Cardiac tamponade
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Varun Kumar, M.B.B.S{{#meta: itemprop="medicalWebPageAudiences" content="patient"}}{{#meta: itemprop="medicalWebPageSpecialities" content="cardiology"}}{{#meta: itemprop="medicalWebPageInfoTypes" content="symptoms,diagnosis,treatment,causes,prognosis,complications"}} Classification Classic::Classification Atypical::Screening::
Overview
|
Cardiac tamponade Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac tamponade On the Web |
|
American Roentgen Ray Society Images of Cardiac tamponade |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [4]; Varun Kumar, M.B.B.S Ramyar Ghandriz MD[5]
Overview
Cardiac tamponade is a medical emergency condition in which fluid/blood accumulates in the pericardium (the sac in which the heart is enclosed). The elevated pericardial pressure puts significant pressure on the heart, causing a decrease in the diastolic filling of the ventricles, and hence in stroke volume. The end result is ineffective pumping of blood, shock, and potentially death. It is caused mainly by the accumulation of a large or uncontrolled pericardial effusion. The effusion can occur rapidly (as in the case of trauma or myocardial rupture), or over a more gradual period of time (as in cancer). The fluid involved is often blood, but pus is also found in some circumstances. Common causes of increased pericardial effusion include hypothyroidism, trauma (either penetrating trauma involving the pericardium or blunt chest trauma), pericarditis (inflammation of the pericardium), iatrogenic trauma (during an invasive procedure), and ventricular rupture. It should be differentiated from tension pneumothorax, hypovolemia and acute congestive heart failure. Patients with cardiac tamponade may present with sudden onset of chest pain, palpitations, breathlessness and lightheadedness. Physical examination may show the classic Beck's triad (hypotension, muffled heart sound, and elevated jugular venous distension), tachycardia, pulsus paradoxus, and pericardial rub depending on the type, and severity of tamponade. The electrocardiogram in cardiac tamponade usually demonstrates sinus tachycardia, and may sometimes show reduced QRS voltage and electrical alternans. Chest X ray will demonstrate pneumopericardium and cardiac silhouette changes. Echocardiography findings include pericardial effusion, diastolic compression of the RV, diastolic compression of the right atrium (RA), plethora of the inferior vena cava and paradoxical septal motion. Pericardiocentesis can provide a diagnostic sampling of pericardial fluid and can be used as a therapeutic maneuver to evacuate pericardial fluid and lower the pericardial pressure.
Historical Perspective
Cardiac tamponade is a very common emergent manifestation, which can be caused by traumatic injuries, since the emulation of the disease tracks back to centuries ago. Acknowledgment of existing pericardial is first done by hippocrates, which was continued by Galen to describing what is now known as pericardial effusion.
Classification
Cardiac tamponade is an emergency form of cardiac effusion. it is more over classified by the pathological causes. The management of emergent situation is not very differed by the basic cause.
Pathophysiology
Cardiac tamponade occurs when the pericardial space fills up with fluid faster than the pericardial sac can stretch. If the amount of fluid increases slowly (such as in hypothyroidism) the pericardial sac can expand to contain a liter or more of fluid prior to tamponade occurring. If the fluid occurs rapidly (as may occur after trauma or myocardial rupture) as little as 100 ml can cause tamponade. However, if the volume of the fluid accumulation is too rapid and or large, then the hemodynamic compromise can occur with a rise in pericardial pressure. This in turn reduces stroke volume, and eventually, cardiac output. If fluid continues to accumulate, then with each successive diastole, less and less blood enters the ventricles, as the increasing pressure presses on the heart and forces the septum to bend into the left ventricle, leading to a decreased stroke volume.
Causes
Cardiac tamponade is caused by the accumulation of a large or uncontrolled pericardial effusion. The effusion can occur rapidly (as in the case of trauma or myocardial rupture), or over a more gradual period of time (as in cancer). The fluid involved is often blood, but pus is also found in some circumstances. Common causes of increased pericardial effusion include hypothyroidism, trauma (either penetrating trauma involving the pericardium or blunt chest trauma), pericarditis (inflammation of the pericardium), iatrogenic trauma (during an invasive procedure), and ventricular rupture.
Differentiating cardiac tamponade from Other Diseases
The initial diagnosis of cardiac tamponade can be challenging, as there are a number of differential diagnoses, including tension pneumothorax, hypovolemia and acute congestive heart failure. The differential diagnosis of cardiac tamponade differs based on the type of cardiac tamponade (either acute or subacute).
Epidemiology and Demographics
The cardiac tamponade is most often attributed to the rupture of an acute myocardial infarction or an intrapericardial rupture of a dissecting ascending aortic aneurysm. In developed countries malignancy is the leading cause of cardiac tamponade secondary to pericardial effusion. The incidence of cardiac tamponade based on a giant sample size of about 216 million emergency admissions was about 115,638(0.05%). The incidence of cardiac tamponade increases with age; the mean age was around 61.9. Cardiac temponade mortality rate is significantly different due to its underlying cause.
Risk Factors
Most potent risk factors for cardiac tamponade include heart surgeries, cardiac myxomas, myocardial infarction and traumas.
Screening
Cardiac tamponade is more of a clinical diagnosis. If the patient clinical manifestation was raising suspicious toward tamponade, CT scan and echocardiogram are diagnostic gold standards for the disease.
Natural History, Complications, and Prognosis
Cardiac tamponade is a life-threatening condition requiring urgent intervention to remove the pericardial fluid. Complications include pulmonary edema, cardiac failure, cardiogenic shock and ultimately death.
Cardiac tamponade has a good prognosis if detected early and treated immediately. Short-term survival is mostly dependent on early diagnosis and relief of tamponade. Long-term survival depends upon the prognosis of the underlying cause, irrespective of the mode of treatment.
Diagnosis
Diagnostic Study of Choice
Cardiac tamponade is more of a clinical diagnosis, but still some diagnostic studies may be helpful.
History and Symptoms
Patients with cardiac tamponade may present with sudden onset of chest pain, palpitations, breathlessness and lightheadedness. Presentation vary with the cause and acuteness of development of tamponade. An acute cardiac tamponade follows trauma to the chest or rupture of the aorta or heart. A subacute cardiac tamponade occurs in the setting of a neoplasm or renal failure. A low pressure cardiac tamponade occurs in patients who are hypovolemic secondary to hemorrhage or over diuresis.
Physical Examination
Physical examination may vary depending on the type of cardiac tamponade. Physical examination may show the classic Beck's triad (hypotension, muffled heart sound, and elevated jugular venous distension), tachycardia, pulsus paradoxus, and pericardial rub depending on the type, and severity of tamponade. Initial diagnosis can be challenging, as there are a number of differential diagnoses, including tension pneumothorax, and acute heart failure.
Laboratory Findings
Non-specific markers of inflammation are generally elevated in pericarditis. This include the CBC, elevated C-reactive protein, ESR. The cardiac troponin is elevated if there is injury to the underlying myocardium, a condition termed myopericarditis. Diagnostic pericardiocentesis and biopsy help in identifying an underlying infectious or malignant process.
Electrocardiogram
The electrocardiogram in cardiac tamponade usually demonstrates sinus tachycardia, and may sometimes show reduced QRS voltage and electrical alternans.
X-ray
Cardiac tamponade is a clinical diagnosis, however chest X ray can be helpful sometimes. It will demonstrate pneumopericardium and cardiac silhouette changes.
Echocardiography and Ultrasound
The role of echocardiography in the evaluation of the patient with pericarditis is to characterize the presence, size, location and hemodynamic impact of a pericardial effusion. Tamponade is characterized by pericardial effusion, diastolic compression of the RV, diastolic compression of the right atrium (RA), plethora of the inferior vena cava and paradoxical septal motion.
CT scan
A CT scan is not commonly used for the diagnosis of cardiac tamponade as it is effectively diagnosed based on clinical features and echocardiography. Findings on CT include [Superior vena cava]] andInferior vena cava enlargement, Hepatic and renal vein enlargment, periportal edema, reflux of contrast material, collapse of the right atrium, Pericardial thickening.
MRI
Cardiovascular MRI is not commonly used for the diagnosis of cardiac tamponade as it is effectively diagnosed based on clinical features and echocardiography. Findings include Pericardial effusion, distension of the vena cavae and hepatic vein, collapse of the right sided cardiac chambers, interventricular septum shifts towards the left, paradoxical septal motion.
Other Imaging Findings
There are no other imaging findings associated with cardiac tamponade.
Other Diagnostic Studies
There are no other diagnostic studies associated with cardiac tampnoade.
Treatment
Medical Therapy
If the patient is symptomatic, and if there are signs of cardiac tamponade, urgent pericardiocentesis should be performed. Additional supportive therapy includes the administration of oxygen, fluid repletion, echocardiographic monitoring, treatment of underlying pathology, reversal of anticoagulation and monitoring.
Surgery
Percutaneous pericardiocentesis is a procedure where fluid is aspirated from the pericardium (the sac enveloping the heart) using a needle via a percutaneous approach. Pericardiocentesis can provide a diagnostic sampling of pericardial fluid and can be used as a therapeutic maneuver to evacuate pericardial fluid and lower the pericardial pressure.
Primary Prevention
There are no established measures for the primary prevention of cardiac tamponade.
Secondary Prevention
There are no established measures for the secondary prevention of cardiac tamponade.
References
Pathophysiology
|
Cardiac tamponade Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac tamponade On the Web |
|
American Roentgen Ray Society Images of Cardiac tamponade |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [6]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [7]; Varun Kumar, M.B.B.S. Ramyar Ghandriz MD[8]
Overview
Cardiac tamponade occurs when the pericardial space fills up with fluid faster than the pericardial sac can stretch. If the amount of fluid increases slowly (such as in hypothyroidism) the pericardial sac can expand to contain a liter or more of fluid prior to tamponade occurring. If the fluid occurs rapidly (as may occur after trauma or myocardial rupture) as little as 100 ml can cause tamponade. However, if the volume of the fluid accumulation is too rapid and or large, then the hemodynamic compromise can occur with a rise in pericardial pressure. This in turn reduces stroke volume, and eventually, cardiac output. If fluid continues to accumulate, then with each successive diastole, less and less blood enters the ventricles, as the increasing pressure presses on the heart and forces the septum to bend into the left ventricle, leading to a decreased stroke volume.
Pathophysiology
Anatomy and Physiology of Pericardium
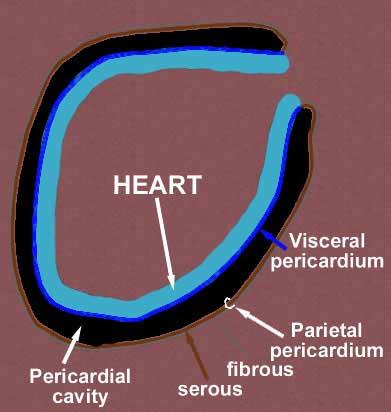
Layers of the Pericardium
- The pericardium is made up of two layers[1][2][3][4]
- Fibrous pericardium
- Serous pericardium
- Smooth internal layer made up of 2 components:
- Parietal: reflects onto fibrous pericardium
- Visceral: reflects onto heart and great vessels and forms the epicardium, the external layer of the heart wall
- Smooth internal layer made up of 2 components:
- Pericardial cavity: Potential space between parietal and visceral layers. It contains a serous fluid film that occupies the cavity and functions as lubricant against friction by all chest movements.
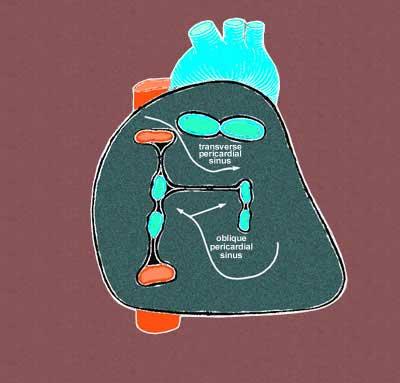
Pericardial Sinuses
- There are two small chambers or sinuses located where the visceral and parietal pericardia are continuous with one another within the pericardial cavity.[5][6][7]
- Transverse sinus:
- Located posterior to the pulmonary trunk and ascending aorta at the level between the superior vena cava and aortic arch
- Formed after dorsal mesocardium rupture embryonically
- Functional role is to allow the unhindered expansion of great arteries posteriorly during cardiac systole
- Utilized surgically to pass surgical clamps or place ligatures around great arteries.
- Oblique sinus:
- A blind recess (cul-de-sac) posterior to the left atrium between superior vena cava, right and left pulmonary veins inferior to the transverse sinus
- Formed embryonically by the incorporation of the pulmonary vein tributaries into the left atrium
- Functional role believed to be the expansion of the left atrium upon the normal collapse of the thorax
Pathogenesis
- The outer pericardium is made of fibrous tissue which does not easily stretch, and so once fluid begins to enter the pericardial space, pressure starts to increase. This causes obstructive shock to develop, and if left untreated, cardiac arrest may occur (in which case the presenting rhythm is likely to be Pulseless electrical activity). [8][9][10].
- Ordinarily, drainage from the pericardium occurs via the thoracic duct and the right lymphatic duct into the right pleural space. In the absence of disease, the normal pericardium contains only 20-50 cc of serous fluid due to ultrafiltration from the blood. Up to about 75 cc can accumulate acutely in the pericardium without hemodynamic compromise. Much greater amounts of fluid can accumulate chronically over a prolonged period of time as the pericardial sac stretches slowly to accommodate the fluid without hemodynamic compromise. However, if the volume of the fluid accumulation is too rapid and or large, then the hemodynamic compromise can occur with a rise in pericardial pressure. This in turn reduces stroke volume, and eventually, cardiac output.
- If fluid continues to accumulate, then with each successive diastole, less and less blood enters the ventricles, as the increasing pressure presses on the heart and forces the septum to bend into the left ventricle, leading to a decreased stroke volume.
Below is a video demonstrating hemorrhagic effusion leading to cardiac tamponade. {{#ev:youtube|QwgfuDegC5Y}}
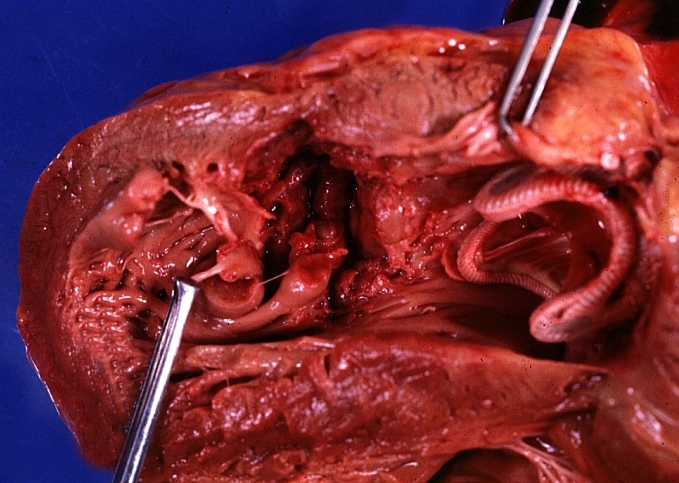
Gross Pathology
-
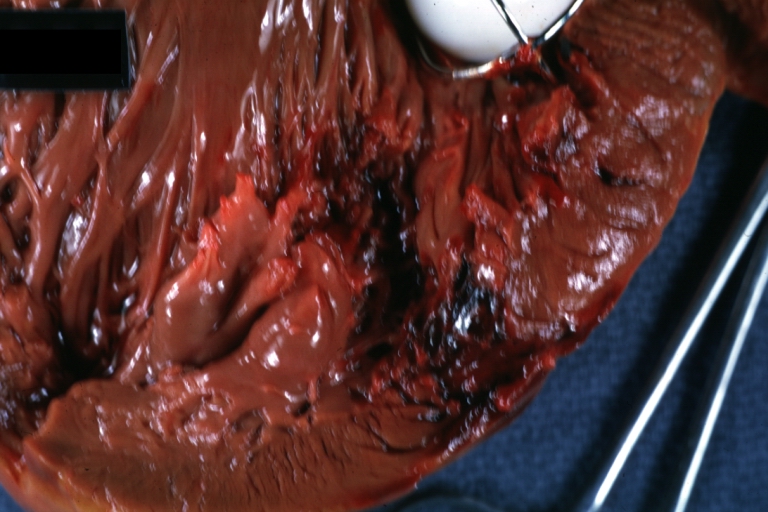
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, an excellent example with valve and obviously ruptured heart wall.
-
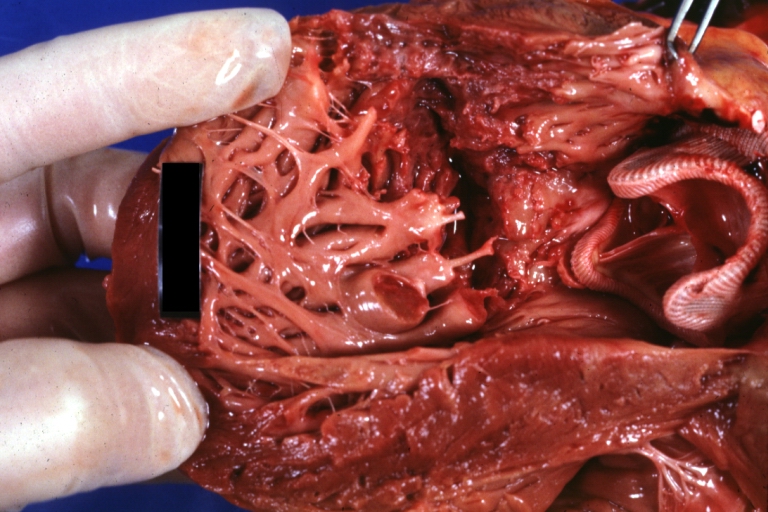
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color view from within left ventricle caged plastic ball with steel complete struts [11]
-
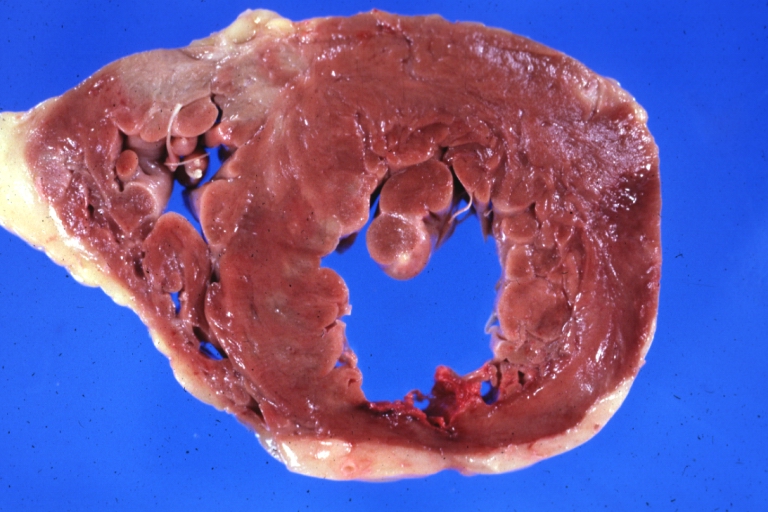
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color portion of caged plastic ball prosthesis shown with close-up of ruptured left ventricular wall
-
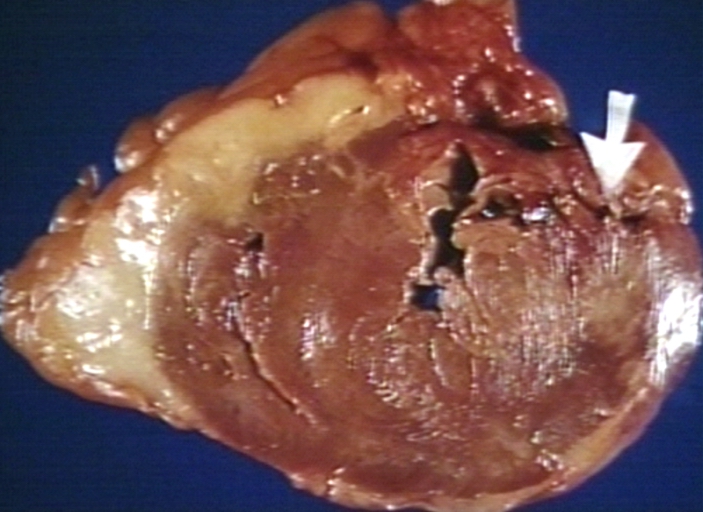
HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color close-up view of torn myocardium and bottom of hetero or homograft valve
-
HEART: Infarct; Acute, Ruptured: Gross, natural color horizontal section ventricle anterior infarct not easily appreciated with thinning of myocardium
-
HEART: Rupture after myocardial infarction.
References
- ↑ *Fornauer, Andrew (2003). "Pericardial Tamponade Complicating Central Venous Interventions". Journal of Vascular and Interventional Radiology. PMID 12582195. Unknown parameter
|coauthors=ignored (help); Unknown parameter|month=ignored (help) - ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Kishore, K. (2003). The Heart of Structural Development: The Functional Basis of the Location and Morphology of the Human Vascular Pump. J Postgrad Med, 49:282-4.
- ↑ Moore, K. L., Agur, A. M., & Dalley, A. F. (2011). Essential Clinical Anatomy - Fourth Edition. Lippincott Williams & Wilkins.
- ↑ Tank, P. W. (2009). Grant's Dissector - Fourteenth Edition. Lippincott Williams & Wilkins.
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886
- ↑ Thibodeau, G.A., Patton, K.T. (2000). Anatomy & Physiology. Missouri: Mosby ISBN 9780323010962
- ↑ Habibi R, Faramarzi N, Altamirano AJ, Dadkhah S (2018). "A Patient Presenting with Cardiac Tamponade and the Challenges of Finding Its Cause: A Cardiac Angiosarcoma". Case Rep Cardiol. 2018: 2084390. doi:10.1155/2018/2084390. PMC 5851018. PMID 29682355.
Causes
|
Cardiac tamponade Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cardiac tamponade On the Web |
|
American Roentgen Ray Society Images of Cardiac tamponade |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [9]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [10]; Varun Kumar, M.B.B.S.
Overview
Cardiac tamponade is caused by the accumulation of a large or uncontrolled pericardial effusion. The effusion can occur rapidly (as in the case of trauma or myocardial rupture), or over a more gradual period of time (as in cancer). The fluid involved is often blood, but pus is also found in some circumstances. Common causes of increased pericardial effusion include hypothyroidism, trauma (either penetrating trauma involving the pericardium or blunt chest trauma), pericarditis (inflammation of the pericardium), iatrogenic trauma (during an invasive procedure), and ventricular rupture.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Any cause of pericardial effusion capable of compromising the hemodynamic status of a patient is potentially life threatening.[1][2]
Common Causes
The most common cause of cardiac tamponade include the following[3][4][5][6][7][8][9]
- Ascending aortic dissection
- Collagen vascular diseases
- Iatrogenic - central line insertion, pacemaker insertion, coronary interventions, myocardial biopsy
- Idiopathic
- Malignancy - breast cancer, Kaposi's sarcoma, lung cancer, lymphomas
- Penetrating trauma
- Pericarditis
- Bacteria - pneumococcus, streptococcus, staphylococcus
- Fungus - blastomyces, cryptococcus, histoplasma, pneumocystis carinii
- Tuberculous
- Virus - coxsackie virus, echovirus, CMV
Causes by Organ System
Causes in Alphabetical Order
References
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886
- ↑ Mattson Porth, C. (Ed.) (2005) (7th Ed.) Pathophysiology: Concepts of Altered Health States. Philadelphia : Lippincott Williams & Wilkins ISBN 978-0781749886
- ↑ Mittal A, Ray A, Talupula RM, Sood R (February 2018). "Sheehan's syndrome presenting as cardiac tamponade". BMJ Case Rep. 2018. doi:10.1136/bcr-2017-223129. PMC 5812377. PMID 29431100.
- ↑ Kurth BJ, Wagler V, Keith M (September 2016). "Cardiac tamponade as a manifestation of severe dermatomyositis". BMJ Case Rep. 2016. doi:10.1136/bcr-2016-216860. PMC 5051378. PMID 27664227.
- ↑ Fadel R, El-Menyar A, ElKafrawy S, Gad MG (2019). "Traumatic blunt cardiac injuries: An updated narrative review". Int J Crit Illn Inj Sci. 9 (3): 113–119. doi:10.4103/IJCIIS.IJCIIS_29_19. PMC 6792398 Check
|pmc=value (help). PMID 31620349. - ↑ Almehmadi F, Chandy M, Connelly KA, Edwards J (2016). "Delayed Tamponade after Traumatic Wound with Left Ventricular Compression". Case Rep Cardiol. 2016: 2154748. doi:10.1155/2016/2154748. PMC 5019924. PMID 27651957.
- ↑ Zadra AR, Ripellino P, Barzaghi N (April 2015). "Cardiac tamponade as presenting symptom of tuberculosis". BMJ Case Rep. 2015. doi:10.1136/bcr-2014-208787. PMC 4422911. PMID 25926581.
- ↑ Chiu MH, Sharma NC (July 2018). "A case of hypertensive emergency, primary hypothyroidism and large pericardial effusion with early tamponade". J Cardiol Cases. 18 (1): 29–32. doi:10.1016/j.jccase.2018.03.005. PMC 6149587. PMID 30279905.
- ↑ Sinha A, Yeruva SL, Kumar R, Curry BH (2015). "Early Cardiac Tamponade in a Patient with Postsurgical Hypothyroidism". Case Rep Cardiol. 2015: 310350. doi:10.1155/2015/310350. PMC 4534597. PMID 26294982.
Natural History, Complications & Prognosis
Natural History
Diagnosis
{{#ask:Used To Diagnose::Cardiac tamponade |?Sort Order |format=list |headers=plain |link=none |sep= | |template=MedicalTestQuery |sort=Sort Order }}
Treatment
{{#ask:Used To Treat::Cardiac tamponade |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery |sort=Sort Order }} {{#ask:Prevents::Cardiac tamponade |?Sort Order |intro= | |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery2 |sort=Sort Order }}
Related Chapters
{{#!:*Pericardial effusion
![HEART: Myocardial Rupture Following Mitral Valve Replacement: Gross, natural color view from within left ventricle caged plastic ball with steel complete struts [11]](/images/a/a2/Myocardial_rupture_2.jpg)