Indacaterol and glycopyrrolate: Difference between revisions
No edit summary |
No edit summary |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 14: | Line 14: | ||
*This finding with salmeterol is considered a class effect of all LABAs, including indacaterol, one of the active ingredients in indacaterol and glycopyrrolate. | *This finding with salmeterol is considered a class effect of all LABAs, including indacaterol, one of the active ingredients in indacaterol and glycopyrrolate. | ||
*The safety and efficacy of indacaterol and glycopyrrolate in patients with asthma have not been established. Indacaterol and glycopyrrolate is not indicated for the treatment of asthma. | *The safety and efficacy of indacaterol and glycopyrrolate in patients with asthma have not been established. Indacaterol and glycopyrrolate is not indicated for the treatment of asthma. | ||
|fdaLIADAdult=[[Indacaterol]] and [[glycopyrrolate]] is indicated for the long-term, maintenance treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema. [[Indacaterol]] and [[glycopyrrolate]] is NOT indicated for the relief of acute bronchospasm or for the treatment of asthma. | |fdaLIADAdult=[[Indacaterol]] and [[glycopyrrolate]] is indicated for the long-term, maintenance treatment of airflow obstruction in patients with [[chronic obstructive pulmonary disease]] (COPD), including [[chronic bronchitis]] and/or [[emphysema]]. [[Indacaterol]] and [[glycopyrrolate]] is NOT indicated for the relief of [[acute bronchospasm]] or for the treatment of [[asthma]]. | ||
'''Dosing Information''' | '''Dosing Information''' | ||
*The recommended dosage of [[indacaterol]] and [[glycopyrrolate]] is the inhalation of the contents of one [[indacaterol]] and [[glycopyrrolate]] capsule twice-daily using the NEOHALER device. | *The recommended dosage of [[indacaterol]] and [[glycopyrrolate]] is the inhalation of the contents of one [[indacaterol]] and [[glycopyrrolate]] capsule twice-daily using the NEOHALER device. | ||
*No dosage adjustment is required for geriatric patients, patients with mild and moderate hepatic impairment, or patients with mild to moderate renal impairment. | *No dosage adjustment is required for geriatric patients, patients with mild and moderate hepatic impairment, or patients with mild to moderate [[renal impairment]]. | ||
|offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of indacaterol and glycopyrrolate in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of indacaterol and glycopyrrolate in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of indacaterol and glycopyrrolate in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of indacaterol and glycopyrrolate in adult patients. | ||
|offLabelPedGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Indacaterol and glycopyrrolate in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Indacaterol and glycopyrrolate in pediatric patients. | ||
|offLabelPedNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of Indacaterol and glycopyrrolate in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding ''Off-Label Non–Guideline-Supported Use'' of Indacaterol and glycopyrrolate in pediatric patients. | ||
|contraindications=*All LABAs are contraindicated in patients with asthma without use of a long-term asthma control medication. | |contraindications=*All [[LABA|LABAs]] are contraindicated in patients with [[asthma]] without use of a long-term [[asthma]] control medication. | ||
*[[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of asthma. | *[[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of [[asthma]]. | ||
*[[Indacaterol]] and [[glycopyrrolate]] is contraindicated in patients who have demonstrated hypersensitivity to indacaterol, glycopyrrolate, or to any of the ingredients. | *[[Indacaterol]] and [[glycopyrrolate]] is contraindicated in patients who have demonstrated [[hypersensitivity]] to [[indacaterol]], [[glycopyrrolate]], or to any of the ingredients. | ||
|warnings=*Asthma-Related Death | |warnings=*[[Asthma]]-Related Death | ||
**Data from a large, placebo-controlled U.S. study in asthma patients showed that LABAs may increase the risk of asthma-related death. | **Data from a large, placebo-controlled U.S. study in [[asthma]] patients showed that [[LABA|LABAs]] may increase the risk of [[asthma]]-related death. | ||
**Data are not available to determine whether the rate of death in patients with COPD is increased by LABAs. | **Data are not available to determine whether the rate of death in patients with [[COPD]] is increased by [[LABA|LABAs]]. | ||
**A 28-week, placebo-controlled U.S. study comparing the safety of another LABA (salmeterol) with placebo, each added to usual asthma therapy, showed an increase in asthma-related deaths in patients receiving salmeterol (13/13,176 in patients treated with salmeterol versus 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34). | **A 28-week, placebo-controlled U.S. study comparing the safety of another [[LABA]] ([[salmeterol]]) with placebo, each added to usual [[asthma]] therapy, showed an increase in [[asthma]]-related deaths in patients receiving [[salmeterol]] (13/13,176 in patients treated with [[salmeterol]] versus 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34). | ||
**The increased risk of asthma-related death is considered a class effect of the LABAs, including | **The increased risk of [[asthma]]-related death is considered a class effect of the [[LABA|LABAs]], including [[indacaterol]]. | ||
**No study adequate to determine whether the rate of asthma-related death is increased in patients treated with [[indacaterol]] and [[glycopyrrolate]] has been conducted. The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] in patients with asthma have not been established. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of asthma. | **No study adequate to determine whether the rate of [[asthma]]-related death is increased in patients treated with [[indacaterol]] and [[glycopyrrolate]] has been conducted. The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] in patients with [[asthma]] have not been established. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of [[asthma]]. | ||
*Deterioration of Disease and Acute Episodes | *Deterioration of Disease and Acute Episodes | ||
**[[Indacaterol]] and [[glycopyrrolate]] should not be initiated in patients with acutely deteriorating or potentially life-threatening episodes of COPD. [[Indacaterol]] and [[glycopyrrolate]] has not been studied in patients with acutely deteriorating COPD. The initiation of [[indacaterol]] and [[glycopyrrolate]] in this setting is not appropriate. | **[[Indacaterol]] and [[glycopyrrolate]] should not be initiated in patients with acutely deteriorating or potentially life-threatening episodes of [[COPD]]. [[Indacaterol]] and [[glycopyrrolate]] has not been studied in patients with acutely deteriorating [[COPD]]. The initiation of [[indacaterol]] and [[glycopyrrolate]] in this setting is not appropriate. | ||
**[[Indacaterol]] and [[glycopyrrolate]] should not be used for the relief of acute symptoms, i.e., as rescue therapy for the treatment of acute episodes of bronchospasm. [[Indacaterol]] and [[glycopyrrolate]] has not been studied in the relief of acute symptoms, and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist. | **[[Indacaterol]] and [[glycopyrrolate]] should not be used for the relief of acute symptoms, i.e., as rescue therapy for the treatment of acute episodes of [[bronchospasm]]. [[Indacaterol]] and [[glycopyrrolate]] has not been studied in the relief of acute symptoms, and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, [[SABA|short-acting beta2-agonist]]. | ||
**When beginning [[indacaterol]] and [[glycopyrrolate]], patients who have been taking oral or inhaled, short-acting beta2-agonists on a regular basis (e.g., 4 times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. | **When beginning [[indacaterol]] and [[glycopyrrolate]], patients who have been taking oral or inhaled, [[SABA|short-acting beta2-agonists]] on a regular basis (e.g., 4 times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. | ||
**When prescribing [[indacaterol]] and [[glycopyrrolate]], the healthcare provider should also prescribe an inhaled, short-acting beta2-agonist and instruct the patient on how it should be used. Increasing inhaled beta2-agonist use is a signal of deteriorating disease for which prompt medical attention is indicated. | **When prescribing [[indacaterol]] and [[glycopyrrolate]], the healthcare provider should also prescribe an inhaled, [[SABA|short-acting beta2-agonist]] and instruct the patient on how it should be used. Increasing inhaled [[Beta2-adrenergic receptor agonist|beta2-agonist]] use is a signal of deteriorating disease for which prompt medical attention is indicated. | ||
**COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If [[indacaterol]] and [[glycopyrrolate]] no longer controls the symptoms of bronchoconstriction; the patient’s inhaled, short-acting beta2-agonist becomes less effective; or the patient needs more inhalation of short-acting beta2-agonist than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dose of [[indacaterol]] and [[glycopyrrolate]] beyond the recommended dose is not appropriate in this situation. | **[[COPD]] may deteriorate acutely over a period of hours or chronically over several days or longer. If [[indacaterol]] and [[glycopyrrolate]] no longer controls the symptoms of [[bronchoconstriction]]; the patient’s inhaled, [[SABA|short-acting beta2-agonist]] becomes less effective; or the patient needs more inhalation of [[SABA|short-acting beta2-agonist]] than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the [[COPD]] treatment regimen should be undertaken at once. Increasing the daily dose of [[indacaterol]] and [[glycopyrrolate]] beyond the recommended dose is not appropriate in this situation. | ||
*Excessive Use of [[ | *Excessive Use of [[Indacaterol]] and [[Glycopyrrolate]] and Use with Other [[LABA|Long-Acting Beta2-Adrenergic Agonists]] | ||
**As with other inhaled drugs containing beta2-adrenergics, [[indacaterol]] and [[glycopyrrolate]] should not be used more often than recommended, at higher doses than recommended, or in conjunction with other medications containing LABAs, as an overdose may result. | **As with other inhaled drugs containing [[Beta2-adrenergic receptor agonist|beta2-adrenergics]], [[indacaterol]] and [[glycopyrrolate]] should not be used more often than recommended, at higher doses than recommended, or in conjunction with other medications containing [[LABA|LABAs]], as an overdose may result. | ||
**Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs. | **Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled [[sympathomimetic]] drugs. | ||
**Patients using [[indacaterol]] and [[glycopyrrolate]] should not use another medicine containing a LABA for any reason. | **Patients using [[indacaterol]] and [[glycopyrrolate]] should not use another medicine containing a [[LABA]] for any reason. | ||
*Paradoxical Bronchospasm | *Paradoxical [[Bronchospasm]] | ||
**As with other inhaled medicines, [[indacaterol]] and [[glycopyrrolate]] can produce paradoxical bronchospasm that may be life-threatening. | **As with other inhaled medicines, [[indacaterol]] and [[glycopyrrolate]] can produce paradoxical [[bronchospasm]] that may be life-threatening. | ||
**If paradoxical bronchospasm occurs following dosing with [[indacaterol]] and [[glycopyrrolate]], it should be treated immediately with an inhaled, short-acting bronchodilator; [[indacaterol]] and [[glycopyrrolate]] should be discontinued immediately and alternative therapy instituted. | **If paradoxical [[bronchospasm]] occurs following dosing with [[indacaterol]] and [[glycopyrrolate]], it should be treated immediately with an inhaled, short-acting [[bronchodilator]]; [[indacaterol]] and [[glycopyrrolate]] should be discontinued immediately and alternative therapy instituted. | ||
*Immediate Hypersensitivity Reactions | *Immediate [[Hypersensitivity]] Reactions | ||
**Immediate hypersensitivity reactions have been reported after administration of indacaterol or glycopyrrolate, the components of [[indacaterol]] and [[glycopyrrolate]]. If signs suggesting allergic reactions occur, in particular, angioedema (including difficulties in breathing or swallowing, swelling of tongue, lips and face), urticaria, or skin rash, [[indacaterol]] and [[glycopyrrolate]] should be discontinued immediately and alternative therapy instituted. [[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with severe hypersensitivity to milk proteins. | **Immediate [[hypersensitivity]] reactions have been reported after administration of [[indacaterol]] or [[glycopyrrolate]], the components of [[indacaterol]] and [[glycopyrrolate]]. If signs suggesting [[allergic reactions]] occur, in particular, [[angioedema]] (including difficulties in breathing or swallowing, swelling of tongue, lips and face), [[urticaria]], or [[skin rash]], [[indacaterol]] and [[glycopyrrolate]] should be discontinued immediately and alternative therapy instituted. [[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with severe [[hypersensitivity]] to milk proteins. | ||
*Cardiovascular Effects | *Cardiovascular Effects | ||
**Indacaterol, like other beta2-agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic or diastolic blood pressure, or symptoms. If such effects occur, [[indacaterol]] and [[glycopyrrolate]] may need to be discontinued. | **[[Indacaterol]], like other [[Beta2-adrenergic receptor agonist|beta2-agonists]], can produce a clinically significant cardiovascular effect in some patients as measured by increases in [[pulse rate]], [[systolic]] or [[diastolic blood pressure]], or symptoms. If such effects occur, [[indacaterol]] and [[glycopyrrolate]] may need to be discontinued. | ||
**In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T-wave, prolongation of the QTc interval, and ST segment depression, although the clinical significance of these findings is unknown. | **In addition, [[beta-agonists]] have been reported to produce [[ECG]] changes, such as flattening of the [[T-wave]], prolongation of the [[QTc interval]], and [[ST segment]] depression, although the clinical significance of these findings is unknown. | ||
**Therefore, [[indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension. | **Therefore, [[indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, [[cardiac arrhythmias]], and [[hypertension]]. | ||
*Coexisting Conditions | *Coexisting Conditions | ||
**[[Indacaterol]] and [[glycopyrrolate]], like all medicines containing sympathomimetic amines, should be used with caution in patients with convulsive disorders or thyrotoxicosis, and in patients who are unusually responsive to sympathomimetic amines. | **[[Indacaterol]] and [[glycopyrrolate]], like all medicines containing [[sympathomimetic amine|sympathomimetic amines]], should be used with caution in patients with convulsive disorders or [[thyrotoxicosis]], and in patients who are unusually responsive to [[sympathomimetic amine|sympathomimetic amines]]. | ||
**Doses of the related beta2-agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis. | **Doses of the related [[Beta2-adrenergic receptor agonist|beta2-agonist]] albuterol, when administered [[intravenous|intravenously]], have been reported to aggravate preexisting [[diabetes mellitus]] and [[ketoacidosis]]. | ||
*Worsening of Narrow-Angle Glaucoma | *Worsening of [[Narrow-angle glaucoma|Narrow-Angle Glaucoma]] | ||
**[[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with narrow-angle glaucoma. Prescribers and patients should be alert for signs and symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion and corneal edema). | **[[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with [[narrow-angle glaucoma]]. Prescribers and patients should be alert for signs and symptoms of acute [[narrow-angle glaucoma]] (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from [[conjunctiva|conjunctival]] congestion and [[cornea|corneal]] [[edema]]). | ||
**Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | **Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | ||
*Worsening of Urinary Retention | *Worsening of [[Urinary Retention]] | ||
**[[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with urinary retention. Prescribers and patients should be alert for signs and symptoms of urinary retention (e.g., difficulty passing urine, painful urination), especially in patients with prostatic hyperplasia or bladder-neck obstruction. | **[[Indacaterol]] and [[glycopyrrolate]] should be used with caution in patients with [[urinary retention]]. Prescribers and patients should be alert for signs and symptoms of [[urinary retention]] (e.g., [[difficulty passing urine]], [[painful urination]]), especially in patients with prostatic [[hyperplasia]] or bladder-neck obstruction. | ||
**Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | **Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | ||
*Hypokalemia and Hyperglycemia | *[[Hypokalemia]] and [[Hyperglycemia]] | ||
**Beta2-adrenergic agonists may produce significant hypokalemia in some patients, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation. | **[[Beta2-adrenergic receptor agonist|Beta2-adrenergic agonists]] may produce significant [[hypokalemia]] in some patients, which has the potential to produce adverse cardiovascular effects. The decrease in serum [[potassium]] is usually transient, not requiring supplementation. | ||
**Inhalation of high doses of beta2-adrenergic agonists may produce increases in plasma glucose. | **Inhalation of high doses of [[Beta2-adrenergic receptor agonist|beta2-adrenergic agonists]] may produce increases in plasma [[glucose]]. | ||
**In patients with severe COPD, hypokalemia may be potentiated by hypoxia and concomitant treatment, which may increase the susceptibility for cardiac arrhythmias. | **In patients with severe [[COPD]], [[hypokalemia]] may be potentiated by [[hypoxia]] and concomitant treatment, which may increase the susceptibility for [[cardiac arrhythmias]]. | ||
**In 2 clinical trials of 12-weeks duration evaluating [[indacaterol]] and [[glycopyrrolate]] in subjects with COPD, there was no evidence of a treatment effect on serum glucose or potassium. | **In 2 clinical trials of 12-weeks duration evaluating [[indacaterol]] and [[glycopyrrolate]] in subjects with [[COPD]], there was no evidence of a treatment effect on serum [[glucose]] or [[potassium]]. | ||
|clinicalTrials=LABAs, such as indacaterol, one of the active ingredients in [[indacaterol]] and [[glycopyrrolate]], increase the risk of asthma-related death. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of asthma. | |clinicalTrials=[[LABA|LABAs]], such as indacaterol, one of the active ingredients in [[indacaterol]] and [[glycopyrrolate]], increase the risk of [[asthma]]-related death. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of [[asthma]]. | ||
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in clinical practice. | Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in clinical practice. | ||
The [[indacaterol]] and [[glycopyrrolate]] safety database included 2654 subjects with COPD in two 12-week lung function trials and one 52-week long-term safety study. A total of 712 subjects received treatment with [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg twice daily (BID). The safety data described below are based on the two 12-week trials and the one 52-week trial. | The [[indacaterol]] and [[glycopyrrolate]] safety database included 2654 subjects with [[COPD]] in two 12-week lung function trials and one 52-week long-term safety study. A total of 712 subjects received treatment with [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg twice daily (BID). The safety data described below are based on the two 12-week trials and the one 52-week trial. | ||
'''12-Week Trials:''' | '''12-Week Trials:''' | ||
The most common adverse reaction (incidence greater than or equal to 2% and higher than placebo) was nasopharyngitis and hypertension. | The incidence of adverse reactions associated with [[indacaterol]] and [[glycopyrrolate]] in Table 1 is based on two 12-week, placebo-controlled trials (Trials 1 and 2; N=1,001 and N=1,042 respectively). Of the 2040 subjects, 63% were male and 91% were Caucasian. They had a mean age of 63 years and an average smoking history of 47 pack-years, with 52% identified as current smokers. At screening, the mean post-[[bronchodilator]] percent predicted [[forced expiratory volume]] in 1 second ([[FEV1]]) was 55% (range: 29% to 79%), the mean post-[[bronchodilator]] [[FEV1]]/[[forced vital capacity]] ([[FVC]]) ratio was 50% (range: 19% to 71%), and the mean percent reversibility was 23% (range: 0% to 144%). | ||
The most common adverse reaction (incidence greater than or equal to 2% and higher than placebo) was [[nasopharyngitis]] and [[hypertension]]. | |||
The proportion of patients who discontinued treatment due to adverse reactions was 2.95% for the [[indacaterol]] and [[glycopyrrolate]] treated patients and 4.13% for placebo-treated patients. | The proportion of patients who discontinued treatment due to adverse reactions was 2.95% for the [[indacaterol]] and [[glycopyrrolate]] treated patients and 4.13% for placebo-treated patients. | ||
Subjects received 1 dose twice-daily of the following: [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg, indacaterol 27.5 mcg, glycopyrrolate 15.6 mcg, or placebo. | Subjects received 1 dose twice-daily of the following: [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg, [[indacaterol]] 27.5 mcg, [[glycopyrrolate]] 15.6 mcg, or placebo. | ||
[[File:Indacaterol and glycopyrrolate T1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate T1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
Other adverse reactions occurring more frequently with [[indacaterol]] and [[glycopyrrolate]] than with placebo, but with an incidence of less than 1% include dyspepsia, gastroenteritis, chest pain, fatigue, peripheral edema, rash/pruritus, insomnia, dizziness, bladder obstruction/urinary retention, atrial fibrillation, palpitations, tachycardia. | Other adverse reactions occurring more frequently with [[indacaterol]] and [[glycopyrrolate]] than with placebo, but with an incidence of less than 1% include [[dyspepsia]], [[gastroenteritis]], [[chest pain]], [[fatigue]], [[peripheral edema]], [[rash]]/[[pruritus]], [[insomnia]], [[dizziness]], [[bladder]] obstruction/[[urinary retention]], [[atrial fibrillation]], [[palpitations]], [[tachycardia]]. | ||
'''52-Week Trial''' | '''52-Week Trial:''' | ||
In a long-term safety trial, 614 subjects were treated for up to 52 weeks with indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg twice-daily, indacaterol/glycopyrrolate 27.5/31.2 mcg twice-daily or indacaterol 75 mcg once-daily. The demographic and baseline characteristics of the long-term safety trial were similar to those of the placebo-controlled efficacy trials described above. The adverse reactions reported in the long-term safety trial were consistent with those observed in the placebo-controlled trials of 12 weeks. Additional adverse reactions that occurred with a frequency greater than or equal to 2% in the group receiving indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg twice-daily that exceeded the frequency of indacaterol 75 mcg once-daily in this trial were upper and lower respiratory tract infection, pneumonia, diarrhea, headache, gastroesophageal reflux disease, hyperglycemia, rhinitis. | |||
|postmarketing=The following additional adverse reactions of angioedema and dysphonia have been identified during worldwide post-approval use of indacaterol/glycopyrrolate at higher than the recommended dose. Because this reaction is reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure. | In a long-term safety trial, 614 subjects were treated for up to 52 weeks with [[indacaterol]]/[[glycopyrrolate]] 27.5 mcg/15.6 mcg twice-daily, [[indacaterol]]/[[glycopyrrolate]] 27.5/31.2 mcg twice-daily or [[indacaterol]] 75 mcg once-daily. The demographic and baseline characteristics of the long-term safety trial were similar to those of the placebo-controlled efficacy trials described above. The adverse reactions reported in the long-term safety trial were consistent with those observed in the placebo-controlled trials of 12 weeks. Additional adverse reactions that occurred with a frequency greater than or equal to 2% in the group receiving [[indacaterol]]/[[glycopyrrolate]] 27.5 mcg/15.6 mcg twice-daily that exceeded the frequency of [[indacaterol]] 75 mcg once-daily in this trial were upper and [[lower respiratory tract infection]], [[pneumonia]], [[diarrhea]], [[headache]], [[gastroesophageal reflux disease]], [[hyperglycemia]], [[rhinitis]]. | ||
|drugInteractions=*Adrenergic Drugs | |postmarketing=The following additional adverse reactions of [[angioedema]] and [[dysphonia]] have been identified during worldwide post-approval use of [[indacaterol]]/[[glycopyrrolate]] at higher than the recommended dose. Because this reaction is reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure. | ||
**If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of indacaterol, a component of [[indacaterol]] and [[glycopyrrolate]], may be potentiated. | |drugInteractions=*[[Adrenergic]] Drugs | ||
*Xanthine Derivatives, Steroids, or Diuretics | **If additional [[adrenergic]] drugs are to be administered by any route, they should be used with caution because the sympathetic effects of [[indacaterol]], a component of [[indacaterol]] and [[glycopyrrolate]], may be potentiated. | ||
**Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of beta2-adrenergic agonists such as indacaterol, a component of [[indacaterol]] and [[glycopyrrolate]]. | *[[Xanthine]] Derivatives, [[steroid|Steroids]], or [[diuretic|Diuretics]] | ||
*Non-Potassium-Sparing Diuretics | **Concomitant treatment with [[xanthine]] derivatives, [[steroids]], or [[diuretics]] may potentiate any hypokalemic effect of [[Beta2-adrenergic agonist|beta2-adrenergic agonists]] such as [[indacaterol]], a component of [[indacaterol]] and [[glycopyrrolate]]. | ||
**The electrocardiographic (ECG) changes and/or hypokalemia that may result from the administration of non-potassium-sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, such as indacaterol, a component of [[indacaterol]] and [[glycopyrrolate]], especially when the recommended dose of the beta-agonist is exceeded. | *Non-[[Potassium-sparing diuretics|Potassium-Sparing Diuretics]] | ||
**Although the clinical relevance of these effects is not known, caution is advised in the coadministration of [[indacaterol]] and [[glycopyrrolate]] with non-potassium-sparing diuretics. | **The [[electrocardiographic]] (ECG) changes and/or [[hypokalemia]] that may result from the administration of non-[[potassium-sparing diuretics]] (such as loop or [[thiazide diuretics]]) can be acutely worsened by [[beta-agonists]], such as [[indacaterol]], a component of [[indacaterol]] and [[glycopyrrolate]], especially when the recommended dose of the [[beta-agonist]] is exceeded. | ||
*Monoamine Oxidase Inhibitors, Tricyclic Antidepressants, QTc-Prolonging Drugs | **Although the clinical relevance of these effects is not known, caution is advised in the coadministration of [[indacaterol]] and [[glycopyrrolate]] with non-[[potassium-sparing diuretics]]. | ||
**Indacaterol, one of the components of [[indacaterol]] and [[glycopyrrolate]], as with other beta2-agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors, tricyclic antidepressants, or other drugs known to prolong the QTc interval because the action of adrenergic agonists on the cardiovascular system may be potentiated by these agents. | *[[Monoamine oxidase inhibitors|Monoamine Oxidase Inhibitors]], [[Tricyclic antidepressants|Tricyclic Antidepressants]], [[QTc]]-Prolonging Drugs | ||
**Drugs that are known to prolong the QTc interval may have an increased risk of ventricular arrhythmias. | **[[Indacaterol]], one of the components of [[indacaterol]] and [[glycopyrrolate]], as with other [[Beta2-adrenergic receptor agonist|beta2-agonists]], should be administered with extreme caution to patients being treated with [[monoamine oxidase inhibitors]], [[tricyclic antidepressants]], or other drugs known to prolong the [[QTc interval]] because the action of [[adrenergic agonists]] on the cardiovascular system may be potentiated by these agents. | ||
*Beta-Blockers | **Drugs that are known to prolong the [[QTc interval]] may have an increased risk of [[ventricular arrhythmias]]. | ||
**Beta-adrenergic receptor antagonists (beta-blockers) and [[indacaterol]] and [[glycopyrrolate]] may interfere with the effect of each other when administered concurrently. | *[[Beta-blockers|Beta-Blockers]] | ||
**Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. | **[[beta-blockers|Beta-adrenergic receptor antagonists]] (beta-blockers) and [[indacaterol]] and [[glycopyrrolate]] may interfere with the effect of each other when administered concurrently. | ||
**However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution. | **[[Beta-blockers]] not only block the therapeutic effects of [[beta-agonists]], but may produce severe [[bronchospasm]] in [[COPD]] patients. Therefore, patients with [[COPD]] should not normally be treated with [[beta-blockers]]. | ||
*Anticholinergics | **However, under certain circumstances, e.g., as [[prophylaxis]] after [[myocardial infarction]], there may be no acceptable alternatives to the use of [[beta-blockers]] in patients with [[COPD]]. In this setting, cardioselective [[beta-blockers]] could be considered, although they should be administered with caution. | ||
**There is potential for an additive interaction with concomitantly used anticholinergic medicines. Therefore, avoid coadministration of [[indacaterol]] and [[glycopyrrolate]] with other anticholinergic-containing drugs as this may lead to an increase in anticholinergic adverse effects. | *[[anticholinergic|Anticholinergics]] | ||
*Inhibitors of Cytochrome P450 3A4 and P-gp Efflux Transporter | **There is potential for an additive interaction with concomitantly used [[anticholinergic]] medicines. Therefore, avoid coadministration of [[indacaterol]] and [[glycopyrrolate]] with other [[anticholinergic]]-containing drugs as this may lead to an increase in [[anticholinergic]] adverse effects. | ||
**Drug interaction studies with indacaterol, a component of [[indacaterol]] and [[glycopyrrolate]], were carried out using potent and specific inhibitors of CYP3A4 and P-gp (i.e., ketoconazole, erythromycin, verapamil, and ritonavir). | *[[inhibitor|Inhibitors]] of [[Cytochrome P450 3A4]] and [[P-gp]] Efflux Transporter | ||
**The data suggest that systemic clearance of indacaterol is influenced by modulation of both P-gp and CYP3A4 activities and that the 2-fold area under the curve (AUC) increase caused by the strong dual inhibitor ketoconazole reflects the impact of maximal combined inhibition. | **Drug interaction studies with [[indacaterol]], a component of [[indacaterol]] and [[glycopyrrolate]], were carried out using potent and specific [[inhibitor|inhibitors]] of [[CYP3A4]] and [[P-gp]] (i.e., [[ketoconazole]], [[erythromycin]], [[verapamil]], and [[ritonavir]]). | ||
**Indacaterol was evaluated in clinical trials for up to 1 year at doses up to 600 mcg. Inhibition of the key contributors of indacaterol clearance, CYP3A4 and P-gp, has no impact on safety of therapeutic doses of indacaterol. Therefore, no dose adjustment is warranted at the recommended 27.5/15.6 mcg twice-daily dose for [[indacaterol]] and [[glycopyrrolate]] when administered concomitantly with inhibitors of CYP3A4 and P-gp. | **The data suggest that systemic clearance of [[indacaterol]] is influenced by modulation of both [[P-gp]] and [[CYP3A4]] activities and that the 2-fold area under the curve ([[AUC]]) increase caused by the strong dual inhibitor [[ketoconazole]] reflects the impact of maximal combined inhibition. | ||
**[[Indacaterol]] was evaluated in clinical trials for up to 1 year at doses up to 600 mcg. Inhibition of the key contributors of [[indacaterol]] clearance, [[CYP3A4]] and [[P-gp]], has no impact on safety of therapeutic doses of [[indacaterol]]. Therefore, no dose adjustment is warranted at the recommended 27.5/15.6 mcg twice-daily dose for [[indacaterol]] and [[glycopyrrolate]] when administered concomitantly with inhibitors of [[CYP3A4]] and [[P-gp]]. | |||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA='''Teratogenic Effects - Pregnancy Category C''' | |useInPregnancyFDA= | ||
There are no adequate and well-controlled studies with [[indacaterol]] and [[glycopyrrolate]] or its individual components, indacaterol and glycopyrrolate, in pregnant women. Animal reproduction studies were conducted with individual components, indacaterol and glycopyrrolate. Because animal reproduction studies are not always predictive of human response, [[indacaterol]] and [[glycopyrrolate]] should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking [[indacaterol]] and [[glycopyrrolate]]. | |||
'''[[Teratogenic]] Effects - Pregnancy Category C''' | |||
There are no adequate and well-controlled studies with [[indacaterol]] and [[glycopyrrolate]] or its individual components, [[indacaterol]] and [[glycopyrrolate]], in pregnant women. Animal reproduction studies were conducted with individual components, [[indacaterol]] and [[glycopyrrolate]]. Because animal reproduction studies are not always predictive of human response, [[indacaterol]] and [[glycopyrrolate]] should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking [[indacaterol]] and [[glycopyrrolate]]. | |||
''Indacaterol'': Indacaterol was not teratogenic in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1 mg/kg/day in rats and rabbits). | ''[[Indacaterol]]'': [[Indacaterol]] was not [[teratogenic]] in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an [[AUC]] basis at maternal [[subcutaneous]] doses up to 1 mg/kg/day in rats and rabbits). | ||
''Glycopyrrolate'': Glycopyrrolate was not teratogenic in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an AUC basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits). | ''[[Glycopyrrolate]]'': [[Glycopyrrolate]] was not [[teratogenic]] in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an AUC basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits). | ||
Teratogenic Effects: Pregnancy Category C | [[Teratogenic]] Effects: Pregnancy Category C | ||
There are no adequate and well-controlled studies with [[indacaterol]] and [[glycopyrrolate]] or its individual components, indacaterol and glycopyrrolate, in pregnant women. Animal reproduction studies were conducted with individual components, indacaterol and glycopyrrolate. Because animal reproduction studies are not always predictive of human response, [[indacaterol]] and [[glycopyrrolate]] should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking [[indacaterol]] and [[glycopyrrolate]]. | There are no adequate and well-controlled studies with [[indacaterol]] and [[glycopyrrolate]] or its individual components, [[indacaterol]] and [[glycopyrrolate]], in pregnant women. Animal reproduction studies were conducted with individual components, [[indacaterol]] and [[glycopyrrolate]]. Because animal reproduction studies are not always predictive of human response, [[indacaterol]] and [[glycopyrrolate]] should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking [[indacaterol]] and [[glycopyrrolate]]. | ||
Indacaterol: Indacaterol was not teratogenic in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1 mg/kg/day in rats and rabbits). | [[Indacaterol]]: [[Indacaterol]] was not [[teratogenic]] in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an [[AUC]] basis at maternal [[subcutaneous]] doses up to 1 mg/kg/day in rats and rabbits). | ||
Glycopyrrolate: Glycopyrrolate was not teratogenic in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an AUC basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits). | [[Glycopyrrolate]]: [[Glycopyrrolate]] was not [[teratogenic]] in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an [[AUC]] basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits). | ||
'''Non-teratogenic Effects:''' | '''Non-[[teratogenic]] Effects:''' | ||
''Indacaterol'': There were no effects on perinatal and postnatal developments in rats at approximately 110 times the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 0.3 mg/kg/day). | ''[[Indacaterol]]'': There were no effects on perinatal and postnatal developments in rats at approximately 110 times the MRHD in adults (on an [[AUC]] basis at maternal [[subcutaneous]] doses up to 0.3 mg/kg/day). | ||
''Glycopyrrolate'': There were no effects on perinatal and postnatal developments in rats at approximately 1100 times the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1.88 mg/kg/day) | ''[[Glycopyrrolate]]'': There were no effects on perinatal and postnatal developments in rats at approximately 1100 times the MRHD in adults (on an [[AUC]] basis at maternal [[subcutaneous]] doses up to 1.88 mg/kg/day). | ||
In human parturients undergoing Caesarean section, 86 minutes after a single intramuscular injection of 0.006 mg/kg glycopyrrolate, umbilical plasma concentrations were low. | |useInLaborDelivery=There are no adequate and well-controlled human trials that have investigated the effects of [[indacaterol]] and [[glycopyrrolate]] during labor and delivery. Because [[beta-agonists]] may potentially interfere with uterine contractility, [[indacaterol]] and [[glycopyrrolate]] should be used during labor only if the potential benefit justifies the potential risk. | ||
In human parturients undergoing [[Caesarean section]], 86 minutes after a single intramuscular injection of 0.006 mg/kg [[glycopyrrolate]], umbilical plasma concentrations were low. | |||
|useInNursing=''[[Indacaterol]] and [[Glycopyrrolate]]'': It is not known whether [[indacaterol]] and [[glycopyrrolate]] is excreted in human breast milk. Because many drugs are excreted in human milk, caution should be exercised when [[indacaterol]] and [[glycopyrrolate]] is administered to a nursing woman. Since there are no data from well-controlled human studies on the use of [[indacaterol]] and [[glycopyrrolate]] by nursing mothers, based on the data for the individual components, a decision should be made whether to discontinue nursing or to discontinue [[indacaterol]] and [[glycopyrrolate]], taking into account the importance of [[indacaterol]] and [[glycopyrrolate]] to the mother. | |useInNursing=''[[Indacaterol]] and [[Glycopyrrolate]]'': It is not known whether [[indacaterol]] and [[glycopyrrolate]] is excreted in human breast milk. Because many drugs are excreted in human milk, caution should be exercised when [[indacaterol]] and [[glycopyrrolate]] is administered to a nursing woman. Since there are no data from well-controlled human studies on the use of [[indacaterol]] and [[glycopyrrolate]] by nursing mothers, based on the data for the individual components, a decision should be made whether to discontinue nursing or to discontinue [[indacaterol]] and [[glycopyrrolate]], taking into account the importance of [[indacaterol]] and [[glycopyrrolate]] to the mother. | ||
''Indacaterol'': It is not known whether indacaterol is excreted in human breast milk. Indacaterol (including its metabolites) have been detected in the milk of lactating rats. | ''[[Indacaterol]]'': It is not known whether [[indacaterol]] is excreted in human breast milk. [[Indacaterol]] (including its [[metabolites]]) have been detected in the milk of lactating rats. | ||
''Glycopyrrolate'': It is not known whether glycopyrrolate is excreted in human breast milk. Glycopyrrolate (including its metabolites) have been detected in the milk of lactating rats and reached up to 10-fold higher concentrations in the milk than in the blood of the dam. | ''[[Glycopyrrolate]]'': It is not known whether [[glycopyrrolate]] is excreted in human breast milk. [[Glycopyrrolate]] (including its [[metabolites]]) have been detected in the milk of lactating rats and reached up to 10-fold higher concentrations in the milk than in the blood of the dam. | ||
|useInPed=[[Indacaterol]] and [[glycopyrrolate]] is not indicated for use in children. The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] in pediatric patients have not been established. | |useInPed=[[Indacaterol]] and [[glycopyrrolate]] is not indicated for use in children. The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] in pediatric patients have not been established. | ||
|useInGeri=Based on available data, no adjustment of [[indacaterol]] and [[glycopyrrolate]] dosage in geriatric patients is warranted. [[Indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in elderly patients 75 years of age and older. | |useInGeri=Based on available data, no adjustment of [[indacaterol]] and [[glycopyrrolate]] dosage in geriatric patients is warranted. [[Indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in elderly patients 75 years of age and older. | ||
Of the total number of subjects in clinical studies of [[indacaterol]] and [[glycopyrrolate]], 45% were aged 65 and older, while 11% were aged 75 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | Of the total number of subjects in clinical studies of [[indacaterol]] and [[glycopyrrolate]], 45% were aged 65 and older, while 11% were aged 75 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | ||
|useInRenalImpair=Based on the pharmacokinetic characteristics of its monotherapy components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild to moderate renal impairment. In patients with severe renal impairment (estimated GFR less than 30 mL/min/1.73 m2) or end-stage renal disease requiring dialysis, [[indacaterol]] and [[glycopyrrolate]] should be used if the expected benefit outweighs the potential risk since the systemic exposure to glycopyrrolate may be increased in this population. | |useInRenalImpair=Based on the pharmacokinetic characteristics of its [[monotherapy]] components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild to moderate [[renal impairment]]. In patients with severe [[renal impairment]] (estimated [[GFR]] less than 30 mL/min/1.73 m2) or [[end-stage renal disease]] requiring [[dialysis]], [[indacaterol]] and [[glycopyrrolate]] should be used if the expected benefit outweighs the potential risk since the systemic exposure to [[glycopyrrolate]] may be increased in this population. | ||
|useInHepaticImpair=Based on the pharmacokinetic characteristics of its monotherapy components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild to moderate hepatic impairment. Studies in subjects with severe hepatic impairment have not been performed. | |useInHepaticImpair=Based on the pharmacokinetic characteristics of its [[monotherapy]] components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild to moderate hepatic impairment. Studies in subjects with severe hepatic impairment have not been performed. | ||
|administration=Indacaterold and glycopyrrolate is for oral inhalation only. Do not swallow [[Indacaterol]] and [[glycopyrrolate]] capsules, as the intended effects on the lungs will not be obtained. [[Indacaterol]] and [[glycopyrrolate]] capsules should only be used with the NEOHALER device. [[Indacaterol]] and [[glycopyrrolate]] should be administered at the same time of the day (1 capsule in the morning and 1 capsule in the evening) every day. More frequent administration or a greater number of inhalations (more than 1 capsule twice-daily) of [[indacaterol]] and [[glycopyrrolate]] is not recommended. Store [[indacaterol]] and [[glycopyrrolate]] capsules in the blister, and only remove IMMEDIATELY BEFORE USE with the NEOHALER device. | |administration=[[Indacaterold]] and [[glycopyrrolate]] is for oral inhalation only. Do not swallow [[Indacaterol]] and [[glycopyrrolate]] capsules, as the intended effects on the lungs will not be obtained. [[Indacaterol]] and [[glycopyrrolate]] capsules should only be used with the NEOHALER device. [[Indacaterol]] and [[glycopyrrolate]] should be administered at the same time of the day (1 capsule in the morning and 1 capsule in the evening) every day. More frequent administration or a greater number of inhalations (more than 1 capsule twice-daily) of [[indacaterol]] and [[glycopyrrolate]] is not recommended. Store [[indacaterol]] and [[glycopyrrolate]] capsules in the blister, and only remove IMMEDIATELY BEFORE USE with the NEOHALER device. | ||
|overdose=In COPD patients, doses of up to 600/124.8 mcg [[indacaterol]] and [[glycopyrrolate]] were inhaled over 2 weeks and there were no relevant effects on heart rate, QTc interval, blood glucose or serum potassium. There was an increase in ventricular ectopies after 14 days of dosing with 300/124.8 mcg and 600/124.8 mcg [[indacaterol]] and [[glycopyrrolate]], but low prevalence and small patient numbers (N=49 and N=51 for 600/124.8 mcg and 300/124.8 mcg [[indacaterol]] and [[glycopyrrolate]], respectively) precluded accurate analysis. In a total of four patients, non-sustained ventricular tachycardia was recorded, with the longest episode recorded being 9 beats (4 seconds). | |overdose=In [[COPD]] patients, doses of up to 600/124.8 mcg [[indacaterol]] and [[glycopyrrolate]] were inhaled over 2 weeks and there were no relevant effects on heart rate, [[QTc interval]], [[blood glucose]] or serum [[potassium]]. There was an increase in ventricular ectopies after 14 days of dosing with 300/124.8 mcg and 600/124.8 mcg [[indacaterol]] and [[glycopyrrolate]], but low prevalence and small patient numbers (N=49 and N=51 for 600/124.8 mcg and 300/124.8 mcg [[indacaterol]] and [[glycopyrrolate]], respectively) precluded accurate analysis. In a total of four patients, non-sustained [[ventricular tachycardia]] was recorded, with the longest episode recorded being 9 beats (4 seconds). | ||
In healthy volunteers, single dose administration of [[indacaterol]] and [[glycopyrrolate]] at up to a dose of 440/499.2 mcg indacaterol/glycopyrrolate was well-tolerated without clinically significant effects on the ECG, serum potassium or blood glucose. | In healthy volunteers, single dose administration of [[indacaterol]] and [[glycopyrrolate]] at up to a dose of 440/499.2 mcg [[indacaterol]]/[[glycopyrrolate]] was well-tolerated without clinically significant effects on the [[ECG]], serum [[potassium]] or [[blood glucose]]. | ||
[[Indacaterol]] and [[glycopyrrolate]] contains both indacaterol and glycopyrrolate; therefore, the risks associated with overdosage for the individual components described below apply to [[indacaterol]] and [[glycopyrrolate]]. Treatment of overdosage consists of discontinuation of [[indacaterol]] and [[glycopyrrolate]] together with institution of appropriate symptomatic and/or supportive therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medicine can produce bronchospasm. Cardiac monitoring is recommended in cases of overdosage. | [[Indacaterol]] and [[glycopyrrolate]] contains both [[indacaterol]] and [[glycopyrrolate]]; therefore, the risks associated with overdosage for the individual components described below apply to [[indacaterol]] and [[glycopyrrolate]]. Treatment of overdosage consists of discontinuation of [[indacaterol]] and [[glycopyrrolate]] together with institution of appropriate symptomatic and/or supportive therapy. The judicious use of a cardioselective [[beta-receptor blocker]] may be considered, bearing in mind that such medicine can produce [[bronchospasm]]. Cardiac monitoring is recommended in cases of overdosage. | ||
''Indacaterol'': The potential signs and symptoms associated with overdosage of indacaterol are those of excessive beta-adrenergic stimulation and occurrence or exaggeration of any of the signs and symptoms, e.g., angina, hypertension or hypotension, tachycardia, with rates up to 200 bpm, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, muscle cramps, nausea, vomiting, drowsiness, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, metabolic acidosis and insomnia. As with all inhaled sympathomimetic medications, cardiac arrest and even death may be associated with an overdose of indacaterol. | ''[[Indacaterol]]'': The potential signs and symptoms associated with overdosage of [[indacaterol]] are those of excessive [[beta-adrenergic]] stimulation and occurrence or exaggeration of any of the signs and symptoms, e.g., [[angina]], [[hypertension]] or [[hypotension]], [[tachycardia]], with rates up to 200 bpm, [[arrhythmias]], [[nervousness]], [[headache]], [[tremor]], [[dry mouth]], [[palpitation]], [[muscle cramps]], [[nausea]], [[vomiting]], [[drowsiness]], [[dizziness]], [[fatigue]], [[malaise]], [[hypokalemia]], [[hyperglycemia]], [[metabolic acidosis]] and [[insomnia]]. As with all inhaled [[sympathomimetic]] medications, [[cardiac arrest]] and even death may be associated with an overdose of [[indacaterol]]. | ||
In COPD patients, single doses of indacaterol 3000 mcg were associated with moderate increases in pulse rate, systolic blood pressure and QTc interval. | In [[COPD]] patients, single doses of indacaterol 3000 mcg were associated with moderate increases in [[pulse rate]], [[systolic blood pressure]] and [[QTc interval]]. | ||
Glycopyrrolate: An overdose of glycopyrrolate may lead to anticholinergic signs and symptoms such as nausea, vomiting, dizziness, lightheadedness, blurred vision, increased intraocular pressure (causing pain, vision disturbances or reddening of the eye), obstipation or difficulties in voiding. | [[Glycopyrrolate]]: An overdose of [[glycopyrrolate]] may lead to [[anticholinergic]] signs and symptoms such as [[nausea]], [[vomiting]], [[dizziness]], [[lightheadedness]], [[blurred vision]], increased [[intraocular pressure]] (causing [[pain]], vision disturbances or reddening of the eye), [[obstipation]] or difficulties in voiding. | ||
In COPD patients, repeated orally inhaled administration of glycopyrrolate at total doses of 124.8 mcg and 249.6 mcg once-daily for 28 days were well tolerated. | In [[COPD]] patients, repeated orally inhaled administration of [[glycopyrrolate]] at total doses of 124.8 mcg and 249.6 mcg once-daily for 28 days were well tolerated. | ||
Peak plasma levels and total systemic exposure following intravenous administration of 150 mcg glycopyrrolate (equivalent to 120 mcg active moiety) in healthy volunteers were respectively about 270-fold and 13-fold higher than the peak and total systemic exposure at steady-state achieved with the recommended daily dose of 31.2 mcg of glycopyrrolate (i.e., 15.6 mcg glycopyrrolate twice-daily) and were well tolerated. | Peak plasma levels and total systemic exposure following [[intravenous]] administration of 150 mcg [[glycopyrrolate]] (equivalent to 120 mcg active moiety) in healthy volunteers were respectively about 270-fold and 13-fold higher than the peak and total systemic exposure at steady-state achieved with the recommended daily dose of 31.2 mcg of [[glycopyrrolate]] (i.e., 15.6 mcg [[glycopyrrolate]] twice-daily) and were well tolerated. | ||
|drugBox={{Drugbox2 | |drugBox={{Drugbox2 | ||
| verifiedrevid = | | verifiedrevid = | ||
| Line 190: | Line 196: | ||
<!--Chemical data--> | <!--Chemical data--> | ||
}} | }} | ||
|mechAction=[[Indacaterol]] and [[glycopyrrolate]] contains both indacaterol and glycopyrrolate. The mechanisms of action described below for the individual components apply to [[indacaterol]] and [[glycopyrrolate]]. These drugs represent 2 different classes of medications (a LABA and an anticholinergic) that have different and additive effects on clinical and physiological indices. | |mechAction=[[Indacaterol]] and [[glycopyrrolate]] contains both [[indacaterol]] and [[glycopyrrolate]]. The mechanisms of action described below for the individual components apply to [[indacaterol]] and [[glycopyrrolate]]. These drugs represent 2 different classes of medications (a [[LABA]] and an [[anticholinergic]]) that have different and additive effects on clinical and physiological indices. | ||
''Indacaterol'': Indacaterol is a long-acting beta2-adrenergic agonist (LABA). When inhaled, indacaterol acts locally in the lung as a bronchodilator. Although beta2-receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta1-receptors are the predominant receptors in the heart, there are also beta2-adrenergic receptors in the human heart comprising 10% to 50% of the total adrenergic receptors. The precise function of these receptors is not known, but their presence raises the possibility that even highly selective beta2-adrenergic agonists may have cardiac effects. | ''[[Indacaterol]]'': [[Indacaterol]] is a [[LABA|long-acting beta2-adrenergic agonist]] (LABA). When inhaled, [[indacaterol]] acts locally in the lung as a [[bronchodilator]]. Although [[Beta-2 adrenergic receptor|beta2-receptors]] are the predominant [[adrenergic receptors]] in bronchial [[smooth muscle]] and [[Beta-1 adrenergic receptor|beta1-receptors]] are the predominant receptors in the heart, there are also [[Beta-2 adrenergic receptor|beta2-adrenergic receptors]] in the human heart comprising 10% to 50% of the total [[adrenergic receptors]]. The precise function of these receptors is not known, but their presence raises the possibility that even highly selective [[Beta2-adrenergic receptor agonist|beta2-adrenergic agonists]] may have cardiac effects. | ||
The pharmacological effects of beta2-adrenoceptor agonist drugs, including indacaterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3’, 5’-adenosine monophosphate (cyclic monophosphate). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells. In vitro studies have shown that indacaterol has more than 24-fold greater agonist activity at beta2-receptors compared to beta1-receptors and 20-fold greater agonist activity compared to beta3-receptors. The clinical significance of these findings is unknown. | The pharmacological effects of beta2-adrenoceptor agonist drugs, including [[indacaterol]], are at least in part attributable to stimulation of intracellular adenyl cyclase, the [[enzyme]] that catalyzes the conversion of [[adenosine triphosphate]] (ATP) to cyclic-3’, 5’-[[adenosine monophosphate]] (cyclic monophosphate). Increased [[cyclic AMP]] levels cause relaxation of bronchial [[smooth muscle]] and inhibition of release of mediators of immediate [[hypersensitivity]] from cells, especially from [[mast cells]]. In vitro studies have shown that [[indacaterol]] has more than 24-fold greater agonist activity at [[Beta-2 adrenergic receptor|beta2-receptors]] compared to [[Beta-1 adrenergic receptor|beta1-receptors]] and 20-fold greater agonist activity compared to [[Beta-3 adrenergic receptor|beta3-receptors]]. The clinical significance of these findings is unknown. | ||
''Glycopyrrolate'': Glycopyrrolate is a long-acting muscarinic antagonist, which is often referred to as an anticholinergic. It has similar affinity to the subtypes of muscarinic receptors M1 to M5. In the airways, it exhibits pharmacological effects through inhibition of M3 receptor at the smooth muscle leading to bronchodilation. The competitive and reversible nature of antagonism was shown with human and animal origin receptors and isolated organ preparations. In preclinical in vitro as well as in vivo studies, prevention of methacholine-induced broncho-constrictive effects was dose-dependent and lasted longer than 24 hours. The clinical relevance of these findings is unknown. The bronchodilation following inhalation of glycopyrrolate is predominantly a site-specific effect. | ''[[Glycopyrrolate]]'': [[Glycopyrrolate]] is a long-acting [[muscarinic antagonist]], which is often referred to as an [[anticholinergic]]. It has similar affinity to the subtypes of [[Muscarinic acetylcholine receptor|muscarinic receptors]] [[Muscarinic acetylcholine receptor M1|M1]] to [[Muscarinic acetylcholine receptor M5|M5]]. In the airways, it exhibits pharmacological effects through inhibition of [[M3 receptor]] at the [[smooth muscle]] leading to [[bronchodilation]]. The competitive and reversible nature of antagonism was shown with human and animal origin receptors and isolated organ preparations. In preclinical in vitro as well as in vivo studies, prevention of [[methacholine]]-induced broncho-constrictive effects was dose-dependent and lasted longer than 24 hours. The clinical relevance of these findings is unknown. The [[bronchodilation]] following inhalation of [[glycopyrrolate]] is predominantly a site-specific effect. | ||
|structure=Indacaterol maleate is a selective beta2-adrenergic agonist. Its chemical name is (R)-5-[2-(5,6-Diethylindan-2-ylamino)-1-hydroxyethyl]-8-hydroxy-1H-quinolin-2-one maleate; its structural formula is: | |structure=[[Indacaterol]] maleate is a selective [[beta2-adrenergic agonist]]. Its chemical name is (R)-5-[2-(5,6-Diethylindan-2-ylamino)-1-hydroxyethyl]-8-hydroxy-1H-quinolin-2-one maleate; its structural formula is: | ||
[[File:Indacaterol structure | [[File:Indacaterol structure.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
Indacaterol maleate has a molecular weight of 508.56, and its empirical formula is C24H28N2O3 • C4H4O4. Indacaterol maleate is a white to very slightly grayish or very slightly yellowish powder. Indacaterol maleate is slightly soluble in ethanol and very slightly soluble in water. | [[Indacaterol]] maleate has a molecular weight of 508.56, and its empirical formula is C24H28N2O3 • C4H4O4. [[Indacaterol]] maleate is a white to very slightly grayish or very slightly yellowish powder. [[Indacaterol]] maleate is slightly soluble in [[ethanol]] and very slightly soluble in water. | ||
Glycopyrrolate is chemically described as (3RS)-3-[(2SR)-(2-cyclopentyl-2-hydroxy-2-phenylacetyl) oxy]-1,1-dimethylpyrrolidinium bromide. This synthetic quaternary ammonium compound acts as a competitive antagonist at muscarinic acetylcholine receptors, also referred to as anticholinergic. Glycopyrrolate, C19H28BrNO3, is a white powder that is freely soluble in water and sparingly soluble in absolute ethanol. It has a molecular mass of 398.33. The structural formula is: | [[Glycopyrrolate]] is chemically described as (3RS)-3-[(2SR)-(2-cyclopentyl-2-hydroxy-2-phenylacetyl) oxy]-1,1-dimethylpyrrolidinium bromide. This synthetic quaternary ammonium compound acts as a competitive antagonist at [[muscarinic acetylcholine receptors]], also referred to as [[anticholinergic]]. [[Glycopyrrolate]], C19H28BrNO3, is a white powder that is freely soluble in water and sparingly soluble in absolute [[ethanol]]. It has a molecular mass of 398.33. The structural formula is: | ||
[[File:Glycopyrrolate structure.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Glycopyrrolate structure.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
|PD='''Cardiac Electrophysiology''' | |PD='''Cardiac Electrophysiology''' | ||
The QTc interval was studied in TQT studies with [[indacaterol]] and [[glycopyrrolate]] and with each of the monotherapy components. The TQT studies with indacaterol and glycopyrrolate demonstrated that neither of the compounds had a relevant effect on the corrected QT interval at supratherapeutic and therapeutic doses (for glycopyrrolate only a supratherapeutic dose was tested). | The [[QTc interval]] was studied in TQT studies with [[indacaterol]] and [[glycopyrrolate]] and with each of the [[monotherapy]] components. The TQT studies with [[indacaterol]] and [[glycopyrrolate]] demonstrated that neither of the compounds had a relevant effect on the corrected [[QT interval]] at supratherapeutic and therapeutic doses (for [[glycopyrrolate]] only a supratherapeutic dose was tested). | ||
In a randomized, partially-blinded, placebo- and positive-controlled, crossover TQT study in 84 healthy subjects a supratherapeutic dose of [[indacaterol]] and [[glycopyrrolate]] (indacaterol/glycopyrrolate 440/499.2 mcg) was administered. This is a 16/32 dose multiple compared to a single dose of the recommended 27.5/15.6 mcg twice-daily dosage of [[indacaterol]] and [[glycopyrrolate]] which resulted in exposure multiples for mean Cmax of 9.3 for indacaterol and 35.2 for glycopyrrolate compared to steady-state pharmacokinetics of [[indacaterol]] and [[glycopyrrolate]] 27.5/15.6 mcg twice-daily. The mean maximal change from baseline in QTcI compared to placebo was 8.70 msec (2-sided 90% CI 7.3, 10.1) at 30 minutes after dosing. Although a marginal QT effect of [[indacaterol]] and [[glycopyrrolate]] was observed at the supratherapeutirapeutic exposure. | In a randomized, partially-blinded, placebo- and positive-controlled, crossover TQT study in 84 healthy subjects a supratherapeutic dose of [[indacaterol]] and [[glycopyrrolate]] ([[indacaterol]]/[[glycopyrrolate]] 440/499.2 mcg) was administered. This is a 16/32 dose multiple compared to a single dose of the recommended 27.5/15.6 mcg twice-daily dosage of [[indacaterol]] and [[glycopyrrolate]] which resulted in exposure multiples for mean [[Cmax]] of 9.3 for [[indacaterol]] and 35.2 for [[glycopyrrolate]] compared to steady-state pharmacokinetics of [[indacaterol]] and [[glycopyrrolate]] 27.5/15.6 mcg twice-daily. The mean maximal change from baseline in QTcI compared to placebo was 8.70 msec (2-sided 90% CI 7.3, 10.1) at 30 minutes after dosing. Although a marginal [[QT]] effect of [[indacaterol]] and [[glycopyrrolate]] was observed at the supratherapeutirapeutic exposure. | ||
|PK='''Absorption''' | |PK='''Absorption''' | ||
Following inhalation of [[indacaterol]] and [[glycopyrrolate]], the median time to reach peak plasma concentrations of indacaterol and glycopyrrolate was achieved rapidly at approximately 15 minutes and 5 minutes, respectively. | Following inhalation of [[indacaterol]] and [[glycopyrrolate]], the median time to reach peak plasma concentrations of [[indacaterol]] and [[glycopyrrolate]] was achieved rapidly at approximately 15 minutes and 5 minutes, respectively. | ||
The steady-state systemic exposure ( | The steady-state systemic exposure ([[AUC]]0-12h,ss; [[Cmax]],ss) to [[indacaterol]] and [[glycopyrrolate]] is similar after the twice-daily inhalation of 2 (times 2) capsules of [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg as compared to the twice-daily inhalation of the [[monotherapy]] products [[indacaterol]] 27.5 mcg (times 2) alone or [[glycopyrrolate]] 15.6 mcg (times 2) alone respectively. | ||
Indacaterol: Absolute bioavailability of indacaterol after an inhalation dose was on average 43% to 45%. Systemic exposure results from a composite of pulmonary and intestine absorption. Indacaterol serum concentrations increased with repeated once-daily administration. Steady-state was achieved within 12 to 15 days. The mean accumulation ratio of indacaterol, i.e., AUC over the 24-hour dosing interval on Day 14 or Day 15 compared to Day 1, was in the range of 2.9 to 3.8 for once-daily inhaled doses between 75 mcg and 600 mcg. | [[Indacaterol]]: Absolute bioavailability of [[indacaterol]] after an inhalation dose was on average 43% to 45%. Systemic exposure results from a composite of pulmonary and intestine absorption. [[Indacaterol]] serum concentrations increased with repeated once-daily administration. Steady-state was achieved within 12 to 15 days. The mean accumulation ratio of [[indacaterol]], i.e., AUC over the 24-hour dosing interval on Day 14 or Day 15 compared to Day 1, was in the range of 2.9 to 3.8 for once-daily inhaled doses between 75 mcg and 600 mcg. | ||
Glycopyrrolate: Following repeated once-daily inhalation in patients with COPD, pharmacokinetic steady-state of glycopyrrolate was reached within 1 week of treatment. There was no indication that the glycopyrrolate pharmacokinetics changes over time. With once-daily doses of 124.8 mcg and 249.6 mcg, steady-state exposure to glycopyrrolate (AUC over the dosing interval) was about 1.4- to 1.7-fold higher than after the first dose. | [[Glycopyrrolate]]: Following repeated once-daily inhalation in patients with [[COPD]], pharmacokinetic steady-state of [[glycopyrrolate]] was reached within 1 week of treatment. There was no indication that the [[glycopyrrolate]] pharmacokinetics changes over time. With once-daily doses of 124.8 mcg and 249.6 mcg, steady-state exposure to [[glycopyrrolate]] ([[AUC]] over the dosing interval) was about 1.4- to 1.7-fold higher than after the first dose. | ||
'''Distribution''' | '''Distribution''' | ||
''Indacaterol'': After intravenous infusion, the volume of distribution (Vz) of indacaterol was 2,361 to 2,557 L, indicating an extensive distribution. The in vitro human serum and plasma protein binding was 94.1% to 95.3% and 95.1% to 96.2%, respectively. | ''[[Indacaterol]]'': After [[intravenous]] [[infusion]], the volume of distribution (Vz) of [[indacaterol]] was 2,361 to 2,557 L, indicating an extensive distribution. The in vitro human serum and [[plasma protein]] binding was 94.1% to 95.3% and 95.1% to 96.2%, respectively. | ||
''Glycopyrrolate'': After intravenous administration, the steady-state volume of distribution (Vss) of glycopyrrolate was 83 L and the volume of distribution in the terminal phase (Vz) was 376 L. The in vitro human plasma protein binding of glycopyrrolate was 38% to 41% at concentrations of 1 to 10 ng/mL. | ''[[Glycopyrrolate]]'': After [[intravenous]] administration, the steady-state volume of distribution (Vss) of [[glycopyrrolate]] was 83 L and the volume of distribution in the terminal phase (Vz) was 376 L. The in vitro human [[plasma protein]] binding of [[glycopyrrolate]] was 38% to 41% at concentrations of 1 to 10 ng/mL. | ||
'''[[Metabolism]]''' | '''[[Metabolism]]''' | ||
''Indacaterol'': In vitro investigations indicated that UGT1A1 is the only UGT isoform that metabolized indacaterol to the phenolic O-glucuronide. The oxidative metabolites were found in incubations with recombinant CYP1A1, CYP2D6, and CYP3A4. CYP3A4 is concluded to be the predominant isoenzyme responsible for hydroxylation of indacaterol. In vitro investigations further indicated that indacaterol is a low affinity substrate for the efflux pump P-gp. | ''[[Indacaterol]]'': In vitro investigations indicated that [[UGT1A1]] is the only UGT isoform that metabolized [[indacaterol]] to the phenolic O-[[glucuronide]]. The oxidative [[metabolites]] were found in incubations with recombinant [[CYP1A1]], [[CYP2D6]], and [[CYP3A4]]. [[CYP3A4]] is concluded to be the predominant isoenzyme responsible for hydroxylation of [[indacaterol]]. In vitro investigations further indicated that [[indacaterol]] is a low affinity substrate for the efflux pump [[P-gp]]. | ||
After oral administration of radiolabelled indacaterol in a human ADME (absorption, distribution, metabolism, excretion) study, unchanged indacaterol was the main component in serum, accounting for about one-third of total drug-related AUC over 24 hours. A hydroxylated derivative was the most prominent metabolite in serum. Phenolic O-glucuronides of indacaterol and hydroxylated indacaterol were further prominent metabolites. A diastereomer of the hydroxylated derivative, a N-glucuronide of indacaterol, and C- and N-dealkylated products were further metabolites identified. | After oral administration of radiolabelled [[indacaterol]] in a human ADME (absorption, distribution, [[metabolism]], excretion) study, unchanged [[indacaterol]] was the main component in serum, accounting for about one-third of total drug-related [[AUC]] over 24 hours. A hydroxylated derivative was the most prominent [[metabolite]] in serum. Phenolic O-[[glucuronide|glucuronides]] of [[indacaterol]] and hydroxylated [[indacaterol]] were further prominent [[metabolites]]. A diastereomer of the hydroxylated derivative, a N-[[glucuronide]] of [[indacaterol]], and C- and N-dealkylated products were further [[metabolites]] identified. | ||
''Glycopyrrolate'': In vitro metabolism studies show glycopyrrolate hydroxylation resulting in a variety of mono- and bis-hydroxylated metabolites and direct hydrolysis resulting in the formation of a carboxylic acid derivative (M9). Further in vitro investigations showed that multiple CYP isoenzymes contribute to the oxidative biotransformation of glycopyrrolate and the hydrolysis to M9 is likely to be catalyzed by members from the cholinesterase family pre-systemically and/or via first pass metabolism from the swallowed dose fraction of orally inhaled glycopyrrolate. Glucuronide and/or sulfate conjugates of glycopyrrolate were found in urine of humans after repeated inhalation, accounting for about 3% of the dose. | ''[[Glycopyrrolate]]'': In vitro metabolism studies show [[glycopyrrolate]] hydroxylation resulting in a variety of mono- and bis-hydroxylated [[metabolites]] and direct [[hydrolysis]] resulting in the formation of a carboxylic acid derivative (M9). Further in vitro investigations showed that multiple [[CYP]] isoenzymes contribute to the oxidative biotransformation of [[glycopyrrolate]] and the hydrolysis to M9 is likely to be catalyzed by members from the [[cholinesterase]] family pre-systemically and/or via first pass [[metabolism]] from the swallowed dose fraction of orally inhaled [[glycopyrrolate]]. [[Glucuronide]] and/or sulfate conjugates of [[glycopyrrolate]] were found in [[urine]] of humans after repeated inhalation, accounting for about 3% of the dose. | ||
'''Elimination''': | '''Elimination''': | ||
''Indacaterol'': In clinical studies which included urine collection, the amount of indacaterol excreted unchanged via urine was generally lower than 2% of the dose. Renal clearance of indacaterol was, on average, between 0.46 L/h and 1.20 L/h. When compared with the serum clearance of indacaterol of 18.8 L/h to 23.3 L/h, it is evident that renal clearance plays a minor role (about 2% to 6% of systemic clearance) in the elimination of systemically available indacaterol. | ''[[Indacaterol]]'': In clinical studies which included [[urine]] collection, the amount of [[indacaterol]] excreted unchanged via [[urine]] was generally lower than 2% of the dose. [[Renal clearance]] of [[indacaterol]] was, on average, between 0.46 L/h and 1.20 L/h. When compared with the serum clearance of [[indacaterol]] of 18.8 L/h to 23.3 L/h, it is evident that [[renal clearance]] plays a minor role (about 2% to 6% of systemic clearance) in the elimination of systemically available [[indacaterol]]. | ||
In a human ADME study where indacaterol was given orally, the fecal route of excretion was dominant over the urinary route. Indacaterol was excreted into human feces primarily as unchanged parent drug (54% of the dose) and, to a lesser extent, hydroxylated indacaterol metabolites (23% of the dose). Mass balance was complete with greater than or equal to 90% of the dose recovered in the excreta. | In a human ADME study where [[indacaterol]] was given orally, the fecal route of excretion was dominant over the urinary route. [[Indacaterol]] was excreted into human feces primarily as unchanged parent drug (54% of the dose) and, to a lesser extent, hydroxylated [[indacaterol]] [[metabolites]] (23% of the dose). Mass balance was complete with greater than or equal to 90% of the dose recovered in the excreta. | ||
Indacaterol serum concentrations declined in a multi-phasic manner with an average terminal half-life ranging from 45.5 to 126 hours. The effective half-life, calculated from the accumulation of indacaterol after repeated dosing ranged from 40 to 56 hours which is consistent with the observed time to steady-state of approximately 12 to 15 days. | [[Indacaterol]] serum concentrations declined in a multi-phasic manner with an average terminal half-life ranging from 45.5 to 126 hours. The effective half-life, calculated from the accumulation of indacaterol after repeated dosing ranged from 40 to 56 hours which is consistent with the observed time to steady-state of approximately 12 to 15 days. | ||
''Glycopyrrolate'': Renal elimination of parent drug accounts for about 60% to 70% of total clearance of systemically available glycopyrrolate whereas non-renal clearance processes account for about 30% to 40%. Biliary clearance contributes to the non-renal clearance, but the majority of non-renal clearance is thought to be due to metabolism. | ''[[Glycopyrrolate]]'': Renal elimination of parent drug accounts for about 60% to 70% of total clearance of systemically available [[glycopyrrolate]] whereas non-renal clearance processes account for about 30% to 40%. Biliary clearance contributes to the non-[[renal clearance]], but the majority of non-[[renal clearance]] is thought to be due to [[metabolism]]. | ||
Following inhalation of single and repeated once-daily doses between 62.4 mcg and 249.6 mcg glycopyrrolate by healthy volunteers and patients with COPD, mean renal clearance of glycopyrrolate was in the range of 17.4 L/h and 24.4 L/h. Active tubular secretion contributes to the renal elimination of glycopyrrolate. | Following inhalation of single and repeated once-daily doses between 62.4 mcg and 249.6 mcg [[glycopyrrolate]] by healthy volunteers and patients with [[COPD]], mean [[renal clearance]] of [[glycopyrrolate]] was in the range of 17.4 L/h and 24.4 L/h. Active tubular secretion contributes to the renal elimination of [[glycopyrrolate]]. | ||
Glycopyrrolate plasma concentrations declined in a multi-phasic manner. The mean terminal elimination half-life of glycopyrrolate was much longer after inhalation (33 to 53 hours) than after intravenous (6.2 hours) and oral (2.8 hours) administration. | [[Glycopyrrolate]] plasma concentrations declined in a multi-phasic manner. The mean terminal elimination half-life of [[glycopyrrolate]] was much longer after inhalation (33 to 53 hours) than after [[intravenous]] (6.2 hours) and oral (2.8 hours) administration. | ||
'''Drug Interactions''': | '''Drug Interactions''': | ||
There is no pharmacokinetic drug-drug interaction resulting from the concomitant administration of inhaled | There is no pharmacokinetic drug-drug interaction resulting from the concomitant administration of inhaled [[glycopyrrolate]] and inhaled [[indacaterol]] based on steady-state exposure data. | ||
No specific drug-drug interaction studies were conducted with [[indacaterol]] and [[glycopyrrolate]]. Information on the potential for interactions for [[indacaterol]] and [[glycopyrrolate]] is based on the potential for each of its 2 [[monotherapy]] components. | |||
'' | ''Effect of co-administered drugs on [[indacaterol]] and [[glycopyrrolate]] exposure'': | ||
''[[Indacaterol]]'': | |||
Inhibitors of [[Cytochrome P450 3A4]] and [[P-gp]] Efflux Transporter: Drug interaction studies were carried out using potent and specific inhibitors of [[CYP3A4]] and [[P-gp]] (i.e., [[ketoconazole]], [[erythromycin]], [[verapamil]] and [[ritonavir]]). Coadministration of [[indacaterol]] 300 mcg (single dose) with [[verapamil]] (80 mg 3 times a day for 4 days) showed 2-fold increase in [[indacaterol]] [[AUC]]0-24h, and 1.5-fold increase in [[indacaterol]] [[Cmax]]. Coadministration of [[indacaterol]] inhalation powder 300 mcg (single dose) with [[erythromycin]] (400 mg 4 times a day for 7 days) showed a 1.4-fold increase in [[indacaterol]] [[AUC]]0-24h, and 1.2-fold increase in [[indacaterol]] [[Cmax]]. Coadministration of [[indacaterol]] inhalation powder 300 mcg (single dose) with [[ketoconazole]] (200 mg twice-daily for 7 days) caused a 1.9-fold increase in [[indacaterol]] [[AUC]]0-24h, and 1.3-fold increase in [[indacaterol]] [[Cmax]]. Coadministration of [[indacaterol]] 300 mcg (single dose) with [[ritonavir]] (300 mg twice-daily for 7.5 days) resulted in a 1.7-fold increase in [[indacaterol]] [[AUC]]0-24h whereas [[indacaterol]] [[Cmax]] was unaffected. | |||
Cimetidine or Other Inhibitors of Organic Cationic Transport: In a clinical study in healthy volunteers, cimetidine, an inhibitor of organic cation transport which is thought to contribute to the renal excretion of glycopyrrolate, increased total exposure (AUC) to glycopyrrolate by 22% and decreased renal clearance by 23%. | ''[[Glycopyrrolate]]'': [[Cimetidine]] or Other Inhibitors of Organic Cationic Transport: In a clinical study in healthy volunteers, [[cimetidine]], an inhibitor of organic cation transport which is thought to contribute to the renal excretion of [[glycopyrrolate]], increased total exposure ([[AUC]]) to [[glycopyrrolate]] by 22% and decreased [[renal clearance]] by 23%. | ||
''Effect of [[indacaterol]] and [[glycopyrrolate]] on co-administered drugs exposure'': | ''Effect of [[indacaterol]] and [[glycopyrrolate]] on co-administered drugs exposure'': | ||
In vitro studies show that [[indacaterol]] and [[glycopyrrolate]] is not likely to inhibit or induce the metabolism of other drugs, nor processes involving drug transporters. | In vitro studies show that [[indacaterol]] and [[glycopyrrolate]] is not likely to inhibit or induce the [[metabolism]] of other drugs, nor processes involving drug transporters. | ||
''Indacaterol'': In vitro investigations indicated that indacaterol has negligible potential to cause metabolic interactions with medications (by inhibition or induction of cytochrome P450 enzymes, or induction of UGT1A1) at the systemic exposure levels achieved in clinical practice. In vitro investigation furthermore indicated that, in vivo, indacaterol is unlikely to significantly inhibit transporter proteins such as P-gp, MRP2, BCRP, the cationic substrate transporters hOCT1 and hOCT2, and the human multidrug and toxin extrusion transporters hMATE1 and hMATE2K, and that indacaterol has negligible potential to induce P-gp or MRP2. | ''[[Indacaterol]]'': In vitro investigations indicated that [[indacaterol]] has negligible potential to cause metabolic interactions with medications (by inhibition or induction of [[cytochrome P450]] [[enzymes]], or induction of [[UGT1A1]]) at the systemic exposure levels achieved in clinical practice. In vitro investigation furthermore indicated that, in vivo, [[indacaterol]] is unlikely to significantly inhibit transporter proteins such as [[P-gp]], MRP2, BCRP, the cationic substrate transporters hOCT1 and hOCT2, and the human multidrug and toxin extrusion transporters hMATE1 and hMATE2K, and that [[indacaterol]] has negligible potential to induce [[P-gp]] or MRP2. | ||
''Glycopyrrolate'': In vitro inhibition studies demonstrated that glycopyrrolate has no relevant capacity to inhibit CYP1A2, CYP2A6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A4/5, the efflux transporters MDR1, MRP2 or MXR, and the uptake transporters OATP1B1, OATP1B3, OAT1, OAT3, OCT1 or OCT2. In vitro enzyme induction studies did not indicate a clinically relevant induction by glycopyrrolate for any of the cytochrome P450 isoenzymes tested as well as for UGT1A1 and the transporters MDR1 and MRP2. | ''[[Glycopyrrolate]]'': In vitro inhibition studies demonstrated that [[glycopyrrolate]] has no relevant capacity to inhibit [[CYP1A2]], [[CYP2A6]], [[CYP2C8]], [[CYP2C9]], [[CYP2C19]], [[CYP2D6]], [[CYP2E1]] or CYP3A4/5, the efflux transporters MDR1, MRP2 or MXR, and the uptake transporters OATP1B1, OATP1B3, OAT1, OAT3, OCT1 or OCT2. In vitro [[enzyme]] induction studies did not indicate a clinically relevant induction by [[glycopyrrolate]] for any of the [[cytochrome P450]] isoenzymes tested as well as for [[UGT1A1]] and the transporters MDR1 and MRP2. | ||
'''Specific Populations''': | '''Specific Populations''': | ||
Population pharmacokinetic analysis showed no evidence of a clinically significant effect of age (40 to 85 years), body weight (45 to 120 kg), gender, smoking status, and baseline FEV1 on systemic exposure of either indacaterol or glycopyrrolate following inhalation of [[indacaterol]] and [[glycopyrrolate]]. | Population pharmacokinetic analysis showed no evidence of a clinically significant effect of age (40 to 85 years), body weight (45 to 120 kg), gender, smoking status, and baseline [[FEV1]] on systemic exposure of either [[indacaterol]] or [[glycopyrrolate]] following inhalation of [[indacaterol]] and [[glycopyrrolate]]. | ||
Similarly no relevant covariate effect (of age, body weight, gender, smoking status, and baseline FEV1) was observed following the inhalation of the 2 components indacaterol and glycopyrrolate separately. | Similarly no relevant covariate effect (of age, body weight, gender, smoking status, and baseline [[FEV1]]) was observed following the inhalation of the 2 components [[indacaterol]] and [[glycopyrrolate]] separately. | ||
''Patients with Renal Impairment'': | ''Patients with [[renal impairment|Renal Impairment]]'': | ||
Indacaterol: Due to the very low contribution of the urinary pathway to total body elimination of indacaterol, a study in renally impaired subjects was not performed. | [[Indacaterol]]: Due to the very low contribution of the urinary pathway to total body elimination of [[indacaterol]], a study in renally impaired subjects was not performed. | ||
Glycopyrrolate: Renal impairment has an impact on the systemic exposure to glycopyrrolate. A moderate mean increase in total systemic exposure (AUC last) of up to 1.4-fold was seen in subjects with mild and moderate renal impairment [estimated GFR greater than or equal to 30 mL/min/1.73m2] and up to 2.2-fold in subjects with severe renal impairment and end stage renal disease [estimated GFR less than 30 mL/min/1.73m2]. | [[Glycopyrrolate]]: [[Renal impairment]] has an impact on the systemic exposure to [[glycopyrrolate]]. A moderate mean increase in total systemic exposure ([[AUC]] last) of up to 1.4-fold was seen in subjects with mild and moderate [[renal impairment]] [estimated [[GFR]] greater than or equal to 30 mL/min/1.73m2] and up to 2.2-fold in subjects with severe [[renal impairment]] and [[end stage renal disease]] [estimated [[GFR]] less than 30 mL/min/1.73m2]. | ||
''Patients with Hepatic Impairment'': | ''Patients with Hepatic Impairment'': | ||
Based on the clinical pharmacokinetic characteristics of its monotherapy components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild and moderate hepatic impairment. [[Indacaterol]] and [[glycopyrrolate]] has not been evaluated in subjects with severe hepatic impairment. | Based on the clinical pharmacokinetic characteristics of its [[monotherapy]] components, [[indacaterol]] and [[glycopyrrolate]] can be used at the recommended dose in patients with mild and moderate hepatic impairment. [[Indacaterol]] and [[glycopyrrolate]] has not been evaluated in subjects with severe hepatic impairment. | ||
Indacaterol: Patients with mild and moderate hepatic impairment showed no relevant changes in Cmax or AUC of indacaterol, nor did protein binding differ between mild and moderate hepatic impaired subjects and their healthy controls. Studies in subjects with severe hepatic impairment were not performed. | [[Indacaterol]]: Patients with mild and moderate hepatic impairment showed no relevant changes in [[Cmax]] or [[AUC]] of indacaterol, nor did protein binding differ between mild and moderate hepatic impaired subjects and their healthy controls. Studies in subjects with severe hepatic impairment were not performed. | ||
Glycopyrrolate: Clinical studies in patients with hepatic impairment have not been conducted. Glycopyrrolate is cleared predominantly from the systemic circulation by renal excretion. | [[Glycopyrrolate]]: Clinical studies in patients with hepatic impairment have not been conducted. [[Glycopyrrolate]] is cleared predominantly from the systemic circulation by renal excretion. | ||
''Ethnicity'': | ''Ethnicity'': | ||
There was no evidence of a clinically significant ethnic/race effect (across Caucasian, Chinese, and Japanese subjects) on the systemic exposure to indacaterol and glycopyrrolate following inhalation of [[indacaterol]] and [[glycopyrrolate]]. Similarly, no relevant ethnic effect was observed following the inhalation of the 2 components indacaterol and glycopyrrolate separately. | There was no evidence of a clinically significant ethnic/race effect (across Caucasian, Chinese, and Japanese subjects) on the systemic exposure to [[indacaterol]] and [[glycopyrrolate]] following inhalation of [[indacaterol]] and [[glycopyrrolate]]. Similarly, no relevant ethnic effect was observed following the inhalation of the 2 components [[indacaterol]] and [[glycopyrrolate]] separately. | ||
|nonClinToxic='''Carcinogenesis, Mutagenesis, Impairment of Fertility''' | |nonClinToxic='''[[Carcinogenesis]], [[Mutagenesis]], Impairment of [[Fertility]]''' | ||
No studies of carcinogenicity, mutagenicity, or impairment of fertility were conducted with [[indacaterol]] and [[glycopyrrolate]]; however, studies are available for the individual components, indacaterol and glycopyrrolate, as described below. | No studies of [[carcinogenicity]], [[mutagenicity]], or impairment of [[fertility]] were conducted with [[indacaterol]] and [[glycopyrrolate]]; however, studies are available for the individual components, [[indacaterol]] and [[glycopyrrolate]], as described below. | ||
''Indacaterol'': Indacaterol produced no treatment-related increases in the incidence of tumors in a 2-year inhalation study in Wistar rats at inhaled doses up to 2.09 mg/kg/day (approximately 110 times the MRHD in adults on an AUC basis, respectively). A 26-week oral (gavage) study in CB6F1/TgrasH2 hemizygous mice with indacaterol at doses up to 600 mg/kg/day did not show any evidence of tumorigenicity. | ''[[Indacaterol]]'': [[Indacaterol]] produced no treatment-related increases in the incidence of tumors in a 2-year inhalation study in Wistar rats at inhaled doses up to 2.09 mg/kg/day (approximately 110 times the MRHD in adults on an [[AUC]] basis, respectively). A 26-week oral (gavage) study in CB6F1/TgrasH2 hemizygous mice with [[indacaterol]] at doses up to 600 mg/kg/day did not show any evidence of tumorigenicity. | ||
Indacaterol tested negative in the following genotoxicity assays: the in vitro Ames test, in vitro chromosome aberration test in V79 Chinese hamster cells, and in vivo rat bone marrow micronucleus test. | [[Indacaterol]] tested negative in the following genotoxicity assays: the in vitro [[Ames test]], in vitro [[chromosome aberration]] test in V79 Chinese hamster cells, and in vivo rat bone marrow [[micronucleus]] test. | ||
Indacaterol had no effects on fertility and reproductive performance in male and female rats at subcutaneous doses up to 2 mg/kg/day (approximately 890 and 670 times in males and females, respectively, the MRHD in adults on an AUC basis). | [[Indacaterol]] had no effects on [[fertility]] and reproductive performance in male and female rats at [[subcutaneous]] doses up to 2 mg/kg/day (approximately 890 and 670 times in males and females, respectively, the MRHD in adults on an [[AUC]] basis). | ||
''Glycopyrrolate'': Glycopyrrolate produced no treatment-related increases in the incidence of tumors in a 2-year inhalation study in Wistar rats at inhaled doses up to 0.56 mg/kg/day (approximately 170 times the MRHD in adults on an AUC basis). A 26-week oral (gavage) study in male and female TgrasH2 mice that received glycopyrrolate at doses up to 93.8 and 125.1 mg/kg/day, respectively, did not show any evidence of tumorigenicity. | ''[[Glycopyrrolate]]'': [[Glycopyrrolate]] produced no treatment-related increases in the incidence of [[tumors]] in a 2-year inhalation study in Wistar rats at inhaled doses up to 0.56 mg/kg/day (approximately 170 times the MRHD in adults on an [[AUC]] basis). A 26-week oral (gavage) study in male and female TgrasH2 mice that received [[glycopyrrolate]] at doses up to 93.8 and 125.1 mg/kg/day, respectively, did not show any evidence of tumorigenicity. | ||
Glycopyrrolate tested negative in the following genotoxicity assays: the in vitro Ames assay, in vitro human lymphocyte chromosomal aberration assay, and in vivo rat bone marrow micronucleus assay. | [[Glycopyrrolate]] tested negative in the following genotoxicity assays: the in vitro Ames assay, in vitro human lymphocyte [[chromosomal aberration]] assay, and in vivo rat bone marrow [[micronucleus]] assay. | ||
Impairment of fertility was observed in male and female rats at a subcutaneous dose of 1.88 mg/kg/day (approximately 1900 and 1100 times the MRHD in adults on an AUC basis, respectively) based upon findings of decreased corpora lutea, implantation sites and live fetuses. No effects on fertility and reproductive performance in male and female rats were observed at a subcutaneous dose of 0.63 mg/kg/day (approximately 350 times the MRHD in adults on an AUC basis). | Impairment of [[fertility]] was observed in male and female rats at a [[subcutaneous]] dose of 1.88 mg/kg/day (approximately 1900 and 1100 times the MRHD in adults on an [[AUC]] basis, respectively) based upon findings of decreased corpora lutea, implantation sites and live fetuses. No effects on [[fertility]] and reproductive performance in male and female rats were observed at a [[subcutaneous]] dose of 0.63 mg/kg/day (approximately 350 times the MRHD in adults on an [[AUC]] basis). | ||
'''Animal Toxicology''': | '''Animal Toxicology''': | ||
Eye findings were seen for glycopyrrolate and were observed in Wistar rats at inhaled doses of 0.67 mg/kg/day and higher (approximately 280 times the MRHD in adults on an AUC basis) based upon findings of anterior capsule opacity, prominent anterior suture line, and anterior cataract. No eye findings in Wistar rats were observed at an inhaled dose of 0.09 mg/kg/day (approximately 60 times the MRHD in adults on an AUC basis). Eye findings were observed in beagle dogs at an inhaled dose of 0.33 mg/kg/day (approximately 150 times the MRHD in adults on an AUC basis) based upon findings of conjunctival hyperemia and corneal opacity. No eye findings in beagle dogs were observed at an inhaled dose of 0.12 mg/kg/day (approximately 100 times the MRHD in adults on an AUC basis). | Eye findings were seen for [[glycopyrrolate]] and were observed in Wistar rats at inhaled doses of 0.67 mg/kg/day and higher (approximately 280 times the MRHD in adults on an [[AUC]] basis) based upon findings of anterior capsule opacity, prominent anterior suture line, and anterior [[cataract]]. No eye findings in Wistar rats were observed at an inhaled dose of 0.09 mg/kg/day (approximately 60 times the MRHD in adults on an [[AUC]] basis). Eye findings were observed in beagle dogs at an inhaled dose of 0.33 mg/kg/day (approximately 150 times the MRHD in adults on an [[AUC]] basis) based upon findings of conjunctival [[hyperemia]] and [[cornea|corneal]] opacity. No eye findings in beagle dogs were observed at an inhaled dose of 0.12 mg/kg/day (approximately 100 times the MRHD in adults on an [[AUC]] basis). | ||
|clinicalStudies=The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] were evaluated in a clinical development program that included 3 dose-ranging trials, 2 lung function trials of 12 weeks duration (placebo-controlled and active-controlled) and a 12-month long-term safety trial. The efficacy of [[indacaterol]] and [[glycopyrrolate]] is based primarily on the dose-ranging trials in 562 subjects with COPD or asthma and the 2 placebo- and active-controlled confirmatory trials in 2043 subjects with additional support from one active-controlled 12-month trial in 615 subjects with COPD. | |clinicalStudies=The safety and efficacy of [[indacaterol]] and [[glycopyrrolate]] were evaluated in a clinical development program that included 3 dose-ranging trials, 2 lung function trials of 12 weeks duration (placebo-controlled and active-controlled) and a 12-month long-term safety trial. The efficacy of [[indacaterol]] and [[glycopyrrolate]] is based primarily on the dose-ranging trials in 562 subjects with [[COPD]] or [[asthma]] and the 2 placebo- and active-controlled confirmatory trials in 2043 subjects with additional support from one active-controlled 12-month trial in 615 subjects with [[COPD]]. | ||
'''Dose-Ranging Trials''': | '''Dose-Ranging Trials''': | ||
Dose selection for [[indacaterol]] and [[glycopyrrolate]] for COPD was based on data for the individual components | Dose selection for [[indacaterol]] and [[glycopyrrolate]] for [[COPD]] was based on data for the individual components. | ||
''Indacaterol'': Indacaterol dose selection in [[indacaterol]] and [[glycopyrrolate]] is based on the registered dose of 75 mcg once-daily and is also supported by a single-dose, multicenter, randomized, double-blind, placebo-controlled, crossover study in asthma evaluating 5 doses of indacaterol in 91 subjects, (37.5 mcg, 55 mcg, 75 mcg, and 150 mcg once-daily (QD), and 27.5 mcg twice-daily (BID)). A dose-related increase in FEV1 | ''[[Indacaterol]]'': [[Indacaterol]] dose selection in [[indacaterol]] and [[glycopyrrolate]] is based on the registered dose of 75 mcg once-daily and is also supported by a single-dose, multicenter, randomized, double-blind, placebo-controlled, crossover study in [[asthma]] evaluating 5 doses of [[indacaterol]] in 91 subjects, (37.5 mcg, 55 mcg, 75 mcg, and 150 mcg once-daily (QD), and 27.5 mcg twice-daily (BID)). A dose-related increase in [[FEV1]] [[AUC]]0-24h compared with placebo was observed. The differences in change from baseline in [[FEV1]] [[AUC]]0-24h after single dosing for the [[indacaterol]] 37.5 mcg, 55 mcg, 75 mcg, and 150 mcg once-daily and the 27.5 mcg twice-daily doses compared to placebo were 0.099 L (95% CI: 0.069, 0.128), 0.132 L (0.103, 0.162), 0.143 L (0.114, 0.171), 0.187 L (0.157, 0.216), and 0.121 L (0.092, 0.151), respectively. These results supported the evaluation of [[indacaterol]] 27.5 mcg twice-daily in the confirmatory [[COPD]] trials. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for [[asthma]]. | ||
[[File:Indacaterol and glycopyrrolate F1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate F1.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
''Glycopyrrolate'': Dose selection for glycopyrrolate in [[indacaterol]] and [[glycopyrrolate]] in COPD was supported by a 28-day, randomized, double-blind, placebo-controlled, 2-period, crossover study evaluating 7 doses of glycopyrrolate (15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily) or placebo in 388 subjects with COPD. The differences in trough FEV1 from baseline after 28 days compared to placebo for the 15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and for 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily doses were 0.083 L (95% CI: 0.030, 0.136), 0.098 L (0.048, 0.148), 0.090 L (0.038, 0.142), 0.176 L (0.132, 0.220), 0.139 L (0.089, 0.189), 0.167 L (0.115, 0.219), and 0.177 L (0.132, 0.222), respectively. The dose-ranging results supported the evaluation of glycopyrrolate 15.6 mcg twice-daily in the confirmatory COPD trials. | ''[[Glycopyrrolate]]'': Dose selection for [[glycopyrrolate]] in [[indacaterol]] and [[glycopyrrolate]] in [[COPD]] was supported by a 28-day, randomized, double-blind, placebo-controlled, 2-period, crossover study evaluating 7 doses of [[glycopyrrolate]] (15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily) or placebo in 388 subjects with [[COPD]]. The differences in trough [[FEV1]] from baseline after 28 days compared to placebo for the 15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and for 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily doses were 0.083 L (95% CI: 0.030, 0.136), 0.098 L (0.048, 0.148), 0.090 L (0.038, 0.142), 0.176 L (0.132, 0.220), 0.139 L (0.089, 0.189), 0.167 L (0.115, 0.219), and 0.177 L (0.132, 0.222), respectively. The dose-ranging results supported the evaluation of glycopyrrolate 15.6 mcg twice-daily in the confirmatory [[COPD]] trials. | ||
[[File:Indacaterol and glycopyrrolate F2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate F2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
Based on the findings from dose-ranging studies of the individual components, a twice-daily dose of indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg was evaluated in the confirmatory COPD trials. | Based on the findings from dose-ranging studies of the individual components, a twice-daily dose of [[indacaterol]]/[[glycopyrrolate]] 27.5 mcg/15.6 mcg was evaluated in the confirmatory [[COPD]] trials. | ||
'''Confirmatory Trials''': | '''Confirmatory Trials''': | ||
The clinical development program for [[indacaterol]] and [[glycopyrrolate]] included two (Trial 1 and Trial 2) 12-week, randomized, double-blinded, placebo- and active-controlled, parallel-group trials in subjects with COPD designed to evaluate the efficacy and safety of [[indacaterol]] and [[glycopyrrolate]]; and one 12-month, randomized, double-blind, active-controlled trial (Trial 3) that evaluated bronchodilation and effects on long-term safety. | The clinical development program for [[indacaterol]] and [[glycopyrrolate]] included two (Trial 1 and Trial 2) 12-week, randomized, double-blinded, placebo- and active-controlled, parallel-group trials in subjects with [[COPD]] designed to evaluate the efficacy and safety of [[indacaterol]] and [[glycopyrrolate]]; and one 12-month, randomized, double-blind, active-controlled trial (Trial 3) that evaluated bronchodilation and effects on long-term safety. | ||
The 12-week trials evaluated the efficacy of 2038 subjects that had a clinical diagnosis of COPD, were 40 years of age or older, had a history of smoking greater than 10 pack-years, had a post-albuterol FEV1 greater than or equal to 30% and less than 80% of predicted normal values, had a ratio of FEV1/FVC of less than 0.7, and were symptomatic as determined by a Modified Medical Research Council (mMRC) score greater than or equal to 2. Of the 2038 subjects included in the efficacy analysis, 63% were male and 91% were Caucasian. They had a mean age of 63 years and an average smoking history of 47 pack-years, with 52% identified as current smokers, and 46% used concomitant inhaled corticosteroids. At screening, the mean post-bronchodilator percent predicted FEV1 was 55% (range: 29% to 79%), the mean post-bronchodilator FEV1/FVC ratio was 50% (range: 19% to 71%), and the mean percent reversibility was 23% (range: 0% to 144%). | The 12-week trials evaluated the efficacy of 2038 subjects that had a clinical diagnosis of [[COPD]], were 40 years of age or older, had a history of smoking greater than 10 pack-years, had a post-[[albuterol]] [[FEV1]] greater than or equal to 30% and less than 80% of predicted normal values, had a ratio of [[FEV1]]/[[FVC]] of less than 0.7, and were symptomatic as determined by a Modified Medical Research Council (mMRC) score greater than or equal to 2. Of the 2038 subjects included in the efficacy analysis, 63% were male and 91% were Caucasian. They had a mean age of 63 years and an average smoking history of 47 pack-years, with 52% identified as current smokers, and 46% used concomitant inhaled [[corticosteroids]]. At screening, the mean post-[[bronchodilator]] percent predicted [[FEV1]] was 55% (range: 29% to 79%), the mean post-[[bronchodilator]] [[FEV1]]/[[FVC]] ratio was 50% (range: 19% to 71%), and the mean percent reversibility was 23% (range: 0% to 144%). | ||
Trial 1 and Trial 2 evaluated [[indacaterol]] and [[glycopyrrolate]] | Trial 1 and Trial 2 evaluated [[indacaterol]] and [[glycopyrrolate]] 27.5 mcg/15.6 mcg twice-daily (BID), [[indacaterol]] 27.5 mcg BID, [[glycopyrrolate]] 15.6 mcg BID, and placebo BID. The primary endpoint was the change from baseline in [[FEV1]] [[AUC]]0-12h following the morning dose at Day 85 (defined as the mean [[FEV1]] change from baseline over 0 to 12 hours divided by 12 hours) compared with placebo, [[glycopyrrolate]] 15.6 mcg BID, and [[indacaterol]] 27.5 mcg BID. The comparison of [[indacaterol]] and [[glycopyrrolate]] with [[indacaterol]] 27.5 mcg and [[glycopyrrolate]] 15.6 mcg was assessed to evaluate the contribution of the individual comparators to [[indacaterol]] and [[glycopyrrolate]]. In both trials, [[indacaterol]] and [[glycopyrrolate]] demonstrated a larger increase in mean change from baseline in [[FEV1]] [[AUC]]0-12h compared to placebo, [[indacaterol]] 27.5 mcg BID, and [[glycopyrrolate]] 15.6 mcg BID (see Table 2). | ||
[[File:Indacaterol and glycopyrrolate T2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate T2.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
With the limited data available, there was no suggestion of a difference in FEV1 | With the limited data available, there was no suggestion of a difference in [[FEV1]] [[AUC]]0-12h with respect to age, sex, degree of airflow limitation, GOLD stage, smoking status, or inhaled [[corticosteroid]] use. | ||
In Trial 1 and Trial 2, serial spirometric evaluations throughout the 12-hour dosing interval were performed in all subjects at Days 1 and 85. The spirometric curves from Trial 1 at Days 1 and 85 are displayed in Figure 3. In Trial 2, the results for [[indacaterol]] and [[glycopyrrolate]] in FEV1 | In Trial 1 and Trial 2, serial [[spirometry|spirometric]] evaluations throughout the 12-hour dosing interval were performed in all subjects at Days 1 and 85. The spirometric curves from Trial 1 at Days 1 and 85 are displayed in Figure 3. In Trial 2, the results for [[indacaterol]] and [[glycopyrrolate]] in [[FEV1]] [[AUC]]0-12h were similar to those observed in Trial 1. | ||
[[File:Indacaterol and glycopyrrolate F3.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate F3.JPG|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
The peak FEV1 was defined as the maximum FEV1 recorded within 4 hours after the morning dose on Days 1 and 85. The mean peak FEV1 improvement from baseline for [[indacaterol]] and [[glycopyrrolate]] compared with placebo at Day 1 and at Day 85 was 0.185 L and 0.290 L (Trial 1) and 0.151 L and 0.260 L (Trial 2), respectively. The median time to onset on Day 1, defined as a 100 mL increase from baseline in FEV1, was 12 minutes and 16 minutes in Trials 1 and 2, respectively, in subjects receiving [[indacaterol]] and [[glycopyrrolate]]. | The peak [[FEV1]] was defined as the maximum [[FEV1]] recorded within 4 hours after the morning dose on Days 1 and 85. The mean peak [[FEV1]] improvement from baseline for [[indacaterol]] and [[glycopyrrolate]] compared with placebo at Day 1 and at Day 85 was 0.185 L and 0.290 L (Trial 1) and 0.151 L and 0.260 L (Trial 2), respectively. The median time to onset on Day 1, defined as a 100 mL increase from baseline in [[FEV1]], was 12 minutes and 16 minutes in Trials 1 and 2, respectively, in subjects receiving [[indacaterol]] and [[glycopyrrolate]]. | ||
In Trials 1 and 2, patients treated with [[indacaterol]] and [[glycopyrrolate]] used less daily rescue albuterol compared to patients treated with placebo. | In Trials 1 and 2, patients treated with [[indacaterol]] and [[glycopyrrolate]] used less daily rescue [[albuterol]] compared to patients treated with placebo. | ||
The St. George’s Respiratory Questionnaire (SGRQ) was assessed in Trials 1 and 2. In Trial 2, the SGRQ responder rate (defined as an improvement in score of 4 or more as threshold) was 57%, 46%, 48%, and 39%, for [[indacaterol]] and [[glycopyrrolate]], glycopyrrolate, indacaterol, and placebo, respectively, with odds ratios of 1.6 (95% CI 1.1, 2.3), 1.5 (95% CI 1.1, 2.2), and 2.2 (95% CI 1.5, 3.2), for [[indacaterol]] and [[glycopyrrolate]] vs. glycopyrrolate, [[indacaterol]] and [[glycopyrrolate]] vs. indacaterol, and [[indacaterol]] and [[glycopyrrolate]] vs. placebo, respectively. In Trial 1, the trends were similar, with odds ratios of 1.4 (95% CI 1.0, 2.0), 1.1 (95% CI 0.8, 1.7), and 2.9 (95% CI 1.9, 4.2), for [[indacaterol]] and [[glycopyrrolate]] vs. glycopyrrolate, [[indacaterol]] and [[glycopyrrolate]] vs. indacaterol, and [[indacaterol]] and [[glycopyrrolate]] vs placebo, respectively. | The St. George’s Respiratory Questionnaire (SGRQ) was assessed in Trials 1 and 2. In Trial 2, the SGRQ responder rate (defined as an improvement in score of 4 or more as threshold) was 57%, 46%, 48%, and 39%, for [[indacaterol]] and [[glycopyrrolate]], [[glycopyrrolate]], [[indacaterol]], and placebo, respectively, with odds ratios of 1.6 (95% CI 1.1, 2.3), 1.5 (95% CI 1.1, 2.2), and 2.2 (95% CI 1.5, 3.2), for [[indacaterol]] and [[glycopyrrolate]] vs. [[glycopyrrolate]], [[indacaterol]] and [[glycopyrrolate]] vs. [[indacaterol]], and [[indacaterol]] and [[glycopyrrolate]] vs. placebo, respectively. In Trial 1, the trends were similar, with odds ratios of 1.4 (95% CI 1.0, 2.0), 1.1 (95% CI 0.8, 1.7), and 2.9 (95% CI 1.9, 4.2), for [[indacaterol]] and [[glycopyrrolate]] vs. [[glycopyrrolate]], [[indacaterol]] and [[glycopyrrolate]] vs. [[indacaterol]], and [[indacaterol]] and [[glycopyrrolate]] vs placebo, respectively. | ||
52-week Effects on Lung Function: At week 52 (Trial 3), [[indacaterol]] and [[glycopyrrolate]] demonstrated a significant treatment effect with an increase of 0.080 L in pre-dose trough FEV1 compared to indacaterol 75 mcg once-daily. | 52-week Effects on Lung Function: At week 52 (Trial 3), [[indacaterol]] and [[glycopyrrolate]] demonstrated a significant treatment effect with an increase of 0.080 L in pre-dose trough [[FEV1]] compared to [[indacaterol]] 75 mcg once-daily. | ||
|howSupplied=[[Indacaterol]] and [[glycopyrrolate]] contains [[indacaterol]] and [[glycopyrrolate]] (indacaterol/glycopyrrolate, (27.5 mcg, 15.6 mcg) inhalation powder) in hypromellose (HPMC) capsule with yellow transparent cap and uncolored transparent body, with capsules packaged in aluminum blister cards, one NEOHALER device, and an FDA approved Medication Guide. | |howSupplied=[[Indacaterol]] and [[glycopyrrolate]] contains [[indacaterol]] and [[glycopyrrolate]] ([[indacaterol]]/[[glycopyrrolate]], (27.5 mcg, 15.6 mcg) inhalation powder) in hypromellose (HPMC) capsule with yellow transparent cap and uncolored transparent body, with capsules packaged in aluminum blister cards, one NEOHALER device, and an FDA approved Medication Guide. | ||
*Unit Dose (blister pack), Box of 60 (10 blister cards with 6 yellow transparent capsules each) NDC 0078-0664-19 | *Unit Dose (blister pack), Box of 60 (10 blister cards with 6 yellow transparent capsules each) NDC 0078-0664-19 | ||
*Unit Dose (blister pack), Box of 6 (1 blister card with 6 yellow transparent capsules each) NDC 0078-0664-06 | *Unit Dose (blister pack), Box of 6 (1 blister card with 6 yellow transparent capsules each) NDC 0078-0664-06 | ||
| Line 354: | Line 358: | ||
[[File:Indacaterol and glycopyrrolate label.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | [[File:Indacaterol and glycopyrrolate label.jpg|thumb|none|400px|This image is provided by the National Library of Medicine]] | ||
|fdaPatientInfo=Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use). | |fdaPatientInfo=Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use). | ||
*Asthma-Related Death | *[[Asthma]]-Related Death | ||
**Inform patients that LABAs, such as indacaterol, one of the active ingredients in [[indacaterol]] and [[glycopyrrolate]], increase the risk of asthma-related death. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of asthma. | **Inform patients that [[LABA|LABAs]], such as [[indacaterol]], one of the active ingredients in [[indacaterol]] and [[glycopyrrolate]], increase the risk of [[asthma]]-related death. [[Indacaterol]] and [[glycopyrrolate]] is not indicated for the treatment of [[asthma]]. | ||
*Not for Acute Symptoms | *Not for Acute Symptoms | ||
**Inform patients that [[indacaterol]] and [[glycopyrrolate]] is not meant to relieve acute symptoms of COPD and extra doses should not be used for that purpose. Advise them to treat acute symptoms with a rescue inhaler such as albuterol. Provide patients with such medicine and instruct them on how it should be used. | **Inform patients that [[indacaterol]] and [[glycopyrrolate]] is not meant to relieve acute symptoms of [[COPD]] and extra doses should not be used for that purpose. Advise them to treat acute symptoms with a rescue inhaler such as [[albuterol]]. Provide patients with such medicine and instruct them on how it should be used. | ||
**Instruct patients to seek medical attention immediately if they experience any of the following: | **Instruct patients to seek medical attention immediately if they experience any of the following: | ||
***Symptoms get worse | ***Symptoms get worse | ||
***Need for more inhalations than usual of their rescue inhaler | ***Need for more inhalations than usual of their rescue inhaler | ||
**Patients should not stop therapy with [[indacaterol]] and [[glycopyrrolate]] without physician/healthcare provider guidance since symptoms may recur after discontinuation. | **Patients should not stop therapy with [[indacaterol]] and [[glycopyrrolate]] without physician/healthcare provider guidance since symptoms may recur after discontinuation. | ||
*Do Not Use Additional Long-Acting Beta2-Agonists | *Do Not Use Additional [[LABA|Long-Acting Beta2-Agonists]] | ||
**Instruct patients to not use other medicines containing a LABA. Patients should not use more than the recommended twice-daily dose of [[indacaterol]] and [[glycopyrrolate]]. | **Instruct patients to not use other medicines containing a [[LABA]]. Patients should not use more than the recommended twice-daily dose of [[indacaterol]] and [[glycopyrrolate]]. | ||
**Instruct patients who have been taking inhaled, short-acting beta2-agonists on a regular basis to discontinue the regular use of these products and use them only for the symptomatic relief of acute symptoms. | **Instruct patients who have been taking inhaled, [[SABA|short-acting beta2-agonists]] on a regular basis to discontinue the regular use of these products and use them only for the symptomatic relief of acute symptoms. | ||
*Paradoxical Bronchospasm | *Paradoxical [[Bronchospasm]] | ||
**Inform patients that [[indacaterol]] and [[glycopyrrolate]] can produce paradoxical bronchospasm. Advise patients that if paradoxical bronchospasm occurs, patients should discontinue [[indacaterol]] and [[glycopyrrolate]]. | **Inform patients that [[indacaterol]] and [[glycopyrrolate]] can produce paradoxical [[bronchospasm]]. Advise patients that if paradoxical [[bronchospasm]] occurs, patients should discontinue [[indacaterol]] and [[glycopyrrolate]]. | ||
*Risks Associated with Beta2-Agonist Therapy | *Risks Associated with [[Beta2-adrenergic receptor agonist|Beta2-Agonist]] Therapy | ||
**Inform patients of adverse effects associated with beta2-agonists, such as palpitations, chest pain, rapid heart rate, tremor, or nervousness. Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | **Inform patients of adverse effects associated with [[Beta2-adrenergic receptor agonist|beta2-agonists]], such as [[palpitations]], [[chest pain]], [[rapid heart rate]], [[tremor]], or [[nervousness]]. Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | ||
*Worsening of Narrow-Angle Glaucoma | *Worsening of [[narrow-angle glaucoma|Narrow-Angle Glaucoma]] | ||
**Instruct patients to be alert for signs and symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion and corneal edema). Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | **Instruct patients to be alert for signs and symptoms of acute [[narrow-angle glaucoma]] (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from [[conjunctiva|conjunctival]] congestion and [[cornea|corneal]] [[edema]]). Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | ||
*Worsening of Urinary Retention | *Worsening of [[urinary retention|Urinary Retention]] | ||
**Instruct patients to be alert for signs and symptoms of urinary retention (e.g., difficulty passing urine, painful urination). Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | **Instruct patients to be alert for signs and symptoms of [[urinary retention]] (e.g., [[difficulty passing urine]], [[painful urination]]). Instruct patients to consult a physician immediately should any of these signs or symptoms develop. | ||
*Instructions for Administering [[Indacaterol]] and [[Glycopyrrolate]] | *Instructions for Administering [[Indacaterol]] and [[Glycopyrrolate]] | ||
**It is important for patients to understand how to correctly administer [[indacaterol]] and [[glycopyrrolate]] capsules using the NEOHALER device. | **It is important for patients to understand how to correctly administer [[indacaterol]] and [[glycopyrrolate]] capsules using the NEOHALER device. | ||
| Line 380: | Line 384: | ||
**Inform patients to use 1 inhalation of [[indacaterol]] and [[glycopyrrolate]] orally twice-daily (1 capsule in the morning and 1 capsule in the evening) at the same time every day. | **Inform patients to use 1 inhalation of [[indacaterol]] and [[glycopyrrolate]] orally twice-daily (1 capsule in the morning and 1 capsule in the evening) at the same time every day. | ||
**Inform patients that if they miss a dose of [[indacaterol]] and [[glycopyrrolate]], they should use their next capsule at the usual time. Instruct patients to not use 2 capsules at one time and to not use more than 2 capsules in a day. | **Inform patients that if they miss a dose of [[indacaterol]] and [[glycopyrrolate]], they should use their next capsule at the usual time. Instruct patients to not use 2 capsules at one time and to not use more than 2 capsules in a day. | ||
|alcohol=Alcohol-Indacaterol and glycopyrrolate interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-[[Indacaterol]] and [[glycopyrrolate]] interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Latest revision as of 19:32, 28 July 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Allison Tu [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
ASTHMA-RELATED DEATH
See full prescribing information for complete Boxed Warning.
|
Overview
Indacaterol and glycopyrrolate is a combination of a long-acting beta2-adrenergic agonist and an anticholinergic that is FDA approved for the treatment of airflow obstruction in patients with chronic obstructive pulmonary disease. There is a Black Box Warning for this drug as shown here. Common adverse reactions include cough.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indacaterol and glycopyrrolate is indicated for the long-term, maintenance treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema. Indacaterol and glycopyrrolate is NOT indicated for the relief of acute bronchospasm or for the treatment of asthma.
Dosing Information
- The recommended dosage of indacaterol and glycopyrrolate is the inhalation of the contents of one indacaterol and glycopyrrolate capsule twice-daily using the NEOHALER device.
- No dosage adjustment is required for geriatric patients, patients with mild and moderate hepatic impairment, or patients with mild to moderate renal impairment.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of indacaterol and glycopyrrolate in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of indacaterol and glycopyrrolate in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Indacaterol and glycopyrrolate FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Indacaterol and glycopyrrolate in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Indacaterol and glycopyrrolate in pediatric patients.
Contraindications
- All LABAs are contraindicated in patients with asthma without use of a long-term asthma control medication.
- Indacaterol and glycopyrrolate is not indicated for the treatment of asthma.
- Indacaterol and glycopyrrolate is contraindicated in patients who have demonstrated hypersensitivity to indacaterol, glycopyrrolate, or to any of the ingredients.
Warnings
|
ASTHMA-RELATED DEATH
See full prescribing information for complete Boxed Warning.
|
- Asthma-Related Death
- Data from a large, placebo-controlled U.S. study in asthma patients showed that LABAs may increase the risk of asthma-related death.
- Data are not available to determine whether the rate of death in patients with COPD is increased by LABAs.
- A 28-week, placebo-controlled U.S. study comparing the safety of another LABA (salmeterol) with placebo, each added to usual asthma therapy, showed an increase in asthma-related deaths in patients receiving salmeterol (13/13,176 in patients treated with salmeterol versus 3/13,179 in patients treated with placebo; RR 4.37, 95% CI 1.25, 15.34).
- The increased risk of asthma-related death is considered a class effect of the LABAs, including indacaterol.
- No study adequate to determine whether the rate of asthma-related death is increased in patients treated with indacaterol and glycopyrrolate has been conducted. The safety and efficacy of indacaterol and glycopyrrolate in patients with asthma have not been established. Indacaterol and glycopyrrolate is not indicated for the treatment of asthma.
- Deterioration of Disease and Acute Episodes
- Indacaterol and glycopyrrolate should not be initiated in patients with acutely deteriorating or potentially life-threatening episodes of COPD. Indacaterol and glycopyrrolate has not been studied in patients with acutely deteriorating COPD. The initiation of indacaterol and glycopyrrolate in this setting is not appropriate.
- Indacaterol and glycopyrrolate should not be used for the relief of acute symptoms, i.e., as rescue therapy for the treatment of acute episodes of bronchospasm. Indacaterol and glycopyrrolate has not been studied in the relief of acute symptoms, and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist.
- When beginning indacaterol and glycopyrrolate, patients who have been taking oral or inhaled, short-acting beta2-agonists on a regular basis (e.g., 4 times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms.
- When prescribing indacaterol and glycopyrrolate, the healthcare provider should also prescribe an inhaled, short-acting beta2-agonist and instruct the patient on how it should be used. Increasing inhaled beta2-agonist use is a signal of deteriorating disease for which prompt medical attention is indicated.
- COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If indacaterol and glycopyrrolate no longer controls the symptoms of bronchoconstriction; the patient’s inhaled, short-acting beta2-agonist becomes less effective; or the patient needs more inhalation of short-acting beta2-agonist than usual, these may be markers of deterioration of disease. In this setting, a re-evaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dose of indacaterol and glycopyrrolate beyond the recommended dose is not appropriate in this situation.
- Excessive Use of Indacaterol and Glycopyrrolate and Use with Other Long-Acting Beta2-Adrenergic Agonists
- As with other inhaled drugs containing beta2-adrenergics, indacaterol and glycopyrrolate should not be used more often than recommended, at higher doses than recommended, or in conjunction with other medications containing LABAs, as an overdose may result.
- Clinically significant cardiovascular effects and fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs.
- Patients using indacaterol and glycopyrrolate should not use another medicine containing a LABA for any reason.
- Paradoxical Bronchospasm
- As with other inhaled medicines, indacaterol and glycopyrrolate can produce paradoxical bronchospasm that may be life-threatening.
- If paradoxical bronchospasm occurs following dosing with indacaterol and glycopyrrolate, it should be treated immediately with an inhaled, short-acting bronchodilator; indacaterol and glycopyrrolate should be discontinued immediately and alternative therapy instituted.
- Immediate Hypersensitivity Reactions
- Immediate hypersensitivity reactions have been reported after administration of indacaterol or glycopyrrolate, the components of indacaterol and glycopyrrolate. If signs suggesting allergic reactions occur, in particular, angioedema (including difficulties in breathing or swallowing, swelling of tongue, lips and face), urticaria, or skin rash, indacaterol and glycopyrrolate should be discontinued immediately and alternative therapy instituted. Indacaterol and glycopyrrolate should be used with caution in patients with severe hypersensitivity to milk proteins.
- Cardiovascular Effects
- Indacaterol, like other beta2-agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic or diastolic blood pressure, or symptoms. If such effects occur, indacaterol and glycopyrrolate may need to be discontinued.
- In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T-wave, prolongation of the QTc interval, and ST segment depression, although the clinical significance of these findings is unknown.
- Therefore, indacaterol and glycopyrrolate should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
- Coexisting Conditions
- Indacaterol and glycopyrrolate, like all medicines containing sympathomimetic amines, should be used with caution in patients with convulsive disorders or thyrotoxicosis, and in patients who are unusually responsive to sympathomimetic amines.
- Doses of the related beta2-agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis.
- Worsening of Narrow-Angle Glaucoma
- Indacaterol and glycopyrrolate should be used with caution in patients with narrow-angle glaucoma. Prescribers and patients should be alert for signs and symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion and corneal edema).
- Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
- Worsening of Urinary Retention
- Indacaterol and glycopyrrolate should be used with caution in patients with urinary retention. Prescribers and patients should be alert for signs and symptoms of urinary retention (e.g., difficulty passing urine, painful urination), especially in patients with prostatic hyperplasia or bladder-neck obstruction.
- Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
- Hypokalemia and Hyperglycemia
- Beta2-adrenergic agonists may produce significant hypokalemia in some patients, which has the potential to produce adverse cardiovascular effects. The decrease in serum potassium is usually transient, not requiring supplementation.
- Inhalation of high doses of beta2-adrenergic agonists may produce increases in plasma glucose.
- In patients with severe COPD, hypokalemia may be potentiated by hypoxia and concomitant treatment, which may increase the susceptibility for cardiac arrhythmias.
- In 2 clinical trials of 12-weeks duration evaluating indacaterol and glycopyrrolate in subjects with COPD, there was no evidence of a treatment effect on serum glucose or potassium.
Adverse Reactions
Clinical Trials Experience
LABAs, such as indacaterol, one of the active ingredients in indacaterol and glycopyrrolate, increase the risk of asthma-related death. Indacaterol and glycopyrrolate is not indicated for the treatment of asthma.
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in clinical practice.
The indacaterol and glycopyrrolate safety database included 2654 subjects with COPD in two 12-week lung function trials and one 52-week long-term safety study. A total of 712 subjects received treatment with indacaterol and glycopyrrolate 27.5 mcg/15.6 mcg twice daily (BID). The safety data described below are based on the two 12-week trials and the one 52-week trial.
12-Week Trials:
The incidence of adverse reactions associated with indacaterol and glycopyrrolate in Table 1 is based on two 12-week, placebo-controlled trials (Trials 1 and 2; N=1,001 and N=1,042 respectively). Of the 2040 subjects, 63% were male and 91% were Caucasian. They had a mean age of 63 years and an average smoking history of 47 pack-years, with 52% identified as current smokers. At screening, the mean post-bronchodilator percent predicted forced expiratory volume in 1 second (FEV1) was 55% (range: 29% to 79%), the mean post-bronchodilator FEV1/forced vital capacity (FVC) ratio was 50% (range: 19% to 71%), and the mean percent reversibility was 23% (range: 0% to 144%).
The most common adverse reaction (incidence greater than or equal to 2% and higher than placebo) was nasopharyngitis and hypertension.
The proportion of patients who discontinued treatment due to adverse reactions was 2.95% for the indacaterol and glycopyrrolate treated patients and 4.13% for placebo-treated patients.
Subjects received 1 dose twice-daily of the following: indacaterol and glycopyrrolate 27.5 mcg/15.6 mcg, indacaterol 27.5 mcg, glycopyrrolate 15.6 mcg, or placebo.
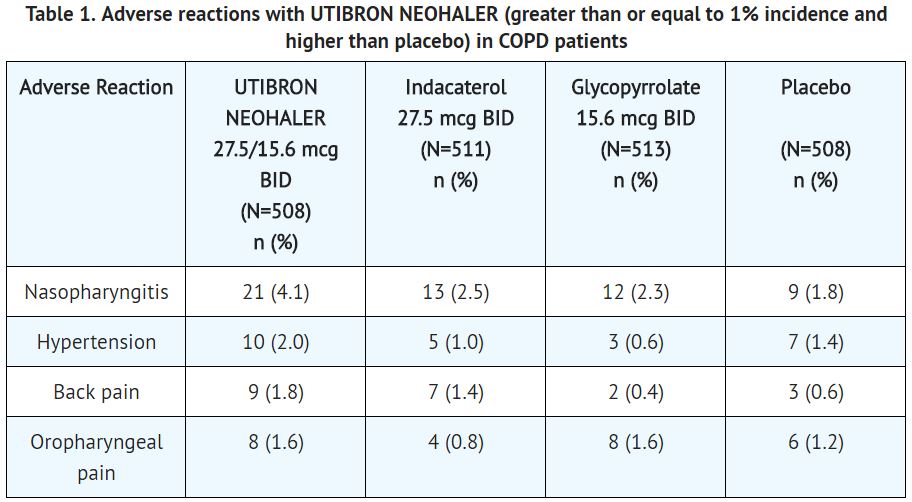
Other adverse reactions occurring more frequently with indacaterol and glycopyrrolate than with placebo, but with an incidence of less than 1% include dyspepsia, gastroenteritis, chest pain, fatigue, peripheral edema, rash/pruritus, insomnia, dizziness, bladder obstruction/urinary retention, atrial fibrillation, palpitations, tachycardia.
52-Week Trial:
In a long-term safety trial, 614 subjects were treated for up to 52 weeks with indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg twice-daily, indacaterol/glycopyrrolate 27.5/31.2 mcg twice-daily or indacaterol 75 mcg once-daily. The demographic and baseline characteristics of the long-term safety trial were similar to those of the placebo-controlled efficacy trials described above. The adverse reactions reported in the long-term safety trial were consistent with those observed in the placebo-controlled trials of 12 weeks. Additional adverse reactions that occurred with a frequency greater than or equal to 2% in the group receiving indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg twice-daily that exceeded the frequency of indacaterol 75 mcg once-daily in this trial were upper and lower respiratory tract infection, pneumonia, diarrhea, headache, gastroesophageal reflux disease, hyperglycemia, rhinitis.
Postmarketing Experience
The following additional adverse reactions of angioedema and dysphonia have been identified during worldwide post-approval use of indacaterol/glycopyrrolate at higher than the recommended dose. Because this reaction is reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate the frequency or establish a causal relationship to drug exposure.
Drug Interactions
- Adrenergic Drugs
- If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of indacaterol, a component of indacaterol and glycopyrrolate, may be potentiated.
- Xanthine Derivatives, Steroids, or Diuretics
- Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of beta2-adrenergic agonists such as indacaterol, a component of indacaterol and glycopyrrolate.
- Non-Potassium-Sparing Diuretics
- The electrocardiographic (ECG) changes and/or hypokalemia that may result from the administration of non-potassium-sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, such as indacaterol, a component of indacaterol and glycopyrrolate, especially when the recommended dose of the beta-agonist is exceeded.
- Although the clinical relevance of these effects is not known, caution is advised in the coadministration of indacaterol and glycopyrrolate with non-potassium-sparing diuretics.
- Monoamine Oxidase Inhibitors, Tricyclic Antidepressants, QTc-Prolonging Drugs
- Indacaterol, one of the components of indacaterol and glycopyrrolate, as with other beta2-agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors, tricyclic antidepressants, or other drugs known to prolong the QTc interval because the action of adrenergic agonists on the cardiovascular system may be potentiated by these agents.
- Drugs that are known to prolong the QTc interval may have an increased risk of ventricular arrhythmias.
- Beta-Blockers
- Beta-adrenergic receptor antagonists (beta-blockers) and indacaterol and glycopyrrolate may interfere with the effect of each other when administered concurrently.
- Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers.
- However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
- Anticholinergics
- There is potential for an additive interaction with concomitantly used anticholinergic medicines. Therefore, avoid coadministration of indacaterol and glycopyrrolate with other anticholinergic-containing drugs as this may lead to an increase in anticholinergic adverse effects.
- Inhibitors of Cytochrome P450 3A4 and P-gp Efflux Transporter
- Drug interaction studies with indacaterol, a component of indacaterol and glycopyrrolate, were carried out using potent and specific inhibitors of CYP3A4 and P-gp (i.e., ketoconazole, erythromycin, verapamil, and ritonavir).
- The data suggest that systemic clearance of indacaterol is influenced by modulation of both P-gp and CYP3A4 activities and that the 2-fold area under the curve (AUC) increase caused by the strong dual inhibitor ketoconazole reflects the impact of maximal combined inhibition.
- Indacaterol was evaluated in clinical trials for up to 1 year at doses up to 600 mcg. Inhibition of the key contributors of indacaterol clearance, CYP3A4 and P-gp, has no impact on safety of therapeutic doses of indacaterol. Therefore, no dose adjustment is warranted at the recommended 27.5/15.6 mcg twice-daily dose for indacaterol and glycopyrrolate when administered concomitantly with inhibitors of CYP3A4 and P-gp.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C Teratogenic Effects - Pregnancy Category C
There are no adequate and well-controlled studies with indacaterol and glycopyrrolate or its individual components, indacaterol and glycopyrrolate, in pregnant women. Animal reproduction studies were conducted with individual components, indacaterol and glycopyrrolate. Because animal reproduction studies are not always predictive of human response, indacaterol and glycopyrrolate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking indacaterol and glycopyrrolate.
Indacaterol: Indacaterol was not teratogenic in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1 mg/kg/day in rats and rabbits).
Glycopyrrolate: Glycopyrrolate was not teratogenic in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an AUC basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits).
Teratogenic Effects: Pregnancy Category C
There are no adequate and well-controlled studies with indacaterol and glycopyrrolate or its individual components, indacaterol and glycopyrrolate, in pregnant women. Animal reproduction studies were conducted with individual components, indacaterol and glycopyrrolate. Because animal reproduction studies are not always predictive of human response, indacaterol and glycopyrrolate should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Women should be advised to contact their physician if they become pregnant while taking indacaterol and glycopyrrolate.
Indacaterol: Indacaterol was not teratogenic in Wistar rats and New Zealand rabbits at approximately 340 and 770 times, respectively, the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1 mg/kg/day in rats and rabbits).
Glycopyrrolate: Glycopyrrolate was not teratogenic in Wistar rats or New Zealand White rabbits at approximately 1400 and 530 times, respectively, the MRHD in adults (on an AUC basis at maternal inhaled doses up to 3.83 mg/kg/day in rats and up to 4.4 mg/kg/day in rabbits).
Non-teratogenic Effects:
Indacaterol: There were no effects on perinatal and postnatal developments in rats at approximately 110 times the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 0.3 mg/kg/day).
Glycopyrrolate: There were no effects on perinatal and postnatal developments in rats at approximately 1100 times the MRHD in adults (on an AUC basis at maternal subcutaneous doses up to 1.88 mg/kg/day).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Indacaterol and glycopyrrolate in women who are pregnant.
Labor and Delivery
There are no adequate and well-controlled human trials that have investigated the effects of indacaterol and glycopyrrolate during labor and delivery. Because beta-agonists may potentially interfere with uterine contractility, indacaterol and glycopyrrolate should be used during labor only if the potential benefit justifies the potential risk.
In human parturients undergoing Caesarean section, 86 minutes after a single intramuscular injection of 0.006 mg/kg glycopyrrolate, umbilical plasma concentrations were low.
Nursing Mothers
Indacaterol and Glycopyrrolate: It is not known whether indacaterol and glycopyrrolate is excreted in human breast milk. Because many drugs are excreted in human milk, caution should be exercised when indacaterol and glycopyrrolate is administered to a nursing woman. Since there are no data from well-controlled human studies on the use of indacaterol and glycopyrrolate by nursing mothers, based on the data for the individual components, a decision should be made whether to discontinue nursing or to discontinue indacaterol and glycopyrrolate, taking into account the importance of indacaterol and glycopyrrolate to the mother.
Indacaterol: It is not known whether indacaterol is excreted in human breast milk. Indacaterol (including its metabolites) have been detected in the milk of lactating rats.
Glycopyrrolate: It is not known whether glycopyrrolate is excreted in human breast milk. Glycopyrrolate (including its metabolites) have been detected in the milk of lactating rats and reached up to 10-fold higher concentrations in the milk than in the blood of the dam.
Pediatric Use
Indacaterol and glycopyrrolate is not indicated for use in children. The safety and efficacy of indacaterol and glycopyrrolate in pediatric patients have not been established.
Geriatic Use
Based on available data, no adjustment of indacaterol and glycopyrrolate dosage in geriatric patients is warranted. Indacaterol and glycopyrrolate can be used at the recommended dose in elderly patients 75 years of age and older.
Of the total number of subjects in clinical studies of indacaterol and glycopyrrolate, 45% were aged 65 and older, while 11% were aged 75 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Indacaterol and glycopyrrolate with respect to specific gender populations.
Race
There is no FDA guidance on the use of Indacaterol and glycopyrrolate with respect to specific racial populations.
Renal Impairment
Based on the pharmacokinetic characteristics of its monotherapy components, indacaterol and glycopyrrolate can be used at the recommended dose in patients with mild to moderate renal impairment. In patients with severe renal impairment (estimated GFR less than 30 mL/min/1.73 m2) or end-stage renal disease requiring dialysis, indacaterol and glycopyrrolate should be used if the expected benefit outweighs the potential risk since the systemic exposure to glycopyrrolate may be increased in this population.
Hepatic Impairment
Based on the pharmacokinetic characteristics of its monotherapy components, indacaterol and glycopyrrolate can be used at the recommended dose in patients with mild to moderate hepatic impairment. Studies in subjects with severe hepatic impairment have not been performed.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Indacaterol and glycopyrrolate in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Indacaterol and glycopyrrolate in patients who are immunocompromised.
Administration and Monitoring
Administration
Indacaterold and glycopyrrolate is for oral inhalation only. Do not swallow Indacaterol and glycopyrrolate capsules, as the intended effects on the lungs will not be obtained. Indacaterol and glycopyrrolate capsules should only be used with the NEOHALER device. Indacaterol and glycopyrrolate should be administered at the same time of the day (1 capsule in the morning and 1 capsule in the evening) every day. More frequent administration or a greater number of inhalations (more than 1 capsule twice-daily) of indacaterol and glycopyrrolate is not recommended. Store indacaterol and glycopyrrolate capsules in the blister, and only remove IMMEDIATELY BEFORE USE with the NEOHALER device.
Monitoring
There is limited information regarding Indacaterol and glycopyrrolate Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Indacaterol and glycopyrrolate and IV administrations.
Overdosage
In COPD patients, doses of up to 600/124.8 mcg indacaterol and glycopyrrolate were inhaled over 2 weeks and there were no relevant effects on heart rate, QTc interval, blood glucose or serum potassium. There was an increase in ventricular ectopies after 14 days of dosing with 300/124.8 mcg and 600/124.8 mcg indacaterol and glycopyrrolate, but low prevalence and small patient numbers (N=49 and N=51 for 600/124.8 mcg and 300/124.8 mcg indacaterol and glycopyrrolate, respectively) precluded accurate analysis. In a total of four patients, non-sustained ventricular tachycardia was recorded, with the longest episode recorded being 9 beats (4 seconds).
In healthy volunteers, single dose administration of indacaterol and glycopyrrolate at up to a dose of 440/499.2 mcg indacaterol/glycopyrrolate was well-tolerated without clinically significant effects on the ECG, serum potassium or blood glucose.
Indacaterol and glycopyrrolate contains both indacaterol and glycopyrrolate; therefore, the risks associated with overdosage for the individual components described below apply to indacaterol and glycopyrrolate. Treatment of overdosage consists of discontinuation of indacaterol and glycopyrrolate together with institution of appropriate symptomatic and/or supportive therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medicine can produce bronchospasm. Cardiac monitoring is recommended in cases of overdosage.
Indacaterol: The potential signs and symptoms associated with overdosage of indacaterol are those of excessive beta-adrenergic stimulation and occurrence or exaggeration of any of the signs and symptoms, e.g., angina, hypertension or hypotension, tachycardia, with rates up to 200 bpm, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, muscle cramps, nausea, vomiting, drowsiness, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, metabolic acidosis and insomnia. As with all inhaled sympathomimetic medications, cardiac arrest and even death may be associated with an overdose of indacaterol.
In COPD patients, single doses of indacaterol 3000 mcg were associated with moderate increases in pulse rate, systolic blood pressure and QTc interval.
Glycopyrrolate: An overdose of glycopyrrolate may lead to anticholinergic signs and symptoms such as nausea, vomiting, dizziness, lightheadedness, blurred vision, increased intraocular pressure (causing pain, vision disturbances or reddening of the eye), obstipation or difficulties in voiding.
In COPD patients, repeated orally inhaled administration of glycopyrrolate at total doses of 124.8 mcg and 249.6 mcg once-daily for 28 days were well tolerated.
Peak plasma levels and total systemic exposure following intravenous administration of 150 mcg glycopyrrolate (equivalent to 120 mcg active moiety) in healthy volunteers were respectively about 270-fold and 13-fold higher than the peak and total systemic exposure at steady-state achieved with the recommended daily dose of 31.2 mcg of glycopyrrolate (i.e., 15.6 mcg glycopyrrolate twice-daily) and were well tolerated.
Pharmacology
Indacaterol and glycopyrrolate
| |
| Combination of | |
| Indacaterol | Ultra-long-acting beta-adrenoceptor agonist |
| Glycopyrronium bromide | Muscarinic anticholinergic |
| Identifiers | |
| CAS number | |
| ATC code | R03 |
| PubChem | |
| Therapeutic considerations | |
| Pregnancy cat. |
B3(AU) |
| Legal status |
Prescription Only (S4)(AU) POM(UK) Template:Unicode Prescription only |
| Routes | Inhalation only |
Mechanism of Action
Indacaterol and glycopyrrolate contains both indacaterol and glycopyrrolate. The mechanisms of action described below for the individual components apply to indacaterol and glycopyrrolate. These drugs represent 2 different classes of medications (a LABA and an anticholinergic) that have different and additive effects on clinical and physiological indices.
Indacaterol: Indacaterol is a long-acting beta2-adrenergic agonist (LABA). When inhaled, indacaterol acts locally in the lung as a bronchodilator. Although beta2-receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta1-receptors are the predominant receptors in the heart, there are also beta2-adrenergic receptors in the human heart comprising 10% to 50% of the total adrenergic receptors. The precise function of these receptors is not known, but their presence raises the possibility that even highly selective beta2-adrenergic agonists may have cardiac effects.
The pharmacological effects of beta2-adrenoceptor agonist drugs, including indacaterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3’, 5’-adenosine monophosphate (cyclic monophosphate). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells. In vitro studies have shown that indacaterol has more than 24-fold greater agonist activity at beta2-receptors compared to beta1-receptors and 20-fold greater agonist activity compared to beta3-receptors. The clinical significance of these findings is unknown.
Glycopyrrolate: Glycopyrrolate is a long-acting muscarinic antagonist, which is often referred to as an anticholinergic. It has similar affinity to the subtypes of muscarinic receptors M1 to M5. In the airways, it exhibits pharmacological effects through inhibition of M3 receptor at the smooth muscle leading to bronchodilation. The competitive and reversible nature of antagonism was shown with human and animal origin receptors and isolated organ preparations. In preclinical in vitro as well as in vivo studies, prevention of methacholine-induced broncho-constrictive effects was dose-dependent and lasted longer than 24 hours. The clinical relevance of these findings is unknown. The bronchodilation following inhalation of glycopyrrolate is predominantly a site-specific effect.
Structure
Indacaterol maleate is a selective beta2-adrenergic agonist. Its chemical name is (R)-5-[2-(5,6-Diethylindan-2-ylamino)-1-hydroxyethyl]-8-hydroxy-1H-quinolin-2-one maleate; its structural formula is:
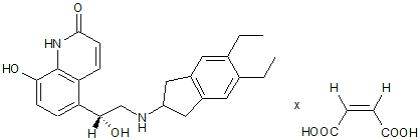
Indacaterol maleate has a molecular weight of 508.56, and its empirical formula is C24H28N2O3 • C4H4O4. Indacaterol maleate is a white to very slightly grayish or very slightly yellowish powder. Indacaterol maleate is slightly soluble in ethanol and very slightly soluble in water.
Glycopyrrolate is chemically described as (3RS)-3-[(2SR)-(2-cyclopentyl-2-hydroxy-2-phenylacetyl) oxy]-1,1-dimethylpyrrolidinium bromide. This synthetic quaternary ammonium compound acts as a competitive antagonist at muscarinic acetylcholine receptors, also referred to as anticholinergic. Glycopyrrolate, C19H28BrNO3, is a white powder that is freely soluble in water and sparingly soluble in absolute ethanol. It has a molecular mass of 398.33. The structural formula is:
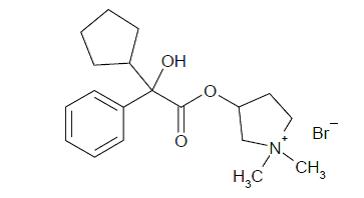
Pharmacodynamics
Cardiac Electrophysiology
The QTc interval was studied in TQT studies with indacaterol and glycopyrrolate and with each of the monotherapy components. The TQT studies with indacaterol and glycopyrrolate demonstrated that neither of the compounds had a relevant effect on the corrected QT interval at supratherapeutic and therapeutic doses (for glycopyrrolate only a supratherapeutic dose was tested).
In a randomized, partially-blinded, placebo- and positive-controlled, crossover TQT study in 84 healthy subjects a supratherapeutic dose of indacaterol and glycopyrrolate (indacaterol/glycopyrrolate 440/499.2 mcg) was administered. This is a 16/32 dose multiple compared to a single dose of the recommended 27.5/15.6 mcg twice-daily dosage of indacaterol and glycopyrrolate which resulted in exposure multiples for mean Cmax of 9.3 for indacaterol and 35.2 for glycopyrrolate compared to steady-state pharmacokinetics of indacaterol and glycopyrrolate 27.5/15.6 mcg twice-daily. The mean maximal change from baseline in QTcI compared to placebo was 8.70 msec (2-sided 90% CI 7.3, 10.1) at 30 minutes after dosing. Although a marginal QT effect of indacaterol and glycopyrrolate was observed at the supratherapeutirapeutic exposure.
Pharmacokinetics
Absorption
Following inhalation of indacaterol and glycopyrrolate, the median time to reach peak plasma concentrations of indacaterol and glycopyrrolate was achieved rapidly at approximately 15 minutes and 5 minutes, respectively.
The steady-state systemic exposure (AUC0-12h,ss; Cmax,ss) to indacaterol and glycopyrrolate is similar after the twice-daily inhalation of 2 (times 2) capsules of indacaterol and glycopyrrolate 27.5 mcg/15.6 mcg as compared to the twice-daily inhalation of the monotherapy products indacaterol 27.5 mcg (times 2) alone or glycopyrrolate 15.6 mcg (times 2) alone respectively.
Indacaterol: Absolute bioavailability of indacaterol after an inhalation dose was on average 43% to 45%. Systemic exposure results from a composite of pulmonary and intestine absorption. Indacaterol serum concentrations increased with repeated once-daily administration. Steady-state was achieved within 12 to 15 days. The mean accumulation ratio of indacaterol, i.e., AUC over the 24-hour dosing interval on Day 14 or Day 15 compared to Day 1, was in the range of 2.9 to 3.8 for once-daily inhaled doses between 75 mcg and 600 mcg.
Glycopyrrolate: Following repeated once-daily inhalation in patients with COPD, pharmacokinetic steady-state of glycopyrrolate was reached within 1 week of treatment. There was no indication that the glycopyrrolate pharmacokinetics changes over time. With once-daily doses of 124.8 mcg and 249.6 mcg, steady-state exposure to glycopyrrolate (AUC over the dosing interval) was about 1.4- to 1.7-fold higher than after the first dose.
Distribution
Indacaterol: After intravenous infusion, the volume of distribution (Vz) of indacaterol was 2,361 to 2,557 L, indicating an extensive distribution. The in vitro human serum and plasma protein binding was 94.1% to 95.3% and 95.1% to 96.2%, respectively.
Glycopyrrolate: After intravenous administration, the steady-state volume of distribution (Vss) of glycopyrrolate was 83 L and the volume of distribution in the terminal phase (Vz) was 376 L. The in vitro human plasma protein binding of glycopyrrolate was 38% to 41% at concentrations of 1 to 10 ng/mL.
Indacaterol: In vitro investigations indicated that UGT1A1 is the only UGT isoform that metabolized indacaterol to the phenolic O-glucuronide. The oxidative metabolites were found in incubations with recombinant CYP1A1, CYP2D6, and CYP3A4. CYP3A4 is concluded to be the predominant isoenzyme responsible for hydroxylation of indacaterol. In vitro investigations further indicated that indacaterol is a low affinity substrate for the efflux pump P-gp.
After oral administration of radiolabelled indacaterol in a human ADME (absorption, distribution, metabolism, excretion) study, unchanged indacaterol was the main component in serum, accounting for about one-third of total drug-related AUC over 24 hours. A hydroxylated derivative was the most prominent metabolite in serum. Phenolic O-glucuronides of indacaterol and hydroxylated indacaterol were further prominent metabolites. A diastereomer of the hydroxylated derivative, a N-glucuronide of indacaterol, and C- and N-dealkylated products were further metabolites identified.
Glycopyrrolate: In vitro metabolism studies show glycopyrrolate hydroxylation resulting in a variety of mono- and bis-hydroxylated metabolites and direct hydrolysis resulting in the formation of a carboxylic acid derivative (M9). Further in vitro investigations showed that multiple CYP isoenzymes contribute to the oxidative biotransformation of glycopyrrolate and the hydrolysis to M9 is likely to be catalyzed by members from the cholinesterase family pre-systemically and/or via first pass metabolism from the swallowed dose fraction of orally inhaled glycopyrrolate. Glucuronide and/or sulfate conjugates of glycopyrrolate were found in urine of humans after repeated inhalation, accounting for about 3% of the dose.
Elimination:
Indacaterol: In clinical studies which included urine collection, the amount of indacaterol excreted unchanged via urine was generally lower than 2% of the dose. Renal clearance of indacaterol was, on average, between 0.46 L/h and 1.20 L/h. When compared with the serum clearance of indacaterol of 18.8 L/h to 23.3 L/h, it is evident that renal clearance plays a minor role (about 2% to 6% of systemic clearance) in the elimination of systemically available indacaterol.
In a human ADME study where indacaterol was given orally, the fecal route of excretion was dominant over the urinary route. Indacaterol was excreted into human feces primarily as unchanged parent drug (54% of the dose) and, to a lesser extent, hydroxylated indacaterol metabolites (23% of the dose). Mass balance was complete with greater than or equal to 90% of the dose recovered in the excreta.
Indacaterol serum concentrations declined in a multi-phasic manner with an average terminal half-life ranging from 45.5 to 126 hours. The effective half-life, calculated from the accumulation of indacaterol after repeated dosing ranged from 40 to 56 hours which is consistent with the observed time to steady-state of approximately 12 to 15 days.
Glycopyrrolate: Renal elimination of parent drug accounts for about 60% to 70% of total clearance of systemically available glycopyrrolate whereas non-renal clearance processes account for about 30% to 40%. Biliary clearance contributes to the non-renal clearance, but the majority of non-renal clearance is thought to be due to metabolism.
Following inhalation of single and repeated once-daily doses between 62.4 mcg and 249.6 mcg glycopyrrolate by healthy volunteers and patients with COPD, mean renal clearance of glycopyrrolate was in the range of 17.4 L/h and 24.4 L/h. Active tubular secretion contributes to the renal elimination of glycopyrrolate.
Glycopyrrolate plasma concentrations declined in a multi-phasic manner. The mean terminal elimination half-life of glycopyrrolate was much longer after inhalation (33 to 53 hours) than after intravenous (6.2 hours) and oral (2.8 hours) administration.
Drug Interactions:
There is no pharmacokinetic drug-drug interaction resulting from the concomitant administration of inhaled glycopyrrolate and inhaled indacaterol based on steady-state exposure data.
No specific drug-drug interaction studies were conducted with indacaterol and glycopyrrolate. Information on the potential for interactions for indacaterol and glycopyrrolate is based on the potential for each of its 2 monotherapy components.
Effect of co-administered drugs on indacaterol and glycopyrrolate exposure:
Inhibitors of Cytochrome P450 3A4 and P-gp Efflux Transporter: Drug interaction studies were carried out using potent and specific inhibitors of CYP3A4 and P-gp (i.e., ketoconazole, erythromycin, verapamil and ritonavir). Coadministration of indacaterol 300 mcg (single dose) with verapamil (80 mg 3 times a day for 4 days) showed 2-fold increase in indacaterol AUC0-24h, and 1.5-fold increase in indacaterol Cmax. Coadministration of indacaterol inhalation powder 300 mcg (single dose) with erythromycin (400 mg 4 times a day for 7 days) showed a 1.4-fold increase in indacaterol AUC0-24h, and 1.2-fold increase in indacaterol Cmax. Coadministration of indacaterol inhalation powder 300 mcg (single dose) with ketoconazole (200 mg twice-daily for 7 days) caused a 1.9-fold increase in indacaterol AUC0-24h, and 1.3-fold increase in indacaterol Cmax. Coadministration of indacaterol 300 mcg (single dose) with ritonavir (300 mg twice-daily for 7.5 days) resulted in a 1.7-fold increase in indacaterol AUC0-24h whereas indacaterol Cmax was unaffected.
Glycopyrrolate: Cimetidine or Other Inhibitors of Organic Cationic Transport: In a clinical study in healthy volunteers, cimetidine, an inhibitor of organic cation transport which is thought to contribute to the renal excretion of glycopyrrolate, increased total exposure (AUC) to glycopyrrolate by 22% and decreased renal clearance by 23%.
Effect of indacaterol and glycopyrrolate on co-administered drugs exposure:
In vitro studies show that indacaterol and glycopyrrolate is not likely to inhibit or induce the metabolism of other drugs, nor processes involving drug transporters.
Indacaterol: In vitro investigations indicated that indacaterol has negligible potential to cause metabolic interactions with medications (by inhibition or induction of cytochrome P450 enzymes, or induction of UGT1A1) at the systemic exposure levels achieved in clinical practice. In vitro investigation furthermore indicated that, in vivo, indacaterol is unlikely to significantly inhibit transporter proteins such as P-gp, MRP2, BCRP, the cationic substrate transporters hOCT1 and hOCT2, and the human multidrug and toxin extrusion transporters hMATE1 and hMATE2K, and that indacaterol has negligible potential to induce P-gp or MRP2.
Glycopyrrolate: In vitro inhibition studies demonstrated that glycopyrrolate has no relevant capacity to inhibit CYP1A2, CYP2A6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A4/5, the efflux transporters MDR1, MRP2 or MXR, and the uptake transporters OATP1B1, OATP1B3, OAT1, OAT3, OCT1 or OCT2. In vitro enzyme induction studies did not indicate a clinically relevant induction by glycopyrrolate for any of the cytochrome P450 isoenzymes tested as well as for UGT1A1 and the transporters MDR1 and MRP2.
Specific Populations:
Population pharmacokinetic analysis showed no evidence of a clinically significant effect of age (40 to 85 years), body weight (45 to 120 kg), gender, smoking status, and baseline FEV1 on systemic exposure of either indacaterol or glycopyrrolate following inhalation of indacaterol and glycopyrrolate.
Similarly no relevant covariate effect (of age, body weight, gender, smoking status, and baseline FEV1) was observed following the inhalation of the 2 components indacaterol and glycopyrrolate separately.
Patients with Renal Impairment:
Indacaterol: Due to the very low contribution of the urinary pathway to total body elimination of indacaterol, a study in renally impaired subjects was not performed.
Glycopyrrolate: Renal impairment has an impact on the systemic exposure to glycopyrrolate. A moderate mean increase in total systemic exposure (AUC last) of up to 1.4-fold was seen in subjects with mild and moderate renal impairment [estimated GFR greater than or equal to 30 mL/min/1.73m2] and up to 2.2-fold in subjects with severe renal impairment and end stage renal disease [estimated GFR less than 30 mL/min/1.73m2].
Patients with Hepatic Impairment:
Based on the clinical pharmacokinetic characteristics of its monotherapy components, indacaterol and glycopyrrolate can be used at the recommended dose in patients with mild and moderate hepatic impairment. Indacaterol and glycopyrrolate has not been evaluated in subjects with severe hepatic impairment.
Indacaterol: Patients with mild and moderate hepatic impairment showed no relevant changes in Cmax or AUC of indacaterol, nor did protein binding differ between mild and moderate hepatic impaired subjects and their healthy controls. Studies in subjects with severe hepatic impairment were not performed.
Glycopyrrolate: Clinical studies in patients with hepatic impairment have not been conducted. Glycopyrrolate is cleared predominantly from the systemic circulation by renal excretion.
Ethnicity:
There was no evidence of a clinically significant ethnic/race effect (across Caucasian, Chinese, and Japanese subjects) on the systemic exposure to indacaterol and glycopyrrolate following inhalation of indacaterol and glycopyrrolate. Similarly, no relevant ethnic effect was observed following the inhalation of the 2 components indacaterol and glycopyrrolate separately.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies of carcinogenicity, mutagenicity, or impairment of fertility were conducted with indacaterol and glycopyrrolate; however, studies are available for the individual components, indacaterol and glycopyrrolate, as described below.
Indacaterol: Indacaterol produced no treatment-related increases in the incidence of tumors in a 2-year inhalation study in Wistar rats at inhaled doses up to 2.09 mg/kg/day (approximately 110 times the MRHD in adults on an AUC basis, respectively). A 26-week oral (gavage) study in CB6F1/TgrasH2 hemizygous mice with indacaterol at doses up to 600 mg/kg/day did not show any evidence of tumorigenicity. Indacaterol tested negative in the following genotoxicity assays: the in vitro Ames test, in vitro chromosome aberration test in V79 Chinese hamster cells, and in vivo rat bone marrow micronucleus test. Indacaterol had no effects on fertility and reproductive performance in male and female rats at subcutaneous doses up to 2 mg/kg/day (approximately 890 and 670 times in males and females, respectively, the MRHD in adults on an AUC basis).
Glycopyrrolate: Glycopyrrolate produced no treatment-related increases in the incidence of tumors in a 2-year inhalation study in Wistar rats at inhaled doses up to 0.56 mg/kg/day (approximately 170 times the MRHD in adults on an AUC basis). A 26-week oral (gavage) study in male and female TgrasH2 mice that received glycopyrrolate at doses up to 93.8 and 125.1 mg/kg/day, respectively, did not show any evidence of tumorigenicity. Glycopyrrolate tested negative in the following genotoxicity assays: the in vitro Ames assay, in vitro human lymphocyte chromosomal aberration assay, and in vivo rat bone marrow micronucleus assay. Impairment of fertility was observed in male and female rats at a subcutaneous dose of 1.88 mg/kg/day (approximately 1900 and 1100 times the MRHD in adults on an AUC basis, respectively) based upon findings of decreased corpora lutea, implantation sites and live fetuses. No effects on fertility and reproductive performance in male and female rats were observed at a subcutaneous dose of 0.63 mg/kg/day (approximately 350 times the MRHD in adults on an AUC basis).
Animal Toxicology:
Eye findings were seen for glycopyrrolate and were observed in Wistar rats at inhaled doses of 0.67 mg/kg/day and higher (approximately 280 times the MRHD in adults on an AUC basis) based upon findings of anterior capsule opacity, prominent anterior suture line, and anterior cataract. No eye findings in Wistar rats were observed at an inhaled dose of 0.09 mg/kg/day (approximately 60 times the MRHD in adults on an AUC basis). Eye findings were observed in beagle dogs at an inhaled dose of 0.33 mg/kg/day (approximately 150 times the MRHD in adults on an AUC basis) based upon findings of conjunctival hyperemia and corneal opacity. No eye findings in beagle dogs were observed at an inhaled dose of 0.12 mg/kg/day (approximately 100 times the MRHD in adults on an AUC basis).
Clinical Studies
The safety and efficacy of indacaterol and glycopyrrolate were evaluated in a clinical development program that included 3 dose-ranging trials, 2 lung function trials of 12 weeks duration (placebo-controlled and active-controlled) and a 12-month long-term safety trial. The efficacy of indacaterol and glycopyrrolate is based primarily on the dose-ranging trials in 562 subjects with COPD or asthma and the 2 placebo- and active-controlled confirmatory trials in 2043 subjects with additional support from one active-controlled 12-month trial in 615 subjects with COPD.
Dose-Ranging Trials:
Dose selection for indacaterol and glycopyrrolate for COPD was based on data for the individual components.
Indacaterol: Indacaterol dose selection in indacaterol and glycopyrrolate is based on the registered dose of 75 mcg once-daily and is also supported by a single-dose, multicenter, randomized, double-blind, placebo-controlled, crossover study in asthma evaluating 5 doses of indacaterol in 91 subjects, (37.5 mcg, 55 mcg, 75 mcg, and 150 mcg once-daily (QD), and 27.5 mcg twice-daily (BID)). A dose-related increase in FEV1 AUC0-24h compared with placebo was observed. The differences in change from baseline in FEV1 AUC0-24h after single dosing for the indacaterol 37.5 mcg, 55 mcg, 75 mcg, and 150 mcg once-daily and the 27.5 mcg twice-daily doses compared to placebo were 0.099 L (95% CI: 0.069, 0.128), 0.132 L (0.103, 0.162), 0.143 L (0.114, 0.171), 0.187 L (0.157, 0.216), and 0.121 L (0.092, 0.151), respectively. These results supported the evaluation of indacaterol 27.5 mcg twice-daily in the confirmatory COPD trials. Indacaterol and glycopyrrolate is not indicated for asthma.
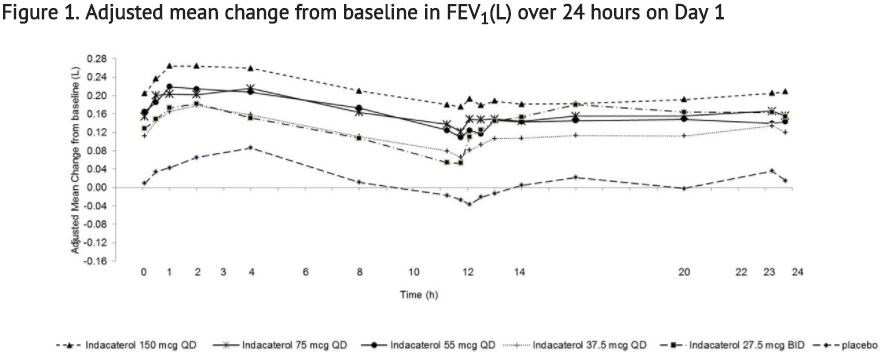
Glycopyrrolate: Dose selection for glycopyrrolate in indacaterol and glycopyrrolate in COPD was supported by a 28-day, randomized, double-blind, placebo-controlled, 2-period, crossover study evaluating 7 doses of glycopyrrolate (15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily) or placebo in 388 subjects with COPD. The differences in trough FEV1 from baseline after 28 days compared to placebo for the 15.6 mcg, 31.2 mcg, 62.4 mcg, and 124.8 mcg once-daily and for 15.6 mcg, 31.2 mcg, and 62.4 mcg twice-daily doses were 0.083 L (95% CI: 0.030, 0.136), 0.098 L (0.048, 0.148), 0.090 L (0.038, 0.142), 0.176 L (0.132, 0.220), 0.139 L (0.089, 0.189), 0.167 L (0.115, 0.219), and 0.177 L (0.132, 0.222), respectively. The dose-ranging results supported the evaluation of glycopyrrolate 15.6 mcg twice-daily in the confirmatory COPD trials.
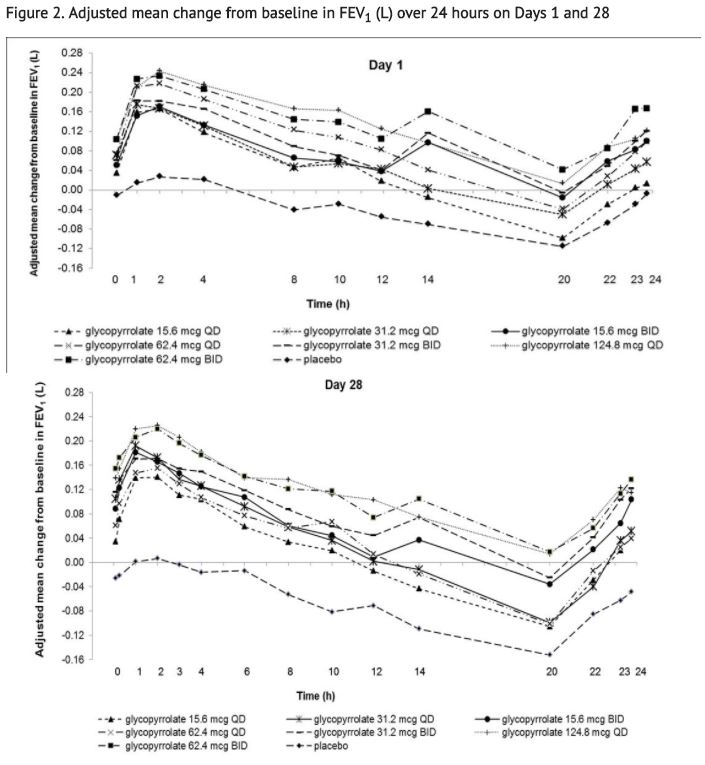
Based on the findings from dose-ranging studies of the individual components, a twice-daily dose of indacaterol/glycopyrrolate 27.5 mcg/15.6 mcg was evaluated in the confirmatory COPD trials.
Confirmatory Trials:
The clinical development program for indacaterol and glycopyrrolate included two (Trial 1 and Trial 2) 12-week, randomized, double-blinded, placebo- and active-controlled, parallel-group trials in subjects with COPD designed to evaluate the efficacy and safety of indacaterol and glycopyrrolate; and one 12-month, randomized, double-blind, active-controlled trial (Trial 3) that evaluated bronchodilation and effects on long-term safety.
The 12-week trials evaluated the efficacy of 2038 subjects that had a clinical diagnosis of COPD, were 40 years of age or older, had a history of smoking greater than 10 pack-years, had a post-albuterol FEV1 greater than or equal to 30% and less than 80% of predicted normal values, had a ratio of FEV1/FVC of less than 0.7, and were symptomatic as determined by a Modified Medical Research Council (mMRC) score greater than or equal to 2. Of the 2038 subjects included in the efficacy analysis, 63% were male and 91% were Caucasian. They had a mean age of 63 years and an average smoking history of 47 pack-years, with 52% identified as current smokers, and 46% used concomitant inhaled corticosteroids. At screening, the mean post-bronchodilator percent predicted FEV1 was 55% (range: 29% to 79%), the mean post-bronchodilator FEV1/FVC ratio was 50% (range: 19% to 71%), and the mean percent reversibility was 23% (range: 0% to 144%).
Trial 1 and Trial 2 evaluated indacaterol and glycopyrrolate 27.5 mcg/15.6 mcg twice-daily (BID), indacaterol 27.5 mcg BID, glycopyrrolate 15.6 mcg BID, and placebo BID. The primary endpoint was the change from baseline in FEV1 AUC0-12h following the morning dose at Day 85 (defined as the mean FEV1 change from baseline over 0 to 12 hours divided by 12 hours) compared with placebo, glycopyrrolate 15.6 mcg BID, and indacaterol 27.5 mcg BID. The comparison of indacaterol and glycopyrrolate with indacaterol 27.5 mcg and glycopyrrolate 15.6 mcg was assessed to evaluate the contribution of the individual comparators to indacaterol and glycopyrrolate. In both trials, indacaterol and glycopyrrolate demonstrated a larger increase in mean change from baseline in FEV1 AUC0-12h compared to placebo, indacaterol 27.5 mcg BID, and glycopyrrolate 15.6 mcg BID (see Table 2).
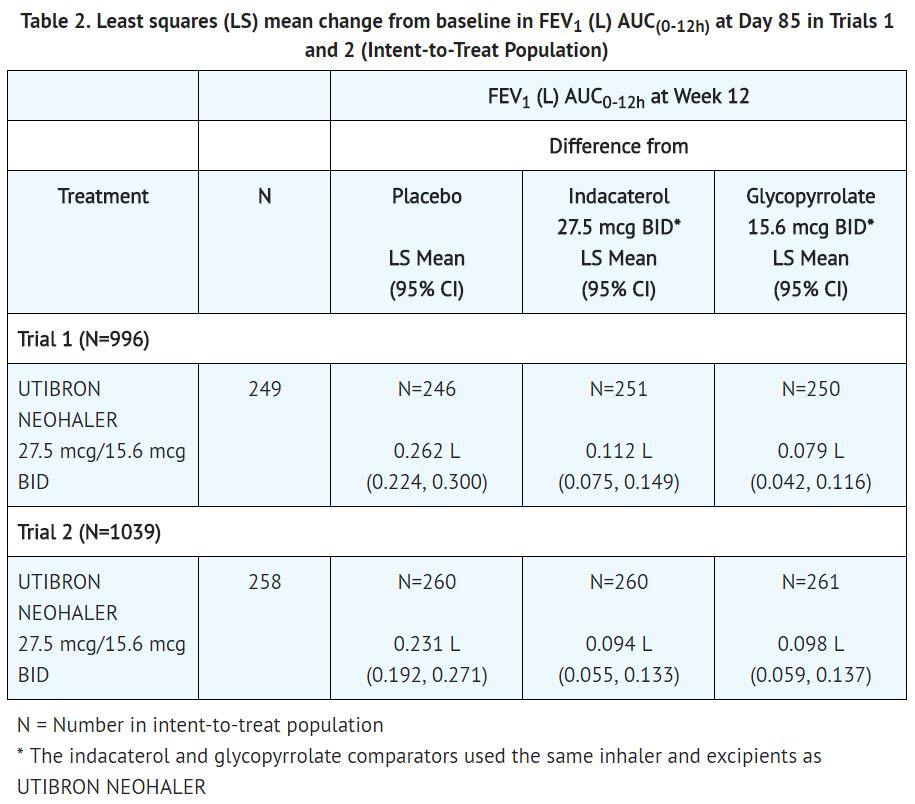
With the limited data available, there was no suggestion of a difference in FEV1 AUC0-12h with respect to age, sex, degree of airflow limitation, GOLD stage, smoking status, or inhaled corticosteroid use.
In Trial 1 and Trial 2, serial spirometric evaluations throughout the 12-hour dosing interval were performed in all subjects at Days 1 and 85. The spirometric curves from Trial 1 at Days 1 and 85 are displayed in Figure 3. In Trial 2, the results for indacaterol and glycopyrrolate in FEV1 AUC0-12h were similar to those observed in Trial 1.
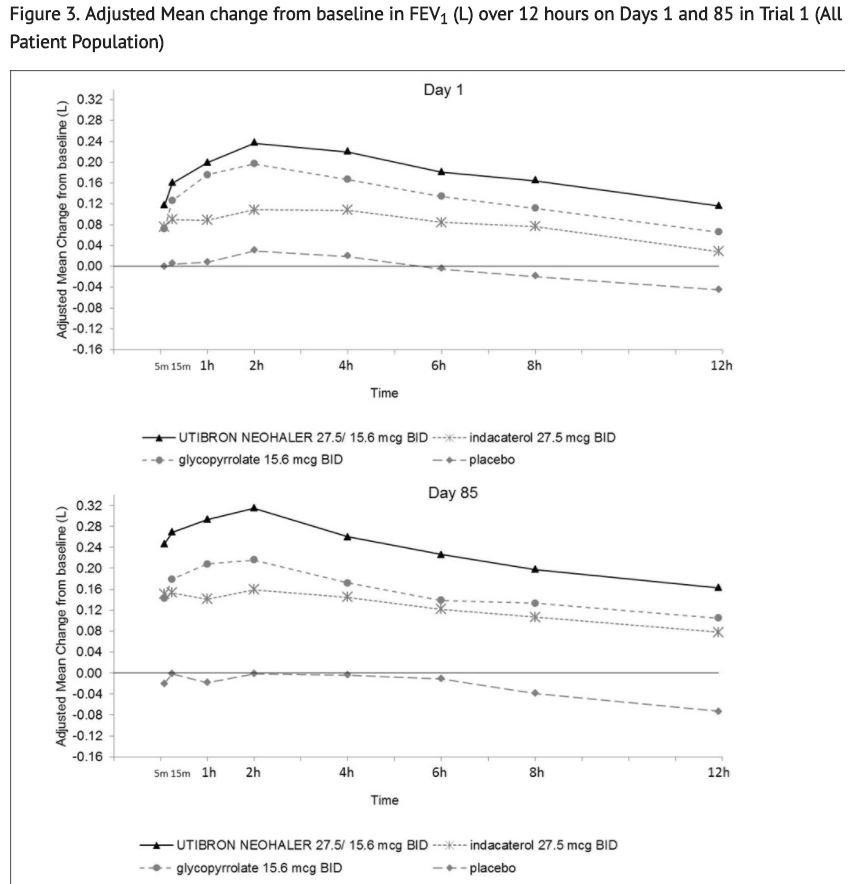
The peak FEV1 was defined as the maximum FEV1 recorded within 4 hours after the morning dose on Days 1 and 85. The mean peak FEV1 improvement from baseline for indacaterol and glycopyrrolate compared with placebo at Day 1 and at Day 85 was 0.185 L and 0.290 L (Trial 1) and 0.151 L and 0.260 L (Trial 2), respectively. The median time to onset on Day 1, defined as a 100 mL increase from baseline in FEV1, was 12 minutes and 16 minutes in Trials 1 and 2, respectively, in subjects receiving indacaterol and glycopyrrolate.
In Trials 1 and 2, patients treated with indacaterol and glycopyrrolate used less daily rescue albuterol compared to patients treated with placebo.
The St. George’s Respiratory Questionnaire (SGRQ) was assessed in Trials 1 and 2. In Trial 2, the SGRQ responder rate (defined as an improvement in score of 4 or more as threshold) was 57%, 46%, 48%, and 39%, for indacaterol and glycopyrrolate, glycopyrrolate, indacaterol, and placebo, respectively, with odds ratios of 1.6 (95% CI 1.1, 2.3), 1.5 (95% CI 1.1, 2.2), and 2.2 (95% CI 1.5, 3.2), for indacaterol and glycopyrrolate vs. glycopyrrolate, indacaterol and glycopyrrolate vs. indacaterol, and indacaterol and glycopyrrolate vs. placebo, respectively. In Trial 1, the trends were similar, with odds ratios of 1.4 (95% CI 1.0, 2.0), 1.1 (95% CI 0.8, 1.7), and 2.9 (95% CI 1.9, 4.2), for indacaterol and glycopyrrolate vs. glycopyrrolate, indacaterol and glycopyrrolate vs. indacaterol, and indacaterol and glycopyrrolate vs placebo, respectively.
52-week Effects on Lung Function: At week 52 (Trial 3), indacaterol and glycopyrrolate demonstrated a significant treatment effect with an increase of 0.080 L in pre-dose trough FEV1 compared to indacaterol 75 mcg once-daily.
How Supplied
Indacaterol and glycopyrrolate contains indacaterol and glycopyrrolate (indacaterol/glycopyrrolate, (27.5 mcg, 15.6 mcg) inhalation powder) in hypromellose (HPMC) capsule with yellow transparent cap and uncolored transparent body, with capsules packaged in aluminum blister cards, one NEOHALER device, and an FDA approved Medication Guide.
- Unit Dose (blister pack), Box of 60 (10 blister cards with 6 yellow transparent capsules each) NDC 0078-0664-19
- Unit Dose (blister pack), Box of 6 (1 blister card with 6 yellow transparent capsules each) NDC 0078-0664-06
The NEOHALER device consists of a white protective cap and a base with mouthpiece, capsule chamber and 2 yellow push buttons.
Storage
Store in a dry place at 77°F (25°C); excursions permitted to 59°F to 86°F (15°C to 30°C). Indacaterol and glycopyrrolate capsules should be used with the NEOHALER device only. Do not use the NEOHALER device with any other capsules. Store indacaterol and glycopyrrolate capsules in the blister protected from light and moisture. Remove the indacaterol and glycopyrrolate capsules from the blister immediately before use. Always use the new NEOHALER inhaler provided with each new prescription. Keep out of the reach of children.
Images
Drug Images
{{#ask: Page Name::Indacaterol and glycopyrrolate |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
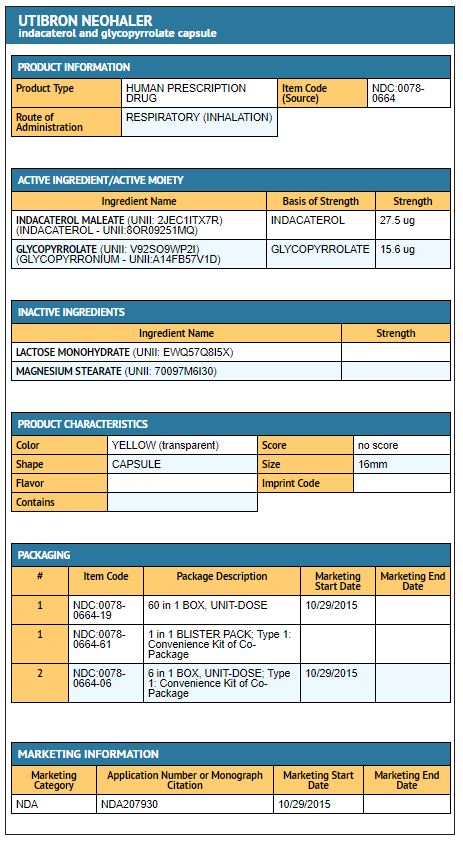
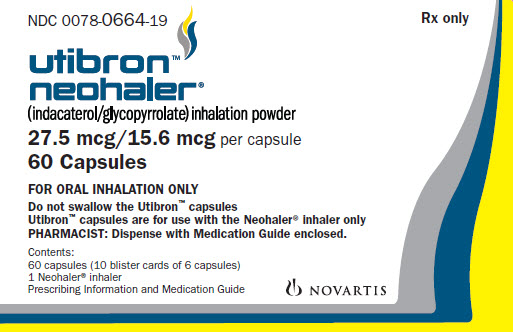
{{#ask: Label Page::Indacaterol and glycopyrrolate |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
- Asthma-Related Death
- Inform patients that LABAs, such as indacaterol, one of the active ingredients in indacaterol and glycopyrrolate, increase the risk of asthma-related death. Indacaterol and glycopyrrolate is not indicated for the treatment of asthma.
- Not for Acute Symptoms
- Inform patients that indacaterol and glycopyrrolate is not meant to relieve acute symptoms of COPD and extra doses should not be used for that purpose. Advise them to treat acute symptoms with a rescue inhaler such as albuterol. Provide patients with such medicine and instruct them on how it should be used.
- Instruct patients to seek medical attention immediately if they experience any of the following:
- Symptoms get worse
- Need for more inhalations than usual of their rescue inhaler
- Patients should not stop therapy with indacaterol and glycopyrrolate without physician/healthcare provider guidance since symptoms may recur after discontinuation.
- Do Not Use Additional Long-Acting Beta2-Agonists
- Instruct patients to not use other medicines containing a LABA. Patients should not use more than the recommended twice-daily dose of indacaterol and glycopyrrolate.
- Instruct patients who have been taking inhaled, short-acting beta2-agonists on a regular basis to discontinue the regular use of these products and use them only for the symptomatic relief of acute symptoms.
- Paradoxical Bronchospasm
- Inform patients that indacaterol and glycopyrrolate can produce paradoxical bronchospasm. Advise patients that if paradoxical bronchospasm occurs, patients should discontinue indacaterol and glycopyrrolate.
- Risks Associated with Beta2-Agonist Therapy
- Inform patients of adverse effects associated with beta2-agonists, such as palpitations, chest pain, rapid heart rate, tremor, or nervousness. Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
- Worsening of Narrow-Angle Glaucoma
- Instruct patients to be alert for signs and symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion and corneal edema). Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
- Worsening of Urinary Retention
- Instruct patients to be alert for signs and symptoms of urinary retention (e.g., difficulty passing urine, painful urination). Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
- Instructions for Administering Indacaterol and Glycopyrrolate
- It is important for patients to understand how to correctly administer indacaterol and glycopyrrolate capsules using the NEOHALER device.
- Instruct patients that indacaterol and glycopyrrolate capsules should only be administered via the NEOHALER device and the NEOHALER device should not be used for administering other medications.
- Remind patients that the contents of indacaterol and glycopyrrolate capsules are for oral inhalation only and must not be swallowed.
- Instruct patients always to store indacaterol and glycopyrrolate capsules in sealed blisters and to only remove 1 indacaterol and glycopyrrolate capsule immediately before use or it may not be as effective. Instruct patients to discard unused additional indacaterol and glycopyrrolate capsules that are exposed to air (i.e., not intended for immediate use).
- Inform patients to use 1 inhalation of indacaterol and glycopyrrolate orally twice-daily (1 capsule in the morning and 1 capsule in the evening) at the same time every day.
- Inform patients that if they miss a dose of indacaterol and glycopyrrolate, they should use their next capsule at the usual time. Instruct patients to not use 2 capsules at one time and to not use more than 2 capsules in a day.
Precautions with Alcohol
Alcohol-Indacaterol and glycopyrrolate interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Indacaterol and glycopyrrolate Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Indacaterol and glycopyrrolate Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.