Brucellosis differential diagnosis: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (11 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
[[Image:Home_logo1.png|right|250px|link=https://www.wikidoc.org/index.php/Brucellosis]] | |||
{{CMG}} {{AE}}{{DL}} {{VD}} | {{CMG}} {{AE}}{{DL}} {{VD}} | ||
==Overview== | ==Overview== | ||
[[Brucellosis]] must be differentiated from [[ | [[Brucellosis]] must be differentiated from [[typhoid fever]], [[malaria]], [[tuberculosis]], [[lymphoma]], [[Dengue fever|dengue]], [[leptospirosis]], [[Rheumatology|rheumatic disease]], [[epstein-barr virus]], [[toxoplasmosis]], [[cytomegalovirus]], and [[Human Immunodeficiency Virus|HIV]]. | ||
==Differentiating Brucellosis from other Diseases== | ==Differentiating Brucellosis from other Diseases== | ||
[[Brucellosis]] must be differentiated from [[ | [[Brucellosis]] must be differentiated from [[typhoid fever]], [[malaria]], [[tuberculosis]], [[lymphoma]], [[Dengue]], [[Leptospirosis]], [[Rheumatic disease]], [[Epstein Barr virus|epstein-barr virus]], [[Toxoplasmosis]], [[Cytomegalovirus causes|cytomegalovirus]], and [[Human Immunodeficiency Virus|HIV]].<ref name="pmid1593042322">{{cite journal|author=Pappas G, Akritidis N, Bosilkovski M, Tsianos E|title=Brucellosis.|journal=N Engl J Med|year=2005|volume=352|issue=22|pages=2325-36|pmid=15930423|doi=10.1056/NEJMra050570|pmc=|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15930423}}</ref><ref>Brucellosis "Dennis Kasper, Anthony Fauci, Stephen Hauser, Dan Longo, J. Larry Jameson, Joseph Loscalzo"Harrison's Principles of Internal Medicine, 19e Accessed on January,2017</ref><ref name="pmid754636422">{{cite journal|year=1995|title=Brucellosis: current epidemiology, diagnosis, and management.|url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7546364|journal=Curr Clin Top Infect Dis|volume=15|issue=|pages=115-28|doi=|pmc=|pmid=7546364|author=Young EJ}}</ref><ref name="enf22">Enfermedades infecciosas: Brucelosis -Diagnóstico de Brucelosis,Guia para el Equipo de Salud. Ministerio de Salud-Argentina. http://www.msal.gob.ar/images/stories/bes/graficos/0000000304cnt-guia-medica-brucelosis.pdf. Accessed on February 2, 2016</ref> | ||
A detailed clinical history which includes recent travel history, recent camping or hunting, consumption of unpasteurized milk or raw meat products, and occupational history should be obtained, in order to differentiate [[ | A detailed clinical history which includes recent travel history, recent camping or hunting, consumption of unpasteurized milk or raw meat products, and occupational history should be obtained, in order to differentiate [[brucellosis]] from other diseases. | ||
{| class="wikitable" | {| class="wikitable" | ||
! | !Differential diagnosis of Brucellosis | ||
! colspan="5" |Symptoms | ! colspan="5" |Symptoms | ||
! colspan="3" |Signs | ! colspan="3" |Signs | ||
| Line 30: | Line 30: | ||
|- | |- | ||
|[[Brucellosis]] | |[[Brucellosis]] | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | + | ||
| | | + | ||
| | | + | ||
|[[Lymphocytosis|Relative lymphocytosis]] | |[[Lymphocytosis|Relative lymphocytosis]] | ||
| | | | ||
[[Night sweats]], often with characteristic smell, likened to wet hay | [[Night sweats]], often with characteristic smell, likened to wet hay | ||
|- | |- | ||
|[[Typhoid fever]] | |[[Typhoid fever]] | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | + | ||
| | | + | ||
|Decreased [[hemoglobin]] | |Decreased [[hemoglobin]] | ||
|Incremental increase in temperature initially and than sustained [[fever]] as high as 40°C (104°F) | |Incremental increase in temperature initially and than sustained [[fever]] as high as 40°C (104°F) | ||
|- | |- | ||
|[[Malaria]] | |[[Malaria]] | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | + | ||
| | | + | ||
|Microcytosis, | |Microcytosis, | ||
| Line 70: | Line 69: | ||
|- | |- | ||
|[[Tuberculosis]] | |[[Tuberculosis]] | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
|Mild normocytic [[anemia]], [[hyponatremia]], and | |Mild normocytic [[anemia]], [[hyponatremia]], and | ||
[[hypercalcemia]] | [[hypercalcemia]] | ||
|[[Night sweats]], constant fatigue | |[[Night sweats]], constant [[fatigue]] | ||
|- | |- | ||
|[[Lymphoma]] | |[[Lymphoma]] | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | - | ||
|Increase [[ESR]], increased [[LDH]] | |Increase [[ESR]], increased [[LDH]] | ||
|[[Night sweats]], constant fatigue | |[[Night sweats]], constant fatigue | ||
|- | |- | ||
|[[Mumps]] | |[[Mumps]] | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | + | ||
| | | - | ||
| | | - | ||
|[[Lymphocytosis|Relative lymphocytosis]], serum [[amylase]] elevated | |[[Lymphocytosis|Relative lymphocytosis]], serum [[amylase]] elevated | ||
|[[Parotid gland|Parotid]] swelling/tenderness | |[[Parotid gland|Parotid]] swelling/tenderness | ||
|- | |- | ||
|[[Rheumatoid arthritis]] | |[[Rheumatoid arthritis]] | ||
| | | - | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | + | ||
|[[ESR]] and [[CRP]] elevated, positive [[rheumatoid factor]] | |[[ESR]] and [[CRP]] elevated, positive [[rheumatoid factor]] | ||
|Morning stiffness | |Morning [[stiffness]] | ||
|- | |- | ||
|[[SLE]] | |[[SLE]] | ||
| | | - | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | - | ||
| | | + | ||
|[[ESR]] and [[CRP]] elevated, positive [[ANA]] | |[[ESR]] and [[CRP]] elevated, positive [[ANA]] | ||
|[[Fatigue]] | |[[Fatigue]] | ||
|- | |- | ||
|[[Human Immunodeficiency Virus|HIV]] | |[[Human Immunodeficiency Virus|HIV]] | ||
| | | - | ||
| | | - | ||
| | | - | ||
| | | + | ||
| | | + | ||
| | | + | ||
| | | - | ||
| | | + | ||
| | | | ||
|Constant fatigue | |Constant fatigue | ||
|} | |} | ||
'''Differentiating psittacosis from other diseases''' | |||
{| class="wikitable" | |||
!Clinical feature | |||
![[Cough]] | |||
![[Sputum]] | |||
![[Dyspnea]] | |||
![[Sore throat]] | |||
![[Headache]] | |||
![[Confusion]] | |||
![[Diarrhea]] | |||
!Chest radiograph changes | |||
!Hyponatremia | |||
![[Leukopenia]] | |||
!Abnormal Liver function tests | |||
!Treatment | |||
|- | |||
|Psittacosis | |||
| ++ | |||
| - | |||
| + | |||
| - | |||
| +++ | |||
| + | |||
|Minimal | |||
| | |||
* No changes seen | |||
| - | |||
| + | |||
| - | |||
|[[Doxycycline]] | |||
|- | |||
|[[Chlamydia pneumoniae|''C.pneumoniae'']] pneumonia | |||
| + | |||
| + | |||
| + | |||
| +++ | |||
| ++ | |||
| + | |||
| - | |||
| | |||
* Minimal changes observed | |||
| - | |||
| - | |||
| - | |||
|[[Doxycycline]], [[Azithromycin]] | |||
|- | |||
|[[Mycoplasma pneumoniae|''M. pneumoniae'']] pneumonia | |||
| ++ | |||
| ++ | |||
| ++ | |||
| - | |||
| - | |||
| - | |||
| - | |||
| | |||
* Bronchial wall thickening | |||
* Centrilobular nodules | |||
* [[Ground glass opacification on CT|Ground-glass attenuation]] | |||
* [[Consolidation (medicine)|Consolidation]] | |||
| - | |||
| - | |||
| + | |||
|[[Doxycycline]] | |||
|- | |||
|[[Legionella pneumophila|''L. Pneumophila'']] infection | |||
| + | |||
| +++ | |||
| +++ | |||
| - | |||
| + | |||
| ++ | |||
| + | |||
|Often Multifocal | |||
| ++ | |||
| + | |||
| ++ | |||
|[[Doxycycline]] | |||
|- | |||
|[[Influenza (Flu) (For Patients)|Influenza]] | |||
| ++ | |||
| ++ | |||
| ++ | |||
| ++ | |||
| ++ | |||
| +/- | |||
| +/- | |||
| | |||
* Bi-basal air-space opacities | |||
* Perihilar [[reticular]] and [[Alveolar|alveolar infiltrates]] | |||
| - | |||
| - | |||
| - | |||
|[[zanamivir]], [[oseltamivir]], | |||
|- | |||
|[[Endocarditis]] | |||
| ++ | |||
| ++ | |||
| + | |||
| - | |||
| - | |||
| - | |||
| - | |||
| | |||
* Hazy opacities at [[lung]] | |||
bases bilaterally | |||
| - | |||
| +/- | |||
| +/- | |||
|[[Vancomycin]] | |||
|- | |||
|[[Coxiella burnetii infection|''Coxiella burnetii'' infection]] | |||
| ++ | |||
| - | |||
| + | |||
| +/- | |||
| - | |||
| +/- | |||
|Minimal | |||
| | |||
* [[Segmental analysis (biology)|Segmental]] or [[Lobar pneumonia|lobar]] opacification | |||
* Occasional [[pleural effusions]] | |||
| - | |||
| +/- | |||
|=/- | |||
|[[Doxycycline]] | |||
|- | |||
|[[Leptospirosis]] | |||
| ++ | |||
| + | |||
| ++ | |||
| + | |||
| + | |||
| ++ | |||
| - | |||
| | |||
* Multiple ill-defined [[Nodule (medicine)|nodules]] in both lungs. | |||
| +++ | |||
| | |||
| | |||
|[[Doxycycline]], [[azithromycin]], [[amoxicillin]] | |||
|- | |||
|[[Brucellosis]] | |||
| ++ | |||
| - | |||
| + | |||
| - | |||
| ++ | |||
| + | |||
| - | |||
| | |||
* Soft [[Miliary TB|miliary]] mottling | |||
* [[Parenchymal lung disease|Parenchymal nodules]] | |||
* [[Consolidation (medicine)|Consolidation]] | |||
* [[Chronic (medical)|Chronic]] [[diffuse]] changes | |||
* [[Hilar]] or [[Paratracheal lymph nodes|paratracheal]] [[lymphadenopathy]] | |||
* [[Pneumothorax]]. | |||
| -/+ | |||
| +/- | |||
| +/- | |||
|[[Doxycycline]], [[rifampin]] | |||
|} | |||
Key; | |||
+, occurs in some cases | |||
++, occurs in many cases, | |||
+++, occurs frequently | |||
Brucellosis must be differentiated from other diseases that cause [[atypical pneumonia]] such as Q fever and legionaellosis | |||
{| class="wikitable" | |||
!Disease | |||
!Prominent clinical features | |||
!Lab findings | |||
!Chest X-ray | |||
|- | |||
|Q fever | |||
| | |||
* Q fever is characterized by abrupt onset of [[fever]], [[myalgia]], [[headache]], and other constitutional symptoms. | |||
* [[Cough]] is the most prominent respiratory symptom and it is usually dry.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* [[Cough]] is associated with [[dyspnea]] and [[pleuritic chest pain]]. | |||
| | |||
* [[Antibody]] detection using [[Immunofluorescence|indirect immunofluorescence]] (IIF) is the preferred method for diagnosis. | |||
* [[Polymerase chain reaction|PCR]] can be used if IIF is negative, or very early once disease is suspected. | |||
* [[Coxiella burnetii|''C. burnetii'']] does not grow on ordinary blood cultures, but can be cultivated on special media such as embryonated eggs or cell culture. | |||
* A two-to-three fold increase in [[Aspartate transaminase|AST]] and [[ALT]] is seen in most patients. | |||
| | |||
[[Image:Q fever.gif|center|300px|thumb|Q fever pneumonia - - Case courtesy of Royal Melbourne Hospital Respiratory, Radiopaedia.org, rID 21993 ]] | |||
|- | |||
|[[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] | |||
| | |||
* [[mycoplasma pneumonia|''Mycoplasma'' pneumonia]] can be [[asymptomatic]]. | |||
* [[Headache]], [[Nausea and vomiting|nausea]], and [[malaise]] usually precede the onset of symptoms.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* [[Cough]] is intractable and nonproductive. | |||
| | |||
* Postitve [[Coombs test]] | |||
* [[Leukocytosis]] | |||
* [[Thrombocytosis]] | |||
| | |||
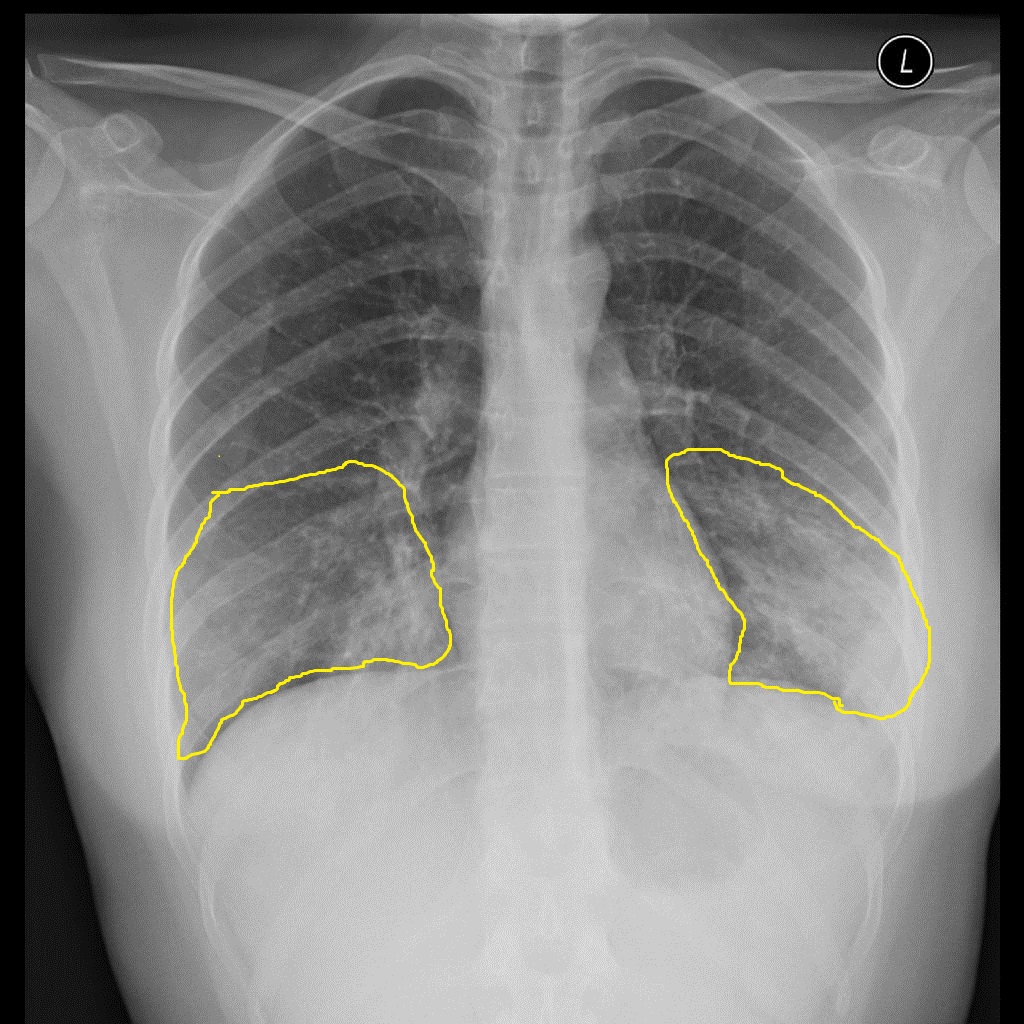
[[Image:Atypical-pneumonia-mycoplasma - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781.jpg|center|300px|thumb|Mycoplasma pneumonia - Case courtesy of Dr Alborz Jahangiri, Radiopaedia.org, rID 45781]] | |||
|- | |||
|[[Legionellosis]] | |||
| | |||
* [[Legionellosis]] is characterized by cough that is slightly productive.<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
* Constitutional symptoms such as [[chills]], [[myalgia]], and [[arthralgia]]. | |||
* Gastrointestinal symptoms such as [[diarrhea]], [[nausea]], and [[vomiting]]. | |||
| | |||
* Labs are nonspecific for diagnosing [[legionellosis]] | |||
* [[Renal dysfunction|Renal]] and [[hepatic dysfunction]] | |||
* [[Thrombocytopenia]] and [[leukocytosis]] | |||
* [[Hyponatremia]] | |||
| | |||
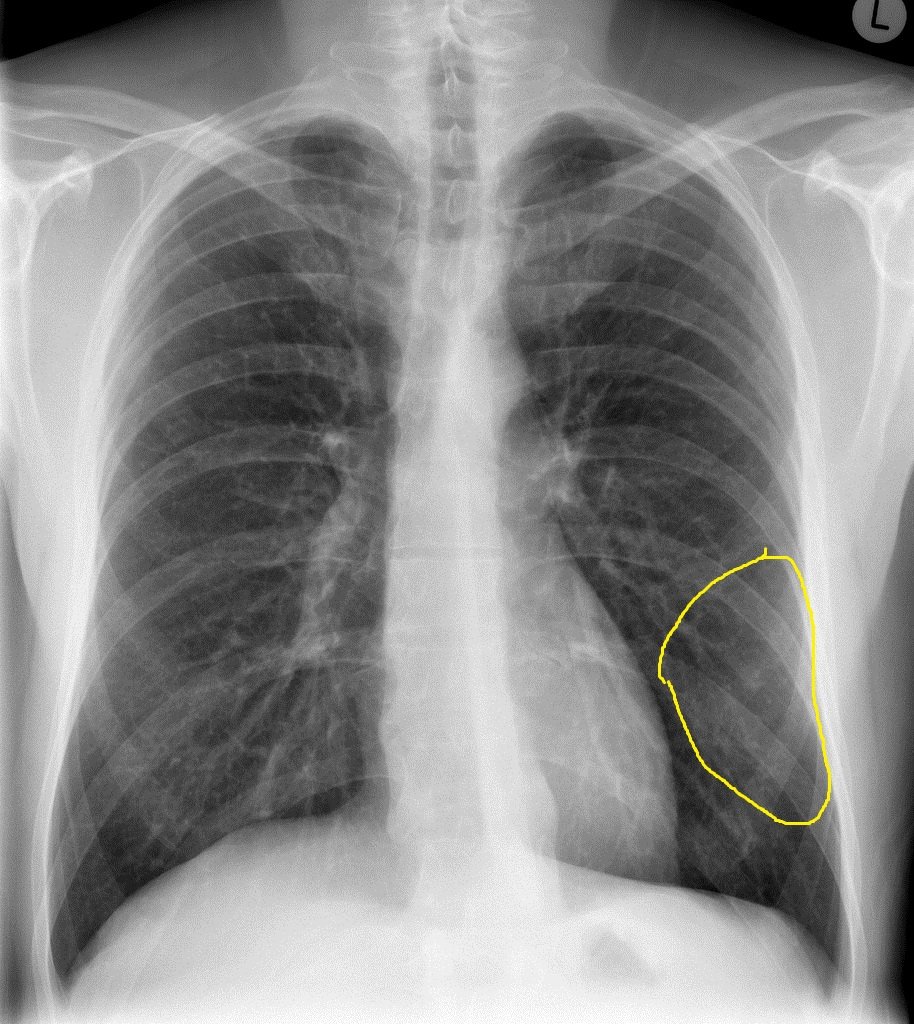
[[Image:Legionella-pneumonia - Case courtesy of Dr Henry Knipe, Radiopaedia.org, rID 31816.jpg|center|300px|thumb|Legionella pneumonia - Case courtesy of Dr Henry Knipe, Radiopaedia.org, rID 31816 ]] | |||
|- | |||
|[[Chlamydia pneumonia]] | |||
| | |||
* There are no specific clinical features of [[chlamydia pneumonia]]. | |||
* Symptoms appear gradually. | |||
* [[Chlamydia infection]] is usually associated with [[upper respiratory tract]] symptoms ([[pharyngitis]], [[sinusitis]], etc). | |||
* It might be associated with extrapulmonary maifestations such as [[meningitis]] and [[Guillain-Barre syndrome]].<ref name="pmid23422417">{{cite journal |vauthors=Irfan M, Farooqi J, Hasan R |title=Community-acquired pneumonia |journal=Curr Opin Pulm Med |volume=19 |issue=3 |pages=198–208 |year=2013 |pmid=23422417 |doi=10.1097/MCP.0b013e32835f1d12 |url=}}</ref> | |||
| | |||
* [[Chlamydia pneumonia]] is usually associated with normal [[WBC|WBC count.]] | |||
* Diagnosed with the presence of [[Antibody|antichlamydial antibody]] (through [[complement fixation]] or direct immunofluoroscence) or direct antigen detection. | |||
| | |||
[[Image:Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567.jpg|center|300px|thumb|Chlamydia-pneumonia - Case courtesy of Dr Andrew Dixon, Radiopaedia.org, rID 14567]] | |||
|} | |||
==Reference== | ==Reference== | ||
{{reflist|2}}<references /> | {{reflist|2}} | ||
[[Category: | <references /> | ||
[[Category: | |||
[[Category: | [[Category:Disease]] | ||
[[Category:Up-To-Date]] | |||
[[Category:Pulmonology]] | |||
[[Category:Hepatology]] | |||
[[Category:Rheumatology]] | |||
[[Category:Nephrology]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
Latest revision as of 20:44, 29 July 2020

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Danitza Lukac Vishal Devarkonda, M.B.B.S[2]
Overview
Brucellosis must be differentiated from typhoid fever, malaria, tuberculosis, lymphoma, dengue, leptospirosis, rheumatic disease, epstein-barr virus, toxoplasmosis, cytomegalovirus, and HIV.
Differentiating Brucellosis from other Diseases
Brucellosis must be differentiated from typhoid fever, malaria, tuberculosis, lymphoma, Dengue, Leptospirosis, Rheumatic disease, epstein-barr virus, Toxoplasmosis, cytomegalovirus, and HIV.[1][2][3][4]
A detailed clinical history which includes recent travel history, recent camping or hunting, consumption of unpasteurized milk or raw meat products, and occupational history should be obtained, in order to differentiate brucellosis from other diseases.
| Differential diagnosis of Brucellosis | Symptoms | Signs | Diagnosis | Additional Findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fever | Rash | Diarrhea | Abdominal pain | Weight loss | Painful lymphadenopathy | Hepatosplenomegaly | Arthritis | Lab Findings | ||
| Brucellosis | + | + | - | + | + | + | + | + | Relative lymphocytosis |
Night sweats, often with characteristic smell, likened to wet hay |
| Typhoid fever | + | + | - | + | - | - | + | + | Decreased hemoglobin | Incremental increase in temperature initially and than sustained fever as high as 40°C (104°F) |
| Malaria | + | - | + | + | - | - | + | + | Microcytosis,
elevated LDH |
"Tertian" fever: paroxysms occur every second day |
| Tuberculosis | + | + | - | + | + | + | - | + | Mild normocytic anemia, hyponatremia, and | Night sweats, constant fatigue |
| Lymphoma | + | - | - | + | + | - | + | - | Increase ESR, increased LDH | Night sweats, constant fatigue |
| Mumps | + | - | - | - | - | + | - | - | Relative lymphocytosis, serum amylase elevated | Parotid swelling/tenderness |
| Rheumatoid arthritis | - | + | - | - | - | - | - | + | ESR and CRP elevated, positive rheumatoid factor | Morning stiffness |
| SLE | - | + | - | + | + | - | - | + | ESR and CRP elevated, positive ANA | Fatigue |
| HIV | - | - | - | + | + | + | - | + | Constant fatigue | |
Differentiating psittacosis from other diseases
| Clinical feature | Cough | Sputum | Dyspnea | Sore throat | Headache | Confusion | Diarrhea | Chest radiograph changes | Hyponatremia | Leukopenia | Abnormal Liver function tests | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psittacosis | ++ | - | + | - | +++ | + | Minimal |
|
- | + | - | Doxycycline |
| C.pneumoniae pneumonia | + | + | + | +++ | ++ | + | - |
|
- | - | - | Doxycycline, Azithromycin |
| M. pneumoniae pneumonia | ++ | ++ | ++ | - | - | - | - |
|
- | - | + | Doxycycline |
| L. Pneumophila infection | + | +++ | +++ | - | + | ++ | + | Often Multifocal | ++ | + | ++ | Doxycycline |
| Influenza | ++ | ++ | ++ | ++ | ++ | +/- | +/- |
|
- | - | - | zanamivir, oseltamivir, |
| Endocarditis | ++ | ++ | + | - | - | - | - |
bases bilaterally |
- | +/- | +/- | Vancomycin |
| Coxiella burnetii infection | ++ | - | + | +/- | - | +/- | Minimal |
|
- | +/- | =/- | Doxycycline |
| Leptospirosis | ++ | + | ++ | + | + | ++ | - |
|
+++ | Doxycycline, azithromycin, amoxicillin | ||
| Brucellosis | ++ | - | + | - | ++ | + | - |
|
-/+ | +/- | +/- | Doxycycline, rifampin |
Key;
+, occurs in some cases
++, occurs in many cases,
+++, occurs frequently
Brucellosis must be differentiated from other diseases that cause atypical pneumonia such as Q fever and legionaellosis
| Disease | Prominent clinical features | Lab findings | Chest X-ray |
|---|---|---|---|
| Q fever |
|
 | |
| Mycoplasma pneumonia |
|
|
 |
| Legionellosis |
|
|
 |
| Chlamydia pneumonia |
|
|
 |
Reference
- ↑ Pappas G, Akritidis N, Bosilkovski M, Tsianos E (2005). "Brucellosis". N Engl J Med. 352 (22): 2325–36. doi:10.1056/NEJMra050570. PMID 15930423.
- ↑ Brucellosis "Dennis Kasper, Anthony Fauci, Stephen Hauser, Dan Longo, J. Larry Jameson, Joseph Loscalzo"Harrison's Principles of Internal Medicine, 19e Accessed on January,2017
- ↑ Young EJ (1995). "Brucellosis: current epidemiology, diagnosis, and management". Curr Clin Top Infect Dis. 15: 115–28. PMID 7546364.
- ↑ Enfermedades infecciosas: Brucelosis -Diagnóstico de Brucelosis,Guia para el Equipo de Salud. Ministerio de Salud-Argentina. http://www.msal.gob.ar/images/stories/bes/graficos/0000000304cnt-guia-medica-brucelosis.pdf. Accessed on February 2, 2016
- ↑ 5.0 5.1 5.2 5.3 Irfan M, Farooqi J, Hasan R (2013). "Community-acquired pneumonia". Curr Opin Pulm Med. 19 (3): 198–208. doi:10.1097/MCP.0b013e32835f1d12. PMID 23422417.