Paget's disease of the breast pathophysiology: Difference between revisions
Preeti Singh (talk | contribs) No edit summary |
No edit summary |
||
| Line 76: | Line 76: | ||
{| | {| | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |'''Immunohistochemical marker''' | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Positivity | |||
| style="background: # | |||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px;" |Oncoproteins | | style="background: #F5F5F5; padding: 5px;" |Oncoproteins | ||
| Line 100: | Line 85: | ||
| style="background: #F5F5F5; padding: 5px;" |Her 2 80e100% | | style="background: #F5F5F5; padding: 5px;" |Her 2 80e100% | ||
| style="background: #F5F5F5; padding: 5px;" | | | style="background: #F5F5F5; padding: 5px;" | | ||
|- | |- | ||
|Her 1 0e13% | | style="background: #F5F5F5; padding: 5px;" |Her 1 0e13% | ||
| | | style="background: #F5F5F5; padding: 5px;" | | ||
| | |||
|- | |- | ||
| style="background: #F5F5F5; padding: 5px;" |Her 3 0e57% | | style="background: #F5F5F5; padding: 5px;" |Her 3 0e57% | ||
| Line 267: | Line 250: | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:Needs content]] | [[Category:Needs content]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Gynecology]] | [[Category:Gynecology]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Revision as of 14:53, 4 March 2019
|
Paget's disease of the breast Microchapters |
|
Differentiating Paget's disease of the breast from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Paget's disease of the breast pathophysiology On the Web |
|
American Roentgen Ray Society Images of Paget's disease of the breast pathophysiology |
|
Directions to Hospitals Treating Paget's disease of the breast |
|
Risk calculators and risk factors for Paget's disease of the breast pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4];Associate Editor(s)-in-Chief: Suveenkrishna Pothuru, M.B,B.S. [5]
Overview
On gross pathology, eczematoid, erythematous, moist or crusted lesion, with or without fine scaling, infiltration of the nipple, and inversion of the nipple are characteristic findings of Paget's disease of the breast. Eczema changes of the nipple-areolar complex are said to occur due to invasion of the overlying epidermis by malignant (Paget) cells. On microscopic histopathological analysis, epidermal Paget cells which are malignant glandular epithelial cells organized in groups with nest-like patterns or gland-like structures and are preferably located in the epidermal basal layer are characteristic findings of Paget's disease of the breast.
Pathophysiology
Pathogenesis
- The pathogenesis of Paget’s disease of the breast still remains controversial.
- The commonly accepted hypothesis is that most cases of Paget's disease of the breast originate from in situ or invasive ductal carcinoma of the underlying breast tissue.This is supported by two different theories:[1][2]
- Epidermotropic theory
- Intraepidermal transformation theory
Epidermotropic Theory
- According to this hypothesis malignant epithelial cells from intraductal carcinoma, extend into the overlying epidermis through mammary duct epithelium and proliferate in the epidermis causing thickening of the nipple and areolar skin.[1]
- Normal epidermal keratinocytes produce and release the mobility factor heregulin-alpha which is chemotactic for heregulin receptors (Her-2) and coreceptors Her 3 and Her 4 which are produced by Pagets cells. This is thought to result in migration of these cells to the nipple epidermis.
- HER-2/neu has been shown to enhance the motility of tumor cells by interacting with a motility factor called heregulin-alpha secreted by epidermal keratinocytes.
- This chemotactic hypothesis is supported by the relatively high over-expression of HER-2/neu in Paget cells (90%) in comparison to it's expression in breast cancer without Paget's disease.
- This is supported by the observation that Paget cells often share cell surface markers with the underlying breast carcinoma (e.g CAM 5.2, CEA, c-erb 2 and EMA).[3]
Intraepidermal transformation theory
- According to this hypothesis Paget cells are keratinocytes that have undergone malignant transformation.
- Thus it is speculated that Paget's disease is an in situ carcinoma and is independent from any underlying parenchymal carcinoma.
- It is assumed that the underlying intraductal carcinoma coexisting with this disease is unrelated to the overlying eczematous change.
- Toker cells also known as pre-Paget cells are normal cells in the nipple epithelium which histologically demonstrate characteristics of both keratinocytes and Paget cells.
- This theory is further supported by:
- Cases in which there is no underlying malignancy nor there is any dermal invasion.
- Cases of collision tumors in which breast cancer is located peripherally to the nipple lesion, suggesting two concurrent but separate processes.
- Cases suggesting the Paget cells may have originated intraepidermally, by the presence of microvilli and desmosomal attachments between Paget cells and keratinocytes.
- Cases in which there is genetic variation between Paget cells and cells of the underlying carcinoma.[4]
Gross Pathology
- On gross pathology, eczematoid, erythematous, moist or crusted lesion, with or without fine scaling, infiltration of the nipple, and inversion of the nipple are characteristic findings of Paget's disease of the breast.[2]
 |
Microscopic pathology
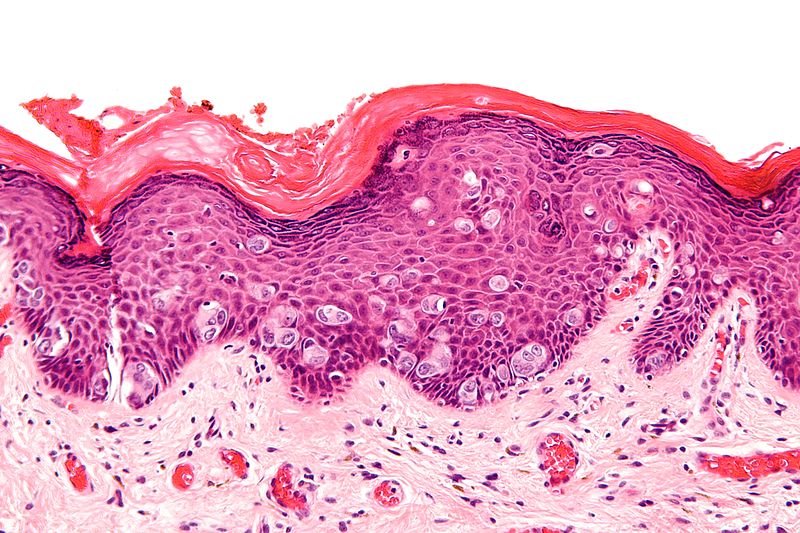
- Paget's disease of the breast is histopathologically characterized by the presence of epidermal Paget cells.
- Paget cells are malignant glandular epithelial cells with abundant and clear cytoplasm, usually containing mucin and pleomorphic and hyperchromatic, centrally situated, variably atypical nucleus.[2]
- Mitotic figures are frequently observed in cells which may be arranged singly or in form of clusters, solid nests, or gland-like structures with a central lumen.
- Paget cells are abundant mostly in the basal epidermal layer, mainly along the pilosebaceous apparatus.
- These cells stain positive for aldehyde fuchsin, mucin and periodic acid-Schiff. And are resistant to diastase digestion.[7].
- The number of cells vary from a few to large quantities; even completely replacing the epidermal cells.
- This radial distribution of neoplastic cells along the basal layers of the epithelium is known as Pagetoid spread. It is also observed in malignant melanoma, Bowen'sdisease, mycosis fungoides, Langerhans cell histiocytosis, and Spitz nevus.[8][7][9][10]
- Invasion of adnexal structures can occur.
- Orthokeratosis and parakeratosis may be present.
- The dermis displays reactive characteristics, with telangiectasia, chronic inflammation, and ulceration in more advanced cases.
- There are several histologic variants of Paget's disease include:[6]
- Adenocarcinoma-like cell type
- Spindle cell type
- Anaplastic cell type
- Acantholytic cell type
- Pigmented cell type
 |
Immunohistochemistry
- Immunohistochemistry is very useful in Paget's disease of the breast for differential diagnoses and histogenesis.[2][12]
- The current understanding of immunohistochemistry of mammary Paget's disease of breast is largely based on female cases.
- Previous studies have shown significantly difference in the immunohistochemical profiles and the prognostic roles of these markers, between male and female patients.
- The single most useful stain for differentiation Paget's disease of the Breast from other intraepidermal neoplasms is cytokeratin 7.
- The overexpression of the low molecular weight cytokeratins, notably CK7, and lack of expression of high molecular weight cytokeratins, such as CK10, CK14 and CK20 are observed in 98-100% of Paget's disease of the Breast.
- Furthermore, they also express carcinoembryonic antigen, epithelial membrane antigen, and some mucins.
- Since breast cancers associated to Paget's disease are poorly differentiated, estrogen and progesterone antigens are frequently negative.
- Mori et al found overexpression of oncogenic ras and p21 in mammary and extramammary diseases.
- Paget cells express p53, p21, Ki-67, cyclin D1, androgen receptors and Her-2 oncoprotein.
| Immunohistochemical marker | Positivity |
|---|---|
| Oncoproteins | |
| Her 2 80e100% | |
| Her 1 0e13% | |
| Her 3 0e57% | |
| Her 4 0e79% | |
References
- ↑ 1.0 1.1 Subramanian, Ashok; Birch, Hilary; McAvinchey, Rita; Stacey-Clear, Adam (2007). "Pagets disease of uncertain origin: case report". International Seminars in Surgical Oncology. 4 (1): 12. doi:10.1186/1477-7800-4-12. ISSN 1477-7800.
- ↑ 2.0 2.1 2.2 2.3 Lopes Filho, Lauro Lourival; Lopes, Ione Maria Ribeiro Soares; Lopes, Lauro Rodolpho Soares; Enokihara, Milvia M. S. S.; Michalany, Alexandre Osores; Matsunaga, Nobuo (2015). "Mammary and extramammary Paget's disease". Anais Brasileiros de Dermatologia. 90 (2): 225–231. doi:10.1590/abd1806-4841.20153189. ISSN 1806-4841.
- ↑ 3.0 3.1 Sakorafas, G.H.; Blanchard, K.; Sarr, M.G.; Farley, D.R. (2001). "Paget's disease of the breast". Cancer Treatment Reviews. 27 (1): 9–18. doi:10.1053/ctrv.2000.0203. ISSN 0305-7372.
- ↑ Morandi, Luca; Pession, Annalisa; Marucci, Gian Luca; Foschini, Maria Pia; Pruneri, Giancarlo; Viale, Giuseppe; Eusebi, Vincenzo (2003). "Intraepidermal cells of paget's carcinoma of the breast can be genetically different from those of the underlying carcinoma". Human Pathology. 34 (12): 1321–1330. doi:10.1016/S0046-8177(03)00405-2. ISSN 0046-8177.
- ↑ Nofech-Mozes, Sharon; Hanna, Wedad (2009). "Toker Cells Revisited". The Breast Journal. 15 (4): 394–398. doi:10.1111/j.1524-4741.2009.00743.x. ISSN 1075-122X.
- ↑ 6.0 6.1 Image courtesy of Dr Garth Kruger. Radiopaedia (original file [1]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC
- ↑ 7.0 7.1 Serour, F.; Birkenfeld, S.; Amsterdam, E.; Krispin, M.; Treshchan, O. (1988). "Paget's disease of the male breast". Cancer. 62 (3): 601–605. doi:10.1002/1097-0142(19880801)62:3<601::AID-CNCR2820620326>3.0.CO;2-7. ISSN 0008-543X.
- ↑ Lloyd, J (2000). "Mammary and extramammary Paget's disease". Journal of Clinical Pathology. 53 (10): 742–749. doi:10.1136/jcp.53.10.742. ISSN 0021-9746.
- ↑ Kanitakis, J (2007). "Mammary and extramammary Paget's disease". Journal of the European Academy of Dermatology and Venereology. 0 (0): 070328074210008–???. doi:10.1111/j.1468-3083.2007.02154.x. ISSN 0926-9959.
- ↑ Guitera, P.; Scolyer, R.A.; Gill, M.; Akita, H.; Arima, M.; Yokoyama, Y.; Matsunaga, K.; Longo, C.; Bassoli, S.; Bencini, P.L.; Giannotti, R.; Pellacani, G.; Alessi-Fox, C.; Dalrymple, C. (2013). "Reflectance confocal microscopy for diagnosis of mammary and extramammary Paget's disease". Journal of the European Academy of Dermatology and Venereology. 27 (1): e24–e29. doi:10.1111/j.1468-3083.2011.04423.x. ISSN 0926-9959.
- ↑ Paget's disease of the breast. [2] (original file [3])
- ↑ Sandoval-Leon, Ana C.; Drews-Elger, Katherine; Gomez-Fernandez, Carmen R.; Yepes, Monica M.; Lippman, Marc E. (2013). "Paget's disease of the nipple". Breast Cancer Research and Treatment. 141 (1): 1–12. doi:10.1007/s10549-013-2661-4. ISSN 0167-6806.