Meningioma pathophysiology: Difference between revisions
| Line 68: | Line 68: | ||
'''[[Anaplastic]] (Grade III) meningioma''' | '''[[Anaplastic]] (Grade III) meningioma''' | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
20 or more mitoses/10 HPF, histology similar to [[carcinoma]] or [[sarcoma]] | 20 or more mitoses/10 HPF, histology may be similar to [[carcinoma]] or [[sarcoma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
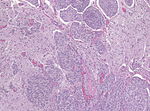
[[File:Grade 3 menigioma.jpg|thumb|none|300px|Grade 3 menigioma]] | [[File:Grade 3 menigioma.jpg|thumb|none|300px|Grade 3 menigioma]] | ||
Revision as of 15:06, 28 September 2015
|
Meningioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Meningioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Meningioma pathophysiology |
|
Risk calculators and risk factors for Meningioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [2]
Overview
Meningioma arises from the arachnoid "cap" cells, which are normally involved in the protection of the central nervous system by forming a thick envelope of meninges around the brain and spinal cord.[1][2][3] The majority of meningiomas are benign.[1][2][3] Development of meningioma is the result of multiple genetic mutations.[1] On gross pathology, a gray, well-circumscribed, dome-shaped mass is a characteristic finding of meningioma.[1] On microscopic histopathological analysis, whorled appearance, calcification, and psammoma bodies are characteristic findings of of meningioma.[4]
Pathogenesis
- Meningioma arises from the arachnoid "cap" cells, which are normally involved in the protection of the central nervous system by forming a thick envelope of meninges around the brain and spinal cord.[1]
- The majority of meningiomas are benign; however, a minority of cases may develop a malignant nature.[1]
- The exact pathophysiology of meningioma depends on the histological subtype of the tumor.[1]
- Meningioma may be located either intradural or extradural along the central nervous system.[5][6]
- Meningiomas are frequently found attached to the dura surrounding the brain tissue in several locations that include:[1]
- Frontaparietal region
- Brain convexity
- Sphenoid ridge
- Sella turcica
- Posterior fossa
- Olfactory groove
- Meckel's cave
- Tentorium cerebelli
- Cerebellopontine angle
- Confluence of sinuses
- Parafalcine region
- Meningiomas is commonly associated with neurofibromatosis type 2 syndrome and gorlin syndrome.[4]
- Meningiomas demonstrate estrogen and progesterone sensitivity and may grow during pregnancy.[4][3]
Genetics
- Development of meningioma is the result of multiple genetic mutations.[1]
- The majority of meningioma cases involve a deletion of the neurofibromatosis 2 gene located on chromosome 22.[1]
- Other genes involved in the pathogenesis of meningioma include:[1]
- Protein kinase AKT1 gene located on human chromosome 14
- Meningioma 1 MN1 gene located on human chromosome 22
- Phosphatase and tensin homolog PTEN gene located on both human chromosomes 10 and 19
- SMO gene located on human chromosome 6 and 7
Gross Pathology
- On gross pathology, a gray, well-circumscribed, dome-shaped mass is a characteristic finding of meningioma.[1]

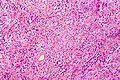
Microscopic Pathology
- On microscopic histopathological analysis, whorled appearance, calcification, and psammoma bodies are characteristic findings of of meningioma.[4]
- The table below differentiates between the three main groups of meningioma according to WHO histological classification:[4][2][3]
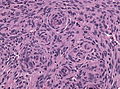
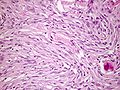
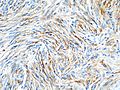
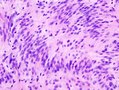
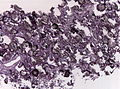
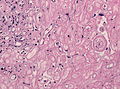
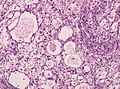
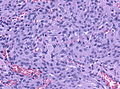
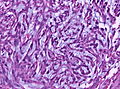
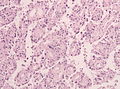
| Grade | Histologic features | Image |
|---|---|---|
|
Benign (Grade I) meningioma |
 | |
|
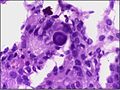
Atypical (Grade II) meningioma |
Brain invasion, 4 or more mitosis/10 HPF, necrosis, increased cell count, high nucleus:cytoplasm ratio, increased nucleoli size, presence of sheeting |
 |
|
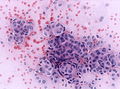
Anaplastic (Grade III) meningioma |
20 or more mitoses/10 HPF, histology may be similar to carcinoma or sarcoma |
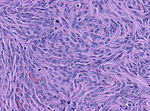 |
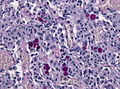
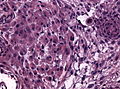
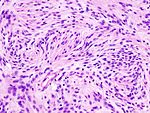
- Demonstrated below is a series of microscopic smears which feature specific findings observed in each subtype of meningioma:[4]
-
Meningothelial meningioma with syncytial appearance and whorl formation
-
Meningothelial meningioma with psammoma body
-
Meningothelial meningioma with onion bulb formation
-
Meningothelial meningioma on HPS stain
-
Fibrous meningioma with spindle cells in parallel bundles
-
Fibrous meingioma on EMA stain
-
Transitional meningioma with coexisting lobular and fasicular growth patterns
-
Psammomatous meningioma with numerous psammoma bodies
-
Angiomatous meningioma with hyalinized vessels
-
Microcystic meningioma with cystic appearance and increased pleomorphism of the elongated cells
-
Secretory meningioma with secretory granules
-
Secretory meningioma with PAS stain positive secretory granules
-
Chordoid meningioma with myxoid appearance
-
Rhabdoid meningioma with abundant cytoplasm and cross-striations
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 Meningioma. Wikipedia(2015) https://en.wikipedia.org/wiki/Meningioma#cite_note-pmid7731706-9 Accessed on September, 25th 2015
- ↑ 2.0 2.1 2.2 Meningioma. Canadian Cancer Society http://www.cancer.ca/en/cancer-information/cancer-type/brain-spinal/brain-and-spinal-tumours/meningioma/?region=mb September, 25th 2015
- ↑ 3.0 3.1 3.2 3.3 Meningeoma. Radiopaedia(2015)http://radiopaedia.org/articles/meningioma Accessed on September, 25th 2015
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Meningioma. Liberpathology(2015) http://librepathology.org/wiki/index.php/Meningioma#Quick_overview accessed on September, 25th 2015
- ↑ Meningioma diagnosi. Wikipedia(2015) https://en.wikipedia.org/wiki/Meningioma#History_and_nomenclature Accessed on September, 25th 2015
- ↑ Meningioma. Liberpathology(2015) http://librepathology.org/wiki/index.php/Meningioma#Quick_overview Accessed on September, 25th 2015
- ↑ Image courtesy of Dr Dharam Ramnani Radiopaedia(original file "here"). Creative Commons BY-SA-NC