Sexcord/ stromal ovarian tumors pathophysiology: Difference between revisions
| Line 205: | Line 205: | ||
|} | |} | ||
==Immunohistochemistry== | ==Immunohistochemistry== | ||
Adult granulosa cell tumors | Adult granulosa cell tumors stain Positive for: | ||
Positive for | |||
*Inhibin | *Inhibin | ||
*Calretinin | *Calretinin | ||
*FOXL2 and | *FOXL2 and | ||
*SF-1 | *SF-1 | ||
*WT1 | |||
*CD56 | |||
==References== | ==References== | ||
Revision as of 15:53, 28 March 2019
|
Sexcord/ stromal ovarian tumors Microchapters |
|
Differentiating Sexcord/ Stromal Ovarian Tumors from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Sexcord/ stromal ovarian tumors pathophysiology On the Web |
|
American Roentgen Ray Society Images of Sexcord/ stromal ovarian tumors pathophysiology |
|
Risk calculators and risk factors for Sexcord/ stromal ovarian tumors pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
The exact pathogenesis of [disease name] is not fully understood.
OR
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
OR
[Pathogen name] is usually transmitted via the [transmission route] route to the human host.
OR
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
OR
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
OR
The progression to [disease name] usually involves the [molecular pathway].
OR
The pathophysiology of [disease/malignancy] depends on the histological subtype.
Pathophysiology
Physiology
The normal physiology of [name of process] can be understood as follows:
Pathogenesis
- The exact pathogenesis of [disease name] is not completely understood.
OR
- It is understood that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
- [Pathogen name] is usually transmitted via the [transmission route] route to the human host.
- Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
- [Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
- The progression to [disease name] usually involves the [molecular pathway].
- The pathophysiology of [disease/malignancy] depends on the histological subtype.
Genetics
- The recent advancing analyses have made us understand the pathophysiology of some of these tumor subtypes
- Mutations mainly involving DICER1, STK11, and FOXL2 influence the development of some of these neoplasms
- FOXL2 is a tumor suppressor gene
- It is a member of the forkhead box (FOX) family of evolutionarily conserved transcription factors
- It plays a fundamental and crucial role in ovarian development
- It regulates the ovarian granulosa cell proliferation, follicle development and ovarian hormones synthesis
- Almost all like 97% of adult granulosa cell tumors are characterized by missense somatic point mutations (402 C→G) in FOXL2 gene
- Infact this mutation is a sensitive and specific biomarker for adult granulosa cell tumors making it a pathognomonic feature
- The phosphorylation modification of FOXL2 in particular is responsible to the growth of granulosa cell tumors
- Importantly this mutation alter's antiproliferative pathways and also limit the apoptosis, as a result contributing to the pathogenesis of adult granulosa cell tumors
- Other factors that play an important role in the pathogenesis of granulosa cell tuomrs are PI3K/AKT (phosphatidylinositol-3-kinase; serine/threonine kinase), TGF-β (Transforming growth factor beta) signaling pathway, Notch signaling pathway, GATA4 and VEGF (vascular endothelial growth factor)

- DICER1 mutations are associated with leydig cell tumors and gynandroblastomas
- Although both germ line and somatic mutations play a role, approximately 60% of sexcord leydig cell tumors have somatic DICER1 mutations
- This particular gene DICER1 encodes for a RNA endoribonuclease that helps to cleave precursor miRNA into mature miRNAs
- DICER1 mutations are associated with a lot of tumors of which pleuropulmonary blastoma, is the most common lung tumor of infancy and early childhood
- Others are embryonal rhabdomyosarcoma of the uterine cervix, renal tumors, thyroid nodules and carcinoma, nasal chondromesenchymal hamartoma, ciliary body medulloepithelioma, pineoblastoma, and pituitary blastoma
- The above mentioned tumors typically have biallelic DICER1 mutations that are composed of a loss of function in one allele and a missense mutation in the RNase IIIb domain
STK11:
- Mutations in the STK11 gene is associated with sex cord-stromal tumors with annular tubules
Associated Conditions
- Ollier disease and Maffucci syndrome are associated with an increased risk of juvenile granulosa cell tumors[9][5]
- Somatic mosaic mutations in IDH1 and IDH2 are observed
- Ollier disease includes enchondromatosis, whereas Mafucci syndrome includes enchondromatosis and hemangiomas
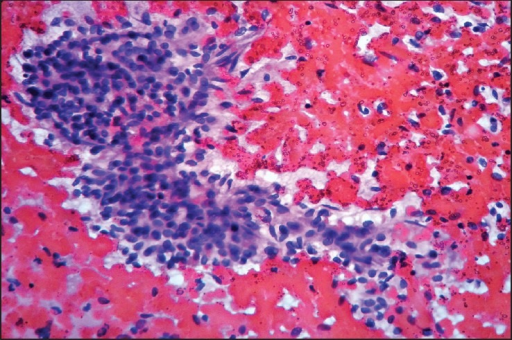
Gross and Microscopic Pathology
The gross and microscopic features of the most common tumors are described below:[5][12][13][14][15][16][17][6][18][19][20]
| Types | Gross pathology | Microscopic pathology | Images |
|---|---|---|---|
| Adult granulosa cell tumours |
|
|
 |
| Juvenile granulosa cell tumours |
|
|
 |
| Sex cord tumour with annular tubules |
|
|
 |
| Sertoli–Leydig cell tumours |
|
|
 |
| Sclerosing stromal tumour |
|
|
 |
| Luteinised thecomas with sclerosing peritonitis |
|
|
 |
| Microcystic stromal tumour |
|
The microscopic appearance consists of three components:
The microcystic pattern is characterised by small round to oval cystic spaces, focally coalescing into larger irregular channels; intracytoplasmic vacuoles are also common The solid cellular areas are usually intersected by fibrous bands and hyalineplaques |
|
| Fibroma |
|
|
 |
| Thecoma |
|
|
 |
| Fibrosarcoma |
|
|
Immunohistochemistry
Adult granulosa cell tumors stain Positive for:
- Inhibin
- Calretinin
- FOXL2 and
- SF-1
- WT1
- CD56
References
- ↑ 1.0 1.1 Lim, Diana; Oliva, Esther (2018). "Ovarian sex cord-stromal tumours: an update in recent molecular advances". Pathology. 50 (2): 178–189. doi:10.1016/j.pathol.2017.10.008. ISSN 0031-3025.
- ↑ 2.0 2.1 Fuller PJ, Leung D, Chu S (February 2017). "Genetics and genomics of ovarian sex cord-stromal tumors". Clin. Genet. 91 (2): 285–291. doi:10.1111/cge.12917. PMID 27813081.
- ↑ Li, Jiaheng; Bao, Riqiang; Peng, Shiwei; Zhang, Chunping (2018). "The molecular mechanism of ovarian granulosa cell tumors". Journal of Ovarian Research. 11 (1). doi:10.1186/s13048-018-0384-1. ISSN 1757-2215.
- ↑ Li J, Bao R, Peng S, Zhang C (February 2018). "The molecular mechanism of ovarian granulosa cell tumors". J Ovarian Res. 11 (1): 13. doi:10.1186/s13048-018-0384-1. PMC 5802052. PMID 29409506.
- ↑ 5.0 5.1 5.2 Schultz KA, Harris AK, Schneider DT, Young RH, Brown J, Gershenson DM, Dehner LP, Hill DA, Messinger YH, Frazier AL (October 2016). "Ovarian Sex Cord-Stromal Tumors". J Oncol Pract. 12 (10): 940–946. doi:10.1200/JOP.2016.016261. PMC 5063189. PMID 27858560.
- ↑ 6.0 6.1 Boussios, Stergios; Moschetta, Michele; Zarkavelis, George; Papadaki, Alexandra; Kefas, Aristides; Tatsi, Konstantina (2017). "Ovarian sex-cord stromal tumours and small cell tumours: Pathological, genetic and management aspects". Critical Reviews in Oncology/Hematology. 120: 43–51. doi:10.1016/j.critrevonc.2017.10.007. ISSN 1040-8428.
- ↑ Leung, Dilys T.H.; Fuller, Peter J.; Chu, Simon (2016). "Impact of FOXL2 mutations on signaling in ovarian granulosa cell tumors". The International Journal of Biochemistry & Cell Biology. 72: 51–54. doi:10.1016/j.biocel.2016.01.003. ISSN 1357-2725.
- ↑ Goulvent T, Ray-Coquard I, Borel S, Haddad V, Devouassoux-Shisheboran M, Vacher-Lavenu MC, Pujade-Laurraine E, Savina A, Maillet D, Gillet G, Treilleux I, Rimokh R (January 2016). "DICER1 and FOXL2 mutations in ovarian sex cord-stromal tumours: a GINECO Group study". Histopathology. 68 (2): 279–85. doi:10.1111/his.12747. PMID 26033501.
- ↑ 9.0 9.1 Stewart CJ, Charles A, Foulkes WD (June 2016). "Gynecologic Manifestations of the DICER1 Syndrome". Surg Pathol Clin. 9 (2): 227–41. doi:10.1016/j.path.2016.01.002. PMID 27241106.
- ↑ Wang Y, Karnezis AN, Magrill J, Tessier-Cloutier B, Lum A, Senz J, Gilks CB, McCluggage WG, Huntsman DG, Kommoss F (August 2018). "DICER1 hot-spot mutations in ovarian gynandroblastoma". Histopathology. 73 (2): 306–313. doi:10.1111/his.13630. PMID 29660837.
- ↑ Xu Q, Zou Y, Zhang XF (October 2018). "Sertoli-Leydig cell tumors of ovary: A case series". Medicine (Baltimore). 97 (42): e12865. doi:10.1097/MD.0000000000012865. PMC 6211859. PMID 30334998.
- ↑ Bremmer F, Schweyer S (February 2016). "[Leydig cell, Sertoli cell and adult granulosa cell tumors]". Pathologe (in German). 37 (1): 71–7. doi:10.1007/s00292-015-0131-y. PMID 26782032.
- ↑ Bremmer F, Behnes CL, Radzun HJ, Bettstetter M, Schweyer S (May 2014). "[Sex cord gonadal stromal tumors]". Pathologe (in German). 35 (3): 245–51. doi:10.1007/s00292-014-1901-7. PMID 24819979.
- ↑ Roth LM, Czernobilsky B (March 2011). "Perspectives on pure ovarian stromal neoplasms and tumor-like proliferations of the ovarian stroma". Am. J. Surg. Pathol. 35 (3): e15–33. doi:10.1097/PAS.0b013e31820acb89. PMID 21317704.
- ↑ Young RH (January 2018). "Ovarian sex cord-stromal tumours and their mimics". Pathology. 50 (1): 5–15. doi:10.1016/j.pathol.2017.09.007. PMID 29132723.
- ↑ Zhang HY, Zhu JE, Huang W, Zhu J (2014). "Clinicopathologic features of ovarian Sertoli-Leydig cell tumors". Int J Clin Exp Pathol. 7 (10): 6956–64. PMC 4230071. PMID 25400781.
- ↑ Chen, Vivien W.; Ruiz, Bernardo; Killeen, Jeffrey L.; Cot�, Timothy R.; Wu, Xiao Cheng; Correa, Catherine N.; Howe, Holly L. (2003). "Pathology and classification of ovarian tumors". Cancer. 97 (S10): 2631–2642. doi:10.1002/cncr.11345. ISSN 0008-543X. replacement character in
|last4=at position 4 (help) - ↑ Irving JA, Lee CH, Yip S, Oliva E, McCluggage WG, Young RH (October 2015). "Microcystic Stromal Tumor: A Distinctive Ovarian Sex Cord-Stromal Neoplasm Characterized by FOXL2, SF-1, WT-1, Cyclin D1, and β-catenin Nuclear Expression and CTNNB1 Mutations". Am. J. Surg. Pathol. 39 (10): 1420–6. doi:10.1097/PAS.0000000000000482. PMID 26200099.
- ↑ Irving JA, Young RH (March 2009). "Microcystic stromal tumor of the ovary: report of 16 cases of a hitherto uncharacterized distinctive ovarian neoplasm". Am. J. Surg. Pathol. 33 (3): 367–75. doi:10.1097/PAS.0b013e31818479c3. PMID 18971779.
- ↑ Mathur A, Seth A, Pant L (2018). "Ovarian fibroma with luteinized thecal cells and minor sex cord element: A rare case report". Indian J Pathol Microbiol. 61 (2): 264–267. doi:10.4103/IJPM.IJPM_446_17. PMID 29676374.