Palpitations resident survival guide: Difference between revisions
Sergekorjian (talk | contribs) (→Do's) |
|||
| (113 intermediate revisions by 3 users not shown) | |||
| Line 4: | Line 4: | ||
<div style="width: 80%;"> | <div style="width: 80%;"> | ||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | {| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0" ; | ||
|- | |- | ||
! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align=center| {{fontcolor|#2B3B44| | ! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align="center" | {{fontcolor|#2B3B44|Palpitations Resident Survival Guide Microchapters}} | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Overview|Overview]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Overview|Overview]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Causes|Causes]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Causes|Causes]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Complete Diagnostic Approach|Diagnosis]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Complete Diagnostic Approach|Diagnosis]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Treatment|Treatment]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Treatment|Treatment]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Do's|Do's]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Do's|Do's]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#EKG gallery|Gallery]] | ||
|} | |} | ||
==Overview== | ==Overview== | ||
==Causes== | ==Causes== | ||
| Line 32: | Line 29: | ||
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. | Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. | ||
*[[Ventricular arrhythmia]] | |||
*[[Cardiac tamponade]] | |||
*[[Acute coronary syndrome]] | *[[Acute coronary syndrome]] | ||
*[[Third degree AV block]] | *[[Third degree AV block]] | ||
===Common causes=== | ===Common causes=== | ||
*Cardiac causes | *'''Cardiac causes''' | ||
:* | :*Arrhythmic | ||
::* [[Premature ventricular contraction]] | ::* [[Premature ventricular contraction]]s | ||
::* [[ | ::* [[Supraventricular tachycardia causes|Narrow complex tachycardia]] | ||
::* [[Wide complex tachycardia|Wide complex tachycardia]] | ::* [[Wide complex tachycardia causes|Wide complex tachycardia]] | ||
:* Non-arrhythmic | :* Non-arrhythmic | ||
::* [[Diseases of the valvular structures]] | ::* [[Diseases of the valvular structures|Valvular disease]] | ||
::* [[Pericarditis | ::* [[Pericarditis causes|Pericarditis]] | ||
::* | ::* Structural heart disease | ||
:* Malfunctioning | ::* Malfunctioning pacemaker | ||
*Psychiatric causes | *'''Psychiatric causes''' | ||
:* [[Anxiety]] | :* [[Anxiety]] | ||
:* [[Panic attack]] | :* [[Panic attack]] | ||
* | *'''Substance - drug causes''' | ||
:* [[Cardiac glycoside|Cardiac Glycosides]] | |||
:* [[Antiarrhythmics]] | |||
:* [[Sympathomimetics]] | |||
:* [[Insulin]] | |||
:* [[Thyroxine]] | |||
:* [[Alcohol]] | :* [[Alcohol]] | ||
:* [[Caffeine]] | :* [[Caffeine]] | ||
:* | :* [[Beta-blocker]] withdrawal | ||
:* [[Amphetamines]] | |||
:* [[Cannabis]] | |||
:* [[Cocaine]] | |||
*'''Systemic causes''' | |||
*Systemic causes | |||
:* [[Anemia]] | :* [[Anemia]] | ||
:* [[Fever]] | :* [[Fever]] | ||
:* [[Hyperthyroidism]] | :* [[Hyperthyroidism]] | ||
:* [[Hypoglycemia]] | :* [[Hypoglycemia]] | ||
:* [[Hypoxia]] | |||
:* [[Hypercapnia]] | |||
Click [[Palpitation causes#Causes|here]] for a | Click [[Palpitation causes#Causes|here]] for a complete list of causes. | ||
==FIRE: Focused Initial Rapid Evaluation== | ==FIRE: Focused Initial Rapid Evaluation== | ||
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 | A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="ACLS">{{Cite web | last = | first = | title = Part 8: Adult Advanced Cardiovascular Life Support | url = http://circ.ahajournals.org/content/122/18_suppl_3/S729.full | publisher = | date = | accessdate = 3 April 2014 }}</ref><br> | ||
<span style="font-size:85%">Boxes in the red signify that an urgent management is needed.</span | <span style="font-size:85%">Boxes in the red signify that an urgent management is needed.</span> | ||
<span style="font-size:85%">'''Abbreviations:''' | <span style="font-size:85%">'''Abbreviations:''' '''EKG:''' [[Electrocardiogram]]; '''IV:''' [[Intravenous therapy|Intravenous]]; '''NSTEMI:''' [[Non ST elevation myocardial infarction]]; '''STEMI:''' [[ST elevation myocardial infarction]]; '''TTE:''' [[Echocardiography|Transthoracic echocardiography]]; '''VT:''' [[Ventricular tachycardia]]; '''WPW:''' [[Wolff-Parkinson-White syndrome]]</span> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | {{familytree | | | | | | | | | | | | | B01 | | | | | | |B01=<div style="float: left; width: 15em; text-align: left; padding:1em;">'''Does the patient have any of the following findings that require urgent management?'''<br> | ||
❑ [[Syncope]] <br>(suggestive of [[VT]], complete AV block)<br> | |||
❑ | ❑ [[Hypotension]] or shock <br>(suggestive of [[VT]])<br> | ||
❑ [[Chest pain]] <br>(suggestive of [[ischemia]], complete AV block)<br> | |||
❑ | ❑ [[Shortness of breath]] <br>(suggestive of PE, cardiac tamponade, complete AV block)</div>}} | ||
{{familytree | | | | | | | | | | |,|-|-|^|-|-|.| | |}} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | W01 | | | | W02 | |W01={{fontcolor|#F8F8FF|'''Yes'''}}|W02=<div style="text-align: center; background: #FFFFFF; height: 25px; line-height: 25px;">'''No'''</div>}} | |||
{{familytree | | | | | | | | | | |!| | | | | |!| | }} | |||
{{familytree | | | | | | | | | | |!| | | | | S01 | | | | | |S01=<div style="width:15em">'''[[Palpitations resident survival guide#Complete_Diagnostic_Approach|Continue with the complete diagnostic approach below]]'''</div>}} | |||
{{familytree | | | | | | | | | | DAA | | | | | | | DAA=<div style=" background: #FA8072; text-align: center; width:15em; padding:0.7em"> {{fontcolor|#F8F8FF|'''Stabilize the patient'''}}</div> <div style=" background: #FA8072; text-align: left; padding:0.7em"> {{fontcolor|#F8F8FF|❑ Consider intubation if the patient's airway is compromised, has a Glasgow coma scale (GCS < 8) or profound hemodynamic instability<br> | |||
❑ Administer oxygen and maintain a saturation >90%<br> | |||
❑ Secure 2 large-bore intravenous lines (IVs) and initiate fluid resuscitation<br> | |||
: | ❑ Consider vasopressors only if patient remains hypotensive despite fluids<br> | ||
{{familytree | | | | | | | | | | |!| | | | | | |}} | |||
{{familytree | | | | | | | | | | | |||
❑ | |||
❑ | |||
❑ | |||
---- | ---- | ||
<center>'''Obtain the following'''</center><br> | |||
❑ 12 lead ECG <br> | |||
❑ Blood for [[CBC|<span style="color:white;">CBC</span>]], electrolytes, [[Cardiac enzymes|<span style="color:white;">troponin I, CK-MB</span>]], free T3/T4, toxicology screen | |||
❑ | |||
❑ [[ | |||
❑ Consider CTA if patient has a Wells score >4}} </div>|boxstyle= background: #FA8072}} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | |!| | | | | | | | | | |}} | |||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | F01 | | | | | | | | | |F01=<div style="float: center; width: 14em; padding:1em; color: #FFFFFF;"><center>Does the patient have any characteristic signs and symptoms or any [[EKG|<span style="color:white;">ECG</span>]] / lab abnormalities?</center></div>}} | |||
{{familytree | | | | | | |,|-|-|-|^|-|-|-|-|-|-|-|-|-|-|.|}} | |||
{{familytree | | | | | | C01 | | | | | | | | | | | | | C02 |C01={{fontcolor|#F8F8FF|'''Yes'''}}|C02={{fontcolor|#F8F8FF|'''No'''}}|boxstyle= background-color: #FA8072}} | |||
{{familytree | | | | | | |!| | | | | | | | | | | | | | |!| | }} | |||
{{familytree | | |,|-|-|-|+|-|-|-|v|-|-|-|v|-|-|-|.| | L01 | |L01=<div style="float: center; width: 14em; padding:1em; color: #FFFFFF;"><center>'''❑ Continue supportive care<br>❑ Place patient on cardiac monitor <br>❑ Re-evaluate if status worsens'''</center></div>|boxstyle= background-color: #FA8072}} | |||
{{familytree | | H01 | | H02 | | H03 | | H04 | | H05 | | | | | |H01=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Tachyarrhythmia'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Abnormal rhythm w/ a ventricular rate of ≥100/min<br><br><br></div> | |||
|H02=<div style="float: center; padding:1em; color: #FFFFFF; width:8em;"><center>'''Ischemia'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ ST-segment deviation<br>❑ Elevated cardiac biomarkers</div> | |||
|H03=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Cardiac Tamponade'''</center></div> | |||
---- | ---- | ||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Elevated JVP<br>❑ Pulsus paradoxus<br>❑ Low-voltage QRS complexes<br>❑ Electrical alternans<br> | |||
❑ PR segment depression</div> | |||
❑ | |H04=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Thyroid Storm'''</center></div> | ||
---- | ---- | ||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Suppressed TSH<br>❑ Elevated free T3/T4<br><br><br><br></div> | |||
❑ | |H05=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Pulmonary Embolism'''</center></div> | ||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Tachypnea<br>❑ Wells Score >4<br>❑ Positive chest CTA<br><br></div> | |||
❑ | |boxstyle= background-color: #FA8072}} | ||
</div>}} | {{familytree | | |!| | | |!| | | |!| | | |!| | | |!| | | | | | | |}} | ||
{{familytree | | | | | | | | {{familytree | | I01 | | I02 | | I03 | | I04 | | I05 | | | | | | |I01=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | ||
*[[Narrow_complex_tachycardia_resident_survival_guide#Treatment|<span style="color:white;">Supraventricular / Narrow-Complex Tachyarrhythmia Treatment Algorithm</span>]] | |||
{{familytree | | | | | | |||
*[[Wide_complex_tachycardia_resident_survival_guide#Treatment|<span style="color:white;">Ventricular / Wide-Complex Tachyarrhythmia Treatment Algorithm</span>]]</div> | |||
|I02=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Unstable_angina/_NSTEMI_resident_survival_guide|<span style="color:white;">UA / NSTEMI Treatment Algorithm</span>]] | |||
*[[STEMI_resident_survival_guide#FIRE:_Focused_Initial_Rapid_Evaluation|<span style="color:white;">STEMI Treatment Algorithm</span>]]<br><br><br><br><br><br></div> | |||
|I03=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Cardiac_tamponade_resident_survival_guide#Treatment|<span style="color:white;">Cardiac Tamponade Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|I04=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Hyperthroidism_resident_survival_guide#Treatment|<span style="color:white;">Thyroid Storm Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|I05=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Pulmonary_embolism_resident_survival_guide#Treatment|<span style="color:white;">Pulmonary Embolism Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|boxstyle= background-color: #FA8072}} | |||
{{familytree/end}} | {{familytree/end}} | ||
| Line 165: | Line 146: | ||
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Zimetbaum-1998">{{Cite journal | last1 = Zimetbaum | first1 = P. | last2 = Josephson | first2 = ME. | title = Evaluation of patients with palpitations. | journal = N Engl J Med | volume = 338 | issue = 19 | pages = 1369-73 | month = May | year = 1998 | doi = 10.1056/NEJM199805073381907 | PMID = 9571258 }}</ref><ref name="har">{{Cite web | last = | first = | title = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | url = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | publisher = | date = | accessdate = 16 April 2014 }}</ref><ref name="Abbott-2005">{{Cite journal | last1 = Abbott | first1 = AV. | title = Diagnostic approach to palpitations. | journal = Am Fam Physician | volume = 71 | issue = 4 | pages = 743-50 | month = Feb | year = 2005 | doi = | PMID = 15742913 }}</ref><ref name="Thavendiranathan-2009">{{Cite journal | last1 = Thavendiranathan | first1 = P. | last2 = Bagai | first2 = A. | last3 = Khoo | first3 = C. | last4 = Dorian | first4 = P. | last5 = Choudhry | first5 = NK. | title = Does this patient with palpitations have a cardiac arrhythmia? | journal = JAMA | volume = 302 | issue = 19 | pages = 2135-43 | month = Nov | year = 2009 | doi = 10.1001/jama.2009.1673 | PMID = 19920238 }}</ref><ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref> | A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Zimetbaum-1998">{{Cite journal | last1 = Zimetbaum | first1 = P. | last2 = Josephson | first2 = ME. | title = Evaluation of patients with palpitations. | journal = N Engl J Med | volume = 338 | issue = 19 | pages = 1369-73 | month = May | year = 1998 | doi = 10.1056/NEJM199805073381907 | PMID = 9571258 }}</ref><ref name="har">{{Cite web | last = | first = | title = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | url = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | publisher = | date = | accessdate = 16 April 2014 }}</ref><ref name="Abbott-2005">{{Cite journal | last1 = Abbott | first1 = AV. | title = Diagnostic approach to palpitations. | journal = Am Fam Physician | volume = 71 | issue = 4 | pages = 743-50 | month = Feb | year = 2005 | doi = | PMID = 15742913 }}</ref><ref name="Thavendiranathan-2009">{{Cite journal | last1 = Thavendiranathan | first1 = P. | last2 = Bagai | first2 = A. | last3 = Khoo | first3 = C. | last4 = Dorian | first4 = P. | last5 = Choudhry | first5 = NK. | title = Does this patient with palpitations have a cardiac arrhythmia? | journal = JAMA | volume = 302 | issue = 19 | pages = 2135-43 | month = Nov | year = 2009 | doi = 10.1001/jama.2009.1673 | PMID = 19920238 }}</ref><ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref> | ||
<span style="font-size:85%"> '''Abbreviations:''' '''AF:''' [[Atrial fibrillation]]; '''AVRT:''' [[AV reentry tachycardia]]; '''AVNRT:''' [[AV nodal reentry tachycardia]]; '''BP:''' [[Blood pressure]]; '''CBC:''' [[Complete blood count]]; '''EKG:''' [[Electrocardiogram]]; '''EPS:''' [[Electrophysiology|Electrophysiological study]] '''SVT:''' [[Supraventricular tachycardia]] '''TSH:''' [[Thyroid stimulating hormone]]; '''TTE:''' [[Echocardiography| | <span style="font-size:85%"> '''Abbreviations:''' '''AF:''' [[Atrial fibrillation]]; '''AVRT:''' [[AV reentry tachycardia]]; '''AVNRT:''' [[AV nodal reentry tachycardia]]; '''BP:''' [[Blood pressure]]; '''CBC:''' [[Complete blood count]]; '''EKG:''' [[Electrocardiogram]]; '''EPS:''' [[Electrophysiology|Electrophysiological study]] '''SVT:''' [[Supraventricular tachycardia]] '''TSH:''' [[Thyroid stimulating hormone]]; '''TTE:''' [[Echocardiography|Transthoracic echocardiography]]; '''VT:''' [[Ventricular tachycardia]]; '''WPW:''' [[Wolff-Parkinson-White syndrome]] </span> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | A01 | | | | |A01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Characterize the symptoms:'''<br> | {{familytree | | | | | | | A01 | | | | |A01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Characterize the symptoms:'''<br> | ||
❑ ''' | ❑ '''Character of palpitations'''<br> | ||
: ❑ Flip-flopping of the [[chest]]<br> | |||
: ❑ Rapid fluttering of the [[chest]] <br> | |||
: ❑ Pounding in the [[neck]] <br> | |||
: ❑ Pulsation [[palpitations]] <br> | |||
: ❑ Flip-flopping of the [[chest]] | |||
: ❑ Rapid fluttering of the [[chest]] | |||
: ❑ Pounding in the [[neck]] | |||
: ❑ Pulsation [[palpitations]] | |||
: ❑ [[Anxiety|Anxiety-related]] palpitations<br> | : ❑ [[Anxiety|Anxiety-related]] palpitations<br> | ||
❑ ''' | ❑ '''Onset'''<br> | ||
: ❑ [[ | : ❑ Sudden <br> | ||
: ❑ [[ | : ❑ Gradual<br> | ||
❑ '''Duration'''<br> | |||
: ❑ Brief<br> | |||
: ❑ Persistent<br> | |||
❑ '''Frequency'''<br> | |||
: ❑ Daily | |||
: ❑ Weekly | |||
: ❑ Monthly<br> | |||
❑ '''Termination'''<br> | |||
: ❑ Successful with [[vagal maneuvers]] (suggestive of [[SVT]])<br> | |||
❑ '''Associated with'''<br> | |||
: ❑ Sudden changes of posture (suggestive of [[Orthostatic hypotension|intolerance to orthostasis]] or [[AVNRT]])<br> | |||
: ❑ [[Syncope]]<br> | : ❑ [[Syncope]]<br> | ||
: | : ❑ [[Angina]], [[dyspnea]], [[fatigue]], [[vertigo]], [[dizziness]]<br> | ||
: ❑ [[Polyuria]] (suggestive of [[AF]])<br> | |||
: ❑ Rapid regular pulse in the [[neck]]<br> | |||
❑ [[Angina]], [[dyspnea]], [[fatigue]] | |||
❑ [[Polyuria]] (suggestive of [[AF]])<br> | |||
❑ Rapid regular pulse in the [[neck]] | |||
</div>}} | </div>}} | ||
{{familytree | | | | | | | |!| | | | | | | |}} | {{familytree | | | | | | | |!| | | | | | | |}} | ||
{{familytree | | | | | | | B01 | | | | | |B01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Inquire about drugs that can cause palpitations:'''<br> | {{familytree | | | | | | | B01 | | | | | |B01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Inquire about drugs that can cause palpitations:'''<br> | ||
❑ [[Sympathomimetic | ❑ [[Sympathomimetic|Sympathomimetic agents]] <br> | ||
❑ Inhaled beta-agonists <br> | |||
❑ [[Vasodilator|Vasodilators]]<br> | ❑ [[Vasodilator|Vasodilators]]<br> | ||
❑ [[Anticholinergic|Anticholinergic agents]]<br> | ❑ [[Anticholinergic|Anticholinergic agents]]<br> | ||
❑ | ❑ [[Beta-blocker]] withdrawal<br> | ||
❑ [[Alcohol]]<br> | ❑ Recreational drugs<br> | ||
❑ [[Cocaine]]<br> | : ❑ [[Alcohol]]<br> | ||
❑ [[Heroin]]<br> | : ❑ [[Cocaine]]<br> | ||
❑ [[Amphetamines]]<br> | : ❑ [[Heroin]]<br> | ||
❑ [[Caffeine]]<br> | : ❑ [[Amphetamines]]<br> | ||
❑ [[Nicotine]]<br> | : ❑ [[Caffeine]]<br> | ||
❑ [[Cannabis]]<br> | : ❑ [[Nicotine]]<br> | ||
❑ Synthetic drugs<br> | : ❑ [[Cannabis]]<br> | ||
: ❑ Synthetic drugs<br> | |||
❑ Weight reduction drugs<br> | ❑ Weight reduction drugs<br> | ||
</div>}} | </div>}} | ||
| Line 222: | Line 197: | ||
❑ Previous episodes of palpitations<br> | ❑ Previous episodes of palpitations<br> | ||
: ❑ First episode | : ❑ First episode | ||
: ❑ Number of episodes<br> | : ❑ Number of episodes<br> | ||
: ❑ Time since last episode<br> | : ❑ Time since last episode<br> | ||
| Line 246: | Line 219: | ||
: ❑ [[Rhythm]]<br> | : ❑ [[Rhythm]]<br> | ||
:: ❑ Regular (suggestive of [[SVT]] or [[VT]])<br> | :: ❑ Regular (suggestive of [[SVT]] or [[VT]])<br> | ||
:: ❑ Irregular (suggestive of [[ | :: ❑ Irregular (suggestive of [[premature ventricular beats]])<br> | ||
:: ❑ Irregularly irregular (suggestive of [[AF]])<br> | :: ❑ Irregularly irregular (suggestive of [[AF]])<br> | ||
: ❑ [[Rate]]<br> | : ❑ [[Rate]]<br> | ||
:: ❑ [[Tachycardia]]<br> | :: ❑ [[Tachycardia]]<br> | ||
:: ❑ [[Bradycardia]] (suggestive of [[sinus bradycardia]], [[AV block]]) | :: ❑ [[Bradycardia]] (suggestive of [[sinus bradycardia]], [[AV block]]) | ||
: ❑ [[Pulse]] deficit (suggestive of [[AF]] or [[premature ventricular beats]]) | : ❑ [[Pulse]] deficit (suggestive of [[AF]] or [[premature ventricular beats]]) | ||
❑ [[Blood pressure]]<br> | ❑ [[Blood pressure]]<br> | ||
: ❑ [[Hypotension]] | : ❑ [[Hypotension]]<br> | ||
: ❑ [[Orthostatic hypotension]] | : ❑ [[Orthostatic hypotension]]<br> | ||
: ❑ [[Hypertension]]<br> | : ❑ [[Hypertension]]<br> | ||
❑ [[Temperature]]<br> | ❑ [[Temperature]]<br> | ||
: ❑ [[Fever]] (suggestive of [[infection]])<br> | : ❑ [[Fever]] (suggestive of [[infection]])<br> | ||
❑ [[ | ❑ [[Tachypnea]] (non-specific)<br> | ||
''' | '''Eyes'''<br> | ||
❑ [[Exophthalmos]] (suggestive of [[Graves disease]])<br> | ❑ [[Exophthalmos]] (suggestive of [[Graves disease]])<br> | ||
'''Neck'''<br> | '''Neck'''<br> | ||
| Line 267: | Line 238: | ||
❑ [[Jugular venous pulse]]: [[cannon A wave]] (suggestive of [[Atrioventricular dissociation|AV dissociation]])<br> | ❑ [[Jugular venous pulse]]: [[cannon A wave]] (suggestive of [[Atrioventricular dissociation|AV dissociation]])<br> | ||
'''Skin'''<br> | '''Skin'''<br> | ||
❑ Hot and sweaty (suggestive of [[hyperthyroidism]])<br> | ❑ Hot and sweaty (suggestive of [[hyperthyroidism]] or [[fever]])<br> | ||
'''Hair'''<br> | '''Hair'''<br> | ||
❑ Thin (suggestive of [[hyperthyroidism]])<br> | ❑ Thin (suggestive of [[hyperthyroidism]])<br> | ||
| Line 274: | Line 245: | ||
❑ [[Wheezing]] (non-specific)<br> | ❑ [[Wheezing]] (non-specific)<br> | ||
'''Cardiovascular'''<br> | '''Cardiovascular'''<br> | ||
❑ [[Muffled heart sounds]] | ❑ [[Muffled heart sounds]]<br> | ||
❑ [[Pericardial friction rub]] (suggestive of [[pericarditis]])<br> | ❑ [[Pericardial friction rub]] (suggestive of [[pericarditis]])<br> | ||
❑ [[Murmurs]] (suggestive of [[valve disease]])<br> | ❑ [[Murmurs]] (suggestive of [[valve disease]])<br> | ||
❑ Displaced [[apex beat]] (suggestive of [[cardiomegaly]]<br> | ❑ Displaced [[apex beat]] (suggestive of [[cardiomegaly]]<br> | ||
❑ [[S3]] (suggestive of [[heart failure]])<br> | ❑ [[S3]] (suggestive of [[heart failure]])<br> | ||
❑ [[S4]]<br> | |||
'''Neurologic'''<br> | '''Neurologic'''<br> | ||
❑ [[Tremors]] (suggestive of [[panic attacks]] or [[hyperthyroidism]])<br> | ❑ [[Tremors]] (suggestive of [[panic attacks]] or [[hyperthyroidism]])<br> | ||
| Line 289: | Line 259: | ||
: ❑ Determine if the rhythm is regular or irregular | : ❑ Determine if the rhythm is regular or irregular | ||
: ❑ Assess the [[p wave]] and [[QRS]] morphology | : ❑ Assess the [[p wave]] and [[QRS]] morphology | ||
: ❑ Rate over 100 bpm, QRS <120 ms (suggestive of [[Narrow complex tachycardia resident survival guide|narrow complex tachycardia]]) | : ❑ Rate over 100 bpm, QRS < 120 ms (suggestive of [[Narrow complex tachycardia resident survival guide|narrow complex tachycardia]]) | ||
: ❑ Search for short [[PR intervals]] and [[delta waves]] (suggestive of [[WPW]]) | : ❑ Search for short [[PR intervals]] and [[delta waves]] (suggestive of [[WPW]]) | ||
: ❑ Irregular rhythm, change in [[p wave]] morphology (suggestive of [[AF]]) | : ❑ Irregular rhythm, change in [[p wave]] morphology (suggestive of [[AF]]) | ||
: ❑ Regular rhythm, saw-tooth appearance (suggestive of [[atrial flutter]]) | : ❑ Regular rhythm, saw-tooth appearance (suggestive of [[atrial flutter]]) | ||
: ❑ Rate over 100 bpm, [[QRS]] >120 ms (suggestive of [[Wide complex tachycardia resident survival guide|wide complex tachycardia | : ❑ Rate over 100 bpm, [[QRS]] > 120 ms (suggestive of [[Wide complex tachycardia resident survival guide|wide complex tachycardia]]) | ||
: ❑ Search for deep septal [[Q waves]] in [[Introduction to ECG#Leads|I]], [[Introduction to ECG#Leads|V4]] to [[Introduction to ECG#Leads|V6]] and signs of [[left ventricular hypertrophy]] (suggestive of [[hypertrophic obstructive cardiomyopathy]]) | : ❑ Search for deep septal [[Q waves]] in [[Introduction to ECG#Leads|I]], [[Introduction to ECG#Leads|V4]] to [[Introduction to ECG#Leads|V6]] and signs of [[left ventricular hypertrophy]] (suggestive of [[hypertrophic obstructive cardiomyopathy]]) | ||
: ❑ Normal [[EKG]] (suggestive of [[anxiety]] or [[panic attack]]) | : ❑ Normal [[EKG]] (suggestive of [[anxiety]] or [[panic attack]]) | ||
❑ [[CBC]] (to rule out [[anemia]] or [[infection]])<br> | ❑ [[CBC]] (to rule out [[anemia]] or [[infection]])<br> | ||
❑ [[Electrolyte disturbances|Electrolytes]] (to rule out | ❑ [[Electrolyte disturbances|Electrolytes]] (to rule out potassium and magnesium imbalances)<br> | ||
❑ [[TSH]] (to rule out [[hyperthyroidism]])<br> | ❑ [[TSH]] (to rule out [[hyperthyroidism]])<br> | ||
❑ [[Blood sugar|Glucose level]] (to rule out [[hypoglycemia]])<br> | ❑ [[Blood sugar|Glucose level]] (to rule out [[hypoglycemia]])<br> | ||
| Line 306: | Line 275: | ||
❑ [[TTE]] (to rule out [[structural heart disease]])<br> | ❑ [[TTE]] (to rule out [[structural heart disease]])<br> | ||
</div>}} | </div>}} | ||
{{familytree | {{familytree | | | | | | |!| | | | | | | |}} | ||
{{familytree | {{familytree | | | | | | W01 | | | | | | | |W01= <div style="float: left; text-align: left; width: 24em; padding:1em;">'''Consider hospitalization'''<br> | ||
❑ Recurrent episodes when no ambulatory [[EKG]] devices are available<br> | ❑ Recurrent episodes when no ambulatory [[EKG]] devices are available<br> | ||
❑ [[Structural heart disease|Severe structural heart disease]], family history of [[sudden cardiac death]] and/or [[Electrical conduction system of the heart|heart conduction abnormalities]]</div>}} | ❑ [[Structural heart disease|Severe structural heart disease]], family history of [[sudden cardiac death]] and/or [[Electrical conduction system of the heart|heart conduction abnormalities]]</div>}} | ||
{{familytree | {{familytree | | | | | | |!| | | | | | | }} | ||
{{familytree | {{familytree | | | | | | Y01 | | | | | |Y01='''Does the patient have clinical or [[EKG]] findings suggestive of a cardiac cause of the palpitations?'''}} | ||
{{familytree | | | |, | {{familytree | | | |,|-|-|^|-|-|-|-|-|-|-|-|-|.| |}} | ||
{{familytree | | | F01 | | | | | | | | | | | F02 | | | F01='''Yes''' | F02='''No'''}} | |||
{{familytree | | | | {{familytree | |,|-|^|-|v|-|-|-|.| | | | | | |!|}} | ||
{{familytree | S01 | | S02 | | S03 | | | | | S04 | | | |S01=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Arrhythmia'''<br> | |||
{{familytree | |,|-|^|-| | ❑ [[Premature ventricular beat]]<br> | ||
{{familytree | | |||
❑ [[ | |||
❑ [[Narrow complex tachycardia resident survival guide#Complete Diagnostic Approach|Narrow complex tachycardia]]<br> | ❑ [[Narrow complex tachycardia resident survival guide#Complete Diagnostic Approach|Narrow complex tachycardia]]<br> | ||
❑ [[Wide complex tachycardia resident survival guide#Complete Diagnostic Approach|Wide complex tachycardia]]<br> | ❑ [[Wide complex tachycardia resident survival guide#Complete Diagnostic Approach|Wide complex tachycardia]]<br> | ||
❑ [[Bradycardia resident survival guide#Complete Diagnostic Approach|Bradyarrhythmias]]<br> | ❑ [[Bradycardia resident survival guide#Complete Diagnostic Approach|Bradyarrhythmias]]<br> | ||
❑ [[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|Wolff-Parkinson-White syndrome]]<br> | ❑ [[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|Wolff-Parkinson-White syndrome]]<br> | ||
</div>| | </div>|S02=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Myocardial ischemia'''<br> | ||
<span style=" | ❑ [[Acute coronary syndrome]]<br> | ||
: ❑ [[STEMI resident survival guide#Diagnosis|STEMI]]<br> | |||
: ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|NSTEMI]]<br> | |||
: ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|Unstable angina]]<br> | |||
</div>|S03=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Other EKG findings'''</div>|S04=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Does the patient have a history of [[psychiatric disorder]]s?'''</div>}} | |||
{{familytree | | | | | | |,|-|^|-|.| | | |,|-|^|-|.| | |}} | |||
{{familytree | | | | | | R01 | | R02 | | R03 | | R04 | | |R01=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''EKG findings suggestive of pericarditis'''<br> | |||
[[Pericarditis resident survival guide#FIRE: Focused Initial Rapid Evaluation|<span style="color:white;">Pericarditis</span>]]<br> | |||
❑ [[ST segment elevation]] in leads I, II, aVL, aVF, and V3-V6<br> | |||
❑ [[PR segment depression]]<br> | |||
❑ [[Low QRS voltage]] (in large [[Pericardial effusion]] and [[Constrictive pericarditis]])<br> | |||
</div>|R02='''Non-specific EKG findings'''|R03='''Yes'''|R04='''No'''}} | |||
{{familytree | | | | | | | | | | | |!| | | |!| | | |!| | }} | |||
{{familytree | | | | | | | | | | | T01 | | T02 | | T03 | | |T01='''Order a TTE'''|T02=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | |||
Consider the following if all diagnostic tests are normal:<br> | |||
❑ [[ | ❑ [[Anxiety]]<br> | ||
❑ [[Panic attack]]<br> | |||
❑ [[Depression]]<br> | |||
❑ [[Somatization]]<br> | |||
</div>|T03=<div style="float: left; text-align: left; width: 12em; padding:1em;">'''Is the patient taking any substances/drugs that can cause palpitations?'''</div>}} | |||
{{familytree | | | | | | | | | | | |!| | | | |,|-|-|^|-|-|.| | |}} | |||
{{familytree | | | | | | | | | | | Q01 | | | Z01 | | | | Z02 | | | | |Q01=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | |||
❑ [[Congenital heart disease]]<br> | ❑ [[Congenital heart disease]]<br> | ||
❑ [[Cardiomyopathy]]<br> | ❑ [[Cardiomyopathy]]<br> | ||
❑ [[Heart failure resident survival guide#Complete Diagnostic Approach|Congestive heart failure]]<br> | ❑ [[Heart failure resident survival guide#Complete Diagnostic Approach|Congestive heart failure]]<br> | ||
❑ [[Pericarditis resident survival guide#Complete Diagnostic Approach|Pericarditis]]<br> | ❑ [[Pericarditis resident survival guide#Complete Diagnostic Approach|Pericarditis]]<br> | ||
❑ [[Valvular disease]]<br> | ❑ [[Valvular disease]]<br> | ||
: ❑ [[Aortic stenosis resident survival guide#Complete Diagnostic Approach|Aortic stenosis]]<br> | : ❑ [[Aortic stenosis resident survival guide#Complete Diagnostic Approach|Aortic stenosis]]<br> | ||
: ❑ [[ | : ❑ [[Mitral valve prolapse]]<br> | ||
</div>| | </div>|Z01='''Yes'''|Z02='''No'''}} | ||
{{familytree | | | | | | | | | | | | | | | | |!| | | | | |!| | | |}} | |||
{{familytree | | | | | | | | | | | | | | | | I03 | | | | I04 | | | |I03=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | |||
<span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | <span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | ||
❑ [[Acute alcohol intoxication|Alcohol]]<br> | ❑ [[Acute alcohol intoxication|Alcohol]]<br> | ||
❑ [[Caffeine#Overuse|Caffeine]]<br> | ❑ [[Caffeine#Overuse|Caffeine]]<br> | ||
| Line 360: | Line 331: | ||
: ❑ [[Vasodilator|Vasodilators]]<br> | : ❑ [[Vasodilator|Vasodilators]]<br> | ||
: ❑ [[Anticholinergic#Effects|Anticholinergic agents]]<br> | : ❑ [[Anticholinergic#Effects|Anticholinergic agents]]<br> | ||
: ❑ | : ❑ [[Beta-blocker]] withdrawal<br> | ||
: ❑ [[Beta-agonists]]<br> | : ❑ [[Beta-agonists]]<br> | ||
: ❑ [[Digoxin#Wanrings|Digitalis]]<br> | : ❑ [[Digoxin#Wanrings|Digitalis]]<br> | ||
| Line 369: | Line 340: | ||
: ❑ [[Amphetamines]] | : ❑ [[Amphetamines]] | ||
❑ [[Nicotine]] | ❑ [[Nicotine]] | ||
</div>| | </div>|I04=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | ||
<span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | <span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | ||
❑ [[Anemia]]<br> | ❑ [[Anemia]]<br> | ||
❑ [[Electrolyte disturbances]]<br> | ❑ [[Electrolyte disturbances]]<br> | ||
| Line 384: | Line 354: | ||
==Treatment== | ==Treatment== | ||
The management of palpitations | The management of palpitations should be directed towards the underlying cause. If the etiology can be determined and low risk, potentially curative treatments are available these should be the first choice of management. For benign arrhythmias, such as extrasystole, lifestyle changes may be sufficient to prevent future episodes. For patients in whom no clear disease has been established, patients should be advised to avoid possible triggers of palpitations such as caffeine, alcohol, nicotine, recreational drugs.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Zimetbaum-1998">{{Cite journal | last1 = Zimetbaum | first1 = P. | last2 = Josephson | first2 = ME. | title = Evaluation of patients with palpitations. | journal = N Engl J Med | volume = 338 | issue = 19 | pages = 1369-73 | month = May | year = 1998 | doi = 10.1056/NEJM199805073381907 | PMID = 9571258 }}</ref><ref name="har">{{Cite web | last = | first = | title = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | url = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | publisher = | date = | accessdate = 16 April 2014 }}</ref><ref name="Abbott-2005">{{Cite journal | last1 = Abbott | first1 = AV. | title = Diagnostic approach to palpitations. | journal = Am Fam Physician | volume = 71 | issue = 4 | pages = 743-50 | month = Feb | year = 2005 | doi = | PMID = 15742913 }}</ref><ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | ||
<span style="font-size:85%">'''Abbreviations:''' '''NSTEMI:''' [[Non ST elevation myocardial infarction]]; '''STEMI:''' [[ST elevation myocardial infarction]]</span> | <span style="font-size:85%">'''Abbreviations:''' '''NSTEMI:''' [[Non ST elevation myocardial infarction]]; '''STEMI:''' [[ST elevation myocardial infarction]]</span> | ||
| Line 390: | Line 360: | ||
{{familytree | | | | | | | | A01 | | | | | | | | | | |A01='''Determine the cause of the palpitations'''}} | {{familytree | | | | | | | | A01 | | | | | | | | | | |A01='''Determine the cause of the palpitations'''}} | ||
{{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | | | | | | }} | {{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | | | | | | }} | ||
{{familytree | | | B01 | | | | | | | | B02 | | | | | | |B01=<div style="float: left; text-align: left; width: 08em; padding:1em;">'''Cardiac cause'''</div>|B02=''' | {{familytree | | | B01 | | | | | | | | B02 | | | | | | |B01=<div style="float: left; text-align: left; width: 08em; padding:1em;">'''Cardiac cause'''</div>|B02='''Non-cardiac cause'''}} | ||
{{familytree | |,|-|^|-|.| | | |,|-|-|-|+|-|-|-|.| | | |}} | {{familytree | |,|-|^|-|.| | | |,|-|-|-|+|-|-|-|.| | | |}} | ||
{{familytree | C01 | | C02 | | C03 | | C04 | | C05 | | | |C01=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Arrhythmia'''<br> | {{familytree | C01 | | C02 | | C03 | | C04 | | C05 | | | |C01=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Arrhythmia'''<br> | ||
| Line 414: | Line 384: | ||
: [[Aortic stenosis resident survival guide#treatment|Aortic stenosis]]<br> | : [[Aortic stenosis resident survival guide#treatment|Aortic stenosis]]<br> | ||
: [[Aortic regurgitation resident survival guide#Treatment|Aortic regurgitation]]<br> | : [[Aortic regurgitation resident survival guide#Treatment|Aortic regurgitation]]<br> | ||
</div>|C03=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Psychiatric | </div>|C03=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Psychiatric disorder'''<br> | ||
[[Anxiety]]<br> | [[Anxiety]]<br> | ||
[[Panic attack]]<br> | [[Panic attack]]<br> | ||
[[Depression]]<br> | [[Depression]]<br> | ||
[[Somatization]]<br> | [[Somatization]]<br> | ||
</div>|C04=<div style="float: left; text-align: left; width: 16em; padding:1em;">''' | </div>|C04=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Substance/drug intake'''<br> | ||
❑ [[Alcohol]]<br> | ❑ [[Alcohol]]<br> | ||
❑ [[Caffeine]]<br> | ❑ [[Caffeine]]<br> | ||
| Line 426: | Line 396: | ||
: ❑ [[Vasodilators]]<br> | : ❑ [[Vasodilators]]<br> | ||
: ❑ [[Anticholinergic|Anticholinergic agents]]<br> | : ❑ [[Anticholinergic|Anticholinergic agents]]<br> | ||
: ❑ | : ❑ [[Beta-blocker]] withdrawal<br> | ||
: ❑ [[Beta-agonists]]<br> | : ❑ [[Beta-agonists]]<br> | ||
: ❑ [[Digitalis]]<br> | : ❑ [[Digitalis]]<br> | ||
| Line 458: | Line 428: | ||
==Do's== | ==Do's== | ||
* If possible, perform physical exam and [[EKG]] when the patient is symptomatic.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | * If possible, perform a physical exam and an [[EKG|ECG]] when the patient is symptomatic.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* | * If a patient is asymptomatic, search for signs of [[structural heart disease]] such as [[murmurs]], displaced [[apex beat]] or [[S3]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an ambulatory [[EKG]] in patients with recurrent episodes of [[palpitations]] | * Perform an ambulatory [[EKG|ECG]] in patients with recurrent episodes of [[palpitations]] of undetermined etiology.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[Electrophysiology|EPS]] | * Perform an electrophysiologic study ([[Electrophysiology|EPS]]) for patients with inconclusive ambulatory [[EKG|ECG]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[Electrophysiology|EPS]], with [[Catheter ablation|ablation therapy]] if necessary, in patients severe [[heart disease]], when [[palpitations]] preceded [[syncope]] and when the patient | * Perform an [[Electrophysiology|EPS]], with [[Catheter ablation|ablation therapy]] if necessary, in patients with severe [[heart disease]], particularly when [[palpitations]] preceded [[syncope]] and when the patient required cardio-respiratory resuscitation maneuvers.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Thavendiranathan-2009">{{Cite journal | last1 = Thavendiranathan | first1 = P. | last2 = Bagai | first2 = A. | last3 = Khoo | first3 = C. | last4 = Dorian | first4 = P. | last5 = Choudhry | first5 = NK. | title = Does this patient with palpitations have a cardiac arrhythmia? | journal = JAMA | volume = 302 | issue = 19 | pages = 2135-43 | month = Nov | year = 2009 | doi = 10.1001/jama.2009.1673 | PMID = 19920238 }}</ref> | ||
* | * Advise life-style changes that may lower the possibility of future episodes, such as exercise, lower [[alcohol]] and [[caffeine]] intake, and [[Smoking|smoking cessation]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[exercise stress test]] in patients with exercise induced [[palpitations]].<ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | * Perform an [[exercise stress test]] in patients with exercise induced [[palpitations]].<ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | ||
==EKG | ==EKG gallery== | ||
===Narrow complex tachycardia=== | ===Narrow complex tachycardia=== | ||
{| style="cellpadding=0; cellspacing= 0; width: 800px;" | {| style="cellpadding=0; cellspacing= 0; width: 800px;" | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Type of [[Arrhythmia]]'''||style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''[[EKG]]''' (lead II) | | style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''Type of [[Arrhythmia]]'''|| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''[[EKG]]''' (lead II) || style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''Clues''' | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left| '''[[Sinus tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:Sinus tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': gradual<br> '''Rhythm''': regular<br> '''Rate''': >220 minus the age of the patient <br> '''Response to adenosine''': transient decrease of the rate | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" | '''[[Sinus tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:Sinus tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': gradual<br> '''Rhythm''': regular<br> '''Rate''': >220 minus the age of the patient <br> '''Response to adenosine''': transient decrease of the rate | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Atrial fibrillation]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:atrial fibrillation.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': irregular <br> '''Rate''':100-180 bpm <br> '''Response to adenosine''': transient decrease of the ventricular rate | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Atrial fibrillation]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:atrial fibrillation.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': irregular <br> '''Rate''':100-180 bpm <br> '''Response to adenosine''': transient decrease of the ventricular rate | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Atrial flutter]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:atrial flutter.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': >150 bpm <br> '''Response to adenosine''': transient decrease of the rate <br> Presence of saw-tooth appearance | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Atrial flutter]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:atrial flutter.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': >150 bpm <br> '''Response to adenosine''': transient decrease of the rate <br> Presence of saw-tooth appearance | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[AVNRT]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:AVNRT.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[AVNRT]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:AVNRT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[AVRT]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:AVRT.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left| '''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[AVRT]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:AVRT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" | '''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Focal atrial tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:focal atrial tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Focal atrial tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:focal atrial tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Junctional tachycardia|Nonparoxysmal junctional tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:JTS.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Rhythm''': regular <br> Retrograde P wave<br> Most commonly due to ischemia or digitalis toxicity | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Junctional tachycardia|Nonparoxysmal junctional tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:JTS.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Rhythm''': regular <br> Retrograde P wave<br> Most commonly due to ischemia or digitalis toxicity | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Multifocal atrial tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:MAT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': gradual<br> '''Rhythm''': irregular<br> '''Rate''': 100-150 bpm <br> '''Response to adenosine''': no effect<br>3 different [[P wave]] morphologies | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Multifocal atrial tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:MAT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': gradual<br> '''Rhythm''': irregular<br> '''Rate''': 100-150 bpm <br> '''Response to adenosine''': no effect<br>3 different [[P wave]] morphologies | ||
|- | |- | ||
|} | |} | ||
===Wide complex tachycardia=== | ===Wide complex tachycardia=== | ||
| Line 505: | Line 472: | ||
!p-wave | !p-wave | ||
!Effect of adenosine | !Effect of adenosine | ||
|- | |- | ||
| colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Wide complex (QRS > 0.12)''' | | colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Wide complex (QRS > 0.12)''' | ||
|- | |- | ||
| Line 561: | Line 528: | ||
| [[AV-dissociation]] | | [[AV-dissociation]] | ||
| no rate reduction | | no rate reduction | ||
|- | |- | ||
|colspan="8"|* Bundle-branch re-entrant tachycardia is extremely rare | | colspan="8" |* Bundle-branch re-entrant tachycardia is extremely rare | ||
|} | |} | ||
| Line 569: | Line 536: | ||
[[Image:STEMI evolution.png|center|800px]] | [[Image:STEMI evolution.png|center|800px]] | ||
===[[Unstable angina/non ST elevation myocardial infarction electrocardiogram|NSTEMI]]=== | ===[[Unstable angina/non ST elevation myocardial infarction electrocardiogram|NSTEMI]]=== | ||
Shown below is an EKG showing an [[ST depression]] in [[Electrocardiogram#Precordial|V2]], [[Electrocardiogram#Precordial|V3]], [[Electrocardiogram#Precordial|V4]] and [[Electrocardiogram#Precordial|V6]]. | Shown below is an EKG showing an [[ST depression]] in [[Electrocardiogram#Precordial|V2]], [[Electrocardiogram#Precordial|V3]], [[Electrocardiogram#Precordial|V4]] and [[Electrocardiogram#Precordial|V6]]. | ||
[[Image:unstable-angina.jpg|center| | [[Image:unstable-angina.jpg|center|800px]] | ||
---- | |||
Shown below is an [[EKG]] showing an inversion in the T wave at leads [[Electrocardiogram#Precordial|V4]], [[Electrocardiogram#Precordial|V5]] and [[Electrocardiogram#Precordial|V6]]. | |||
[[Image:T wave inversion in V4, V5 and V6.png|center|800px]] | |||
===Pericarditis=== | ===Pericarditis=== | ||
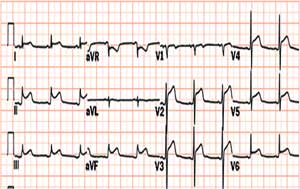
Shown below is an [[EKG]] with [[ST elevation]] in lead I, II, V2, V3, V4, V5 and V6. | Shown below is an [[EKG]] with [[ST elevation]] in lead [[Electrocardiogram#Augmented limb Leads|I]], [[Electrocardiogram#Augmented limb Leads|II]], [[Electrocardiogram#Precordial|V2]], [[Electrocardiogram#Precordial|V3]], [[Electrocardiogram#Precordial|V4]], [[Electrocardiogram#Precordial|V5]] and [[Electrocardiogram#Precordial|V6]]. | ||
[[Image:Acute-pericarditis.jpg|center| | [[Image:Acute-pericarditis.jpg|center|800px|thumb|ST elevation in leads I, II, V2, V3, V4, V5, and V6 depicting acute pericarditis]] | ||
==References== | ==References== | ||
| Line 588: | Line 556: | ||
[[Category:Resident survival guide]] | [[Category:Resident survival guide]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Emergency]] | [[Category:Emergency medicine]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
</div> | </div> | ||
Latest revision as of 16:20, 4 May 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D.
| Palpitations Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Gallery |
Overview
Causes
Life-Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common causes
- Cardiac causes
- Arrhythmic
- Non-arrhythmic
- Valvular disease
- Pericarditis
- Structural heart disease
- Malfunctioning pacemaker
- Psychiatric causes
- Substance - drug causes
- Systemic causes
Click here for a complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[1][2]
Boxes in the red signify that an urgent management is needed.
Abbreviations: EKG: Electrocardiogram; IV: Intravenous; NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Does the patient have any of the following findings that require urgent management? ❑ Syncope (suggestive of PE, cardiac tamponade, complete AV block) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Stabilize the patient ❑ Consider intubation if the patient's airway is compromised, has a Glasgow coma scale (GCS < 8) or profound hemodynamic instability ❑ Administer oxygen and maintain a saturation >90% ❑ 12 lead ECG | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Place patient on cardiac monitor ❑ Re-evaluate if status worsens | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Abnormal rhythm w/ a ventricular rate of ≥100/min | ❑ ST-segment deviation ❑ Elevated cardiac biomarkers | ❑ Elevated JVP ❑ Pulsus paradoxus ❑ Low-voltage QRS complexes ❑ Electrical alternans ❑ PR segment depression | ❑ Suppressed TSH ❑ Elevated free T3/T4 | ❑ Tachypnea ❑ Wells Score >4 ❑ Positive chest CTA | |||||||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1][3][4][5][6][7]
Abbreviations: AF: Atrial fibrillation; AVRT: AV reentry tachycardia; AVNRT: AV nodal reentry tachycardia; BP: Blood pressure; CBC: Complete blood count; EKG: Electrocardiogram; EPS: Electrophysiological study SVT: Supraventricular tachycardia TSH: Thyroid stimulating hormone; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Characterize the symptoms: ❑ Character of palpitations
❑ Onset
❑ Duration
❑ Frequency
❑ Termination
❑ Associated with | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Inquire about drugs that can cause palpitations: ❑ Sympathomimetic agents ❑ Weight reduction drugs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed past medical history: ❑ Previous episodes of palpitations
❑ Cardiac arrhythmia ❑ History of panic attacks | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vitals
❑ Tachypnea (non-specific) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order labs and tests: ❑ EKG
❑ CBC (to rule out anemia or infection) Order imaging studies | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Recurrent episodes when no ambulatory EKG devices are available | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have clinical or EKG findings suggestive of a cardiac cause of the palpitations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Other EKG findings | Does the patient have a history of psychiatric disorders? | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
EKG findings suggestive of pericarditis Pericarditis | Non-specific EKG findings | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order a TTE | Consider the following if all diagnostic tests are normal: ❑ Anxiety | Is the patient taking any substances/drugs that can cause palpitations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Click in each link for the specific diagnostic approach and management
❑ Recreational drugs
❑ Nicotine | Click in each link for the specific diagnostic approach and management | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
The management of palpitations should be directed towards the underlying cause. If the etiology can be determined and low risk, potentially curative treatments are available these should be the first choice of management. For benign arrhythmias, such as extrasystole, lifestyle changes may be sufficient to prevent future episodes. For patients in whom no clear disease has been established, patients should be advised to avoid possible triggers of palpitations such as caffeine, alcohol, nicotine, recreational drugs.[1][3][4][5][7]
Abbreviations: NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction
| Determine the cause of the palpitations | |||||||||||||||||||||||||||||||||||||||||||
Cardiac cause | Non-cardiac cause | ||||||||||||||||||||||||||||||||||||||||||
Psychiatric disorder | Substance/drug intake ❑ Alcohol
❑ Recreational drugs
❑ Nicotine | ||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Implantations or replacement of pacemakers for bradyarrhythmias | |||||||||||||||||||||||||||||||||||||||||||
Do's
- If possible, perform a physical exam and an ECG when the patient is symptomatic.[1]
- If a patient is asymptomatic, search for signs of structural heart disease such as murmurs, displaced apex beat or S3.[1]
- Perform an ambulatory ECG in patients with recurrent episodes of palpitations of undetermined etiology.[1]
- Perform an electrophysiologic study (EPS) for patients with inconclusive ambulatory ECG.[1]
- Perform an EPS, with ablation therapy if necessary, in patients with severe heart disease, particularly when palpitations preceded syncope and when the patient required cardio-respiratory resuscitation maneuvers.[1][6]
- Advise life-style changes that may lower the possibility of future episodes, such as exercise, lower alcohol and caffeine intake, and smoking cessation.[1]
- Perform an exercise stress test in patients with exercise induced palpitations.[7]
EKG gallery
Narrow complex tachycardia
| Type of Arrhythmia | EKG (lead II) | Clues |
| Sinus tachycardia |  |
Onset and termination: gradual Rhythm: regular Rate: >220 minus the age of the patient Response to adenosine: transient decrease of the rate |
| Atrial fibrillation | 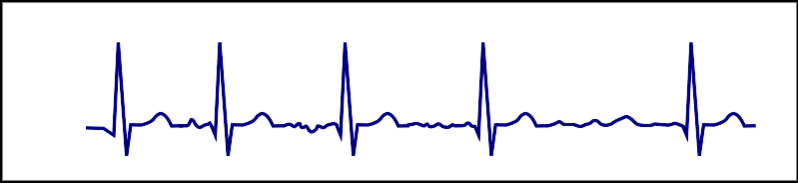 |
Onset and termination: abrupt Rhythm: irregular Rate:100-180 bpm Response to adenosine: transient decrease of the ventricular rate |
| Atrial flutter | 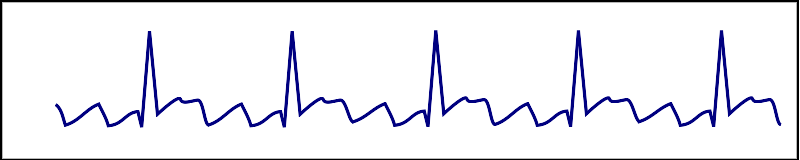 |
Onset and termination: abrupt Rhythm: regular Rate: >150 bpm Response to adenosine: transient decrease of the rate Presence of saw-tooth appearance |
| AVNRT | 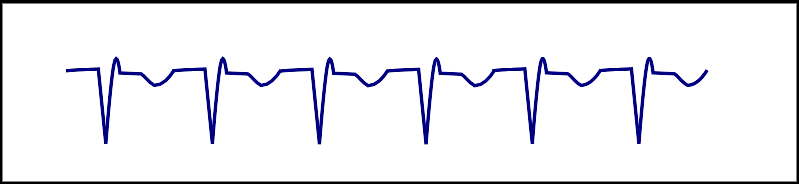 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| AVRT |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| Focal atrial tachycardia |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm |
| Nonparoxysmal junctional tachycardia |  |
Rhythm: regular Retrograde P wave Most commonly due to ischemia or digitalis toxicity |
| Multifocal atrial tachycardia | 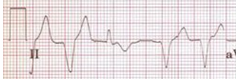 |
Onset and termination: gradual Rhythm: irregular Rate: 100-150 bpm Response to adenosine: no effect 3 different P wave morphologies |
Wide complex tachycardia
| Example | Regularity | Atrial frequency | Ventricular frequency | Origin (SVT/VT) | p-wave | Effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Wide complex (QRS > 0.12) | |||||||
| Ventricular Tachycardia | regular (mostly) | 60-100 bpm | 110-250 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Ventricular Fibrillation | irregular | 60-100 bpm | 400-600 bpm | ventricle (VT) | AV-dissociation | none | |
| Ventricular Flutter | regular | 60-100 bpm | 150-300 bpm | ventricle (VT) | AV-dissociation | none | |
| Accelerated Idioventricular Rhythm | regular (mostly) | 60-100 bpm | 50-110 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Torsade de Pointes | regular | 150-300 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | ||
| Bundle-branch re-entrant Tachycardia* | regular | 60-100 bpm | 150-300 bpm | ventricles (VT) | AV-dissociation | no rate reduction | |
| * Bundle-branch re-entrant tachycardia is extremely rare | |||||||
STEMI
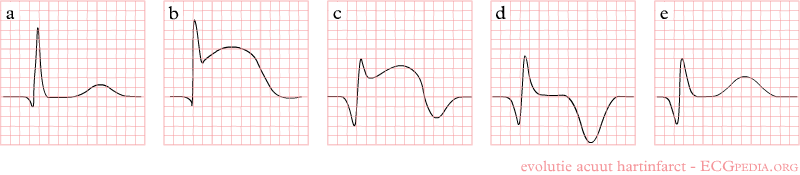
Shown below is an EKG demonstrating the evolution of an infarct on the EKG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave suggest STEMI.
NSTEMI
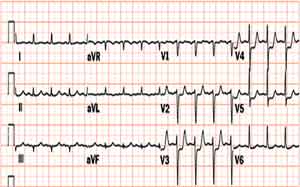
Shown below is an EKG showing an ST depression in V2, V3, V4 and V6.
Shown below is an EKG showing an inversion in the T wave at leads V4, V5 and V6.
Pericarditis
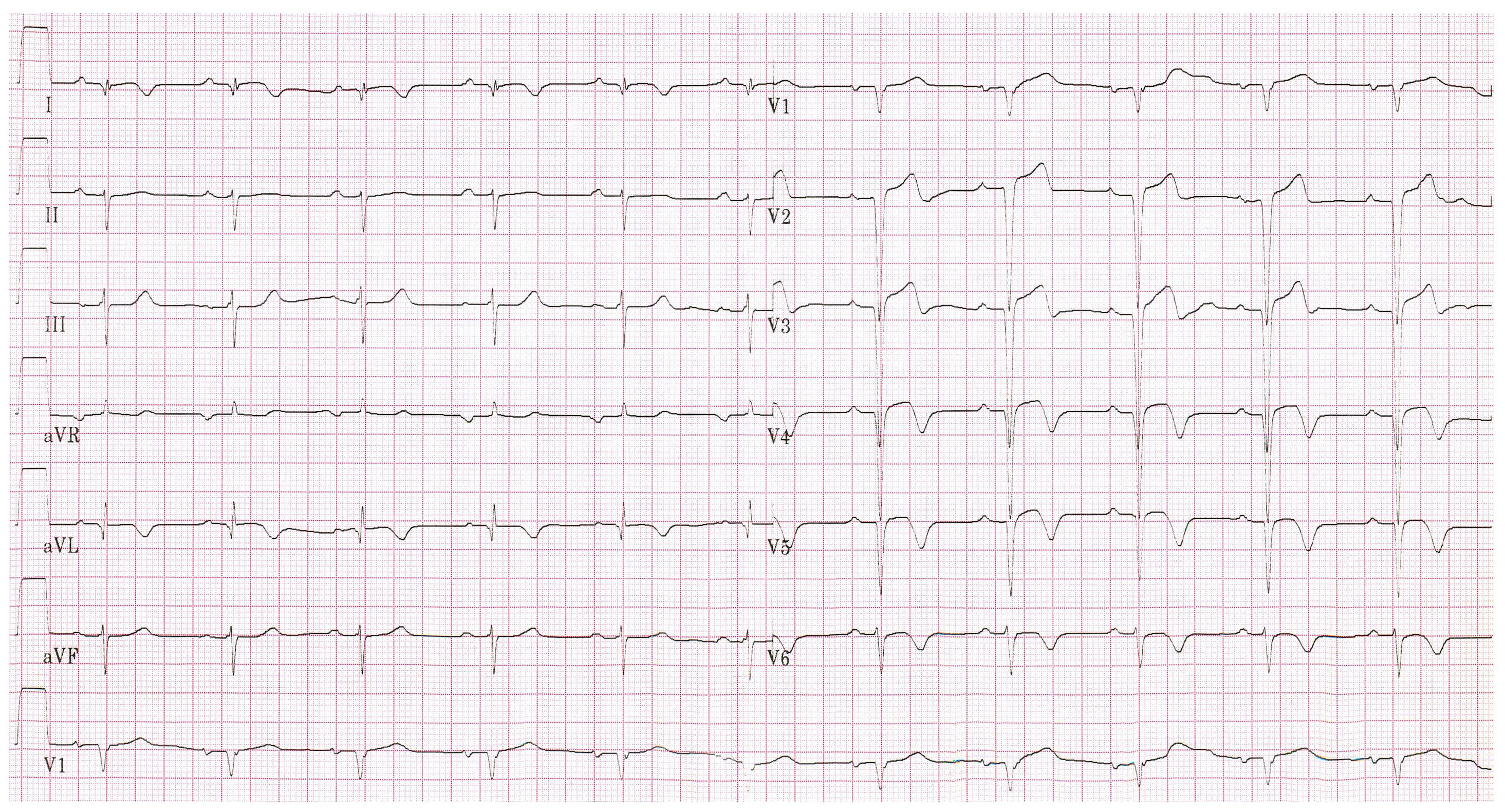
Shown below is an EKG with ST elevation in lead I, II, V2, V3, V4, V5 and V6.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L; et al. (2011). "Management of patients with palpitations: a position paper from the European Heart Rhythm Association". Europace. 13 (7): 920–34. doi:10.1093/europace/eur130. PMID 21697315.
- ↑ "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ 3.0 3.1 Zimetbaum, P.; Josephson, ME. (1998). "Evaluation of patients with palpitations". N Engl J Med. 338 (19): 1369–73. doi:10.1056/NEJM199805073381907. PMID 9571258. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 "http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf" (PDF). Retrieved 16 April 2014. External link in
|title=(help) - ↑ 5.0 5.1 Abbott, AV. (2005). "Diagnostic approach to palpitations". Am Fam Physician. 71 (4): 743–50. PMID 15742913. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Thavendiranathan, P.; Bagai, A.; Khoo, C.; Dorian, P.; Choudhry, NK. (2009). "Does this patient with palpitations have a cardiac arrhythmia?". JAMA. 302 (19): 2135–43. doi:10.1001/jama.2009.1673. PMID 19920238. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 7.2 "http://www.turner-white.com/pdf/hp_jan03_methods.pdf" (PDF). Retrieved 25 April 2014. External link in
|title=(help)