Abdominal pain differential diagnosis: Difference between revisions
Iqra Qamar (talk | contribs) No edit summary |
m (Bot: Removing from Primary care) |
||
| (33 intermediate revisions by 7 users not shown) | |||
| Line 2: | Line 2: | ||
{| class="infobox" style="float:right;" | {| class="infobox" style="float:right;" | ||
|- | |- | ||
| | |[[image:Siren.gif|link=Abdominal pain resident survival guide|41x41px]] | ||
| [[Abdominal pain resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |[[Abdominal pain resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | ||
|} | |} | ||
[[Image:Home_logo1.png|right|250px|https://www.wikidoc.org/index.php/Abdominal pain]] | |||
| | {{CMG}};{{AE}}{{ADS}}{{MehdiP}}{{IQ}} | ||
{{CMG}};{{AE}}{{ | |||
==Overview== | ==Overview== | ||
Diagnosing the cause of abdominal pain can be difficult, because many diseases can cause this symptom. Most frequently the cause is benign and/or self-limiting, but more serious causes may require urgent intervention. Acute abdominal pain is a severe, persistent abdominal pain of sudden onset that is likely to require surgical intervention to treat its cause. The following table summarizes differential diagnosis for abdominal pain. | Diagnosing the cause of abdominal pain can be difficult, because many diseases can cause this symptom. Most frequently the cause is benign and/or self-limiting, but more serious causes may require urgent intervention. Acute abdominal pain is a severe, persistent abdominal pain of sudden onset that is likely to require surgical intervention to treat its cause. The following table summarizes differential diagnosis for abdominal pain. | ||
==Differential diagnosis of | ==Differential Diagnosis of Abdominal Pain== | ||
<span style="font-size:85%">'''Abbreviations:''' | '''''To review the differential diagnosis of Abdominal pain, click [[Abdominal pain differential diagnosis#Abdominal Pain|here]]'''.'' | ||
'''[[RUQ]]'''= Right upper quadrant of the abdomen, '''LUQ'''= Left upper quadrant, '''LLQ'''= Left lower quadrant, '''RLQ'''= Right lower quadrant, '''LFT'''= Liver function test, SIRS= [[Systemic inflammatory response syndrome]], '''[[ERCP]]'''= [[Endoscopic retrograde cholangiopancreatography]], '''IV'''= Intravenous, '''N'''= Normal, '''AMA'''= Anti mitochondrial antibodies, '''[[LDH]]'''= [[Lactate dehydrogenase]], '''GI'''= Gastrointestinal, '''CXR'''= Chest X ray, '''IgA'''= [[Immunoglobulin A]], '''IgG'''= [[Immunoglobulin G]], '''IgM'''= [[Immunoglobulin M]], '''CT'''= [[Computed tomography]], '''[[PMN]]'''= Polymorphonuclear cells, '''[[ESR]]'''= [[Erythrocyte sedimentation rate]], '''[[CRP]]'''= [[C-reactive protein]], TS= [[Transferrin saturation]], SF= Serum [[Ferritin]], SMA= [[Superior mesenteric artery]], SMV= [[Superior mesenteric vein]], ECG= [[Electrocardiogram]]</span> | |||
'''''To review the differential diagnosis of Abdominal pain and fever, click [[Abdominal pain and fever|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea and vomiting, click [[Abdominal pain, nausea and vomiting|here]]'''.'' | |||
{| | |||
'''''To review the differential diagnosis of Abdominal pain and jaundice, click [[Abdominal pain and jaundice|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain and weight loss, click [[Abdominal pain and weight loss|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain and constipation, click [[Abdominal pain and constipation|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain and diarrhea, click [[Abdominal pain and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain and GI bleeding, click [[Abdominal pain and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever and jaundice, click [[Abdominal pain, fever and jaundice|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever, nausea and vomiting, click [[Abdominal pain, fever, nausea and vomiting|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever, and diarrhea, click [[Abdominal pain, fever and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever and constipation, click [[Abdominal pain, fever and constipation|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever and weight loss, click [[Abdominal pain, fever and weight loss|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, fever and GI bleeding, click [[Abdominal pain, fever and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea,vomiting and jaundice, click [[Abdominal pain, nausea,vomiting and jaundice|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea,vomiting and weight loss, click [[Abdominal pain, nausea,vomiting and weight loss|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea,vomiting and constipation, click [[Abdominal pain, nausea,vomiting and constipation|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea,vomiting and diarrhea, click [[Abdominal pain, nausea,vomiting and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, nausea, vomiting and GI bleeding, click [[Abdominal pain, nausea,vomiting and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, jaundice and weight loss, click [[Abdominal pain, jaundice and weight loss|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, jaundice and diarrhea, click [[Abdominal pain, jaundice and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, jaundice and GI bleeding, click [[Abdominal pain, jaundice and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain,weight loss and constipation, click [[Abdominal pain,weight loss and constipation|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain,weight loss and diarrhea, click [[Abdominal pain,weight loss and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, weight loss and GI bleeding, click [[Abdominal pain,weight loss and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, constipation and diarrhea, click [[Abdominal pain, constipation and diarrhea|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, constipation and GI bleeding, click [[Abdominal pain, constipation and GI bleeding|here]]'''.'' | |||
'''''To review the differential diagnosis of Abdominal pain, diarrhea and GI bleeding, click [[Abdominal pain, diarrhea and GI bleeding|here]]'''.'' | |||
===Abdominal Pain=== | |||
'''The following table outlines the major differential diagnoses of abdominal pain.''' | |||
<span style="font-size:85%">'''Abbreviations:''' | |||
'''[[RUQ]]'''= Right upper quadrant of the abdomen, '''LUQ'''= Left upper quadrant, '''LLQ'''= Left lower quadrant, '''RLQ'''= Right lower quadrant, '''LFT'''= Liver function test, SIRS= [[Systemic inflammatory response syndrome]], '''[[ERCP]]'''= [[Endoscopic retrograde cholangiopancreatography]], '''IV'''= Intravenous, '''N'''= Normal, '''AMA'''= Anti mitochondrial antibodies, '''[[LDH]]'''= [[Lactate dehydrogenase]], '''GI'''= Gastrointestinal, '''CXR'''= Chest X ray, '''IgA'''= [[Immunoglobulin A]], '''IgG'''= [[Immunoglobulin G]], '''IgM'''= [[Immunoglobulin M]], '''CT'''= [[Computed tomography]], '''[[PMN]]'''= Polymorphonuclear cells, '''[[ESR]]'''= [[Erythrocyte sedimentation rate]], '''[[CRP]]'''= [[C-reactive protein]], TS= [[Transferrin saturation]], SF= Serum [[Ferritin]], SMA= [[Superior mesenteric artery]], SMV= [[Superior mesenteric vein]], ECG= [[Electrocardiogram]], US = [[Ultrasound]]</span> | |||
<small><small> | |||
{| align="center" | |||
|- | |- | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | | | ||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | ! colspan="3" rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Classification of pain in the abdomen based on etiology | ||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | |||
| colspan="13" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Clinical manifestations''' | |||
! colspan="2" rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" |Diagnosis | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
| colspan="9" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |'''Symptoms''' | |||
! colspan="4" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Signs | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Abdominal Pain | |||
! colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" | Fever | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Rigors and chills | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Nausea or vomiting | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Jaundice | ||
| Line 123: | Line 182: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |− | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| Line 258: | Line 317: | ||
* [[Biliary]] dilatation and diverticula | * [[Biliary]] dilatation and diverticula | ||
* Distortion of biliary tree | * Distortion of biliary tree | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |The risk of [[cholangiocarcinoma]] in patients with primary sclerosing cholangitis is 400 times higher than the risk in the general population. | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* The risk of [[cholangiocarcinoma]] in patients with primary sclerosing cholangitis is 400 times higher than the risk in the general population. | |||
|- | |- | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Cholelithiasis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Cholelithiasis]] | ||
| Line 341: | Line 401: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[H.pylori infection diagnostic tests]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Endoscopy]] | * [[H.pylori infection diagnostic tests]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[H.pylori gastritis guideline recommendation]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Endoscopy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[H.pylori gastritis guideline recommendation]] | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastroesophageal reflux disease|Gastroesophageal reflux disease]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastroesophageal reflux disease|Gastroesophageal reflux disease]] | ||
| Line 360: | Line 423: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Gastric emptying studies | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Esophageal]] [[manometry]] | * Gastric emptying studies | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Esophageal]] [[manometry]] | |||
* [[Endoscopy]] for alarm signs | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastric outlet obstruction|Gastric outlet obstruction]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastric outlet obstruction|Gastric outlet obstruction]] | ||
| Line 382: | Line 448: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Abdominal x-ray]]- air fluid level | * [[Abdominal x-ray]]- air fluid level | ||
* Barium upper GI studies- narrowed pylorus | * Barium [[Upper GI series|upper GI studies]]- narrowed pylorus | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Succussion splash | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Succussion splash | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gastroparesis | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Gastroparesis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Epigastric | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Epigastric]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 400: | Line 467: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Hyperactive/hypoactive | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Hyperactive/hypoactive | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Hemoglobin | *[[Hemoglobin]] | ||
*Fasting plasma glucose | *Fasting plasma glucose | ||
*Serum total protein, albumin, thyrotropin (TSH), and an antinuclear antibody (ANA) titer | *Serum total protein, albumin, [[thyrotropin]] ([[Thyroid-stimulating hormone|TSH]]), and an [[antinuclear antibody]] (ANA) titer | ||
*HbA1c | *[[HbA1c]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Scintigraphic gastric emptying | *Scintigraphic gastric emptying | ||
| Line 427: | Line 494: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* WBC> 10,000 | * WBC> 10,000 | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Air under [[diaphragm]] in upright [[CXR]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Hamman's sign]] | * Air under [[diaphragm]] in upright [[CXR]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Hamman's sign]] | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Dumping syndrome]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Dumping syndrome]] | ||
| Line 446: | Line 515: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Glucose challenge test | * Glucose challenge test | ||
* Hydrogen breath test | * [[Hydrogen Breath Test|Hydrogen breath test]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Upper GI series | * [[Upper gastrointestinal series|Upper GI series]] | ||
* Gastric emptying study | * Gastric emptying study | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Postgastrectomy | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Postgastrectomy | |||
|- | |- | ||
! rowspan="13" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intestinal causes | ! rowspan="13" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intestinal causes | ||
| Line 488: | Line 558: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | * [[Leukocytosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ct scan | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
Ultrasound | * Ct scan | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | * Ultrasound | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Positive Rovsing sign | |||
* Positive Obturator sign | |||
* Positive Iliopsoas sign | |||
|- | |- | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diverticulitis|Acute diverticulitis]] | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Diverticulitis|Acute diverticulitis]] | ||
| Line 508: | Line 582: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | * [[Leukocytosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of [[constipation]] | * CT scan | ||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[constipation]] | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Inflammatory bowel disease]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Inflammatory bowel disease]] | ||
| Line 528: | Line 605: | ||
* [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | * [[Anti-neutrophil cytoplasmic antibody]] ([[P-ANCA]]) in [[Ulcerative colitis]] | ||
* [[Anti saccharomyces cerevisiae antibodies]] (ASCA) in [[Crohn's disease]] | * [[Anti saccharomyces cerevisiae antibodies]] (ASCA) in [[Crohn's disease]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[String sign]] on [[abdominal x-ray]] in [[Crohn's disease]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[String sign]] on [[abdominal x-ray]] in [[Crohn's disease]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
Extra intestinal findings: | Extra intestinal findings: | ||
| Line 654: | Line 732: | ||
* [[Hypoalbuminemia]] | * [[Hypoalbuminemia]] | ||
* Fecal stool test | * Fecal stool test | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Barium studies | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Barium studies: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Steatorrhea]]- 10-40 g/day (Normal=5 g/day) | * Dilation and edema of mucosal folds | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Steatorrhea]]- 10-40 g/day (Normal=5 g/day) | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Celiac disease]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Celiac disease]] | ||
| Line 676: | Line 756: | ||
* [[Anti-gliadin antibodies|Anti-gliadin antibody]] | * [[Anti-gliadin antibodies|Anti-gliadin antibody]] | ||
* Small bowel biopsy | * Small bowel biopsy | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |US: | ||
* Bull’s eye or target pattern | * Bull’s eye or target pattern | ||
* Pseudokidney sign | * Pseudokidney sign | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Gluten allergy | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Gluten allergy | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Infective colitis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Infective colitis]] | ||
| Line 723: | Line 804: | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Colon carcinoma | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Colon carcinoma]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse/ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse/ RLQ/LLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 737: | Line 818: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Normal | * Normal or hyperactive if obstruction present | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* CBC | * CBC | ||
| Line 747: | Line 827: | ||
* Barium enema | * Barium enema | ||
* CT colonography | * CT colonography | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |PILLCAM 2: A colon capsule for CRC screening may be used in patients with an incomplete colonoscopy who lacks obstruction | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* PILLCAM 2: A colon capsule for CRC screening may be used in patients with an incomplete colonoscopy who lacks obstruction | |||
|- | |- | ||
! rowspan="8" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hepatic causes | ! rowspan="8" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hepatic causes | ||
| Line 796: | Line 877: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hepatocellular carcinoma]]/Metastasis | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Hepatocellular carcinoma]]/[[Metastasis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 928: | Line 1,009: | ||
* [[Hyponatremia]] | * [[Hyponatremia]] | ||
* [[Thrombocytopenia]] | * [[Thrombocytopenia]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |US | ||
* Nodular, shrunken liver | * Nodular, shrunken liver | ||
* [[Ascites]] | * [[Ascites]] | ||
| Line 1,025: | Line 1,106: | ||
|- | |- | ||
! colspan="2" rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Hollow Viscous Obstruction | ! colspan="2" rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" | Hollow Viscous Obstruction | ||
| colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Small bowel obstruction | | colspan="1" rowspan="1" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Small bowel obstruction]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 1,050: | Line 1,131: | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Volvulus]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Volvulus]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Diffuse | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| Line 1,084: | Line 1,165: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[bilirubin]] and [[alkaline phosphatase]] | * ↑ [[bilirubin]] and [[alkaline phosphatase]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | * Ultrasound | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |- | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
| Line 1,129: | Line 1,211: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT angiography | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT angiography | ||
* SMA or SMV thrombosis | * SMA or SMV thrombosis | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Also known as abdominal angina | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Also known as abdominal angina that worsens with eating | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ischemic colitis|Acute ischemic colitis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Ischemic colitis|Acute ischemic colitis]] | ||
| Line 1,145: | Line 1,228: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive then absent | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |Hyperactive then absent | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Leukocytosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal x-ray]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Abdominal x-ray]] | ||
* Distension and pneumatosis | * Distension and pneumatosis | ||
| Line 1,151: | Line 1,235: | ||
* Double halo appearance, thumbprinting | * Double halo appearance, thumbprinting | ||
* Thickening of bowel | * Thickening of bowel | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |May lead to shock | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* May lead to shock | |||
|- | |- | ||
! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hemorrhagic causes | ! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Hemorrhagic causes | ||
| Line 1,171: | Line 1,256: | ||
* [[Fibrinogen]] | * [[Fibrinogen]] | ||
* [[D-dimer]] | * [[D-dimer]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Focused Assessment with Sonography in Trauma (FAST) | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Unstable hemodynamics | * Focused Assessment with Sonography in Trauma (FAST) | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Unstable hemodynamics | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intra-abdominal or [[retroperitoneal hemorrhage]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Intra-abdominal or [[retroperitoneal hemorrhage]] | ||
| Line 1,188: | Line 1,275: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |CT scan | * ↓ Hb | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of [[trauma]] | * ↓ Hct | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT scan | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[trauma]] | |||
|- | |- | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Disease | ||
| Line 1,213: | Line 1,304: | ||
! rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gynaecological Causes | ! rowspan="4" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Gynaecological Causes | ||
! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Tubal causes | ! rowspan="3" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Tubal causes | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Torsion of the cyst | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Torsion of the cyst/ovary | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RLQ / LLQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| Line 1,227: | Line 1,318: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound | * ↑ [[ESR]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Sudden onset & severe pain | * ↑ [[CRP]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Sudden onset & severe pain | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Salpingitis|Acute salpingitis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Salpingitis|Acute salpingitis]] | ||
| Line 1,245: | Line 1,340: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Leukocytosis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Pelvic ultrasound]] | * [[Leukocytosis]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Vaginal discharge]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Pelvic ultrasound]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Vaginal discharge]] | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cyst rupture | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |Cyst rupture | ||
| Line 1,263: | Line 1,361: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound | * ↑ [[ESR]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | * ↑ [[CRP]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pregnancy | ! style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pregnancy | ||
| Line 1,282: | Line 1,383: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Positive [[pregnancy test]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Ultrasound | * Positive [[pregnancy test]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Ultrasound | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |History of | |||
* Missed period | |||
* Vaginal bleeding | |||
|- | |- | ||
! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra-abdominal causes | ! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" |Extra-abdominal causes | ||
| Line 1,302: | Line 1,407: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | − | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |N | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Thoracentesis]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Thoracentesis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Chest X-ray]] | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Chest X-ray]] | ||
* Pleural opacity | * Pleural opacity | ||
| Line 1,312: | Line 1,418: | ||
* Increased [[tactile fremitus]] | * Increased [[tactile fremitus]] | ||
|- | |- | ||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |Pulmonary embolism | | colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Pulmonary embolism]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | ± | ||
| Line 1,338: | Line 1,444: | ||
* Pleuretic chest pain | * Pleuretic chest pain | ||
|- | |- | ||
| colspan="2" style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Pneumonia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |RUQ/LUQ | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
| Line 1,356: | Line 1,462: | ||
* Leukocytosis | * Leukocytosis | ||
* Pancytopenia | * Pancytopenia | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=" | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* CXR | *CXR | ||
* CT chest | *CT chest | ||
* Bronchoscopy | *Bronchoscopy | ||
| style="padding: 5px 5px; background: #F5F5F5;" align=" | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Shortness of breath | * Shortness of breath | ||
* Cough | * Cough | ||
| Line 1,396: | Line 1,502: | ||
|} | |} | ||
|} | |} | ||
</small></small> | |||
{| | {| | ||
|- | |- | ||
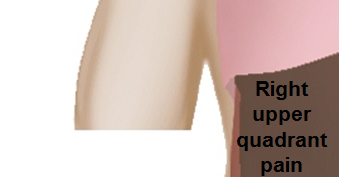
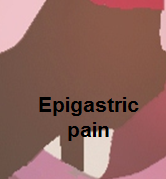
| | | [[Image:Right_upper_quadrant.PNG|link=Right upper quadrant abdominal pain resident survival guide]]||[[Image:Epigastric_quadrant_pain.PNG|link=Epigastric pain resident survival guide]]||[[Image:Left_upper_quadrant.PNG|link=Left upper quadrant abdominal pain resident survival guide]] | ||
|- | |- | ||
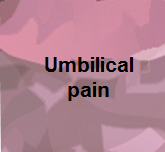
| | | [[Image:Right_flank_quadrant.PNG|link=Right flank pain resident survival guide]]||[[Image:Umbilical_pain.PNG|link=Umbilical region pain resident survival guide]]||[[Image:Left_flank_quadrant.PNG|link=Left flank quadrant abdominal pain resident survival guide]] | ||
|- | |- | ||
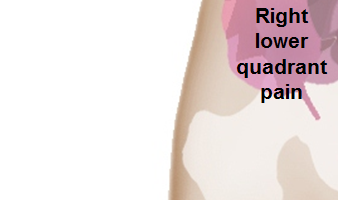
| | | [[Image:Right_lower_quadrant.PNG|link=Right lower quadrant abdominal pain resident survival guide]]||[[Image:Hypogastric.PNG|link=Hypogastric pain resident survival guide]]||[[Image:Left_lower_quadrant.PNG|link=Left lower quadrant abdominal pain resident survival guide]] | ||
|} | |} | ||
| Line 1,435: | Line 1,541: | ||
| title = Etiology and management of the acute urethral syndrome | | title = Etiology and management of the acute urethral syndrome | ||
| journal = [[Sexually transmitted diseases]] | | journal = [[Sexually transmitted diseases]] | ||
| volume = 8 | | volume = 8 | ||
| issue = 3 | | issue = 3 | ||
| pages = 235–238 | | pages = 235–238 | ||
| year = 1981 | | year = 1981 | ||
| month = July-September | | month = July-September | ||
| pmid = 7292216 | | pmid = 7292216 | ||
</ref><ref>{{Cite journal | </ref><ref>{{Cite journal | ||
<nowiki> </nowiki><nowiki>|</nowiki> author = [[W. E. Stamm]], [[K. F. Wagner]], [[R. Amsel]], [[E. R. Alexander]], [[M. Turck]], [[G. W. Counts]] & [[K. K. Holmes]] | <nowiki> </nowiki><nowiki>|</nowiki> author = [[W. E. Stamm]], [[K. F. Wagner]], [[R. Amsel]], [[E. R. Alexander]], [[M. Turck]], [[G. W. Counts]] & [[K. K. Holmes]] | ||
| title = Causes of the acute urethral syndrome in women | | title = Causes of the acute urethral syndrome in women | ||
| journal = [[The New England journal of medicine]] | | journal = [[The New England journal of medicine]] | ||
| volume = 303 | | volume = 303 | ||
| issue = 8 | | issue = 8 | ||
| pages = 409–415 | | pages = 409–415 | ||
| year = 1980 | | year = 1980 | ||
| month = August | | month = August | ||
| doi = 10.1056/NEJM198008213030801 | | doi = 10.1056/NEJM198008213030801 | ||
| pmid = 6993946</ref> | | pmid = 6993946</ref> | ||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{Gastroenterology}} | {{Gastroenterology}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
<references /> | |||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
| Line 1,462: | Line 1,571: | ||
[[Category:Gynecology]] | [[Category:Gynecology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Latest revision as of 20:13, 29 July 2020
| Resident Survival Guide |

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Amandeep Singh M.D.[2]Seyedmahdi Pahlavani, M.D. [3]Iqra Qamar M.D.[4]
Overview
Diagnosing the cause of abdominal pain can be difficult, because many diseases can cause this symptom. Most frequently the cause is benign and/or self-limiting, but more serious causes may require urgent intervention. Acute abdominal pain is a severe, persistent abdominal pain of sudden onset that is likely to require surgical intervention to treat its cause. The following table summarizes differential diagnosis for abdominal pain.
Differential Diagnosis of Abdominal Pain
To review the differential diagnosis of Abdominal pain, click here.
To review the differential diagnosis of Abdominal pain and fever, click here.
To review the differential diagnosis of Abdominal pain, nausea and vomiting, click here.
To review the differential diagnosis of Abdominal pain and jaundice, click here.
To review the differential diagnosis of Abdominal pain and weight loss, click here.
To review the differential diagnosis of Abdominal pain and constipation, click here.
To review the differential diagnosis of Abdominal pain and diarrhea, click here.
To review the differential diagnosis of Abdominal pain and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain, fever and jaundice, click here.
To review the differential diagnosis of Abdominal pain, fever, nausea and vomiting, click here.
To review the differential diagnosis of Abdominal pain, fever, and diarrhea, click here.
To review the differential diagnosis of Abdominal pain, fever and constipation, click here.
To review the differential diagnosis of Abdominal pain, fever and weight loss, click here.
To review the differential diagnosis of Abdominal pain, fever and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain, nausea,vomiting and jaundice, click here.
To review the differential diagnosis of Abdominal pain, nausea,vomiting and weight loss, click here.
To review the differential diagnosis of Abdominal pain, nausea,vomiting and constipation, click here.
To review the differential diagnosis of Abdominal pain, nausea,vomiting and diarrhea, click here.
To review the differential diagnosis of Abdominal pain, nausea, vomiting and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain, jaundice and weight loss, click here.
To review the differential diagnosis of Abdominal pain, jaundice and diarrhea, click here.
To review the differential diagnosis of Abdominal pain, jaundice and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain,weight loss and constipation, click here.
To review the differential diagnosis of Abdominal pain,weight loss and diarrhea, click here.
To review the differential diagnosis of Abdominal pain, weight loss and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain, constipation and diarrhea, click here.
To review the differential diagnosis of Abdominal pain, constipation and GI bleeding, click here.
To review the differential diagnosis of Abdominal pain, diarrhea and GI bleeding, click here.
Abdominal Pain
The following table outlines the major differential diagnoses of abdominal pain.
Abbreviations: RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein, TS= Transferrin saturation, SF= Serum Ferritin, SMA= Superior mesenteric artery, SMV= Superior mesenteric vein, ECG= Electrocardiogram, US = Ultrasound
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
 |

|
 |
 |

|
 |
 |

|
The following is a list of diseases that present with acute onset severe lower abdominal pain:
| Disease | Findings |
|---|---|
| Ectopic pregnancy | History of missed menses, positive pregnancy test, ultrasound reveals an empty uterus and may show a mass in the fallopian tubes.[1] |
| Appendicitis | Pain localized to the right iliac fossa, vomiting, abdominal ultrasound sensitivity for diagnosis of acute appendicitis is 75% to 90%.[2] |
| Rupturedovarian cyst | Usually spontaneous, can follow history of trauma, mild chronic lower abdominal discomfort may suddenly intensify, ultrasound is diagnostic.[3] |
| Ovarian cyst torsion | Presents with acute severe unilateral lower quadrant abdominal pain, nausea and vomiting, tender adnexal mass palpated in 90%, ultrasound is diagnostic.[4] |
| Hemorrhagic ovarian cyst | Presents with localized abdominal pain, nausea and vomiting. Hypovolemic shock may be present, abdominal tenderness and guarding are physical exam findings, ultrasound is diagnostic.[4] |
| Endometriosis | Presents with cyclic pain that is exacerbated by onset of menses, dyspareunia. laparoscopic exploration is diagnostic.[4] |
| Acute cystitis | Presents with features of increased urinary frequency, urgency, dysuria, and suprapubic pain.[5][6] |
References
- ↑ Morin L, Cargill YM, Glanc P (2016). "Ultrasound Evaluation of First Trimester Complications of Pregnancy". J Obstet Gynaecol Can. 38 (10): 982–988. doi:10.1016/j.jogc.2016.06.001. PMID 27720100.
- ↑ Balthazar EJ, Birnbaum BA, Yee J, Megibow AJ, Roshkow J, Gray C (1994). "Acute appendicitis: CT and US correlation in 100 patients". Radiology. 190 (1): 31–5. doi:10.1148/radiology.190.1.8259423. PMID 8259423.
- ↑ Bottomley C, Bourne T (2009). "Diagnosis and management of ovarian cyst accidents". Best Pract Res Clin Obstet Gynaecol. 23 (5): 711–24. doi:10.1016/j.bpobgyn.2009.02.001. PMID 19299205.
- ↑ 4.0 4.1 4.2 Bhavsar AK, Gelner EJ, Shorma T (2016). "Common Questions About the Evaluation of Acute Pelvic Pain". Am Fam Physician. 93 (1): 41–8. PMID 26760839.
- ↑ {{Cite journal | author = W. E. Stamm | title = Etiology and management of the acute urethral syndrome | journal = Sexually transmitted diseases | volume = 8 | issue = 3 | pages = 235–238 | year = 1981 | month = July-September | pmid = 7292216
- ↑ {{Cite journal | author = W. E. Stamm, K. F. Wagner, R. Amsel, E. R. Alexander, M. Turck, G. W. Counts & K. K. Holmes | title = Causes of the acute urethral syndrome in women | journal = The New England journal of medicine | volume = 303 | issue = 8 | pages = 409–415 | year = 1980 | month = August | doi = 10.1056/NEJM198008213030801 | pmid = 6993946