Hemodynamics
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor(s)-in-Chief: Rim Halaby
Overview
- The circulatory system transports blood and helps in delivering oxygen, nutrients and chemicals to the cells of the body and in removing cell wastes.
- Hemodynamics, meaning literally "blood movement", is the study of blood flow or the circulation and it includes studying the following concepts:
- The factors influencing hemodynamics are extensive and include circulating fluid volume, respiration, vascular diameter and resistance, and blood viscosity. Each of these may in turn be influenced by physiological factors, such as diet, exercise, disease, drugs or alcohol, obesity and excess weight.
The Circulatory System
- The circulatory system is a connected series of tubes, which includes the heart, the arteries, the micro-circulation, and the veins. The “beating” of the heart generates pulsatile blood flow which is conducted into the arteries, across the micro-circulation and eventually, back via the venous system to the heart.
- The heart, vessels and lungs are all actively involved in maintaining healthy cells and organs, and all influence hemodynamics.
The Components of the Circulatory System
- The Heart
- The heart is the driver of the circulatory system generating cardiac output (CO) by rhythmically contracting and relaxing. This creates changes in regional pressures, and, combined with a complex valvular system in the heart and the veins, ensures that the blood moves around the circulatory system in one direction.
- The Arterial System
- The aorta, the main artery, leaves the left heart and proceeds to divide into smaller and smaller arteries until they become arterioles, and eventually capillaries, where oxygen transfer occurs.
- The microcirculation
- The micro-circulation, formed by the arterioles, capillaries and venules, constitutes most of the area of the vascular system and is the site of the transfer of, O2, glucose and substrates into the cells.
- The Venous System
- The venous system returns the deoxygenated blood to the right heart where it is pumped into the lungs to become oxygenated and CO2 and other gaseous wastes exchanged and expelled during breathing. Blood then returns to the left side of the heart where it begins the process again.
Cardiac Output
- Cardiac output (CO) is defined as the amount of blood pumped by the left ventricle in unit time.
- CO = Stroke Volume x Heart Rate
- The normal cardiac output is 5-6L/min and it can increase up to 5 times during exercise.
- CO is an indicator of the left ventricular function.
- Cardiac index (CI) is the output of the heart per minute per body surface area.
- CI = CO / Body Surface Area
- The normal cardiac index is 3.2 L/min/m2.[1]
- Stroke volume (SV) is the amount of blood pumped by the left ventricle in a single cardiac cycle.
Factors affecting the cardiac output
- CO = Stroke volume x Heart rate
- The cardiac output changes when there is any change in the stroke volume, the heart rate or both.
Factors affecting the heart rate:
- The electrical activity of the heart is generated spontaneously in the sinoatrial node. However, the autonomic nervous system affects the speed at which the electrical activity of the heart is generated and hence affects the heart rate.
- The sympathetic nervous system increases the heart rate (positive chronotropy).
- The parasympathetic nervous system decreases the heart rate (negative chronotropy).[2]
Factors affecting the stroke volume
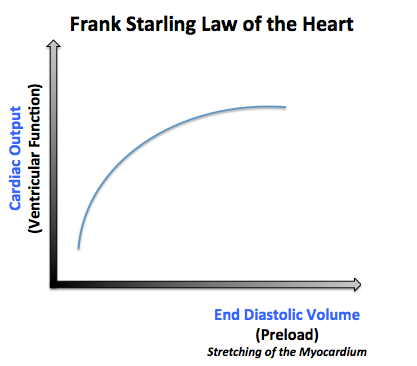
- 1- Preload:
- 2- Afterload:
- The afterload is the pressure corresponding to the mean arterial pressure that the heart needs to overcome when pumping blood.
- When the afterload increases, it makes it harder for the heart to pump the blood, and thus the volume remaining in the ventricles after ventricular contraction (end systolic volume) will increase and the stroke volume will be low.
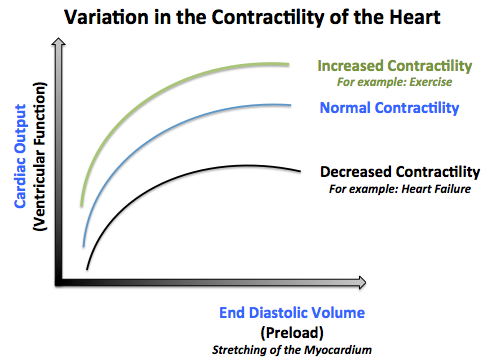
- 3- The contractility of the heart:
- The contractility of the heart is defined as the intrinsic force with which the heart contracts.
- Factors that increase the contractility of the heart (positive ionotropy) are: catecholamines, xanthines (caffeine), medications (Digitalis).
- Factors that decrease the contractlity of the heart (negative ionotropy) are: hypercapnea, hypoxia, acidosis, medications (quinidine, procainamide, barbiturates), heart failure.[3]
Clinical Correlation
- Diseases of the cardiovascular system are often associated with changes in CO.
- Cardiomyopathy and heart failure cause a reduction in cardiac output.
- Hypertension, infection and sepsis are known to increase cardiac output.
Blood Flow
- Blood flows from one site to another proportionally to the difference of pressures between these sites and inversely proportionally to the resistance of conduits (which are the vessels) in which blood is circulating.
- This is the same concept of Ohm's law and it can be illustrated in the following formula:
- Flow = Difference in Pressure/Resistance
- Difference in pressure= Pressure at the first site - Pressure at the second site
- Resistance= 8 x viscosity of blood x length of vessels/ Pi x radius of vessels^4
- Circulation is influenced by the resistance of the vascular bed against which the heart is pumping.
- Pulmonary Vascular Resistance (PVR) is created by the pulmonary bed on the right side of the heart.
- Systemic Vascular Resistance (SVR) is created by the systemic vascular bed on the left side of the heart.
- The vessels actively change diameter under the influence of physiology or therapy:
- Vasoconstrictors decrease vessel diameter and increase resistance and hence decrease the blood flow.
- Vasodilators increase vessel diameter and decrease resistance and hence increase the blood flow.
Blood Pressure
- Blood pressure (BP) is the pressure exerted by the circulating blood on the walls of the blood vessels.
- The blood pressure can be clinically measured using a plethysmograph or cuff connected to a pressure sensor (mercury or aneroid manometer).
- Blood pressure varies during each cardiac cycle:
- Systolic blood pressure:
- It is the maximal blood pressure during each cycle.
- It is normally around 120 mmHg.
- It corresponds to the pressure exerted by the circulating blood on the walls of the vessels as the left ventricle is contracting and pushing blood into the aorta.
- Diastolic blood pressure:
- It is the minimal blood pressure during each cycle.
- It is normally around 70 mmHg.
- It corresponds to the pressure exerted by the circulating blood on the walls of the vessels as the left ventricle is relaxing.
- Systolic blood pressure:
- The average pressure throughout the cardiac cycle is referred to as mean arterial pressure (MAP).
- MAP = diastolic BP + (systolic BP - diastolic BP)/3= (systolic BP + 2x diastolic pressure)/3 [4]
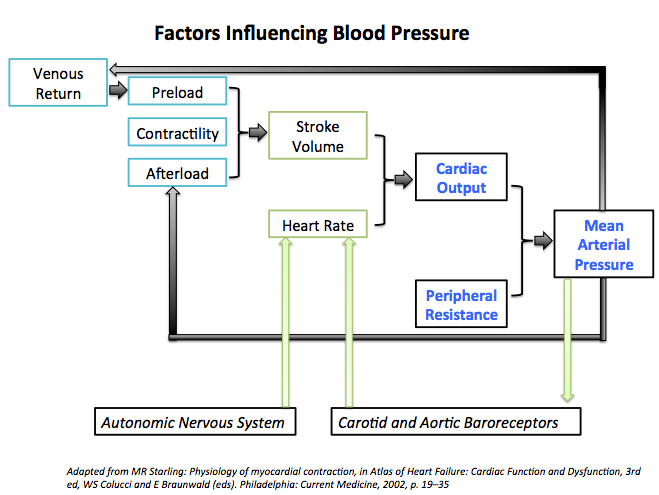
Factors Influencing Blood Pressure
- Blood Pressure = Cardiac Output x Peripheral vascular resistance
- Any factor that affects the cardiac output, peripheral resistance or both will alter the blood pressure.
Regulation of Blood Pressure
- The regulation of the blood pressure is complex as it involves the interaction between the cardiovascular, renal and neurological systems among others.
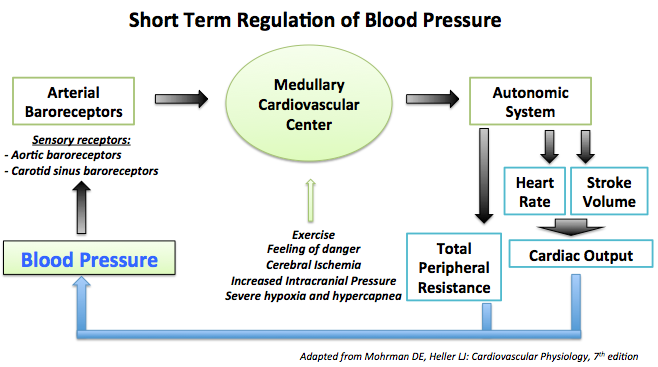
1- Short term regulation of the blood pressure:
- Arterial baroreceptor reflex is the most important factor in the short term regulation of the blood pressure.
- Other cardiovascular reflexes:
2- Long term regulation of the blood pressure:
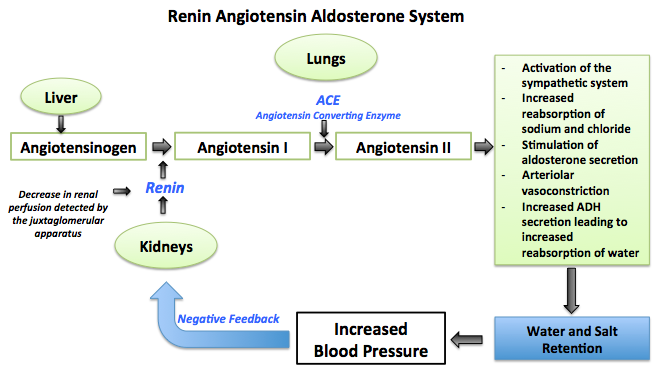
- Fluid balance by the renin-angiotensin system(RAAS) is the main contributor of the long term regulation of the blood pressure.[6]
See also
External links
Sources
1. Berne RM, Levy MN. Cardiovascular physiology. 7th Ed Mosby 1997
2. Rowell LB. Human Cardiovascular Control. Oxford University press 1993
3. Braunwald E (Editor). Heart Disease: A Textbook of Cardiovascular Medicine. 5th Ed. W.B.Saunders 1997
4. Siderman S, Beyar R, Kleber AG. Cardiac Electrophysiology, Circulation and Transport. Kluwer Academic Publishers 1991
6. Otto CM, Stoddard M, Waggoner A, Zoghbi WA. Recommendations for Quantification of Doppler Echocardiography: A Report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr 2002;15:167-184
References
- ↑ Barrett KE, Barman SM, Boitano S, Brooks HL. Chapter 30. The Heart as a Pump. In: Barrett KE, Barman SM, Boitano S, Brooks HL, eds. Ganong's Review of Medical Physiology. 24th ed. New York: McGraw-Hill; 2012.
- ↑ Barrett KE, Barman SM, Boitano S, Brooks HL. Chapter 30. The Heart as a Pump. In: Barrett KE, Barman SM, Boitano S, Brooks HL, eds. Ganong's Review of Medical Physiology. 24th ed. New York: McGraw-Hill; 2012.
- ↑ Barrett KE, Barman SM, Boitano S, Brooks HL. Chapter 30. The Heart as a Pump. In: Barrett KE, Barman SM, Boitano S, Brooks HL, eds. Ganong's Review of Medical Physiology. 24th ed. New York: McGraw-Hill; 2012.
- ↑ Mohrman DE, Heller LJ. Chapter 9. Regulation of Arterial Pressure. In: Mohrman DE, Heller LJ, eds. Cardiovascular Physiology. 7th ed. New York: McGraw-Hill; 2010.
- ↑ Mohrman DE, Heller LJ. Chapter 9. Regulation of Arterial Pressure. In: Mohrman DE, Heller LJ, eds. Cardiovascular Physiology. 7th ed. New York: McGraw-Hill; 2010.
- ↑ Mohrman DE, Heller LJ. Chapter 9. Regulation of Arterial Pressure. In: Mohrman DE, Heller LJ, eds. Cardiovascular Physiology. 7th ed. New York: McGraw-Hill; 2010.