COVID-19-associated encephalitis: Difference between revisions
| Line 309: | Line 309: | ||
*[[Anti-inflammatory]] like pulse [[steroids]] ([[methylprednisolone]] 1,000 mg/day) are also helpful in this [[disease]]. | *[[Anti-inflammatory]] like pulse [[steroids]] ([[methylprednisolone]] 1,000 mg/day) are also helpful in this [[disease]]. | ||
*Severe disease in these [[patients]] required [[intubation]] and [[mechanical ventilation]]. | *Severe disease in these [[patients]] required [[intubation]] and [[mechanical ventilation]]. | ||
*IVIG can be administrated in severe cases.<ref name="pmid32454137">{{cite journal| author=Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M | display-authors=etal| title=Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 179-181 | pmid=32454137 | doi=10.1016/j.bbi.2020.05.054 | pmc=7255176 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32454137 }}</ref><ref name="pmid32389697">{{cite journal| author=Dogan L, Kaya D, Sarikaya T, Zengin R, Dincer A, Akinci IO | display-authors=etal| title=Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: Case series. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 155-158 | pmid=32389697 | doi=10.1016/j.bbi.2020.05.022 | pmc=7204750 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32389697 }}</ref> | |||
*[[Hydroxychloroquine|Hydorxychloroquine]] and some [[antivirals]] were used in these [[patients]] but they did not resolve the [[condition]]. | *[[Hydroxychloroquine|Hydorxychloroquine]] and some [[antivirals]] were used in these [[patients]] but they did not resolve the [[condition]]. | ||
<br /> | <br /> | ||
Revision as of 01:57, 31 August 2020
For COVID-19 frequently asked outpatient questions, click here.
For COVID-19 frequently asked inpatient questions, click here.
For COVID-19 patient information, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2], Fahimeh Shojaei, M.D.
Synonyms and keywords: Encephalitis covid-19
Overview
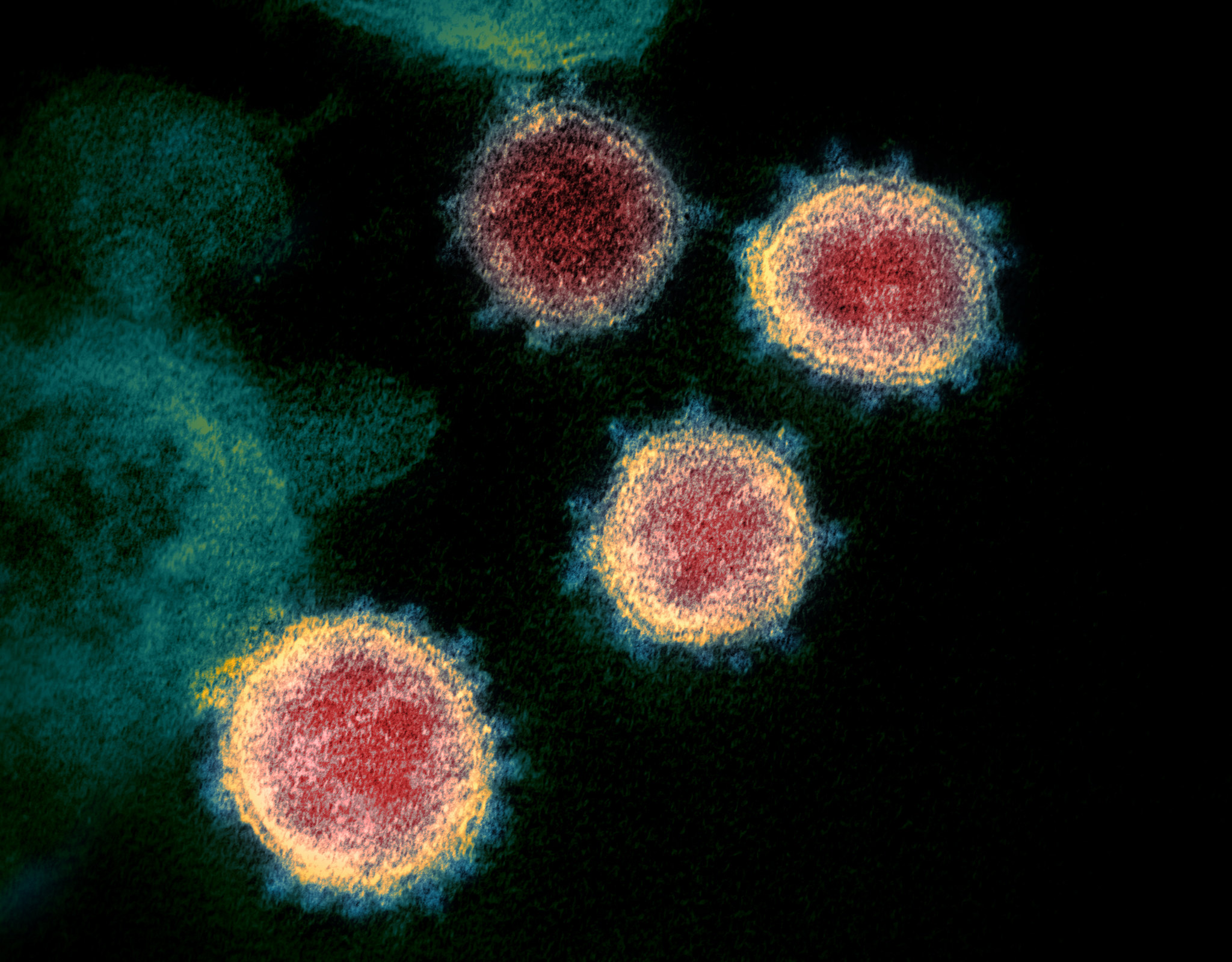
Encephalitis is inflammation of the brain parenchyma and it is commonly caused by viruses. COVID-19 is a virus related to the severe acute respiratory syndrome coronavirus (SARS-CoV) group and named as SARS-CoV-2. COVID-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2. The association between COVID-19 and encephalitis was made early in the pandemic in the Wuhan province of China. There is no established system for the classification of COVID-19 associated encephalitis. The exact pathogenesis of COVID-19 encephalitis is not fully understood. COVID-19-associated encephalitis must be differentiated from other diseases that cause fever, headache, and altered mental status with or without cough.
Historical Perspective
- Covid-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2.[1][2]
- The association between COVID-19 and encephalitis was made during this pandemic started in December in Wuhan, China and named as Wuhan coronavirus.[3]
- In March 2020, Dr. Ali A. was the first to discover the association between COVID-19 and neurological diseases e.g. encephalitis. He made a clinical diagnosis along with his team and then MRI used to diagnose the disease.[4]
- In January 2020, Chinese doctors confirmed the first case of encephalitis due to COVID-19 in a 56 year old male and they conducted gene sequencing on cerebrospinal fluid (CSF) samples and confirmed the novel virus inside the brain, but it was not published.
- There have been several outbreaks of SARS and MERS.
Classification
- There is no established system for the classification of COVID-19 associated encephalitis.
- Based on the duration of symptoms, this disease is classified as acute.
Pathophysiology
- The exact pathogenesis of COVID-19 encephalitis is not fully understood.[5]
- It is thought that this viral encephalitis is the result of multiple pathophysiologic pathways.
| SARS-CoV-2 | |||||||||||||||||||||||||||||||||||||||||
| ACE2 | Direct Injury due to Infection | Immune Injury | Hypoxic Injury | Hypercoagulability | |||||||||||||||||||||||||||||||||||||
| Viral Encephalitis | |||||||||||||||||||||||||||||||||||||||||
- ACE2: Angiotensin converting enzyme receptor 2 is present in multiple organs e.g. lungs, brain, and kidney, etc.
- Hypercoagulability: With elevated D-dimer
- Immune injury: Cytokine activation and vascular involvement.
- Direct injury: Due to hematogenous and neuronal pathway involvement.
- Hypoxic injury: Due to anaerobic metabolism.
Causes
- Coronavirus disease 2019 (COVID-19) associated encephalitis is caused by SARS-CoV-2.
- To read more about this virus, click here.
Differentiating COVID-19-associated encephalitis from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- There are approximately 50 cases of COVID-19-associated encephalitis reported in the first six months of the pandemic.[6][7]
- MERS and SARS-CoV had neurologic manifestation like encephalitis at the time of outbreaks.
- Patients of all age groups may develop COVID-19-associated encephalitis
- The incidence of COVID-19-associated encephalitis increases with age; the median age at diagnosis is 54 years.
- There is no racial predilection to COVID-19-associated encephalitis but more cases were present in African Americans.
- COVID-19-associated encephalitis affects men and women equally.
Risk Factors
- Common risk factors in the development of COVID-19-associated encephalitis may be occupational, environmental, and genetic.[8]
- Risk factors for this disease are the same as for COVID-19.
- To view the risk factors of COVID-19, click here.
- Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapy.
| Autoimmune disease | Immunosuppression |
|---|---|
| Multiple sclerosis | Interferon beta |
| Myasthenia gravis | Corticosteroids |
| Neuromyelitis optica | Monoclonal antibody |
| Sarcoidosis | Corticosteroids |
| Sickle cell disease (SCD) | Crizanlizumab |
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis.
- To view screening for COVID-19, click here.
Natural History, Complications, and Prognosis
- To view Natural History for COVID-19, click here.
- If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause:
| Encephalitis | |||||||||||||||||||||||||||||||||||||||||
| Memory loss | Epilepsy | Personality changes | Hearing/vision loss | Coma/Death | |||||||||||||||||||||||||||||||||||||
Diagnosis
Diagnostic Study of Choice
- The diagnostic study of choice for COVID-19-associated encephalitis is CSF analysis for ruling out other viral and bacterial panels with the help of RT-PCR.
History and Symptoms
- The majority of patients with COVID-19-associated encephalitis present with respiratory symptoms. e.g. cough, shortness of breath etc.
Common Symptoms
- The common symptoms of COVID-19-associated encephalitis include:
- Cough,
- Shortness of breath
- Headache,
- Fever
- Fatigue
- Impaired consciousness
Less Common Symptoms
- Less common symptoms of COVID-19-associated encephalitis include:
- Transient generalized seizure
- Dizziness,
- Paralysis
- Sedation
- Coma
- Clinical manifestation of 3 cases of COVID-19 associated encephalitis are shown below:
| Patient No. | Early symptoms | Later presentation | GCS | Lab. Findings | Specific Tests | Imaging studies | |
|---|---|---|---|---|---|---|---|
| CBC | CSF | MRI/CT scan | |||||
| 24-year-old man from Japan[2] | Headache, | Worsening headache, Sore throat. (Day 5)
Impaired consciousness and transient generalized seizure, (Day 9) |
E4V1M1 | ↑WBCs and neutrophils ↓lymphocytes ↑ CRP |
Clear and colorless fluid,
Pressure=320 mmH2O, Cell count was 12/μL–10 |
RT-PCR of SARS-CoV-2 RNA was positive in CSF | Brain MRI:
Hyperintensity in the right lateral ventricle's inferior horn along the wall, |
| In Wuhan, in a letter to editor, Ye M et.al, reported COVID-19 associated encephalitis case in a male with laboratory finding [9] | Fever
SOB |
Confusion | NA | WBC count (3.3 × 109/L) and lymphopenia (0.8 × 109/L) | Pressure=220 mmg
WBC (0.001 × 109/L) protein (0.27 g/L) sugar (3.14 mmol/L) |
SARS-CoV-2 was positive on nasopharyngeal swab but negative on CSF testing
All other bacterial and viral causes of encephlitis were negative |
|
| 35-year-old woman from Turkey[10][11] whose COVID-19 associated encephalitis mimicking as glial tumor of CNS | Flu like symptoms | Headache, nausea, dizziness, and
drug-refractory seizures. |
E4V5M6 | NA | NA | RT-PCR and antibody tests positive | Brain MRI: Hyperintensity in the left temporal lobe.
MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak. |
| 31-year-old African American woman[12] | SCD patient with dyspnea | Paralysis and sedation (Day 13)
Comatose (Day 15) and death (Day 16) |
E0V0M0 | NA | Pressure=30cmH2O
115 nucleated cell /ml 7374 erythrocytes /ml Protein> 200mg/dl
|
RT=PCR for SARS-CoV-2 was positive in nasopharyngeal swab | Brain MRI: Nonenhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation. |
Physical Examination
- Common physical examination findings of COVID-19-associated encephalitis include
Neuromuscular
- Generalized seizure
- Headache
- Neck stiffness
- Focal neurological deficits can be present in this disease.
Laboratory Findings
- Positive RT-PCR in CSF or nasopharyngeal swab is diagnostic of COVID-19-associated encephalitis.
- Laboratory findings consistent with the diagnosis of COVID-19-associated encephalitis include CSF analysis, RT-PCR and brain MRI.
- D-dimer or white blood cells can be normal among patients with COVID-19-associated encephalitis.
- Some patients with COVID-19-associated encephalitis may have elevated erythrocytes in CSF which is usually suggestive of COVID-19-associated encephalitis.
Electrocardiogram
- There are no ECG findings associated with COVID-19-associated encephalitis.
X-ray
- There are no x-ray findings associated with COVID-19-associated encephalitis.
- However, an x-ray chest may be helpful in the diagnosis of COVID-19-associated respiratory disease.
Echocardiography or Ultrasound
- There are no echocardiography findings associated with COVID-19-associated encephalitis.
CT scan
- The findings on the CT scans associated with COVID-19-associated encephalitis are similar to MRI which is the preferred modality.
MRI
- Brain MRI may be helpful in the diagnosis of COVID-19 associated encephalitis. Findings on MRI suggestive of COVID-19-associated encephalitis include:
- Hyper-intensity in the right lateral ventricle's inferior horn along the wall and pan-paranasal sinusitis.
- Hyper-intensity in the left temporal lobe.
- MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak.
- Non-enhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation.
Other Diagnostic Studies
- Other diagnostic studies for COVID-19-associated encephalitis include:
Treatment
Medical Therapy
The mainstays of medical therapy for viral encephalitis are:[10][13][2][14]
Symptomatic treatments:
- Anti-epileptic drugs like levetiracetam (50-60 mg/kg/day) is necessary for seizure management.
- Anti-inflammatory like pulse steroids (methylprednisolone 1,000 mg/day) are also helpful in this disease.
- Severe disease in these patients required intubation and mechanical ventilation.
- IVIG can be administrated in severe cases.[15][16]
- Hydorxychloroquine and some antivirals were used in these patients but they did not resolve the condition.
Surgery
- Focal epilepsy having focal involvement of brain parenchyma can be treated with surgery[10].
- One of these patients undergone left anterior temporal lobectomy, which improved symptoms completely without any postoperative neurologic deficit[10].
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated encephalitis.
- Effective measure for the primary prevention of COVID-19 associated encephalitis. include social distancing and avoidance behaviors.
- There are no available vaccines against COVID-19 associated encephalitis. Multiple trials are under process for vaccinations.
- To view primary prevention for COVID-19 click here.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19 associated encephalitis.
- To view secondary prevention for COVID-19 click here.
References
- ↑ Velavan TP, Meyer CG (2020). "The COVID-19 epidemic". Trop Med Int Health. 25 (3): 278–280. doi:10.1111/tmi.13383. PMC 7169770 Check
|pmc=value (help). PMID 32052514 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Riou J, Althaus CL (2020). "Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020". Euro Surveill. 25 (4). doi:10.2807/1560-7917.ES.2020.25.4.2000058. PMC 7001239 Check
|pmc=value (help). PMID 32019669 Check|pmid=value (help). - ↑ Asadi-Pooya AA, Simani L (2020). "Central nervous system manifestations of COVID-19: A systematic review". J Neurol Sci. 413: 116832. doi:10.1016/j.jns.2020.116832. PMC 7151535 Check
|pmc=value (help). PMID 32299017 Check|pmid=value (help). - ↑ Baig AM (2020). "Neurological manifestations in COVID-19 caused by SARS-CoV-2". CNS Neurosci Ther. 26 (5): 499–501. doi:10.1111/cns.13372. PMC 7163592 Check
|pmc=value (help). PMID 32266761 Check|pmid=value (help). - ↑ Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK; et al. (2017). "Middle East Respiratory Syndrome". N Engl J Med. 376 (6): 584–594. doi:10.1056/NEJMsr1408795. PMC 5362064. PMID 28177862.
- ↑ Tsai LK, Hsieh ST, Chang YC (2005). "Neurological manifestations in severe acute respiratory syndrome". Acta Neurol Taiwan. 14 (3): 113–9. PMID 16252612.
- ↑ Nath A (2020). "Neurologic complications of coronavirus infections". Neurology. 94 (19): 809–810. doi:10.1212/WNL.0000000000009455. PMID 32229625 Check
|pmid=value (help). - ↑ Ye M, Ren Y, Lv T (2020). "Encephalitis as a clinical manifestation of COVID-19". Brain Behav Immun. 88: 945–946. doi:10.1016/j.bbi.2020.04.017. PMC 7146652 Check
|pmc=value (help). PMID 32283294 Check|pmid=value (help). - ↑ 10.0 10.1 10.2 10.3
- ↑ Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K (2020). "COVID-19-Associated Encephalitis Mimicking Glial Tumor". World Neurosurg. 140: 46–48. doi:10.1016/j.wneu.2020.05.194. PMC 7256557 Check
|pmc=value (help). PMID 32479911 Check|pmid=value (help). - ↑ Benameur K, Agarwal A, Auld SC, Butters MP, Webster AS, Ozturk T; et al. (2020). "Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020". Emerg Infect Dis. 26 (9). doi:10.3201/eid2609.202122. PMID 32487282 Check
|pmid=value (help). - ↑ Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y (May 2015). "Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase". Brain Dev. 37 (5): 471–7. doi:10.1016/j.braindev.2014.08.003. PMID 25174548.
- ↑ Nakano A, Yamasaki R, Miyazaki S, Horiuchi N, Kunishige M, Mitsui T (2003). "Beneficial effect of steroid pulse therapy on acute viral encephalitis". Eur. Neurol. 50 (4): 225–9. doi:10.1159/000073864. PMID 14634267.
- ↑ Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M; et al. (2020). "Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report". Brain Behav Immun. 87: 179–181. doi:10.1016/j.bbi.2020.05.054. PMC 7255176 Check
|pmc=value (help). PMID 32454137 Check|pmid=value (help). - ↑ Dogan L, Kaya D, Sarikaya T, Zengin R, Dincer A, Akinci IO; et al. (2020). "Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: Case series". Brain Behav Immun. 87: 155–158. doi:10.1016/j.bbi.2020.05.022. PMC 7204750 Check
|pmc=value (help). PMID 32389697 Check|pmid=value (help).