Abdominal pain differential diagnosis: Difference between revisions
Iqra Qamar (talk | contribs) No edit summary |
Iqra Qamar (talk | contribs) |
||
| Line 22: | Line 22: | ||
! colspan="3" rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Classification of pain in the abdomen based on etiology | ! colspan="3" rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Classification of pain in the abdomen based on etiology | ||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
| colspan=" | | colspan="13" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Clinical manifestations''' | ||
! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diagnosis | ! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diagnosis | ||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | ! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | ||
|- | |- | ||
| colspan=" | | colspan="9" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Symptoms''' | ||
! colspan="4" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Signs | ! colspan="4" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Signs | ||
|- | |- | ||
| Line 32: | Line 32: | ||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | ! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI bleeding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | ||
tension | tension | ||
| Line 43: | Line 46: | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | ||
|- | |- | ||
! rowspan=" | ! rowspan="55" style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal causes | ||
! | ! rowspan="40" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Inflammatory causes | ||
! rowspan=" | ! rowspan="10" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pancreato-biliary disorders | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Acute suppurative cholangitis | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Acute suppurative cholangitis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 58: | Line 64: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Abnormal [[LFT]] | *Abnormal [[LFT]] | ||
* WBC >10,000 | *WBC >10,000 | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[biliary]] dilatation/stents/tumor | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[biliary]] dilatation/stents/tumor | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Septic shock occurs with features of [[SIRS]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Septic shock occurs with features of [[SIRS]] | ||
| Line 67: | Line 73: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 81: | Line 90: | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | [[Acute cholecystitis|Acute cholecystitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | [[Acute cholecystitis|Acute cholecystitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | [[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | [[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 100: | Line 112: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 116: | Line 131: | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Chronic pancreatitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Chronic pancreatitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Increased [[amylase]] / [[lipase]] | * Increased [[amylase]] / [[lipase]] | ||
* | * Increased stool fat content | ||
* Pancreatic function test | * Pancreatic function test | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | ||
| Line 135: | Line 152: | ||
* Dilation of main pancreatic duct | * Dilation of main pancreatic duct | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Predisposes to pancreatic cancer | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Predisposes to pancreatic cancer | ||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Pancreatic carcinoma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* ↑ [[Alkaline phosphatase]] | |||
* ↑ [[Bilirubin|serum bilirubin]] | |||
* ↑ [[gamma-glutamyl transpeptidase]] | |||
* ↑ [[CA 19-9]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Computed tomography|MDCT]] with [[Positron emission tomography|PET]]/[[Computed tomography|CT]] | |||
* MRI | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[Skin]] manifestations may include: | |||
* [[Bullous pemphigoid]] | |||
* [[Mucous membrane pemphigoid|Cicatricial pemphigoid]] | |||
* [[Thrombophlebitis|Migratory superficial thrombophlebitis]] (classic [[Trousseau's syndrome]]) | |||
* [[Panniculitis|Pancreatic panniculitis]] | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI bleeding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Primary biliary cirrhosis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Primary biliary cirrhosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]]/[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]]/[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 150: | Line 218: | ||
* Increased AMA level, abnormal [[LFTs]] | * Increased AMA level, abnormal [[LFTs]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* ERCP | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Pruritis | |||
|- | |- | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Primary sclerosing cholangitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Primary sclerosing cholangitis]] | ||
| Line 156: | Line 226: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 183: | Line 256: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 188: | Line 264: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal to hyperactive for dislodged stone | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | * [[Leukocytosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound shows [[gallstone]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Fatty food intolerance | * Ultrasound shows [[gallstone]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Fatty food intolerance | |||
|- | |- | ||
! colspan="1" rowspan=" | ! colspan="1" rowspan="8" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Gastric causes | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | [[Peptic Ulcer Disease|Peptic ulcer disease]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | [[Peptic Ulcer Disease|Peptic ulcer disease]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | | ||
* Gastric ulcer- [[melena]] and [[hematemesis]] | * Gastric ulcer- [[melena]] and [[hematemesis]] | ||
* Duodenal ulcer- [[melena]] and [[hematochezia]] | * Duodenal ulcer- [[melena]] and [[hematochezia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if perforated | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 213: | Line 294: | ||
** Glucose < 50mg/dl | ** Glucose < 50mg/dl | ||
** Total protein > 1g/dl | ** Total protein > 1g/dl | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Air under [[diaphragm]] in upright [[CXR]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Upper GI [[endoscopy]] for diagnosis | * Air under [[diaphragm]] in upright [[CXR]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Upper GI [[endoscopy]] for diagnosis | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI bleeding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastritis|Gastritis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastritis|Gastritis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + in chronic gastritis | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in chronic gastritis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[H.pylori infection diagnostic tests]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[H.pylori infection diagnostic tests]] | ||
| Line 233: | Line 338: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastroesophageal reflux disease|Gastroesophageal reflux disease]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastroesophageal reflux disease|Gastroesophageal reflux disease]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Gastric emptying studies | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Gastric emptying studies | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Endoscopy]] for alarm signs | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Esophageal]] [[manometry]], [[Endoscopy]] for alarm signs | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastric outlet obstruction|Gastric outlet obstruction]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastric outlet obstruction|Gastric outlet obstruction]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | <nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 264: | Line 375: | ||
* Barium upper GI studies- narrowed pylorus | * Barium upper GI studies- narrowed pylorus | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Succussion splash | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Succussion splash | ||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gastroparesis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Epigastric | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Hyperactive/hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Hemoglobin | |||
*Fasting plasma glucose | |||
*Serum total protein, albumin, thyrotropin (TSH), and an antinuclear antibody (ANA) titer | |||
*HbA1c | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Scintigraphic gastric emptying | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Succussion splash | |||
*Single photon emission computed tomography (SPECT) | |||
*Full thickness gastric and small intestinal biopsy | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastrointestinal perforation]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastrointestinal perforation]] | ||
| Line 269: | Line 406: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 283: | Line 423: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Dumping syndrome]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Dumping syndrome]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Lower and then diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Lower and then diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 300: | Line 443: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Postgastrectomy | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Postgastrectomy | ||
|- | |- | ||
! rowspan=" | ! rowspan="13" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intestinal causes | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Acute appendicitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Acute appendicitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Starts in [[epigastrium]], migrates to RLQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Starts in [[epigastrium]], migrates to RLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in pyogenic appendicitis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated appendicitis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 314: | Line 479: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | * [[Leukocytosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ct scan and | ||
Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]], [[decreased appetite]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]], [[decreased appetite]] | ||
|- | |- | ||
| Line 321: | Line 487: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + in perforated diverticulitis | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated diverticulitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 336: | Line 505: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal or hyperactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | * [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | ||
| Line 355: | Line 527: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Irritable bowel syndrome]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Irritable bowel syndrome]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 364: | Line 539: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Symptomatic treatment | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Symptomatic treatment | ||
* High [[dietary fiber]] | * High [[dietary fiber]] | ||
| Line 375: | Line 550: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| Line 401: | Line 579: | ||
* [[Arthritis]] | * [[Arthritis]] | ||
* [[Ascites]] | * [[Ascites]] | ||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Toxic megacolon]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Toxic megacolon]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 419: | Line 619: | ||
*[[Metabolic alkalosis]] associated with a poor [[prognosis]] | *[[Metabolic alkalosis]] associated with a poor [[prognosis]] | ||
*[[Metabolic acidosis]] secondary to [[ischemic colitis]] | *[[Metabolic acidosis]] secondary to [[ischemic colitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT and [[Ultrasound]] shows: | ||
*Loss of colonic haustration | |||
[[Ultrasound]] shows: | |||
*Loss of | |||
*Hypoechoic and thickened bowel walls with irregular internal margins in the [[sigmoid]] and descending colon | *Hypoechoic and thickened bowel walls with irregular internal margins in the [[sigmoid]] and descending colon | ||
*Prominent dilation of the transverse colon (>6 cm) | *Prominent dilation of the transverse colon (>6 cm) | ||
| Line 435: | Line 630: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 452: | Line 650: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Celiac disease]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Celiac disease]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 474: | Line 675: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in fulminant colitis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 491: | Line 695: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
|- | |- | ||
! rowspan=" | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Colon carcinoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse/localized | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal | |||
* Hyperactive if obstruction present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CBC | |||
* Carcinoembryonic antigen (CEA) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Colonoscopy | |||
* Flexible sigmoidoscopy | |||
* Barium enema | |||
* CT colonography | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |PILLCAM 2: A colon capsule for CRC screening may be used in patients with an incomplete colonoscopy who lacks obstruction | |||
|- | |||
! rowspan="8" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hepatic causes | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hepatitis|Viral hepatitis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hepatitis|Viral hepatitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + in fulminant hepatitis | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in Hep A and E | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in fulminant hepatitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in acute | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| Line 506: | Line 758: | ||
* Abnormal LFTs | * Abnormal LFTs | ||
* Viral serology | * Viral serology | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |US | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hep A and E have fecoral route of transmission and Hep B and C transmits via blood transfusion and sexual contact. | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hep A and E have fecoral route of transmission and Hep B and C transmits via blood transfusion and sexual contact. | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Liver | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Liver abscess]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal or hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* CBC | * CBC | ||
* | * Blood cultures | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | * Abnormal [[Liver function test|liver function tests]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* US | |||
* CT | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hepatocellular carcinoma]]/Metastasis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal | |||
* Hyperactive if obstruction present | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* High levels of [[Alpha-fetoprotein|AFP]] in serum | |||
* Abnormal [[Liver function test|liver function tests]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* US | |||
* CT | |||
* Liver biopsy | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
Other symptoms: | |||
* [[Splenomegaly]] | |||
* [[Variceal bleeding]] | |||
* [[Ascites]] | |||
* [[Spider nevi]] | |||
* [[Asterixis]] | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Budd-Chiari syndrome|Budd-Chiari syndrome]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Budd-Chiari syndrome|Budd-Chiari syndrome]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in liver failure leading to varices | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 557: | Line 868: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=" | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in cirrhotic patients | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* >60% TS | * >60% TS | ||
| Line 583: | Line 897: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Cirrhosis|Cirrhosis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Cirrhosis|Cirrhosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| Line 605: | Line 922: | ||
* Cruveilhier- Baumgarten murmur | * Cruveilhier- Baumgarten murmur | ||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="center" | Peritoneal causes | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
! rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Peritoneal causes | |||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Spontaneous bacterial peritonitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Spontaneous bacterial peritonitis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in cirrhotic patients | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| Line 619: | Line 958: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Ascitic fluid [[PMN]]>250 cells/mm<small>³</small> | * Ascitic fluid [[PMN]]>250 cells/mm<small>³</small> | ||
* Culture: Positive for single organism | * Culture: Positive for single organism | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound for evaluation of liver cirrhosis | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound for evaluation of liver cirrhosis | ||
! style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
|- | |||
! colspan="2" rowspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Renal causes | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pyelonephritis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Unilateral | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Urinalysis | |||
* Urine culture | |||
* Blood culture | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT | |||
* MRI | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*CVA tenderness | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Renal colic]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Flank pain]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Hematuria]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan and ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Colicky [[abdominal pain]] | |||
* [[Dysuria]] | |||
|- | |- | ||
! colspan="2" rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Hollow Viscous Obstruction | ! colspan="2" rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Hollow Viscous Obstruction | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Small | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Small bowel obstruction | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 638: | Line 1,024: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] with left shift indicates complications | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] with left shift indicates complications | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal X-ray|Abdominal X ray]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal X-ray|Abdominal X ray]] | ||
* | * Dilated loops of bowel with air fluid levels | ||
* | * Gasless abdomen | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* "Target sign"– , indicative of intussusception | * "Target sign"– , indicative of intussusception | ||
| Line 646: | Line 1,032: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Volvulus]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Volvulus]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated cases | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in perforated cases | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 664: | Line 1,053: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 675: | Line 1,067: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Nausea and vomiting|Nausea & vomiting]] | ||
|- | |- | ||
| style=" | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
| style=" | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
! rowspan=" | ! rowspan="5" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Vascular Disorders | ||
! rowspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Ischemic causes | ! rowspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Ischemic causes | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Mesenteric ischemia]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Mesenteric ischemia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Periumbilical | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Periumbilical | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Positive if bowel becomes gangrenous | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + if bowel becomes gangrenous | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive if bowel becomes gangrenous | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive to absent | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive to absent | ||
| Line 717: | Line 1,114: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| Line 730: | Line 1,130: | ||
* Double halo appearance, thumbprinting | * Double halo appearance, thumbprinting | ||
* Thickening of bowel | * Thickening of bowel | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |May lead to shock | ||
|- | |- | ||
! rowspan=" | ! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hemorrhagic causes | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ruptured abdominal aortic aneurysm]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ruptured abdominal aortic aneurysm]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 753: | Line 1,156: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 764: | Line 1,170: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of [[trauma]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of [[trauma]] | ||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Constipation | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Diarrhea | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Weight loss | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |GI Bleed | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Hypo- | |||
tension | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Guarding | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rebound Tenderness | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Bowel sounds | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Lab Findings | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Imaging | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |- | ||
! rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gynaecological Causes | ! rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gynaecological Causes | ||
| Line 769: | Line 1,194: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Torsion of the cyst | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Torsion of the cyst | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 774: | Line 1,203: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| Line 786: | Line 1,214: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 799: | Line 1,230: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cyst rupture | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cyst rupture | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 815: | Line 1,249: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Ruptured [[ectopic pregnancy]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Ruptured [[ectopic pregnancy]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 828: | Line 1,265: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of missed period and [[vaginal bleeding]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of missed period and [[vaginal bleeding]] | ||
|- | |- | ||
! rowspan=" | ! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra-abdominal causes | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pulmonary disorders | ! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pulmonary disorders | ||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Pleural empyema]] | | colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Pleural empyema]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]]/[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[RUQ]]/[[Epigastric]] | ||
| Line 836: | Line 1,273: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 850: | Line 1,290: | ||
* [[Egophony]] | * [[Egophony]] | ||
* Increased [[tactile fremitus]] | * Increased [[tactile fremitus]] | ||
|- | |||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pulmonary embolism | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* ABGs | |||
* D-dimer | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CXR | |||
* V/Q scan | |||
* Spiral [[CT pulmonary angiogram]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Dyspnea | |||
* Tachycardia | |||
* Pleuretic chest pain | |||
|- | |||
! colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pneumonia | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Normal or hypoactive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* ABGs | |||
* Eosinophilia | |||
* Pancytopenia | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
* CXR | |||
* CT chest | |||
* Bronchoscopy | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cardiovascular disorders | ! style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cardiovascular disorders | ||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Myocardial Infarction]] | | colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Myocardial Infarction]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 859: | Line 1,352: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | Positive in cardiogenic shock | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Cardiac enzymes]] | * [[Cardiac enzymes]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Echocardiogram]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[ECG]] | ||
[[Echocardiogram]] | |||
* Wall motion abnormality | * Wall motion abnormality | ||
* Wall rupture | * Wall rupture | ||
| Line 878: | Line 1,371: | ||
|} | |} | ||
|} | |} | ||
{| | {| | ||
|- | |- | ||
| [[Image:Right_upper_quadrant.PNG|link=Right upper quadrant abdominal pain resident survival guide]]||[[Image:Epigastric_quadrant_pain.PNG|link=Epigastric pain resident survival guide]]||[[Image:Left_upper_quadrant.PNG|link=Left upper quadrant abdominal pain resident survival guide]] | | [[Image:Right_upper_quadrant.PNG|link=Right upper quadrant abdominal pain resident survival guide]]||[[Image:Epigastric_quadrant_pain.PNG|link=Epigastric pain resident survival guide]]||[[Image:Left_upper_quadrant.PNG|link=Left upper quadrant abdominal pain resident survival guide]] | ||
|- | |- | ||
| Line 887: | Line 1,380: | ||
| [[Image:Right_lower_quadrant.PNG|link=Right lower quadrant abdominal pain resident survival guide]]||[[Image:Hypogastric.PNG|link=Hypogastric pain resident survival guide]]||[[Image:Left_lower_quadrant.PNG|link=Left lower quadrant abdominal pain resident survival guide]] | | [[Image:Right_lower_quadrant.PNG|link=Right lower quadrant abdominal pain resident survival guide]]||[[Image:Hypogastric.PNG|link=Hypogastric pain resident survival guide]]||[[Image:Left_lower_quadrant.PNG|link=Left lower quadrant abdominal pain resident survival guide]] | ||
|} | |} | ||
The following is a list of diseases that present with acute onset severe lower abdominal pain: | The following is a list of diseases that present with acute onset severe lower abdominal pain: | ||
Revision as of 01:13, 30 November 2017
| <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline> |
Resident Survival Guide |
|
Abdominal pain Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Abdominal pain On the Web |
|
American Roentgen Ray Society Images of Abdominal pain |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]Amandeep Singh M.D.[3]
Overview
Diagnosing the cause of abdominal pain can be difficult, because many diseases can cause this symptom. Most frequently the cause is benign and/or self-limiting, but more serious causes may require urgent intervention. Acute abdominal pain is a severe, persistent abdominal pain of sudden onset that is likely to require surgical intervention to treat its cause. The following table summarizes differential diagnosis for abdominal pain.
Differential diagnosis of abdominal pain
Abbreviations: RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein, TS= Transferrin saturation, SF= Serum Ferritin, SMA= Superior mesenteric artery, SMV= Superior mesenteric vein, ECG= Electrocardiogram
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
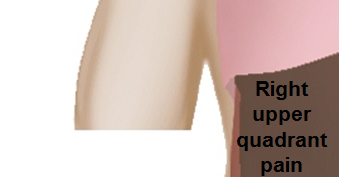 |
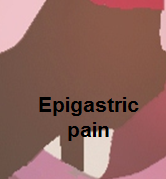 |

|
 |
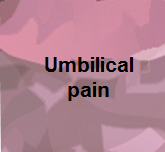 |

|
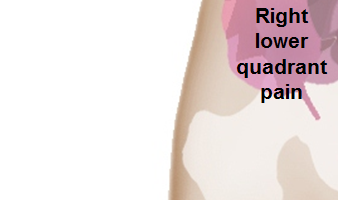 |
 |

|
The following is a list of diseases that present with acute onset severe lower abdominal pain:
| Disease | Findings |
|---|---|
| Ectopic pregnancy | History of missed menses, positive pregnancy test, ultrasound reveals an empty uterus and may show a mass in the fallopian tubes.[1] |
| Appendicitis | Pain localized to the right iliac fossa, vomiting, abdominal ultrasound sensitivity for diagnosis of acute appendicitis is 75% to 90%.[2] |
| Rupturedovarian cyst | Usually spontaneous, can follow history of trauma, mild chronic lower abdominal discomfort may suddenly intensify, ultrasound is diagnostic.[3] |
| Ovarian cyst torsion | Presents with acute severe unilateral lower quadrant abdominal pain, nausea and vomiting, tender adnexal mass palpated in 90%, ultrasound is diagnostic.[4] |
| Hemorrhagic ovarian cyst | Presents with localized abdominal pain, nausea and vomiting. Hypovolemic shock may be present, abdominal tenderness and guarding are physical exam findings, ultrasound is diagnostic.[4] |
| Endometriosis | Presents with cyclic pain that is exacerbated by onset of menses, dyspareunia. laparoscopic exploration is diagnostic.[4] |
| Acute cystitis | Presents with features of increased urinary frequency, urgency, dysuria, and suprapubic pain.[5][6] |
References
- ↑ Morin L, Cargill YM, Glanc P (2016). "Ultrasound Evaluation of First Trimester Complications of Pregnancy". J Obstet Gynaecol Can. 38 (10): 982–988. doi:10.1016/j.jogc.2016.06.001. PMID 27720100.
- ↑ Balthazar EJ, Birnbaum BA, Yee J, Megibow AJ, Roshkow J, Gray C (1994). "Acute appendicitis: CT and US correlation in 100 patients". Radiology. 190 (1): 31–5. doi:10.1148/radiology.190.1.8259423. PMID 8259423.
- ↑ Bottomley C, Bourne T (2009). "Diagnosis and management of ovarian cyst accidents". Best Pract Res Clin Obstet Gynaecol. 23 (5): 711–24. doi:10.1016/j.bpobgyn.2009.02.001. PMID 19299205.
- ↑ 4.0 4.1 4.2 Bhavsar AK, Gelner EJ, Shorma T (2016). "Common Questions About the Evaluation of Acute Pelvic Pain". Am Fam Physician. 93 (1): 41–8. PMID 26760839.
- ↑ {{Cite journal | author = W. E. Stamm | title = Etiology and management of the acute urethral syndrome | journal = Sexually transmitted diseases | volume = 8 | issue = 3 | pages = 235–238 | year = 1981 | month = July-September | pmid = 7292216
- ↑ {{Cite journal | author = W. E. Stamm, K. F. Wagner, R. Amsel, E. R. Alexander, M. Turck, G. W. Counts & K. K. Holmes | title = Causes of the acute urethral syndrome in women | journal = The New England journal of medicine | volume = 303 | issue = 8 | pages = 409–415 | year = 1980 | month = August | doi = 10.1056/NEJM198008213030801 | pmid = 6993946