Cirrhosis
| Cirrhosis | |
 | |
|---|---|
| Gross, natural color of liver and stomach view from external surfaces, micronodular cirrhosis and hemorrhagic gastritis (as the surgeon would see these in natural color). Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | K70.3, K71.7, K74 |
| ICD-9 | 571 |
| DiseasesDB | 2729 |
| MeSH | D008103 |
|
Cirrhosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case studies |
|
Cirrhosis On the Web |
|
American Roentgen Ray Society Images of Cirrhosis |
|
WikiDoc Resources for Cirrhosis |
|
Articles |
|---|
|
Most recent articles on Cirrhosis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cirrhosis at Clinical Trials.gov Clinical Trials on Cirrhosis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cirrhosis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cirrhosis Discussion groups on Cirrhosis Directions to Hospitals Treating Cirrhosis Risk calculators and risk factors for Cirrhosis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cirrhosis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Aditya Govindavarjhulla, M.B.B.S. [3]
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differential Diagnosis
Epidemiology and Demographics
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
Symptoms | Physical Examination |Laboratory tests | ECG | Endoscopy |CT | MRI |Echocardiography or Ultrasound |Other imaging studies | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Prevention | Financial costs| Future therapies
Diagnosis
Imaging
Computer Tomography
-
Liver cirrhosis as seen on an axial CT of the abdomen.
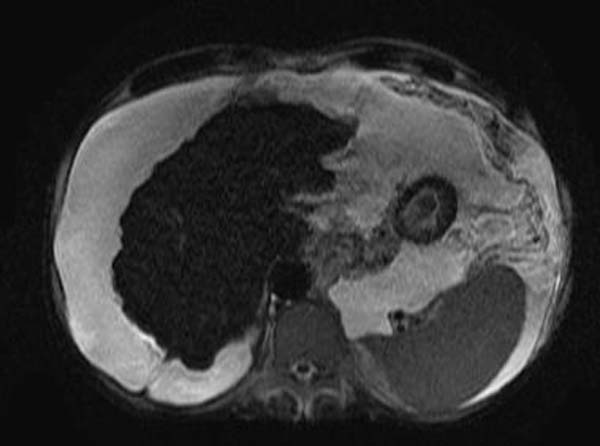
MRI
-
T2
-
T2
Other Diagnostic Modalities
If biliary pathology (primary sclerosing cholangitis - PSC) is suspected, ERCP may be performed.
Generally MRCP (MRI of biliary tract and pancreas) is sufficient for diagnosis, but ERCP allows for particular interventions, such as placement of a biliary stent or extraction of gallstones.
Grading
The severity of cirrhosis is commonly classified with the Child-Pugh score. This score uses bilirubin, albumin, INR, presence and severity of ascites and encephalopathy to classify patients in class A, B or C; class A has a favourable prognosis, while class C is at high risk of death. It was devised in 1964 by Child and Turcotte and modified in 1973 by Pugh et al.[1]
More modern scores, used in the allocation of liver transplants but also in other contexts, are the Model for End-Stage Liver Disease (MELD) score and its pediatric counterpart, the Pediatric End-Stage Liver Disease (PELD) score.
Treatment
Traditionally, liver damage from cirrhosis cannot be reversed, but treatment could stop or delay further progression and reduce complications. A healthy diet is encouraged, as cirrhosis may be an energy-consuming process. Close follow-up is often necessary. Antibiotics will be prescribed for infections, and various medications can help with itching. Laxatives, such as lactulose, decrease risk of constipation; their role in preventing encephalopathy is limited.
Treating underlying causes
Alcoholic cirrhosis caused by alcohol abuse is treated by abstaining from alcohol. Treatment for hepatitis-related cirrhosis involves medications used to treat the different types of hepatitis, such as interferon for viral hepatitis and corticosteroids for autoimmune hepatitis. Cirrhosis caused by Wilson's disease, in which copper builds up in organs, is treated with chelation therapy (e.g. penicillamine) to remove the copper.
Preventing further liver damage
Regardless of underlying cause of cirrhosis, alcohol and acetaminophen, as well as other potentially damaging substances, are discouraged. Vaccination of susceptible patients should be considered for Hepatitis A and Hepatitis B.
Chronic Pharmacotherapies
Varices
- Endoscopic screening in all cirrhotic patients
- If varices present--treat with propranolol or nadolol
Hepatocellular Cancer
- Incidence 1-6%/year in HCV-, HBV-, EtOH-related cirrhosis
- Screening frequency & benefit controversial
- Serum alpha-fetoprotein (AFP) every 6 months (~60% sensitive, ~90% specific)
- Ultrasound every 6 months (~75% sensitive, ~90% specific)
Preventing complications
Ascites
Salt restriction is often necessary, as cirrhosis leads to accumulation of salt (sodium retention). Diuretics may be necessary to suppress ascites.
Esophageal variceal bleeding
For portal hypertension, propranolol is a commonly used agent to lower blood pressure over the portal system. In severe complications from portal hypertension, transjugular intrahepatic portosystemic shunting is occasionally indicated to relieve pressure on the portal vein. As this can worsen encephalopathy, it is reserved for those at low risk of encephalopathy, and is generally regarded only as a bridge to liver transplantation or as a palliative measure.
Hepatic encephalopathy
High-protein food increases the nitrogen balance, and would theoretically increase encephalopathy; in the past, this was therefore eliminated as much as possible from the diet. Recent studies show that this assumption was incorrect, and high-protein foods are even encouraged to maintain adequate nutrition.
Hepatorenal syndrome
The hepatorenal syndrome is defined as a urine sodium less than 10 mmol/L and a serum creatinine > 1.5 mg/dl (or 24 hour creatinine clearance less than 40 ml/min) after a trial of volume expansion without diuretics.[2]
Spontaneous bacterial peritonitis
Cirrhotic patients with ascites are at risk of spontaneous bacterial peritonitis.
Transplantation
If complications cannot be controlled or when the liver ceases functioning, liver transplantation is necessary. Survival from liver transplantation has been improving over the 1990s, and the five-year survival rate is now around 80%, depending largely on the severity of disease and other medical problems in the recipient.[3] In the United States, the MELD score (online calculator)[4] is used to prioritize patients for transplantation. Transplantation necessitates the use of immune suppressants (ciclosporin or tacrolimus).
Decompensated cirrhosis
In patients with previously stable cirrhosis, decompensation may occur due to various causes, such as constipation, infection (of any source), increased alcohol intake, medication, bleeding from esophageal varices or dehydration. It may take the form of any of the complications of cirrhosis listed above.
Patients with decompensated cirrhosis generally require admission to hospital, with close monitoring of the fluid balance, mental status, and emphasis on adequate nutrition and medical treatment - often with diuretics, antibiotics, laxatives and/or enemas, thiamine and occasionally steroids, acetylcysteine and pentoxifylline. Administration of saline is generally avoided as it would add to the already high total body sodium content that typically occurs in cirrhosis.
Primary Prevention
- Education about hepatotoxins:
- EtOH
- Acetaminophen
- Herbals
- Maintenance of adequate caloric intake: 2000-3000 kcal/d
- Hepatitis A Virus vaccination, Pneumovax
References
- ↑ Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973;60:646-9. PMID 4541913.
- ↑ Ginés P, Arroyo V, Quintero E; et al. (1987). "Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites. Results of a randomized study". Gastroenterology. 93 (2): 234–41. PMID 3297907.
- ↑ E-medicine liver transplant outlook and survival rates
- ↑ Cosby RL, Yee B, Schrier RW (1989). "New classification with prognostic value in cirrhotic patients". Mineral and electrolyte metabolism. 15 (5): 261–6. PMID 2682175.
External links
- Cirrhosis of the Liver at the National Digestive Diseases Information Clearinghouse (NDDIC). NIH Publication No. 04-1134, December 2003.
- [4] at the National Library of Medicine and the National Institutes of Health. Medline Plus: Cirrhosis -- also called: Hepatic fibrosis
zh-min-nan:Koaⁿ-ngē-hoà da:Skrumplever de:Leberzirrhose eu:Zirrosi hr:Ciroza jetre is:Skorpulifur it:Cirrosi epatica he:שחמת הכבד la:Cirrosis iecuris ln:Bokɔnɔ bwa libale mk:Цироза nl:Levercirrose no:Skrumplever sq:Cirroza sl:Ciroza jeter fi:Kirroosi sv:Skrumplever