Peripartum mood disturbances pathophysiology: Difference between revisions
Homa Najafi (talk | contribs) (Created page with "__NOTOC__ {{Peripartum mood disturbances}} {{CMG}}; {{AE}}{{Sunita}} ==Overview== The exact pathogenesis of [disease name] is not fully understood. OR It is thought that [d...") |
|||
| (38 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Peripartum mood disturbances]] are mainly the mood alterations or changes seen in the [[women]] during and after the [[delivery]]. It involes the complex [[pathophysiology]] which is regulated by expression of different [[genes]] and [[neuroendocrine]] [[hormones]]. The [[genes]] playing important role are mainly [[Estrogen receptor]] alpha gene [[polymorphisms|Polymorphisms i]]<nowiki/>n the [[serotonin transporter]] gene, [[5-HT|5-HTT]][[gene]] encoding for [[MAO-A|MAOA]] and the [[gene]] encoding for [[Catechol-O-methyltransferase]] (COMT), [[Genetic variation|Genetic variants]] for the [[TPH2 gene]], [[SNP]] in OXT; [[SNP]] in the [[OXTR gene]] and [[methylation]] state was detected in association with [[postpartum]] [[depression]]. [[Hemicentin 1 gene]] [[Hemicentin 1|(HMNC1]]) along with the [[neuroendocrine]] [[hormones]] maily [[GABA]], [[Glutamate]], [[serotonin]] and , or [[dopamine]]. | |||
It | |||
[ | |||
[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
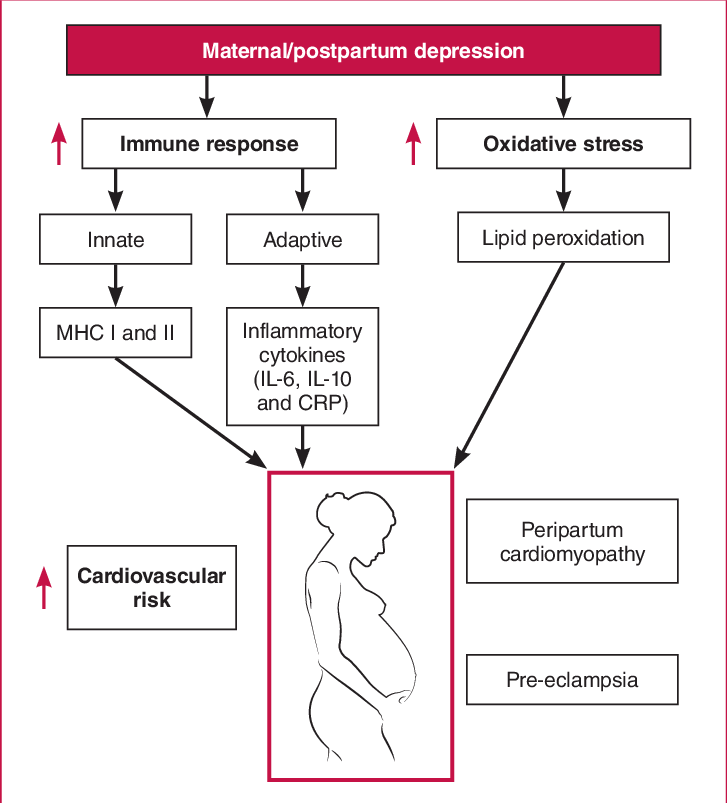
[[File:A-hypothetical-mechanism-by-which-depression-during-pregnancy-and-postpartum-may.png|alt=Pathophysiology.|left|thumb|547x547px|Pathophysiology of postpartum depression.]] | |||
[[Pathophysiology]] of [[Peripartum mood disturbances]]- [[Pathophysiology]] of [[Peripartum mood disturbances]] includes the role of various [[genes]] and [[hormones]] as described below: | |||
= | |||
[ | |||
*<u>[[Genetics|Genetic Mechanism]] of [[postpartum]] [[depression]]</u>: <ref name="pmid30552910">{{cite journal |vauthors=Payne JL, Maguire J |title=Pathophysiological mechanisms implicated in postpartum [[depression]] |journal=Front Neuroendocrinol |volume=52 |issue= |pages=165–180 |date=January 2019 |pmid=30552910 |pmc=6370514 |doi=10.1016/j.yfrne.2018.12.001 |url=}}</ref>Numerous [[gene]] playing significant role in deciding the [[pathophysiology]] are:<br> | |||
*[ | **[[Estrogen receptor]] alpha gene<ref name="pmid24495551">{{cite journal |vauthors=Mehta D, Newport DJ, Frishman G, Kraus L, Rex-Haffner M, Ritchie JC, Lori A, Knight BT, Stagnaro E, Ruepp A, Stowe ZN, Binder EB |title=Early predictive biomarkers for postpartum depression point to a role for estrogen receptor signaling |journal=Psychol Med |volume=44 |issue=11 |pages=2309–22 |date=August 2014 |pmid=24495551 |doi=10.1017/S0033291713003231 |url=}}</ref> | ||
*[ | **[[polymorphisms|Polymorphisms i]]<nowiki/>n the [[serotonin transporter]] gene,<ref name="pmid20045118">{{cite journal |vauthors=Binder EB, Newport DJ, Zach EB, Smith AK, Deveau TC, Altshuler LL, Cohen LS, Stowe ZN, Cubells JF |title=A serotonin transporter gene polymorphism predicts peripartum depressive symptoms in an at-risk psychiatric cohort |journal=J Psychiatr Res |volume=44 |issue=10 |pages=640–6 |date=July 2010 |pmid=20045118 |pmc=2891911 |doi=10.1016/j.jpsychires.2009.12.001 |url=}}</ref> | ||
*[ | **[[5-HT|5-HTT]] | ||
**[[gene]] encoding for [[MAO-A|MAOA]]<ref name="pmid19625011">{{cite journal |vauthors=Doornbos B, Dijck-Brouwer DA, Kema IP, Tanke MA, van Goor SA, Muskiet FA, Korf J |title=The development of peripartum depressive symptoms is associated with gene polymorphisms of MAOA, 5-HTT and COMT |journal=Prog Neuropsychopharmacol Biol Psychiatry |volume=33 |issue=7 |pages=1250–4 |date=October 2009 |pmid=19625011 |doi=10.1016/j.pnpbp.2009.07.013 |url=}}</ref> | |||
**[[gene]] encoding for [[Catechol-O-methyltransferase]] (COMT)<ref name="pmid23636476">{{cite journal |vauthors=Alvim-Soares A, Miranda D, Campos SB, Figueira P, Romano-Silva MA, Correa H |title=Postpartum depression symptoms associated with Val158Met COMT polymorphism |journal=Arch Womens Ment Health |volume=16 |issue=4 |pages=339–40 |date=August 2013 |pmid=23636476 |doi=10.1007/s00737-013-0349-8 |url=}}</ref>, | |||
**[[Genetic variation|Genetic variants]] for the [[TPH2 gene]] | |||
**[[SNP]] in OXT; SNP in the [[OXTR gene]] and [[methylation]] state was detected in association with [[postpartum]] [[depression]]. | |||
**[[Hemicentin 1 gene]] [[Hemicentin 1|(HMNC1]]) and its association with [[postpartum]] [[depression]]<ref name="pmid21912392">{{cite journal |vauthors=Bouma EM, Riese H, Doornbos B, Ormel J, Oldehinkel AJ |title=Genetically based reduced MAOA and COMT functioning is associated with the cortisol stress response: a replication study |journal=Mol Psychiatry |volume=17 |issue=2 |pages=119–21 |date=February 2012 |pmid=21912392 |doi=10.1038/mp.2011.115 |url=}}</ref>. | |||
*<u>[[Epigenetic]] mechanisms of [[postpartum depression]]</u><ref name="pmid23689534">{{cite journal |vauthors=Guintivano J, Arad M, Gould TD, Payne JL, Kaminsky ZA |title=Antenatal prediction of postpartum depression with blood DNA methylation biomarkers |journal=Mol Psychiatry |volume=19 |issue=5 |pages=560–7 |date=May 2014 |pmid=23689534 |pmc=7039252 |doi=10.1038/mp.2013.62 |url=}}</ref><br> | |||
**In women with [[postpartum depression]], there was a substantial interaction between [[OXTR]] [[DNA methylation]], [[estradiol]], and the ratio of [[allopregnanolone]] to [[progesterone]].Alterations in [[DNA methylation]] of the [[OXTR gene]] are adversely linked with [[blood]] [[estradiol]] levels in women with [[postpartum depression]]. | |||
**As a result, [[epigenetic]] alterations can affect [[metabolic]] processes linked to [[postpartum depression]]. | |||
*<u>[[Neuroendocrine]] mechanisms of [[postpartum depression]]</u>:<ref name="pmid16554740">{{cite journal |vauthors=Walf AA, Frye CA |title=A review and update of mechanisms of estrogen in the hippocampus and amygdala for anxiety and depression behavior |journal=Neuropsychopharmacology |volume=31 |issue=6 |pages=1097–111 |date=June 2006 |pmid=16554740 |pmc=3624621 |doi=10.1038/sj.npp.1301067 |url=}}</ref> <br> | |||
**In [[postpartum depression]], there is an interaction between the [[Hypothalamus]]-[[pituitary]]-[[gonadal]] (HPG) and [[Hypothalamus]]-[[Pituitary]]-[[Adrenal]]([[HPA]]) axis. | |||
**[[HPA axis]] function has been found to be influenced by [[reproductive]] [[hormones]] and vice versa.<ref name="pmid21562482">{{cite journal |vauthors=Skrundz M, Bolten M, Nast I, Hellhammer DH, Meinlschmidt G |title=Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression |journal=Neuropsychopharmacology |volume=36 |issue=9 |pages=1886–93 |date=August 2011 |pmid=21562482 |pmc=3154107 |doi=10.1038/npp.2011.74 |url=}}</ref> | |||
**As a result, any change in [[reproductive hormones]] may cause [[stress hormone]] levels to fluctuate, resulting in [[postpartum depression]]. | |||
**Alterations of the [[HPA axis]]' function may also affect [[reproductive]] [[hormone]] levels, contributing to [[postpartum depression]]. | |||
== | *<u>[[Neurotransmitters]] and [[postpartum depression]]</u><ref name="pmid21079608">{{cite journal |vauthors=Luscher B, Shen Q, Sahir N |title=The GABAergic deficit hypothesis of major depressive disorder |journal=Mol Psychiatry |volume=16 |issue=4 |pages=383–406 |date=April 2011 |pmid=21079608 |pmc=3412149 |doi=10.1038/mp.2010.120 |url=}}</ref><ref name="pmid22805604">{{cite journal |vauthors=McEwen AM, Burgess DT, Hanstock CC, Seres P, Khalili P, Newman SC, Baker GB, Mitchell ND, Khudabux-Der J, Allen PS, LeMelledo JM |title=Increased glutamate levels in the medial prefrontal cortex in patients with postpartum depression |journal=Neuropsychopharmacology |volume=37 |issue=11 |pages=2428–35 |date=October 2012 |pmid=22805604 |pmc=3442339 |doi=10.1038/npp.2012.101 |url=}}</ref><ref name="pmid17543959">{{cite journal |vauthors=Moses-Kolko EL, Wisner KL, Price JC, Berga SL, Drevets WC, Hanusa BH, Loucks TL, Meltzer CC |title=Serotonin 1A receptor reductions in postpartum depression: a positron emission tomography study |journal=Fertil Steril |volume=89 |issue=3 |pages=685–92 |date=March 2008 |pmid=17543959 |pmc=2410091 |doi=10.1016/j.fertnstert.2007.03.059 |url=}}</ref><ref name="pmid23235822">{{cite journal |vauthors=Tye KM, Mirzabekov JJ, Warden MR, Ferenczi EA, Tsai HC, Finkelstein J, Kim SY, Adhikari A, Thompson KR, Andalman AS, Gunaydin LA, Witten IB, Deisseroth K |title=Dopamine neurons modulate neural encoding and expression of depression-related behaviour |journal=Nature |volume=493 |issue=7433 |pages=537–541 |date=January 2013 |pmid=23235822 |pmc=4160519 |doi=10.1038/nature11740 |url=}}</ref> : | ||
{| class="wikitable" | |||
|+ | |||
!GABA | |||
!Glutamate | |||
!Serotonin | |||
!Dopamine | |||
|- | |||
|[[GABA]] which is an inhibitory [[neurotransmitter]] in the [[brain]] | |||
|[[Glutamate]] is the [[excitatory neurotransmitter]] in the brain | |||
|[[Serotonin]] to [[5HT1A]] [[receptors]] is decreased in the following brain regions | |||
|[[Mutations]] in [[DR1]] | |||
|- | |||
|Level is inversely related with the [[depression]] [[symptoms]] in the [[postpartum]] period | |||
|[[postpartum depression]] its level are increased in the [[Medial prefrontal cortex|medial prefrontal]] [[cortex]] | |||
|[[mesiotemporal]] and anterior [[Cingulate cortex|cingulate cortices]]. | |||
|Relates to the attention and affection of mother for the baby | |||
|- | |||
| | |||
|In [[postpartum depression]] decreased in the dorsolateral [[prefrontal cortex]]. | |||
| | |||
|} | |||
*[[Neuroinflammatory]] mechanisms in [[postpartum depression]]: <br>There is a negative relationship between [[T-cell]] number and [[postpartum depression]] symptoms, whereas [[IL-6]] and [[IL-1β]] have a significant positive relationship with it.<br /> | |||
*It is thought that in [[postpartum]] [[psychosis]], immunoneuroendocrine set point is dysregulated with overactivation of the [[immune system]]'s [[macrophage]] and [[monocyte]] arm. <ref name="pmid28713685">{{cite journal |vauthors=Davies W |title=Understanding the pathophysiology of [[postpartum]] [[psychosis]]: Challenges and new approaches |journal=World J Psychiatry |volume=7 |issue=2 |pages=77–88 |date=June 2017 |pmid=28713685 |pmc=5491479 |doi=10.5498/wjp.v7.i2.77 |url=}}</ref> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Primary care]] | |||
[[Category:Obstetrics]] | |||
[[Category:Medicine]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Psychiatry]] | |||
Latest revision as of 19:07, 5 August 2021
|
Peripartum mood disturbances Microchapters |
|
Differentiating Peripartum mood disturbances from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Peripartum mood disturbances pathophysiology On the Web |
|
American Roentgen Ray Society Images of Peripartum mood disturbances pathophysiology |
|
Risk calculators and risk factors for Peripartum mood disturbances pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sunita Kumawat, M.B.B.S[2]
Overview
Peripartum mood disturbances are mainly the mood alterations or changes seen in the women during and after the delivery. It involes the complex pathophysiology which is regulated by expression of different genes and neuroendocrine hormones. The genes playing important role are mainly Estrogen receptor alpha gene Polymorphisms in the serotonin transporter gene, 5-HTTgene encoding for MAOA and the gene encoding for Catechol-O-methyltransferase (COMT), Genetic variants for the TPH2 gene, SNP in OXT; SNP in the OXTR gene and methylation state was detected in association with postpartum depression. Hemicentin 1 gene (HMNC1) along with the neuroendocrine hormones maily GABA, Glutamate, serotonin and , or dopamine.
Pathophysiology
Pathophysiology of Peripartum mood disturbances- Pathophysiology of Peripartum mood disturbances includes the role of various genes and hormones as described below:
- Genetic Mechanism of postpartum depression: [1]Numerous gene playing significant role in deciding the pathophysiology are:
- Estrogen receptor alpha gene[2]
- Polymorphisms in the serotonin transporter gene,[3]
- 5-HTT
- gene encoding for MAOA[4]
- gene encoding for Catechol-O-methyltransferase (COMT)[5],
- Genetic variants for the TPH2 gene
- SNP in OXT; SNP in the OXTR gene and methylation state was detected in association with postpartum depression.
- Hemicentin 1 gene (HMNC1) and its association with postpartum depression[6].
- Epigenetic mechanisms of postpartum depression[7]
- In women with postpartum depression, there was a substantial interaction between OXTR DNA methylation, estradiol, and the ratio of allopregnanolone to progesterone.Alterations in DNA methylation of the OXTR gene are adversely linked with blood estradiol levels in women with postpartum depression.
- As a result, epigenetic alterations can affect metabolic processes linked to postpartum depression.
- Neuroendocrine mechanisms of postpartum depression:[8]
- In postpartum depression, there is an interaction between the Hypothalamus-pituitary-gonadal (HPG) and Hypothalamus-Pituitary-Adrenal(HPA) axis.
- HPA axis function has been found to be influenced by reproductive hormones and vice versa.[9]
- As a result, any change in reproductive hormones may cause stress hormone levels to fluctuate, resulting in postpartum depression.
- Alterations of the HPA axis' function may also affect reproductive hormone levels, contributing to postpartum depression.
| GABA | Glutamate | Serotonin | Dopamine |
|---|---|---|---|
| GABA which is an inhibitory neurotransmitter in the brain | Glutamate is the excitatory neurotransmitter in the brain | Serotonin to 5HT1A receptors is decreased in the following brain regions | Mutations in DR1 |
| Level is inversely related with the depression symptoms in the postpartum period | postpartum depression its level are increased in the medial prefrontal cortex | mesiotemporal and anterior cingulate cortices. | Relates to the attention and affection of mother for the baby |
| In postpartum depression decreased in the dorsolateral prefrontal cortex. |
- Neuroinflammatory mechanisms in postpartum depression:
There is a negative relationship between T-cell number and postpartum depression symptoms, whereas IL-6 and IL-1β have a significant positive relationship with it.
- It is thought that in postpartum psychosis, immunoneuroendocrine set point is dysregulated with overactivation of the immune system's macrophage and monocyte arm. [14]
References
- ↑ Payne JL, Maguire J (January 2019). "Pathophysiological mechanisms implicated in postpartum [[depression]]". Front Neuroendocrinol. 52: 165–180. doi:10.1016/j.yfrne.2018.12.001. PMC 6370514. PMID 30552910. URL–wikilink conflict (help)
- ↑ Mehta D, Newport DJ, Frishman G, Kraus L, Rex-Haffner M, Ritchie JC, Lori A, Knight BT, Stagnaro E, Ruepp A, Stowe ZN, Binder EB (August 2014). "Early predictive biomarkers for postpartum depression point to a role for estrogen receptor signaling". Psychol Med. 44 (11): 2309–22. doi:10.1017/S0033291713003231. PMID 24495551.
- ↑ Binder EB, Newport DJ, Zach EB, Smith AK, Deveau TC, Altshuler LL, Cohen LS, Stowe ZN, Cubells JF (July 2010). "A serotonin transporter gene polymorphism predicts peripartum depressive symptoms in an at-risk psychiatric cohort". J Psychiatr Res. 44 (10): 640–6. doi:10.1016/j.jpsychires.2009.12.001. PMC 2891911. PMID 20045118.
- ↑ Doornbos B, Dijck-Brouwer DA, Kema IP, Tanke MA, van Goor SA, Muskiet FA, Korf J (October 2009). "The development of peripartum depressive symptoms is associated with gene polymorphisms of MAOA, 5-HTT and COMT". Prog Neuropsychopharmacol Biol Psychiatry. 33 (7): 1250–4. doi:10.1016/j.pnpbp.2009.07.013. PMID 19625011.
- ↑ Alvim-Soares A, Miranda D, Campos SB, Figueira P, Romano-Silva MA, Correa H (August 2013). "Postpartum depression symptoms associated with Val158Met COMT polymorphism". Arch Womens Ment Health. 16 (4): 339–40. doi:10.1007/s00737-013-0349-8. PMID 23636476.
- ↑ Bouma EM, Riese H, Doornbos B, Ormel J, Oldehinkel AJ (February 2012). "Genetically based reduced MAOA and COMT functioning is associated with the cortisol stress response: a replication study". Mol Psychiatry. 17 (2): 119–21. doi:10.1038/mp.2011.115. PMID 21912392.
- ↑ Guintivano J, Arad M, Gould TD, Payne JL, Kaminsky ZA (May 2014). "Antenatal prediction of postpartum depression with blood DNA methylation biomarkers". Mol Psychiatry. 19 (5): 560–7. doi:10.1038/mp.2013.62. PMC 7039252 Check
|pmc=value (help). PMID 23689534. - ↑ Walf AA, Frye CA (June 2006). "A review and update of mechanisms of estrogen in the hippocampus and amygdala for anxiety and depression behavior". Neuropsychopharmacology. 31 (6): 1097–111. doi:10.1038/sj.npp.1301067. PMC 3624621. PMID 16554740.
- ↑ Skrundz M, Bolten M, Nast I, Hellhammer DH, Meinlschmidt G (August 2011). "Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression". Neuropsychopharmacology. 36 (9): 1886–93. doi:10.1038/npp.2011.74. PMC 3154107. PMID 21562482.
- ↑ Luscher B, Shen Q, Sahir N (April 2011). "The GABAergic deficit hypothesis of major depressive disorder". Mol Psychiatry. 16 (4): 383–406. doi:10.1038/mp.2010.120. PMC 3412149. PMID 21079608.
- ↑ McEwen AM, Burgess DT, Hanstock CC, Seres P, Khalili P, Newman SC, Baker GB, Mitchell ND, Khudabux-Der J, Allen PS, LeMelledo JM (October 2012). "Increased glutamate levels in the medial prefrontal cortex in patients with postpartum depression". Neuropsychopharmacology. 37 (11): 2428–35. doi:10.1038/npp.2012.101. PMC 3442339. PMID 22805604.
- ↑ Moses-Kolko EL, Wisner KL, Price JC, Berga SL, Drevets WC, Hanusa BH, Loucks TL, Meltzer CC (March 2008). "Serotonin 1A receptor reductions in postpartum depression: a positron emission tomography study". Fertil Steril. 89 (3): 685–92. doi:10.1016/j.fertnstert.2007.03.059. PMC 2410091. PMID 17543959.
- ↑ Tye KM, Mirzabekov JJ, Warden MR, Ferenczi EA, Tsai HC, Finkelstein J, Kim SY, Adhikari A, Thompson KR, Andalman AS, Gunaydin LA, Witten IB, Deisseroth K (January 2013). "Dopamine neurons modulate neural encoding and expression of depression-related behaviour". Nature. 493 (7433): 537–541. doi:10.1038/nature11740. PMC 4160519. PMID 23235822.
- ↑ Davies W (June 2017). "Understanding the pathophysiology of [[postpartum]] [[psychosis]]: Challenges and new approaches". World J Psychiatry. 7 (2): 77–88. doi:10.5498/wjp.v7.i2.77. PMC 5491479. PMID 28713685. URL–wikilink conflict (help)