Pneumonia
Editor(s)-in-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753; Philip Marcus, M.D., M.P.H.[2]{{#meta: itemprop="medicalWebPageAudiences" content="patient"}}{{#meta: itemprop="medicalWebPageSpecialities" content="cardiology"}}{{#meta: itemprop="medicalWebPageInfoTypes" content="symptoms,diagnosis,treatment,causes,prognosis,complications"}} [[Natural Progression::{{{naturalProgression}}}| ]] Classification Classic::Classification Atypical::
Overview
| https://https://www.youtube.com/watch?v=X-CnwZDXr9g%7C350}} |
|
Pneumonia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumonia On the Web |
|
American Roentgen Ray Society Images of Pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [4], Priyamvada Singh, M.D. [5], Alejandro Lemor, M.D. [6]
Overview
Pneumonia is an illness of the lungs and respiratory system in which the alveoli (microscopic air-filled sacs of the lung responsible for absorbing oxygen from the atmosphere) become inflamed and flooded with fluid. Pneumonia can result from a variety of causes, including infection with bacteria, viruses, fungi, parasites, and chemical or physical injury to the lungs. Typical symptoms associated with pneumonia include cough, chest pain, fever, and difficulty in breathing. Diagnostic tools include x-rays and an examination of the sputum. Treatment depends on the cause of pneumonia; bacterial pneumonia is treated with antibiotics. Pneumonia is a common illness which occurs in all age groups, and is a leading cause of death among the elderly and people who are chronically and terminally ill. Vaccines to prevent certain types of pneumonia are available. The prognosis depends on the type of pneumonia, the appropriate treatment, any complications, and the person's underlying health.
Historical Perspective
Pneumonia has been recognized since ancient times. It was initally described by Hippocrates who recorded his observations of its symptoms and complications. Edwin Klebs was the first to identify bacteria in the lungs of patients who died from pneumonia in 1875. This discovery was soon-after substantiated by the works of Carl Friedländer and Albert Fränkel who were the first to identify Streptococcus pneumoniae as a causative agent. The introduction of the gram stain subsequently led to the discovery of other causative organisms. Despite being an important cause of mortality before the late twentieth century, the advent of antibiotics, modern surgical techniques, and vaccination drastically lowered the morbidity and mortality of pneumonia with the turn of the century.
Classification
Several pneumonia classification schemes have been described. The earliest classification was based on the anatomical distribution of the infectious process observed on autopsy and eventually on medical imaging. Advances in microbiology led to a classification based on etiologic group (bacterial, viral, fungal) despite difficulties often encountered in identifying the etiologic agent. With the advent of antibiotics and the rise in resistance, a classification scheme taking into account the setting in which the pneumonia was acquired was introduced to guide empiric therapy. Pneumonia was classified into community-acquired pneumonia (CAP), healthcare-associated pneumonia (HCAP), ventilator-associated pneumonia (VAP), and hospital-acquired pneumonia (HAP). Despite significant overlap, this classification is essential in selecting appropriate antimicrobial therapy.
Pathophysiology
Bacteria and fungi typically enter the lung with inhalation. Once inside the alveoli, these microbes travel into the spaces between the cells and also between adjacent alveoli through connecting pores. This invasion triggers the immune system response by sending white blood cells responsible for attacking microorganisms (neutrophils) to the lungs resulting in manifestations of pneumonia.
Causes
Pneumonia can result from a variety of causes including infection with bacteria, viruses, fungi, parasites, and chemical or physical injury to the lungs. The etiology will depend upon various factors such as age, immune status, geographical area, and comorbidities.
Epidemiology and Demographics
Pneumonia is a common illness in all parts of the world. It is a major cause of death among all age groups. Mortality from pneumonia generally decreases with age until late adulthood. Elderly individuals, however, are at particular risk for pneumonia and associated mortality. More cases of pneumonia occur during the winter months than during other times of the year. Pneumonia occurs more commonly in males than females, and more often in African Americans than Caucasians. People who are hospitalized for any reason are also at high risk for pneumonia. Following urinary tract infections, pneumonia is the second most common cause of nosocomial infections, and its prevalence is 15-20% of the total number.
Risk Factors
The risk factors for pneumonia include smoking, age, immuno-suppression, exposure to chemicals, underlying lung disease, and exposure to chemicals.
Diagnosis
Diagnostic Criteria
Community acquired pneumonia should be distinguished from healthcare-associated pneumonia as these diseases have different causative organism, prognosis, diagnostic, and treatment guidelines.
History and Symptoms
People with pneumonia often have a productive cough, fever, shaking chills, shortness of breath, pleuritic chest pain,hemoptysis, headaches, diaphoresis, and clammy skin. Other possible symptoms are loss of appetite, fatigue,blueness of the skin, nausea, vomiting, mood swings, andjoint pains or muscle aches. In elderly people manifestations of pneumonia may not be typical. They may develop a new or worsening confusion or may experience unsteadiness, leading to falls. Infants with pneumonia may have many of the symptoms above, but in many cases they are simply sleepy or have a decreased appetite.
Physical Examination
Physical examination may reveal fever or sometimes low body temperature, an increased respiratory rate, low blood pressure, a fast heart rate, or a low oxygen saturation, which is the amount of oxygen in the blood as indicated by either pulse oximetry or blood gas analysis. Patients who are struggling to breathe, who are confused, or who have cyanosis (blue-tinged skin) require immediate attention. Auscultation findings include lack of normal breath sounds, the presence of crackling sounds (rales), or increased loudness of whispered speech (whispered pectoriloquy) with areas of the lung that are stiff and full of fluid, called consolidation. Vital signs are useful in determining the severity of illness and have predictive values. However, a high degree of suspicion should be kept in elderly as the presentation could be subtle in them.
Laboratory Findings
Laboratory findings such as leukocytosis are helpful for the diagnosis of bacterial pneumonia or to assess the status of the patient. Sputum samples need to be collected from every patient and sent for gram staining and culture that need to be performed to determine the exact pathogen causing the pneumonia. Other tests include urine antigen test, PCR, C-reactive protein, and procalcitonin.
Chest X Ray
An important test for making a diagnosis of pneumonia is a chest x-ray. Chest x-rays can reveal areas of opacity (seen as white) which represent consolidation. Pneumonia is not always seen on x-rays, either because the disease is only in its initial stages, or because it involves a part of the lung not easily seen by x-ray.
CT
A chest CT scan is not routinely done in patients with pneumonia, but is a diagnostic test that may be useful when a chest x-ray is not conclusive. CT findings may include lobar consolidation, ground-glass opacities, pleural effusion, lymphadenopathy, and tree-in-bud appereance.
Other Imaging Findings
Bronchoscopy with bronchoalveolar lavage is useful to obtain samples for gram stain and culture in patients with certain conditions, such as immunocompromised patients, ICU admission or antibiotic failure.
Treatment
Medical Therapy
The treatment of pneumonia involves three critical decisions: firstly whether the patient truly has pneumonia, secondly what is the severity of the pneumonia, and lastly whether hospitalization is required for adequate management. Most cases of pneumonia can be treated without hospitalization. Typically, oral antibiotics, rest, fluids, and home care are sufficient for complete resolution. However, people with pneumonia who are having trouble breathing, comorbidities, and the elderly may need more advanced treatment. If the symptoms get worse, the pneumonia does not improve with home treatment, or complications occur, the person will often have to be hospitalized.
Prevention
There are several ways to prevent infectious pneumonia. Appropriately treating underlying illnesses (such as AIDS), smoking cessation, vaccination against pneumococcal, and influenza are the commonly used methods.
References
Historical Perspective
|
Pneumonia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumonia On the Web |
|
American Roentgen Ray Society Images of Pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [8], Serge Korjian M.D., Priyamvada Singh, M.D. [9]
Overview
The pneumonia syndrome has been recognized since ancient times. It was initially described by Hippocrates who recorded his observations of its symptoms and complications. Edwin Klebs was the first to identify bacteria in the lungs of patients who died from pneumonia in 1875. This discovery was soon-after substantiated by the works of Carl Friedländer and Albert Fränkel who were the first to identify Streptococcus pneumoniae as a causative agent. The introduction of the gram stain subsequently led to the discovery of other causative organisms. Despite being an important cause of mortality before the late twentieth century, the advent of antibiotics, modern surgical techniques, and vaccination drastically lowered the morbidity and mortality of pneumonia with the turn of the century.
Historical Perspective
Discovery
- Pneumonia was first discovered by Hippocrates.
- In 1817, Dr. Simpson of United Kingdom was the first to report a case of pneumonia treated with blood letting.[1]
- In 1842, Dr. Edward Newfold of United Kingdom was the first to report a case of typhoid pneumonia.[2]
- In 1875, Dr. Edwin Klebs was the first to discover the association between bacteria and the development of pneumonia.
Landmark Events in the Development of Treatment Strategies
- In 1902, Dr. Wright discovered the pneumococcal vaccine as a preventative treatment of pneumonia.[3]
References
- ↑ "Case ofPneumonia, Where the Extent to Which Blood-Letting May Be Successfully Carried Is Fully Exemplified". Med Chir J Rev. 4 (24): 460–463. 1817. PMC 5570882. PMID 29257545.
- ↑ Newbold E (1842). "Case of Typhoid Pneumonia". Prov Med J Retrosp Med Sci. 4 (84): 87. PMC 2489819. PMID 21373079.
- ↑ Harris AB (1909). "Observations on the Therapeutic Value of the Pneumococcus Vaccine in the Treatment of Pneumonia and some of its Complications". Br Med J. 1 (2530): 1530–5. PMC 2320626. PMID 20764553.
Pathophysiology
|
Pneumonia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumonia On the Web |
|
American Roentgen Ray Society Images of Pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [10]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [11], Priyamvada Singh, M.D. [12]
Overview
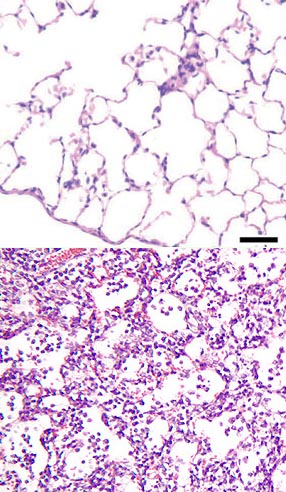
Bacteria and fungi typically enter the lung with inhalation. Once inside the alveoli, these microbes travel into the spaces between the cells and also between adjacent alveoli through connecting pores. This invasion triggers the immune system response by sending white blood cells responsible for attacking microorganisms (neutrophils) to the lungs resulting in manifestations of pneumonia.
Pathophysiology
Mode of Transmission
1. Inhalation of Aerosolized Droplets
- Inhalation of aerosolized droplets of 0.5 to 1 micrometer is the most common pathway of acquiring pneumonia.
- A few bacterial and viral infections are transmitted in this fashion.
- The lung can normally filter out particles between 0.5 to 2 micrometer by recruiting the alveolar macrophages.[1]
2. Microaspiration of Oropharyngeal Contents
- Aspiration of oropharyngeal contents containing pathogenic microorganisms is one of the mechanism of acquiring pneumonia.
- It most commonly occurs in normal persons during sleep, in unconscious persons due to gastroesopahegeal reflux or impaired gag reflex and cough reflex.[1]
3. Blood-Borne or Systemic Infection
- Microbial entered through circulation may also result in pulmonary infections.
- Blood-borne pneumonia is seen more commonly in intravenous drug users. Staphylococcus aureus causes pneumonia in this way.
- Gram negative bacteria typically account for pneumonia in immunocompromised individuals.
4. Trauma or Local Spread
- Pneumonia can occur after a pulmonary procedure or a penetrating trauma to the lungs.
- A local spread of a hepatic abscess can also lead to pneumonia.
Agent Specific Virulence Factors
Several strategies are evolved to evade host defence mechanisms and facilitate spreading before establishing an infection.
- Influenza virus possesses neuraminidases for cleavage of sialic acid residues on the cell surface and viral proteins, which prevent aggregation and facilitate propagation of viral particles.
- Chlamydophila pneumoniae induces complete abortion of cilia motions which assists colonization at the respiratory epithelium.[2]
- Mycoplasma pneumoniae produces a virulence factor with ADP-ribosylating activity which is responsible for airway cellular damage and mucociliary dysfunction.[3]
- Haemophilus influenzae, Streptococcus pneumoniae, and Neisseria meningitidis produce proteases that split mucosal IgA.
- Streptococcus pneumoniae possesses pneumolysin that aid the bacteria during colonization, by facilitating adherence to the host,[4] during invasion by damaging host cells,[5] and during infection by interfering with the host immune response.[6]
Host Factors
- The lungs can normally filter out large droplets of aerosols.
- Smaller droplets of the size of 0.5 to 2 micrometer are deposited on the alveoli and then engulfed by alevolar macrophages.
- These macrophages release cytokines and chemokines, which also includes tumor necrosis factor-alpha, interleukin-8 and LTB4.
- The neutrophils are recruited by these cells to eliminate these microorganisms.[7][8]
1. Diminished Mucociliary Clearance
- The cilia lining the respiratory epithelium serve to move secreted mucus containing trapped foreign particles including pathogens towards the oropharynx for either expectoration or swallowing.
- Elevated incidence of pneumonia in patients with genetic defects affecting mucociliary clearance such as primary ciliary dyskinesia suggests its role in the pathogenesis of community-acquired pneumonia.
2. Impaired Cough Reflex
- Cough, together with mucociliary clearance, prevent pathogens from entering the lower respiratory tract.
- Cough suppression or cough reflex inhibition seen in patients with cerebrovascular accidents and drug overdosages is associated with an enhanced risk for aspiration pneumonia.
- Another relation to cough is genetic polymorphisms in the angiotensin-converting enzyme (ACE) gene.
- The role of cough in preventing pneumonia may be explained by a higher risk for developing pneumonia in homozygotes carrying deletion/deletion (DD) genotype who are found to have lower levels of bradykinin and tachykinins such as substance P.[9][10]
3. Defective Immune System
- Pathogen-associated molecular patterns (PAMPs) are initially recognized by Toll-like receptors (TLRs) and other pattern-recognition receptors (PRRs) of the innate immune system.
- Effectors in the acquired immune system are involved in elimination of microorganisms and generation of immunological memory.
- Other components in the immune system such as complement system, cytokines, and collectins, also mediate the defense against microorganisms causing pneumonia.
Microscopic Pathology
Microbial PathogenesisVirulence FactorsSeveral mechanisms have evolved to evade host defense mechanisms and facilitate microbial spread to establish an infection.
Aspiration Pneumonia{{#ev:youtube|bTqgAfQv0p4}}
Lobar Pneumonia{{#ev:youtube|dxXrxYIXbL8}}
Pneumocystis Pneumonia{{#ev:youtube|KfF_pPUjR8o}} Pneumocystis Pneumonia{{#ev:youtube|zSdK_yWe_S4}} Aspiration Pneumonia{{#ev:youtube|bTqgAfQv0p4}} Aspiration Pneumonia, Infant{{#ev:youtube|RXnnEuEZ0BY}} Desquamative Interstitial Pneumonia{{#ev:youtube|G0TFmAAYjWU}} Legionella Pneumonia{{#ev:youtube|BDWEnPilfIQ}} Measles Pneumonia{{#ev:youtube|v80kA_dt6EE}} Abscess, Bronchopneumonia{{#ev:youtube|wO2x7O2KEZY}} |
References
- ↑ 1.0 1.1 Wunderink, RG.; Waterer, GW. (2004). "Community-acquired pneumonia: pathophysiology and host factors with focus on possible new approaches to management of lower respiratory tract infections". Infect Dis Clin North Am. 18 (4): 743–59, vii. doi:10.1016/j.idc.2004.07.004. PMID 15555822. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Shemer-Avni, Y.; Lieberman, D. (1995). "Chlamydia pneumoniae-induced ciliostasis in ciliated bronchial epithelial cells". J Infect Dis. 171 (5): 1274–8. PMID 7751703. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 Kannan, TR.; Baseman, JB. (2006). "ADP-ribosylating and vacuolating cytotoxin of Mycoplasma pneumoniae represents unique virulence determinant among bacterial pathogens". Proc Natl Acad Sci U S A. 103 (17): 6724–9. doi:10.1073/pnas.0510644103. PMID 16617115. Unknown parameter
|month=ignored (help) - ↑ Rubins, JB (December 1998). "Pneumolysin in pneumococcal adherence and colonization". Microbial pathogenesis. 25 (6): 337–42. doi:10.1006/mpat.1998.0239. PMID 9895272. Unknown parameter
|coauthors=ignored (help) - ↑ Rubins, JB (January 1998). "Pneumolysin: a multifunctional pneumococcal virulence factor". The Journal of laboratory and clinical medicine. 131 (1): 21–7. PMID 9452123. Unknown parameter
|coauthors=ignored (help) - ↑ Cockeran, R (June 2002). "The role of pneumolysin in the pathogenesis of Streptococcus pneumoniae infection". Current Opinion in Infectious Diseases. 15 (3): 235–9. PMID 12015456. Unknown parameter
|coauthors=ignored (help) - ↑ Strieter, RM.; Belperio, JA.; Keane, MP. (2003). "Host innate defenses in the lung: the role of cytokines". Curr Opin Infect Dis. 16 (3): 193–8. doi:10.1097/01.qco.0000073766.11390.0e. PMID 12821807. Unknown parameter
|month=ignored (help) - ↑ Mason, CM.; Nelson, S. (2005). "Pulmonary host defenses and factors predisposing to lung infection". Clin Chest Med. 26 (1): 11–7. doi:10.1016/j.ccm.2004.10.018. PMID 15802161. Unknown parameter
|month=ignored (help) - ↑ Morimoto, S.; Okaishi, K.; Onishi, M.; Katsuya, T.; Yang, J.; Okuro, M.; Sakurai, S.; Onishi, T.; Ogihara, T. (2002). "Deletion allele of the angiotensin-converting enzyme gene as a risk factor for pneumonia in elderly patients". Am J Med. 112 (2): 89–94. PMID 11835945. Unknown parameter
|month=ignored (help) - ↑ Rigat, B.; Hubert, C.; Alhenc-Gelas, F.; Cambien, F.; Corvol, P.; Soubrier, F. (1990). "An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels". J Clin Invest. 86 (4): 1343–6. doi:10.1172/JCI114844. PMID 1976655. Unknown parameter
|month=ignored (help) - ↑ Rubins, JB (December 1998). "Pneumolysin in pneumococcal adherence and colonization". Microbial pathogenesis. 25 (6): 337–42. doi:10.1006/mpat.1998.0239. PMID 9895272. Unknown parameter
|coauthors=ignored (help) - ↑ Rubins, JB (January 1998). "Pneumolysin: a multifunctional pneumococcal virulence factor". The Journal of laboratory and clinical medicine. 131 (1): 21–7. PMID 9452123. Unknown parameter
|coauthors=ignored (help) - ↑ Cockeran, R (June 2002). "The role of pneumolysin in the pathogenesis of Streptococcus pneumoniae infection". Current Opinion in Infectious Diseases. 15 (3): 235–9. PMID 12015456. Unknown parameter
|coauthors=ignored (help)
{{#ask:Caused By::Pneumonia |format=list |headers=hide |link=none |sep= | |template=MedicalCauseQuery }}
Natural History, Complications & Prognosis
Diagnosis
{{#ask:Used To Diagnose::Pneumonia |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTestQuery |sort=Sort Order }}
Treatment
{{#ask:Used To Treat::Pneumonia |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery |sort=Sort Order }} {{#ask:Prevents::Pneumonia |?Sort Order |intro= | |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery2 |sort=Sort Order }}