Palpitations resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D.
| Palpitations Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Gallery |
Overview
Causes
Life-Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common causes
- Cardiac causes
- Arrhythmic
- Non-arrhythmic
- Valvular disease
- Pericarditis
- Structural heart disease
- Malfunctioning pacemaker
- Psychiatric causes
- Substance - drug causes
- Systemic causes
Click here for a complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[1][2]
Boxes in the red signify that an urgent management is needed.
Abbreviations: EKG: Electrocardiogram; IV: Intravenous; NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Does the patient have any of the following findings that require urgent management? ❑ Syncope (suggestive of cardiac tamponade, complete AV block) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stabilize the patient ❑ Consider intubation if the patient's airway is compromised, has a Glasgow coma scale (GCS < 8) or profound hemodynamic instability ❑ Administer oxygen and maintain a saturation >90% ❑ 12 lead ECG | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Place patient on cardiac monitor ❑ Re-evaluate if status worsens | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Abnormal rhythm w/ a ventricular rate of ≥100/min | ❑ ST-segment deviation ❑ Elevated cardiac biomarkers | ❑ Elevated JVP ❑ Pulsus paradoxus ❑ Low-voltage QRS complexes ❑ Electrical alternans ❑ PR segment depression | ❑ Suppressed TSH ❑ Elevated free T3/T4 | ❑ Tachypnea ❑ Wells Score >4 ❑ Positive chest CTA | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| {{{ I04 }}} | {{{ I05 }}} | {{{ I06 }}} | {{{ I07 }}} | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1][3][4][5][6][7]
Abbreviations: AF: Atrial fibrillation; AVRT: AV reentry tachycardia; AVNRT: AV nodal reentry tachycardia; BP: Blood pressure; CBC: Complete blood count; EKG: Electrocardiogram; EPS: Electrophysiological study SVT: Supraventricular tachycardia TSH: Thyroid stimulating hormone; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Characterize the symptoms: ❑ Character of palpitations
❑ Onset
❑ Duration
❑ Frequency (daily, weekly, monthly) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Inquire about drugs that can cause palpitations: ❑ Sympathomimetic agents ❑ Weight reduction drugs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed past medical history: ❑ Previous episodes of palpitations
❑ Cardiac arrhythmia ❑ History of panic attacks | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vitals
❑ Tchypnea (non-specific) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order labs and tests: ❑ EKG
❑ CBC (to rule out anemia or infection) Order imaging studies | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Recurrent episodes when no ambulatory EKG devices are available | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have clinical or EKG findings suggestive of a cardiac cause of the palpitations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Myocardial ischemia ❑ Acute coronary syndrome
| Other EKG findings | Does the patient have history signs of a psychiatric disorder? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
EKG findings suggestive of pericarditis Pericarditis | Unspecific EKG findings | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order a TTE | ❑ Anxiety | Does the patient has history of taking drugs or medications that can cause palpitaations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Click in each link for the specific diagnostic approach and management ❑ Alcohol
❑ Recreational drugs
❑ Nicotine | Systemic disease Click in each link for the specific diagnostic approach and management ❑ Anemia | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
The management of palpitations will be directed to the specific underlying cuase. If the etiology can be determined and low risk, potentialy curative treatments are available that should be the first choice of management. For benign arrhythmias, such as extrasystole, lifestyle changes may be sufficient to prevent future episodes. For patients in whom no clear disease has been established, advise should be made for them to avoid possible triggers for palpitations as caffeine, alcohol, nicotine, recreational drugs.[1][3][4][5][7]
Abbreviations: NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction
| Determine the cause of the palpitations | |||||||||||||||||||||||||||||||||||||||||||
Cardiac cause | Extracardiac cause | ||||||||||||||||||||||||||||||||||||||||||
Psychiatric cause | Drugs or medication intake ❑ Alcohol
❑ Recreational drugs
❑ Nicotine | ||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Implantations or replacement of pacemakers for bradyarrhythmias | |||||||||||||||||||||||||||||||||||||||||||
Do's
- If possible, perform physical exam and EKG when the patient is symptomatic.[1]
- While asymptomatic, search for signs of structural heart disease such as murmurs, displaced apex beat or S3.[1]
- Perform an ambulatory EKG in patients with recurrent episodes of palpitations in which the cause couldn't be determined.[1]
- Perform an EPS in patients in whom the ambulatory EKG is inconclusive.[1]
- Perform an EPS, with ablation therapy if necessary, in patients severe heart disease, when palpitations preceded syncope and when the patient need cardiorespiratory resuscitation maneuvers.[1][6]
- Estimulate life-style changes that may lower the posibility of future episodes, such as exercise, lower alcohol and caffeine intake, smoke cesation.[1]
- Perform an exercise stress test in patients with exercise induced palpitations.[7]
EKG gallery
Narrow complex tachycardia
| Type of Arrhythmia | EKG (lead II) | Clues |
| Sinus tachycardia |  |
Onset and termination: gradual Rhythm: regular Rate: >220 minus the age of the patient Response to adenosine: transient decrease of the rate |
| Atrial fibrillation | 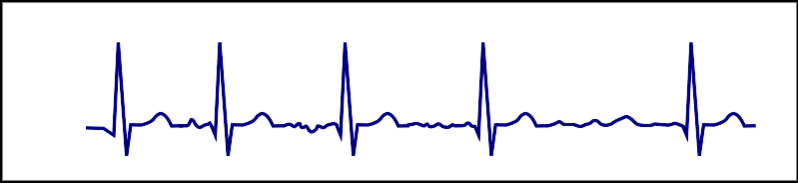 |
Onset and termination: abrupt Rhythm: irregular Rate:100-180 bpm Response to adenosine: transient decrease of the ventricular rate |
| Atrial flutter | 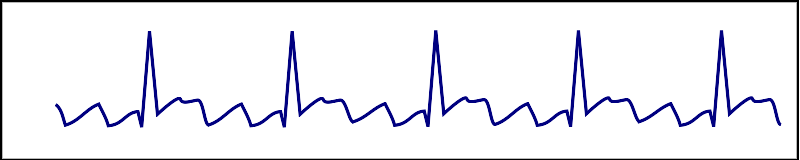 |
Onset and termination: abrupt Rhythm: regular Rate: >150 bpm Response to adenosine: transient decrease of the rate Presence of saw-tooth appearance |
| AVNRT | 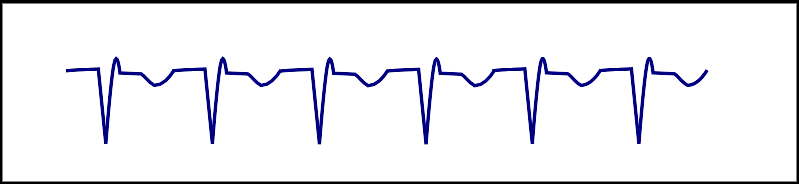 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| AVRT |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| Focal atrial tachycardia |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm |
| Nonparoxysmal junctional tachycardia |  |
Rhythm: regular Retrograde P wave Most commonly due to ischemia or digitalis toxicity |
| Multifocal atrial tachycardia | 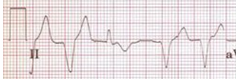 |
Onset and termination: gradual Rhythm: irregular Rate: 100-150 bpm Response to adenosine: no effect 3 different P wave morphologies |
Wide complex tachycardia
| Example | Regularity | Atrial frequency | Ventricular frequency | Origin (SVT/VT) | p-wave | Effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Wide complex (QRS > 0.12) | |||||||
| Ventricular Tachycardia | regular (mostly) | 60-100 bpm | 110-250 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Ventricular Fibrillation | irregular | 60-100 bpm | 400-600 bpm | ventricle (VT) | AV-dissociation | none | |
| Ventricular Flutter | regular | 60-100 bpm | 150-300 bpm | ventricle (VT) | AV-dissociation | none | |
| Accelerated Idioventricular Rhythm | regular (mostly) | 60-100 bpm | 50-110 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Torsade de Pointes | regular | 150-300 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | ||
| Bundle-branch re-entrant Tachycardia* | regular | 60-100 bpm | 150-300 bpm | ventricles (VT) | AV-dissociation | no rate reduction | |
| * Bundle-branch re-entrant tachycardia is extremely rare | |||||||
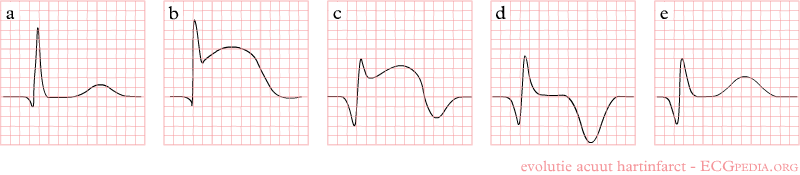
STEMI
Shown below is an EKG demonstrating the evolution of an infarct on the EKG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave suggest STEMI.
NSTEMI
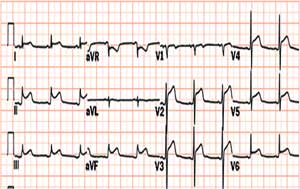
Shown below is an EKG showing an ST depression in V2, V3, V4 and V6.
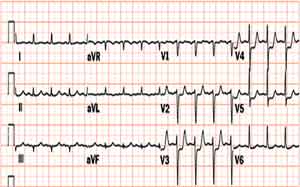
Shown below is an EKG showing an inversion in the T wave at leads V4, V5 and V6.
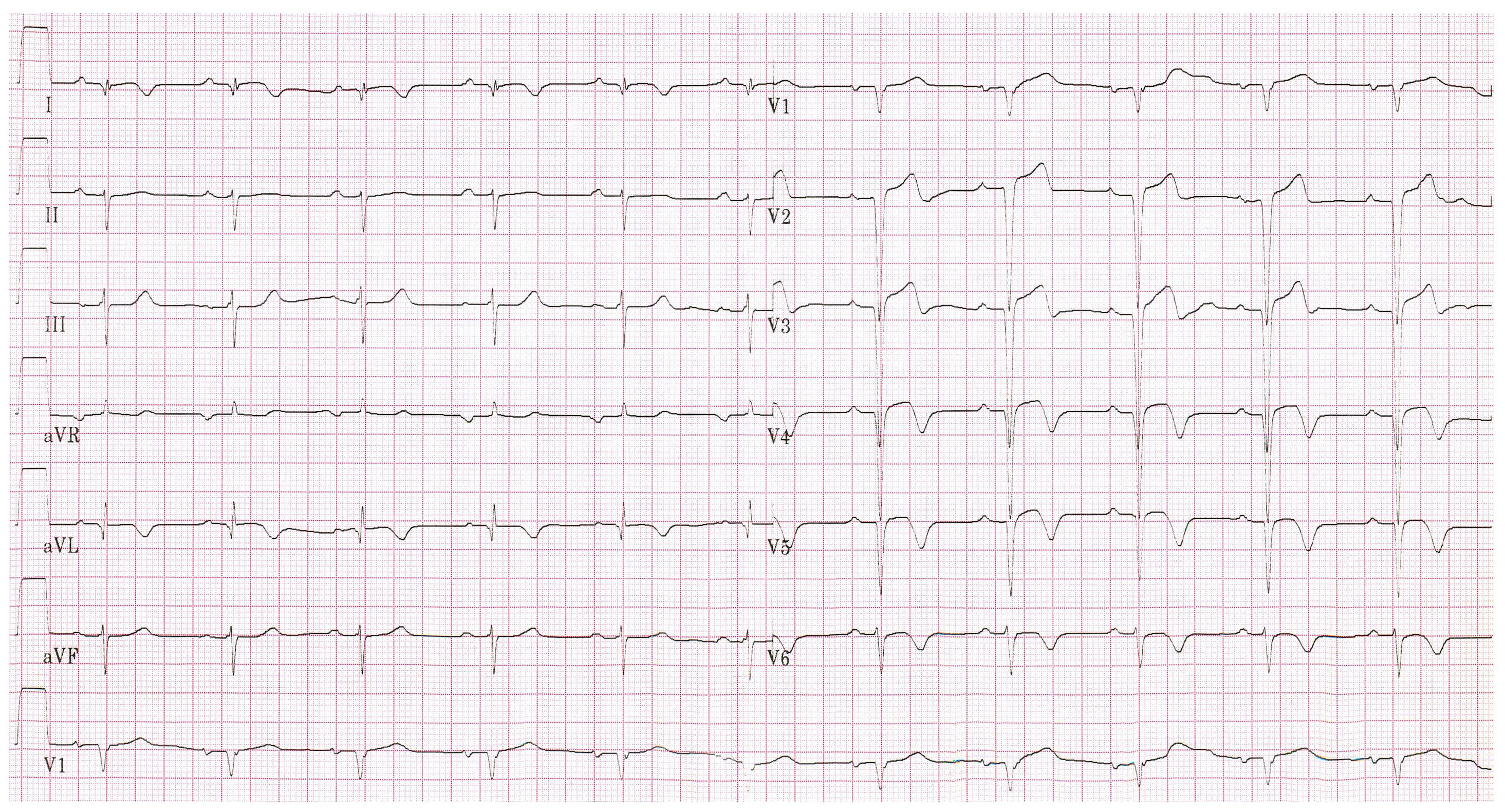
Pericarditis
Shown below is an EKG with ST elevation in lead I, II, V2, V3, V4, V5 and V6.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L; et al. (2011). "Management of patients with palpitations: a position paper from the European Heart Rhythm Association". Europace. 13 (7): 920–34. doi:10.1093/europace/eur130. PMID 21697315.
- ↑ "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ 3.0 3.1 Zimetbaum, P.; Josephson, ME. (1998). "Evaluation of patients with palpitations". N Engl J Med. 338 (19): 1369–73. doi:10.1056/NEJM199805073381907. PMID 9571258. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 "http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf" (PDF). Retrieved 16 April 2014. External link in
|title=(help) - ↑ 5.0 5.1 Abbott, AV. (2005). "Diagnostic approach to palpitations". Am Fam Physician. 71 (4): 743–50. PMID 15742913. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Thavendiranathan, P.; Bagai, A.; Khoo, C.; Dorian, P.; Choudhry, NK. (2009). "Does this patient with palpitations have a cardiac arrhythmia?". JAMA. 302 (19): 2135–43. doi:10.1001/jama.2009.1673. PMID 19920238. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 7.2 "http://www.turner-white.com/pdf/hp_jan03_methods.pdf" (PDF). Retrieved 25 April 2014. External link in
|title=(help)