Papillary thyroid cancer pathophysiology: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 102: | Line 102: | ||
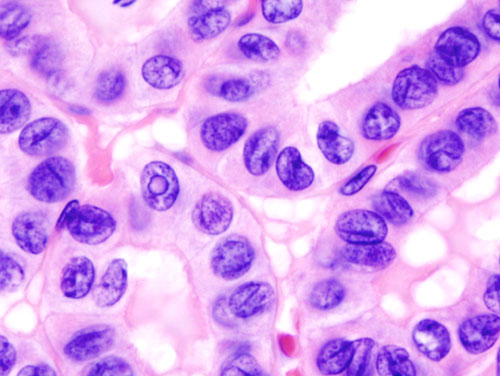
* Abundant [[eosinophilic]] [[cytoplasm]] | * Abundant [[eosinophilic]] [[cytoplasm]] | ||
* Lack of pseudostratification is a significant differentiator from columnar cell variant of papillary thyroid carcinoma | * Lack of pseudostratification is a significant differentiator from columnar cell variant of papillary thyroid carcinoma | ||
|[[File:Papillary thyroid carcinoma tall cell var high mag.jpg|thumb|none|250px| H&E stain | |[[File:Papillary thyroid carcinoma tall cell var high mag.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
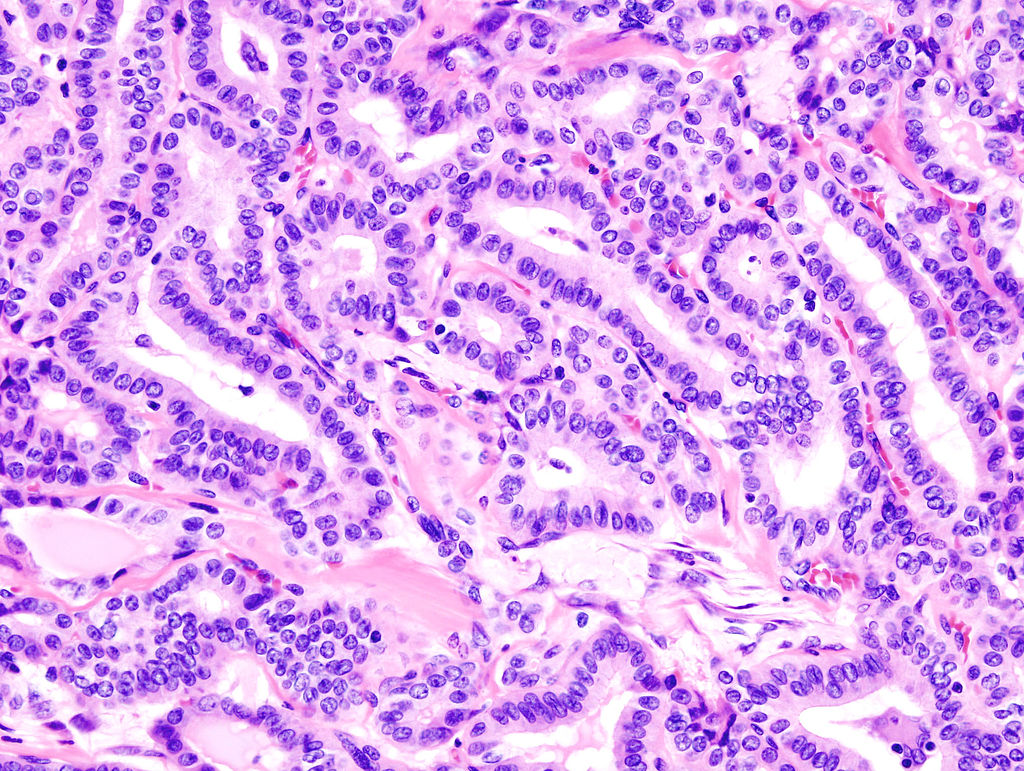
* Micrograph showing oncocytic variant of papillary thyroid carcinoma | * Micrograph showing oncocytic variant of papillary thyroid carcinoma | ||
* Large cells with abundant eosinophilic cytoplasm | * Large cells with abundant eosinophilic cytoplasm | ||
|[[File:Papillary thyroid carcinoma oncocytic variant -- low mag.jpg|thumb|none|250px| H&E stain, Contributed | |[[File:Papillary thyroid carcinoma oncocytic variant -- low mag.jpg|thumb|none|250px| H&E stain, Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
| Line 113: | Line 113: | ||
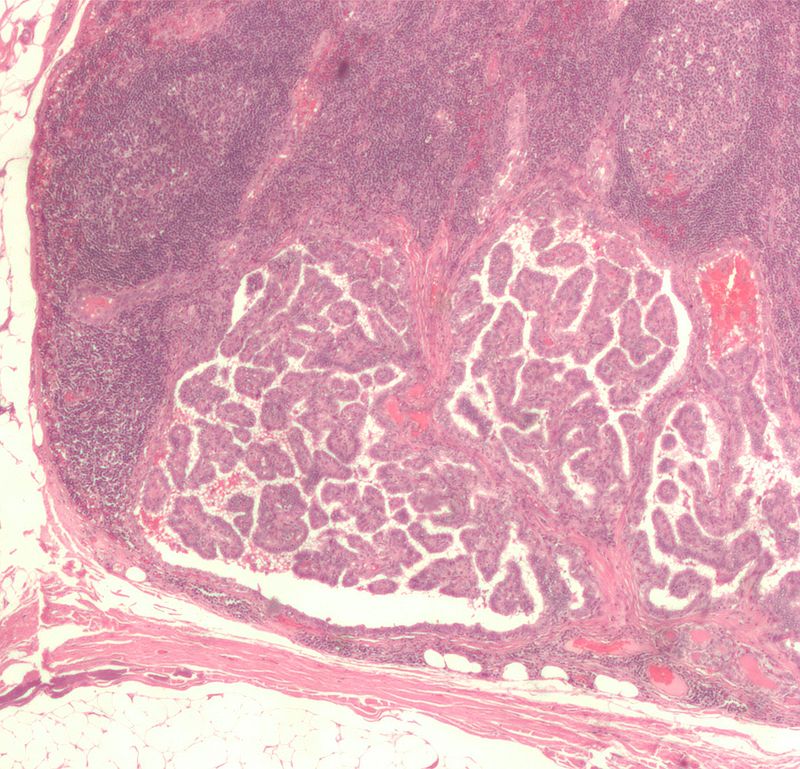
* Cribriform pattern with [[solid]] and [[spindle]] [[cell]] areas | * Cribriform pattern with [[solid]] and [[spindle]] [[cell]] areas | ||
* [[Squamous]] morules | * [[Squamous]] morules | ||
|[[File:Thyroid PapillaryCarcinoma CribriformMorularVariant HP2 13BR (1).jpg|thumb|none|250px| H&E stain, Contributed | |[[File:Thyroid PapillaryCarcinoma CribriformMorularVariant HP2 13BR (1).jpg|thumb|none|250px| H&E stain, Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
| Line 120: | Line 120: | ||
** Optical clearing | ** Optical clearing | ||
** Eosinophilic inclusions and overlapping of nuclei | ** Eosinophilic inclusions and overlapping of nuclei | ||
|[[File:Thyroid papillary carcinoma histopathology (3).jpg|thumb|none|250px| H&E stain. | |[[File:Thyroid papillary carcinoma histopathology (3).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
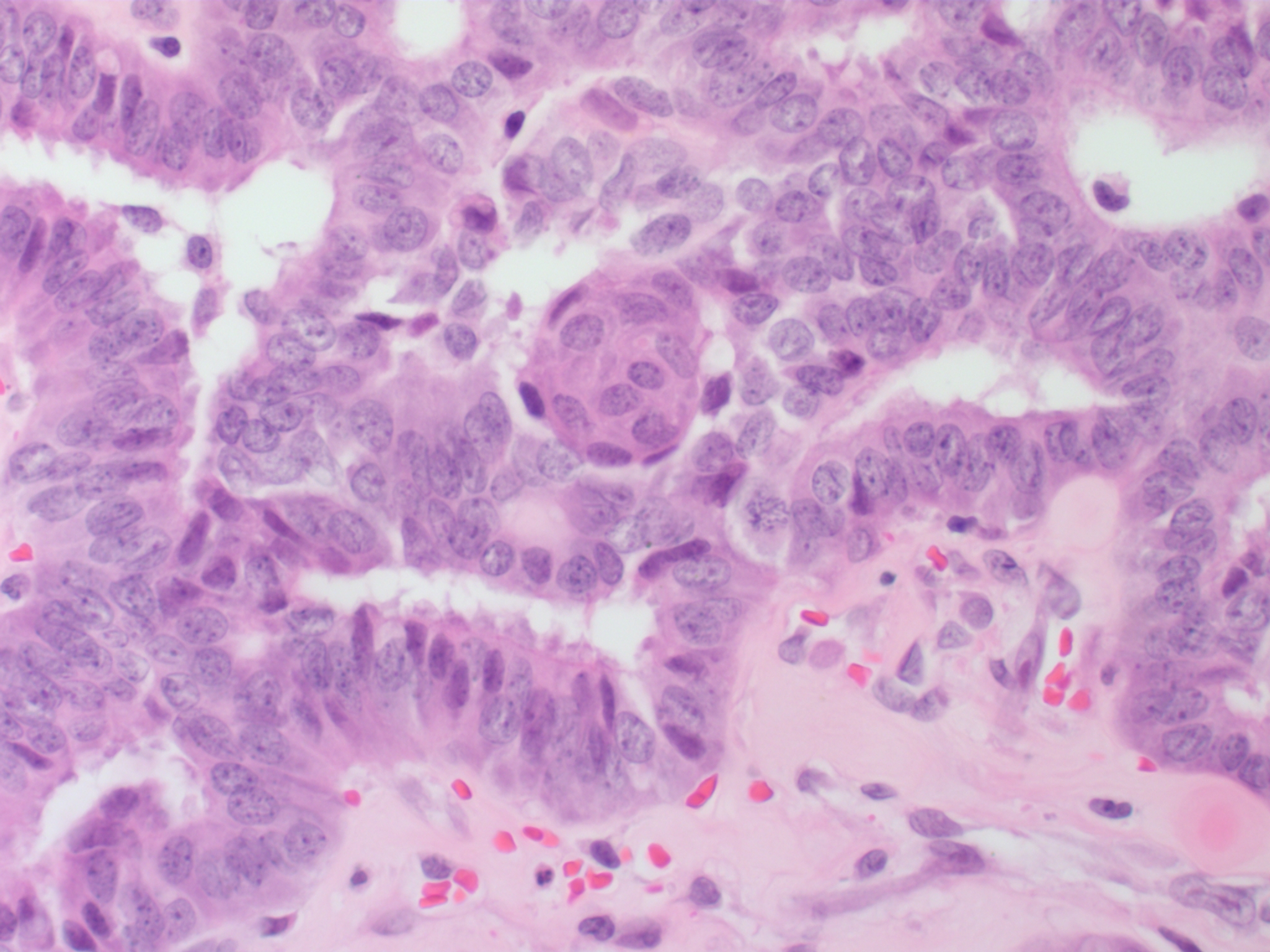
* Micrograph (high power view) of PTC demonstrating [[nuclear]] clearing and overlapping [[nuclei]] | * Micrograph (high power view) of PTC demonstrating [[nuclear]] clearing and overlapping [[nuclei]] | ||
|[[File:Thyroid papillary carcinoma histopathology (2).jpg|thumb|none|250px| H&E stain. | |[[File:Thyroid papillary carcinoma histopathology (2).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
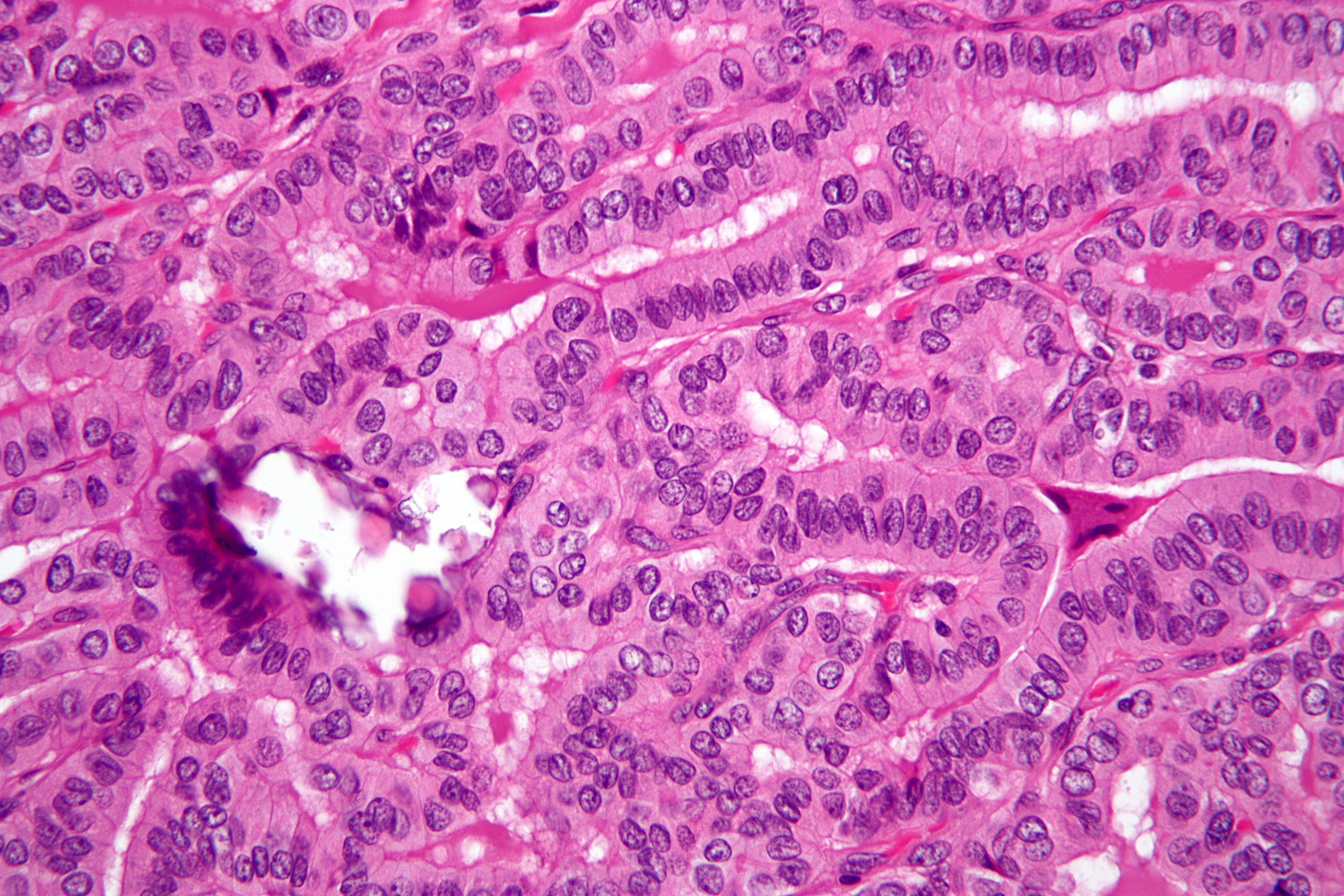
* Micrograph of papillary thyroid carcinoma demonstrating prominent [[papillae]] with fibrovascular cores | * Micrograph of papillary thyroid carcinoma demonstrating prominent [[papillae]] with fibrovascular cores | ||
|[[File:Thyroid papillary carcinoma histopatholgy (1).jpg|thumb|none|250px| H&E stain. | |[[File:Thyroid papillary carcinoma histopatholgy (1).jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|- | |- | ||
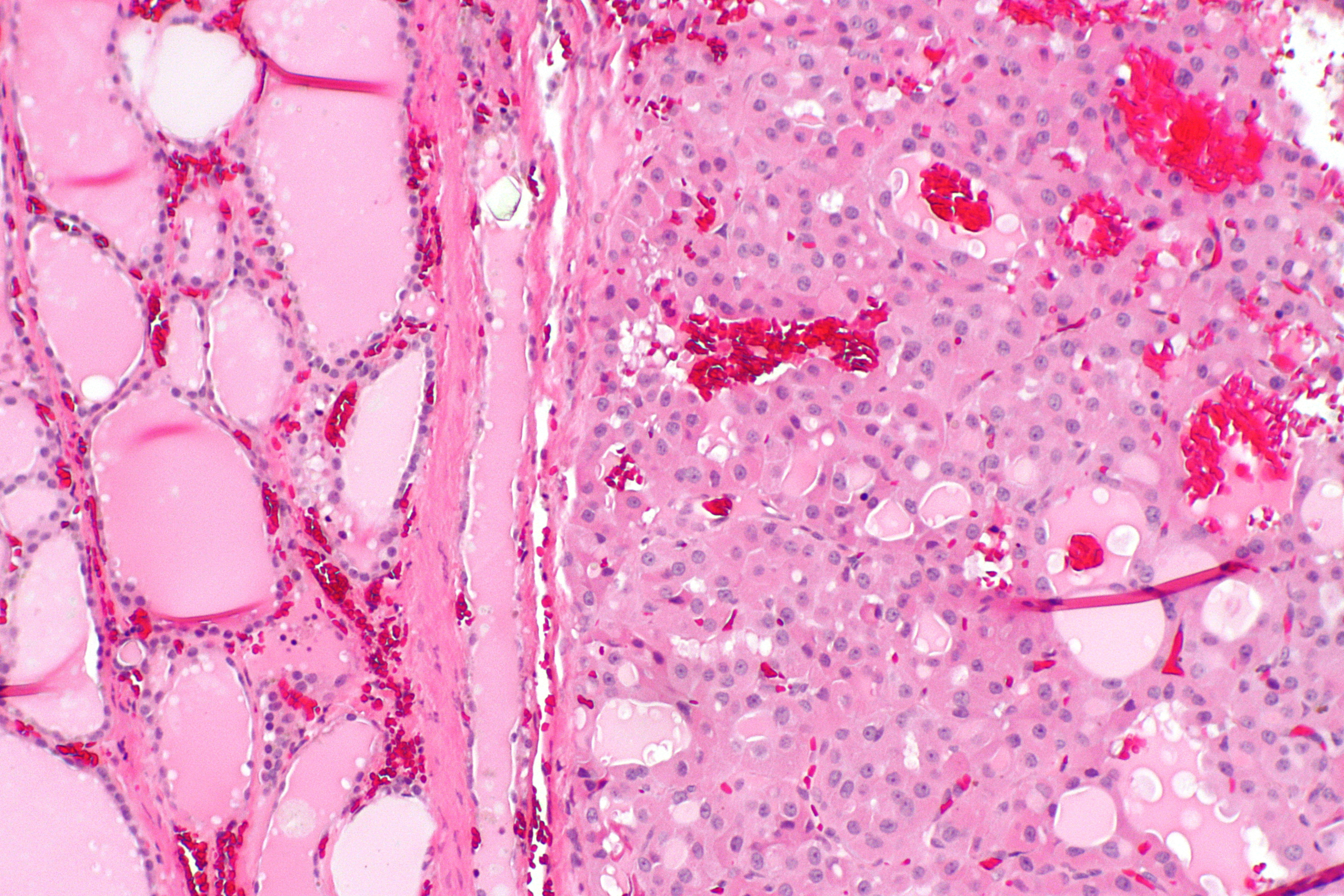
| | | | ||
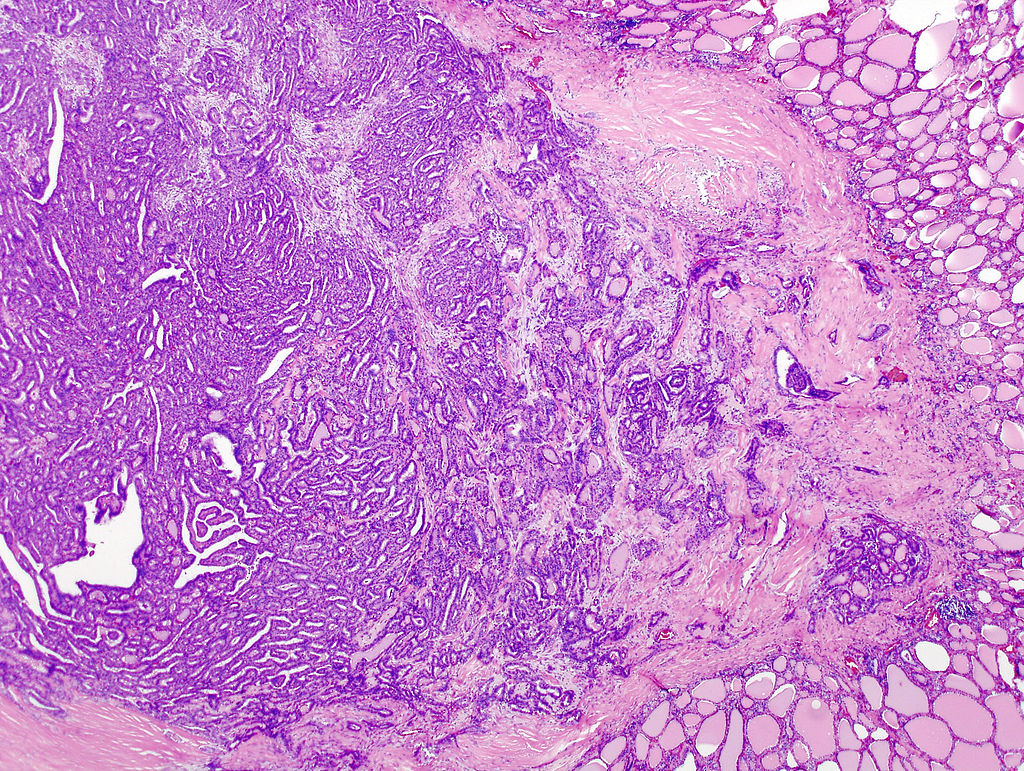
| Line 135: | Line 135: | ||
* [[Lymph node]] with several [[germinal centers]] (left, top/right of image) | * [[Lymph node]] with several [[germinal centers]] (left, top/right of image) | ||
* [[Adipose tissue]] (fat) is seen at the edge of the image (bottom and left) | * [[Adipose tissue]] (fat) is seen at the edge of the image (bottom and left) | ||
|[[File:-Lymph node with papillary thyroid carcinoma.jpg|thumb|none|250px| H&E stain | |[[File:-Lymph node with papillary thyroid carcinoma.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|- | |- | ||
| | | | ||
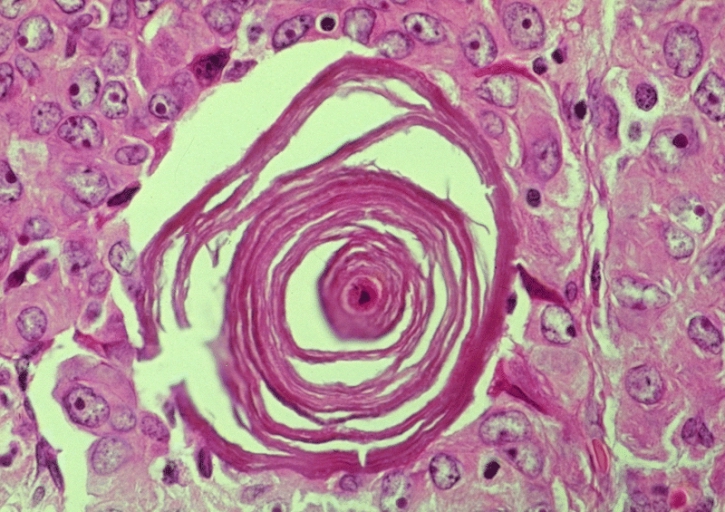
* Micrograph of psammoma body in papillary thyroid cancer | * Micrograph of psammoma body in papillary thyroid cancer | ||
* A single necrotic tumor cell in the center of this structure acts as the nidus for its formation | * A single necrotic tumor cell in the center of this structure acts as the nidus for its formation | ||
|[[File:WBR0863.jpg|thumb|none|250px|Contributed in wikimedia.commons]] | |[[File:WBR0863.jpg|thumb|none|250px| H&E stain. Contributed in wikimedia.commons]] | ||
|} | |} | ||
Revision as of 14:42, 12 August 2019
|
Papillary thyroid cancer Microchapters |
|
Differentiating Papillary thyroid cancer from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Papillary thyroid cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Papillary thyroid cancer pathophysiology |
|
Risk calculators and risk factors for Papillary thyroid cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
On gross pathology, a painless enlarging mass is a characteristic finding of papillary thyroid cancer. On microscopic histopathological analysis, Orphan Annie eye nuclear inclusions and psammoma bodies are characteristic findings of papillary thyroid cancer.
Pathogenesis
- Papillary thyroid tumors are most commonly unencapsulated, and they have a high tendency to metastasize locally to lymph nodes, which may produce cystic structures near the thyroid that are difficult to diagnose because of the paucity of malignant tissue.[1][2]
- Although papillary carcinoma has a propensity to invade lymphatics, it is less likely to invade blood vessels.[3]
- Furthermore, papillary tumors may metastasize to the lungs and produce a few nodules or the lung fields may exhibit a snowflake appearance throughout.
- Lateral aberrant thyroid is actually a lymph node metastasis from papillary thyroid carcinoma.[4]
- Other characteristics of the papillary carcinoma is that E.M. shows increased mitochondria, increased RER, as well as increased apical microvilli. Moreover, papillary carcinomas have an indolent growth, and 40 percent of cases spread out of the capsule.[5]
Genetics
- Mutations associated with papillary thyroid cancer are mainly two forms of chromosomal translocation and one form of point mutation. These alterations lead to activation of a common carcinogenic pathway known as the MAPK/ERK pathway.
- Chromosomal translocations involving the RET proto-oncogene (encoding a tyrosine kinase receptor that plays essential roles in the development of neuroendocrine cells) located on chromosome 10q11 occur in approximately a fifth of papillary thyroid cancers. The fusion oncoproteins generated are termed RET/PTC proteins (ret/papillary thyroid carcinoma), and constitutively activate RET and the downstream MAPK/ERK pathway. The frequency of ret/PTC translocations is significantly higher in papillary cancers arising in children and after radiation exposure. The gene NTRK1 (encoding the TrkA receptor), located on chromosome 1q, is similarly translocated in approximately 5 percent to 10 percent of papillary thyroid cancers.
- Approximately a third to a half of papillary thyroid carcinomas harbor point mutations in the BRAF oncogene, also activating the MAPK/ERK pathway. In those cases the BRAF mutations found were V600E mutation. According to recent studies, papillary cancers carrying the common V600E mutation tend to have a more aggressive long term course. BRAF mutations are frequent in papillary carcinoma and in undifferentiated cancers that have developed from papillary tumors.
Associated Conditions
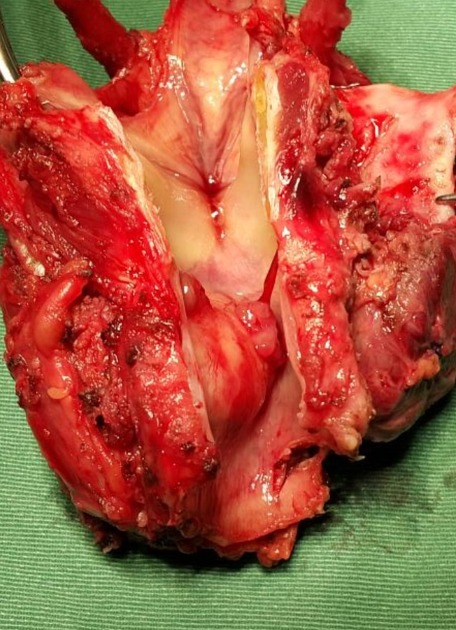
Gross Pathology
- Solitary nodule which can extend into trachea and vocal cords.
Microscopic Pathology
- Characteristic Orphan Annie eye nuclear inclusions (nuclei with uniform staining, which appear empty)[8] and psammoma bodies on light microscopy. The former is useful in identifying the follicular variant of papillary thyroid carcinomas.[9]
- Histologically papillary carcinoma demonstrates 'delicate stalks of epithelial cells' which account for its name.
| Papillary thyroid cancer subtype | Features on Histopathological Microscopic Analysis |
| Follicular |
|
| Conventional |
|
| Tall cell |
|
| Columnar cell |
|
| Oncocytic |
|
| Solid | |
| Diffuse sclerosing |
|
| Papillary thyroid carcinoma with prominent hobnail features | |
| Clear cell |
|
| Cribriform-Morular | |
| Macrofollicular |
|
| Papillary thyroid cancer | Image |
|
 |
|
 |
 | |
|
 |
 | |
|
 |
|
 |
|
 |
Histopathological Video
Video
{{#ev:youtube|JwymE_Lfs44}}
References
- ↑ Grani, G; Fumarola, A (Jun 2014). "Thyroglobulin in Lymph Node Fine-Needle Aspiration Washout: A Systematic Review and Meta-analysis of Diagnostic Accuracy". The Journal of Clinical Endocrinology and Metabolism. 99 (6): 1970–82. doi:10.1210/jc.2014-1098. PMID 24617715.
- ↑ "The Thyroid and its Diseases". Retrieved 2010-07-15.
- ↑ "Thyroid, Papillary Carcinoma". Retrieved 2010-07-15.
- ↑ Escofet X, Khan AZ, Mazarani W, Woods WG (2007). "Lessons to be learned: a case study approach. Lateral aberrant thyroid tissue: is it always malignant?". J R Soc Health. 127 (1): 45–6. doi:10.1177/1466424007073207. PMID 17319317.
- ↑ "Papillary Carcinomas". Retrieved 2010-07-15.[dead link]
- ↑ Accessed on October, 29 2015 "Papillary thyroid cancer [Dr Yuranga Weerakkody and Dr Frank Gaillard et al.].Radiopedia 2015" Check
|url=value (help). - ↑ Image courtesy of Dr David Cuete. Radiopaedia (original file ‘’here’’.Creative Commons BY-SA-NC
- ↑ "Papillary Carcinoma of Thyroid (Hi Pow)". University of Connecticut Health Center. Retrieved 2008-09-14.
- ↑ Yang GC, Liebeskind D, Messina AV (2001). "Ultrasound-guided fine-needle aspiration of the thyroid assessed by Ultrafast Papanicolaou stain: data from 1135 biopsies with a two- to six-year follow-up". Thyroid. 11 (6): 581–89. doi:10.1089/105072501750302895. PMID 11442006.
Categories:
- CS1 maint: Multiple names: authors list
- All articles with dead external links
- Articles with dead external links from October 2010
- Articles with invalid date parameter in template
- Pages with URL errors
- Endocrine system
- Endocrinology
- Otolaryngology
- Disease
- Genetic disorders
- Types of cancer
- Hereditary cancers
- Thyroid disease
- Primary care