Saphenous vein graft: Difference between revisions
| Line 93: | Line 93: | ||
===Saphenous Vein Graft Degeneration=== | ===Saphenous Vein Graft Degeneration=== | ||
===Saphenous Vein Graft Occlusion=== | ===Saphenous Vein Graft Failure and Occlusion=== | ||
Saphenous vein graft occlusion is defined as a complete, 100% occlusion of a saphenous vein graft. Saphenous vein | |||
The rate of failure or occlusion of saphenous vein grafts is calculated on a per graft basis and a per patient basis. The per patient basis is higher, becuase only one vein graft out of several must fail for the patient to be characterized as a failure. | |||
===Amyloidosis of Saphenous Coronary Bypass Grafts <small> <ref>Marti MC, Bouchardy B, Cox JN. Aortocoronary bypass with autogenous saphenous vein grafts: histopathological aspects. Virchows Arch Abt A Path Anat 1971; 352: 255–66.</ref> <ref>Garrett HE, Dennis EW, DeBakey ME. Aortocoronary bypass with saphenous vein graft. JAMA 1973; 223: 792–4.</ref> <ref>Zemva A, Ferluga D, Zorc M, Popovic M, Porenta OV, Radovanovic N. Amyloidosis in saphenous vein aortocoronary bypass grafts. J Cardiovasc Surg 1990; 31: 441–4.</ref> <ref>Salerno TA, Wasan SM, Charrette EJ. Prospective analysis of heart biopsies in coronary artery surgery. Ann Thorac Surg 1979; 28: 436–9.</ref> <ref>Pelosi F, Capehart J, Roberts WC. Effectiveness of cardiac transplantation for primary (AL) cardiac amyloidosis. Am J Cardiol 1997; 79: 532–5.</ref> </small>=== | ===Amyloidosis of Saphenous Coronary Bypass Grafts <small> <ref>Marti MC, Bouchardy B, Cox JN. Aortocoronary bypass with autogenous saphenous vein grafts: histopathological aspects. Virchows Arch Abt A Path Anat 1971; 352: 255–66.</ref> <ref>Garrett HE, Dennis EW, DeBakey ME. Aortocoronary bypass with saphenous vein graft. JAMA 1973; 223: 792–4.</ref> <ref>Zemva A, Ferluga D, Zorc M, Popovic M, Porenta OV, Radovanovic N. Amyloidosis in saphenous vein aortocoronary bypass grafts. J Cardiovasc Surg 1990; 31: 441–4.</ref> <ref>Salerno TA, Wasan SM, Charrette EJ. Prospective analysis of heart biopsies in coronary artery surgery. Ann Thorac Surg 1979; 28: 436–9.</ref> <ref>Pelosi F, Capehart J, Roberts WC. Effectiveness of cardiac transplantation for primary (AL) cardiac amyloidosis. Am J Cardiol 1997; 79: 532–5.</ref> </small>=== | ||
Revision as of 16:36, 12 July 2010
| Saphenous vein graft | |
 | |
|---|---|
| Saphenous vein grafts for coronary arteries |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [3]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Since Rene Favaloro first described it in 1967, coronary artery revascularization with saphenous veins (saphenous vein grafts or SVGs) has become a surgical standard for treatment of coronary artery disease. When a native coronary artery is obstructed, the sutured graft provides a connection between the aorta and the coronary artery beyond the area of obstruction. The procedure is repeated on all the coronary artery segments that are significantly diseased.
The vein is often removed by cardiac surgeons and used for autotransplantation in coronary artery bypass operations, when arterial grafts are not available or many grafts are required, such as in a triple bypass or quadruple bypass.
The great saphenous vein is the conduit of choice for vascular surgeons,[1] [2] when available, for doing peripheral arterial bypass operations because it has superior long-term patency compared to synthetic grafts (PTFE, PETE (Dacron)), human umbilical vein grafts or biosynthetic grafts [Omniflow]. Often, it is used in situ (in place), after tying off smaller tributaries and stripping the valves with a device called LeMaitre's valvulotome.
The saphenous nerve is a branch of the femoral nerve that runs with the great saphenous vein and is often damaged in surgeries that make use of the similarly named vein.
Normal Anatomy
The great saphenous vein (GSV) originates from where the dorsal vein of the first digit (the large toe) merges with the dorsal venous arch of the foot.
After passing anterior to the medial malleolus (where it often can be visualized and palpated), it runs up the medial side of the leg. At the knee, it runs over the posterior border of the medial epicondyle of the femur bone.
The great saphenous vein then courses laterally to lie on the anterior surface of the thigh before entering an opening in the fascia lata called the saphenous opening. It joins with the femoral vein in the region of the femoral triangle at the saphenofemoral junction.
The small saphenous vein (also lesser saphenous vein) is originated where the dorsal vein from the fifth digit (smallest toe) merges with the dorsal venous arch of the foot, which attaches to the great saphenous vein. It is considered a superficial vein and is subcutaneous (just under the skin). From its origin, it courses around the lateral aspect of the foot (inferior and posterior to the lateral malleolus) and runs along the posterior aspect of the leg (with the sural nerve), passes between the heads of the gastrocnemius muscle, and drains into the popliteal vein, approximately at or above the level of the knee joint.
-
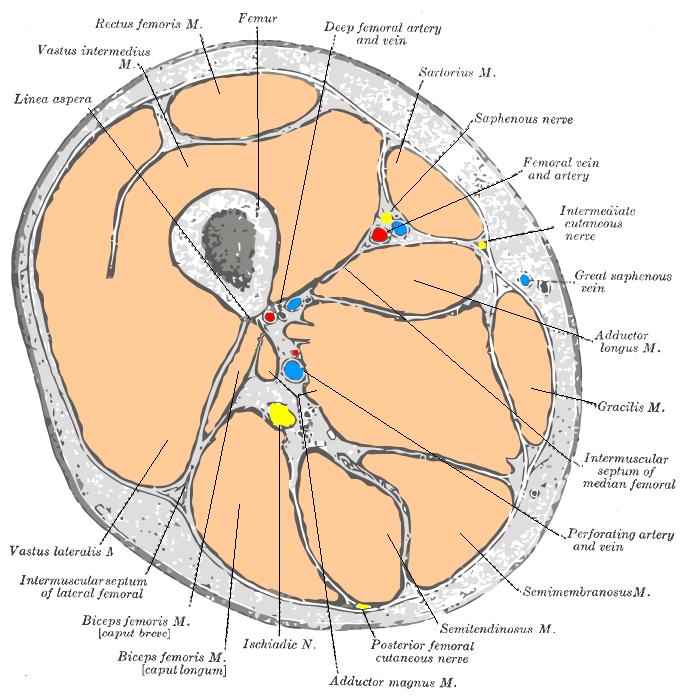
Cross-section through the middle of the thigh.
-
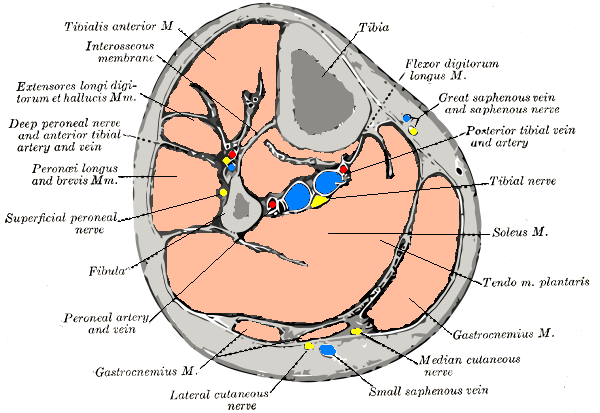
Cross-section through middle of leg.
-
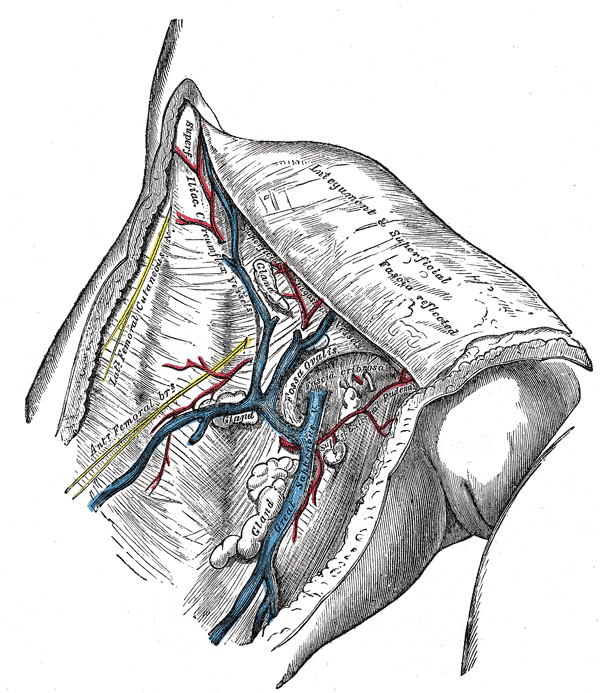
The great saphenous vein and landmarks along its course
-
The great saphenous vein and its tributaries at the fossa ovalis in the groin.
-
Small saphenous vein and its tributaries.
Preparation (Saphenous vein harvesting)
Saphenous Vein Stripping
Minimal Invasive Technique
Side Effects of Saphenous Vein Stripping
- Saphenous nerve injury
- Infection at incision sites or sepsis.
- Deep vein thrombosis (DVT)
- Keloid scarring
- Chronic pain at incision sites
Graft Patency
Grafts can become diseased and may occlude in the months to years after bypass surgery is performed. Patency is a term used to describe the chance that a graft remain open. A graft is considered patent if there is flow through the graft without any significant (>70% diameter) stenosis in the graft.
Graft patency is dependent on a number of factors, including the type of graft used (internal thoracic artery, radial artery, or great saphenous vein), the size or the coronary artery that the graft is anastomosed with, and, of course, the skill of the surgeon(s) performing the procedure. Arterial grafts (e.g. LITA, radial) are far more sensitive to rough handling than the saphenous veins and may go into spasm if handled improperly.
Generally the best patency rates are achieved with the in-situ (the proximal end is left connected to the subclavian artery) left internal thoracic artery with the distal end being anastomosed with the coronary artery (typically the left anterior descending artery or a diagonal branch artery). Lesser patency rates can be expected with radial artery grafts and "free" internal thoracic artery grafts (where the proximal end of the thoracic artery is excised from its origin from the subclavian artery and re-anastomosed with the ascending aorta). Saphenous vein grafts have worse patency rates, but are more available, as the patients can have multiple segments of the saphenous vein used to bypass different arteries.
Veins that are used either have their valves removed or are turned around so that the valves in them do not occlude blood flow in the graft.
LITA grafts are longer-lasting than vein grafts, both because the artery is more robust than a vein and because, being already connected to the arterial tree, the LITA need only be grafted at one end. The LITA is usually grafted to the left anterior descending coronary artery (LAD) because of its superior long-term patency when compared to saphenous vein grafts.[3][4]
Saphenous Vein Graft Diseases
Venospastic Phenomena of Saphenous Vein Bypass Grafts
Saphenous Vein Graft Aneurysms
It is also known as SVGA, aortocoronary saphenous vein graft aneurysms, saphenous vein graft aneurysm disease and saphenous vein graft aneurysmal dilatation.
Causes of Saphenous Vein Graft Aneurysms
- Atherosclerosis
- Hypertension
- Mycotic
- Postoperative mediastinitis
- Previous aneurysms
- Torn sutures
Saphenous Vein Graft Degeneration
Saphenous Vein Graft Failure and Occlusion
Saphenous vein graft occlusion is defined as a complete, 100% occlusion of a saphenous vein graft. Saphenous vein The rate of failure or occlusion of saphenous vein grafts is calculated on a per graft basis and a per patient basis. The per patient basis is higher, becuase only one vein graft out of several must fail for the patient to be characterized as a failure.
Amyloidosis of Saphenous Coronary Bypass Grafts [5] [6] [7] [8] [9]
Rupture of the Saphenous Vein Coronary Artery Bypass Grafts
- Aspergillus species necrotizing vasculitis
Diagnostic & Evaluation Findings
Chest X-Ray
-
Median sternotomy wires and CABG clips
-
Lateral graphy: Median sternotomy wires and CABG clips
Coronary Angiography
CT Angiography
MR Angiography
Postmortem Angiography
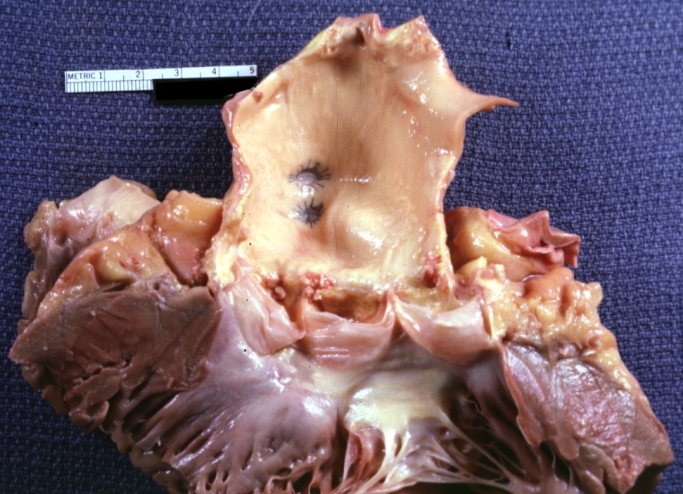
Pathological Findings
-
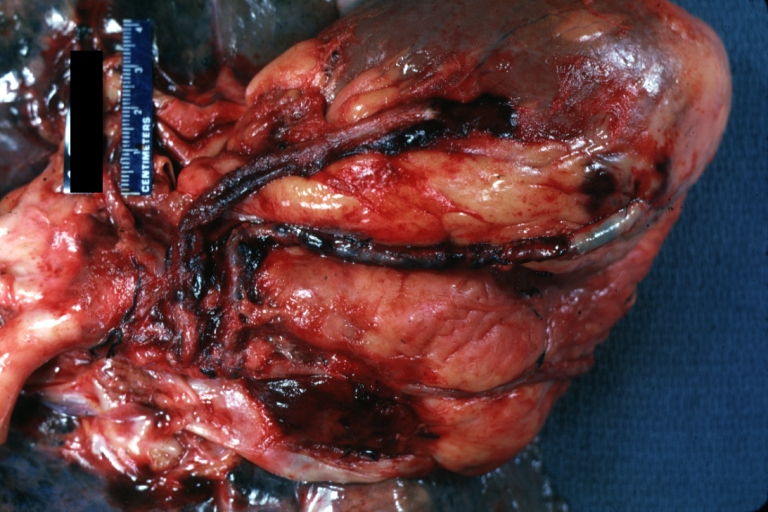
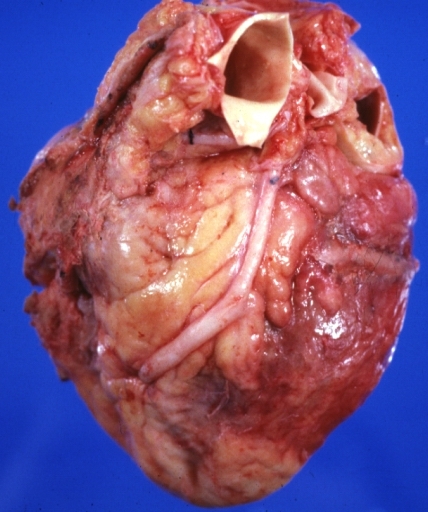
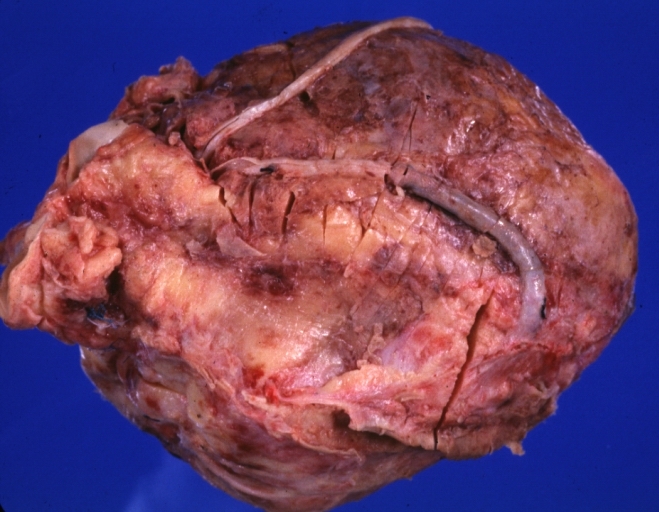
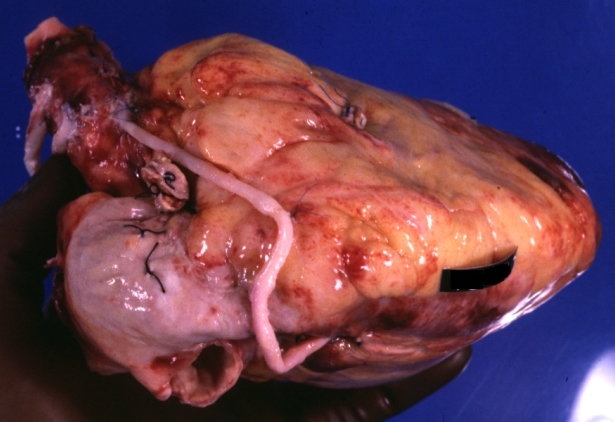
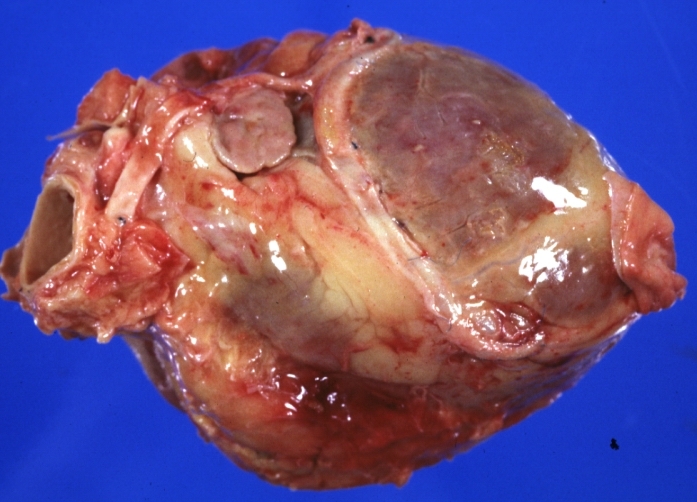
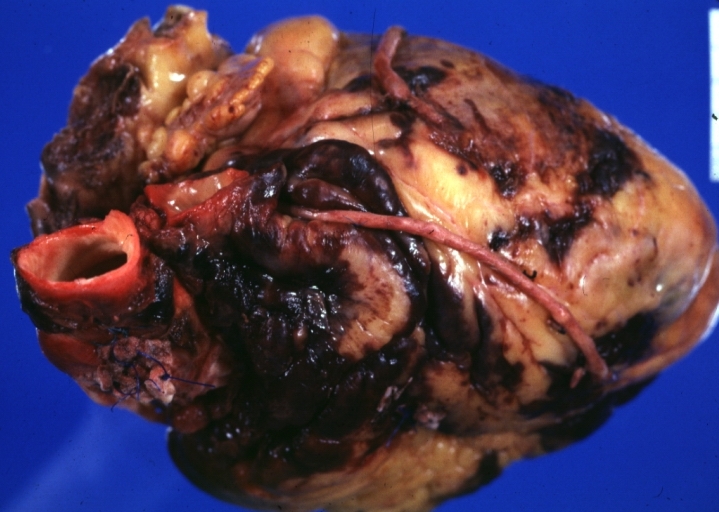
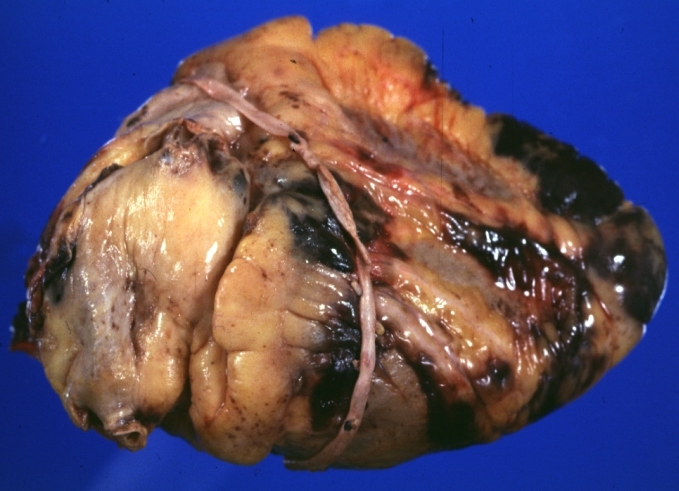
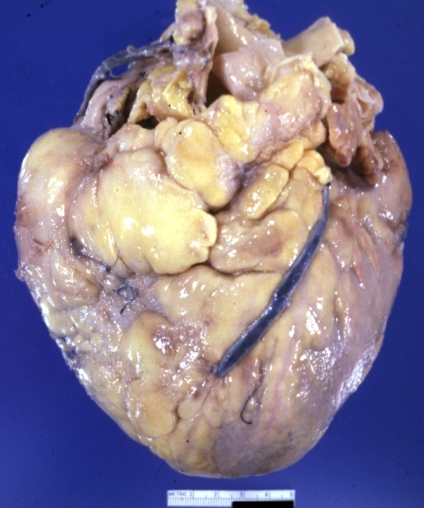
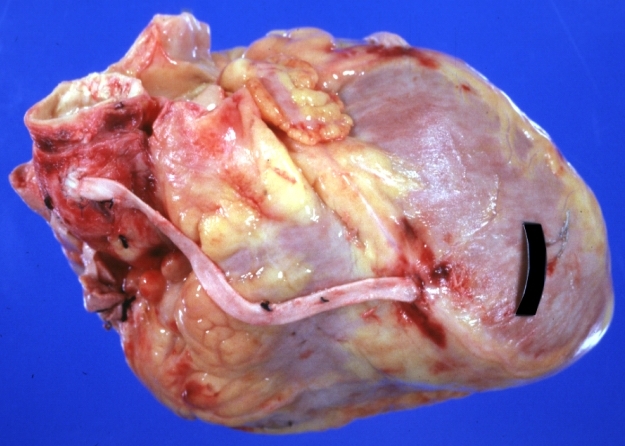
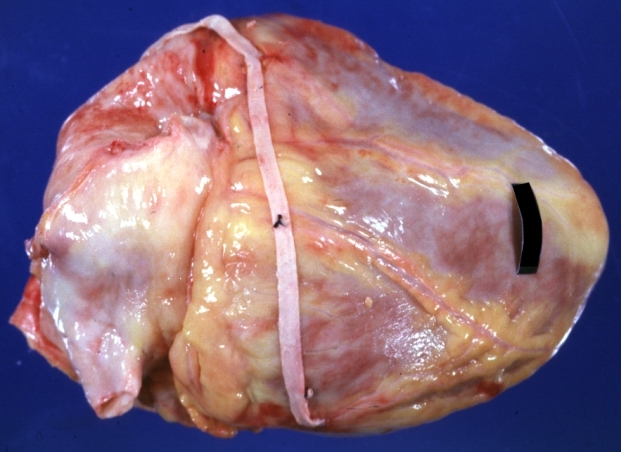
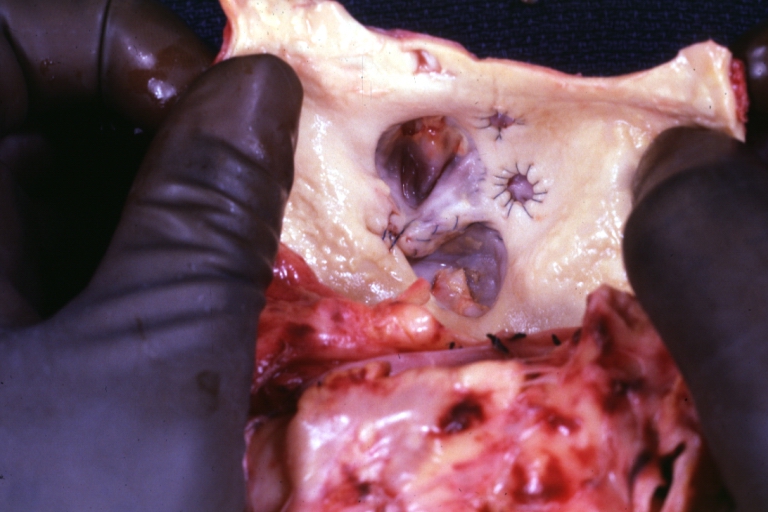
Saphenous vein coronary bypass graft: Gross, natural color, external view of heart with thrombosed veins
-
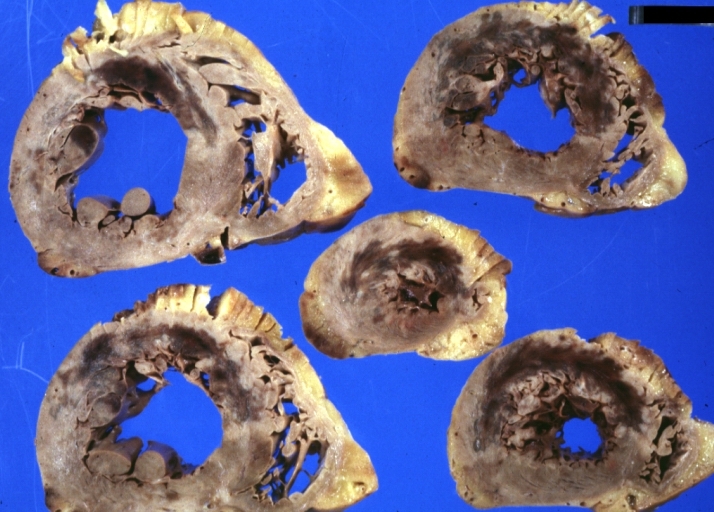
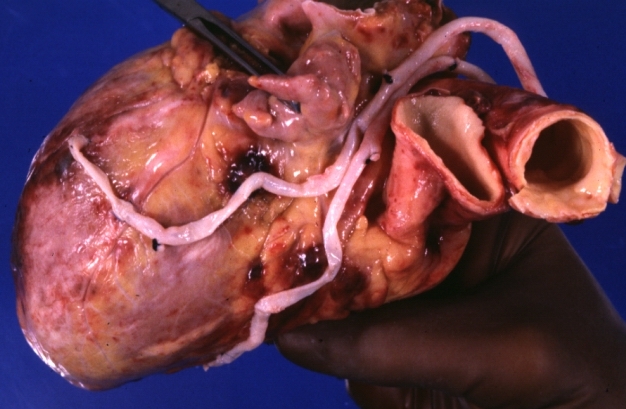
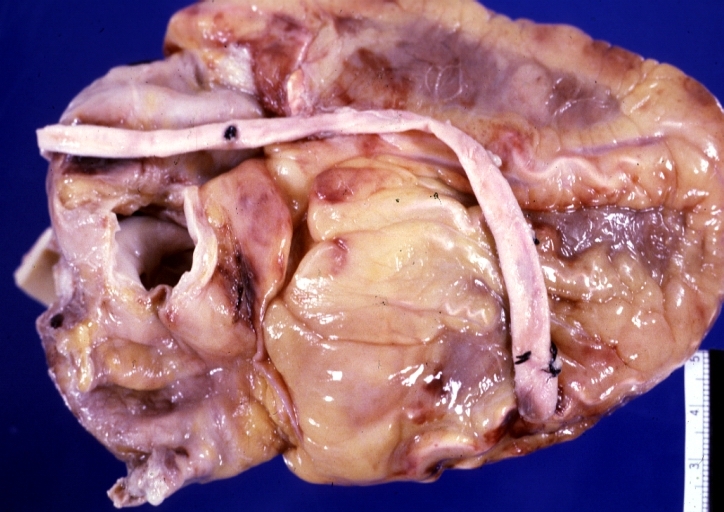
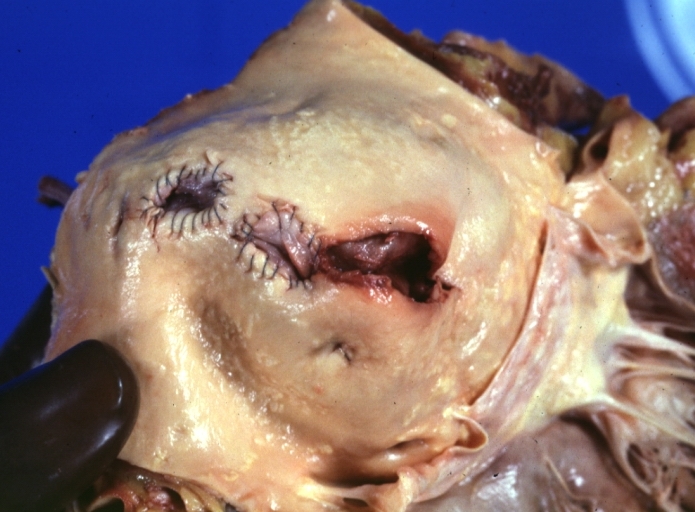
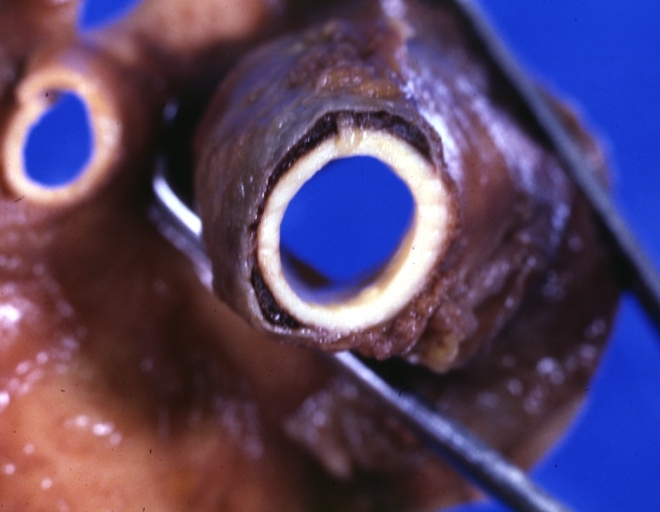
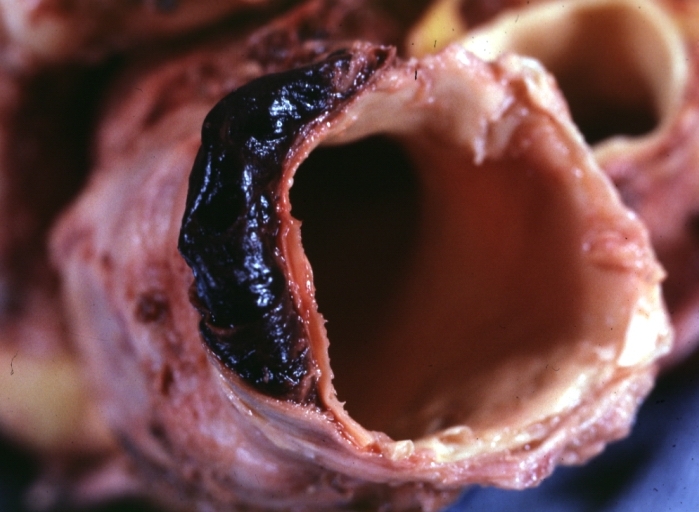
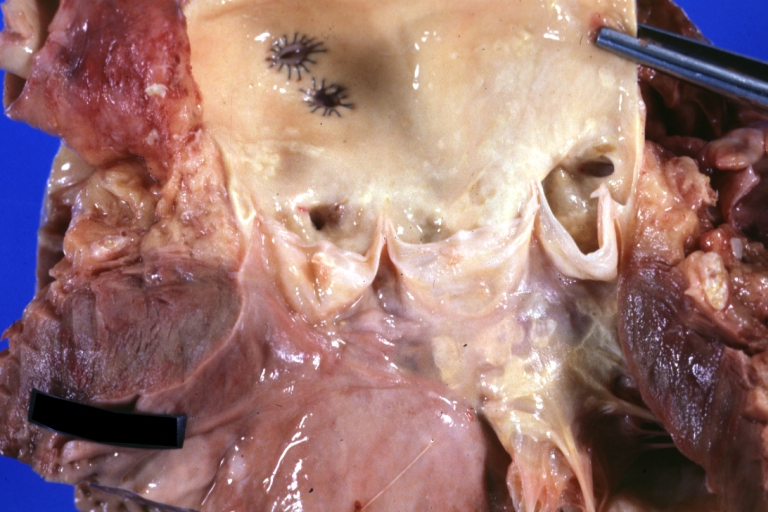
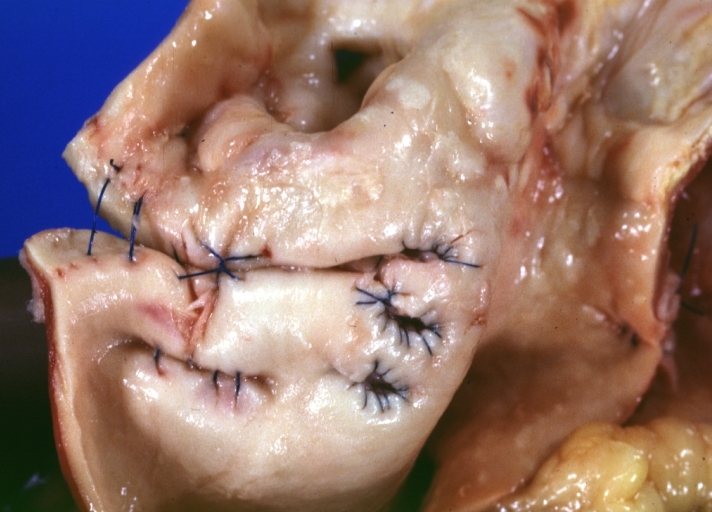
Saphenous vein coronary bypass graft: Thrombosis, Acute: Gross, fixed tissue but well shown cross sections of bypass graft and anastomotic site with thrombosis. 61 yo male, with and acute infarct treated with streptokinase and two days later had bypass. Died 5 days post op. Two veins are thrombosed
-
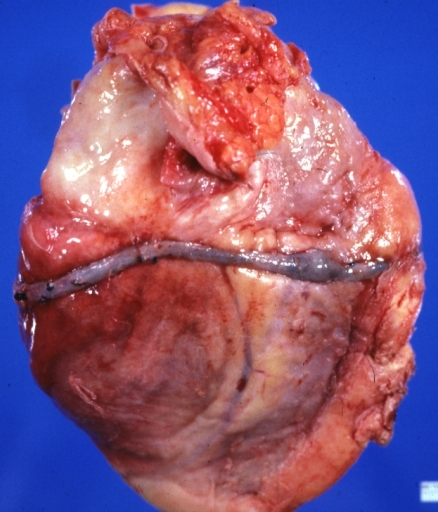
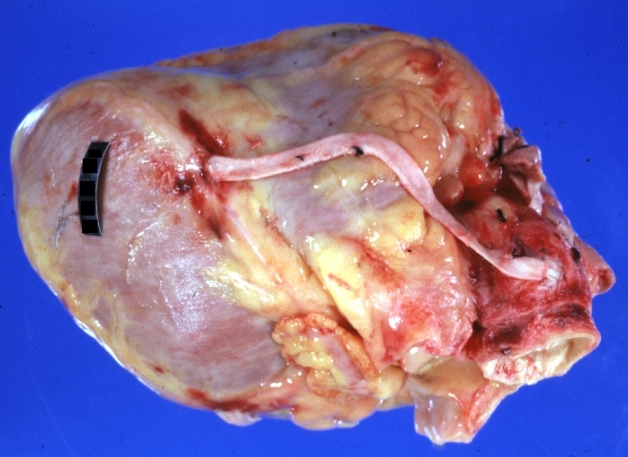
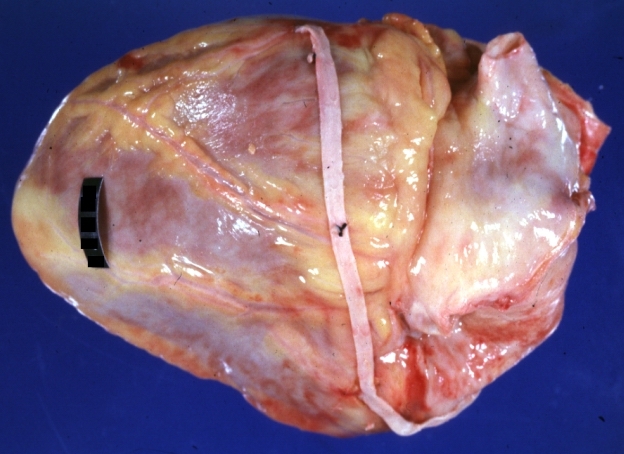
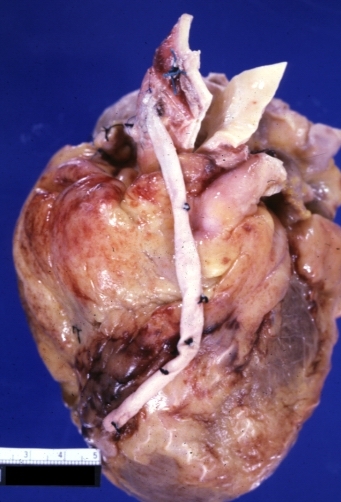
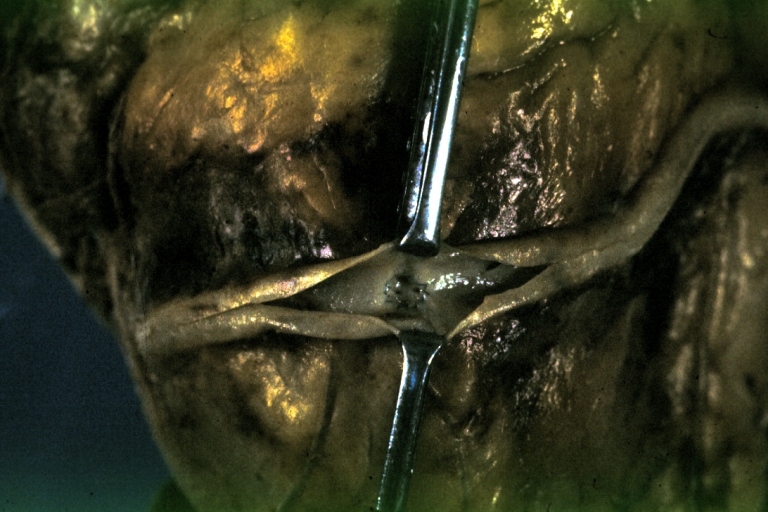
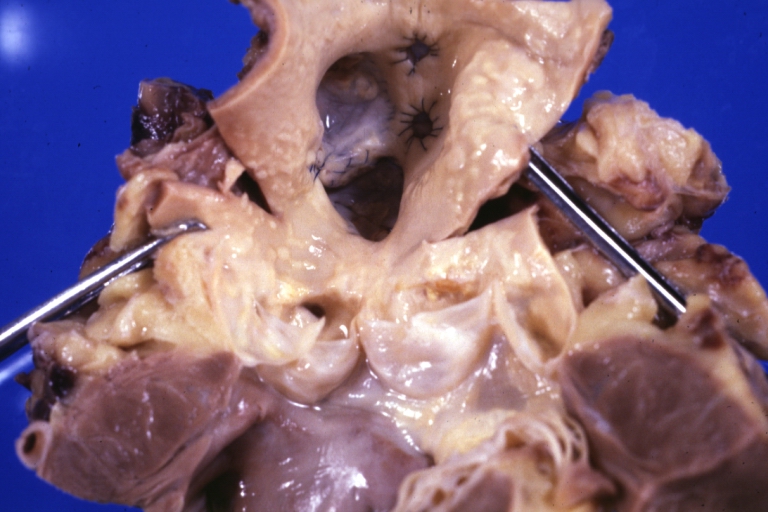
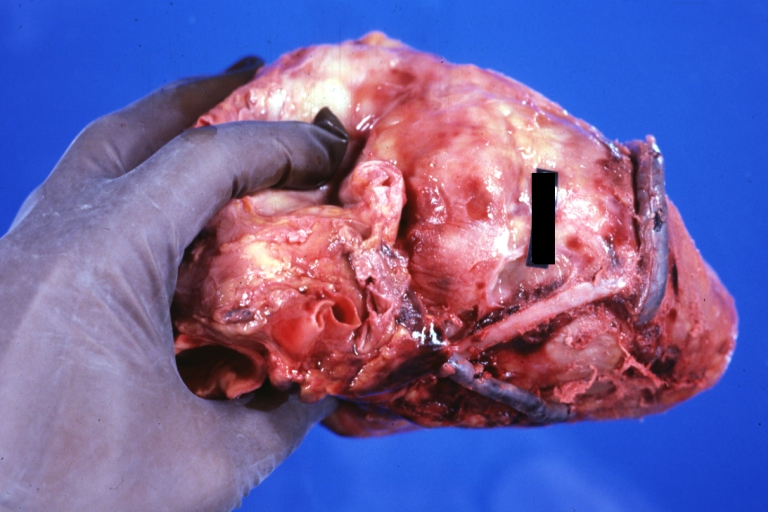
Myocardial Infarct Acute Reflow Type: Gross, fixed tissue but good color. A very enlarged heart with moderate LV dilation and high anterior wall hemorrhagic infarct. Initially treated with streptokinase and two days later had saphenous vein grafts. Both grafts are thrombosed. He died after 5 days
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Treatment
Thrombolysis
PCI
Plain Old Balloon Angioplasty (POBA)
Bare Metal Stents
Drug Eluting Stents
Excimer Laser Coronary Angioplasty (ELCA) of Saphenous Vein Grafts
At the end of 80's [10], ELCA was introduced and thought to be particularly suitable for saphenous vein grafts that were otherwise difficult to treat with balloon angioplasty alone.[11]
Cardiac Surgery (Re-do)
Number of bypasses
The terms single bypass, double bypass, triple bypass, quadruple bypass and quintuple bypass refer to the number of coronary arteries bypassed in the procedure.
In other words, a double bypass means two coronary arteries are bypassed (e.g. the left anterior descending (LAD) coronary artery and right coronary artery (RCA)); a triple bypass means three vessels are bypassed (e.g. LAD, RCA, left circumflex artery (LCX)); a quadruple bypass means four vessels are bypassed (e.g. LAD, RCA, LCX, first diagonal artery of the LAD) while quintuple means five. Less commonly more than four coronary arteries may be bypassed.
A greater number of bypasses does not imply a person is "sicker," nor does a lesser number imply a person is "healthier."[12] A person with a large amount of coronary artery disease (CAD) may receive fewer bypass grafts owing to the lack of suitable "target" vessels.
A coronary artery may be unsuitable for bypass grafting if it is small (< 1 mm or < 1.5 mm depending on surgeon preference), heavily calcified (meaning the artery does not have a section free of CAD) or intramyocardial (the coronary artery is located within the heart muscle rather than on the surface of the heart). Similarly, a person with a single stenosis ("narrowing") of the left main coronary artery requires only two bypasses (to the LAD and the LCX). However, a left main lesion places a person at the highest risk for death from a cardiac cause.
The surgeon reviews the coronary angiogram prior to surgery and identifies the lesions (or "blockages") in the coronary arteries and will estimate the number of bypass grafts prior to surgery, but the final decision is made in the operating room upon examination of the heart.
Videos
Saphenous Vein Harvesting
<youtube v=VbdE6JWdY1s/>
<youtube v=QthyR0bTHzc/>
<youtube v=sV-qE2SIkJU/>
Animation: Saphenous Vein Grafts Use in CABG
<youtube v=3Nf6Q2skGOM/>
Clinical Trials
- Radial Artery Versus Saphenous Vein Grafts in Coronary Artery Bypass Surgery
- The RETRIEVE Study: Use of the FiberNet Embolic Protection System in Saphenous Vein Grafts
- The SOS (Stenting Of Saphenous Vein Grafts) Trial
- Symbiot III: A Prospective Randomized Trial Evaluating the Symbiot Covered Stent System in Saphenous Vein Grafts
- Comparison of Safety and Efficacy of Two Different Drug Eluting Stents Implanted Into Saphenous Vein Grafts
- Evaluating the Role of Thrombin in Saphenous Vein Graft Failure After Heart Bypass Surgery
- Acupuncture and Post-Surgical Wound Healing
- RRISC Study: Reduction of Restenosis In Saphenous Vein Grafts With Cypher Sirolimus-Eluting Stent.
- Treatment of Moderate Vein Graft Lesions With Paclitaxel Drug Eluting Stents: The VELETI Trial
- Trial of Clopidogrel After Surgery for Coronary Artery Disease (CASCADE Trial)
- Multicentre Radial Artery Patency Study: 5 Year Results
- Study to Test the Efficacy and Safety of Drug Eluting vs. Bare-Metal Stents for Saphenous Vein Graft Interventions (BASKETSAVAGE)
- Vein-Coronary Atherosclerosis And Rosiglitazone After Bypass Surgery: The VICTORY Trial
- Copenhagen Arterial Revascularization Randomized Patency and Outcome Trial (CARRPO)
- The SOS (Stenting Of Saphenous Vein Grafts) Trial
- The eSVS (TM) Mesh External Saphenous Vein Support Trial
References
- ↑ Muhs BE, Gagne P, Sheehan P. Peripheral arterial disease: clinical assessment and indications for revascularization in the patient with diabetes. Curr Diab Rep. 2005 Feb;5(1):24-9. PMID 15663913.
- ↑ Mamode N, Scott RN. Graft type for femoro-popliteal bypass surgery. Cochrane Database Syst Rev. 2000;(2):CD001487. PMID 10796649.
- ↑ Kitamura S, Kawachi K, Kawata T, Kobayashi S, Mizuguchi K, Kameda Y, Nishioka H, Hamada Y, Yoshida Y. [Ten-year survival and cardiac event-free rates in Japanese patients with the left anterior descending artery revascularized with internal thoracic artery or saphenous vein graft: a comparative study] Nippon Geka Gakkai Zasshi. 1996 Mar;97(3):202-9. PMID 8649330.
- ↑ Arima M, Kanoh T, Suzuki T, Kuremoto K, Tanimoto K, Oigawa T, Matsuda S. Serial Angiographic Follow-up Beyond 10 Years After Coronary Artery Bypass Grafting. Circ J. 2005 Aug;69(8):896-902. PMID 16041156. [1].
- ↑ Marti MC, Bouchardy B, Cox JN. Aortocoronary bypass with autogenous saphenous vein grafts: histopathological aspects. Virchows Arch Abt A Path Anat 1971; 352: 255–66.
- ↑ Garrett HE, Dennis EW, DeBakey ME. Aortocoronary bypass with saphenous vein graft. JAMA 1973; 223: 792–4.
- ↑ Zemva A, Ferluga D, Zorc M, Popovic M, Porenta OV, Radovanovic N. Amyloidosis in saphenous vein aortocoronary bypass grafts. J Cardiovasc Surg 1990; 31: 441–4.
- ↑ Salerno TA, Wasan SM, Charrette EJ. Prospective analysis of heart biopsies in coronary artery surgery. Ann Thorac Surg 1979; 28: 436–9.
- ↑ Pelosi F, Capehart J, Roberts WC. Effectiveness of cardiac transplantation for primary (AL) cardiac amyloidosis. Am J Cardiol 1997; 79: 532–5.
- ↑ Litvack F, Grundfest WS, Goldenberg T, et al. Percutaneous excimer laser angioplasty of aortocoronary saphenous vein grafts. J Am CoIlCardiol 1989; 14:803-8.
- ↑ Bittl JA, Sanborn TA, Tcheng JE, et al. Clinical success, complications and restenosis rates with excimer laser coronary angioplasty. Am J Cardiol 1992; 70: 1533-9.
- ↑ Ohki S, Kaneko T, Satoh Y; et al. (2002). "[Coronary artery bypass grafting in octogenarian]". Kyobu geka. The Japanese journal of thoracic surgery (in Japanese). 55 (10): 829–33, discussion 833–6. PMID 12233100.
Additional Resources
- S. A. Hassantash, B. Bikdeli, S. Kalantarian, M. Sadeghian, and H. Afshar Pathophysiology of Aortocoronary Saphenous Vein Bypass Graft Disease Asian Cardiovasc Thorac Ann, August 1, 2008; 16(4): 331 - 336.
- A. Coolong, D. S. Baim, R. E. Kuntz, A. J. O'Malley, S. Marulkar, D. E. Cutlip, J. J. Popma, and L. Mauri. Saphenous Vein Graft Stenting and Major Adverse Cardiac Events: A Predictive Model Derived From a Pooled Analysis of 3958 Patients. Circulation, February 12, 2008; 117(6): 790 - 797.
- R. F. Padera Jr. and F. J. Schoen. Pathology of Cardiac Surgery Card. Surg. Adult, January 1, 2008; 3(2008): 111 - 178.
- E. Gongora and T. M. Sundt III. Myocardial Revascularization with Cardiopulmonary Bypass. Card. Surg. Adult, January 1, 2008; 3(2008): 599 - 632.
- P. Widimsky, Z. Straka, P. Stros, K. Jirasek, J. Dvorak, J. Votava, L. Lisa, T. Budesinsky, M. Kolesar, T. Vanek, et al. One-Year Coronary Bypass Graft Patency: A Randomized Comparison Between Off-Pump and On-Pump Surgery Angiographic Results of the PRAGUE-4 Trial Circulation, November 30, 2004; 110 (22): 3418 - 3423.
- M. A. Hlatky, D. B. Boothroyd, K. A. Melsop, M. M. Brooks, D. B. Mark, B. Pitt, G. S. Reeder, W. J. Rogers, T. J. Ryan, P. L. Whitlow, et al. Medical Costs and Quality of Life 10 to 12 Years After Randomization to Angioplasty or Bypass Surgery for Multivessel Coronary Artery Disease Circulation, October 5, 2004; 110 (14): 1960 - 1966.
- J. G. Lobo Filho, M. C. d. A. Leitao, and A. J. d. V. Forte Studying the lumen in composite Y internal thoracic artery-saphenous vein grafts J. Thorac. Cardiovasc. Surg., September 1, 2004; 128(3): 490 - 491.
- E. McGregor, L. Kempster, R. Wait, M. Gosling, M. J. Dunn, and J. T. Powell. F-actin Capping (CapZ) and Other Contractile Saphenous Vein Smooth Muscle Proteins Are Altered by Hemodynamic Stress: a proteomic approach Mol. Cell. Proteomics, February 1, 2004; 3(2): 115 - 124.
- M. Endo, Y. Tomizawa, and H. Nishida Bilateral Versus Unilateral Internal Mammary Revascularization in Patients with Diabetes Circulation, September 16, 2003; 108(11): 1343 - 1349.
- T. D. Rea, M. Crouthamel, M. S. Eisenberg, L. J. Becker, and A. R. Lima. Temporal Patterns in Long-Term Survival After Resuscitation From Out-of-Hospital Cardiac Arrest Circulation, September 9, 2003; 108(10): 1196 - 1201.
- M. Hilker, T. Langin, U. Hake, F.-X. Schmid, W. Kuroczynski, H.-A. Lehr, H. Oelert, and M. Buerke Gene expression profiling of human stenotic aorto-coronary bypass grafts by cDNA array analysis Eur. J. Cardiothorac. Surg., April 1, 2003; 23(4): 620 - 625.
- J. L. Sperry, C. B. Deming, C. Bian, P. L. Walinsky, D. A. Kass, F. D. Kolodgie, R. Virmani, A. Y. Kim, and J. J. Rade Wall Tension Is a Potent Negative Regulator of In Vivo Thrombomodulin Expression Circ. Res., January 10, 2003; 92(1): 41 - 47.
- F. J. Schoen and R. F. Padera Jr. Cardiac Surgical Pathology Card. Surg. Adult, January 1, 2003; 2(2003): 119 - 185.
- A. Y. Kim, P. L. Walinsky, F. D. Kolodgie, C. Bian, J. L. Sperry, C. B. Deming, E. A. Peck, J. G. Shake, G. B. Ang, R. H. Sohn, et al. Early Loss of Thrombomodulin Expression Impairs Vein Graft Thromboresistance: Implications for Vein Graft Failure Circ. Res., February 8, 2002; 90(2): 205 - 212.
- K. B. Kim, C. Lim, C. Lee, I.-H. Chae, B.-H. Oh, M.-M. Lee, and Y.-B. Park Off-pump coronary artery bypass may decrease the patency of saphenous vein grafts Ann. Thorac. Surg., September 1, 2001; 72(3): S1033 - 1037.
- Z. Yang, T. Kozai, B. van de Loo, H. Viswambharan, M. Lachat, M. I. Turina, T. Malinski, and T. F. Luscher. HMG-CoA reductase inhibition improves endothelial cell function and inhibits smooth muscle cell proliferation in human saphenous veins J. Am. Coll. Cardiol., November 1, 2000; 36(5): 1691 - 1697.
- H. Hirose, A. Amano, S. Yoshida, A. Takahashi, N. Nagano, and T. Kohmoto Coronary Artery Bypass Grafting in the Elderly Chest, May 1, 2000; 117(5): 1262 - 1270.
- D. R. Holmes Jr and P. B. Berger. Percutaneous Revascularization of Occluded Vein Grafts : Is It Still a Temptation to Be Resisted? Circulation, January 12, 1999; 99(1): 8 - 11.
- Y. K. Wong, M. Thomas, V. Tsang, P. J. Gallagher, and M. E. Ward. The prevalence of Chlamydia pneumoniae in atherosclerotic and nonatherosclerotic blood vessels of patients attending for redo and first time coronary artery bypass graft surgery. J. Am. Coll. Cardiol., January 1, 1999; 33(1): 152 - 156.
- F. D. Loop Coronary artery surgery: the end of the beginning Eur. J. Cardiothorac. Surg., December 1, 1998; 14(6): 554 - 571.
- Z. G. Zhu, H.-H. Li, and B.-R. Zhang. Expression of Endothelin-1 and Constitutional Nitric Oxide Synthase Messenger RNA in Saphenous Vein Endothelial Cells Exposed to Arterial Flow Shear Stress Ann. Thorac. Surg., November 1, 1997; 64(5): 1333 - 1338.
- A. Y. Kim, P. L. Walinsky, F. D. Kolodgie, C. Bian, J. L. Sperry, C. B. Deming, E. A. Peck, J. G. Shake, G. B. Ang, R. H. Sohn, et al. Early Loss of Thrombomodulin Expression Impairs Vein Graft Thromboresistance: Implications for Vein Graft Failure. Circ. Res., February 8, 2002; 90(2): 205 - 212.
See Also
- CABG
- Hybrid bypass
- Off-pump coronary artery bypass surgery (OPCAB)
- Minimally invasive direct coronary artery bypass surgery (MIDCAB)