Saphenous vein graft
| Saphenous vein graft | |
 | |
|---|---|
| Saphenous vein grafts for coronary arteries |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [3], Jason C. Choi, M.D., Xin Yang, M.D.
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Since Rene Favaloro first described it in 1967, coronary artery revascularization with saphenous veins (saphenous vein grafts or SVGs) has become a surgical standard for treatment of coronary artery disease. When a native coronary artery is obstructed, the sutured graft provides a connection between the aorta and the coronary artery beyond the area of obstruction. The procedure is repeated on all the coronary artery segments that are significantly diseased.
The vein is often removed by cardiac surgeons and used for autotransplantation in coronary artery bypass operations, when arterial grafts are not available or many grafts are required, such as in a triple bypass or quadruple bypass.
SVG Anatomy
Saphenous Vein Graft Harvesting
Saphenous Vein Graft Nomenclature
Assessment of Target Vessels for Saphenous Vein Grafting
A coronary artery may be unsuitable for bypass grafting if it is small (< 1 mm or < 1.5 mm depending on surgeon preference), heavily calcified (meaning the artery does not have a section free of CAD) or intramyocardial (the coronary artery is located within the heart muscle rather than on the surface of the heart). Similarly, a person with a single stenosis ("narrowing") of the left main coronary artery requires only two bypasses (to the LAD and the LCX). However, a left main lesion places a person at the highest risk for death from a cardiac cause.
Although the cardiothoracic surgeon reviews the coronary angiogram prior to surgery and identifies the lesions (or "blockages") in the coronary arteries and will estimate the number of bypass grafts prior to surgery, the final decision is made in the operating room upon examination of the heart and the suitability of the vessel for bypassing.
Pathophysiology of Saphenous Vein Graft Disease
Several factors contribute to stenosis of saphenous vein grafts, including intimal hyperplasia, plaque formation, and graft remodeling. Additionally, arterialization of the graft accelerates atherosclerosis. Furthermore, atheroma found in SVGs are more friable (easily break into small pieces) and more prone to thrombus than plaques found in native vessels. Another reason why SVGs are more susceptible to thrombotic occlusion is that they lack side branches.
Saphenous Vein Graft Patency
Definitions
Saphenous vein graft occlusion is defined as a complete, 100% occlusion of a saphenous vein graft. [1]
Saphenous vein failure is defined as an occlusion of the vein graft or a 75% or greater stenosis.
The rate of occlusion or failure of saphenous vein grafts is calculated on a per graft basis and a per patient basis. The per patient basis is higher, because only one vein graft out of several must fail for the patient to be characterized as a failure. Analyses should be presented on both a per patient basis (the unit of randomization) and a per SVG basis (the unit that is associated with clinical events). Because the behavior of multiple SVGs may be correlated, and this within patient correlation may reduce the estimate of the variance in the population, an adjustment for the within patient correlation must be provided when presenting the results on a per SVG basis[2]. The within patient conocrdance can be adjusted for using a General Linear Model of Intraclass Correlation (GLIMIC) [2].
Current rates of graft occlusion and failure are as follows:[1] The rate of per patient vein graft occlusion at 12-18 months is about 42%
The rate of per patient vein graft failure at 12-18 months is about 46%
The rate of per graft vein graft occlusion at 12-18 months is about 26%
The rate of per graft vein graft failure at 12-18 months is about 29%
As a comparison, the rate of internal mammary artery failure at 12-18 months was only 8%.
These carefully ascertained current rates of occlusion are higher than what are often quoted in the literature which were [3]:
- 15% rate of SVG occlusion at 1 year
- 25% rate of SVG occlusion at 6 years
- 40% rate of SVG occlusion at 10 years
Determinants of Sapheous Vein Graft Patency
Graft patency is dependent on a number of factors, including the type of graft used (internal thoracic artery, radial artery, or great saphenous vein), the size or the coronary artery that the graft is anastomosed with, and, of course, the skill of the surgeon(s) performing the procedure. Arterial grafts (e.g. left internal mammary (LIMA), radial) are far more sensitive to rough handling than the saphenous veins and may go into spasm if handled improperly.
In-situ vs Free Grafts
Generally the best patency rates are achieved with the in-situ (the proximal end is left connected to the subclavian artery) left internal thoracic artery (a LIMA) with the distal end being anastomosed with the coronary artery (typically the left anterior descending artery or a diagonal branch artery). Lesser patency rates can be expected with radial artery grafts and "free" internal thoracic artery grafts (where the proximal end of the thoracic artery is excised from its origin from the subclavian artery and re-anastomosed with the ascending aorta).
Venous vs Arterial Conduits
Saphenous vein grafts have poorer patency rates than arterial grafts, but are more available, as the patients can have multiple segments of the saphenous vein used to bypass different arteries.
LITA grafts are longer-lasting than vein grafts, both because the artery is more robust than a vein and because, being already connected to the arterial tree, the LITA need only be grafted at one end. The LITA is usually grafted to the left anterior descending coronary artery (LAD) because of its superior long-term patency when compared to saphenous vein grafts.[4][5]
Impact of Harvesting Method on Saphenous Vein Graft Patency
The method of harvesting vein grafts may be associated with late vein graft patency at 12-18 months.[6] In a non-randomized subgroup analysis from the PREVENT IV study, harvesting of vein-grafts with the use of endoscopy (endoscopic harvesting) was associated with a higher rate of saphenous vein graft failure compared with open harvesting of the veins under direct visualization (46.7% vs. 38.0%, P<0.001 at 12-18 months). Likewise, clinical outcomes were worse at 3 years: use of endoscopy was associated with higher rates of death, myocardial infarction, or repeat revascularization (20.2% vs. 17.4%; p=0.04), death or myocardial infarction (9.3% vs. 7.6%; p=0.01), and death (7.4% vs. 5.8%; adjusted hazard ratio, 1.52; 95% CI, 1.13 to 2.04; p=0.005). Although these observational data are provocative, further randomized clinical trials would be needed to compare the safety and effectiveness of the two harvesting technique.
Pharmacotherapy
In a relatively modest sized study, there was a significant improvement in SVG patency to 91.6% (219/239) among patients treated with both aspirin and clopidogrel versus 85.7% (198/231) in those patients treated with aspirin alone (relative risk: 1.707; 95% confidence interval: 1.010 to 2.886; multivariat p = 0.043)[7]
Impact of Initial CABG Results and Runoff
Greater runoff, and higher mean graft flow have been associated with improved SVG patency, whereas the pulsatile index has been associated with worse patency[8].
Saphenous Vein Graft Diseases
Saphenous Vein Graft Aneurysms
It is also known as SVGA, aortocoronary saphenous vein graft aneurysms, saphenous vein graft aneurysm disease and saphenous vein graft aneurysmal dilatation.
Causes of Saphenous Vein Graft Aneurysms
- Atherosclerosis
- Hypertension
- Mycotic
- Postoperative mediastinitis
- Previous aneurysms
- Torn sutures
Amyloidosis of Saphenous Coronary Bypass Grafts
Amyloid has been associated with accelarated disease in saphenous vein grafts.[9] [10] [11] [12] [13]
Rupture of the Saphenous Vein Coronary Artery Bypass Grafts
Aspergillus species causing a necrotizing vasculitis have been associated with rupture of a saphenous vein grafts.
Diagnosis and Evaluation of SVG Disease
Symptoms of SVG Occlusion
SVG occlusion is often asymptomatic. The sensitivity of new or recurrent chest pain in the detection of SVG occlusion is 60% and the specificity is 20% [14].
Chest X-Ray
In a patient who has undergone CABG, a chest X-ray will demonstrate multiple small clips near the heart and coronary arteries. Large circular sternal wires will also be seen. Examples are shown in the images below.
-
Median sternotomy wires and CABG clips
-
Lateral graphy: Median sternotomy wires and CABG clips
Coronary Angiography
Coronary angiography is often used to ascertain the patency and percent stenoses of saphenous vein grafts.
Technique
Most often a Judkin's Right 4 catheter (JR 4) catheter is used to engage the saphenous vein grafts. If this diagnostic catheter has insufficient "reach" to engage the SVG ostium, then an Amplatz catheter can be used. The optimal view to engage the ostium of the SVG varies from operator to operator. The most popular views to engage the ostium are the left anterior oblique 45 degrees view (LAO 45) with no cranial angulation. Some operator will use the right anterior oblique view (RAO) with 45 degrees of angulation and no cranial angulation. It should be noted that the SVGs supplying the left coronary arteries will come off of the left hand side of the screen and those supplying the right coronary artery will come off of the right hand side of the screen.
If an SVG is known from the operative report to exist, but cannot be selectively engaged, then a non-selective aortogram can be performed to aid in identifying the presence and location of patent SVGs. The aortogram is performed with an injection through an angled pigtail catheter with the camera gantry located in the 45 degree left anterior oblique (LAO) position with no cranial angulation.
In order to engage the left internal mammary artery (which is not a saphenous vein graft but is often interrogated during the process of evaluating SVGs), a view with slight cranial, and slight left anterior oblique (LAO) angulation is used. a Judkin's Right 4 catheter (JR 4) catheter is used to engage the ostium of the subclavian artery. With the catheter near the anticipated origin of the subclavian artery, a counterclockwise motion of the catheter is needed to engage the ostium. Once the ostium is engaged, an exchange length 0.038 J tipped wire is then advance into the subclavian artery. A left internal mammary artery (LIMA) catheter is then exchanged to engage the origin of the left internal mammary artery. Again, this engagement is accomplished with counterclockwise motion of the catheter. An injection with the camera in this angulation is a suitable first view of the LIMA, with careful attention in this view paid to the ostium of the LIMA. the next view is often a left anterior oblique (LAO) view with 90 degrees of angulation (LAO 90). This allows for accurate assessment of the LIMA anastomosis to the left anterior descending artery.
Impact of saphenous vein graft radiographic markers on clinical events and angiographic parameters
One technique that has been used to improve the ascertainment of SVG patency and stenosis is the placement of radio-opaque markers. Use of such markers has been associated with shorter cardiac catheterization procedure times and reduced contrast agent volume for postoperative coronary artery bypass graft (CABG) catheterizations. In the large PREVENT 4 study [1][15], approximately half the patients had SVG markers present (51.2% or 910 of 1,778 patients) and half the SVGs (52.3% of SVGs or 2,228 of 4,240). If the patient had a totally occluded SVG (n = 911), visual identification of the occluded SVG was obtained more frequently among those patients who had an SVG marker (90.7% vs 72.1%, p < 0.001). The identification of SVG stenosis which were > 70% did not differ by the use of SVG markers (25.8% with marker vs 24.4% without marker, p = not significant). These findings were also consistent in ostial lesions (n = 942). The use of an SVG marker was not associated with a difference in the long-term risk of death or myocardial infarction (MI). However, it was noted that the rate of perioperative CABG MI was higher among patients who had an SVG marker (10.1% vs 5.5%, odds ratio adjusted 1.86, p = 0.021).
Use of Coronary Angiography of Saphenous Vein Graft Disease as Endpoint in Clinical Trials Evaluating Pharmacotherapy and Device Based Therapies
SVG Patency and SVG Narrowing as a Surrogate Endpoint for Clinical Events
One issue that arises is the suitability of SVG patency, and SVG narrowing as a surrogate endpoint for clinical events.
There are multiple studies demonstrating that SVG closure or failure is associated with clinical events. The association of SVG failure or narrowing with clinical events is complex and should be interpreted in light of the following nuances:
- The SVG may close and the native artery may remain open minimizing the symptoms associated with SVG failure. SVG failure may therefore by clinically "silent" or may not be closely associated with "hard endpoints" such as myocardial infarction(MI).
- Placement of SVGs has been associated with improved survival over medical therapy particularly in patients with left main disease and three vessel disease. In so far as the mechanism of clinical benefit of SVGs is predicated upon their ongoing patency, this supports the relevance of SVG patency as a surrogate endpoint.
- Despite the native artery remaining open after SVG failure, it should be realized that placement of an SVG is associated with more rapid disease progression in the grafted native coronary artery. SVG placement therefore exposes the patient to a risk of more rapid native disease progression. There is a 4 to 6 fold increase in the risk of proximal native vessel occlusion following the placement of an SVG, while there is limited impact upon disease progression downstream from the SVG [16][17][18][19] . While long-term studies demonstrate that as many as 22/23 grafted vessels occlude proximal to the SVG insertion site, the patency beyond the SVG insertion remains better (only 8 of 39 segments failed)[19]. Progression of native disease is more rapid in segments bypassed by and SVG than those bypassed by an arterial conduit (p = 0.001, odds ratio = 2.03)[20]. In summary, if the SVG fails, the patient most often is left with greater progression of the underlying native vessel disease than they would have had had they not had an SVG placed. It is difficult to ascertain the impact of native vessel disease acceleration given the limited duration of follow-up in trials of SVGs. The impact of disease progression may not be apparent for many years and may be underestimated in current trials and analyses.
- As a nuance of the above, the impact of SVG failure may depend in part upon when it occurs.
- SVG failure not only leads to a potential reduction in antegrade blood flow to the bypassed segment as a result of vessel closure, there is also the potential for embolizaiton from a large occluded conduit into the downstream native circulation. SVGs do not have sidebranches and there is therefore no capacity for alternate run off when occlusion occurs. As a result, SVGs often occlude back to the origin of the SVG. Furthermore, the diameter of SVG often exceeds that of native arteries. As a result of the fact that the SVG occludes back to the ostium and is of a larger volume than a native coronary artery, there is a much larger embolic burden associated with a SVG.
- Consistent with the embolic hazard cited above, is the fact that dilation of an SVG failure does not lead to improved clinical outcomes. The fact that opening a closed SVG does not lead to improved outcomes may lead to inappropriate confusion surrounding SVG failure as a relevant clinical outcome. While it may be intuitive that opening an occluded or failed SVG would lead to improved outcomes (consistent with SVG failure being a surrogate), opening the occluded SVG may instead lead to embolizaiton of a large amount of the thrombotic material downstream. Preventing SVG occlusion may be related to improved outcomes, but treating SVG occlusion after it occurs may not be related to improved outcomes. The failure of reopening an occluded SVG to improve outcomes should not detract from the importance and relevance of preventing SVG occlusion in the first place as a valid surrogate endpoint.
- The patient is the unit of randomization, but the SVG is the unit most closely related to clinical events.
In summary there are multiple mechanisms whereby SVG patency is related to clinical outcomes.
- Closure of the conduit may reduce antegrade blood flow
- There may be embolization into the native vessel from the thrombosed SVG conduit, the diameter of which often exceeds the native coronary artery
- The SVG may have accelerate native vessel disease which predisposes the patient to adverse outcomes when the vessel occludes
Is the timing of SVG failure relevant? If an anticoagulant (either antiplatelet or antithrombin) is undergoing evaluation of its efficacy in the prevention of thrombotic graft closure, then it is irrelevant if this thrombotic closure is early (in the immediate peri-operative period) or late. It could be hypothesized that the clinical benefit of the anticoagulant agent would be operative during both the early and late follow-up periods.
Potential for Ascertainment Bias
There are several issues that arise with respect to ascertainment bias in the use of coronary angiograms as an endpoint.
- The patient may not return for follow-up angiography. Maybe the patient is feeling so well they don't feel compelled to return for repeat angiography (you missed a positive treatment effect), or maybe they are so sick they can't show up (you missed a negative treatment effect). If patients died, traditionally they are counted or imputed as having SVG failure on both a per patient and a per SVG conduit basis. The percent of patients who returned for follow-up angiography was 80% in the PREVENT 4 study [1]
- The patient may return for follow-up angiography, but one or more of the SVGs cannot be engaged and selectively injected. As stated above, in the PREVENT 4 study, the use of saphenous vein graft markers improved the odds of finding SVGs in particular occluded SVGs [15]. However, the SVG stenosis 70% or greater at follow-up did not differ by use of markers (25.8% with marker vs 24.4% without marker, p = not significant). In other words, there does not seem to be ascertainment bias whereby failure to find the SVG results in a different outcome (the outcomes in patients with SVG markers with a greater degree of ascertainment of the endpoint were no different).
Per Patient versus Per SVG as the Unit of Analysis
Analyses should be presented on both a per patient basis (the unit of randomization) and a per SVG basis (the unit that is associated with clinical events). Because the behavior of multiple SVGs may be correlated, and this within patient correlation may reduce the estimate of the variance in the population, an adjustment for the within patient correlation must be provided when presenting the results on a per SVG basis[2]. The within patient conocrdance can be adjusted for using a General Linear Model of Intraclass Correlation (GLIMIC) [2].
CT Angiography
There is interest in the non-invasive assessment of SVG patency using CT imaging.
In a recent study that used SVG patency as the primary endpoint, 224/249 (90.3%) of patients returned for follow-up CT at 3 months. There were 704 grafts in these 224 patients. Only 11 segments were non-diagnostic (1.6%). In this relatively modest sized study, there was a significant improvement in SVG patency to 91.6% (219/239) among patients treated with both aspirin and clopidogrel versus 85.7% (198/231) in those patients treated with aspirin alone (relative risk: 1.707; 95% confidence interval: 1.010 to 2.886; p = 0.043)[21].
Early Studies Using 16 Slice CT
Early studies demonstrated a sensitivity of 92% to 100% and a specificity of 89% to 100% in the evaluation of SVG patency with invasive angiography as the gold standard. In the same studies, in the detection of IMA patency, the sensitivity has ranged from 80% to 100% and the specificity has ranged from 82% to 100% [22][23][24].
Methodologic Issues
There are methodologic issues that should be highlighted when evaluating comparisons of CT to angiography as the gold standard. In the above studies, between 4% and 29% of the SVGs were unevaluable[22][23][24]. In the study by Anand, only those patients with disease on CT underwent angiography [25]. More than half of the patients in the study did not undergo invasive angiography, so statements regarding sensitivity and specificity cannot be made. 6 out of 102 SVGs could not be evaluated. Among those selected patients who underwent angiography, there were two false positive diagnoses of a stenosis, and there was "100% predictice accuracy in detecting graft occlusion, and 85% predictive accuracy in detecting graft stenosis". Again, this is an overstatement given that not all patients underwent protocol mandated angiography.
Contemporary Studies Using 64 Slice CT
The resolution of CT angiography improved with the introduction of 64 slice CT. The assessment of the presence of either a stenosis or occlusion of SVG has been associated with high rates of sensitivity of (97%), specificity (97%), and positive and negative predictive values of 93% and of 99%, respectively [26]. Arrhythmias and heart rates > 65 beats/minute during scanning were associated with errors in assessment. It should be noted that in modern studies such as the one above, 12 segments were excluded from analysis because of the presence of stents which are associated with blooming artifact. IT should also be noted that 9 out of 406 grafts demonstrated insufficient image quality for the assessment of the SVGs due either to motion artifacts (8 SVGs) or numerous metallic clips adjacent to the bypass graft (1 SVG). When the data is analyzed on a per patient basis rather than a per SVG basis, among evaluable patients the following were observed [26]:
- Sensitivity: 100% (95% CI 94% to 100%)
- Specificity: 92% (95% CI 82% to 97%)
- Positive predictive value (PPV): 93% (95% CI 85% to 97%)
- Negative predictive value (NPV): 100% (95% CI 93% to 100%)
When all patients were included in the analysis (including those in whom the CT was unevaluable) the rates were as follows [26]:
- Sensitivity: 100% (95% CI 94% to 100%)
- Specificity: 87% (95% CI 76% to 93%)
- Positive predictive value (PPV): 89% (95% CI 79% to 94%)
- Negative predictive value (NPV): 100% (95% CI 93% to 100%)
It should also be noted that these patients were symptomatic and the pre-test probability was high. These rates may be poorer in an asymptomatic population with a low pre-test probability.
Radiation Dose with CT Scans
It should be noted that the radiation dose is more than twice as high for CT scans as it was for invasive angiography (17.8 +/- 5.4 mSv and 8.8 +/- 4.5 mSv, respectively, p < 0.05)[26].
Simultaneous Assessment of Native and SVG Disease
The assessment of SVGs is simplified by the fact that the SVGs are stationary while there is motion artifact in the assessment of native coronary arteries. The assessment of native coronary artery disease in addition to SVG conduits was investigated by Ropers et al [27]. Fifty patients with a total of 138 arterial and venous conduits were assessed a mean of 106 months after CABG. All the arterial and the venous conduits were both evaluable and were correctly classified as either being occluded (n=38) or patent (n=100) when compared with angiography as the "gold standard". With respect to SVG stenosis severity, Sensitivity for stenosis detection in patent grafts was 100% (16/16) with a specificity of 94% (79/84). For the per-segment evaluation of native coronary arteries and distal runoff vessels, sensitivity in evaluable segments (91%) was 86% (87/101) with a specificity of 76% (354/465). If evaluation was restricted to nongrafted arteries and distal runoff vessels, sensitivity was 86% (38/44) with a specificity of 90% (302/334). On a per-patient basis, classifying patients with at least 1 detected stenosis in a CABG, a distal runoff vessel, or a nongrafted artery or with at least 1 unevaluable segment as "positive," MDCT yielded a sensitivity of 97% (35/36) and specificity of 86% (12/14).
Incidental Findings on CT
One study indicated that about 20% of patients undergoing cardiac CT have an incidental finding at the time of the imaging. 9.3% of patients had a cardiac finding such as a pseudoaneurysm or intracardiac thrombus, and 13.1% of patients had a noncardiac finding including pulmonary embolism, lung cancer, or pneumonia[28].
MR Angiography
Postmortem Angiography
Pathological Findings
-
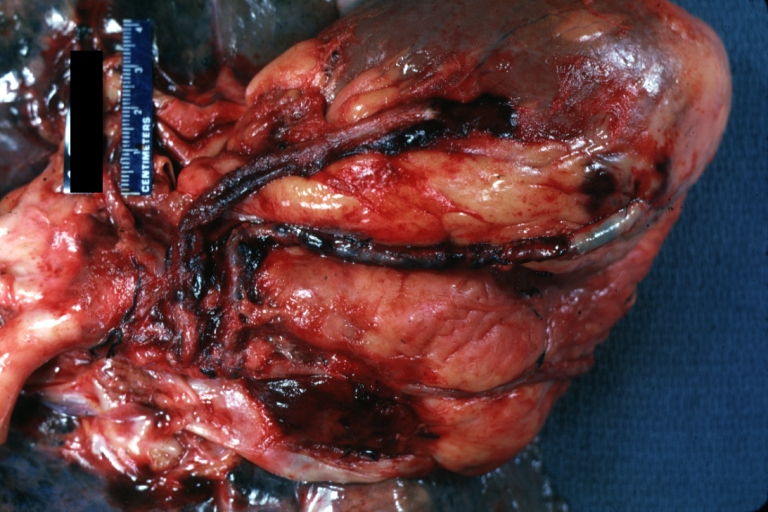
Saphenous vein coronary bypass graft: Gross, natural color, external view of heart with thrombosed veins
-
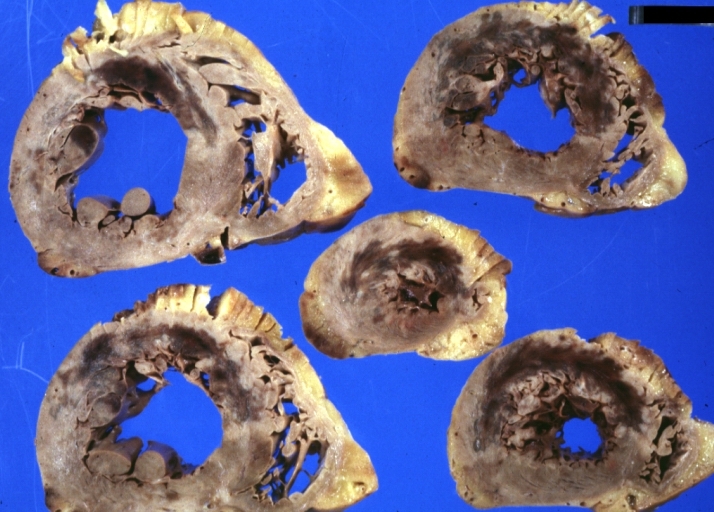
Saphenous vein coronary bypass graft: Thrombosis, Acute: Gross, fixed tissue but well shown cross sections of bypass graft and anastomotic site with thrombosis. 61 yo male, with and acute infarct treated with streptokinase and two days later had bypass. Died 5 days post op. Two veins are thrombosed
-
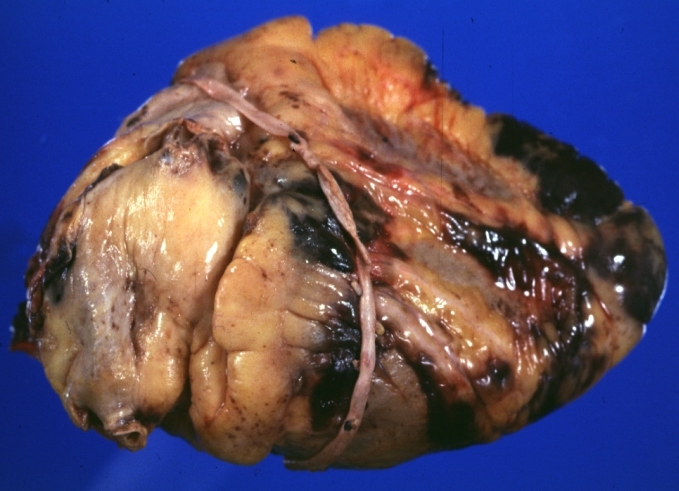
Myocardial Infarct Acute Reflow Type: Gross, fixed tissue but good color. A very enlarged heart with moderate LV dilation and high anterior wall hemorrhagic infarct. Initially treated with streptokinase and two days later had saphenous vein grafts. Both grafts are thrombosed. He died after 5 days
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Treatment
Goals of Treatment
Primarily, the goal should be to detect and treat a SVG stenosis early in the development of ischemia while the SVG is still patent. Although intervention on a chronic total occlusion of a SVG may seem like an effective treatment strategy, it is best avoided. As long as the SVG is not completely occluded, intervention can be performed.
Two additional overall goals of treating SVG stenosis include the resolution of symptomatic ischemia and the prevention/treatment of distal embolization.
Treatment Options
There are many different choices to consider when deciding the most appropriate treatment for SVG stenosis, including PTCA, PCI with bare metal or drug-eluting stents, PCI with covered stents, embolic protection devices, debulking/thrombus removal, and surgical revascularization.
Percutaneous Transluminal Coronary Angioplasty (PTCA)
PTCA has high initial revascularization success rates in the treatment of SVG stenosis. However, it is also associated with high rates of periprocedural complications, including acute vessel closure secondary to dissection and in-situ thrombosis. Additional complications include distal embolization and no reflow, which can lead to periprocedural infarction.
In modern interventional cardiology, PTCA is not often used as the sole means of treatment for SVG stenosis. Instead, stenting has become the cornerstone of treatment, while the use of PTCA has been limited to pre-dilation and post-dilation.
PCI with Bare Metal Stents (BMS) or Drug-eluting Stents (DES)
Most current vein graft treatment strategies utilize PCI with stents (BMS or DES), since stenting is a superior treatment when compared to PTCA alone. As demonstrated in the SAVED (Saphenous Vein De Novo) Trial[29], the use of stents is associated with higher revascularization success rates, decreased restenosis rates, and improved clinical outcomes when compared to PTCA. Generally, DES are preferred over BMS, since DES are associated with reduced rates of restenosis and target vessel revascularization.
Despite their higher success rates, stents are not immune to restenosis. Predictors for restenosis include long stent length, multiple stents, overlapping stents, smaller vessel size, diabetes mellitus, and stenosis at the coronary or aortic anastomosis.
PCI with Covered Stents
Theoretically, stents covered with a polymer membrane would have higher success rates than standard BMS and DES. One would expect covered stents to effectively trap friable atheroma and isolate the graft lumen from the diseased wall, thereby reducing incidence of restenosis, distal embolization, and no reflow in comparison to traditional stents. However, the RECOVERS (The Randomized Evaluation of polytetrafluoroethylene COVERed stent in Saphenous vein grafts)[30] and STING (STents IN Grafts)[31] trials did not show any advantage in using covered stents when compared to bare metal stents for SVG lesions.
Embolic Protection Devices
During PCI of SVGs, atheroembolic debris can be liberated. This debris contains vasoactive substances that can contribute to no reflow, which can in turn considerably increase the risk of major adverse clinical events (MACE)[32]. Fortunately, embolic protection devices help capture this debris and improve outcomes in PCI for SVG stenosis. Therefore, it is recommended that these devices should be utilized in the intervention of most SVG lesions.
Currently, the FDA has approved five embolic protection devices in the United States. Specifically, these devices include one distal occlusion device, three filters, and one proximal occlusion device.
The FDA-approved distal occlusion device is called the PercuSurge Guardwire®, which involves inflating a balloon distal to the stenosis to occlude flow, thereby trapping the debris and vasoactive substances and preventing them from flowing downstream. Due to its small size, it requires little landing zone to deploy. The SAFER (Saphenous vein graft Angioplasty Free of Emboli Randomized) trial[33] showed that when compared to conventional guidewires, balloon occlusion devices (PercuSurge Guardwire®) reduced the rates of infarction and no-reflow after intervention. Despite these advantages, the PercuSurge Guardwire® may not be the best option for all, as some patients may not tolerate the necessary 3-5 minutes of ischemic time associated with this device. Additionally, it is known to cause both hemodynamic and arrhythmic complications.
Filter devices allow continual distal perfusion while macroscopic emboli are trapped in the filter. The FIRE (FilterWire EX During Transluminal Intervention of Saphenous Vein Grafts) trial[34][35] showed that FilterWire may be preferred over PercuSurge Guardwire® due to improved clinical outcomes. While they may reduce ischemic time, filter devices are associated with their own set of potential complications. They are more difficult to deliver than balloon occlusion devices, so their own delivery may lead to distal embolization, and they may not trap microscopic mediators of no reflow. Additionally, they require a significant landing zone distal to the lesion for the filter placement, which can be problematic for certain distal lesions that do not have enough room. There have also been case reports of filter entrapment in the graft after the completion of the PCI.
The FDA-approved proximal occlusion device is called the Proxis® device. Some advantages of this decide are that its deployment does not require crossing the stenosis, it provides superior support that is helpful where balloon or stent delivery is difficult, and it provides protected crossing of the lesion, if required. However, as shown by the PROXIMAL (Proximal Protection During Saphenous Vein Graft Intervention Using the Proxis Embolic Protection System) trial[36], in terms of overall outcomes, there is no significant difference in death, MI, or target vessel revascularization (TVR) between distal and proximal embolic protection devices.
Debulking/Thrombus Removal
Data has not demonstrated a durable clinical benefit associated with debulking/thrombus removal. However, there are certain situations in which debulking techniques may be useful when treating saphenous vein grafts. For instance, severely calcified and stenotic lesions can make regular stent insertion especially difficult. When SVG lesions are too calcified to be crossed by a balloon or adequately dilated prior to stent placement, debulking and thrombus removal can change the compliance of the vessel wall. In addition, this technique is also useful if a lesion is at the aorto-ostial junction. Adjunctive stenting leads to better short and long term results.
There are several debulking/thrombus removal techniques, including directional coronary atherectomy, transluminal extraction catheter thrombectomy, rotational atherectomy, and laser atherectomy.
- Directional coronary atherectomy (DCA) uses a circular cutting blade that excises atheroma into a chamber for removal. It is useful for aorto-ostial lesions and focal lesions in large vessels. However, due to its bulky nature, it is generally not used in vessels with angulation, tortuosity, or heavy calcification. CAVEAT II (Coronary Angioplasty Versus Excisional Atherectomy Trial)[37] examined how PTCA and DCA compared in the treatment of patients with coronary artery bypass graft stenoses. This study demonstrated that DCA was associated with higher initial angiographic success rates and larger acute luminal dimensions in comparison to PTCA. However, despite these successes, DCA also displayed an increased rate of non-Q wave myocardial infusion and distal embolization than PTCA. Furthermore, both techniques displayed similar restenosis rates.
- Additionally, a retrospective study compared DCA vs. PTCA alone vs. PCI with stenting in SVG lesions. It showed no differences in mortality, angina, infarction, or repeat revascularization among the different methods. However, this study displayed increased angiographic complications with DCA use.
- Transluminal extraction catheter (TEC) thrombectomy is designed to remove thrombus from SVGs prior to stenting. It operates through the use of cutting blades with a rotating catheter and an external suction device. However, because the TEC Best trial showed no benefit of TEC prior to the stenting of SVGs, this technique has fallen out of favor. Furthermore, TEC is also associated with a significant incidence of distal embolization and no reflow.
- Rotational atherectomy (RA) uses a rotating cutting blade to grind calcified atheroma. Despite its ability to grind calcification, this method is associated with high rates of no reflow, distal embolization, perforation, and dissection. Furthermore, this method is contraindicated for lesions located in the body of SVGs or in degenerated vein grafts.
- Laser atherectomy uses monochromatic light energy to disrupt plaques. Despite this approach's innovation, there is no evidence that this strategy improves outcomes in lesions, and it has been complicated by high rates of dissection and perforation.
Surgical Revascularization
Given increased perioperative mortality, surgical revascularization is not an optimal treatment strategy, as many patients with graft disease are poor surgical candidates. However, surgery may be required in patients with multi-vessel disease and when PCI fails.
Additionally, reoperation is not strongly encouraged, as it does not provide the same level of revascularization and resolution of angina as the initial procedure. Furthermore, a LIMA may be jeopardized in a reoperation.
Making a Selection
At the earliest signs of recurrent ischemia, it is important to strongly consider the possibility of a patent but stenosed SVG, so that the graft lesion can be treated before the graft becomes completely occluded. Prompt treatment is essential, since a graft is lost once it becomes completely occluded.
Regardless of treatment choice, all patients should be given statins and aspirin (begun immediately following CABG), which are effective in the secondary prevention of SVG stenosis.
For most SVG lesions, PCI with stenting appears to be the therapy of choice. DES are associated with a decreased restenosis rate over BMS, and should be used preferentially if the patient is able to tolerate dual platelet therapy for a minimum of a year. Furthermore, embolic protection devices should be strongly considered for all SVG lesions, especially those with high risks for distal embolization.
In cases in which stent delivery and expansion may be difficult due to heavily calcified and stenotic lesions, atherectomy devices, used with stenting, may be considered. Furthermore, these devices can be useful in lesions that are aorto-ostial.
Zoghbi et al. conducted a study to investigate the role of pretreatment with nitroprusside before SVG intervention[38]. They studied sixty-four consecutive patients with normal preprocedural cardiac enzymes that underwent SVG PCI, without the use of embolic protection devices. They found that pretreatment with nitroprusside results in a lower magnitude and frequency of post-procedural cardiac enzyme elevation. Thus, it is important to consider nitroprusside use.
Finally, while GP IIb/IIIa inhibitors are frequently used in the setting of SVG intervention, their benefit has not been fully evaluated in randomized trials of this lesion subset.
Other Concerns
As with all medical procedures, complications for SVG intervention can occur. Risk factors for complications include: older graft age (>3-5 years), the presence of thrombus, and diffuse disease.
Although PCI with stenting is effective for focal lesions, there is uncertainty regarding the best treatment for diffusely degenerated SVGs. In these cases, it is often a better choice to abandon the graft and intervene on the native vessel instead.
As mentioned above, prevention of no reflow should be attempted with embolic protection devices, pretreatment using nitroprusside and the avoidance of high-pressure inflations and unnecessary pre/post-dilation and oversizing. However, in the event that no reflow develops, it should be aggressively managed with intracoronary vasodilators (i.e. diltiazem, nicardipine, adenosine, and nitroprusside).
Clinical Trials
- Radial Artery Versus Saphenous Vein Grafts in Coronary Artery Bypass Surgery
- The RETRIEVE Study: Use of the FiberNet Embolic Protection System in Saphenous Vein Grafts
- The SOS (Stenting Of Saphenous Vein Grafts) Trial
- Symbiot III: A Prospective Randomized Trial Evaluating the Symbiot Covered Stent System in Saphenous Vein Grafts
- Comparison of Safety and Efficacy of Two Different Drug Eluting Stents Implanted Into Saphenous Vein Grafts
- Evaluating the Role of Thrombin in Saphenous Vein Graft Failure After Heart Bypass Surgery
- Acupuncture and Post-Surgical Wound Healing
- RRISC Study: Reduction of Restenosis In Saphenous Vein Grafts With Cypher Sirolimus-Eluting Stent.
- Treatment of Moderate Vein Graft Lesions With Paclitaxel Drug Eluting Stents: The VELETI Trial
- Trial of Clopidogrel After Surgery for Coronary Artery Disease (CASCADE Trial)
- Multicentre Radial Artery Patency Study: 5 Year Results
- Study to Test the Efficacy and Safety of Drug Eluting vs. Bare-Metal Stents for Saphenous Vein Graft Interventions (BASKETSAVAGE)
- Vein-Coronary Atherosclerosis And Rosiglitazone After Bypass Surgery: The VICTORY Trial
- Copenhagen Arterial Revascularization Randomized Patency and Outcome Trial (CARRPO)
- The SOS (Stenting Of Saphenous Vein Grafts) Trial
- The eSVS (TM) Mesh External Saphenous Vein Support Trial
References
- ↑ 1.0 1.1 1.2 1.3 Alexander JH, Hafley G, Harrington RA, Peterson ED, Ferguson TB, Lorenz TJ, Goyal A, Gibson M, Mack MJ, Gennevois D, Califf RM, Kouchoukos NT (2005). "Efficacy and safety of edifoligide, an E2F transcription factor decoy, for prevention of vein graft failure following coronary artery bypass graft surgery: PREVENT IV: a randomized controlled trial". JAMA : the Journal of the American Medical Association. 294 (19): 2446–54. doi:10.1001/jama.294.19.2446. PMID 16287955. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ 2.0 2.1 2.2 2.3 Gibson CM, Kuntz RE, Nobuyoshi M, Rosner B, Baim DS (1993). "Lesion-to-lesion independence of restenosis after treatment by conventional angioplasty, stenting, or directional atherectomy. Validation of lesion-based restenosis analysis". Circulation. 87 (4): 1123–9. PMID 8462141. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Motwani JG, Topol EJ. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 1998;97:916-31.
- ↑ Kitamura S, Kawachi K, Kawata T, Kobayashi S, Mizuguchi K, Kameda Y, Nishioka H, Hamada Y, Yoshida Y. [Ten-year survival and cardiac event-free rates in Japanese patients with the left anterior descending artery revascularized with internal thoracic artery or saphenous vein graft: a comparative study] Nippon Geka Gakkai Zasshi. 1996 Mar;97(3):202-9. PMID 8649330.
- ↑ Arima M, Kanoh T, Suzuki T, Kuremoto K, Tanimoto K, Oigawa T, Matsuda S. Serial Angiographic Follow-up Beyond 10 Years After Coronary Artery Bypass Grafting. Circ J. 2005 Aug;69(8):896-902. PMID 16041156. [1].
- ↑ Lopes RD, Hafley GE, Allen KB, Ferguson TB, Peterson ED, Harrington RA, Mehta RH, Gibson CM, Mack MJ, Kouchoukos NT, Califf RM, Alexander JH (2009). "Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery". The New England Journal of Medicine. 361 (3): 235–44. doi:10.1056/NEJMoa0900708. PMID 19605828. Retrieved 2010-07-12. Unknown parameter
|month=ignored (help) - ↑ Gao G et al. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery. J Am Coll Cardiol 2010;56:1639–43.
- ↑ Gao G et al. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery. J Am Coll Cardiol 2010;56:1639–43.
- ↑ Marti MC, Bouchardy B, Cox JN. Aortocoronary bypass with autogenous saphenous vein grafts: histopathological aspects. Virchows Arch Abt A Path Anat 1971; 352: 255–66.
- ↑ Garrett HE, Dennis EW, DeBakey ME. Aortocoronary bypass with saphenous vein graft. JAMA 1973; 223: 792–4.
- ↑ Zemva A, Ferluga D, Zorc M, Popovic M, Porenta OV, Radovanovic N. Amyloidosis in saphenous vein aortocoronary bypass grafts. J Cardiovasc Surg 1990; 31: 441–4.
- ↑ Salerno TA, Wasan SM, Charrette EJ. Prospective analysis of heart biopsies in coronary artery surgery. Ann Thorac Surg 1979; 28: 436–9.
- ↑ Pelosi F, Capehart J, Roberts WC. Effectiveness of cardiac transplantation for primary (AL) cardiac amyloidosis. Am J Cardiol 1997; 79: 532–5.
- ↑ Greenberg BH, Hart R, Botvinik EH, Werner JA, Brundage BH, Shames DM, et al. Thallium-201 myocardial perfusion scintigraphy to evaluate patients after coronary bypass surgery. Am J Cardiol 1978;42:167-76.
- ↑ 15.0 15.1 Olenchock SA, Karmpaliotis D, Gibson WJ, Murphy SA, Southard MC, Ciaglo L, Buros J, Mack MJ, Alexander JH, Harrington RA, Califf RM, Kouchoukos NT, Ferguson TB, Gibson CM (2008). "Impact of saphenous vein graft radiographic markers on clinical events and angiographic parameters". The Annals of Thoracic Surgery. 85 (2): 520–4. doi:10.1016/j.athoracsur.2007.10.061. PMID 18222256. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Borowski A, Vchivkov I, Ghodsizad A, Gams E (2008). "Coronary artery disease progression in patients who need repeat surgical revascularisation: the surgeon's point of view". Journal of Cardiovascular Medicine (Hagerstown, Md.). 9 (1): 85–8. doi:10.2459/JCM.0b013e328011439e. PMID 18268427. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Hamada Y, Kawachi K, Yamamoto T, Nakata T, Kashu Y, Watanabe Y, Sato M (2001). "Effect of coronary artery bypass grafting on native coronary artery stenosis. Comparison of internal thoracic artery and saphenous vein grafts". The Journal of Cardiovascular Surgery. 42 (2): 159–64. PMID 11292927. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Rupprecht HJ, Hamm C, Ischinger T, Dietz U, Reimers J, Meyer J (1996). "Angiographic follow-up results of a randomized study on angioplasty versus bypass surgery (GABI trial). GABI Study Group". European Heart Journal. 17 (8): 1192–8. PMID 8869860. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ 19.0 19.1 Guthaner DF, Robert EW, Alderman EL, Wexler L (1979). "Long-term serial angiographic studies after coronary artery bypass surgery". Circulation. 60 (2): 250–9. PMID 312703. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Manninen HI, Jaakkola P, Suhonen M, Rehnberg S, Vuorenniemi R, Matsi PJ (1998). "Angiographic predictors of graft patency and disease progression after coronary artery bypass grafting with arterial and venous grafts". The Annals of Thoracic Surgery. 66 (4): 1289–94. PMID 9800822. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Gao G et al. Aspirin plus clopidogrel therapy increases early venous graft patency after coronary artery bypass surgery. J Am Coll Cardiol 2010;56:1639–43.
- ↑ 22.0 22.1 Achenbach S, Moshage W, Ropers D, Nossen J, Bachmann K (1997). "Noninvasive, three-dimensional visualization of coronary artery bypass grafts by electron beam tomography". The American Journal of Cardiology. 79 (7): 856–61. PMID 9104894. Unknown parameter
|month=ignored (help) - ↑ 23.0 23.1 Lu B, Dai RP, Zhuang N, Budoff MJ (2002). "Noninvasive assessment of coronary artery bypass graft patency and flow characteristics by electron-beam tomography". The Journal of Invasive Cardiology. 14 (1): 19–24. PMID 11773691. Unknown parameter
|month=ignored (help) - ↑ 24.0 24.1 Stanford W, Brundage BH, MacMillan R, Chomka EV, Bateman TM, Eldredge WJ, Lipton MJ, White CW, Wilson RF, Johnson MR (1988). "Sensitivity and specificity of assessing coronary bypass graft patency with ultrafast computed tomography: results of a multicenter study". Journal of the American College of Cardiology. 12 (1): 1–7. PMID 3288675. Unknown parameter
|month=ignored (help) - ↑ Anand DV, Lim E, Lipkin D, Lahiri A (2008). "Evaluation of graft patency by computed tomographic angiography in symptom-free post-coronary artery bypass surgery patients". Journal of Nuclear Cardiology : Official Publication of the American Society of Nuclear Cardiology. 15 (2): 201–8. doi:10.1016/j.nuclcard.2007.10.007. PMID 18371591.
- ↑ 26.0 26.1 26.2 26.3 Meyer TS, Martinoff S, Hadamitzky M, Will A, Kastrati A, Schömig A, Hausleiter J (2007). "Improved noninvasive assessment of coronary artery bypass grafts with 64-slice computed tomographic angiography in an unselected patient population". Journal of the American College of Cardiology. 49 (9): 946–50. doi:10.1016/j.jacc.2006.10.066. PMID 17336717. Unknown parameter
|month=ignored (help) - ↑ Ropers D, Pohle FK, Kuettner A, Pflederer T, Anders K, Daniel WG, Bautz W, Baum U, Achenbach S (2006). "Diagnostic accuracy of noninvasive coronary angiography in patients after bypass surgery using 64-slice spiral computed tomography with 330-ms gantry rotation". Circulation. 114 (22): 2334–41, quiz 2334. doi:10.1161/CIRCULATIONAHA.106.631051. PMID 17088461. Retrieved 2010-10-31. Unknown parameter
|month=ignored (help) - ↑ Mueller J, Jeudy J, Poston R, White CS (2007). "Cardiac CT angiography after coronary bypass surgery: prevalence of incidental findings". AJR. American Journal of Roentgenology. 189 (2): 414–9. doi:10.2214/AJR.06.0736. PMID 17646469. Unknown parameter
|month=ignored (help) - ↑ Savage MP, Douglas JS, Fischman DL; et al. (1997). "Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators". N. Engl. J. Med. 337 (11): 740–7. PMID 9287229. Unknown parameter
|month=ignored (help) - ↑ Stankovic G, Colombo A, Presbitero P; et al. (2003). "Randomized evaluation of polytetrafluoroethylene-covered stent in saphenous vein grafts: the Randomized Evaluation of polytetrafluoroethylene COVERed stent in Saphenous vein grafts (RECOVERS) Trial". Circulation. 108 (1): 37–42. doi:10.1161/01.CIR.0000079106.71097.1C. PMID 12821546. Unknown parameter
|month=ignored (help) - ↑ Schächinger V, Hamm CW, Münzel T; et al. (2003). "A randomized trial of polytetrafluoroethylene-membrane-covered stents compared with conventional stents in aortocoronary saphenous vein grafts". J. Am. Coll. Cardiol. 42 (8): 1360–9. PMID 14563575. Unknown parameter
|month=ignored (help) - ↑ Salloum J, Tharpe C, Vaughan D, Zhao DX (2005). "Release and elimination of soluble vasoactive factors during percutaneous coronary intervention of saphenous vein grafts: analysis using the PercuSurge GuardWire distal protection device". J Invasive Cardiol. 17 (11): 575–9. PMID 16264199. Unknown parameter
|month=ignored (help) - ↑ Baim DS, Wahr D, George B; et al. (2002). "Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts". Circulation. 105 (11): 1285–90. PMID 11901037. Unknown parameter
|month=ignored (help) - ↑ Stone GW, Rogers C, Hermiller J; et al. (2003). "Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts". Circulation. 108 (5): 548–53. doi:10.1161/01.CIR.0000080894.51311.0A. PMID 12874191. Unknown parameter
|month=ignored (help) - ↑ Halkin A, Masud AZ, Rogers C; et al. (2006). "Six-month outcomes after percutaneous intervention for lesions in aortocoronary saphenous vein grafts using distal protection devices: results from the FIRE trial". Am. Heart J. 151 (4): 915.e1–7. doi:10.1016/j.ahj.2005.09.018. PMID 16569562. Unknown parameter
|month=ignored (help) - ↑ Mauri L, Cox D, Hermiller J; et al. (2007). "The PROXIMAL trial: proximal protection during saphenous vein graft intervention using the Proxis Embolic Protection System: a randomized, prospective, multicenter clinical trial". J. Am. Coll. Cardiol. 50 (15): 1442–9. doi:10.1016/j.jacc.2007.06.039. PMID 17919563. Unknown parameter
|month=ignored (help) - ↑ Holmes DR, Topol EJ, Califf RM; et al. (1995). "A multicenter, randomized trial of coronary angioplasty versus directional atherectomy for patients with saphenous vein bypass graft lesions. CAVEAT-II Investigators". Circulation. 91 (7): 1966–74. PMID 7895354. Unknown parameter
|month=ignored (help) - ↑ Zoghbi GJ, Goyal M, Hage F; et al. (2009). "Pretreatment with nitroprusside for microcirculatory protection in saphenous vein graft interventions". J Invasive Cardiol. 21 (2): 34–9. PMID 19182287. Unknown parameter
|month=ignored (help)
Additional Resources
- S. A. Hassantash, B. Bikdeli, S. Kalantarian, M. Sadeghian, and H. Afshar Pathophysiology of Aortocoronary Saphenous Vein Bypass Graft Disease Asian Cardiovasc Thorac Ann, August 1, 2008; 16(4): 331 - 336.
- A. Coolong, D. S. Baim, R. E. Kuntz, A. J. O'Malley, S. Marulkar, D. E. Cutlip, J. J. Popma, and L. Mauri. Saphenous Vein Graft Stenting and Major Adverse Cardiac Events: A Predictive Model Derived From a Pooled Analysis of 3958 Patients. Circulation, February 12, 2008; 117(6): 790 - 797.
- R. F. Padera Jr. and F. J. Schoen. Pathology of Cardiac Surgery Card. Surg. Adult, January 1, 2008; 3(2008): 111 - 178.
- E. Gongora and T. M. Sundt III. Myocardial Revascularization with Cardiopulmonary Bypass. Card. Surg. Adult, January 1, 2008; 3(2008): 599 - 632.
- P. Widimsky, Z. Straka, P. Stros, K. Jirasek, J. Dvorak, J. Votava, L. Lisa, T. Budesinsky, M. Kolesar, T. Vanek, et al. One-Year Coronary Bypass Graft Patency: A Randomized Comparison Between Off-Pump and On-Pump Surgery Angiographic Results of the PRAGUE-4 Trial Circulation, November 30, 2004; 110 (22): 3418 - 3423.
- M. A. Hlatky, D. B. Boothroyd, K. A. Melsop, M. M. Brooks, D. B. Mark, B. Pitt, G. S. Reeder, W. J. Rogers, T. J. Ryan, P. L. Whitlow, et al. Medical Costs and Quality of Life 10 to 12 Years After Randomization to Angioplasty or Bypass Surgery for Multivessel Coronary Artery Disease Circulation, October 5, 2004; 110 (14): 1960 - 1966.
- J. G. Lobo Filho, M. C. d. A. Leitao, and A. J. d. V. Forte Studying the lumen in composite Y internal thoracic artery-saphenous vein grafts J. Thorac. Cardiovasc. Surg., September 1, 2004; 128(3): 490 - 491.
- E. McGregor, L. Kempster, R. Wait, M. Gosling, M. J. Dunn, and J. T. Powell. F-actin Capping (CapZ) and Other Contractile Saphenous Vein Smooth Muscle Proteins Are Altered by Hemodynamic Stress: a proteomic approach Mol. Cell. Proteomics, February 1, 2004; 3(2): 115 - 124.
- M. Endo, Y. Tomizawa, and H. Nishida Bilateral Versus Unilateral Internal Mammary Revascularization in Patients with Diabetes Circulation, September 16, 2003; 108(11): 1343 - 1349.
- T. D. Rea, M. Crouthamel, M. S. Eisenberg, L. J. Becker, and A. R. Lima. Temporal Patterns in Long-Term Survival After Resuscitation From Out-of-Hospital Cardiac Arrest Circulation, September 9, 2003; 108(10): 1196 - 1201.
- M. Hilker, T. Langin, U. Hake, F.-X. Schmid, W. Kuroczynski, H.-A. Lehr, H. Oelert, and M. Buerke Gene expression profiling of human stenotic aorto-coronary bypass grafts by cDNA array analysis Eur. J. Cardiothorac. Surg., April 1, 2003; 23(4): 620 - 625.
- J. L. Sperry, C. B. Deming, C. Bian, P. L. Walinsky, D. A. Kass, F. D. Kolodgie, R. Virmani, A. Y. Kim, and J. J. Rade Wall Tension Is a Potent Negative Regulator of In Vivo Thrombomodulin Expression Circ. Res., January 10, 2003; 92(1): 41 - 47.
- F. J. Schoen and R. F. Padera Jr. Cardiac Surgical Pathology Card. Surg. Adult, January 1, 2003; 2(2003): 119 - 185.
- A. Y. Kim, P. L. Walinsky, F. D. Kolodgie, C. Bian, J. L. Sperry, C. B. Deming, E. A. Peck, J. G. Shake, G. B. Ang, R. H. Sohn, et al. Early Loss of Thrombomodulin Expression Impairs Vein Graft Thromboresistance: Implications for Vein Graft Failure Circ. Res., February 8, 2002; 90(2): 205 - 212.
- K. B. Kim, C. Lim, C. Lee, I.-H. Chae, B.-H. Oh, M.-M. Lee, and Y.-B. Park Off-pump coronary artery bypass may decrease the patency of saphenous vein grafts Ann. Thorac. Surg., September 1, 2001; 72(3): S1033 - 1037.
- Z. Yang, T. Kozai, B. van de Loo, H. Viswambharan, M. Lachat, M. I. Turina, T. Malinski, and T. F. Luscher. HMG-CoA reductase inhibition improves endothelial cell function and inhibits smooth muscle cell proliferation in human saphenous veins J. Am. Coll. Cardiol., November 1, 2000; 36(5): 1691 - 1697.
- H. Hirose, A. Amano, S. Yoshida, A. Takahashi, N. Nagano, and T. Kohmoto Coronary Artery Bypass Grafting in the Elderly Chest, May 1, 2000; 117(5): 1262 - 1270.
- D. R. Holmes Jr and P. B. Berger. Percutaneous Revascularization of Occluded Vein Grafts : Is It Still a Temptation to Be Resisted? Circulation, January 12, 1999; 99(1): 8 - 11.
- Y. K. Wong, M. Thomas, V. Tsang, P. J. Gallagher, and M. E. Ward. The prevalence of Chlamydia pneumoniae in atherosclerotic and nonatherosclerotic blood vessels of patients attending for redo and first time coronary artery bypass graft surgery. J. Am. Coll. Cardiol., January 1, 1999; 33(1): 152 - 156.
- F. D. Loop Coronary artery surgery: the end of the beginning Eur. J. Cardiothorac. Surg., December 1, 1998; 14(6): 554 - 571.
- Z. G. Zhu, H.-H. Li, and B.-R. Zhang. Expression of Endothelin-1 and Constitutional Nitric Oxide Synthase Messenger RNA in Saphenous Vein Endothelial Cells Exposed to Arterial Flow Shear Stress Ann. Thorac. Surg., November 1, 1997; 64(5): 1333 - 1338.
- A. Y. Kim, P. L. Walinsky, F. D. Kolodgie, C. Bian, J. L. Sperry, C. B. Deming, E. A. Peck, J. G. Shake, G. B. Ang, R. H. Sohn, et al. Early Loss of Thrombomodulin Expression Impairs Vein Graft Thromboresistance: Implications for Vein Graft Failure. Circ. Res., February 8, 2002; 90(2): 205 - 212.
See Also
- CABG
- Hybrid bypass
- Off-pump coronary artery bypass surgery (OPCAB)
- Minimally invasive direct coronary artery bypass surgery (MIDCAB)