm are characteristic findings of renal medullary fibroma | |||
| | |||
* Small polygonal/stellate cells | |||
* Abundant loose/myxoid stroma | |||
* Entrapped [[renal tubules]] may be present | |||
| | |||
*None | |||
| | |||
* No associated conditions | |||
|- | |||
|Cemento-ossifying Fibroma <ref name="pmid28439606">{{cite journal |vauthors=Bala TK, Soni S, Dayal P, Ghosh I |title=Cemento-ossifying fibroma of the mandible. A clinicopathological report |journal=Saudi Med J |volume=38 |issue=5 |pages=541–545 |date=May 2017 |pmid=28439606 |pmc=5447217 |doi=10.15537/smj.2017.5.15643 |url=}}</ref><ref name="pmid21760674">{{cite journal |vauthors=Chatterjee A, Ajmera N, Singh A |title=Peripheral cemento-ossifying fibroma of maxilla |journal=J Indian Soc Periodontol |volume=14 |issue=3 |pages=186–9 |date=July 2010 |pmid=21760674 |pmc=3100863 |doi=10.4103/0972-124X.75915 |url=}}</ref><ref name="pmid24303483">{{cite journal |vauthors=Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H |title=Peripheral cemento-ossifying fibroma: A case report with review of literature |journal=World J Clin Cases |volume=1 |issue=3 |pages=128–33 |date=June 2013 |pmid=24303483 |pmc=3845913 |doi=10.12998/wjcc.v1.i3.128 |url=}}</ref><ref name="pmid21503260">{{cite journal |vauthors=Dalghous A, Alkhabuli JO |title=Cemento-ossifying fibroma occurring in an elderly patient. A case report and a review of literature |journal=Libyan J Med |volume=2 |issue=2 |pages=95–8 |date=June 2007 |pmid=21503260 |pmc=3078280 |doi=10.4176/061220 |url=}}</ref><ref name="pmid22091236">{{cite journal |vauthors=Hekmatnia A, Ghazavi A, Saboori M, Mahzouni P, Tayari N, Hekmatnia F |title=A case report of cemento-ossifying fibroma presenting as a mass of the ethmoid sinus |journal=J Res Med Sci |volume=16 |issue=2 |pages=224–8 |date=February 2011 |pmid=22091236 |pmc=3214308 |doi= |url=}}</ref><ref name="pmid27174452">{{cite journal |vauthors=Katti G, Khan MM, Chaubey SS, Amena M |title=Cemento-ossifying fibroma of the jaw |journal=BMJ Case Rep |volume=2016 |issue= |pages= |date=May 2016 |pmid=27174452 |pmc=4885328 |doi=10.1136/bcr-2015-214327 |url=}}</ref><ref name="pmid22557904">{{cite journal |vauthors=Ram R, Singhal A, Singhal P |title=Cemento-ossifying fibroma |journal=Contemp Clin Dent |volume=3 |issue=1 |pages=83–5 |date=January 2012 |pmid=22557904 |pmc=3341766 |doi=10.4103/0976-237X.94553 |url=}}</ref><ref name="pmid22629060">{{cite journal |vauthors=Sah K, Kale AD, Hallikerimath S, Chandra S |title=Peripheral cemento-ossifying fibroma: Report of a recurrence case |journal=Contemp Clin Dent |volume=3 |issue=Suppl 1 |pages=S23–5 |date=April 2012 |pmid=22629060 |pmc=3354807 |doi=10.4103/0976-237X.95098 |url=}}</ref><ref name="pmid24678226">{{cite journal |vauthors=Naik RM, Guruprasad Y, Sujatha D, Gurudath S, Pai A, Suresh K |title=Giant cemento-ossifying fibroma of the mandible |journal=J Nat Sci Biol Med |volume=5 |issue=1 |pages=190–4 |date=January 2014 |pmid=24678226 |pmc=3961933 |doi=10.4103/0976-9668.127326 |url=}}</ref><ref name="PereiraDiniz2018">{{cite journal|last1=Pereira|first1=Thaís dos Santos Fontes|last2=Diniz|first2=Marina Gonçalves|last3=França|first3=Josiane Alves|last4=Moreira|first4=Rennan Garcias|last5=Menezes|first5=Grazielle Helena Ferreira de|last6=Sousa|first6=Sílvia Ferreira de|last7=Castro|first7=Wagner Henriques de|last8=Gomes|first8=Carolina Cavaliéri|last9=Gomez|first9=Ricardo Santiago|title=The Wnt/β-catenin pathway is deregulated in cemento-ossifying fibromas|journal=Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology|volume=125|issue=2|year=2018|pages=172–178|issn=22124403|doi=10.1016/j.oooo.2017.10.004}}</ref> | |||
== | | | ||
*[[Maxillary]] [[gingiva]] is involved more often than the [[mandibular]] [[gingiva]] | |||
| | |||
* Solid, [[sessile]] or [[pedunculated]] [[mass]], which is often [[Ulcerated lesion|ulcerated]], and generally has a diameter of less than 2 cm are characteristic findings of cemento-ossifying fibroma. | |||
*An unencapsulated mass of fibrous connective tissue that contains numerous characteristic large, plump, stellate and spindle-shaped fibroblasts, some of which are multinucleated | | | ||
*The surface epithelium is often atrophic and corrugated. | * Cemento -ossifying tumors are composed of [[fibrous tissue]], calcified tissue resembling [[bone]] and/or [[cementum]]. | ||
* The bone-like component is predominant reminiscent of woven bone and is found in more 'mature' lesions. | |||
* In some instances, this entity has been divided into cementifying fibroma and [[ossifying fibroma]] depending on the relative amounts of the tumor's constituent tissues. | |||
* Surface [[ulceration]] is common | |||
=== | | | ||
[[ | *None | ||
| | |||
* No associated conditions | |||
|- | |||
|Desmoplastic Fibroblastoma <ref name="pmid21221866">{{cite journal |vauthors=de Sousa SF, Caldeira PC, Grossmann Sde M, de Aguiar MC, Mesquita RA |title=Desmoplastic fibroblastoma (collagenous fibroma): a case identified in the buccal mucosa |journal=Head Neck Pathol |volume=5 |issue=2 |pages=175–9 |date=June 2011 |pmid=21221866 |doi=10.1007/s12105-010-0239-6 |url=}}</ref><ref name="pmid26855713">{{cite journal |vauthors=Pereira TD, de Lacerda JC, Porto-Matias MD, de Jesus AO, Gomez RS, Mesquita RA |title=Desmoplastic fibroblastoma (collagenous fibroma) of the oral cavity |journal=J Clin Exp Dent |volume=8 |issue=1 |pages=e89–92 |date=February 2016 |pmid=26855713 |doi=10.4317/jced.52605 |url=}}</ref><ref name="pmid29374633">{{cite journal |vauthors=Grewal R, Natter P, Makary R, Silliman J |title=Desmoplastic fibroblastoma of the left upper arm |journal=BMJ Case Rep |volume=2018 |issue= |pages= |date=January 2018 |pmid=29374633 |doi=10.1136/bcr-2017-221738 |url=}}</ref><ref name="pmid19503798">{{cite journal |vauthors=Osipov V, Carrera GF |title=Collagenous fibroma (desmoplastic fibroblastoma) with vertebral body erosion |journal=Sarcoma |volume=2009 |issue= |pages=682687 |date=2009 |pmid=19503798 |doi=10.1155/2009/682687 |url=}}</ref><ref name="pmid23504494">{{cite journal |vauthors=Nagaraja V, Coleman HG, Morgan GJ |title=Desmoplastic fibroblastoma presenting as a parotid tumour: a case report and review of the literature |journal=Head Neck Pathol |volume=7 |issue=3 |pages=285–90 |date=September 2013 |pmid=23504494 |pmc=3738752 |doi=10.1007/s12105-013-0435-2 |url=}}</ref><ref name="pmid22783503">{{cite journal |vauthors=Kim JH, Oh DY, Kim SW, Lee JH, Ahn ST, Rhie JW |title=Desmoplastic fibroblastoma of the finger tip in an adult |journal=Arch Plast Surg |volume=39 |issue=1 |pages=84–6 |date=January 2012 |pmid=22783503 |pmc=3385291 |doi=10.5999/aps.2012.39.1.84 |url=}}</ref> | |||
| | |||
*[[Shoulder]] region | |||
| | |||
| | |||
* [[Spindle cells]] or [[Stellate cell|stellate cells]] without nuclear [[atypia]] | |||
* Acellular [[stroma]] with abundant [[collagen]] | |||
* Myxoid areas may be present | |||
*[[Mitoses]] is rare | |||
| | |||
* ''[[FOSL1]]'' [[gene]] is involved in the pathogenesis of [[desmoplastic]] fibroblastoma, ''llq 12'' breakpoint described as being characteristic. | |||
* [[Beta-catenin]] -ve | |||
*Positive in desmoid-type fibromatosis | |||
*[[Desmin]] negative | |||
*[[S-100]] negative | |||
*[[CD34]] negative | |||
*[[MSA]] positive | |||
*Alpha-SMA positive | |||
| | |||
* No associated conditions | |||
|- | |||
|Elastofibroma <ref name="pmid21681661">{{cite journal |vauthors=Darling MR, Kutalowski M, MacPherson DG, Jackson-Boeters L, Wysocki GP |title=Oral elastofibromatous lesions: a review and case series |journal=Head Neck Pathol |volume=5 |issue=3 |pages=254–8 |date=September 2011 |pmid=21681661 |pmc=3173539 |doi=10.1007/s12105-011-0274-y |url=}}</ref><ref name="pmid19578045">{{cite journal |vauthors=Daum O, Ferda J, Curik R, Choc M, Mukensnabl P, Michal M |title=Elastofibromatous changes in tissues from spinal biopsies. A degenerative process afflicting a small but important subset of patients operated for spinal canal compression: report of 18 cases |journal=Int. J. Surg. Pathol. |volume=18 |issue=6 |pages=508–15 |date=December 2010 |pmid=19578045 |doi=10.1177/1066896909339736 |url=}}</ref><ref name="pmid20237986">{{cite journal |vauthors=Tosios KI, Economou I, Vasilopoulos NN, Koutlas IG |title=Elastofibromatous changes and hyperelastosis of the oral mucosa |journal=Head Neck Pathol |volume=4 |issue=1 |pages=31–6 |date=March 2010 |pmid=20237986 |pmc=2825534 |doi=10.1007/s12105-009-0153-y |url=}}</ref><ref name="pmid26890837">{{cite journal |vauthors=Smith HG, Hannay JA, Thway K, Messiou C, Smith MJ, Strauss DC, Hayes AJ |title=Elastofibroma dorsi: The clunking tumour that need not cause alarm |journal=Ann R Coll Surg Engl |volume=98 |issue=3 |pages=208–11 |date=March 2016 |pmid=26890837 |pmc=5226161 |doi=10.1308/rcsann.2016.0064 |url=}}</ref><ref name="pmid19628444">{{cite journal |vauthors=Kourda J, Ayadi-Kaddour A, Merai S, Hantous S, Miled KB, Mezni FE |title=Bilateral elastofibroma dorsi. A case report and review of the literature |journal=Orthop Traumatol Surg Res |volume=95 |issue=5 |pages=383–7 |date=September 2009 |pmid=19628444 |doi=10.1016/j.otsr.2009.05.002 |url=}}</ref><ref name="pmid19900325">{{cite journal |vauthors=Hoven-Gondrie ML, IJpma FF, Havenith MG, van Geldere D |title=[Elastofibroma dorsi: a characteristic, benign, subscapular swelling] |language=Dutch; Flemish |journal=Ned Tijdschr Geneeskd |volume=153 |issue= |pages=A569 |date=2009 |pmid=19900325 |doi= |url=}}</ref><ref name="pmid15063901">{{cite journal |vauthors=Hayes AJ, Alexander N, Clark MA, Thomas JM |title=Elastofibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom |journal=Eur J Surg Oncol |volume=30 |issue=4 |pages=450–3 |date=May 2004 |pmid=15063901 |doi=10.1016/j.ejso.2004.01.006 |url=}}</ref> | |||
| | |||
*[[Subscapular]] region. | |||
| | |||
* I'll defined, nonencapsulated, rubbery, firm, white lesion with interspersed [[fat]] and with moderate demarcation to surrounding tissue are characteristic findings of [[elastofibroma]]. | |||
* The [[tumors]] can be quite large (up to 20 cm), although most are around 5 cm. | |||
| | |||
* Thick bundles of [[collagen]] and [[elastin fibers]] are characteristic findings of [[elastofibroma]]. | |||
* Admixture of heavy dense bands of [[collagenous]] tissue dissected by fat and abnormal [[elastic fibers]]. | |||
* The [[elastic fibers]] are coarse, thick, and darkly [[eosinophilic]], often fragmented into globules, creating a "string of pearls" or "pipe cleaner" appearance. Because of degeneration, the [[elastic fibers]] will appear as globules with a serrated or "prickled" edge. | |||
| | |||
* There are alterations of [[short arm]] of [[chromosome]] 1 | |||
* Multifocality may suggest systemic enzymatic defect, resulting in abnormal [[elastogenesis]] | |||
* The [[elastic fibers]] will be visible on a Weigert or von Gieson elastic stains. | |||
| | |||
* No associated conditions | |||
|- | |||
|Sclerotic Fibroma <ref name="pmid20729948">{{cite journal |vauthors=Bhambri A, Del Rosso JQ |title=Solitary sclerotic fibroma |journal=J Clin Aesthet Dermatol |volume=2 |issue=6 |pages=36–8 |date=June 2009 |pmid=20729948 |pmc=2923956 |doi= |url=}}</ref><ref name="pmid18544068">{{cite journal |vauthors=Nakashima K, Yamada N, Adachi K, Yoshida Y, Yamamoto O |title=Solitary sclerotic fibroma of the skin: morphological characterization of the 'plywood-like pattern' |journal=J. Cutan. Pathol. |volume=35 Suppl 1 |issue= |pages=74–9 |date=October 2008 |pmid=18544068 |doi=10.1111/j.1600-0560.2008.01001.x |url=}}</ref><ref name="pmid1430474">{{cite journal |vauthors=Requena L, Gutiérrez J, Sánchez Yus E |title=Multiple sclerotic fibromas of the skin. A cutaneous marker of Cowden's disease |journal=J. Cutan. Pathol. |volume=19 |issue=4 |pages=346–51 |date=August 1992 |pmid=1430474 |doi= |url=}}</ref><ref name="pmid1491554">{{cite journal |vauthors=Mori O, Hachisuka H, Sasai Y |title=Sclerotic fibromas of the skin--reports of two cases and a review of the literature in Japan |journal=Kurume Med J |volume=39 |issue=3 |pages=191–3 |date=1992 |pmid=1491554 |doi= |url=}}</ref><ref name="pmid2258475">{{cite journal |vauthors=Lo WL, Wong CK |title=Solitary sclerotic fibroma |journal=J. Cutan. Pathol. |volume=17 |issue=5 |pages=269–73 |date=October 1990 |pmid=2258475 |doi= |url=}}</ref><ref name="pmid10698210">{{cite journal |vauthors=Hanft VN, Shea CR, McNutt NS, Pullitzer D, Horenstein MG, Prieto VG |title=Expression of CD34 in sclerotic ("plywood") fibromas |journal=Am J Dermatopathol |volume=22 |issue=1 |pages=17–21 |date=February 2000 |pmid=10698210 |doi= |url=}}</ref><ref name="pmid15059222">{{cite journal |vauthors=High WA, Stewart D, Essary LR, Kageyama NP, Hoang MP, Cockerell CJ |title=Sclerotic fibroma-like change in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity? |journal=J. Cutan. Pathol. |volume=31 |issue=5 |pages=373–8 |date=May 2004 |pmid=15059222 |doi=10.1111/j.0303-6987.2004.00199.x |url=}}</ref><ref name="pmid8600796">{{cite journal |vauthors=Shitabata PK, Crouch EC, Fitzgibbon JF, Swanson PE, Adesokan PN, Wick MR |title=Cutaneous sclerotic fibroma. Immunohistochemical evidence of a fibroblastic neoplasm with ongoing type I collagen synthesis |journal=Am J Dermatopathol |volume=17 |issue=4 |pages=339–43 |date=August 1995 |pmid=8600796 |doi= |url=}}</ref><ref name="pmid15166503">{{cite journal |vauthors=Alawi F, Freedman PD |title=Sporadic sclerotic fibroma of the oral soft tissues |journal=Am J Dermatopathol |volume=26 |issue=3 |pages=182–7 |date=June 2004 |pmid=15166503 |doi= |url=}}</ref> | |||
| | |||
*[[Skin]], may be solitary or multifocal | |||
| | |||
| | |||
* Well-delineated but unencapsulated mass of densely collagenized, hypocellular [[fibrous tissue]] with a storiform pattern, and prominent clefts between [[collagen]] bundles are characteristic findings of [[elastofibroma]]. | |||
| | |||
*[[CD34]] | |||
*[[Vimentin]] positive | |||
| | |||
* [[Cowden syndrome]] | |||
|- | |||
|Giant cell fibroma <ref name="pmid28785965">{{cite journal |vauthors=Upadhyaya JD, Cohen DM, Islam MN, Bhattacharyya I |title=Hybrid Central Odontogenic Fibroma with Giant Cell Granuloma like Lesion: A Report of Three Additional Cases and Review of the Literature |journal=Head Neck Pathol |volume=12 |issue=2 |pages=166–174 |date=June 2018 |pmid=28785965 |pmc=5953869 |doi=10.1007/s12105-017-0845-7 |url=}}</ref><ref name="pmid24511398">{{cite journal |vauthors=Sonalika WG, Sahu A, Deogade SC, Gupta P, Naitam D, Chansoria H, Agarwal J, Katoch S |title=Giant cell fibroma of tongue: understanding the nature of an unusual histopathological entity |journal=Case Rep Dent |volume=2014 |issue= |pages=864512 |date=2014 |pmid=24511398 |pmc=3910466 |doi=10.1155/2014/864512 |url=}}</ref><ref name="pmid20614305">{{cite journal |vauthors=Tosios KI, Gopalakrishnan R, Koutlas IG |title=So-called hybrid central odontogenic fibroma/central giant cell lesion of the jaws. A report on seven additional cases, including an example in a patient with cherubism, and hypotheses on the pathogenesis |journal=Head Neck Pathol |volume=2 |issue=4 |pages=333–8 |date=December 2008 |pmid=20614305 |pmc=2807578 |doi=10.1007/s12105-008-0076-z |url=}}</ref><ref name="pmid23248467">{{cite journal |vauthors=Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B |title=Giant cell fibroma: A clinicopathological study |journal=J Oral Maxillofac Pathol |volume=16 |issue=3 |pages=359–62 |date=September 2012 |pmid=23248467 |pmc=3519210 |doi=10.4103/0973-029X.102485 |url=}}</ref><ref name="pmid27822394">{{cite journal |vauthors=Mello-Moura AC, Santos AM, Bonini GA, Del Conte Zardetto CG, Moura-Netto C, Wanderley MT |title=Giant Cell Fibroma in a Two-Year-Old Child |journal=Case Rep Dent |volume=2016 |issue= |pages=7058356 |date=2016 |pmid=27822394 |pmc=5086372 |doi=10.1155/2016/7058356 |url=}}</ref><ref name="pmid30158768">{{cite journal |vauthors=Hosur MB, Puranik RS, Vanaki SS, Puranik SR, Ingaleshwar PS |title=Clinicopathological profile of central giant cell granulomas: An institutional experience and study of immunohistochemistry expression of p63 in central giant cell granuloma |journal=J Oral Maxillofac Pathol |volume=22 |issue=2 |pages=173–179 |date=2018 |pmid=30158768 |pmc=6097366 |doi=10.4103/jomfp.JOMFP_260_17 |url=}}</ref><ref name="pmid29391720">{{cite journal |vauthors=Kulkarni S, Chandrashekar C, Kudva R, Radhakrishnan R |title=Giant-cell fibroma: Understanding the nature of the melanin-laden cells |journal=J Oral Maxillofac Pathol |volume=21 |issue=3 |pages=429–433 |date=2017 |pmid=29391720 |pmc=5763868 |doi=10.4103/jomfp.JOMFP_209_16 |url=}}</ref><ref name="pmid24551733">{{cite journal |vauthors=Jimson S, Jimson S |title=Giant cell fibroma: a case report with immunohistochemical markers |journal=J Clin Diagn Res |volume=7 |issue=12 |pages=3079–80 |date=December 2013 |pmid=24551733 |pmc=3919395 |doi=10.7860/JCDR/2013/6476.3859 |url=}}</ref> | |||
| | |||
*[[Mandibular]] [[gingiva]], followed by the [[maxillary]] [[gingiva]], the [[tongue]], and the [[palate]]. | |||
| | |||
*[[Sessile]] or [[pedunculated]] [[nodule]] that is smaller than 1cm in diameter are characteristic findings of [[giant cell fibroma]]. Often, it has a bosselated or somewhat [[papillary]] surface. | |||
| | |||
* An unencapsulated mass of [[fibrous connective tissue]] that contains numerous characteristic large, plump, [[Stellate cell|stellate]] and spindle-shaped [[fibroblasts]], some of which are multinucleated. | |||
* The surface [[epithelium]] is often [[atrophic]] and corrugated. | |||
| | |||
*None | |||
| | |||
*No associated conditions | |||
|- | |||
|Peripheral Odontogenic Fibroma <ref name="pmid29333009">{{cite journal |vauthors=Chandna P, Srivastava N, Bansal V, Wadhwan V, Dubey P |title=Peripheral and Central Giant Cell Lesions in Children: Institutional Experience at Subharti Dental College and Hospital |journal=Indian J Med Paediatr Oncol |volume=38 |issue=4 |pages=440–446 |date=2017 |pmid=29333009 |pmc=5759061 |doi=10.4103/ijmpo.ijmpo_17_16 |url=}}</ref><ref name="pmid29354306">{{cite journal |vauthors=Wright JM, Soluk Tekkesin M |title=Odontogenic tumors: where are we in 2017 ? |journal=J Istanb Univ Fac Dent |volume=51 |issue=3 Suppl 1 |pages=S10–S30 |date=2017 |pmid=29354306 |pmc=5750825 |doi=10.17096/jiufd.52886 |url=}}</ref><ref name="pmid24920510">{{cite journal |vauthors=Reddy SV, Medikonda SK, Konda A, Natta S |title=A rare benign odontogenic neoplasm: peripheral odontogenic fibroma |journal=BMJ Case Rep |volume=2014 |issue= |pages= |date=June 2014 |pmid=24920510 |pmc=4069815 |doi=10.1136/bcr-2013-201065 |url=}}</ref><ref name="pmid22028517">{{cite journal |vauthors=Baiju CS, Rohatgi S |title=Peripheral odontogenic fibroma: A case report and review |journal=J Indian Soc Periodontol |volume=15 |issue=3 |pages=273–5 |date=July 2011 |pmid=22028517 |pmc=3200026 |doi=10.4103/0972-124X.85674 |url=}}</ref><ref name="pmid25210375">{{cite journal |vauthors=Sreeja C, Vezhavendan N, Shabana F, Vijayalakshmi D, Devi M, Arunakiry N |title=Recurrent peripheral odontogenic fibroma associated with basal cell budding |journal=J Pharm Bioallied Sci |volume=6 |issue=Suppl 1 |pages=S204–7 |date=July 2014 |pmid=25210375 |pmc=4157271 |doi=10.4103/0975-7406.137470 |url=}}</ref> | |||
| | |||
*[[Mandible]] | |||
|Firm, slowly growing, [[sessile]], and [[nodular]] growth of the [[gingiva]] are characteristic findings of peripheral odontogenic fibroma. | |||
| | |||
* An unencapsulated mass of interwoven cellular [[fibrous connective tissue]] that contains scattered nests or strands of [[odontogenic]] [[epithelium]] | |||
* It consists of [[cellular]] [[fibrous connective tissue]] parenchyma with non neoplastic islands, strands of [[Columnar epithelium|columnar]] or [[Cuboidal epithelia|cuboidal]] [[odontogenic]] [[epithelium]]. | |||
* Myxoid foci, osteoid, cementoid, or [[Dystrophic calcification|dystrophic calcifications]] are sometimes seen. | |||
* Generally, the surface is not [[Ulcerated lesion|ulcerated]]. | |||
| | |||
*None | |||
| | |||
*No associated conditions | |||
|} | |||
* | |||
= | {| class="wikitable" | ||
|+ | |||
!Type of fibroma | |||
!Gross image | |||
!Microscopic image | |||
|- | |||
|Ovarian fibroma | |||
|[[File:1200px-Fibroma of the Ovary.jpg|400px|thumb|none|Ed Uthman, MD [CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0)],https://upload.wikimedia.org/wikipedia/commons/0/04/Fibroma_of_the_Ovary.jpg,https://commons.wikimedia.org/wiki/File:Fibroma_of_the_Ovary.jpg]] | |||
|[[File:Ovarian fibroma 1.jpg|300px|thumb|none|Histopathology of ovarian fibroma showing benignspindle cellproliferation,Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M. Large twisted ovarian fibroma in menopausal women: a case report. Pan Afr Med J. 2015;20:322. Published 2015 Apr 6. doi:10.11604/pamj.2015.20.322.5998,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4491469/]] | |||
|- | |||
|Oral fibroma | |||
|[[File:Oral fibroma.jpeg|300px|thumb|center|Fibroma of oral mucosa,Klaus D. Peter, Gummersbach, Germany [CC BY 3.0 de (https://creativecommons.org/licenses/by/3.0/de/deed.en)],https://upload.wikimedia.org/wikipedia/commons/c/c5/Fibroma.jpg,https://commons.wikimedia.org/wiki/File:Fibroma.jpg]] | |||
|[[File:Oral fibroma -- low mag.jpg|300px|thumb|none|Librepath [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)],https://upload.wikimedia.org/wikipedia/commons/d/db/Oral_fibroma_--_low_mag.jpg,https://commons.wikimedia.org/wiki/File:Oral_fibroma_--_low_mag.jpg]] | |||
|- | |||
|Chondromyxoid fibroma | |||
| | |||
|[[File:Bone ChondromyxoidFibroma Calcium MP PA.JPG|300px|thumb|none|arahkayb [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)],https://upload.wikimedia.org/wikipedia/commons/a/a6/Bone_ChondromyxoidFibroma_Calcium_MP_PA.JPG,https://commons.wikimedia.org/wiki/File:Bone_ChondromyxoidFibroma_Calcium_MP_PA.JPG]] | |||
|- | |||
|Uterine fibroma | |||
|[[File:Uterine fibroids.jpg|300px|thumb|center|Hic et nunc [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)],https://upload.wikimedia.org/wikipedia/commons/f/f7/Uterine_fibroids.jpg,https://commons.wikimedia.org/wiki/File:Uterine_fibroids.jpg]] | |||
|[[File:Leiomyoma Uterus 40x.jpg|300px|thumb|none|Calicut Medical College [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)],https://upload.wikimedia.org/wikipedia/commons/e/ea/Leiomyoma_Uterus_40x.jpg,https://commons.wikimedia.org/wiki/File:Leiomyoma_Uterus_40x.jpg]] | |||
|- | |||
|Ossifying Fibroma | |||
| | |||
|[[File:Ossifying fibroma.jpg|300px|thumb|center|Histopathologicaly, this lesion is characterized by spindle cell proliferation packed with globular cementum droplets and round/ovoid fragments of woven bone. These spindle cells appear benign and associated with psammomatoid cementum droplets and some woven bone and consistent with aggressive ossifying fibroma, psammomatous type IV,Alghonaim Y, ALRashed ALHumaid S, Arafat A. Aggressive ossifying fibroma of right ethmoidal sinus: A case report. Int J Surg Case Rep. ;53:513–516. doi:10.1016/j.ijscr.2017.12.026,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290393/]] | |||
|- | |||
|Cardiac fibroma | |||
|[[File:Cardiac fibroma gross.jpg|300px|thumb|center|Jha NK, Kiraly L, Tamas C, et al. Large cardiac fibroma and teratoma in children- case reports. J Cardiothorac Surg. 2015;10:38. Published 2015 Mar 22. doi:10.1186/s13019-015-0242-9,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4373309/]] | |||
|[[File:Cardiac fibroma.jpg|300px|thumb|none|Fibroblast cells in fascicles with abundant collagen fiber,Heidari A, Sabzi F, Faraji R. Right atrial fibroma in an adult patient. Ann Card Anaesth. 2018;21(1):65–67. doi:10.4103/aca.ACA_121_17,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5791493/]] | |||
|- | |||
|Giant cell fibroma | |||
|[[File:Giant cell fibroma.jpg|300px|thumb|center|Pebbly appearance in right retromolar region,Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B. Giant cell fibroma: A clinicopathological study. J Oral Maxillofac Pathol. 2012;16(3):359–362. doi:10.4103/0973-029X.102485,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519210/]] | |||
|[[File:Giant cell fibroma 2.jpg|300px|thumb|none|Artifactual spacing was observed surrounding the giant cells,Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B. Giant cell fibroma: A clinicopathological study. J Oral Maxillofac Pathol. 2012;16(3):359–362. doi:10.4103/0973-029X.102485,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519210/]] | |||
|- | |||
|Peripheral odontogenic fibroma | |||
|[[File:Peripheral odontogenic fibroma.jpg|300px|thumb|center|Baiju CS, Rohatgi S. Peripheral odontogenic fibroma: A case report and review. J Indian Soc Periodontol. 2011;15(3):273–275. doi:10.4103/0972-124X.85674,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200026/]] | |||
|[[File:Peripheral odontogenic fibroma 1.jpg|300px|thumb|none|Baiju CS, Rohatgi S. Peripheral odontogenic fibroma: A case report and review. J Indian Soc Periodontol. 2011;15(3):273–275. doi:10.4103/0972-124X.85674,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3200026/]] | |||
|- | |||
|Elastofibroma | |||
|[[File:Elastofibroma1.jpg|300px|thumb|center|The typical location for bilateral elastofibroma dorsi in prone position and with slightly abducted arm,Sarici IS, Basbay E, Mustu M, et al. Bilateral elastofibroma dorsi: A case report. Int J Surg Case Rep. ;5(12):1139–1141. doi:10.1016/j.ijscr.2014.10.032,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4275815/]] | |||
|[[File:Elastofibroma.jpg|300px|thumb|none|High Power slide showing elastic fibres (pink areas) which confirms the diagnosis of elastofibroma. (Altered elastic fibres in a collagenous matrix),Pillay Y, Sabarathnam R. Elasto fibroma Dorsi: a case report of bilateral tumours and excision of the symptomatic lesion in a male patient. J Surg Case Rep. 2017;2017(11):rjx206. Published 2017 Nov 7. doi:10.1093/jscr/rjx206,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691368/]] | |||
|- | |||
|Desmoplastic fibroblastoma | |||
| | |||
|[[File:Desmoplastic fibroblastoma.jpg|300px|thumb|none|Grewal R, Natter P, Makary R, Silliman J. Desmoplastic fibroblastoma of the left upper arm. BMJ Case Rep. 2018;2018:bcr2017221738. Published 2018 Jan 26. doi:10.1136/bcr-2017-221738,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5786997/]] | |||
|- | |||
|Renal medullary fibroma | |||
|[[File:Renal medullary fibroma.jpg|300px|thumb|center|Renal medullary fibroma showing a firm grayish yellow calcified tumor (black arrow), renal hilum (white arrow),Kumar S, Choudhary GR, Nanjappa B, Bal A. Benign medullary fibroma of the kidney: a rare diagnostic dilemma. J Clin Imaging Sci. 2013;3:43. Published 2013 Oct 29. doi:10.4103/2156-7514.120776,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3823390/]] | |||
|[[File:Renal medullary fibroma1.jpg|300px|thumb|none|H&E stain showing bland spindle-shaped cells occurring singly within a loose stromal matrix (black arrow) and separated by thick collagen bundles (white arrow),Kumar S, Choudhary GR, Nanjappa B, Bal A. Benign medullary fibroma of the kidney: a rare diagnostic dilemma. J Clin Imaging Sci. 2013;3:43. Published 2013 Oct 29. doi:10.4103/2156-7514.120776,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3823390/]] | |||
|- | |||
|Pleural fibroma | |||
|[[File:Pleural fibroma.jpg|300px|thumb|center|Single multi nodular encapsulated pale white firm piece of tissue,Hassan S, Husain SS, Anwar MA, Saeed S. Pleural Fibroma; A meandering path to surgical removal. Pak J Med Sci. 2015;31(1):236–238. doi:10.12669/pjms.311.5517,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4386196/]] | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
|} | |||
==References== | ==References== | ||
| Line 542: | Line 768: | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Medicine]] | [[Category:Medicine]] | ||
Latest revision as of 17:40, 18 September 2019
|
Fibroma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fibroma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Fibroma pathophysiology |
|
Risk calculators and risk factors for Fibroma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Maneesha Nandimandalam, M.B.B.S.[2], Simrat Sarai, M.D. [3]
Overview
On gross pathology, polypoid lesion which is usually small, are characteristic findings of oral fibroma. On microscopic histopathological analysis, fibrous stroma, collagen bundles, prominent vessels, and overlying squamous mucosa with hyperkeratosis and focal ulceration are characteristic findings of oral fibroma. On gross pathology, well circumscribed, metaphyseal lesion, and fragments of white-grey rubbery tissue are characteristic findings of chondromyxoid fibroma. On microscopic histopathological analysis, spindle cells or stellate cells in a myxoid or chondroid stroma, lobules with hypocellular centers and hypercellular peripheries, giant cells in a hypercellular periphery, and scattered calcifications are characteristic findings of chondromyxoid fibroma. On gross pathology, fleshy, fibrous, yellow or tan-brown lesion with variable areas of haemorrhage are characteristic findings of non-ossifying fibroma. On microscopic histopathological analysis, spindle cells without cytologic atypia are arranged in a storiform pattern, scattered chronic inflammatory cells and benign giant cells, foam cells and hemosiderin deposition, and mitoses are characteristic findings of non-ossifying fibroma. On gross pathology, discrete mass that is well delineated from surrounding bone, tan-white, rubbery cut surface, firm to gritty and no encapsulation are characteristic findings of ossifying fibroma. On microscopic histopathological analysis, haphazardly distributed lamellated bony spicules on a background of fibrous stroma, a zonal architecture with a center of immature bone surrounded by more mature lamellar bone, and central spicules of woven bony trabeculae are lined by a layer of osteoblasts are characteristic findings of ossifying fibroma.[1][2]
Pathophysiology
| Type of fibroma | Location | Gross pathology | Microscpoic pathology | Genetics and Immunohistochemistry | Associated conditions |
|---|---|---|---|---|---|
| Ovarian Fibroma [3][4][5][6][7][8][9][10] |
|
|
|
| |
| Oral Fibroma [11][12][13] |
|
|
| ||
| Chondromyxoid fibroma [14][15][16][17][18][19][20][21][22] |
|
|
|
|
|
| Uterine fibroma [23][24][25][26][27][28][29][30][31][32][33] |
|
|
|
| |
| Ossifying Fibroma [34][35][36][37][38][39][40] |
|
|
|
| |
| Non-ossifying Fibroma [41][42][43] |
|
|
|
|
|
| Desmoplastic Fibroma [44][45][46][47][48][49][50] |
|
|
| ||
| Pleural Fibroma [51][52][53][54][55][56][57][58][59][60][61][62] |
|
|
| ||
| Cardiac Fibroma [63][64][65][66][67][68][69][70][71][72] |
|
|
|
|
|
| Renal Medullary Fibroma [73][74][75] |
|
|
|
| |
| Cemento-ossifying Fibroma [76][77][78][79][80][81][82][83][84][85] |
|
|
|
|
|
| Desmoplastic Fibroblastoma [86][87][88][89][90][91] |
|
|
|
| |
| Elastofibroma [92][93][94][95][96][97][98] |
|
|
|
|
|
| Sclerotic Fibroma [99][100][101][102][103][104][105][106][107] |
|
|
|||
| Giant cell fibroma [108][109][110][111][112][113][114][115] |
|
|
|
| |
| Peripheral Odontogenic Fibroma [116][117][118][119][120] | Firm, slowly growing, sessile, and nodular growth of the gingiva are characteristic findings of peripheral odontogenic fibroma. |
|
|
|
Gross Pathology and Microscopic Pathology
| Type of fibroma | Gross image | Microscopic image |
|---|---|---|
| Ovarian fibroma |  |
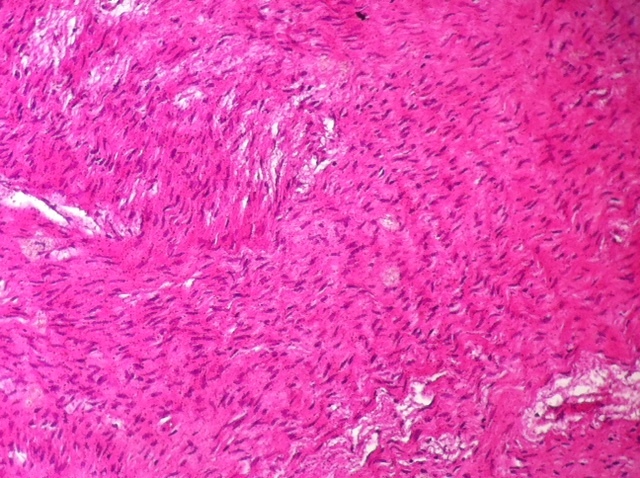 |
| Oral fibroma |  |
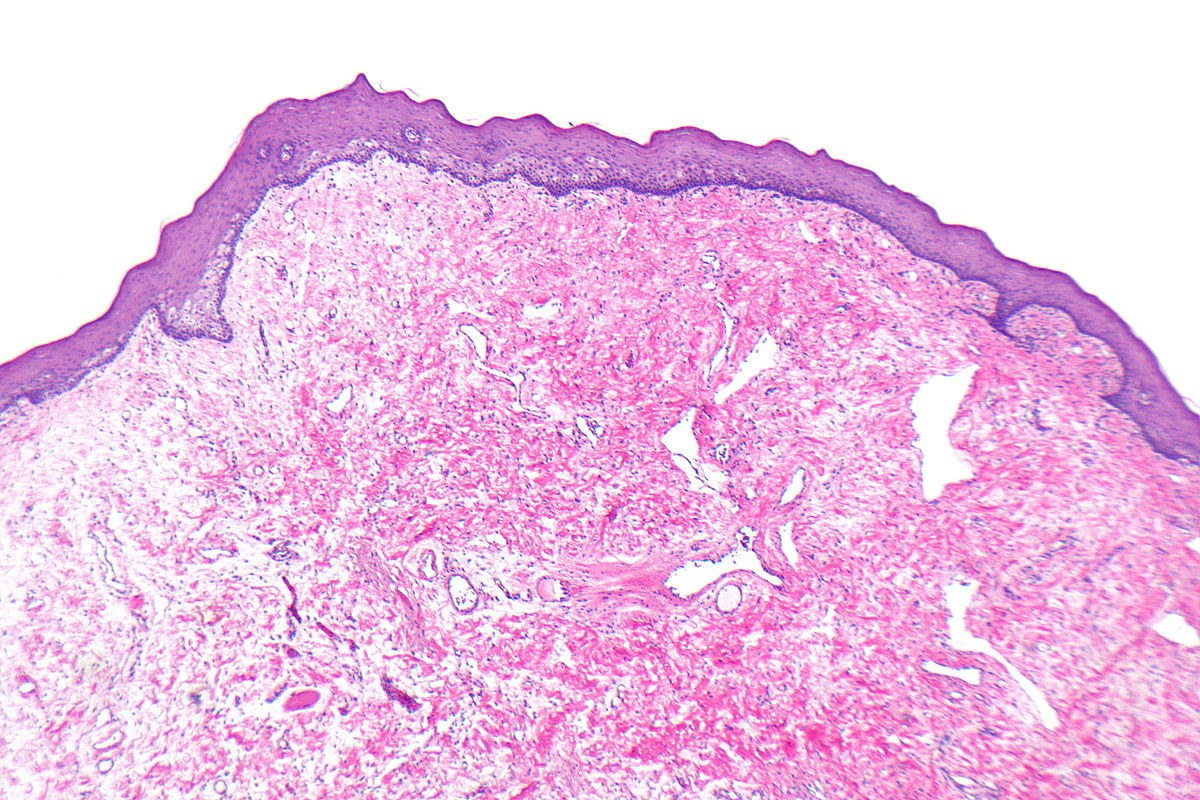 |
| Chondromyxoid fibroma | 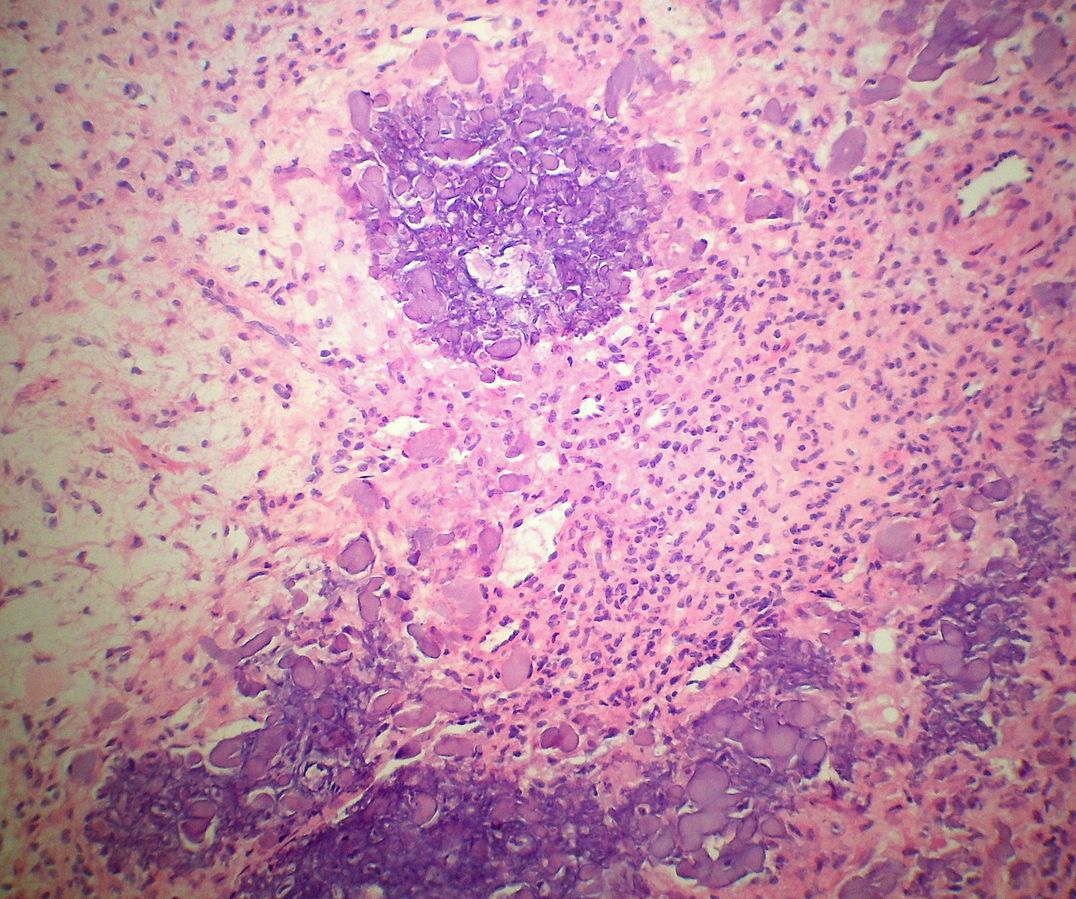 | |
| Uterine fibroma | 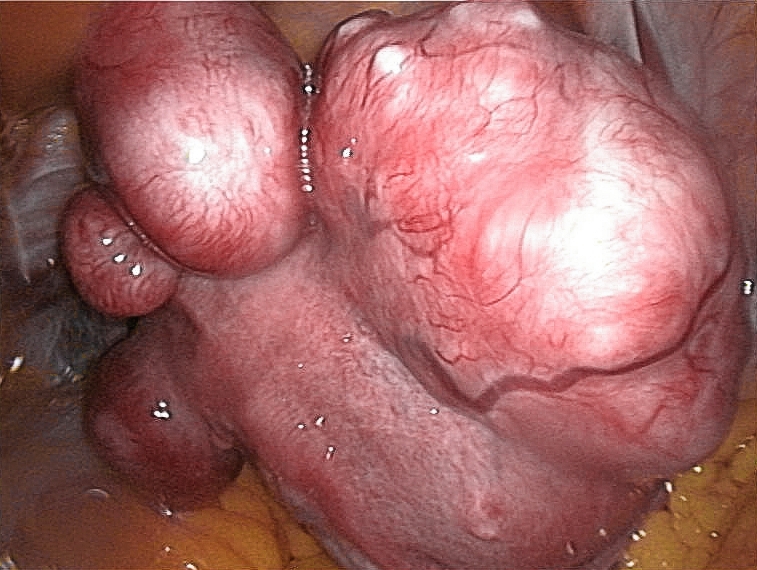 |
 |
| Ossifying Fibroma | 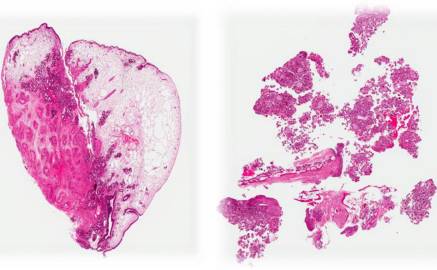 | |
| Cardiac fibroma |  |
 |
| Giant cell fibroma |  |
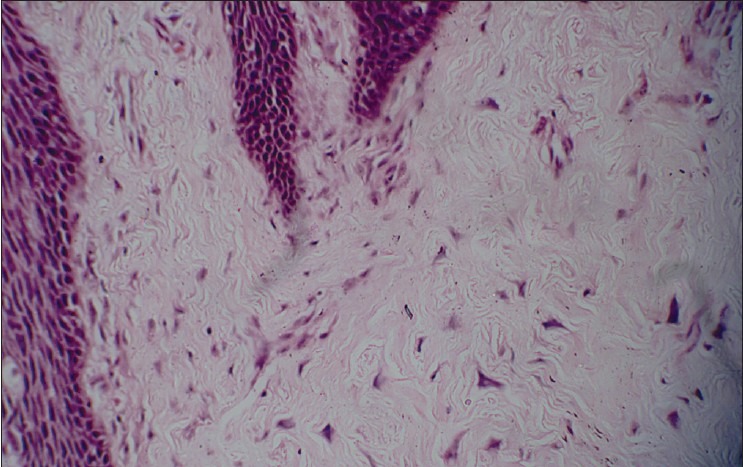 |
| Peripheral odontogenic fibroma |  |
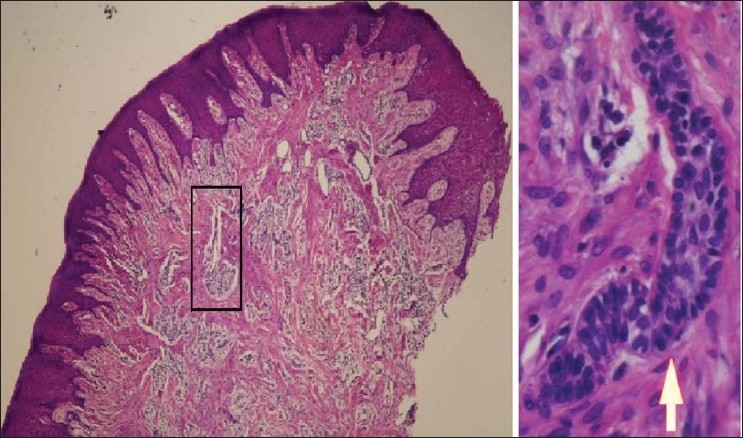 |
| Elastofibroma |  |
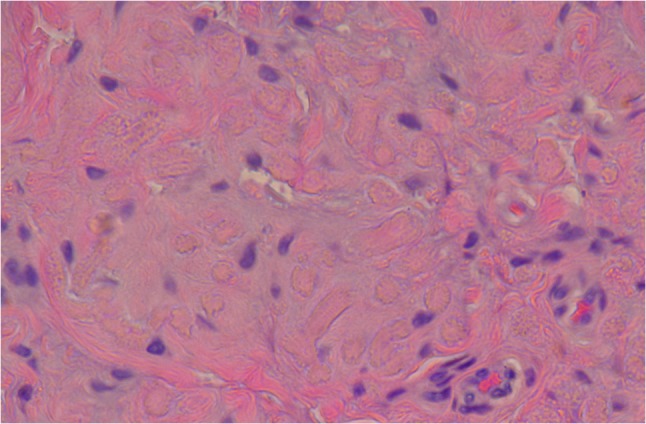 |
| Desmoplastic fibroblastoma | 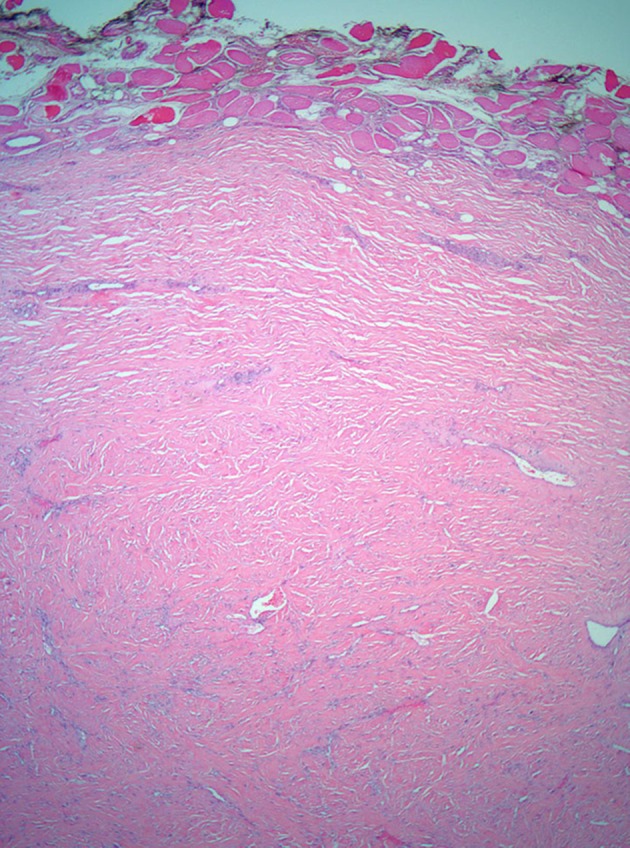 | |
| Renal medullary fibroma | 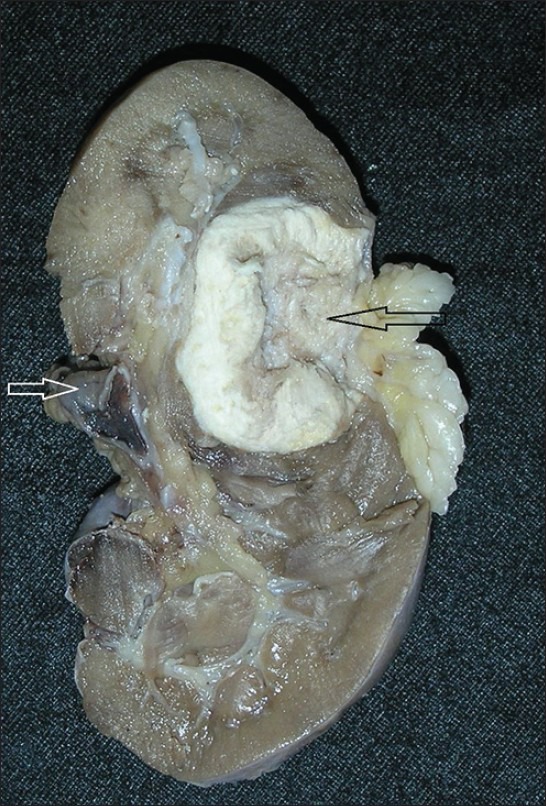 |
 |
| Pleural fibroma |  |
|
Pathophysiology
Physiology
The normal physiology of [name of process] can be understood as follows:
Pathogenesis
- The exact pathogenesis of [disease name] is not completely understood.
OR
- It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics
[Disease name] is transmitted in [mode of genetic transmission] pattern.
OR
Genes involved in the pathogenesis of [disease name] include:
- [Gene1]
- [Gene2]
- [Gene3]
OR
The development of [disease name] is the result of multiple genetic mutations such as:
- [Mutation 1]
- [Mutation 2]
- [Mutation 3]
Associated Conditions
Conditions associated with [disease name] include:
- [Condition 1]
- [Condition 2]
- [Condition 3]
| Type of fibroma | Location | Gross pathology | Microscpoic pathology | Genetics and Immunohistochemistry | Associated conditions |
|---|---|---|---|---|---|
| Ovarian Fibroma [3][4][5][6][7][8][9][10] |
|
|
|
| |
| Oral Fibroma [11][12][13] |
|
|
| ||
| Chondromyxoid fibroma [14][15][16][17][18][19][20][21][22] |
|
|
|
|
|
| Uterine fibroma [23][24][25][26][27][28][29][30][31][32][33] |
|
|
|
| |
| Ossifying Fibroma [34][35][36][37][38][39][40] |
|
|
|
| |
| Non-ossifying Fibroma [41][42][43] |
|
|
|
|
|
| Desmoplastic Fibroma [44][45][46][47][48][49][50] |
|
|
| ||
| Pleural Fibroma [51][52][53][54][55][56][57][58][59][60][61][62] |
|
|
| ||
| Cardiac Fibroma [63][64][65][66][67][68][69][70][71][72] |
|
|
|
|
|
| Renal Medullary Fibroma [73][74][75] |
|
|
|
| |
| Cemento-ossifying Fibroma [76][77][78][79][80][81][82][83][84][85] |
|
|
|
|
|
| Desmoplastic Fibroblastoma [86][87][88][89][90][91] |
|
|
|
| |
| Elastofibroma [92][93][94][95][96][97][98] |
|
|
|
|
|
| Sclerotic Fibroma [99][100][101][102][103][104][105][106][107] |
|
|
|||
| Giant cell fibroma [108][109][110][111][112][113][114][115] |
|
|
|
| |
| Peripheral Odontogenic Fibroma [116][117][118][119][120] | Firm, slowly growing, sessile, and nodular growth of the gingiva are characteristic findings of peripheral odontogenic fibroma. |
|
|
|
| Type of fibroma | Gross image | Microscopic image |
|---|---|---|
| Ovarian fibroma |  |
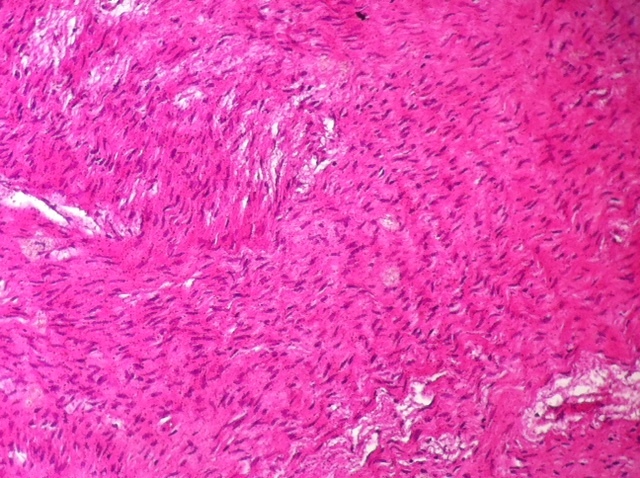 |
| Oral fibroma |  |
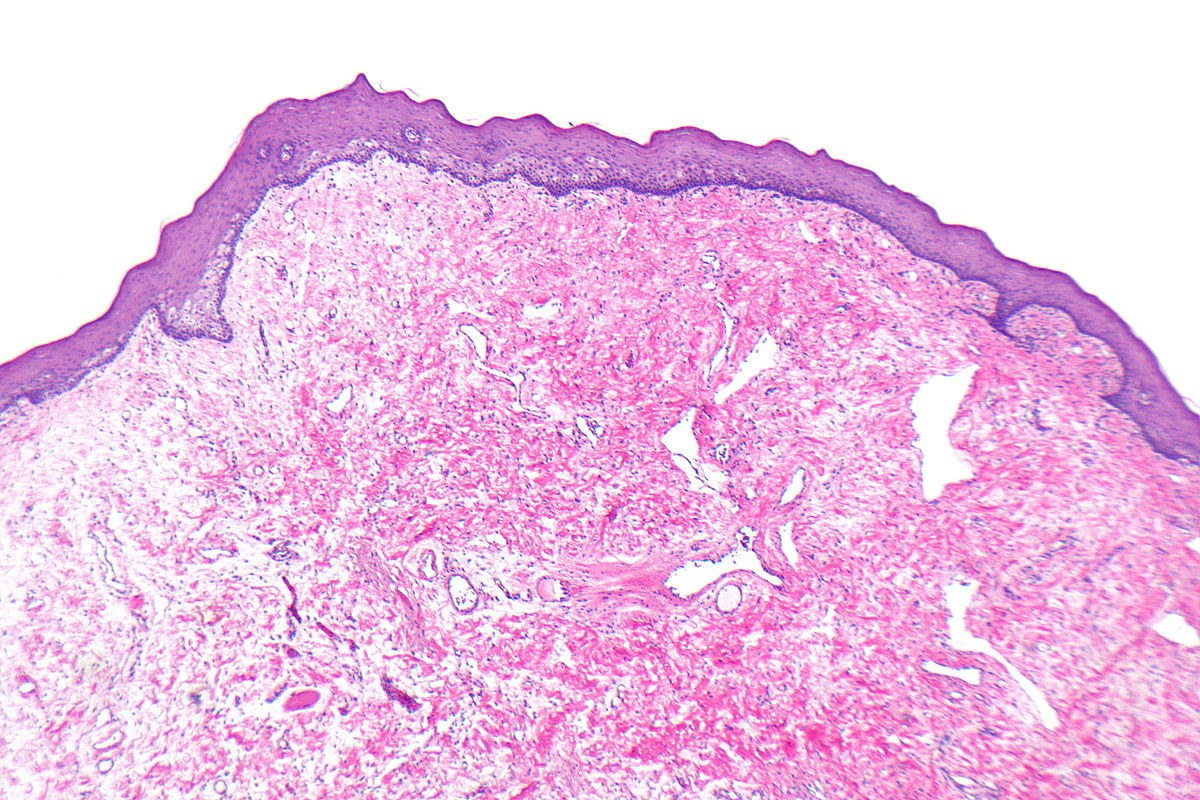 |
| Chondromyxoid fibroma | 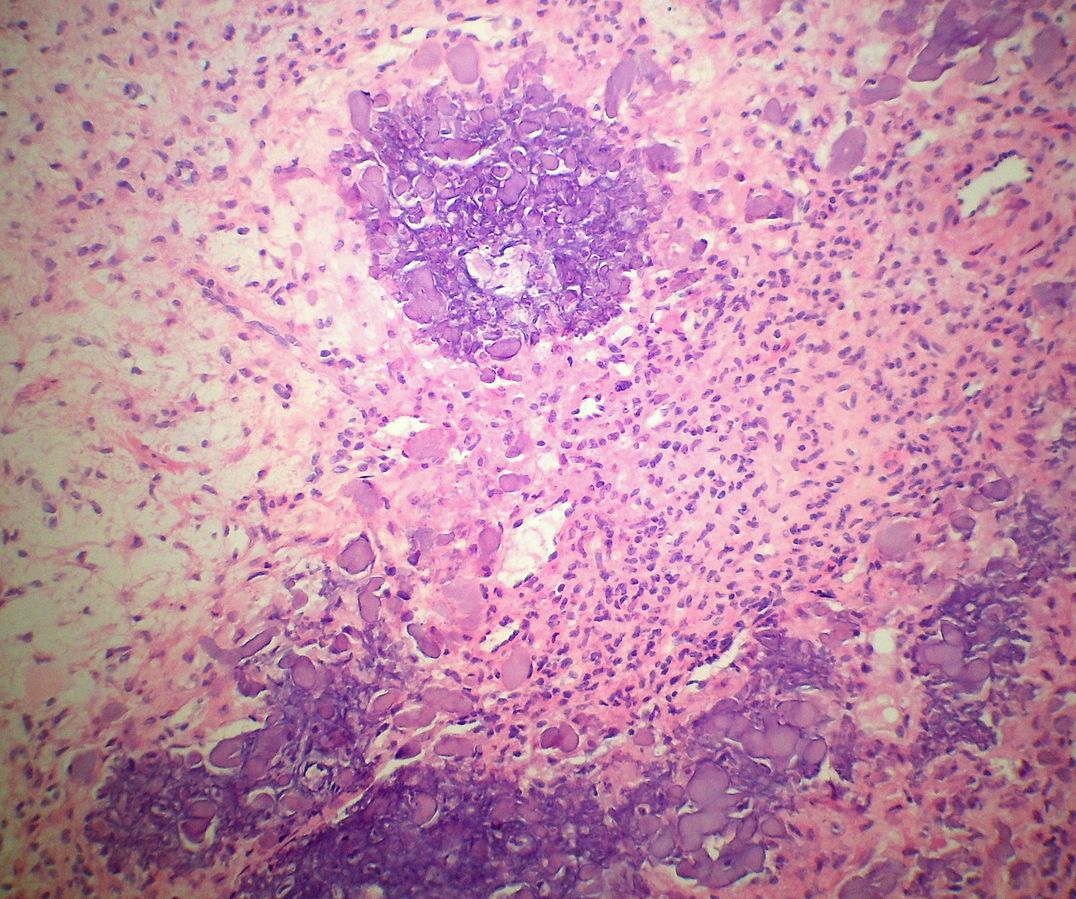 | |
| Uterine fibroma | 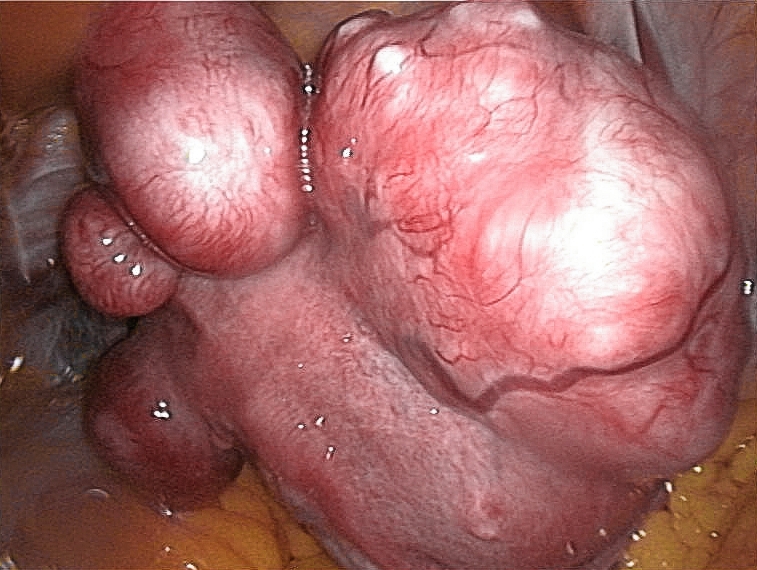 |
 |
| Ossifying Fibroma | 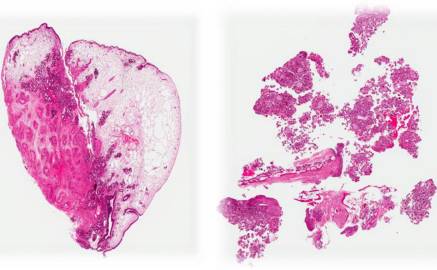 | |
| Cardiac fibroma |  |
 |
| Giant cell fibroma |  |
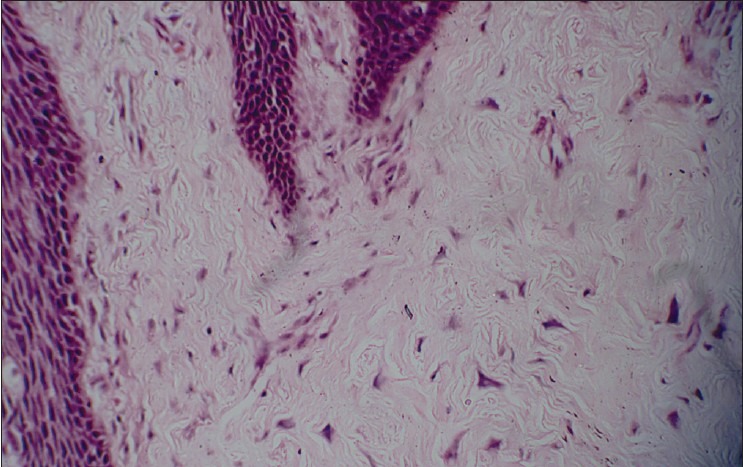 |
| Peripheral odontogenic fibroma |  |
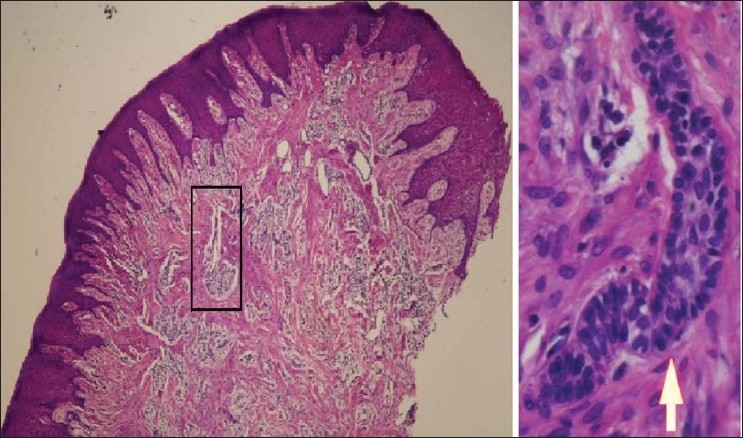 |
| Elastofibroma |  |
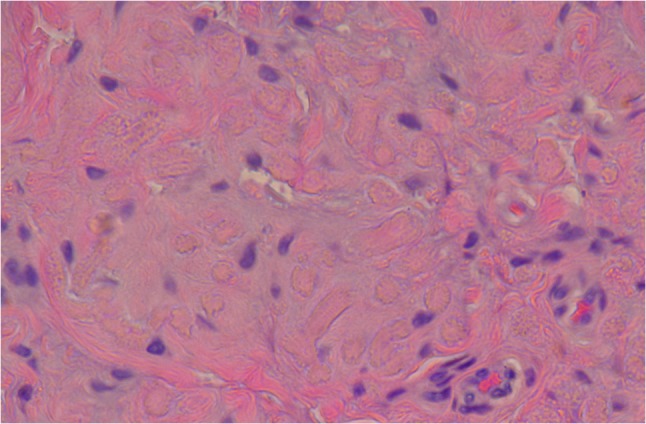 |
| Desmoplastic fibroblastoma | 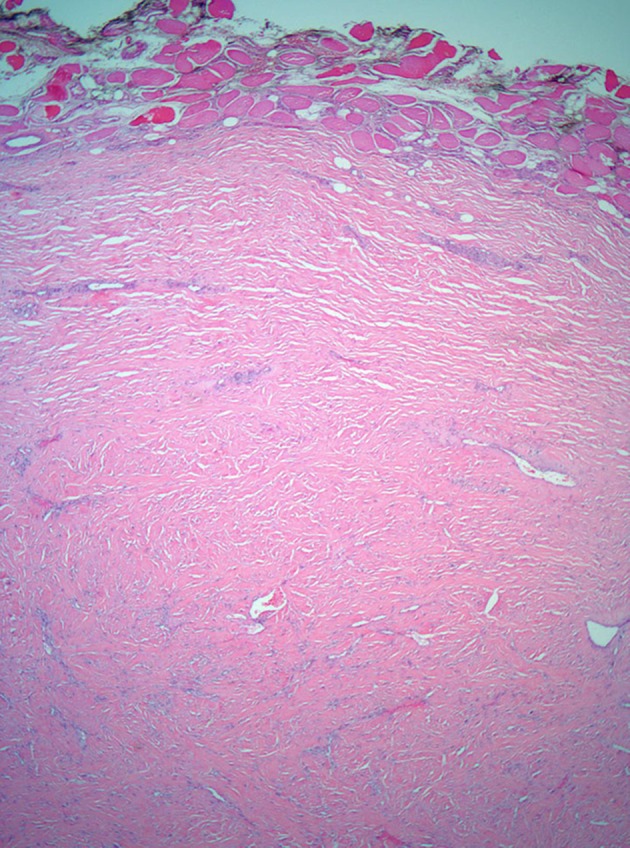 | |
| Renal medullary fibroma | 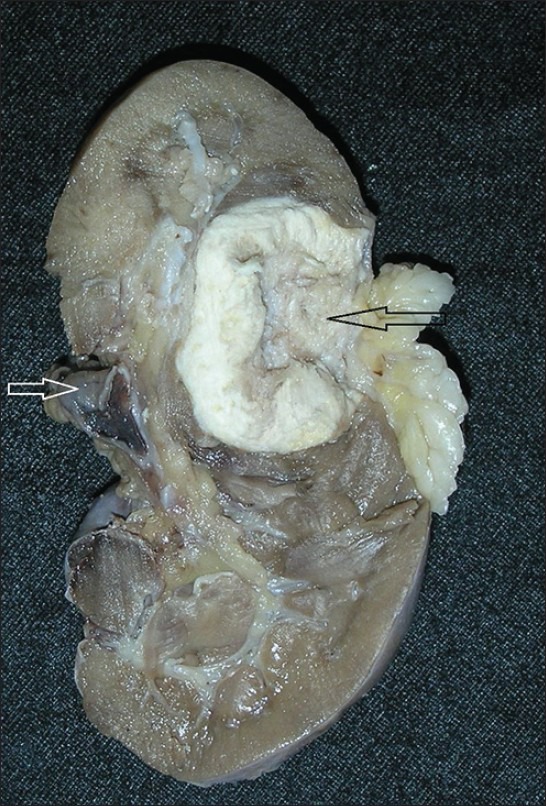 |
 |
| Pleural fibroma |  |
|
References
- ↑ Fibroma. Libre pathology(2015) http://librepathology.org/wiki/Fibroma Accessed on March 12, 2016
- ↑ Fibroma. Radiopedia(2015) http://radiopaedia.org/search?utf8=%E2%9C%93&q=fibroma&scope=all Accessed on March 12, 2016
- ↑ 3.0 3.1 Boujoual M, Hakimi I, Kouach J, Oukabli M, Moussaoui DR, Dehayni M (2015). "Large twisted ovarian fibroma in menopausal women: a case report". Pan Afr Med J. 20: 322. doi:10.11604/pamj.2015.20.322.5998. PMC 4491469. PMID 26175813.
- ↑ 4.0 4.1 Chen H, Liu Y, Shen LF, Jiang MJ, Yang ZF, Fang GP (November 2016). "Ovarian thecoma-fibroma groups: clinical and sonographic features with pathological comparison". J Ovarian Res. 9 (1): 81. doi:10.1186/s13048-016-0291-2. PMC 5120502. PMID 27876070.
- ↑ 5.0 5.1 Matsuda K, Tateishi S, Akazawa Y, Kinoshita A, Yoshida S, Morisaki S, Fukushima A, Matsuwaki T, Yoshiura KI, Nakashima M (October 2016). "Rapid growth of mitotically active cellular fibroma of the ovary: a case report and review of the literature". Diagn Pathol. 11 (1): 101. doi:10.1186/s13000-016-0554-7. PMID 27770806.
- ↑ 6.0 6.1 Yamada T, Hattori K, Satomi H, Hirose Y, Nakai G, Daimon A, Hayashi A, Terai Y, Ohmichi M, Fukunaga M (October 2015). "Mitotically active cellular fibroma of the ovary: a case report and literature review". J Ovarian Res. 8: 65. doi:10.1186/s13048-015-0191-x. PMC 4595272. PMID 26437718.
- ↑ 7.0 7.1 Zong L, Lin M, Fan X (2014). "Mitotically active cellular fibroma of ovary should be differentiated from fibrosarcoma: a case report and review of literature". Int J Clin Exp Pathol. 7 (11): 7578–82. PMC 4270577. PMID 25550794.
- ↑ 8.0 8.1 Parwate NS, Patel SM, Arora R, Gupta M (December 2016). "Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature". J Obstet Gynaecol India. 66 (6): 460–465. doi:10.1007/s13224-015-0717-6. PMC 5080219. PMID 27821988.
- ↑ 9.0 9.1 Finch T, Pushpanathan C, Brown K, El-Gohary Y (June 2012). "Gorlin syndrome presenting with a unilateral ovarian fibroma in a 22-year-old woman: a case report". J Med Case Rep. 6: 148. doi:10.1186/1752-1947-6-148. PMID 22691621.
- ↑ 10.0 10.1 Yazdani S, Alijanpoor A, Sharbatdaran M, Bouzari Z, Abedisamakoosh M, Lakaieandi F, Mohammadpour M (2014). "Meigs' syndrome with elevated serum CA125 in a case of ovarian fibroma /thecoma". Caspian J Intern Med. 5 (1): 43–5. PMC 3894471. PMID 24490014.
- ↑ 11.0 11.1 Panta P (2015). "Traumatic fibroma". Pan Afr Med J. 21: 220. doi:10.11604/pamj.2015.21.220.7498. PMC 4587079. PMID 26448815.
- ↑ 12.0 12.1 Christopoulos P, Sklavounou A, Patrikiou A (April 1994). "True fibroma of the oral mucosa: a case report". Int J Oral Maxillofac Surg. 23 (2): 98–9. PMID 8035060.
- ↑ 13.0 13.1 Krishnan V, Shunmugavelu K (2015). "A clinical challenging situation of intra oral fibroma mimicking pyogenic granuloma". Pan Afr Med J. 22: 263. doi:10.11604/pamj.2015.22.263.8080. PMC 4765330. PMID 26958126.
- ↑ 14.0 14.1 Takenaga RK, Frassica FJ, McCarthy EF (2007). "Subperiosteal chondromyxoid fibroma: a report of two cases". Iowa Orthop J. 27: 104–7. PMC 2150655. PMID 17907440.
- ↑ 15.0 15.1 Sharma H, Jane MJ, Reid R (June 2006). "Chondromyxoid fibroma of the foot and ankle: 40 years' Scottish bone tumour registry experience". Int Orthop. 30 (3): 205–9. doi:10.1007/s00264-005-0046-y. PMC 2532097. PMID 16547720.
- ↑ 16.0 16.1 Yasuda T, Nishio J, Sumegi J, Kapels KM, Althof PA, Sawyer JR, Reith JD, Bridge JA (November 2009). "Aberrations of 6q13 mapped to the COL12A1 locus in chondromyxoid fibroma". Mod. Pathol. 22 (11): 1499–506. doi:10.1038/modpathol.2009.101. PMID 19648885.
- ↑ 17.0 17.1 Choi YS, Kim BS, Joo JE, Park YK, Lee SH, Song BY (2011). "A rare case of epiphyseal chondromyxoid fibroma of the proximal tibia". Korean J Radiol. 12 (6): 761–4. doi:10.3348/kjr.2011.12.6.761. PMC 3194784. PMID 22043162.
- ↑ 18.0 18.1 Gutiérrez-González R, De Reina L, Saab A, Jiménez-Heffernan J, García-Uría J (June 2012). "Chondromyxoid fibroma of the lumbar spine: case report and literature review". Eur Spine J. 21 Suppl 4: S458–62. doi:10.1007/s00586-011-2078-x. PMID 22094389.
- ↑ 19.0 19.1 Morris LG, Rihani J, Lebowitz RA, Wang BY (June 2009). "Chondromyxoid fibroma of sphenoid sinus with unusual calcifications: case report with literature review". Head Neck Pathol. 3 (2): 169–73. doi:10.1007/s12105-009-0121-6. PMID 19644549.
- ↑ 20.0 20.1 Minasian T, Claus C, Hariri OR, Piao Z, Quadri SA, Yuhan R, Leong D, Tashjian V (2016). "Chondromyxoid fibroma of the sacrum: A case report and literature review". Surg Neurol Int. 7 (Suppl 13): S370–4. doi:10.4103/2152-7806.182547. PMC 4879845. PMID 27274412.
- ↑ 21.0 21.1 Kilic D, Findikcioglu A, Tepeoglu M, Vural C (August 2015). "Chondromyxoid Fibroma of the Sternum in a 63-Year-Old Woman". Tex Heart Inst J. 42 (4): 400–2. doi:10.14503/THIJ-14-4381. PMC 4567104. PMID 26413029.
- ↑ 22.0 22.1 Fomete B, Adeosun OO, Awelimobor DI, Olayemi L (January 2014). "Chondromyxoid fibroma of the mandible: Case report and review of the literature". Ann Maxillofac Surg. 4 (1): 78–80. doi:10.4103/2231-0746.133072. PMC 4073468. PMID 24987604.
- ↑ 23.0 23.1 Manta L, Suciu N, Toader O, Purcărea RM, Constantin A, Popa F (2016). "The etiopathogenesis of uterine fibromatosis". J Med Life. 9 (1): 39–45. PMC 5152611. PMID 27974911.
- ↑ 24.0 24.1 Borahay MA, Al-Hendy A, Kilic GS, Boehning D (April 2015). "Signaling Pathways in Leiomyoma: Understanding Pathobiology and Implications for Therapy". Mol. Med. 21: 242–56. doi:10.2119/molmed.2014.00053. PMC 4503645. PMID 25879625.
- ↑ 25.0 25.1 Miettinen M, Felisiak-Golabek A, Wasag B, Chmara M, Wang Z, Butzow R, Lasota J (December 2016). "Fumarase-deficient Uterine Leiomyomas: An Immunohistochemical, Molecular Genetic, and Clinicopathologic Study of 86 Cases". Am. J. Surg. Pathol. 40 (12): 1661–1669. doi:10.1097/PAS.0000000000000703. PMC 5106328. PMID 27454940.
- ↑ 26.0 26.1 Commandeur AE, Styer AK, Teixeira JM (2015). "Epidemiological and genetic clues for molecular mechanisms involved in uterine leiomyoma development and growth". Hum. Reprod. Update. 21 (5): 593–615. doi:10.1093/humupd/dmv030. PMC 4533663. PMID 26141720.
- ↑ 27.0 27.1 Flake GP, Andersen J, Dixon D (June 2003). "Etiology and pathogenesis of uterine leiomyomas: a review". Environ. Health Perspect. 111 (8): 1037–54. doi:10.1289/ehp.5787. PMC 1241553. PMID 12826476.
- ↑ 28.0 28.1 Lobel MK, Somasundaram P, Morton CC (March 2006). "The genetic heterogeneity of uterine leiomyomata". Obstet. Gynecol. Clin. North Am. 33 (1): 13–39. doi:10.1016/j.ogc.2005.12.006. PMID 16504804.
- ↑ 29.0 29.1 Wolańska M, Bańkowski E (February 2007). "Transforming growth factor beta and platelet-derived growth factor in human myometrium and in uterine leiomyomas at various stages of tumour growth". Eur. J. Obstet. Gynecol. Reprod. Biol. 130 (2): 238–44. doi:10.1016/j.ejogrb.2006.01.034. PMID 16564125.
- ↑ 30.0 30.1 Baird DD, Kesner JS, Dunson DB (February 2006). "Luteinizing hormone in premenopausal women may stimulate uterine leiomyomata development". J. Soc. Gynecol. Investig. 13 (2): 130–5. doi:10.1016/j.jsgi.2005.12.001. PMID 16443507.
- ↑ 31.0 31.1 Andersen J (August 1996). "Growth factors and cytokines in uterine leiomyomas". Semin. Reprod. Endocrinol. 14 (3): 269–82. doi:10.1055/s-2007-1016336. PMID 8885057.
- ↑ 32.0 32.1 Laganà AS, Vergara D, Favilli A, La Rosa VL, Tinelli A, Gerli S, Noventa M, Vitagliano A, Triolo O, Rapisarda A, Vitale SG (November 2017). "Epigenetic and genetic landscape of uterine leiomyomas: a current view over a common gynecological disease". Arch. Gynecol. Obstet. 296 (5): 855–867. doi:10.1007/s00404-017-4515-5. PMID 28875276. Vancouver style error: initials (help)
- ↑ 33.0 33.1 Koutsilieris M (May 1992). "Pathophysiology of uterine leiomyomas". Biochem. Cell Biol. 70 (5): 273–8. PMID 1323302.
- ↑ 34.0 34.1 Wang TT, Zhang R, Wang L, Chen Y, Dong Q, Li TJ (March 2014). "Two cases of multiple ossifying fibromas in the jaws". Diagn Pathol. 9: 75. doi:10.1186/1746-1596-9-75. PMC 3974450. PMID 24678936.
- ↑ 35.0 35.1 Chen Y, Hu DY, Wang TT, Zhang R, Dong Q, Xu ZX, Wang L, Li TJ (September 2016). "CDC73 gene mutations in sporadic ossifying fibroma of the jaws". Diagn Pathol. 11 (1): 91. doi:10.1186/s13000-016-0532-0. PMC 5034632. PMID 27658992.
- ↑ 36.0 36.1 Maria A, Sharma Y, Malik M (December 2013). "Juvenile ossifying fibroma of mandible: a case report". J Maxillofac Oral Surg. 12 (4): 447–50. doi:10.1007/s12663-010-0122-8. PMID 24431886.
- ↑ 37.0 37.1 Alghonaim Y, ALRashed ALHumaid S, Arafat A (2018). "Aggressive ossifying fibroma of right ethmoidal sinus: A case report". Int J Surg Case Rep. 53: 513–516. doi:10.1016/j.ijscr.2017.12.026. PMC 6290393. PMID 29373206.
- ↑ 38.0 38.1 Liu Y, Shan XF, Guo XS, Xie S, Cai ZG (2017). "Clinicopathological Characteristics and Prognosis of Ossifying Fibroma in the Jaws of Children: A Retrospective Study". J Cancer. 8 (17): 3592–3597. doi:10.7150/jca.21556. PMC 5687175. PMID 29151945.
- ↑ 39.0 39.1 Liu JJ, Thompson LD, Janisiewicz AM, Shibuya TY, Keschner DB, Garg R, Lee JT (March 2017). "Ossifying fibroma of the maxilla and sinonasal tract: Case series". Allergy Rhinol (Providence). 8 (1): 32–36. doi:10.2500/ar.2017.8.0190. PMC 5380450. PMID 28381325.
- ↑ 40.0 40.1 Misra SR, Saigal A, Rastogi V, Priyadarshini SR, Pati AR (January 2015). "Giant central ossifying fibroma of the maxilla presenting with a pus discharging intra-oral sinus". J Clin Diagn Res. 9 (1): ZD08–11. doi:10.7860/JCDR/2015/11192.5417. PMC 4347180. PMID 25738089.
- ↑ 41.0 41.1 Bowers LM, Cohen DM, Bhattacharyya I, Pettigrew JC, Stavropoulos MF (June 2013). "The non-ossifying fibroma: a case report and review of the literature". Head Neck Pathol. 7 (2): 203–10. doi:10.1007/s12105-012-0399-7. PMID 23008139.
- ↑ 42.0 42.1 Herget GW, Mauer D, Krauß T, El Tayeh A, Uhl M, Südkamp NP, Hauschild O (April 2016). "Non-ossifying fibroma: natural history with an emphasis on a stage-related growth, fracture risk and the need for follow-up". BMC Musculoskelet Disord. 17: 147. doi:10.1186/s12891-016-1004-0. PMC 4820930. PMID 27044378.
- ↑ 43.0 43.1 Goldin A, Muzykewicz DA, Dwek J, Mubarak SJ (October 2017). "The aetiology of the non-ossifying fibroma of the distal femur and its relationship to the surrounding soft tissues". J Child Orthop. 11 (5): 373–379. doi:10.1302/1863-2548.11.170068. PMC 5643931. PMID 29081852.
- ↑ 44.0 44.1 Schneider M, Zimmermann AC, Depprich RA, Kübler NR, Engers R, Naujoks CD, Handschel J (November 2009). "Desmoplastic fibroma of the mandible--review of the literature and presentation of a rare case". Head Face Med. 5: 25. doi:10.1186/1746-160X-5-25. PMID 19930688.
- ↑ 45.0 45.1 Nedopil A, Raab P, Rudert M (2013). "Desmoplastic fibroma: a case report with three years of clinical and radiographic observation and review of the literature". Open Orthop J. 8: 40–6. doi:10.2174/1874325001307010040. PMID 23459513.
- ↑ 46.0 46.1 Gong YB, Qu LM, Qi X, Liu JG (October 2015). "Desmoplastic fibroma in the proximal femur: A case report with long-term follow-up". Oncol Lett. 10 (4): 2465–2467. doi:10.3892/ol.2015.3603. PMID 26622872.
- ↑ 47.0 47.1 Daneyemez M, Akay KM, Izci Y (October 2005). "Desmoplastic fibroma of the cervical spine". Eur Spine J. 14 (8): 799–802. doi:10.1007/s00586-005-0904-8. PMID 15937674.
- ↑ 48.0 48.1 Woods TR, Cohen DM, Islam MN, Rawal Y, Bhattacharyya I (June 2015). "Desmoplastic fibroma of the mandible: a series of three cases and review of literature". Head Neck Pathol. 9 (2): 196–204. doi:10.1007/s12105-014-0561-5. PMID 25113037.
- ↑ 49.0 49.1 Goyal T, Rastogi S, Tripathy SK (March 2013). "Desmoplastic fibroma of ulna: Excision and reconstruction of olecranon with a fibular graft". Indian J Orthop. 47 (2): 207–10. doi:10.4103/0019-5413.108928. PMC 3654474. PMID 23682186.
- ↑ 50.0 50.1 Evans S, Ramasamy A, Jeys L, Grimer R (November 2014). "Desmoplastic fibroma of bone: A rare bone tumour". J Bone Oncol. 3 (3–4): 77–9. doi:10.1016/j.jbo.2014.08.001. PMC 4723648. PMID 26909301.
- ↑ 51.0 51.1 Aremu AA, Oyedeji OA, Asaleye CM, Adetiloye VA (2013). "An elusive chest coin in an African child: a pleural fibroma's long, tortuous path to freedom". Pan Afr Med J. 14: 16. doi:10.11604/pamj.2013.14.16.1874. PMC 3597858. PMID 23503999.
- ↑ 52.0 52.1 Hassan S, Husain SS, Anwar MA, Saeed S (2015). "Pleural Fibroma; A meandering path to surgical removal". Pak J Med Sci. 31 (1): 236–8. doi:10.12669/pjms.311.5517. PMC 4386196. PMID 25878653.
- ↑ 53.0 53.1 Ali JM, Ali A, Van Leuven M, Bartosik WR (July 2017). "Giant solitary fibrous tumour of the pleura an unpredictable entity: case series and literature review". Ann R Coll Surg Engl. 99 (6): e165–e171. doi:10.1308/rcsann.2017.0067. PMC 5696978. PMID 28660826.
- ↑ 54.0 54.1 Supakul R, Sodhi A, Tamashiro CY, Azmi SS, Kadaria D (December 2015). "Solitary Fibrous Tumor of the Pleura: A Rare Cause of Pleural Mass". Am J Case Rep. 16: 854–7. PMC 4671454. PMID 26632548.
- ↑ 55.0 55.1 Guo W, Xiao HL, Jiang YG, Wang RW, Zhao YP, Ma Z, Niu HJ (October 2011). "Retrospective analysis for thirty-nine patients with solitary fibrous tumor of pleura and review of the literature". World J Surg Oncol. 9: 134. doi:10.1186/1477-7819-9-134. PMC 3214850. PMID 22014289.
- ↑ 56.0 56.1 Chu X, Zhang L, Xue Z, Ren Z, Sun YE, Wang M, Liu M (April 2012). "Solitary fibrous tumor of the pleura: An analysis of forty patients". J Thorac Dis. 4 (2): 146–54. doi:10.3978/j.issn.2072-1439.2012.01.05. PMID 22833820.
- ↑ 57.0 57.1 Guo J, Chu X, Sun YE, Zhang L, Zhou N (November 2010). "Giant solitary fibrous tumor of the pleura: an analysis of five patients". World J Surg. 34 (11): 2553–7. doi:10.1007/s00268-010-0715-x. PMC 2949573. PMID 20628740.
- ↑ 58.0 58.1 Moat NE, Teale JD, Lea RE, Matthews AW (December 1991). "Spontaneous hypoglycaemia and pleural fibroma: role of insulin like growth factors". Thorax. 46 (12): 932–3. doi:10.1136/thx.46.12.932. PMC 463503. PMID 1792644.
- ↑ 59.0 59.1 Masson EA, MacFarlane IA, Graham D, Foy P (December 1991). "Spontaneous hypoglycaemia due to a pleural fibroma: role of insulin like growth factors". Thorax. 46 (12): 930–1. doi:10.1136/thx.46.12.930. PMID 1792643.
- ↑ 60.0 60.1 Vejvodova S, Spidlen V, Mukensnabl P, Krakorova G, Molacek J, Vodicka J (February 2017). "Solitary Fibrous Tumor - Less Common Neoplasms of the Pleural Cavity". Ann Thorac Cardiovasc Surg. 23 (1): 12–18. doi:10.5761/atcs.oa.16-00108. PMC 5347482. PMID 28049955.
- ↑ 61.0 61.1 Rahnemai-Azar AA, Rahnemai-Aazr AA, Robinson P, Pham S (July 2013). "Solitary fibrous tumour of the pleura masquerading as catecholamine-secreting paraganglioma". BMJ Case Rep. 2013. doi:10.1136/bcr-2013-009939. PMC 3736364. PMID 23832995.
- ↑ 62.0 62.1 Ichiki Y, Kakizoe K, Hamatsu T, Matsuyama A, Suehiro T, Tanaka F, Hisaoka M, Sugimachi K (December 2017). "Solitary fibrous tumor of the lung: a case report". Surg Case Rep. 3 (1): 10. doi:10.1186/s40792-016-0286-7. PMC 5218951. PMID 28063145.
- ↑ 63.0 63.1 Torimitsu S, Nemoto T, Wakayama M, Okubo Y, Yokose T, Kitahara K, Ozawa T, Nakayama H, Shinozaki M, Sasai D, Ishiwatari T, Takuma K, Shibuya K (March 2012). "Literature survey on epidemiology and pathology of cardiac fibroma". Eur. J. Med. Res. 17: 5. doi:10.1186/2047-783X-17-5. PMC 3351722. PMID 22472419.
- ↑ 64.0 64.1 Jha NK, Kiraly L, Tamas C, Talo H, Khan MD, El Badaoui H, Jain A, Hammad A (March 2015). "Large cardiac fibroma and teratoma in children- case reports". J Cardiothorac Surg. 10: 38. doi:10.1186/s13019-015-0242-9. PMC 4373309. PMID 25887953.
- ↑ 65.0 65.1 Busch U, Kampmann C, Meyer R, Sandring KH, Hausdorf G, Konertz W (1995). "Removal of a giant cardiac fibroma from a 4-year-old child". Tex Heart Inst J. 22 (3): 261–4. PMC 325263. PMID 7580366.
- ↑ 66.0 66.1 Bossert T, Walther T, Vondrys D, Gummert JF, Kostelka M, Mohr FW (2006). "Cardiac fibroma as an inherited manifestation of nevoid basal-cell carcinoma syndrome". Tex Heart Inst J. 33 (1): 88–90. PMC 1413607. PMID 16572881.
- ↑ 67.0 67.1 Heidari A, Sabzi F, Faraji R (2018). "Right atrial fibroma in an adult patient". Ann Card Anaesth. 21 (1): 65–67. doi:10.4103/aca.ACA_121_17. PMC 5791493. PMID 29336396.
- ↑ 68.0 68.1 Scanlan D, Radio SJ, Nelson M, Zhou M, Streblow R, Prasad V, Reyes C, Perry D, Fletcher S, Bridge JA (2008). "Loss of the PTCH1 gene locus in cardiac fibroma". Cardiovasc. Pathol. 17 (2): 93–7. doi:10.1016/j.carpath.2007.08.001. PMC 2342874. PMID 18329553.
- ↑ 69.0 69.1 Ying L, Lin R, Gao Z, Qi J, Zhang Z, Gu W (April 2016). "Primary cardiac tumors in children: a center's experience". J Cardiothorac Surg. 11 (1): 52. doi:10.1186/s13019-016-0448-5. PMID 27067427.
- ↑ 70.0 70.1 Yadava OP (2012). "Cardiac tumours in infancy". Indian Heart J. 64 (5): 492–6. doi:10.1016/j.ihj.2012.05.004. PMC 3861228. PMID 23102388.
- ↑ 71.0 71.1 Cho SH, Fritz T, Cronin LJ, Cohle SD (2015). "Primary Cardiac Fibroma in an Adult". Case Rep Cardiol. 2015: 713702. doi:10.1155/2015/713702. PMID 26457206.
- ↑ 72.0 72.1 Mecchia D, Lavezzi AM, Matturri L (2013). "Primary Cardiac Fibroma and Cardiac Conduction System Alterations in a Case of Sudden Death of a 4-month-old Infant". Open Cardiovasc Med J. 7: 47–9. doi:10.2174/1874192401307010047. PMC 3706798. PMID 23847693.
- ↑ 73.0 73.1 Kumar S, Choudhary GR, Nanjappa B, Bal A (2013). "Benign medullary fibroma of the kidney: a rare diagnostic dilemma". J Clin Imaging Sci. 3: 43. doi:10.4103/2156-7514.120776. PMC 3823390. PMID 24228211.
- ↑ 74.0 74.1 Bircan S, Orhan D, Tulunay O, Safak M (2000). "Renomedullary interstitial cell tumor". Urol. Int. 65 (3): 163–6. doi:10.1159/000064864. PMID 11054036.
- ↑ 75.0 75.1 Bazzi WM, Huang H, Al-Ahmadie H, Russo P (May 2014). "Clinicopathologic features of renomedullary interstitial cell tumor presenting as the main solid renal mass". Urology. 83 (5): 1104–6. doi:10.1016/j.urology.2014.01.008. PMID 24642074.
- ↑ 76.0 76.1 Bala TK, Soni S, Dayal P, Ghosh I (May 2017). "Cemento-ossifying fibroma of the mandible. A clinicopathological report". Saudi Med J. 38 (5): 541–545. doi:10.15537/smj.2017.5.15643. PMC 5447217. PMID 28439606.
- ↑ 77.0 77.1 Chatterjee A, Ajmera N, Singh A (July 2010). "Peripheral cemento-ossifying fibroma of maxilla". J Indian Soc Periodontol. 14 (3): 186–9. doi:10.4103/0972-124X.75915. PMC 3100863. PMID 21760674.
- ↑ 78.0 78.1 Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H (June 2013). "Peripheral cemento-ossifying fibroma: A case report with review of literature". World J Clin Cases. 1 (3): 128–33. doi:10.12998/wjcc.v1.i3.128. PMC 3845913. PMID 24303483.
- ↑ 79.0 79.1 Dalghous A, Alkhabuli JO (June 2007). "Cemento-ossifying fibroma occurring in an elderly patient. A case report and a review of literature". Libyan J Med. 2 (2): 95–8. doi:10.4176/061220. PMC 3078280. PMID 21503260.
- ↑ 80.0 80.1 Hekmatnia A, Ghazavi A, Saboori M, Mahzouni P, Tayari N, Hekmatnia F (February 2011). "A case report of cemento-ossifying fibroma presenting as a mass of the ethmoid sinus". J Res Med Sci. 16 (2): 224–8. PMC 3214308. PMID 22091236.
- ↑ 81.0 81.1 Katti G, Khan MM, Chaubey SS, Amena M (May 2016). "Cemento-ossifying fibroma of the jaw". BMJ Case Rep. 2016. doi:10.1136/bcr-2015-214327. PMC 4885328. PMID 27174452.
- ↑ 82.0 82.1 Ram R, Singhal A, Singhal P (January 2012). "Cemento-ossifying fibroma". Contemp Clin Dent. 3 (1): 83–5. doi:10.4103/0976-237X.94553. PMC 3341766. PMID 22557904.
- ↑ 83.0 83.1 Sah K, Kale AD, Hallikerimath S, Chandra S (April 2012). "Peripheral cemento-ossifying fibroma: Report of a recurrence case". Contemp Clin Dent. 3 (Suppl 1): S23–5. doi:10.4103/0976-237X.95098. PMC 3354807. PMID 22629060.
- ↑ 84.0 84.1 Naik RM, Guruprasad Y, Sujatha D, Gurudath S, Pai A, Suresh K (January 2014). "Giant cemento-ossifying fibroma of the mandible". J Nat Sci Biol Med. 5 (1): 190–4. doi:10.4103/0976-9668.127326. PMC 3961933. PMID 24678226.
- ↑ 85.0 85.1 Pereira, Thaís dos Santos Fontes; Diniz, Marina Gonçalves; França, Josiane Alves; Moreira, Rennan Garcias; Menezes, Grazielle Helena Ferreira de; Sousa, Sílvia Ferreira de; Castro, Wagner Henriques de; Gomes, Carolina Cavaliéri; Gomez, Ricardo Santiago (2018). "The Wnt/β-catenin pathway is deregulated in cemento-ossifying fibromas". Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology. 125 (2): 172–178. doi:10.1016/j.oooo.2017.10.004. ISSN 2212-4403.
- ↑ 86.0 86.1 de Sousa SF, Caldeira PC, Grossmann Sde M, de Aguiar MC, Mesquita RA (June 2011). "Desmoplastic fibroblastoma (collagenous fibroma): a case identified in the buccal mucosa". Head Neck Pathol. 5 (2): 175–9. doi:10.1007/s12105-010-0239-6. PMID 21221866.
- ↑ 87.0 87.1 Pereira TD, de Lacerda JC, Porto-Matias MD, de Jesus AO, Gomez RS, Mesquita RA (February 2016). "Desmoplastic fibroblastoma (collagenous fibroma) of the oral cavity". J Clin Exp Dent. 8 (1): e89–92. doi:10.4317/jced.52605. PMID 26855713.
- ↑ 88.0 88.1 Grewal R, Natter P, Makary R, Silliman J (January 2018). "Desmoplastic fibroblastoma of the left upper arm". BMJ Case Rep. 2018. doi:10.1136/bcr-2017-221738. PMID 29374633.
- ↑ 89.0 89.1 Osipov V, Carrera GF (2009). "Collagenous fibroma (desmoplastic fibroblastoma) with vertebral body erosion". Sarcoma. 2009: 682687. doi:10.1155/2009/682687. PMID 19503798.
- ↑ 90.0 90.1 Nagaraja V, Coleman HG, Morgan GJ (September 2013). "Desmoplastic fibroblastoma presenting as a parotid tumour: a case report and review of the literature". Head Neck Pathol. 7 (3): 285–90. doi:10.1007/s12105-013-0435-2. PMC 3738752. PMID 23504494.
- ↑ 91.0 91.1 Kim JH, Oh DY, Kim SW, Lee JH, Ahn ST, Rhie JW (January 2012). "Desmoplastic fibroblastoma of the finger tip in an adult". Arch Plast Surg. 39 (1): 84–6. doi:10.5999/aps.2012.39.1.84. PMC 3385291. PMID 22783503.
- ↑ 92.0 92.1 Darling MR, Kutalowski M, MacPherson DG, Jackson-Boeters L, Wysocki GP (September 2011). "Oral elastofibromatous lesions: a review and case series". Head Neck Pathol. 5 (3): 254–8. doi:10.1007/s12105-011-0274-y. PMC 3173539. PMID 21681661.
- ↑ 93.0 93.1 Daum O, Ferda J, Curik R, Choc M, Mukensnabl P, Michal M (December 2010). "Elastofibromatous changes in tissues from spinal biopsies. A degenerative process afflicting a small but important subset of patients operated for spinal canal compression: report of 18 cases". Int. J. Surg. Pathol. 18 (6): 508–15. doi:10.1177/1066896909339736. PMID 19578045.
- ↑ 94.0 94.1 Tosios KI, Economou I, Vasilopoulos NN, Koutlas IG (March 2010). "Elastofibromatous changes and hyperelastosis of the oral mucosa". Head Neck Pathol. 4 (1): 31–6. doi:10.1007/s12105-009-0153-y. PMC 2825534. PMID 20237986.
- ↑ 95.0 95.1 Smith HG, Hannay JA, Thway K, Messiou C, Smith MJ, Strauss DC, Hayes AJ (March 2016). "Elastofibroma dorsi: The clunking tumour that need not cause alarm". Ann R Coll Surg Engl. 98 (3): 208–11. doi:10.1308/rcsann.2016.0064. PMC 5226161. PMID 26890837.
- ↑ 96.0 96.1 Kourda J, Ayadi-Kaddour A, Merai S, Hantous S, Miled KB, Mezni FE (September 2009). "Bilateral elastofibroma dorsi. A case report and review of the literature". Orthop Traumatol Surg Res. 95 (5): 383–7. doi:10.1016/j.otsr.2009.05.002. PMID 19628444.
- ↑ 97.0 97.1 Hoven-Gondrie ML, IJpma FF, Havenith MG, van Geldere D (2009). "[Elastofibroma dorsi: a characteristic, benign, subscapular swelling]". Ned Tijdschr Geneeskd (in Dutch; Flemish). 153: A569. PMID 19900325.
- ↑ 98.0 98.1 Hayes AJ, Alexander N, Clark MA, Thomas JM (May 2004). "Elastofibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom". Eur J Surg Oncol. 30 (4): 450–3. doi:10.1016/j.ejso.2004.01.006. PMID 15063901.
- ↑ 99.0 99.1 Bhambri A, Del Rosso JQ (June 2009). "Solitary sclerotic fibroma". J Clin Aesthet Dermatol. 2 (6): 36–8. PMC 2923956. PMID 20729948.
- ↑ 100.0 100.1 Nakashima K, Yamada N, Adachi K, Yoshida Y, Yamamoto O (October 2008). "Solitary sclerotic fibroma of the skin: morphological characterization of the 'plywood-like pattern'". J. Cutan. Pathol. 35 Suppl 1: 74–9. doi:10.1111/j.1600-0560.2008.01001.x. PMID 18544068.
- ↑ 101.0 101.1 Requena L, Gutiérrez J, Sánchez Yus E (August 1992). "Multiple sclerotic fibromas of the skin. A cutaneous marker of Cowden's disease". J. Cutan. Pathol. 19 (4): 346–51. PMID 1430474.
- ↑ 102.0 102.1 Mori O, Hachisuka H, Sasai Y (1992). "Sclerotic fibromas of the skin--reports of two cases and a review of the literature in Japan". Kurume Med J. 39 (3): 191–3. PMID 1491554.
- ↑ 103.0 103.1 Lo WL, Wong CK (October 1990). "Solitary sclerotic fibroma". J. Cutan. Pathol. 17 (5): 269–73. PMID 2258475.
- ↑ 104.0 104.1 Hanft VN, Shea CR, McNutt NS, Pullitzer D, Horenstein MG, Prieto VG (February 2000). "Expression of CD34 in sclerotic ("plywood") fibromas". Am J Dermatopathol. 22 (1): 17–21. PMID 10698210.
- ↑ 105.0 105.1 High WA, Stewart D, Essary LR, Kageyama NP, Hoang MP, Cockerell CJ (May 2004). "Sclerotic fibroma-like change in various neoplastic and inflammatory skin lesions: is sclerotic fibroma a distinct entity?". J. Cutan. Pathol. 31 (5): 373–8. doi:10.1111/j.0303-6987.2004.00199.x. PMID 15059222.
- ↑ 106.0 106.1 Shitabata PK, Crouch EC, Fitzgibbon JF, Swanson PE, Adesokan PN, Wick MR (August 1995). "Cutaneous sclerotic fibroma. Immunohistochemical evidence of a fibroblastic neoplasm with ongoing type I collagen synthesis". Am J Dermatopathol. 17 (4): 339–43. PMID 8600796.
- ↑ 107.0 107.1 Alawi F, Freedman PD (June 2004). "Sporadic sclerotic fibroma of the oral soft tissues". Am J Dermatopathol. 26 (3): 182–7. PMID 15166503.
- ↑ 108.0 108.1 Upadhyaya JD, Cohen DM, Islam MN, Bhattacharyya I (June 2018). "Hybrid Central Odontogenic Fibroma with Giant Cell Granuloma like Lesion: A Report of Three Additional Cases and Review of the Literature". Head Neck Pathol. 12 (2): 166–174. doi:10.1007/s12105-017-0845-7. PMC 5953869. PMID 28785965.
- ↑ 109.0 109.1 Sonalika WG, Sahu A, Deogade SC, Gupta P, Naitam D, Chansoria H, Agarwal J, Katoch S (2014). "Giant cell fibroma of tongue: understanding the nature of an unusual histopathological entity". Case Rep Dent. 2014: 864512. doi:10.1155/2014/864512. PMC 3910466. PMID 24511398.
- ↑ 110.0 110.1 Tosios KI, Gopalakrishnan R, Koutlas IG (December 2008). "So-called hybrid central odontogenic fibroma/central giant cell lesion of the jaws. A report on seven additional cases, including an example in a patient with cherubism, and hypotheses on the pathogenesis". Head Neck Pathol. 2 (4): 333–8. doi:10.1007/s12105-008-0076-z. PMC 2807578. PMID 20614305.
- ↑ 111.0 111.1 Sabarinath B, Sivaramakrishnan M, Sivapathasundharam B (September 2012). "Giant cell fibroma: A clinicopathological study". J Oral Maxillofac Pathol. 16 (3): 359–62. doi:10.4103/0973-029X.102485. PMC 3519210. PMID 23248467.
- ↑ 112.0 112.1 Mello-Moura AC, Santos AM, Bonini GA, Del Conte Zardetto CG, Moura-Netto C, Wanderley MT (2016). "Giant Cell Fibroma in a Two-Year-Old Child". Case Rep Dent. 2016: 7058356. doi:10.1155/2016/7058356. PMC 5086372. PMID 27822394.
- ↑ 113.0 113.1 Hosur MB, Puranik RS, Vanaki SS, Puranik SR, Ingaleshwar PS (2018). "Clinicopathological profile of central giant cell granulomas: An institutional experience and study of immunohistochemistry expression of p63 in central giant cell granuloma". J Oral Maxillofac Pathol. 22 (2): 173–179. doi:10.4103/jomfp.JOMFP_260_17. PMC 6097366. PMID 30158768.
- ↑ 114.0 114.1 Kulkarni S, Chandrashekar C, Kudva R, Radhakrishnan R (2017). "Giant-cell fibroma: Understanding the nature of the melanin-laden cells". J Oral Maxillofac Pathol. 21 (3): 429–433. doi:10.4103/jomfp.JOMFP_209_16. PMC 5763868. PMID 29391720.
- ↑ 115.0 115.1 Jimson S, Jimson S (December 2013). "Giant cell fibroma: a case report with immunohistochemical markers". J Clin Diagn Res. 7 (12): 3079–80. doi:10.7860/JCDR/2013/6476.3859. PMC 3919395. PMID 24551733.
- ↑ 116.0 116.1 Chandna P, Srivastava N, Bansal V, Wadhwan V, Dubey P (2017). "Peripheral and Central Giant Cell Lesions in Children: Institutional Experience at Subharti Dental College and Hospital". Indian J Med Paediatr Oncol. 38 (4): 440–446. doi:10.4103/ijmpo.ijmpo_17_16. PMC 5759061. PMID 29333009.
- ↑ 117.0 117.1 Wright JM, Soluk Tekkesin M (2017). "Odontogenic tumors: where are we in 2017 ?". J Istanb Univ Fac Dent. 51 (3 Suppl 1): S10–S30. doi:10.17096/jiufd.52886. PMC 5750825. PMID 29354306.
- ↑ 118.0 118.1 Reddy SV, Medikonda SK, Konda A, Natta S (June 2014). "A rare benign odontogenic neoplasm: peripheral odontogenic fibroma". BMJ Case Rep. 2014. doi:10.1136/bcr-2013-201065. PMC 4069815. PMID 24920510.
- ↑ 119.0 119.1 Baiju CS, Rohatgi S (July 2011). "Peripheral odontogenic fibroma: A case report and review". J Indian Soc Periodontol. 15 (3): 273–5. doi:10.4103/0972-124X.85674. PMC 3200026. PMID 22028517.
- ↑ 120.0 120.1 Sreeja C, Vezhavendan N, Shabana F, Vijayalakshmi D, Devi M, Arunakiry N (July 2014). "Recurrent peripheral odontogenic fibroma associated with basal cell budding". J Pharm Bioallied Sci. 6 (Suppl 1): S204–7. doi:10.4103/0975-7406.137470. PMC 4157271. PMID 25210375.