Lymphoplasmacytic lymphoma diagnostic study of choice: Difference between revisions
Sara Mohsin (talk | contribs) |
|||
| (35 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}}{{S.M.}} | {{CMG}}; {{AE}}{{S.M.}} | ||
== Overview == | == Overview == | ||
The [[diagnosis]] of [[lymphoplasmacytic lymphoma]] is based on [[ | The [[diagnosis]] of [[lymphoplasmacytic lymphoma]] is [[Based on Symptoms|based]] on [[bone marrow aspiration]] and [[biopsy]] and [[serum]] [[protein]] [[analysis]] [[Study design|studies]] such as [[immunohistochemistry|immunohistochemistry,]] [[flow cytometry]] and [[cytogenetics]] to [[Differentiate|distinguish]] [[Lymphoplasmacytic lymphoma|LPL]] from other types of [[B-cell]] [[lymphomas]]. [[CSF]] [[flow cytometry]], [[protein electrophoresis]] and [[immunofixation]] is [[done]] for the [[diagnosis]] of [[Bing-Neel syndrome]] (a late, but severe, [[rare]] [[Complication (medicine)|complication]]). | ||
== Diagnostic Study of Choice == | == Diagnostic Study of Choice == | ||
There is no single [[diagnostic study of choice]] for the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] (LPL), but '''bone marrow aspiration and biopsy''' is considered to be mandatory for assessment of patients with LPL and further supported by monoclonal protein/immunophenotypic studies such as [[immunohistochemistry]], [[flow cytometry]] and [[cytogenetics]] to distinguish LPL from other types of [[B-cell]] [[lymphomas]].<ref name="pmid15735132">{{cite journal| author=Dimopoulos MA, Kyle RA, Anagnostopoulos A, Treon SP| title=Diagnosis and management of Waldenstrom's macroglobulinemia. | journal=J Clin Oncol | year= 2005 | volume= 23 | issue= 7 | pages= 1564-77 | pmid=15735132 | doi=10.1200/JCO.2005.03.144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15735132 }} </ref><ref name="pmid26980727">{{cite journal| author=Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R et al.| title=The 2016 revision of the World Health Organization classification of lymphoid neoplasms. | journal=Blood | year= 2016 | volume= 127 | issue= 20 | pages= 2375-90 | pmid=26980727 | doi=10.1182/blood-2016-01-643569 | pmc=4874220 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26980727 }} </ref> | *There is no single [[diagnostic study of choice]] for the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] (LPL), but '''[[bone marrow aspiration]]''' and '''[[biopsy]]''' is considered to be [[Mandatory labelling|mandatory]] for the [[Assessment and Plan|assessment]] of [[patients]] with LPL and further [[Support|supported]] by [[monoclonal]] [[protein]]/[[Immunophenotyping|immunophenotypic studies]] such as [[immunohistochemistry]], [[flow cytometry]] and [[cytogenetics]] to distinguish LPL from other types of [[B-cell]] [[lymphomas]].<ref name="pmid15735132">{{cite journal| author=Dimopoulos MA, Kyle RA, Anagnostopoulos A, Treon SP| title=Diagnosis and management of Waldenstrom's macroglobulinemia. | journal=J Clin Oncol | year= 2005 | volume= 23 | issue= 7 | pages= 1564-77 | pmid=15735132 | doi=10.1200/JCO.2005.03.144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15735132 }} </ref><ref name="pmid26980727">{{cite journal| author=Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R et al.| title=The 2016 revision of the World Health Organization classification of lymphoid neoplasms. | journal=Blood | year= 2016 | volume= 127 | issue= 20 | pages= 2375-90 | pmid=26980727 | doi=10.1182/blood-2016-01-643569 | pmc=4874220 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26980727 }} </ref> | ||
*Not all the [[diagnostic]] [[Test|tests]] mentioned are [[Performance status|performed]] in a [[patient]] with [[lymphoplasmacytic lymphoma]]. A [[Doctor of Medicine|doctor]] takes into account the following factors before choosing [[diagnostic]] [[Test|tests]] in a particular [[patient]]: | |||
** Suspected type of [[cancer]] | |||
** [[Signs and Symptoms|Signs]] and [[symptoms]] | |||
** [[Age]] | |||
** [[Medical condition]] of the [[patient]] | |||
** [[Result|Results]] of earlier [[medical]] [[Test|tests]] | |||
===Diagnostic Criteria:=== | ===Diagnostic Criteria:=== | ||
====Diagnostic criteria presented in second International Workshop, Greece, 2002==== | ====Diagnostic criteria presented in second International Workshop, Greece, 2002==== | ||
In September 26-30, 2002, in Athens, Greece,the | * In September 26-30, 2002, in Athens, Greece,the Second International Workshop was held in which a [[Diagnosis|diagnostic]] criteria for [[Waldenström's macroglobulinemia|Waldenstrom's Macroglobulinemia]] was [[Proposition|proposed]]. According to this [[criteria]], the following findings on [[Performance status|performing]] [[Bone marrow examination|bone marrow biopsy]] and [[serum]] [[protein]] analysis are [[Confirmatory factor analysis|confirmatory]] of [[Waldenström macroglobulinemia]] and [[Exclusion criteria|exclude]] other small [[B cell]] [[lymphoid]] [[neoplasms]] with plasmacytic [[differentiation]]:<ref name="pmid15735132" /><ref name="pmid12720118">{{cite journal| author=Owen RG, Treon SP, Al-Katib A, Fonseca R, Greipp PR, McMaster ML et al.| title=Clinicopathological definition of Waldenstrom's macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom's Macroglobulinemia. | journal=Semin Oncol | year= 2003 | volume= 30 | issue= 2 | pages= 110-5 | pmid=12720118 | doi=10.1053/sonc.2003.50082 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12720118 }}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! colspan=" | ! colspan="3" style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Diagnostic criteria presented in second International Workshop, Greece, 2002}} | ||
|- | |- | ||
| colspan="2" |'''1:'''Presence of [[IgM]] | | colspan="2" |'''1:'''[[Presenting symptom|Presence]] of [[Immunoglobulin M|IgM]] [[monoclonal gammopathy]] of any [[concentration]] on [[Serum protein electrophoresis|serum protein analysis]] | ||
|'''Necessary''' criteria | |'''[[Necessary and sufficient|Necessary]]''' [[criteria]] | ||
|- | |- | ||
| rowspan="3" |'''2:'''A [[bone marrow]] [[biopsy]] demonstrating more than 10% infiltration by small [[lymphocytes]], plasmacytoid [[lymphocytes]], and [[plasma cells]], (with variable numbers of admixed immunoblasts), with an intertrabecular pattern consistent with [[lymphoplasmacytic lymphoma]] | | rowspan="3" |'''2:'''A [[bone marrow]] [[biopsy]] demonstrating more than 10% [[Infiltration (medical)|infiltration]] by small [[lymphocytes]], [[plasmacytoid]] [[lymphocytes]], and [[plasma cells]], (with [[variable]] [[Number|numbers]] of admixed [[Immunoblast|immunoblasts]]), with an intertrabecular [[pattern]] consistent with [[lymphoplasmacytic lymphoma]] | ||
|[[Proliferation]] centers (pathognomonic of [[CLL]]/[[SLL]]) and paler-appearing marginal zone type [[differentiation]] (seen in marginal zone lymphoma) are absent | |[[Proliferation]] centers ([[pathognomonic]] of [[CLL]]/[[SLL]]) and [[Paleness|paler]]-[[Appearance|appearing]] [[marginal zone]] type [[differentiation]] (seen in [[marginal zone lymphoma]]) are absent | ||
| rowspan="3" |'''Necessary''' criteria | | rowspan="3" |'''[[Necessary and sufficient|Necessary]]''' [[criteria]] | ||
|- | |- | ||
|[[IgM]] concentration widely varies in WM, and it is not possible to define a concentration that reliably distinguishes WM from other [[lymphoproliferative disorders]]. Hence, a diagnosis of WM can be made irrespective of [[IgM]] concentration if there is evidence of [[bone marrow]] [[Infiltration (medical)|infiltration]] by lymphoplasmacytoid [[lymphoma]] as defined by the Revised European-American [[Lymphoma]] [[classification]] and [[WHO]] criteria. | |[[IgM]] [[concentration]] [[Wide and fast|widely]] [[Variable|varies]] in [[Waldenström's macroglobulinemia|WM]], and it is not [[Possibility theory|possible]] to define a [[concentration]] that reliably distinguishes [[Waldenström's macroglobulinemia|WM]] from other [[lymphoproliferative disorders]]. Hence, a [[diagnosis]] of [[Waldenström's macroglobulinemia|WM]] can be made irrespective of [[IgM]] [[concentration]] if there is an [[evidence]] of [[bone marrow]] [[Infiltration (medical)|infiltration]] by lymphoplasmacytoid [[lymphoma]] as defined by the Revised European-American [[Lymphoma]] [[classification]] and [[WHO]] [[criteria]]. This is a [[tumor]] of small [[lymphocytes]] showing [[evidence]] of [[plasmacytoid]] or [[plasma cell]] [[differentiation]]. | ||
|- | |- | ||
|A recent study found that, in 39% of patients, the [[bone marrow]] [[aspirate]] contained a spectrum of small [[lymphocytes]], plasmacytoid [[lymphocytes]], and [[plasma cells]]; in 39% of patients, there was a predominance of small [[lymphocytes]] with fewer plasmacytoid [[lymphocytes]] or [[plasma cells]], and 22% of patients contained a mixture of small [[lymphocytes]] and [[plasma cells]], with rare plasmacytoid cells. [[Mast cells]] were increased in 26% of patients. | |A [[Recent changes|recent]] [[Study design|study]] found that, in 39% of [[patients]], the [[bone marrow]] [[aspirate]] contained a [[spectrum]] of small [[lymphocytes]], [[plasmacytoid]] [[lymphocytes]], and [[plasma cells]]; in 39% of [[patients]], there was a [[Predominance diagram|predominance]] of small [[lymphocytes]] with [[Fewmets|fewer]] [[plasmacytoid]] [[lymphocytes]] or [[plasma cells]], and 22% of the [[patients]] contained a [[mixture]] of small [[lymphocytes]] and [[plasma cells]], with [[rare]] [[plasmacytoid]] [[Cells (biology)|cells]]. [[Mast cells]] were increased in 26% of [[patients]]. | ||
|- | |- | ||
| colspan="2" |'''3:'''Intertrabecular pattern of [[bone marrow]] [[Infiltration (medical)|infiltration]] | | colspan="2" |'''3:'''Intertrabecular [[pattern]] of [[bone marrow]] [[Infiltration (medical)|infiltration]] | ||
|'''Supportive''' criteria | |'''[[Support|Supportive]]''' [[criteria]] | ||
|- | |- | ||
| colspan="2" |'''4:'''[[Immunophenotype]] of the lymphoplasmacytic infiltrate consistent with [[Waldenström's macroglobulinemia|Waldenstrom's macroglobulinemia]]. This includes: [[IgM]]+, [[CD5]]-, [[CD10]]-, [[CD11c]]-, [[CD19]]+, [[CD20]]+, [[CD22]]+, [[CD23]]-, [[CD25]]+, [[CD27]]+, [[FMC7]]+, [[CD103]]- and [[CD138]]+ | | colspan="2" |'''4:'''[[Immunophenotype]] of the [[Lymphoplasmacytic lymphoma|lymphoplasmacytic]] [[Infiltration (medical)|infiltrate]] consistent with [[Waldenström's macroglobulinemia|Waldenstrom's macroglobulinemia]]. This includes: [[IgM]]+, [[CD5]]-, [[CD10]]-, [[CD11c]]-, [[CD19]]+, [[CD20]]+, [[CD22]]+, [[CD23]]-, [[CD25]]+, [[CD27]]+, [[FMC7]]+, [[CD103]]- and [[CD138]]+ | ||
|'''Supportive''' criteria | |'''[[Support|Supportive]]''' [[criteria]] | ||
|} | |} | ||
====mSMART guidelines for diagnosis of Waldenstrom macroglobulinemia and associated disorders==== | ====mSMART guidelines for diagnosis of Waldenstrom macroglobulinemia and associated disorders==== | ||
Mayo [[Stratification]] of [[Macroglobulinemia]] and Risk-Adapted [[Therapy]] (mSMART) Guidelines 2016 for [[diagnosis]] of [[Waldenstrom macroglobulinemia]] and associated [[disorders]] are as follows:<ref name="AnsellKyle2010">{{cite journal|last1=Ansell|first1=Stephen M.|last2=Kyle|first2=Robert A.|last3=Reeder|first3=Craig B.|last4=Fonseca|first4=Rafael|last5=Mikhael|first5=Joseph R.|last6=Morice|first6=William G.|last7=Bergsagel|first7=P. Leif|last8=Buadi|first8=Francis K.|last9=Colgan|first9=Joseph P.|last10=Dingli|first10=David|last11=Dispenzieri|first11=Angela|last12=Greipp|first12=Philip R.|last13=Habermann|first13=Thomas M.|last14=Hayman|first14=Suzanne R.|last15=Inwards|first15=David J.|last16=Johnston|first16=Patrick B.|last17=Kumar|first17=Shaji K.|last18=Lacy|first18=Martha Q.|last19=Lust|first19=John A.|last20=Markovic|first20=Svetomir N.|last21=Micallef|first21=Ivana N.M.|last22=Nowakowski|first22=Grzegorz S.|last23=Porrata|first23=Luis F.|last24=Roy|first24=Vivek|last25=Russell|first25=Stephen J.|last26=Short|first26=Kristen E. Detweiler|last27=Stewart|first27=A. Keith|last28=Thompson|first28=Carrie A.|last29=Witzig|first29=Thomas E.|last30=Zeldenrust|first30=Steven R.|last31=Dalton|first31=Robert J.|last32=Rajkumar|first32=S. Vincent|last33=Gertz|first33=Morie A.|title=Diagnosis and Management of Waldenström Macroglobulinemia: Mayo Stratification of Macroglobulinemia and Risk-Adapted Therapy (mSMART) Guidelines|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=824–833|issn=00256196|doi=10.4065/mcp.2010.0304}}</ref> | |||
* [[Mayo Clinic|Mayo]] [[Stratification]] of [[Macroglobulinemia]] and [[RiskMetrics|Risk]]-[[Adapted process|Adapted]] [[Therapy]] (mSMART) [[Medical guideline|Guidelines]] 2016 for [[diagnosis]] of [[Waldenstrom macroglobulinemia]] and [[Association (statistics)|associated]] [[disorders]] are as follows:<ref name="AnsellKyle2010">{{cite journal|last1=Ansell|first1=Stephen M.|last2=Kyle|first2=Robert A.|last3=Reeder|first3=Craig B.|last4=Fonseca|first4=Rafael|last5=Mikhael|first5=Joseph R.|last6=Morice|first6=William G.|last7=Bergsagel|first7=P. Leif|last8=Buadi|first8=Francis K.|last9=Colgan|first9=Joseph P.|last10=Dingli|first10=David|last11=Dispenzieri|first11=Angela|last12=Greipp|first12=Philip R.|last13=Habermann|first13=Thomas M.|last14=Hayman|first14=Suzanne R.|last15=Inwards|first15=David J.|last16=Johnston|first16=Patrick B.|last17=Kumar|first17=Shaji K.|last18=Lacy|first18=Martha Q.|last19=Lust|first19=John A.|last20=Markovic|first20=Svetomir N.|last21=Micallef|first21=Ivana N.M.|last22=Nowakowski|first22=Grzegorz S.|last23=Porrata|first23=Luis F.|last24=Roy|first24=Vivek|last25=Russell|first25=Stephen J.|last26=Short|first26=Kristen E. Detweiler|last27=Stewart|first27=A. Keith|last28=Thompson|first28=Carrie A.|last29=Witzig|first29=Thomas E.|last30=Zeldenrust|first30=Steven R.|last31=Dalton|first31=Robert J.|last32=Rajkumar|first32=S. Vincent|last33=Gertz|first33=Morie A.|title=Diagnosis and Management of Waldenström Macroglobulinemia: Mayo Stratification of Macroglobulinemia and Risk-Adapted Therapy (mSMART) Guidelines|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=824–833|issn=00256196|doi=10.4065/mcp.2010.0304}}</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! | ! colspan="2" style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|mSMART guidelines 2016 for diagnosis of Waldenstrom macroglobulinemia and associated disorders}} | ||
|- | |- | ||
|[[Waldenström macroglobulinemia]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Waldenström macroglobulinemia]] | ||
|[[IgM]] monoclonal gammopathy (regardless of the size of the [[M protein]]) with >10% [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] (usually intertrabecular) by small [[lymphocytes]] that exhibit plasmacytoid or [[plasma cell]] [[differentiation]] and a typical [[immunophenotype]] (surface [[IgM]]+, [[CD5]]–, [[CD10]]–, [[CD19]]+, [[CD20]]+, [[CD23]]–) that satisfactorily excludes other [[lymphoproliferative disorders]], including [[chronic lymphocytic leukemia]] and [[mantle cell lymphoma]] | |[[IgM]] [[monoclonal gammopathy]] (regardless of the [[Size consistency|size]] of the [[M protein]]) with >10% [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] (usually intertrabecular) by small [[lymphocytes]] that exhibit plasmacytoid or [[plasma cell]] [[differentiation]] and a [[Typical set|typical]] [[immunophenotype]] ([[Surface chemistry|surface]] [[IgM]]+, [[CD5]]–, [[CD10]]–, [[CD19]]+, [[CD20]]+, [[CD23]]–) that satisfactorily [[Exclusion criteria|excludes]] other [[lymphoproliferative disorders]], including [[chronic lymphocytic leukemia]] and [[mantle cell lymphoma]] | ||
|- | |- | ||
|[[IgM]] [[MGUS]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[IgM]] [[MGUS]] | ||
|[[Serum]] [[IgM monoclonal protein]] level <3 g/dL, [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] <10%, and no evidence of [[anemia]], constitutional [[symptoms]], [[hyperviscosity]], [[lymphadenopathy]], or [[hepatosplenomegaly]] | |[[Serum]] [[IgM monoclonal protein]] level <3 g/dL, [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] <10%, and no [[evidence]] of [[anemia]], constitutional [[symptoms]], [[hyperviscosity]], [[lymphadenopathy]], or [[hepatosplenomegaly]] | ||
|- | |- | ||
|Smoldering [[Waldenström macroglobulinemia]] (indolent /[[asymptomatic]] [[Waldenström macroglobulinemia]]) | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Smoldering [[Waldenström macroglobulinemia]] (indolent /[[asymptomatic]] [[Waldenström macroglobulinemia]]) | ||
|Serum [[IgM monoclonal protein]] level ≥3 g/dL and/or [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] ≥10% and no evidence of end-organ damage, such as [[anemia]], constitutional symptoms, [[hyperviscosity]], [[lymphadenopathy]], or [[hepatosplenomegaly]], that can be attributed to a lymphoplasmacytic proliferative disorder | |[[Serum]] [[IgM monoclonal protein]] level ≥3 g/dL and/or [[bone marrow]] lymphoplasmacytic [[Infiltration (medical)|infiltration]] ≥10% and no [[evidence]] of [[End organ damage|end-organ damage]], such as [[anemia]], constitutional [[symptoms]], [[hyperviscosity]], [[lymphadenopathy]], or [[hepatosplenomegaly]], that can be [[Attribution (psychology)|attributed]] to a lymphoplasmacytic [[Proliferation|proliferative]] [[Disorder (medicine)|disorder]] | ||
|} | |} | ||
====Definitive Diagnostic Tests==== | ====Definitive Diagnostic Tests==== | ||
*[[Genetic]] Testing: | *[[Genetic]] [[Testing]]: | ||
**ARIDA | **ARIDA | ||
**IG [[gene]] [[rearrangement]] | **[[Immunoglobulin|IG]] [[gene]] [[rearrangement]] | ||
**[[CXCR4]] 5338X | **[[CXCR4]] 5338X | ||
**[[MYD88]] L265P | **[[MYD88]] L265P | ||
| Line 62: | Line 67: | ||
===Bone Marrow Aspirate:=== | ===Bone Marrow Aspirate:=== | ||
* A [[Bone marrow aspiration|bone marrow aspirate]] is essential in the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] | * A [[Bone marrow aspiration|bone marrow aspirate]] is [[Essential medicines|essential]] in the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] | ||
* Findings [[Suggestion|suggestive]] of [[lymphoplasmacytic lymphoma]] include:<ref name="pmid18555588">{{cite journal| author=Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J et al.| title=Waldenstrom macroglobulinemia. | journal=Cancer Lett | year= 2008 | volume= 270 | issue= 1 | pages= 95-107 | pmid=18555588 | doi=10.1016/j.canlet.2008.04.040 | pmc=3133633 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18555588 }} </ref> | |||
* Findings suggestive of [[lymphoplasmacytic lymphoma]] include:<ref name="pmid18555588">{{cite journal| author=Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J et al.| title=Waldenstrom macroglobulinemia. | journal=Cancer Lett | year= 2008 | volume= 270 | issue= 1 | pages= 95-107 | pmid=18555588 | doi=10.1016/j.canlet.2008.04.040 | pmc=3133633 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18555588 }} </ref> | ** Hypercellular [[bone marrow]] [[aspirate]] | ||
**[[Lymphoplasmacytic lymphoma|Lymphoplasmacytic]] [[Infiltration (medical)|infiltrate]] with [[Characteristic function (probability theory)|characteristic]] [[immunophenotype]] | |||
** | |||
** Lymphoplasmacytic infiltrate with characteristic [[immunophenotype]] | |||
{| | {| | ||
| | | | ||
[[File:Wm bm aspirate.png|thumb|250px|none| Bone marrow aspirate. Lymphocytes with | [[File:Wm bm aspirate.png|thumb|250px|none| [[Bone marrow]] [[aspirate]]. [[Lymphocytes]] with [[Lymphoplasmacytic lymphoma|lymphoplasmacytic]] appearance (arrows).[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3894394_br-48-300-g001&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=91 Source: D'Angelo G. et al, Laboratorio di Chimica-Clinica, Ematologia e Microbiologia (Ematologia/Coagulazione), Azienda Ospedaliera "S. Antonio Abate" di Gallarate, Varese, Italy.]]] | ||
|} | |} | ||
=== Bone Marrow Biopsy: === | === Bone Marrow Biopsy: === | ||
A [[bone marrow biopsy]] may be helpful in the diagnosis of [[lymphoplasmacytic lymphoma]]. <ref name="pmid18555588">{{cite journal| author=Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J et al.| title=Waldenstrom macroglobulinemia. | journal=Cancer Lett | year= 2008 | volume= 270 | issue= 1 | pages= 95-107 | pmid=18555588 | doi=10.1016/j.canlet.2008.04.040 | pmc=3133633 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18555588 }} </ref> | *A [[bone marrow biopsy]] may be [[Help desk|helpful]] in the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] <ref name="pmid18555588">{{cite journal| author=Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J et al.| title=Waldenstrom macroglobulinemia. | journal=Cancer Lett | year= 2008 | volume= 270 | issue= 1 | pages= 95-107 | pmid=18555588 | doi=10.1016/j.canlet.2008.04.040 | pmc=3133633 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18555588 }} </ref> | ||
*Findings on the [[biopsy]] [[Suggestion|suggestive]] of [[lymphoplasmacytic lymphoma]] include:<ref name="pmid18555588">{{cite journal| author=Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J et al.| title=Waldenstrom macroglobulinemia. | journal=Cancer Lett | year= 2008 | volume= 270 | issue= 1 | pages= 95-107 | pmid=18555588 | doi=10.1016/j.canlet.2008.04.040 | pmc=3133633 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18555588 }} </ref> | |||
**Hypercellular and [[Infiltration (medical)|infiltrated]] with [[lymphoid]] and [[Plasmacytoid|plasmacytoid cells]] | |||
**Dutcher [[Body|bodies]] ([[PAS stain|PAS]] positive intra-nuclear [[vacuoles]] containing [[IgM]] [[monoclonal]] [[protein]]) | |||
***[[Characteristic function (probability theory)|Characteristic]] [[Features (pattern recognition)|feature]] of [[lymphoplasmacytic lymphoma]] | |||
*Three [[Pattern|patterns]] of [[Bone marrow|marrow]] involvement are described, as follows: | |||
**Lymphoplasmacytoid [[Cells (biology)|cells]] (lymphoplasmacytic and small [[lymphocytes]]) in a [[nodular]] [[pattern]] | |||
**[[Lymphoplasmacytic lymphoma|Lymphoplasmacytic]] [[Cells (biology)|cells]] (small [[lymphocytes]], mature [[plasma cells]], [[mast cells]]) in an [[interstitial]]/[[nodular]] [[pattern]] | |||
**A polymorphous [[Infiltration (medical)|infiltrate]] (small [[lymphocytes]], [[plasma cells]], [[plasmacytoid]] [[Cells (biology)|cells]], [[Immunoblast|immunoblasts]] with [[mitotic]] figures) | |||
===Electrophoresis and Immunofixation=== | ===Electrophoresis and Immunofixation=== | ||
[[Serum protein electrophoresis]] is important for the diagnosis of [[lymphoplasmacytic lymphoma]] | *[[Serum protein electrophoresis]] is important for the [[diagnosis]] of [[lymphoplasmacytic lymphoma]] | ||
*Findings on an [[electrophoresis]] [[diagnostic]] of [[lymphoplasmacytic lymphoma]] include:<ref name="pmid1872571">{{cite journal| author=Riches PG, Sheldon J, Smith AM, Hobbs JR| title=Overestimation of monoclonal immunoglobulin by immunochemical methods. | journal=Ann Clin Biochem | year= 1991 | volume= 28 ( Pt 3) | issue= | pages= 253-9 | pmid=1872571 | doi=10.1177/000456329102800310 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1872571 }} </ref> | |||
Findings on an [[electrophoresis]] diagnostic of [[lymphoplasmacytic lymphoma]] include:<ref name="pmid1872571">{{cite journal| author=Riches PG, Sheldon J, Smith AM, Hobbs JR| title=Overestimation of monoclonal immunoglobulin by immunochemical methods. | journal=Ann Clin Biochem | year= 1991 | volume= 28 ( Pt 3) | issue= | pages= 253-9 | pmid=1872571 | doi=10.1177/000456329102800310 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1872571 }} </ref> | **Sharp, narrow [[Spike sorting|spike]] of [[monoclonal]] [[IgM]] [[protein]] | ||
*Sharp, narrow spike of monoclonal [[IgM]] protein | **[[Dense]] band of [[monoclonal]] [[IgM]] [[protein]] | ||
*Dense band of monoclonal [[IgM]] protein | **The [[paraprotein]] can be of any [[Size consistency|size]] | ||
*The [[paraprotein]] can be of any size | *[[Serum]] [[immunofixation]] is important for the [[diagnosis]] of [[lymphoplasmacytic lymphoma]]. It helps in [[Confirmatory factor analysis|confirming]] the [[Presenting symptom|presence]] of a [[Monoclonal|monoclonal protein]], in [[Addition reaction|addition]] to determining its type<ref name="pmid1872571">{{cite journal| author=Riches PG, Sheldon J, Smith AM, Hobbs JR| title=Overestimation of monoclonal immunoglobulin by immunochemical methods. | journal=Ann Clin Biochem | year= 1991 | volume= 28 ( Pt 3) | issue= | pages= 253-9 | pmid=1872571 | doi=10.1177/000456329102800310 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1872571 }} </ref> | ||
[[Serum]] [[immunofixation]] is important for the diagnosis of [[lymphoplasmacytic lymphoma]]. It helps in confirming the presence of a [[Monoclonal|monoclonal protein]], in addition to determining its type | |||
{| | {| | ||
| | | | ||
[[File:Serum immunofixation electrophoresis.png|thumb|250px|none| Serum immunofixation electrophoresis. (A) There is a slightly dense band with IgM, kappa antisera, suggestive of monoclonal gammopathy (B) After the treatment, a dense band with IgM was disappeared.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3102879_jkms-26-824-g002&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=41 Source: Kim YL. et al, Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea.]]] | [[File:Serum immunofixation electrophoresis.png|thumb|250px|none| Serum [[immunofixation]] electrophoresis. (A) There is a slightly dense band with [[IgM]], kappa [[antisera]], suggestive of [[Monoclonal gammopathy|monoclonal]] gammopathy (B) After the treatment, a dense band with [[IgM]] was disappeared.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC3102879_jkms-26-824-g002&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=41 Source: Kim YL. et al, Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea.]]] | ||
|} | |} | ||
===CSF flow cytometry, protein electrophoresis and immunofixation for diagnosis of Bing-Neel syndrome:=== | ===CSF flow cytometry, protein electrophoresis and immunofixation for diagnosis of Bing-Neel syndrome:=== | ||
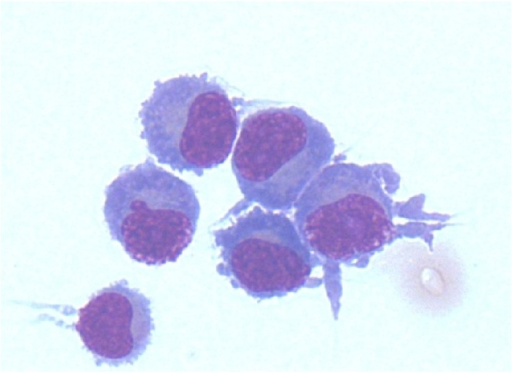
For diagnosing [[Bing-Neel syndrome]], after [[lumbar puncture]], [[CSF]] [[flow cytometry]] is done which shows a [[Lambda (anatomy)|lambda]] [[light chain]]-restricted population of [[B-cells]] consistent with a [[CD5]]+ [[CD10]]+ [[B-cell lymphoma]] | *For [[Diagnosis|diagnosing]] [[Bing-Neel syndrome]], after [[lumbar puncture]], [[CSF]] [[flow cytometry]] is [[done]] which shows a [[Lambda (anatomy)|lambda]] [[light chain]]-[[Restriction|restricted]] [[population]] of [[B-cells]] consistent with a [[CD5]]+ [[CD10]]+ [[B-cell lymphoma]] | ||
*Furthermore, [[protein electrophoresis]] and [[immunofixation]] should be [[done]] for the [[Detection theory|detection]] and [[classification]] of a [[monoclonal]] [[protein]] as well as [[molecular]] [[diagnostic testing]] for [[immunoglobulin]] [[gene]] [[rearrangement]] and [[mutated]] [[MYD88]]<ref name="pmid30228918">{{cite journal| author=O'Neil DS, Francescone MA, Khan K, Bachir A, O'Connor OA, Sawas A| title=A Case of Bing-Neel Syndrome Successfully Treated with Ibrutinib. | journal=Case Rep Hematol | year= 2018 | volume= 2018 | issue= | pages= 8573105 | pmid=30228918 | doi=10.1155/2018/8573105 | pmc=6136466 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30228918 }} </ref><ref name="pmid27758817">{{cite journal| author=Minnema MC, Kimby E, D'Sa S, Fornecker LM, Poulain S, Snijders TJ et al.| title=Guideline for the diagnosis, treatment and response criteria for Bing-Neel syndrome. | journal=Haematologica | year= 2017 | volume= 102 | issue= 1 | pages= 43-51 | pmid=27758817 | doi=10.3324/haematol.2016.147728 | pmc=5210231 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27758817 }} </ref><ref name="pmid30279255">{{cite journal| author=Tallant A, Selig D, Wanko SO, Roswarski J| title=First-line ibrutinib for Bing-Neel syndrome. | journal=BMJ Case Rep | year= 2018 | volume= 2018 | issue= | pages= | pmid=30279255 | doi=10.1136/bcr-2018-226102 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30279255 }} </ref> | |||
{| | {| | ||
| | | | ||
[[File:Brain biopsy. | [[File:Brain biopsy gif.gif|thumb|250px|none| Stereotactic brain [[biopsy]] showing diffuse infiltration of atypical plasmacytoid [[lymphocytes]] into the dural [[fibrous tissue]] (A) [[Hematoxylin and eosin stain|Hematoxylin]] & eosin (original magnification ×200); (B) Positive [[immunohistochemical]] staining for [[CD20]] (original magnification ×40). [https://openi.nlm.nih.gov/detailedresult.php?img=PMC2694623_jkms-22-1079-g002&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=29 Source: Kim HD. et al, Department of Internal Medicine, Yeoungnam University College of Medicine, Daegu, Korea.]]] | ||
| | | | ||
[[File:Csf plasmacytoid cells.png|thumb|250px|none| Plasmacytoid cells found on cytospin of the cerebrospinal fluid confirming cellular infiltration of the central nervous system.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC4837273_CRIHEM2016-3931709.004&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=71 Source: Halperin D. et al, Whipps Cross Hospital, London E11 1NR, UK.]]] | [[File:Csf plasmacytoid cells.png|thumb|250px|none| Plasmacytoid cells found on cytospin of the cerebrospinal fluid confirming cellular infiltration of the central nervous system.[https://openi.nlm.nih.gov/detailedresult.php?img=PMC4837273_CRIHEM2016-3931709.004&query=waldenstrom+macroglobulinaemia&it=xg&req=4&npos=71 Source: Halperin D. et al, Whipps Cross Hospital, London E11 1NR, UK.]]] | ||
| Line 114: | Line 116: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Disease]] | |||
[[Category:Blood]] | |||
[[Category:Hematology]] | |||
Latest revision as of 14:44, 29 October 2019
|
Lymphoplasmacytic lymphoma Microchapters |
|
Differentiating Lymphoplasmacytic Lymphoma from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Lymphoplasmacytic lymphoma diagnostic study of choice On the Web |
|
American Roentgen Ray Society Images of Lymphoplasmacytic lymphoma diagnostic study of choice |
|
FDA on Lymphoplasmacytic lymphoma diagnostic study of choice |
|
CDC on Lymphoplasmacytic lymphoma diagnostic study of choice |
|
Lymphoplasmacytic lymphoma diagnostic study of choice in the news |
|
Blogs on Lymphoplasmacytic lymphoma diagnostic study of choice |
|
Risk calculators and risk factors for Lymphoplasmacytic lymphoma diagnostic study of choice |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
The diagnosis of lymphoplasmacytic lymphoma is based on bone marrow aspiration and biopsy and serum protein analysis studies such as immunohistochemistry, flow cytometry and cytogenetics to distinguish LPL from other types of B-cell lymphomas. CSF flow cytometry, protein electrophoresis and immunofixation is done for the diagnosis of Bing-Neel syndrome (a late, but severe, rare complication).
Diagnostic Study of Choice
- There is no single diagnostic study of choice for the diagnosis of lymphoplasmacytic lymphoma (LPL), but bone marrow aspiration and biopsy is considered to be mandatory for the assessment of patients with LPL and further supported by monoclonal protein/immunophenotypic studies such as immunohistochemistry, flow cytometry and cytogenetics to distinguish LPL from other types of B-cell lymphomas.[1][2]
- Not all the diagnostic tests mentioned are performed in a patient with lymphoplasmacytic lymphoma. A doctor takes into account the following factors before choosing diagnostic tests in a particular patient:
Diagnostic Criteria:
Diagnostic criteria presented in second International Workshop, Greece, 2002
- In September 26-30, 2002, in Athens, Greece,the Second International Workshop was held in which a diagnostic criteria for Waldenstrom's Macroglobulinemia was proposed. According to this criteria, the following findings on performing bone marrow biopsy and serum protein analysis are confirmatory of Waldenström macroglobulinemia and exclude other small B cell lymphoid neoplasms with plasmacytic differentiation:[1][3]
mSMART guidelines for diagnosis of Waldenstrom macroglobulinemia and associated disorders
- Mayo Stratification of Macroglobulinemia and Risk-Adapted Therapy (mSMART) Guidelines 2016 for diagnosis of Waldenstrom macroglobulinemia and associated disorders are as follows:[4]
Definitive Diagnostic Tests
- Genetic Testing:
- ARIDA
- IG gene rearrangement
- CXCR4 5338X
- MYD88 L265P
- Immunophenotyping
- Serum paraprotein
Bone Marrow Aspirate:
- A bone marrow aspirate is essential in the diagnosis of lymphoplasmacytic lymphoma
- Findings suggestive of lymphoplasmacytic lymphoma include:[5]
- Hypercellular bone marrow aspirate
- Lymphoplasmacytic infiltrate with characteristic immunophenotype
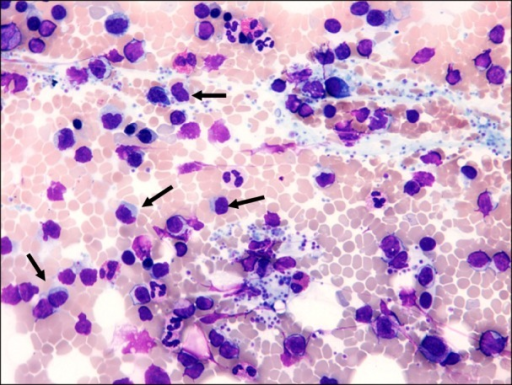 |
Bone Marrow Biopsy:
- A bone marrow biopsy may be helpful in the diagnosis of lymphoplasmacytic lymphoma [5]
- Findings on the biopsy suggestive of lymphoplasmacytic lymphoma include:[5]
- Hypercellular and infiltrated with lymphoid and plasmacytoid cells
- Dutcher bodies (PAS positive intra-nuclear vacuoles containing IgM monoclonal protein)
- Three patterns of marrow involvement are described, as follows:
- Lymphoplasmacytoid cells (lymphoplasmacytic and small lymphocytes) in a nodular pattern
- Lymphoplasmacytic cells (small lymphocytes, mature plasma cells, mast cells) in an interstitial/nodular pattern
- A polymorphous infiltrate (small lymphocytes, plasma cells, plasmacytoid cells, immunoblasts with mitotic figures)
Electrophoresis and Immunofixation
- Serum protein electrophoresis is important for the diagnosis of lymphoplasmacytic lymphoma
- Findings on an electrophoresis diagnostic of lymphoplasmacytic lymphoma include:[6]
- Sharp, narrow spike of monoclonal IgM protein
- Dense band of monoclonal IgM protein
- The paraprotein can be of any size
- Serum immunofixation is important for the diagnosis of lymphoplasmacytic lymphoma. It helps in confirming the presence of a monoclonal protein, in addition to determining its type[6]
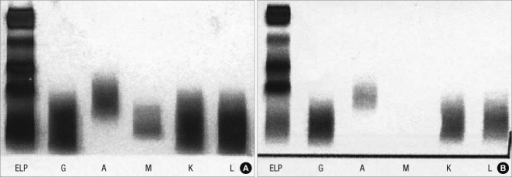 |
CSF flow cytometry, protein electrophoresis and immunofixation for diagnosis of Bing-Neel syndrome:
- For diagnosing Bing-Neel syndrome, after lumbar puncture, CSF flow cytometry is done which shows a lambda light chain-restricted population of B-cells consistent with a CD5+ CD10+ B-cell lymphoma
- Furthermore, protein electrophoresis and immunofixation should be done for the detection and classification of a monoclonal protein as well as molecular diagnostic testing for immunoglobulin gene rearrangement and mutated MYD88[7][8][9]
 |
 |
References
- ↑ 1.0 1.1 Dimopoulos MA, Kyle RA, Anagnostopoulos A, Treon SP (2005). "Diagnosis and management of Waldenstrom's macroglobulinemia". J Clin Oncol. 23 (7): 1564–77. doi:10.1200/JCO.2005.03.144. PMID 15735132.
- ↑ Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R; et al. (2016). "The 2016 revision of the World Health Organization classification of lymphoid neoplasms". Blood. 127 (20): 2375–90. doi:10.1182/blood-2016-01-643569. PMC 4874220. PMID 26980727.
- ↑ Owen RG, Treon SP, Al-Katib A, Fonseca R, Greipp PR, McMaster ML; et al. (2003). "Clinicopathological definition of Waldenstrom's macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom's Macroglobulinemia". Semin Oncol. 30 (2): 110–5. doi:10.1053/sonc.2003.50082. PMID 12720118.
- ↑ Ansell, Stephen M.; Kyle, Robert A.; Reeder, Craig B.; Fonseca, Rafael; Mikhael, Joseph R.; Morice, William G.; Bergsagel, P. Leif; Buadi, Francis K.; Colgan, Joseph P.; Dingli, David; Dispenzieri, Angela; Greipp, Philip R.; Habermann, Thomas M.; Hayman, Suzanne R.; Inwards, David J.; Johnston, Patrick B.; Kumar, Shaji K.; Lacy, Martha Q.; Lust, John A.; Markovic, Svetomir N.; Micallef, Ivana N.M.; Nowakowski, Grzegorz S.; Porrata, Luis F.; Roy, Vivek; Russell, Stephen J.; Short, Kristen E. Detweiler; Stewart, A. Keith; Thompson, Carrie A.; Witzig, Thomas E.; Zeldenrust, Steven R.; Dalton, Robert J.; Rajkumar, S. Vincent; Gertz, Morie A. (2010). "Diagnosis and Management of Waldenström Macroglobulinemia: Mayo Stratification of Macroglobulinemia and Risk-Adapted Therapy (mSMART) Guidelines". Mayo Clinic Proceedings. 85 (9): 824–833. doi:10.4065/mcp.2010.0304. ISSN 0025-6196.
- ↑ 5.0 5.1 5.2 Leleu X, Roccaro AM, Moreau AS, Dupire S, Robu D, Gay J; et al. (2008). "Waldenstrom macroglobulinemia". Cancer Lett. 270 (1): 95–107. doi:10.1016/j.canlet.2008.04.040. PMC 3133633. PMID 18555588.
- ↑ 6.0 6.1 Riches PG, Sheldon J, Smith AM, Hobbs JR (1991). "Overestimation of monoclonal immunoglobulin by immunochemical methods". Ann Clin Biochem. 28 ( Pt 3): 253–9. doi:10.1177/000456329102800310. PMID 1872571.
- ↑ O'Neil DS, Francescone MA, Khan K, Bachir A, O'Connor OA, Sawas A (2018). "A Case of Bing-Neel Syndrome Successfully Treated with Ibrutinib". Case Rep Hematol. 2018: 8573105. doi:10.1155/2018/8573105. PMC 6136466. PMID 30228918.
- ↑ Minnema MC, Kimby E, D'Sa S, Fornecker LM, Poulain S, Snijders TJ; et al. (2017). "Guideline for the diagnosis, treatment and response criteria for Bing-Neel syndrome". Haematologica. 102 (1): 43–51. doi:10.3324/haematol.2016.147728. PMC 5210231. PMID 27758817.
- ↑ Tallant A, Selig D, Wanko SO, Roswarski J (2018). "First-line ibrutinib for Bing-Neel syndrome". BMJ Case Rep. 2018. doi:10.1136/bcr-2018-226102. PMID 30279255.