Acoustic neuroma MRI
|
Acoustic neuroma Microchapters | |
|
Diagnosis | |
|---|---|
|
Treatment | |
|
Case Studies | |
|
Acoustic neuroma MRI On the Web | |
|
American Roentgen Ray Society Images of Acoustic neuroma MRI | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Contrast-enhanced CT will detect almost all acoustic neuromas that are greater than 2.0 cm in diameter and project further than 1.5 cm into the cerebellopontine angle. Those tumors that are smaller may be detected by MRI with gadolinium enhancement. Audiology and vestibular tests should be concurrently evaluated using air conduction and bone conduction threshold testing to assess for sensorineural versus conduction hearing loss.
MRI
Acoustic neuromas are most frequently diagnosed by MRI scan in a patient with unilateral hearing loss. Important information to be determined from the MRI scan are distance the tumor extends laterally in the auditory canal, the extent to which the tumor expands in the cerebello-pontine angle, and whether or not the brain stem is contacted or distorted The definitive diagnostic test for patients with acoustic tumors is gadolinium-enhanced MRI.
- Well-performed scanning can demonstrate tumors as small as 1-2 mm in diameter. On the other hand, thin-cut CT scanning can miss tumors as large as 1.5 cm even when intravenous contrast enhancement is used.
- Gadolinium contrast is critical because nonenhanced MRI can miss small tumors.
- Fast-spin echo techniques do not require gadolinium enhancement and can be performed very rapidly and relatively inexpensively. However, such highly targeted techniques risk missing other important causes of unilateral sensory hearing loss, including intra-axial tumors, demyelinating disease, and infarcts.
- MRI is contraindicated in individuals with ferromagnetic implants.
- Fine-cut CT scanning of the internal auditory canal with contrast can rule out a medium-size or large tumor but cannot be relied upon to detect a tumor smaller than 1-1.5 cm.
- If suspicion is high and MRI is contraindicated, air-contrast cisternography has high sensitivity and can detect relatively small intracanalicular tumors.
References
- Well-performed scanning can demonstrate tumors as small as 1-2 mm in diameter. On the other hand, thin-cut CT scanning can miss tumors as large as 1.5 cm even when intravenous contrast enhancement is used.
- Gadolinium contrast is critical because nonenhanced MRI can miss small tumors.
- Fast-spin echo techniques do not require gadolinium enhancement and can be performed very rapidly and relatively inexpensively. However, such highly targeted techniques risk missing other important causes of unilateral sensory hearing loss, including intra-axial tumors, demyelinating disease, and infarcts.
- MRI is contraindicated in individuals with ferromagnetic implants.>
- Fine-cut CT scanning of the internal auditory canal with contrast can rule out a medium-size or large tumor but cannot be relied upon to detect a tumor smaller than 1-1.5 cm.
- If suspicion is high and MRI is contraindicated, air-contrast cisternography has high sensitivity and can detect relatively small intracanalicular tumors.
MRI Classification of Acoustic Neuroma:
Since these tumors are entirely within the bony canal, they pose no threat to the brain or cranial nervesother than VII and VIII, which are in the canal. Therefore, the crucial questions are how severely affected are the nerves already and how fast is the tumor growing. Since the nerve most susceptible to pressure is the auditory component of nerve VIII, a detailed hearing test and auditory evoked potentials should be performed. If useful hearing is present, it is advisable to remove the tumor or treat it with stereotactic radiation before it becomes larger. With microsurgery, the tumor can be completely removed with minimal risk and a reasonable chance of preserving hearing. Facial nerve and auditory monitoring are, of course, required. With stereotactic radiation therapy, no actual surgery is required but the tumor will still be present and will need to be followed indefinitely by MRI scans. The outcome for preservation of hearing is similar in both techniques.
If useful hearing is not present, it is reasonable to follow the tumor for one year with a repeat MRI scan to see if it is growing before making a decision regarding surgery, radiation, or more waiting. However, if knowing you have a tumor in your head and not doing something is unacceptable, it is appropriate to proceed with surgery or stereotactic radiation.
Intracranial extension without brainstem distortion
These tumors have already demonstrated their propensity to grow, but are not yet life-threatening. They should be surgically removed if the general health of the patient permits; otherwise, they should be treated with stereotactic radiation. The surgical approach depends on the status of the hearing and the preference of the surgeon, but the primary objective other than total removal of the tumor should be to preserve the facial nerve. This requires facial nerve monitoring during the course of the operation. If useful hearing is still present, an effort should be made to preserve it by intraoperative auditory monitoring and selecting a surgical approach which does not damage the cochlea.
Intracranial extension with brainstem distortion
Large tumors which distort the brain stem are potentially life-threatening and should be surgically removed as soon as possible. The goal should be total removal, but great care must be taken to ensure that neither the brain stem nor its blood supply are injured in the process. Preservation of the facial nerve also remains important, and it may be necessary to leave a portion of tumor capsule to protect the brain stem, blood vessels or facial nerve. The possibility of preserving any hearing with large tumors is minimal |}
-
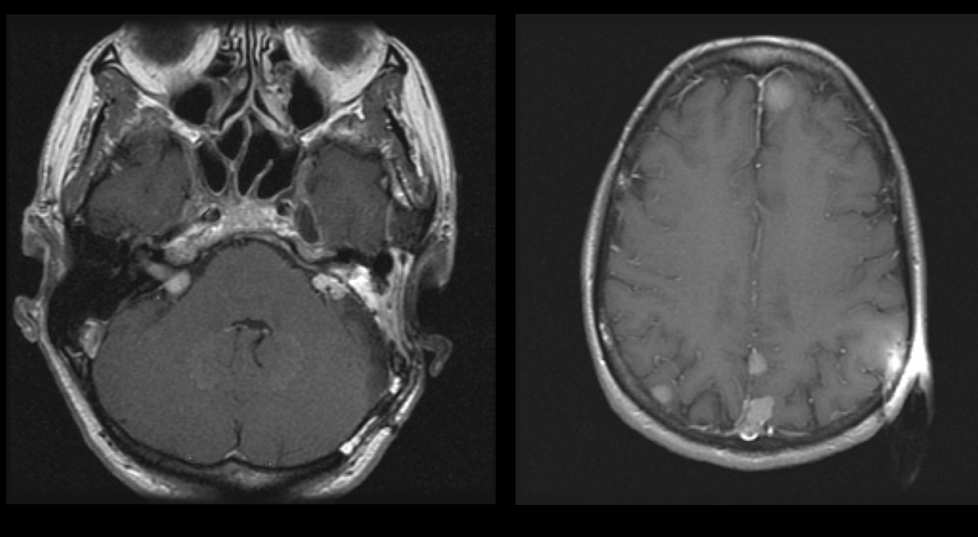
Axial image of a patient with bilateral acoustic neuromas. the patient has NF2. The right image is a higher image in the same patient showing multiple meningiomas
-
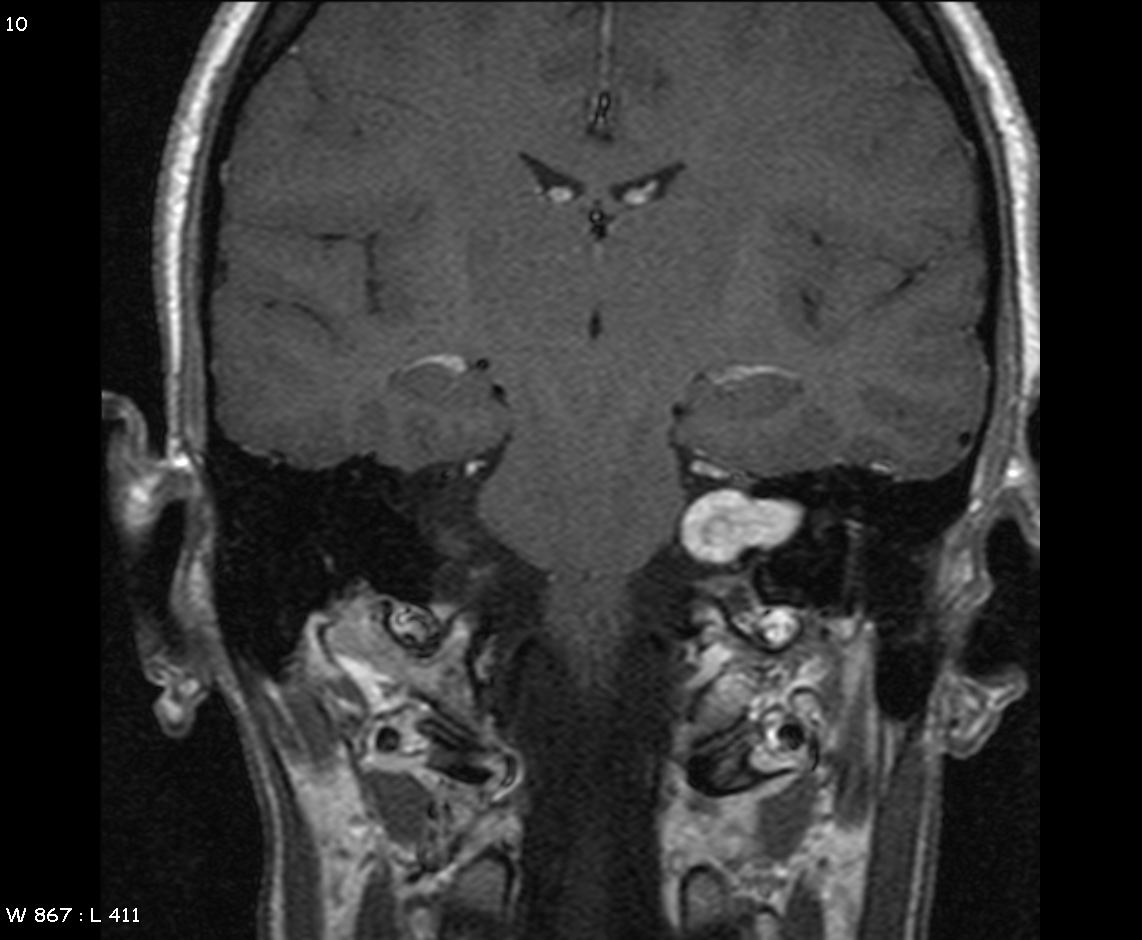
MRI demonstrating left acoustic neuroma in the CP angle