Cardiac amyloidosis: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 15:23, 30 April 2010
For patient information click here
| Cardiac amyloidosis | |
 | |
|---|---|
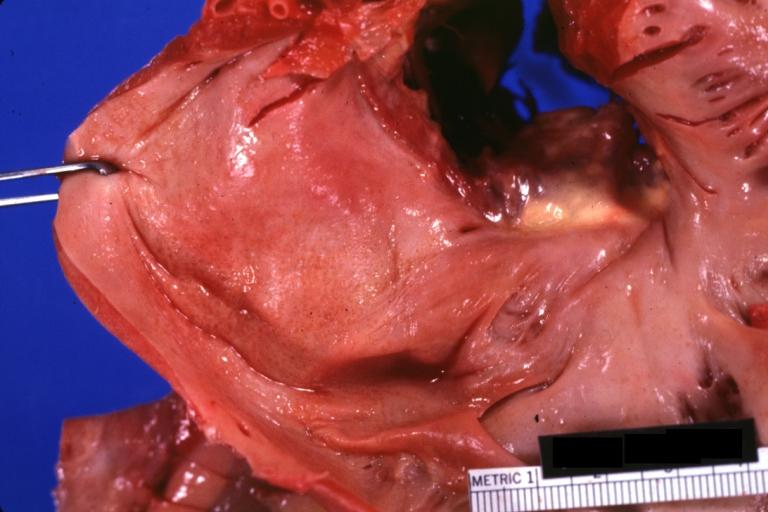
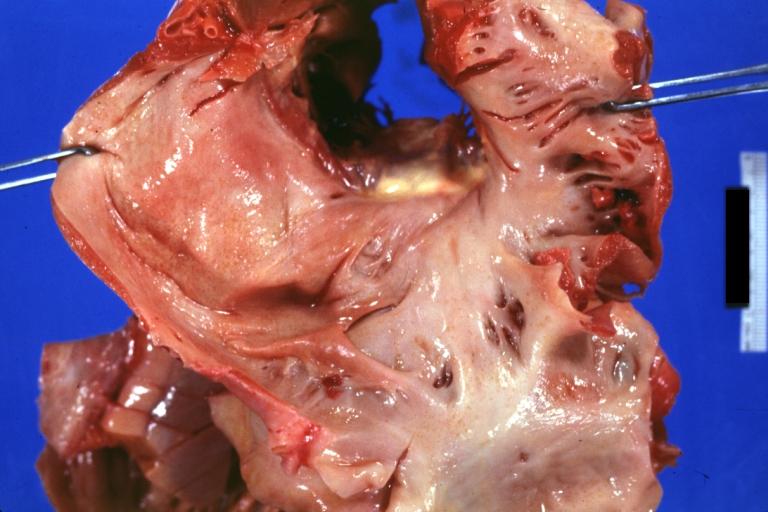
| Amyloidosis Lesion In Left Atrium: Gross natural color view of a diagnostic lesion Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-9 | 277.3 |
| eMedicine | med/3365 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Cardiac amyloidosis is a well-known condition, which has been reported with varying incidence rates. Myocardial involvement results in severe dysfunction and is the leading cause of death in patients with amyloidosis. Systemic amyloidosis of AL and TTR type is often associated with amyloid deposition in heart valves, in addition to blood vessels and myocardium [1] [2] In this classical type of valvular amyloidosis are the deposits occur in previously unaltered valves.
There is also another type of cardiac amyloidosis restricted entirely to the heart valves and can be found in valves, surgically removed for chronic valvular disease. The deposits are small and restricted to the areas of scarring and calcification.[3] The amyloid protein has not been identified but it has been demonstrated not to be AL or AA [4] [5]
Causes
Amyloidosis is the buildup of a fibril called amyloid in any tissue in the body. Fibrils are proteins produced in excess and slowly deposited where they replace normal tissue.
Different types of amyloidosis are caused by different types of proteins, such as "AL" and "AA." In cardiac amyloidosis there may be associated conduction disturbances (changes in the way the cardiac electrical impulse is transmitted through the heart).
Cardiac amyloidosis usually occurs during primary (AL) amyloidosis. Primary amyloidosis usually accompanies multiple myeloma, a blood disorder in which too much of a certain type of protein is produced. This excess protein is deposited in the heart and in other organs such as the kidney. Deteriorating kidney function also occurs.
The heart is less often compromised by secondary (AA) amyloidosis. A type of secondary amyloidosis that involves the heart is senile amyloidosis. It is caused by overproduction of a protein different from both the AA and AL types. This protein is deposited mainly in the heart, but can also infiltrate blood vessels. Senile cardiac amyloidosis is becoming more common as the average age of the population increases.
Cardiac amyloidosis is the most typical restrictive cardiomyopathy, and it is also known as “stiff heart syndrome.” Much less frequently, cardiac amyloidosis leads to dilated cardiomyopathy.
Several lines of evidence indicate that the degree of myocardial dysfunction does not depend only on the extent of amyloid deposits but also on the biochemical characteristics of the amyloidogenic proteins which dictate the aggregation process.[6] [7]
Cardiac amyloidosis is more common in men than in women.
Symptoms
Signs and tests
Cardiac amyloidosis is difficult to diagnose. The findings from an examination are not specific and may indicate enlargement of the heart and fluid retention in the lungs. Auscultation may reveal rales, heart murmurs, and/or other pathologic heart sounds. Hepatomegaly and elevated jugular pressure may occur. The blood pressure may be low or may drop when rising to a standing position (orthostatic hypotension). Orthostatic hypotension is typical especially in kidney involvement.
Cardiomegaly, congestion of the lungs or the veins in the lungs, decreased movement and/or functioning of the heart, heart failure, or signs of amyloidosis in the heart and other organs may show on the following tests:
- Echocardiogram
- Chest x-ray
- Thoracoabdominal CT scan
- Coronary angiography
- Nuclear cardiac scans: MUGA and Radionuclide ventriculography (RNV)
- Magnetic resonance imaging (MRI)
EKG may reveal conduction disturbances, arrhythmias such as atrial fibrillation, ventricular tachycardia, or premature and ectopic beats.
An echocardiogram may be used to assess the thickness of the heart wall, the size of the chambers in the heart, and the ability of the heart to fill and pump blood. Sometimes an unusual texture of the heart muscle or the endocardium (the lining of the heart) can be seen as well.
A cardiac biopsy that reveals amyloid confirms the diagnosis. Biopsy of other tissues may also confirm the diagnosis. Amyloidosis is frequently confirmed by biopsy of abdominal fat, kidney, or bone marrow.
Treatment
Physical activity may continue as long as the patient can tolerate it. Diet restrictions vary with the extent of cardiomyopathy and heart failure. These may include salt and/or fluid restrictions.
Diuretics (water pills) may be given to remove excess fluid. Digoxin may be used cautiously to improve heart control in patients with atrial fibrillation. Daily weight measurement may be recommended. A weight gain of 3 or 4 pounds or more over 1 or 2 days can indicate excessive fluid accumulation.
Some people benefit from chemotherapy or prednisone.
A pacemaker may be needed if the conduction system is involved. When heart function is very poor, a heart transplant may be considered for some patients, but not those with AL type amyloidosis since their disease compromises many organs. In one type of secondary amyloidosis, liver transplantation is also required.
Prognosis
Cardiac amyloidosis is a chronic and progressive condition. A cardiologist may estimate the prognosis according to the thickness of the left ventricle and to the degree of restriction in the heart (diastolic dysfunction). For primary amyloidosis, the median survival after diagnosis is about 2.1 years.
Complications
- Congestive heart failure
- Atrial fibrillation or ventricular arrhythmias
- Sick sinus syndrome (occasionally)
- Symptomatic cardiac conduction system disease (arrhythmias related to abnormal conduction of impulses through the heart muscle)
- Low blood pressure and dizziness from excessive urination (from medication)
- Increased sensitivity to digoxin with the potential for digoxin toxicity and related arrhythmias
- Ascites (fluid accumulation in the abdomen)
Histopathological Findings
-
Amyloidosis Lesion In Left Atrium: Gross natural color view of a diagnostic lesion
-
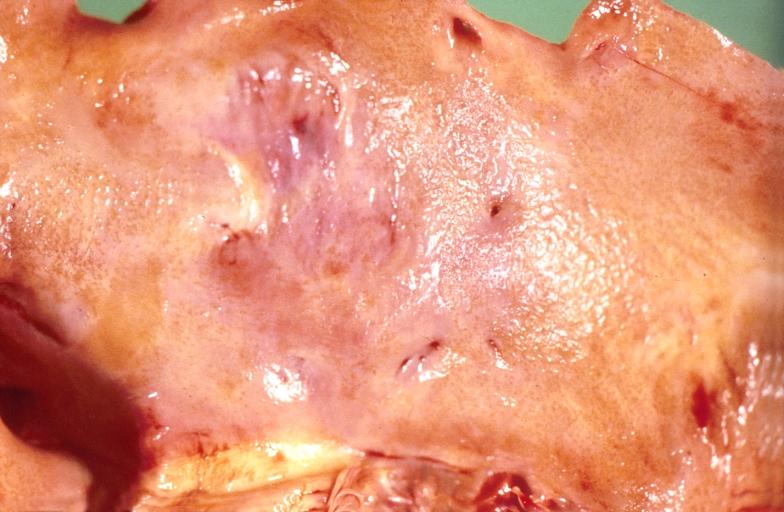
Amyloidosis Lesion In Left Atrium: Gross natural color close-up
-
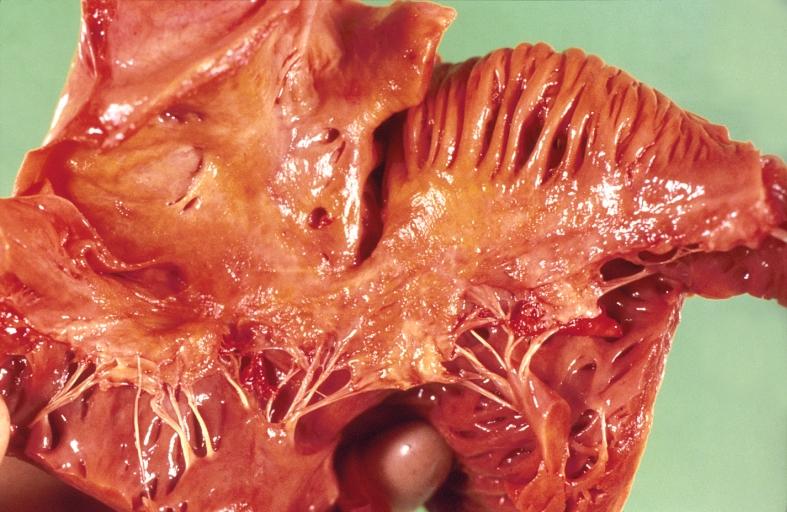
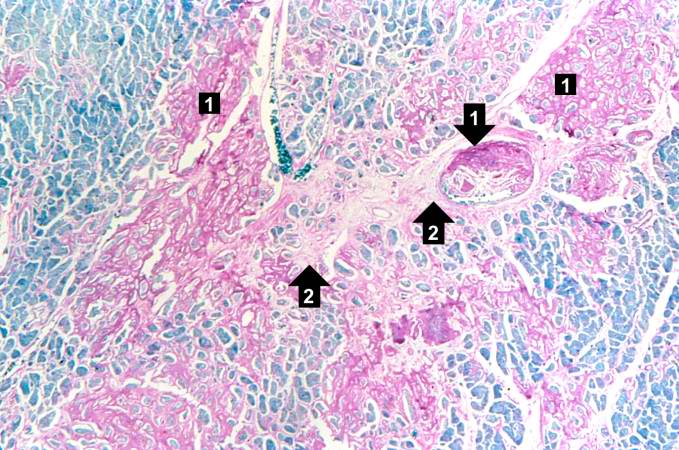
Heart: Perivascular amyloid, amyloidosis, congo red showing birefringence
-
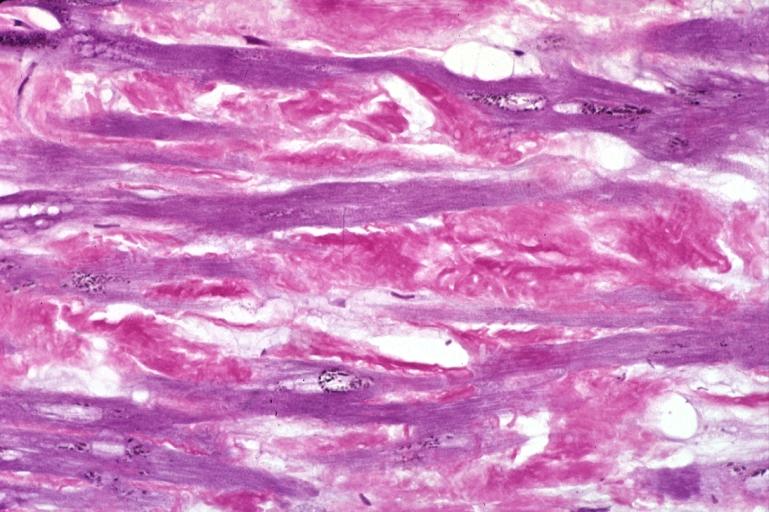
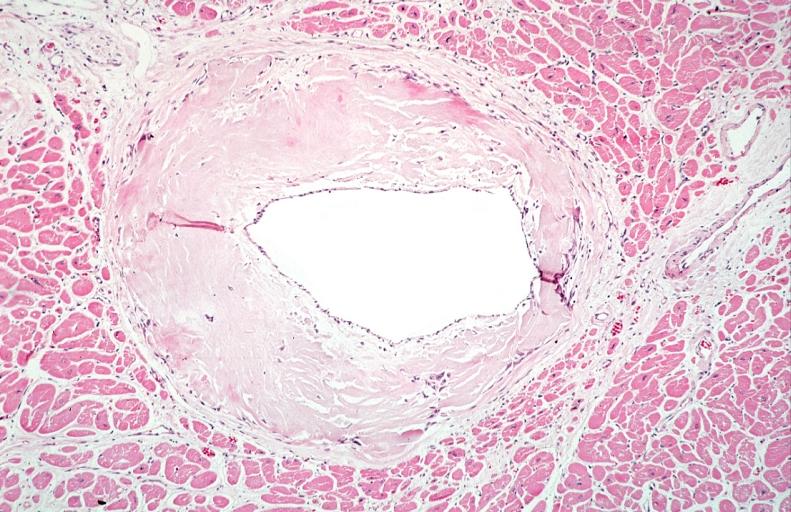
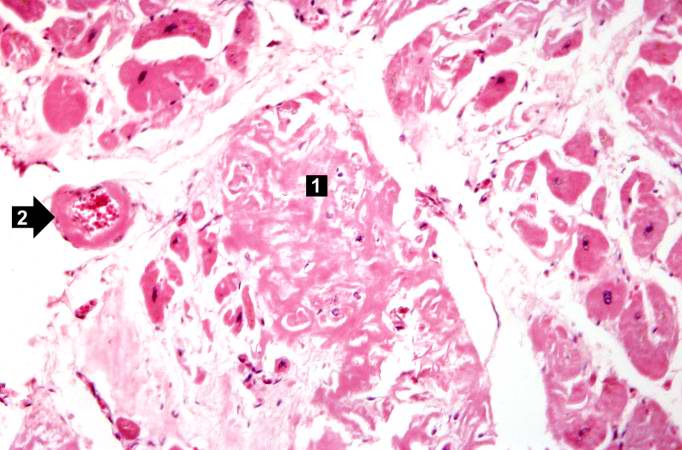
Heart: Perivascular amyloid, amyloidosis (Hematoxylin and eosin staining)
An Case Example
Clinical Summary
This 87-year-old black male diabetic was admitted for amputation of the lower extremity involved by atherosclerotic gangrene and osteomyelitis. Following amputation, the patient's course was one of progressive deterioration. Laboratory studies immediately prior to death revealed a blood glucose of 840 mg/dL and a serum CO2 (bicarbonate) of 8.5 mmol/L.
Autopsy Findings
The heart weighed 540 grams. The endocardial surface of both atria presented a mottled gray-red and gray-white appearance. Multiple sections through the myocardium revealed a marked 'pallor' of the muscle.
Images
-
This is a gross photograph of section of heart tissue from this case. The tissue was firm and had a waxy texture. If you use your imagination you can see pale yellow areas within this tissue which represent the amyloid deposits.
-
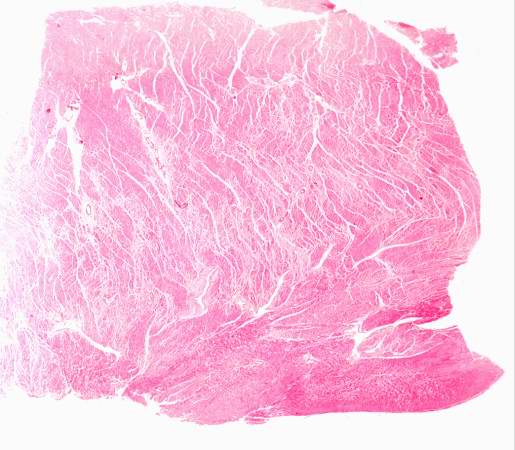
This is a low power photomicrograph of the heart tissue from this case. At this magnification the structure looks relatively normal.
-
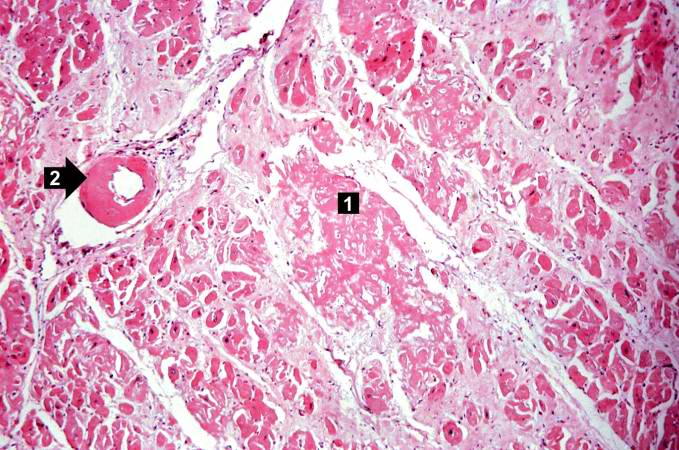
This is a higher-power photomicrograph of the heart tissue from this case. Note the amyloid deposition throughout the myocardium (1) as well as deposition in the wall of the blood vessel (2).
-
This is a higher-power photomicrograph of extracellular amyloid (1) and deposition of amyloid in the vessel wall (2).
-
This is a special stain for amyloid (Luxol PAS) demonstrating the amyloid (1) and fibrosis (2) in the myocardium. The amyloid is darker purple/magenta and tends to be more amorphous. The fibrosis is pink and more fibrillar.
References
- ↑ Pomerance, A. The pathology of senile cardiac amyloidosis. J. Pathol. Bacteriol. 91, 357. 1966
- ↑ Buja, L. M., Khoi, N. B., and Roberts W. C. Clinically significant cardiac amyloidosis. Clinicopathologic findings in 15 patients. Am. J. Cardiol., 26, 394. 1970
- ↑ Goffin, Y. A. Microscopic amyloid deposits in the heart valves: a common local complication of chronic damage and scarring. J. Clin. Pathol., 33, 262. 1980
- ↑ Goffin, Y. A., Murdoch, W., Cornwell, G. G. III, and Sorenson, G. D. Microdeposits of amyloid in sclerocalcific heart valves: a histochemical and immunoflourescence study. J. Clin. Pathol., 36, 1342. 1983
- ↑ Amyloid and amyloidosis. Gilles Grateau, Robert A. Kyle, Martha Skinner, 2005 ISBN 0-8493-3534-5
- ↑ Dubrey SW, Cha K, Skinner M, et al (1997). Familial and primary (AL) cardiac amyloidosis: echocardiographically similar diseases with distinctly different clinical outcomes. Heart; 78: 74-82.
- ↑ Palladini G, Campana C, Clersy C, et al (2003). Serum N-terminal pro Brain Natriuretic Peptide is a sensitive marker of myocardial dysfunction in AL amyloidosis. Circulation; 107: 2440-45.
- ↑ Kyle RA, Gertz MA (1995). Primary systemic amyloidosis: clinical and laboratory features in 474 cases. Semin Hematol; 8: 45-59.
Additional Readings
- Amyloid and amyloidosis. Gilles Grateau, Robert A. Kyle, Martha Skinner, 2005 ISBN 0-8493-3534-5
External Resources
- Amyloid Heart Disease
- Primary cardiac amyloidosis in a young man presenting with angina pectoris
- Microscopic amyloid deposits in the heart valves: a common local complication of chronic damage and scarring
- Obstructive intramural coronary amyloidosis: a distinct phenotype of cardiac amyloidosis that can cause acute heart failure
- Unique type of isolated cardiac valvular amyloidosis
- Intracellular cardiac amyloidosis in familiar amyloid polyneuropathy of the Portuguese type
|
Amyloidosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac amyloidosis On the Web |
|
American Roentgen Ray Society Images of Cardiac amyloidosis |