Radiation induced pericarditis: Difference between revisions
(→MRI) |
No edit summary |
||
| (12 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
The [[survival rate]] in [[Hodgkin lymphoma]], [[Non-Hodgkin's lymphoma]] and [[breast cancer|breast carcinomas]] has significantly improved with use of [[radiation therapy]].However, radiation therapy to [[thoracic]] and [[mediastinal]] cancers have also led to the development of [[pericarditis]], [[coronary artery disease]], [[cardiomyopathy]], [[Conduction System|conduction]] abnormalities in heart and [[valvular heart disease]]s which account for significant [[morbidity]] and [[mortality]]. Radiation-induced pericarditis was first described in the mid-1960s. The radiation-induced pericardial disease may be classified as [[acute pericarditis]], delayed pericarditis, pancarditis, [[constrictive pericarditis]], and [[pericardial effusion]]. Radiation therapy leads to disruption of [[endothelium]] and subsequent episodes of [[ischemia]]. The resulting [[fibrosis]] and [[fibrinous]] [[Exudate|exudates]] replace [[collagen]] fibers. Radiation-induced pericardial disease can occur in any cancer survivor who receive thoracic radiation therapy, including [[breast cancer]], [[Hodgkin's lymphoma]], [[esophageal cancer]], and [[lung cancer]]. Radiation-induced pericarditis depends on the total dose of radiation, the dose per fraction, the amount of cardiac silhouette exposed, and the nature of the radiation source. The incidence is higher with doses greater than 40 Gy (4000 rad). [[Echocardiography]] is the most commonly used [[screening]] modality for the detection and follow-up of radiation-induced cardiac disease. [[Acute pericarditis]] usually develops a few weeks after radiation exposure. Nearly 20% of patients with [[acute pericarditis]] develop [[chronic]] or [[constrictive pericarditis]] in the next 5-10 years following radiation therapy. The risk is increased when [[pericardial effusion]] was present previously. [[Chronic pericarditis]] can also occur in patients without a history of [[acute pericarditis]]. | The [[survival rate]] in [[Hodgkin lymphoma]], [[Non-Hodgkin's lymphoma]] and [[breast cancer|breast carcinomas]] has significantly improved with use of [[radiation therapy]].However, radiation therapy to [[thoracic]] and [[mediastinal]] cancers have also led to the development of [[pericarditis]], [[coronary artery disease]], [[cardiomyopathy]], [[Conduction System|conduction]] abnormalities in heart and [[valvular heart disease]]s which account for significant [[morbidity]] and [[mortality]]. Radiation-induced pericarditis was first described in the mid-1960s. The radiation-induced pericardial disease may be classified as [[acute pericarditis]], delayed pericarditis, pancarditis, [[constrictive pericarditis]], and [[pericardial effusion]]. Radiation therapy leads to disruption of [[endothelium]] and subsequent episodes of [[ischemia]]. The resulting [[fibrosis]] and [[fibrinous]] [[Exudate|exudates]] replace [[collagen]] fibers. Radiation-induced pericardial disease can occur in any cancer survivor who receive [[thoracic]] radiation therapy, including [[breast cancer]], [[Hodgkin's lymphoma]], [[esophageal cancer]], and [[lung cancer]]. Radiation-induced pericarditis depends on the total dose of radiation, the dose per fraction, the amount of cardiac silhouette exposed, and the nature of the radiation source. The incidence is higher with doses greater than 40 Gy (4000 rad). [[Echocardiography]] is the most commonly used [[screening]] modality for the detection and follow-up of radiation-induced cardiac disease. [[Acute pericarditis]] usually develops a few weeks after radiation exposure. Nearly 20% of patients with [[acute pericarditis]] develop [[chronic]] or [[constrictive pericarditis]] in the next 5-10 years following radiation therapy. The risk is increased when [[pericardial effusion]] was present previously. [[Chronic pericarditis]] can also occur in patients without a history of [[acute pericarditis]]. Acute pericarditis is a rare [[complication]] of [[radiation therapy]]. It presents with nonspecific [[pericarditis]] [[symptoms]] such as [[chest pain]] and [[fever]] shortly after [[radiation therapy]]. Delayed [[pericarditis]] occurs from months to years after exposure to [[radiation]]. It usually presents with [[chest pain]], [[dyspnea]], and [[orthopnea]]. The physical examination may show [[fever]] and [[Pericardial friction rub|pericardial rub]]. Laboratory findings include elevated inflammatory markers such as [[neutrophil]] count and [[Erythrocyte sedimentation rate|erythrocyte sedimentation rate (ESR)]]. On [[ECG]], non-specific [[ST-segment|ST]] and [[T wave]] changes or [[ST-segment elevation]] in all leads may be noted. The majority of [[acute pericarditis]] cases are self-limited and respond well to [[nonsteroidal anti-inflammatory drugs]] and [[colchicine]]. In [[Acute pericarditis|acute]] or [[chronic pericarditis]], protein-rich [[exudate]] may accumulate in the [[pericardial sac]] leading to [[pericardial effusion]]. Findings on a chest [[x-ray]] or chest [[Computed tomography|CT]] suggestive of [[chronic pericarditis]] include [[pericardial effusion]] and pericardial thickening. If the effusion is large enough, it may lead to [[Cardiac tamponade|tamponade]]. In patients presenting with [[Cardiac tamponade|tamponade]], the physical examination may show [[hypotension]], [[tachycardia]], and [[jugular venous distention]] with a prominent Y descent, [[Kussmaul’s sign]], and distant [[Heart sounds|heart sound]]. Radiation-induced [[pericardial effusion]] can be confused with [[malignant pericarditis]] and [[hypothyroidism]]-induced pericarditis. Pericarditis with large effusion can be drained either [[percutaneously]] or surgically. Those with recurrent [[pericardial effusion]] can be treated with pericardiotomy([[pericardial window]]) or by surgical [[stripping]]. [[Constrictive pericarditis]] is a late [[Complications|complication]] of [[radiation therapy]]. Patients typically present with [[signs]] and [[symptoms]] of [[heart failure]], similar to other causes of [[constrictive pericarditis]]. [[Cardiac MRI]] may be helpful in the diagnosis of [[constrictive pericarditis]]. It is useful to confirm the pericardial thickening. [[Cardiac catheterization]] may be also helpful in the diagnosis of [[constrictive pericarditis]] associated with [[radiation therapy]]. [[Pericardiectomy]] is recommended for patients who develop [[constrictive pericarditis]]. However, the [[perioperative]] [[mortality rate]] is higher in radiation-induced [[constrictive pericarditis]] compared to that of [[idiopathic]] [[constrictive pericarditis]]. Effective measures for the [[primary prevention]] of radiation-induced pericarditis include reducing the [[dose]] and volume of cardiac [[irradiation]] when possible. | ||
==Historical Perspective== | ==Historical Perspective== | ||
| Line 13: | Line 13: | ||
Based on the presentation and onset of symptoms, the radiation-induced pericardial disease may be classified as:<ref name="pmid21403872">{{cite journal| author=Yusuf SW, Sami S, Daher IN| title=Radiation-induced heart disease: a clinical update. | journal=Cardiol Res Pract | year= 2011 | volume= 2011 | issue= | pages= 317659 | pmid=21403872 | doi=10.4061/2011/317659 | pmc=3051159 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21403872 }} </ref> | Based on the presentation and onset of symptoms, the radiation-induced pericardial disease may be classified as:<ref name="pmid21403872">{{cite journal| author=Yusuf SW, Sami S, Daher IN| title=Radiation-induced heart disease: a clinical update. | journal=Cardiol Res Pract | year= 2011 | volume= 2011 | issue= | pages= 317659 | pmid=21403872 | doi=10.4061/2011/317659 | pmc=3051159 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21403872 }} </ref> | ||
#[[Acute pericarditis]] | #[[Acute pericarditis]] | ||
#Delayed pericarditis | #Delayed [[pericarditis]] | ||
#Pancarditis | #Pancarditis | ||
#[[Constrictive pericarditis]] | #[[Constrictive pericarditis]] | ||
| Line 19: | Line 19: | ||
==Pathophysiology== | ==Pathophysiology== | ||
Radiation therapy disrupts endothelial cells of the microvasculature of the pericardium and leads to repeated episodes of ischemia. The final result is the formation of fibrosis and fibrinous exudates that are ultimately replaced by fibroblasts and collagen fibers <ref name="pmid2697671">{{cite journal| author=Fajardo LF| title=The unique physiology of endothelial cells and its implications in radiobiology. | journal=Front Radiat Ther Oncol | year= 1989 | volume= 23 | issue= | pages= 96-112 | pmid=2697671 | doi=10.1159/000416574 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2697671 }} </ref><ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref><ref name="pmid25741474">{{cite journal| author=Taunk NK, Haffty BG, Kostis JB, Goyal S| title=Radiation-induced heart disease: pathologic abnormalities and putative mechanisms. | journal=Front Oncol | year= 2015 | volume= 5 | issue= | pages= 39 | pmid=25741474 | doi=10.3389/fonc.2015.00039 | pmc=4332338 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25741474 }} </ref><ref name="pmid16446057">{{cite journal| author=Hooning MJ, Aleman BM, van Rosmalen AJ, Kuenen MA, Klijn JG, van Leeuwen FE| title=Cause-specific mortality in long-term survivors of breast cancer: A 25-year follow-up study. | journal=Int J Radiat Oncol Biol Phys | year= 2006 | volume= 64 | issue= 4 | pages= 1081-91 | pmid=16446057 | doi=10.1016/j.ijrobp.2005.10.022 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16446057 }} </ref>. | Radiation therapy disrupts [[endothelial cells]] of the [[microvasculature]] of the [[pericardium]] and leads to repeated episodes of [[ischemia]]. The final result is the formation of [[fibrosis]] and [[fibrinous]] [[Exudate|exudates]] that are ultimately replaced by [[fibroblasts]] and [[collagen]] fibers <ref name="pmid2697671">{{cite journal| author=Fajardo LF| title=The unique physiology of endothelial cells and its implications in radiobiology. | journal=Front Radiat Ther Oncol | year= 1989 | volume= 23 | issue= | pages= 96-112 | pmid=2697671 | doi=10.1159/000416574 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2697671 }} </ref><ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref><ref name="pmid25741474">{{cite journal| author=Taunk NK, Haffty BG, Kostis JB, Goyal S| title=Radiation-induced heart disease: pathologic abnormalities and putative mechanisms. | journal=Front Oncol | year= 2015 | volume= 5 | issue= | pages= 39 | pmid=25741474 | doi=10.3389/fonc.2015.00039 | pmc=4332338 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25741474 }} </ref><ref name="pmid16446057">{{cite journal| author=Hooning MJ, Aleman BM, van Rosmalen AJ, Kuenen MA, Klijn JG, van Leeuwen FE| title=Cause-specific mortality in long-term survivors of breast cancer: A 25-year follow-up study. | journal=Int J Radiat Oncol Biol Phys | year= 2006 | volume= 64 | issue= 4 | pages= 1081-91 | pmid=16446057 | doi=10.1016/j.ijrobp.2005.10.022 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16446057 }} </ref>. | ||
==Causes== | ==Causes== | ||
Radiation-induced pericardial disease can occur in any cancer survivor who receive thoracic radiation therapy, including breast cancer, Hodgkin's lymphoma, esophageal cancer, and lung cancer. However, most data come from patients treated for breast cancer and Hodgkin's lymphoma, in which radiation therapy is a frequent component of management. | Radiation-induced [[pericardial disease]] can occur in any [[cancer]] survivor who receive [[thoracic]] radiation therapy, including [[breast cancer]], [[Hodgkin's lymphoma]], [[esophageal cancer]], and [[lung cancer]]. However, most data come from patients treated for [[breast cancer]] and [[Hodgkin's lymphoma]], in which radiation therapy is a frequent component of management. | ||
==Differentiating Radiation-induced Pericarditis from other Diseases== | ==Differentiating Radiation-induced Pericarditis from other Diseases== | ||
| Line 57: | Line 57: | ||
*Constrictive | *[[Constrictive pericarditis]] should be differentiated from [[restrictive cardiomyopathy]]<ref name="pmid29270320">{{cite journal |vauthors=Rammos A, Meladinis V, Vovas G, Patsouras D |title=Restrictive Cardiomyopathies: The Importance of Noninvasive Cardiac Imaging Modalities in Diagnosis and Treatment-A Systematic Review |journal=Radiol Res Pract |volume=2017 |issue= |pages=2874902 |date=2017 |pmid=29270320 |pmc=5705874 |doi=10.1155/2017/2874902 |url=}}</ref><ref name="pmid28885342">{{cite journal |vauthors=Hong JA, Kim MS, Cho MS, Choi HI, Kang DH, Lee SE, Lee GY, Jeon ES, Cho JY, Kim KH, Yoo BS, Lee JY, Kim WJ, Kim KH, Chung WJ, Lee JH, Cho MC, Kim JJ |title=Clinical features of idiopathic restrictive cardiomyopathy: A retrospective multicenter cohort study over 2 decades |journal=Medicine (Baltimore) |volume=96 |issue=36 |pages=e7886 |date=September 2017 |pmid=28885342 |pmc=6393124 |doi=10.1097/MD.0000000000007886 |url=}}</ref>: | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 84: | Line 84: | ||
*MRI: Thickened pericardium | *MRI: Thickened pericardium | ||
| | | | ||
* LVEDP – RVEDP < 5 mmHg | *[[Left ventricular end diastolic pressure|LVEDP]] – RVEDP < 5 mmHg | ||
* RVSP < 55 mmHg | * RVSP < 55 mmHg | ||
* RVEDP/RVSP > 0.33 | * RVEDP/RVSP > 0.33 | ||
| Line 116: | Line 116: | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Pericardial changes are the most common cardiac complications of radiation therapy<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. Incidence of radiation induced pericarditis has significantly decreased with the use of lower doses and newer radiotherapy techniques <ref name="pmid949701">{{cite journal| author=Carmel RJ, Kaplan HS| title=Mantle irradiation in Hodgkin's disease. An analysis of technique, tumor eradication, and complications. | journal=Cancer | year= 1976 | volume= 37 | issue= 6 | pages= 2813-25 | pmid=949701 | doi=10.1002/1097-0142(197606)37:6<2813::aid-cncr2820370637>3.0.co;2-s | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=949701 }} </ref><ref name="pmid12923044">{{cite journal| author=Maisch B, Ristić AD| title=Practical aspects of the management of pericardial disease. | journal=Heart | year= 2003 | volume= 89 | issue= 9 | pages= 1096-103 | pmid=12923044 | doi= | pmc=PMC1767862 | url= }} </ref><ref name="pmid15120056">{{cite journal| author=Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y et al.| title=Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. | journal=Eur Heart J | year= 2004 | volume= 25 | issue= 7 | pages= 587-610 | pmid=15120056 | doi=10.1016/j.ehj.2004.02.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15120056 }} </ref>. In a study, incidence decreased from 20% to 2.5% with the changes in methods of RT administration<ref name="pmid949701">{{cite journal| author=Carmel RJ, Kaplan HS| title=Mantle irradiation in Hodgkin's disease. An analysis of technique, tumor eradication, and complications. | journal=Cancer | year= 1976 | volume= 37 | issue= 6 | pages= 2813-25 | pmid=949701 | doi= | pmc= | url= }} </ref> | Pericardial changes are the most common cardiac complications of radiation therapy<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. Incidence of radiation-induced pericarditis has significantly decreased with the use of lower doses and newer radiotherapy techniques <ref name="pmid949701">{{cite journal| author=Carmel RJ, Kaplan HS| title=Mantle irradiation in Hodgkin's disease. An analysis of technique, tumor eradication, and complications. | journal=Cancer | year= 1976 | volume= 37 | issue= 6 | pages= 2813-25 | pmid=949701 | doi=10.1002/1097-0142(197606)37:6<2813::aid-cncr2820370637>3.0.co;2-s | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=949701 }} </ref><ref name="pmid12923044">{{cite journal| author=Maisch B, Ristić AD| title=Practical aspects of the management of pericardial disease. | journal=Heart | year= 2003 | volume= 89 | issue= 9 | pages= 1096-103 | pmid=12923044 | doi= | pmc=PMC1767862 | url= }} </ref><ref name="pmid15120056">{{cite journal| author=Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y et al.| title=Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. | journal=Eur Heart J | year= 2004 | volume= 25 | issue= 7 | pages= 587-610 | pmid=15120056 | doi=10.1016/j.ehj.2004.02.002 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15120056 }} </ref>. In a study, [[incidence]] decreased from 20% to 2.5% with the changes in methods of RT administration<ref name="pmid949701">{{cite journal| author=Carmel RJ, Kaplan HS| title=Mantle irradiation in Hodgkin's disease. An analysis of technique, tumor eradication, and complications. | journal=Cancer | year= 1976 | volume= 37 | issue= 6 | pages= 2813-25 | pmid=949701 | doi= | pmc= | url= }} </ref> | ||
In a study among pediatric population with various cancers, radiation therapy with ≥15 GY increased the risk of developing pericarditis by two to six times<ref name="pmid19996459">{{cite journal| author=Mulrooney DA, Yeazel MW, Kawashima T, Mertens AC, Mitby P, Stovall M et al.| title=Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. | journal=BMJ | year= 2009 | volume= 339 | issue= | pages= b4606 | pmid=19996459 | doi=10.1136/bmj.b4606 | pmc= | url= }} </ref> | In a study among [[pediatric]] population with various [[cancers]], radiation therapy with ≥15 GY increased the risk of developing pericarditis by two to six times<ref name="pmid19996459">{{cite journal| author=Mulrooney DA, Yeazel MW, Kawashima T, Mertens AC, Mitby P, Stovall M et al.| title=Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort. | journal=BMJ | year= 2009 | volume= 339 | issue= | pages= b4606 | pmid=19996459 | doi=10.1136/bmj.b4606 | pmc= | url= }} </ref> | ||
==Risk Factors== | ==Risk Factors== | ||
Radiation-induced pericarditis depends on: | Radiation-induced pericarditis depends on: | ||
*Total dose of radiation | *Total [[dose]] of radiation | ||
*The dose per fraction | *The [[dose]] per fraction | ||
*Amount of cardiac silhouette exposed | *Amount of cardiac silhouette exposed | ||
*Nature of the radiation source | *Nature of the radiation source | ||
In a retrospective study, 27.7% of the patients developed [[pericardial effusion]] after median time period of 5.3 months following radiotherapy for [[esophageal carcinoma]] with radiation dose ranging between 3 to 50Gy. It was concluded that high dose-volume of the irradiated pericardium and heart increased the risk of developing pericarditis<ref name="pmid18191334">{{cite journal| author=Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD et al.| title=Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy. | journal=Int J Radiat Oncol Biol Phys | year= 2008 | volume= 70 | issue= 3 | pages= 707-14 | pmid=18191334 | doi=10.1016/j.ijrobp.2007.10.056 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18191334 }} </ref><ref name="pmid1905691">{{cite journal| author=Cosset JM, Henry-Amar M, Pellae-Cosset B, Carde P, Girinski T, Tubiana M | display-authors=etal| title=Pericarditis and myocardial infarctions after Hodgkin's disease therapy. | journal=Int J Radiat Oncol Biol Phys | year= 1991 | volume= 21 | issue= 2 | pages= 447-9 | pmid=1905691 | doi=10.1016/0360-3016(91)90794-5 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1905691 }} </ref>. | In a retrospective study, 27.7% of the patients developed [[pericardial effusion]] after median time period of 5.3 months following radiotherapy for [[esophageal carcinoma]] with radiation [[dose]] ranging between 3 to 50Gy. It was concluded that high dose-volume of the irradiated [[pericardium]] and heart increased the risk of developing [[pericarditis]]<ref name="pmid18191334">{{cite journal| author=Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD et al.| title=Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy. | journal=Int J Radiat Oncol Biol Phys | year= 2008 | volume= 70 | issue= 3 | pages= 707-14 | pmid=18191334 | doi=10.1016/j.ijrobp.2007.10.056 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18191334 }} </ref><ref name="pmid1905691">{{cite journal| author=Cosset JM, Henry-Amar M, Pellae-Cosset B, Carde P, Girinski T, Tubiana M | display-authors=etal| title=Pericarditis and myocardial infarctions after Hodgkin's disease therapy. | journal=Int J Radiat Oncol Biol Phys | year= 1991 | volume= 21 | issue= 2 | pages= 447-9 | pmid=1905691 | doi=10.1016/0360-3016(91)90794-5 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1905691 }} </ref>. | ||
==Screening== | ==Screening== | ||
Echocardiography is the most commonly used screening modality for the detection and follow-up of radiation-induced cardiac disease. It is typically done every two years in asymptomatic individuals and more frequently when symptoms are present<ref name="urlRadiation Associated Cardiac Disease - American College of Cardiology">{{cite web |url=https://www.acc.org/latest-in-cardiology/articles/2017/06/13/07/13/radiation-associated-cardiac-disease |title=Radiation Associated Cardiac Disease - American College of Cardiology |format= |work= |accessdate=}}</ref>. | [[Echocardiography]] is the most commonly used [[screening]] modality for the detection and follow-up of radiation-induced cardiac disease. It is typically done every two years in [[asymptomatic]] individuals and more frequently when symptoms are present<ref name="urlRadiation Associated Cardiac Disease - American College of Cardiology">{{cite web |url=https://www.acc.org/latest-in-cardiology/articles/2017/06/13/07/13/radiation-associated-cardiac-disease |title=Radiation Associated Cardiac Disease - American College of Cardiology |format= |work= |accessdate=}}</ref>. | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
Acute pericarditis usually develops a few weeks after radiation exposure. Nearly 20% of patients with acute pericarditis develop chronic or constrictive pericarditis in the next 5-10 years following radiation therapy.The risk is increased when pericardial effusion was present previously. Chronic pericarditis can also occur in patients without a history of acute pericarditis<ref name="pmid15900998">{{cite journal| author=Gaya AM, Ashford RF| title=Cardiac complications of radiation therapy. | journal=Clin Oncol (R Coll Radiol) | year= 2005 | volume= 17 | issue= 3 | pages= 153-9 | pmid=15900998 | doi=10.1016/j.clon.2004.09.016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15900998 }} </ref>. | [[Acute pericarditis]] usually develops a few weeks after radiation exposure. Nearly 20% of patients with acute pericarditis develop [[Chronic pericarditis|chronic]] or [[constrictive pericarditis]] in the next 5-10 years following radiation therapy.The risk is increased when [[pericardial effusion]] was present previously. [[Chronic pericarditis]] can also occur in patients without a history of acute pericarditis<ref name="pmid15900998">{{cite journal| author=Gaya AM, Ashford RF| title=Cardiac complications of radiation therapy. | journal=Clin Oncol (R Coll Radiol) | year= 2005 | volume= 17 | issue= 3 | pages= 153-9 | pmid=15900998 | doi=10.1016/j.clon.2004.09.016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15900998 }} </ref>. | ||
==Diagnosis== | ==Diagnosis== | ||
===Diagnostic Study of Choice=== | ===Diagnostic Study of Choice=== | ||
There are no established criteria for radiation induced pericarditis. | There are no established [[criteria]] for radiation induced pericarditis. | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
*Acute pericarditis: | *[[Acute pericarditis]]: [[acute pericarditis]] is a rare [[complication]] of radiation therapy. It presents with nonspecific [[pericarditis]] symptoms such as [[chest pain]] and [[fever]] shortly after radiation therapy<ref name="pmid21403872">{{cite journal| author=Yusuf SW, Sami S, Daher IN| title=Radiation-induced heart disease: a clinical update. | journal=Cardiol Res Pract | year= 2011 | volume= 2011 | issue= | pages= 317659 | pmid=21403872 | doi=10.4061/2011/317659 | pmc=3051159 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21403872 }} </ref><ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | ||
*Delayed pericarditis: | *Delayed [[pericarditis]]: delayed [[pericarditis]] occurs from months to years after exposure to radiation <ref name="pmid4127171">{{cite journal| author=Morton DL, Glancy DL, Joseph WL, Adkins PC| title=Management of patients with radiation-induced pericarditis with effusion: a note on the development of aortic regurgitation in two of them. | journal=Chest | year= 1973 | volume= 64 | issue= 3 | pages= 291-7 | pmid=4127171 | doi=10.1378/chest.64.3.291 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4127171 }} </ref><ref name="pmid7224379">{{cite journal| author=Applefeld MM, Cole JF, Pollock SH, Sutton FJ, Slawson RG, Singleton RT | display-authors=etal| title=The late appearance of chronic pericardial disease in patients treated by radiotherapy for Hodgkin's disease. | journal=Ann Intern Med | year= 1981 | volume= 94 | issue= 3 | pages= 338-41 | pmid=7224379 | doi=10.7326/0003-4819-94-3-338 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7224379 }} </ref>. It usually presents with: | ||
**Chest pain | **[[Chest pain]] | ||
**Dyspnea | **[[Dyspnea]] | ||
**Orthopnea | **[[Orthopnea]] | ||
*Pericardial effusion: | *[[Pericardial effusion]]: protein-rich [[exudate]] may accumulate in the [[pericardial sac]] leading to [[pericardial effusion]]. Rapid accumulation may result in the development of [[cardiac tamponade]] presenting with clinical [[Signs and Symptoms|signs and symptoms]] of [[Cardiac tamponade|tamponade]]<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref><ref name="pmid4127171">{{cite journal| author=Morton DL, Glancy DL, Joseph WL, Adkins PC| title=Management of patients with radiation-induced pericarditis with effusion: a note on the development of aortic regurgitation in two of them. | journal=Chest | year= 1973 | volume= 64 | issue= 3 | pages= 291-7 | pmid=4127171 | doi=10.1378/chest.64.3.291 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4127171 }} </ref>. | ||
*Constrictive pericarditis: | *[[Constrictive pericarditis]]: [[constrictive pericarditis]] is a late [[complication]] of radiation therapy. Patients typically present with [[Symptoms and Signs|signs and symptoms]] of [[heart failure]], similar to other causes of [[constrictive pericarditis]]<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | ||
===Physical Examination=== | ===Physical Examination=== | ||
Physical examination of patients with radiation-induced pericarditis depends on the presentation. In acute pericarditis, the physical examination may show fever and pericardial rub. | [[Physical examination]] of patients with radiation-induced pericarditis depends on the presentation. In [[acute pericarditis]], the [[physical examination]] may show [[fever]] and [[pericardial friction rub]]. In patients presenting with [[Cardiac tamponade|tamponade]], the [[physical examination]] may show: | ||
In patients presenting with tamponade physical examination may show: | *[[Hypotension]] | ||
*Hypotension | *[[Tachycardia]] | ||
*Tachycardia | *[[Jugular venous distention]] with a prominent Y descent | ||
*Jugular venous distention with a prominent Y descent | *[[Kussmaul's sign]], and distant [[heart sounds]] | ||
*Kussmaul's sign, and distant heart sounds | |||
In constrictive pericarditis, signs of congestive heart failure may be present, including: | In [[constrictive pericarditis]], [[signs]] of [[congestive heart failure]] may be present, including: | ||
*Hepatomegaly | *[[Hepatomegaly]] | ||
*Ascites | *[[Ascites]] | ||
*Ankle edema <ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref> | *[[Ankle edema]] <ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref> | ||
===Laboratory Findings=== | ===Laboratory Findings=== | ||
Laboratory findings consistent with the diagnosis of radiation-induced acute pericarditis include elevated inflammatory markers such as neutrophil count and erythrocyte sedimentation rate (ESR)<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | [[Laboratory]] findings consistent with the diagnosis of radiation-induced [[acute pericarditis]] include elevated inflammatory markers such as [[Absolute neutrophil count|neutrophil count]] and [[erythrocyte sedimentation rate]] (ESR)<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | ||
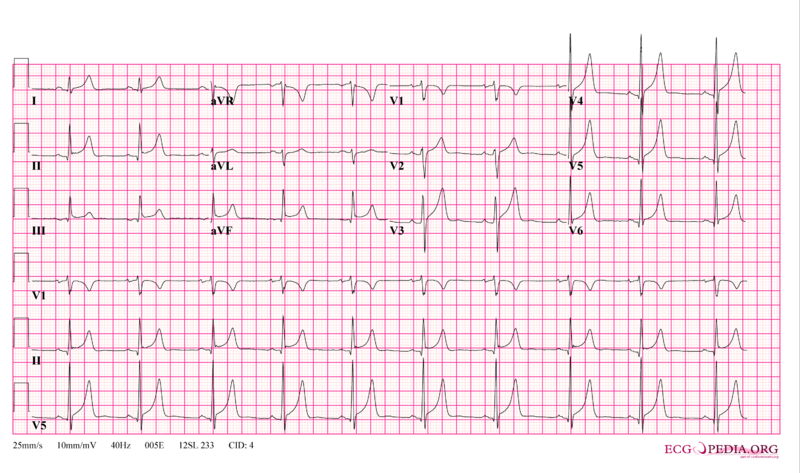
===Electrocardiogram=== | ===Electrocardiogram=== | ||
In acute pericarditis, non-specific ST and T wave changes or ST segment elevation in all leads may be noted<ref name="pmid21403872">{{cite journal| author=Yusuf SW, Sami S, Daher IN| title=Radiation-induced heart disease: a clinical update. | journal=Cardiol Res Pract | year= 2011 | volume= 2011 | issue= | pages= 317659 | pmid=21403872 | doi=10.4061/2011/317659 | pmc=3051159 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21403872 }} </ref><ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | In [[acute pericarditis]], [[Nonspecific ST-Segment and T-Wave Changes|non-specific ST and T wave changes]] or [[ST segment elevation]] in all leads may be noted<ref name="pmid21403872">{{cite journal| author=Yusuf SW, Sami S, Daher IN| title=Radiation-induced heart disease: a clinical update. | journal=Cardiol Res Pract | year= 2011 | volume= 2011 | issue= | pages= 317659 | pmid=21403872 | doi=10.4061/2011/317659 | pmc=3051159 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21403872 }} </ref><ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref>. | ||
[[Image:12leadpericarditis.png|thumb|400px|left|Acute pericarditis]] | [[Image:12leadpericarditis.png|thumb|400px|left|Acute pericarditis]] | ||
<br clear="left"/> | <br clear="left"/> | ||
In patients presenting with constrictive pericarditis, electrocardiographic changes are similar to other causes of constrictive pericarditis. Electrocardiographic signs of constrictive | In patients presenting with [[constrictive pericarditis]], [[electrocardiographic]] changes are similar to other causes of [[constrictive pericarditis]]. [[Electrocardiographic]] [[signs]] of [[constrictive pericarditis]] is usually inconsistent and non specific<ref name="pmid1258748">{{cite journal| author=Chesler E, Mitha AS, Matisonn RE| title=The ECG of constrictive pericarditis--pattern resembling right ventricular hypertrophy. | journal=Am Heart J | year= 1976 | volume= 91 | issue= 4 | pages= 420-4 | pmid=1258748 | doi=10.1016/s0002-8703(76)80321-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1258748 }}</ref> | ||
* Left atrial enlargement | *[[Left atrial enlargement]] | ||
* Frequent atrial arrhythmias | * Frequent [[atrial arrhythmias]] | ||
* Right axis deflection | * Right axis deflection | ||
* Possible reduction in voltages | * Possible reduction in [[Voltage|voltages]] | ||
* Diffuse negative T-waves | * Diffuse negative [[T wave|T-waves]] | ||
*Typical (normal QRS axis, low voltage, and generalized T wave flattening or inversion) | *Typical (normal QRS axis, low voltage, and generalized [[T wave]] flattening or inversion) | ||
*Right ventricular hypertrophy | *[[Right ventricular hypertrophy]] | ||
*Right axis deviation | *[[Right axis deviation]] | ||
===X-ray=== | ===X-ray=== | ||
A chest x-ray may be helpful in the diagnosis of radiation-induced pericarditis<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref> | A [[Chest X-ray|chest x-ray]] may be helpful in the diagnosis of radiation-induced pericarditis. Findings on an [[x-ray]] suggestive of [[chronic pericarditis]] include [[pericardial effusion]] and [[pericardial]] thickening<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref>. | ||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
Echocardiography is the gold standard for definitive diagnosis of acute or chronic pericarditis with pericardial effusion and helps to rule out a cardiac tamponade<ref name=" | [[Echocardiography]] is the gold standard for definitive diagnosis of [[Acute pericarditis|acute]] or [[chronic pericarditis]] with [[pericardial effusion]] and helps to rule out a [[cardiac tamponade]]<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref><ref name="pmid26691443">{{cite journal| author=Yusuf SW, Hassan SA, Mouhayar E, Negi SI, Banchs J, O'Gara PT| title=Pericardial disease: a clinical review. | journal=Expert Rev Cardiovasc Ther | year= 2016 | volume= 14 | issue= 4 | pages= 525-39 | pmid=26691443 | doi=10.1586/14779072.2016.1134317 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26691443 }} </ref>. | ||
===CT scan=== | ===CT scan=== | ||
A chest CT scan may be helpful in the diagnosis of radiation-induced pericarditis<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref> | A chest [[CT scan]] may be helpful in the diagnosis of radiation-induced pericarditis. Findings on a [[CT scan]] suggestive of [[chronic pericarditis]] include [[pericardial effusion]] and [[pericardial]] thickening<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref>. | ||
===MRI=== | ===MRI=== | ||
Cardiac MRI may be helpful in the diagnosis of radiation-induced pericarditis. It is useful to confirm the pericardial thickening in chronic and constrictive pericarditis. It is also helpful to assess for concomitant myocardial involvement<ref name="pmidDOI: 10.1016/j.jacc.2013.01.090">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=DOI: 10.1016/j.jacc.2013.01.090 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref>. | [[Cardiac MRI]] may be helpful in the diagnosis of radiation-induced pericarditis. It is useful to confirm the [[pericardial]] thickening in [[Chronic pericarditis|chronic]] and [[constrictive pericarditis]]. It is also helpful to assess for concomitant [[myocardial]] involvement<ref name="pmid28139844">{{cite journal| author=Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW| title=Short and long term radiation induced cardiovascular disease in patients with cancer. | journal=Clin Cardiol | year= 2017 | volume= 40 | issue= 4 | pages= 255-261 | pmid=28139844 | doi=10.1002/clc.22634 | pmc=6589645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28139844 }} </ref><ref name="pmidDOI: 10.1016/j.jacc.2013.01.090">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=DOI: 10.1016/j.jacc.2013.01.090 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref>. | ||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
| Line 199: | Line 199: | ||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
Cardiac catheterization may be helpful in the diagnosis of constrictive pericarditis associated with radiation therapy. | [[Cardiac catheterization]] may be helpful in the diagnosis of [[constrictive pericarditis]] associated with radiation therapy. | ||
For more information on cardiac catheterization findings in constrictive pericarditis, click '''[[Constrictive pericarditis cardiac catheterization|here]].''' | For more information on [[cardiac catheterization]] findings in [[constrictive pericarditis]], click '''[[Constrictive pericarditis cardiac catheterization|here]].''' | ||
===Pericardiocentesis=== | ===Pericardiocentesis=== | ||
* Radiation induced [[pericardial effusion]] can be confused with [[malignant pericarditis]] and [[hypothyroidism]] | * Radiation induced [[pericardial effusion]] can be confused with [[malignant pericarditis]] and [[hypothyroidism]]-induced pericarditis. | ||
* [[Pericardiocentesis]] can be used to differentiate them with fluid analysis for malignant cells and thyroid function tests. | * [[Pericardiocentesis]] can be used to differentiate them with fluid analysis for malignant cells and [[thyroid function tests]]. | ||
* For more information on pericardiocentesis, click '''[[Pericardiocentesis|here]].''' | * For more information on [[pericardiocentesis]], click '''[[Pericardiocentesis|here]].''' | ||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
The majority of radiation-induced acute | The majority of radiation-induced [[acute pericarditis]] cases are self-limited and respond well to [[nonsteroidal anti-inflammatory drugs]] and [[colchicine]]<ref name="pmid29124057">{{cite journal| author=Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S| title=Radiation-Induced Cardiovascular Disease: A Clinical Perspective. | journal=Front Cardiovasc Med | year= 2017 | volume= 4 | issue= | pages= 66 | pmid=29124057 | doi=10.3389/fcvm.2017.00066 | pmc=5662579 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29124057 }} </ref><ref name="pmid20159360">{{cite journal| author=Darby SC, Cutter DJ, Boerma M, Constine LS, Fajardo LF, Kodama K | display-authors=etal| title=Radiation-related heart disease: current knowledge and future prospects. | journal=Int J Radiat Oncol Biol Phys | year= 2010 | volume= 76 | issue= 3 | pages= 656-65 | pmid=20159360 | doi=10.1016/j.ijrobp.2009.09.064 | pmc=3910096 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20159360 }} </ref>. [[Steroids]] are associated with a higher chance of [[relapse]] and therefore are only used in cases who fail to respond to [[nonsteroidal anti-inflammatory agents]]<ref name="pmid26691443">{{cite journal| author=Yusuf SW, Hassan SA, Mouhayar E, Negi SI, Banchs J, O'Gara PT| title=Pericardial disease: a clinical review. | journal=Expert Rev Cardiovasc Ther | year= 2016 | volume= 14 | issue= 4 | pages= 525-39 | pmid=26691443 | doi=10.1586/14779072.2016.1134317 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26691443 }} </ref>. | ||
===Surgery=== | ===Surgery=== | ||
*Pericarditis with large effusion can be drained either percutaneously or surgically. | *Pericarditis with large effusion can be drained either [[percutaneously]] or surgically. | ||
*Those with recurrent pericardial effusion can be treated with [[pericardiotomy]](pericardial window) or by surgical stripping. | *Those with recurrent [[pericardial effusion]] can be treated with [[pericardiotomy]] ([[pericardial window]]) or by surgical [[stripping]]. | ||
*[[Pericardiectomy]] is recommended for patients who develop [[constrictive pericarditis]]. However, the perioperative mortality rate is higher in | *[[Pericardiectomy]] is recommended for patients who develop [[constrictive pericarditis]]. However, the [[perioperative]] [[mortality rate]] is higher in radiation-induced [[constrictive pericarditis]] compared to that of [[idiopathic]] [[constrictive pericarditis]]<ref name="pmid15093882">{{cite journal| author=Bertog SC, Thambidorai SK, Parakh K, Schoenhagen P, Ozduran V, Houghtaling PL et al.| title=Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. | journal=J Am Coll Cardiol | year= 2004 | volume= 43 | issue= 8 | pages= 1445-52 | pmid=15093882 | doi=10.1016/j.jacc.2003.11.048 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15093882 }} </ref>. | ||
===Primary Prevention=== | ===Primary Prevention=== | ||
Effective measures for the primary prevention of radiation-induced pericarditis include reducing the dose and volume of cardiac irradiation when possible<ref name="pmid26628476">{{cite journal| author=Maraldo MV, Ng AK| title=Minimizing Cardiac Risks With Contemporary Radiation Therapy for Hodgkin Lymphoma. | journal=J Clin Oncol | year= 2016 | volume= 34 | issue= 3 | pages= 208-10 | pmid=26628476 | doi=10.1200/JCO.2015.64.6588 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26628476 }} </ref>. | Effective measures for the [[primary prevention]] of radiation-induced pericarditis include reducing the [[dose]] and volume of cardiac [[irradiation]] when possible<ref name="pmid26628476">{{cite journal| author=Maraldo MV, Ng AK| title=Minimizing Cardiac Risks With Contemporary Radiation Therapy for Hodgkin Lymphoma. | journal=J Clin Oncol | year= 2016 | volume= 34 | issue= 3 | pages= 208-10 | pmid=26628476 | doi=10.1200/JCO.2015.64.6588 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26628476 }} </ref>. | ||
===Secondary Prevention=== | ===Secondary Prevention=== | ||
There are no established measures for the secondary prevention of radiation-induced pericarditis. | There are no established measures for the [[secondary prevention]] of radiation-induced pericarditis. | ||
==References== | ==References== | ||
Latest revision as of 17:27, 4 June 2020
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Radiation induced pericarditis On the Web |
|
American Roentgen Ray Society Images of Radiation induced pericarditis |
|
Risk calculators and risk factors for Radiation induced pericarditis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-In-Chief: Mandana Chitsazan, M.D. [3]; Varun Kumar, M.B.B.S.; Lakshmi Gopalakrishnan, M.B.B.S.
Overview
The survival rate in Hodgkin lymphoma, Non-Hodgkin's lymphoma and breast carcinomas has significantly improved with use of radiation therapy.However, radiation therapy to thoracic and mediastinal cancers have also led to the development of pericarditis, coronary artery disease, cardiomyopathy, conduction abnormalities in heart and valvular heart diseases which account for significant morbidity and mortality. Radiation-induced pericarditis was first described in the mid-1960s. The radiation-induced pericardial disease may be classified as acute pericarditis, delayed pericarditis, pancarditis, constrictive pericarditis, and pericardial effusion. Radiation therapy leads to disruption of endothelium and subsequent episodes of ischemia. The resulting fibrosis and fibrinous exudates replace collagen fibers. Radiation-induced pericardial disease can occur in any cancer survivor who receive thoracic radiation therapy, including breast cancer, Hodgkin's lymphoma, esophageal cancer, and lung cancer. Radiation-induced pericarditis depends on the total dose of radiation, the dose per fraction, the amount of cardiac silhouette exposed, and the nature of the radiation source. The incidence is higher with doses greater than 40 Gy (4000 rad). Echocardiography is the most commonly used screening modality for the detection and follow-up of radiation-induced cardiac disease. Acute pericarditis usually develops a few weeks after radiation exposure. Nearly 20% of patients with acute pericarditis develop chronic or constrictive pericarditis in the next 5-10 years following radiation therapy. The risk is increased when pericardial effusion was present previously. Chronic pericarditis can also occur in patients without a history of acute pericarditis. Acute pericarditis is a rare complication of radiation therapy. It presents with nonspecific pericarditis symptoms such as chest pain and fever shortly after radiation therapy. Delayed pericarditis occurs from months to years after exposure to radiation. It usually presents with chest pain, dyspnea, and orthopnea. The physical examination may show fever and pericardial rub. Laboratory findings include elevated inflammatory markers such as neutrophil count and erythrocyte sedimentation rate (ESR). On ECG, non-specific ST and T wave changes or ST-segment elevation in all leads may be noted. The majority of acute pericarditis cases are self-limited and respond well to nonsteroidal anti-inflammatory drugs and colchicine. In acute or chronic pericarditis, protein-rich exudate may accumulate in the pericardial sac leading to pericardial effusion. Findings on a chest x-ray or chest CT suggestive of chronic pericarditis include pericardial effusion and pericardial thickening. If the effusion is large enough, it may lead to tamponade. In patients presenting with tamponade, the physical examination may show hypotension, tachycardia, and jugular venous distention with a prominent Y descent, Kussmaul’s sign, and distant heart sound. Radiation-induced pericardial effusion can be confused with malignant pericarditis and hypothyroidism-induced pericarditis. Pericarditis with large effusion can be drained either percutaneously or surgically. Those with recurrent pericardial effusion can be treated with pericardiotomy(pericardial window) or by surgical stripping. Constrictive pericarditis is a late complication of radiation therapy. Patients typically present with signs and symptoms of heart failure, similar to other causes of constrictive pericarditis. Cardiac MRI may be helpful in the diagnosis of constrictive pericarditis. It is useful to confirm the pericardial thickening. Cardiac catheterization may be also helpful in the diagnosis of constrictive pericarditis associated with radiation therapy. Pericardiectomy is recommended for patients who develop constrictive pericarditis. However, the perioperative mortality rate is higher in radiation-induced constrictive pericarditis compared to that of idiopathic constrictive pericarditis. Effective measures for the primary prevention of radiation-induced pericarditis include reducing the dose and volume of cardiac irradiation when possible.
Historical Perspective
Radiation-induced pericarditis was first described in the mid-1960s[1].
Classification
Based on the presentation and onset of symptoms, the radiation-induced pericardial disease may be classified as:[2]
- Acute pericarditis
- Delayed pericarditis
- Pancarditis
- Constrictive pericarditis
- Pericardial effusion
Pathophysiology
Radiation therapy disrupts endothelial cells of the microvasculature of the pericardium and leads to repeated episodes of ischemia. The final result is the formation of fibrosis and fibrinous exudates that are ultimately replaced by fibroblasts and collagen fibers [3][4][5][6].
Causes
Radiation-induced pericardial disease can occur in any cancer survivor who receive thoracic radiation therapy, including breast cancer, Hodgkin's lymphoma, esophageal cancer, and lung cancer. However, most data come from patients treated for breast cancer and Hodgkin's lymphoma, in which radiation therapy is a frequent component of management.
Differentiating Radiation-induced Pericarditis from other Diseases
- Pericarditis must be differentiated from diseases presenting with chest pain, shortness of breath and tachypnea.
- For a full discussion of the differential diagnosis of chest pain click here
- For an expert algorithm that aids in the diagnosis of the cause of chest pain click here
- Pericarditis must be differentiated from myocardial infarction as an important cause of chest pain.The differentiating features include:[7]
| Characteristic/Parameter | Pericarditis | Myocardial infarction |
|---|---|---|
| Pain description | Sharp, pleuritic, retro-sternal (under the sternum) or left precordial (left chest) pain. | Crushing, pressure-like, heavy pain. Described as "elephant on the chest". |
| Radiation | Pain radiates to the trapezius ridge (to the lowest portion of the scapula on the back) or no radiation. | Pain radiates to the jaw, or the left or arm, or does not radiate. |
| Exertion | Does not change the pain | Can increase the pain |
| Position | Pain is worse supine or upon inspiration (breathing in) | Not positional |
| Onset/duration | Sudden pain, that lasts for hours or sometimes days before a patient comes to the ER | Sudden or chronically worsening pain that can come and go in paroxysms or it can last for hours before the patient decides to come to the ER |
- Constrictive pericarditis should be differentiated from restrictive cardiomyopathy[8][9]:
| Type of disease | History and Physical examination | Chest X-ray and ECG | 2D and Doppler echo | CT and MRI | Catheterization hemodynamics | Biopsy |
| Constrictive pericarditis[10][11] |
|
|
|
|
|
Normal myocardium |
| Restrictive cardiomyopathy[8][9][12] |
|
|
|
|
May reveal underlying cause |
Epidemiology and Demographics
Pericardial changes are the most common cardiac complications of radiation therapy[4]. Incidence of radiation-induced pericarditis has significantly decreased with the use of lower doses and newer radiotherapy techniques [13][14][15]. In a study, incidence decreased from 20% to 2.5% with the changes in methods of RT administration[13]
In a study among pediatric population with various cancers, radiation therapy with ≥15 GY increased the risk of developing pericarditis by two to six times[16]
Risk Factors
Radiation-induced pericarditis depends on:
- Total dose of radiation
- The dose per fraction
- Amount of cardiac silhouette exposed
- Nature of the radiation source
In a retrospective study, 27.7% of the patients developed pericardial effusion after median time period of 5.3 months following radiotherapy for esophageal carcinoma with radiation dose ranging between 3 to 50Gy. It was concluded that high dose-volume of the irradiated pericardium and heart increased the risk of developing pericarditis[17][18].
Screening
Echocardiography is the most commonly used screening modality for the detection and follow-up of radiation-induced cardiac disease. It is typically done every two years in asymptomatic individuals and more frequently when symptoms are present[19].
Natural History, Complications, and Prognosis
Acute pericarditis usually develops a few weeks after radiation exposure. Nearly 20% of patients with acute pericarditis develop chronic or constrictive pericarditis in the next 5-10 years following radiation therapy.The risk is increased when pericardial effusion was present previously. Chronic pericarditis can also occur in patients without a history of acute pericarditis[20].
Diagnosis
Diagnostic Study of Choice
There are no established criteria for radiation induced pericarditis.
History and Symptoms
- Acute pericarditis: acute pericarditis is a rare complication of radiation therapy. It presents with nonspecific pericarditis symptoms such as chest pain and fever shortly after radiation therapy[2][4].
- Delayed pericarditis: delayed pericarditis occurs from months to years after exposure to radiation [21][22]. It usually presents with:
- Pericardial effusion: protein-rich exudate may accumulate in the pericardial sac leading to pericardial effusion. Rapid accumulation may result in the development of cardiac tamponade presenting with clinical signs and symptoms of tamponade[4][21].
- Constrictive pericarditis: constrictive pericarditis is a late complication of radiation therapy. Patients typically present with signs and symptoms of heart failure, similar to other causes of constrictive pericarditis[4].
Physical Examination
Physical examination of patients with radiation-induced pericarditis depends on the presentation. In acute pericarditis, the physical examination may show fever and pericardial friction rub. In patients presenting with tamponade, the physical examination may show:
- Hypotension
- Tachycardia
- Jugular venous distention with a prominent Y descent
- Kussmaul's sign, and distant heart sounds
In constrictive pericarditis, signs of congestive heart failure may be present, including:
Laboratory Findings
Laboratory findings consistent with the diagnosis of radiation-induced acute pericarditis include elevated inflammatory markers such as neutrophil count and erythrocyte sedimentation rate (ESR)[4].
Electrocardiogram
In acute pericarditis, non-specific ST and T wave changes or ST segment elevation in all leads may be noted[2][4].
In patients presenting with constrictive pericarditis, electrocardiographic changes are similar to other causes of constrictive pericarditis. Electrocardiographic signs of constrictive pericarditis is usually inconsistent and non specific[23]
- Left atrial enlargement
- Frequent atrial arrhythmias
- Right axis deflection
- Possible reduction in voltages
- Diffuse negative T-waves
- Typical (normal QRS axis, low voltage, and generalized T wave flattening or inversion)
- Right ventricular hypertrophy
- Right axis deviation
X-ray
A chest x-ray may be helpful in the diagnosis of radiation-induced pericarditis. Findings on an x-ray suggestive of chronic pericarditis include pericardial effusion and pericardial thickening[24].
Echocardiography or Ultrasound
Echocardiography is the gold standard for definitive diagnosis of acute or chronic pericarditis with pericardial effusion and helps to rule out a cardiac tamponade[24][25].
CT scan
A chest CT scan may be helpful in the diagnosis of radiation-induced pericarditis. Findings on a CT scan suggestive of chronic pericarditis include pericardial effusion and pericardial thickening[24].
MRI
Cardiac MRI may be helpful in the diagnosis of radiation-induced pericarditis. It is useful to confirm the pericardial thickening in chronic and constrictive pericarditis. It is also helpful to assess for concomitant myocardial involvement[24][26].
Other Imaging Findings
There are no other imaging findings associated with radiation-induced pericarditis.
Other Diagnostic Studies
Cardiac catheterization may be helpful in the diagnosis of constrictive pericarditis associated with radiation therapy.
For more information on cardiac catheterization findings in constrictive pericarditis, click here.
Pericardiocentesis
- Radiation induced pericardial effusion can be confused with malignant pericarditis and hypothyroidism-induced pericarditis.
- Pericardiocentesis can be used to differentiate them with fluid analysis for malignant cells and thyroid function tests.
- For more information on pericardiocentesis, click here.
Treatment
Medical Therapy
The majority of radiation-induced acute pericarditis cases are self-limited and respond well to nonsteroidal anti-inflammatory drugs and colchicine[4][27]. Steroids are associated with a higher chance of relapse and therefore are only used in cases who fail to respond to nonsteroidal anti-inflammatory agents[25].
Surgery
- Pericarditis with large effusion can be drained either percutaneously or surgically.
- Those with recurrent pericardial effusion can be treated with pericardiotomy (pericardial window) or by surgical stripping.
- Pericardiectomy is recommended for patients who develop constrictive pericarditis. However, the perioperative mortality rate is higher in radiation-induced constrictive pericarditis compared to that of idiopathic constrictive pericarditis[28].
Primary Prevention
Effective measures for the primary prevention of radiation-induced pericarditis include reducing the dose and volume of cardiac irradiation when possible[29].
Secondary Prevention
There are no established measures for the secondary prevention of radiation-induced pericarditis.
References
- ↑ "Radiation-Induced CAD: Incidence, Diagnosis, and Management Outcomes - American College of Cardiology".
- ↑ 2.0 2.1 2.2 Yusuf SW, Sami S, Daher IN (2011). "Radiation-induced heart disease: a clinical update". Cardiol Res Pract. 2011: 317659. doi:10.4061/2011/317659. PMC 3051159. PMID 21403872.
- ↑ Fajardo LF (1989). "The unique physiology of endothelial cells and its implications in radiobiology". Front Radiat Ther Oncol. 23: 96–112. doi:10.1159/000416574. PMID 2697671.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Yusuf SW, Venkatesulu BP, Mahadevan LS, Krishnan S (2017). "Radiation-Induced Cardiovascular Disease: A Clinical Perspective". Front Cardiovasc Med. 4: 66. doi:10.3389/fcvm.2017.00066. PMC 5662579. PMID 29124057.
- ↑ Taunk NK, Haffty BG, Kostis JB, Goyal S (2015). "Radiation-induced heart disease: pathologic abnormalities and putative mechanisms". Front Oncol. 5: 39. doi:10.3389/fonc.2015.00039. PMC 4332338. PMID 25741474.
- ↑ Hooning MJ, Aleman BM, van Rosmalen AJ, Kuenen MA, Klijn JG, van Leeuwen FE (2006). "Cause-specific mortality in long-term survivors of breast cancer: A 25-year follow-up study". Int J Radiat Oncol Biol Phys. 64 (4): 1081–91. doi:10.1016/j.ijrobp.2005.10.022. PMID 16446057.
- ↑ American College of Physicians (ACP). Medical Knowledge Self-Assessment Program (MKSAP-15): Cardiovascular Medicine. "Pericardial disease." p. 64. ISBN 978-934465-28-8 [1]
- ↑ 8.0 8.1 Rammos A, Meladinis V, Vovas G, Patsouras D (2017). "Restrictive Cardiomyopathies: The Importance of Noninvasive Cardiac Imaging Modalities in Diagnosis and Treatment-A Systematic Review". Radiol Res Pract. 2017: 2874902. doi:10.1155/2017/2874902. PMC 5705874. PMID 29270320.
- ↑ 9.0 9.1 Hong JA, Kim MS, Cho MS, Choi HI, Kang DH, Lee SE, Lee GY, Jeon ES, Cho JY, Kim KH, Yoo BS, Lee JY, Kim WJ, Kim KH, Chung WJ, Lee JH, Cho MC, Kim JJ (September 2017). "Clinical features of idiopathic restrictive cardiomyopathy: A retrospective multicenter cohort study over 2 decades". Medicine (Baltimore). 96 (36): e7886. doi:10.1097/MD.0000000000007886. PMC 6393124. PMID 28885342.
- ↑ Ramasamy V, Mayosi BM, Sturrock ED, Ntsekhe M (September 2018). "Established and novel pathophysiological mechanisms of pericardial injury and constrictive pericarditis". World J Cardiol. 10 (9): 87–96. doi:10.4330/wjc.v10.i9.87. PMC 6189073. PMID 30344956.
- ↑ Biçer M, Özdemir B, Kan İ, Yüksel A, Tok M, Şenkaya I (November 2015). "Long-term outcomes of pericardiectomy for constrictive pericarditis". J Cardiothorac Surg. 10: 177. doi:10.1186/s13019-015-0385-8. PMC 4662820. PMID 26613929.
- ↑ Mogensen J, Kubo T, Duque M, Uribe W, Shaw A, Murphy R, Gimeno JR, Elliott P, McKenna WJ (January 2003). "Idiopathic restrictive cardiomyopathy is part of the clinical expression of cardiac troponin I mutations". J. Clin. Invest. 111 (2): 209–16. doi:10.1172/JCI16336. PMC 151864. PMID 12531876.
- ↑ 13.0 13.1 Carmel RJ, Kaplan HS (1976). "Mantle irradiation in Hodgkin's disease. An analysis of technique, tumor eradication, and complications". Cancer. 37 (6): 2813–25. doi:10.1002/1097-0142(197606)37:6<2813::aid-cncr2820370637>3.0.co;2-s. PMID 949701.
- ↑ Maisch B, Ristić AD (2003). "Practical aspects of the management of pericardial disease". Heart. 89 (9): 1096–103. PMC 1767862. PMID 12923044.
- ↑ Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Mulrooney DA, Yeazel MW, Kawashima T, Mertens AC, Mitby P, Stovall M; et al. (2009). "Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: retrospective analysis of the Childhood Cancer Survivor Study cohort". BMJ. 339: b4606. doi:10.1136/bmj.b4606. PMID 19996459.
- ↑ Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD; et al. (2008). "Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy". Int J Radiat Oncol Biol Phys. 70 (3): 707–14. doi:10.1016/j.ijrobp.2007.10.056. PMID 18191334.
- ↑ Cosset JM, Henry-Amar M, Pellae-Cosset B, Carde P, Girinski T, Tubiana M; et al. (1991). "Pericarditis and myocardial infarctions after Hodgkin's disease therapy". Int J Radiat Oncol Biol Phys. 21 (2): 447–9. doi:10.1016/0360-3016(91)90794-5. PMID 1905691.
- ↑ "Radiation Associated Cardiac Disease - American College of Cardiology".
- ↑ Gaya AM, Ashford RF (2005). "Cardiac complications of radiation therapy". Clin Oncol (R Coll Radiol). 17 (3): 153–9. doi:10.1016/j.clon.2004.09.016. PMID 15900998.
- ↑ 21.0 21.1 Morton DL, Glancy DL, Joseph WL, Adkins PC (1973). "Management of patients with radiation-induced pericarditis with effusion: a note on the development of aortic regurgitation in two of them". Chest. 64 (3): 291–7. doi:10.1378/chest.64.3.291. PMID 4127171.
- ↑ Applefeld MM, Cole JF, Pollock SH, Sutton FJ, Slawson RG, Singleton RT; et al. (1981). "The late appearance of chronic pericardial disease in patients treated by radiotherapy for Hodgkin's disease". Ann Intern Med. 94 (3): 338–41. doi:10.7326/0003-4819-94-3-338. PMID 7224379.
- ↑ Chesler E, Mitha AS, Matisonn RE (1976). "The ECG of constrictive pericarditis--pattern resembling right ventricular hypertrophy". Am Heart J. 91 (4): 420–4. doi:10.1016/s0002-8703(76)80321-3. PMID 1258748.
- ↑ 24.0 24.1 24.2 24.3 Nielsen KM, Offersen BV, Nielsen HM, Vaage-Nilsen M, Yusuf SW (2017). "Short and long term radiation induced cardiovascular disease in patients with cancer". Clin Cardiol. 40 (4): 255–261. doi:10.1002/clc.22634. PMC 6589645 Check
|pmc=value (help). PMID 28139844. - ↑ 25.0 25.1 Yusuf SW, Hassan SA, Mouhayar E, Negi SI, Banchs J, O'Gara PT (2016). "Pericardial disease: a clinical review". Expert Rev Cardiovasc Ther. 14 (4): 525–39. doi:10.1586/14779072.2016.1134317. PMID 26691443.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID 10.1016/j.jacc.2013.01.090 DOI: 10.1016/j.jacc.2013.01.090 Check
|pmid=value (help). - ↑ Darby SC, Cutter DJ, Boerma M, Constine LS, Fajardo LF, Kodama K; et al. (2010). "Radiation-related heart disease: current knowledge and future prospects". Int J Radiat Oncol Biol Phys. 76 (3): 656–65. doi:10.1016/j.ijrobp.2009.09.064. PMC 3910096. PMID 20159360.
- ↑ Bertog SC, Thambidorai SK, Parakh K, Schoenhagen P, Ozduran V, Houghtaling PL; et al. (2004). "Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy". J Am Coll Cardiol. 43 (8): 1445–52. doi:10.1016/j.jacc.2003.11.048. PMID 15093882.
- ↑ Maraldo MV, Ng AK (2016). "Minimizing Cardiac Risks With Contemporary Radiation Therapy for Hodgkin Lymphoma". J Clin Oncol. 34 (3): 208–10. doi:10.1200/JCO.2015.64.6588. PMID 26628476.
- Pages with reference errors
- CS1 maint: Multiple names: authors list
- CS1 maint: PMC format
- CS1 maint: Explicit use of et al.
- CS1 errors: PMC
- CS1 errors: PMID
- Cardiology
- Intensive care medicine
- Emergency medicine
- Radiation health effects
- Diseases involving the fasciae
- Up-To-Date
- Up-To-Date cardiology
- Disease
- Best pages