Levosalbutamol
| Error creating thumbnail: File missing | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category | |
| Routes of administration | Oral, inhalational, IV |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Hepatic |
| Elimination half-life | 1.6 hours |
| Excretion | Urinary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
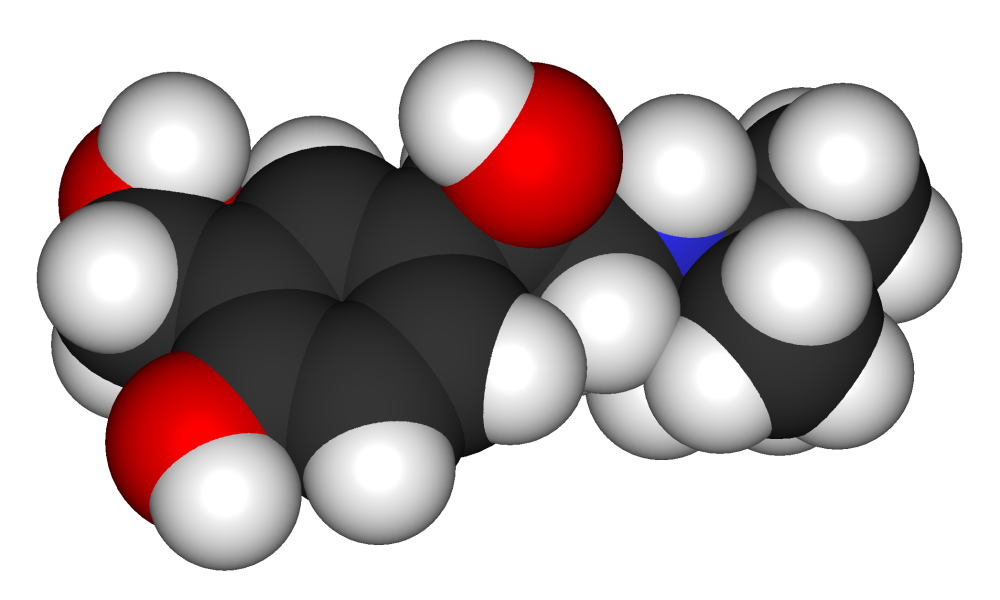
| Formula | C13H21NO3 |
| Molar mass | 239.311 g/mol |
| 3D model (JSmol) | |
| |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Levosalbutamol (INN) or levalbuterol (USAN), trade name Xopenex, is the R-enantiomer of the short-acting β2-adrenergic receptor agonist albuterol (salbutamol).
Uses
As a bronchodilator, it is used to treat asthma and COPD. In general, levalbuterol has similar pharmacokinetic and pharmacodynamic properties to albuterol; however, its manufacturer, Sepracor, has implied (although not directly claimed) that the presence of only the R-enantiomer produces fewer side effects.
Physicians sometimes elect to use levalbuterol in patients with a history of supraventricular tachycardia or other arrhythmias because it is thought that levalbuterol may produce less direct effects on β1-adrenergic receptors in the heart. For similar reasons, some pediatricians also use levalbuterol for patients who experience hyperactivity or jitteriness from racemic albuterol.
Levosalbutamol vs. albuterol
The use of levalbuterol over the more traditionally used racemic albuterol is controversial among health care professionals. That using levalbuterol instead of albuterol produces less direct effect on β1-adrenergic receptors and/or fewer cardiac side effects has been suggested, but not consistently demonstrated by long term, well-designed clinical trials.
There are differing opinions on whether there is sufficient therapeutic benefit to using levalbuterol that outweighs the 5-10 times higher price tag.[1][2] In general, it appears that if a clinician and patient feel that a low dose of racemic mixture is causing undesirable side effects, levalbuterol may be a viable alternative.[3]
Approval
Levalbuterol was originally available only as a solution for nebulizer and eventually become available as a CFC-free metered dose inhaler under the trade name "Xopenex HFA (levalbuterol tartrate) Inhalation Aerosol". The FDA approval date was on March 11, 2005. (See Official FAQ)
Additional studies
In a study conducted by Bill T. Ameredes, PhD, and colleagues from the University of Pittsburgh, that concluded that in combination corticosteroids treatments the (S)-isomer found in Albuterol had a profound nullifying effect. In the (R)- albuterol isomer it shown to enhance anti-inflammatory steroid treatment. [4]
In other works he considers the combination (R)(S)-Albuterol a problematic drug.[5]
References
- ↑ Comparison of racemic albuterol and levalbuterol in the treatment of acute asthma in the ED.
- ↑ Levalbuterol is not more cost-effective than albuterol for COPD.
- ↑ Point-Counterpoint: A Comparison of Levalbuterol and Racemic Albuterol in the Treatment of Pediatric Asthma.
- ↑ Ameredes BT, Calhoun WJ (2005). "Modulation of GM-CSF release by enantiomers of beta-agonists in human airway smooth muscle". J. Allergy Clin. Immunol. 116 (1): 65–72. doi:10.1016/j.jaci.2005.03.007. PMID 15990776.
- ↑ Ameredes BT, Calhoun WJ (2006). "(R)-albuterol for asthma: pro [a.k.a. (S)-albuterol for asthma: con]". Am. J. Respir. Crit. Care Med. 174 (9): 965–9, discussion 972-4. doi:10.1164/rccm.2606001. PMID 17060667.
- Pages with script errors
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- Asthma
- Beta-adrenergic agonists
- Bronchodilators
- Phenethylamines
