Blastic NK cell lymphoma: Difference between revisions
No edit summary |
No edit summary |
||
| (28 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}} | {{CMG}} | ||
{{SK}} Agranular CD4+CD56+ hematodermic neoplasm; CD4+CD56+ hematodermic neoplasm; HDT; Blastic plasmacytoid dendritic cell neoplasm; BPDCN; | {{SK}} Agranular CD4+CD56+ hematodermic neoplasm; CD4+CD56+ hematodermic neoplasm; HDT; Blastic plasmacytoid dendritic cell neoplasm; BPDCN; Blastic natural killer cell lymphoma | ||
==Overview== | ==Overview== | ||
Blastic | Blastic natural killer cell lymphoma was first discovered by Adachi, an American hematologist, in 1994 following an unusual presentation of cutaneous lymphoma that express CD4 and CD56 antigens but no other T cell and B cell antigens. The deletion in ''5q'' has been associated with the development of blastic natural killer cell lymphoma. Blastic natural killer cell lymphoma must be differentiated from other malignancies such as [[acute myeloid leukemia]], human T-cell lymphotropic virus 1 associated adult T-cell leukemia/lymphoma, cutaneous NK/T-cell lymphoma, primary and secondary cutaneous pleomorphic T-cell lymphomas, undifferentiated carcinoma, and [[malignant melanoma]]. Blastic NK cell lymphoma is more commonly observed among middle-aged or elderly patients. The mean age at diagnosis is 66 years.<ref name="HouJaworski2015">{{cite journal|last1=Hou|first1=Steve|last2=Jaworski|first2=Joseph|last3=Swami|first3=Vanlila|last4=Heintzelman|first4=Rebecca|last5=Cusack|first5=Carrie|last6=Chung|first6=Christina|last7=Peck|first7=Jeremy|last8=Fanelli|first8=Matthew|last9=Styler|first9=Michael|last10=Rizk|first10=Sanaa|title=Blastic plasmacytoid dendritic cell neoplasm with absolute monocytosis at presentation|journal=Pathology and Laboratory Medicine International|year=2015|pages=7|issn=1179-2698|doi=10.2147/PLMI.S71492}}</ref>Males are more commonly affected with blastic natural killer cell lymphoma than females. Prognosis is generally poor, and the median survival rate is 15 months. Symptoms of blastic natural killer cell lymphoma may include nodules, plaques and patches of variable sizes on skin. Immunohistochemical staining is positive for r CD4 and CD56, with variable positivity for CD43, TdT, and CD68. The mainstay of therapy for blastic natural killer cell lymphoma is chemotherapy with CHOP or COP-like regimens. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*Blastic | *Blastic natural killer cell lymphoma was first discovered by Adachi, an American [[Hematology|hematologist]], in 1994 following an unusual presentation of [[cutaneous lymphoma]] that express [[CD4]] and [[CD56]] [[Antigen|antigens]] but no other [[T cell]] and [[B cell]] [[Antigen|antigens]].<ref name="pmid7526680">{{cite journal| author=Adachi M, Maeda K, Takekawa M, Hinoda Y, Imai K, Sugiyama S et al.| title=High expression of CD56 (N-CAM) in a patient with cutaneous CD4-positive lymphoma. | journal=Am J Hematol | year= 1994 | volume= 47 | issue= 4 | pages= 278-82 | pmid=7526680 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7526680 }} </ref> | ||
* Chaperot et al demonstrated that predendritic [[Cell (biology)|cells]] ([[Plasma cell|plasmacytoid]] [[Monocyte|monocytes]]) and [[CD4]]/[[CD56]] [[Leukemia|leukemic]] [[Cell (biology)|cells]] are similar in the production of [[Interferon|alpha-interferon]] in response to [[influenza virus]] stimulation, which on maturation with [[Interleukin 3|interleukin 3 (IL-3)]] become powerful inducers for [[CD4]] proliferation and [[Th2 cell|Th-2]] polarization. .<ref name="pmid11342451">{{cite journal| author=Chaperot L, Bendriss N, Manches O, Gressin R, Maynadie M, Trimoreau F et al.| title=Identification of a leukemic counterpart of the plasmacytoid dendritic cells. | journal=Blood | year= 2001 | volume= 97 | issue= 10 | pages= 3210-7 | pmid=11342451 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11342451 }} </ref> | |||
* Petrella and Karube demonstrated that CD123, which is a [[marker]] of predendritic [[Cell (biology)|cells]], are expressed on the [[tumor]] [[Cell (biology)|cells]] in blastic natural killer cell lymphoma and proposed an [[oncogenic]] transformation of NCAM-expressing [[Plasma cell|plasmacytoid]] [[monocyte]]-like [[Cell (biology)|cells]] as [[Cell (biology)|cell]] of origin in [[CD4]]/[[Neural cell adhesion molecule|CD56]] blastic natural killer cell lymphoma.<ref name="pmid15323148">{{cite journal| author=Petrella T, Meijer CJ, Dalac S, Willemze R, Maynadié M, Machet L et al.| title=TCL1 and CLA expression in agranular CD4/CD56 hematodermic neoplasms (blastic NK-cell lymphomas) and leukemia cutis. | journal=Am J Clin Pathol | year= 2004 | volume= 122 | issue= 2 | pages= 307-13 | pmid=15323148 | doi=10.1309/0QPP-AVTU-PCV9-UCLV | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15323148 }} </ref><ref name="pmid14508398">{{cite journal| author=Karube K, Ohshima K, Tsuchiya T, Yamaguchi T, Suefuji H, Suzumiya J et al.| title=Non-B, non-T neoplasms with lymphoblast morphology: further clarification and classification. | journal=Am J Surg Pathol | year= 2003 | volume= 27 | issue= 10 | pages= 1366-74 | pmid=14508398 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14508398 }} </ref> | |||
==Pathophysiology== | ==Pathophysiology== | ||
*Blastic | *Blastic natural killer cell lymphoma is a type of [[lymphoma]]. It does not appear to be associated with [[Epstein Barr virus|Epstein Barr virus (EBV)]] .<ref name="pmid9192774">{{cite journal |author=Chan JK, Sin VC, Wong KF, ''et al'' |title=Nonnasal lymphoma expressing the natural killer cell marker CD56: a clinicopathologic study of 49 cases of an uncommon aggressive neoplasm |journal=Blood |volume=89 |issue=12 |pages=4501–13 |year=1997 |month=June |pmid=9192774 |doi= |url=http://www.bloodjournal.org/cgi/pmidlookup?view=long&pmid=9192774}}</ref> | ||
* Blastic NK cell lymphoma is currently classified by World Health Organization Classification of | * Blastic natural killer cell lymphoma is derived from [[Plasma cell|plasmacytoid]] type 2 [[dendritic cell]] precursors. These [[dendritic cell]] precursors are possibly related to a common [[myeloid]]/[[Natural killer cell|NK-cell]] precursor [[Cell (biology)|cell]].<ref name="pmid15692063">{{cite journal| author=Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH et al.| title=WHO-EORTC classification for cutaneous lymphomas. | journal=Blood | year= 2005 | volume= 105 | issue= 10 | pages= 3768-85 | pmid=15692063 | doi=10.1182/blood-2004-09-3502 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15692063 }} </ref> | ||
*The | * Blastic natural killer cell lymphoma is currently [[Classification|classified]] by [[World Health Organization|World Health Organization (WHO)]] [[Classification]] of [[Tumor|Tumors]] of [[Hematopoiesis|Hematopoietic]] and [[Lymphoid]] [[Tissue (biology)|Tissues]] as an aggressive [[neoplasm]] derived from the precursors of [[Plasma cell|plasmacytoid]] [[Dendritic cell|dendritic cells]] and categorically placed under the heading “[[Acute myeloid leukemia|Acute myeloid leukemia (AML)]] and related precursor [[Neoplasm|neoplasms]].” | ||
*The [[Deletion (genetics)|deletion]] in ''5q'' has been associated with the development of blastic natural killer cell lymphoma. | |||
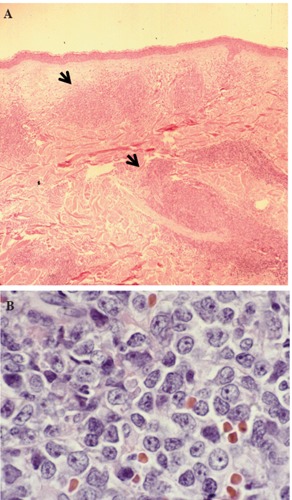
*On | * Other [[Genetics|genetic]] abnormalities associated with blastic natural killer cell lymphoma are [[Deletion (genetics)|deletion]] of ''12p'', abnormalities of [[chromosome]] 13, [[Deletion (genetics)|deletion]] of ''6q'', and loss of [[Chromosome|chromosomes]] 15 and 9. | ||
*Tumor cells are invariably CD4+ and CD56+, and usually HLA-DR and CD45RA are positive as well. CD2 and CD34 are usually negative; and expression of TdT, CD7 and cytoplasmic CD3 is variable. | *On [[hematoxylin]] and [[eosin]] (H&E) staining, fine [[chromatin]] and scanty [[cytoplasm]] resembling [[lymphoblasts]], or in some cases, [[Myeloblast|myeloblasts]], and may on occasion exhibit sub-[[Membrane|membranous]] [[cytoplasmic]] vacuolations surrounding the [[nucleus]] are characteristic findings of blastic natural killer cell lymphoma. | ||
*[[Tumor]] [[Cell (biology)|cells]] are invariably [[CD4+ lymphocytes|CD4+]] and [[CD56|CD56+]], and usually [[HLA-DR]] and CD45RA are positive as well. | |||
*[[CD2]] and [[CD34]] are usually negative; and expression of TdT, CD7 and [[Cytoplasm|cytoplasmic]] [[CD3 (immunology)|CD3]] is variable.<ref name="pmid15981806">{{cite journal| author=Petrella T, Bagot M, Willemze R, Beylot-Barry M, Vergier B, Delaunay M et al.| title=Blastic NK-cell lymphomas (agranular CD4+CD56+ hematodermic neoplasms): a review. | journal=Am J Clin Pathol | year= 2005 | volume= 123 | issue= 5 | pages= 662-75 | pmid=15981806 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15981806 }} </ref> | |||
<gallery> | <gallery> | ||
Image:Rt-2014-4-5474-g003.jpg|Hematoxylin & Eosin stain of skin lesion biopsy. Low power view of leukemic infiltrate corresponding to the raised plaque (A, black arrows) and high power view of the malignant cells in the skin infiltrate | Image:Rt-2014-4-5474-g003.jpg|Hematoxylin & Eosin stain of skin lesion biopsy. Low power view of leukemic infiltrate corresponding to the raised plaque (A, black arrows) and high power view of the malignant cells in the skin infiltrate | ||
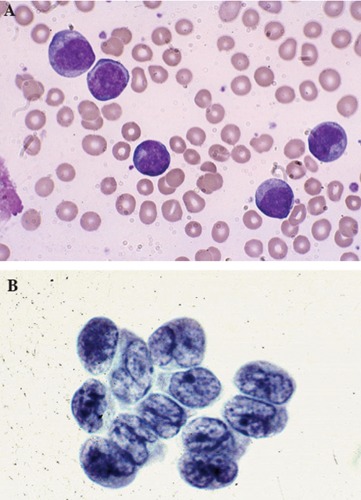
Image:Rt-2014-4-5474-g002 02.jpg|Large malignant-appearing cells, with agranular cytoplasm, cleaved nuclei and prominent neocleoli on peripheral blood smear using Wright stain (A) and similar blast cells present in cerebrospinal fluid | Image:Rt-2014-4-5474-g002 02.jpg|Large malignant-appearing cells, with agranular cytoplasm, cleaved nuclei and prominent neocleoli on peripheral blood smear using Wright stain (A) and similar blast cells present in cerebrospinal fluid | ||
</gallery> | </gallery> | ||
==Differentiating [disease name] | ==Differentiating Blastic NK cell Lymphoma from other Diseases== | ||
*Blastic | '''<small>ABBREVIATIONS''' | ||
'''N/A''': Not available, '''NL''': Normal, '''FISH''': Fluorescence in situ hybridization, '''PCR''': Polymerase chain reaction, '''LDH''': Lactate dehydrogenase, '''PUD''': Peptic ulcer disease, '''EPO''': Erythropoietin, '''LFTs''': Liver function tests, '''RFTs''': Renal function tests, '''LAP''': Leukocyte alkaline phosphatase, '''LAD''': Leukocyte alkaline dehydrgenase, '''WBCs''': White blood cells. </small> | |||
<small> | |||
{| class="wikitable" | |||
! colspan="2" rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Myeloproliferative neoplasms (MPN) | |||
! colspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Clinical manifestations | |||
! colspan="11" style="background:#4479BA; color: #FFFFFF;" align="center" + |Diagnosis | |||
! rowspan="4" style="background:#4479BA; color: #FFFFFF;" align="center" + |Other features | |||
|- | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Symptoms | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Physical examination | |||
! colspan="9" style="background:#4479BA; color: #FFFFFF;" align="center" + |CBC & Peripheral smear | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Bone marrow biopsy | |||
! rowspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + |Other investigations | |||
|- | |||
! colspan="7" style="background:#4479BA; color: #FFFFFF;" align="center" + |WBCs | |||
! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Hb | |||
! rowspan="2" style="background:#4479BA; color: #FFFFFF;" align="center" + |Plat-<br>elets | |||
|- | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Leuko-cytes</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Blasts</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Left<br>shift</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Baso-<br>phils</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Eosino-<br>phils</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Mono-<br>cytes</small> | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |<small>Others</small> | |||
|- | |||
| colspan="2" |[[Chronic myeloid leukemia]]<br>([[CML]]), [[BCR/ABL|BCR-ABL1]]+<ref name="pmid9012696">{{cite journal |vauthors=Savage DG, Szydlo RM, Goldman JM |title=Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period |journal=Br. J. Haematol. |volume=96 |issue=1 |pages=111–6 |date=January 1997 |pmid=9012696 |doi= |url=}}</ref><ref name="pmid26434969">{{cite journal |vauthors=Thompson PA, Kantarjian HM, Cortes JE |title=Diagnosis and Treatment of Chronic Myeloid Leukemia in 2015 |journal=Mayo Clin. Proc. |volume=90 |issue=10 |pages=1440–54 |date=October 2015 |pmid=26434969 |pmc=5656269 |doi=10.1016/j.mayocp.2015.08.010 |url=}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional</small> | |||
* <small>[[Hyperviscosity]] and/or [[anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Splenomegaly]]<br>(46–76%)</small> | |||
* <small>[[Purpura]]</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Priapism]]</small> | |||
|↑ | |||
|<small><2%</small> | |||
| + | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>NL</small> | |||
| | |||
* <small>Hypercellurarity with ↑ [[granuloscytosis]] and ↓ [[erythrocytosis]]</small> | |||
* <small>[[Fibrosis]]</small> | |||
| | |||
* <small>[[FISH]] for t(9;22)(q34;q11.2)</small> | |||
* <small>[[Reverse transcriptase]] quantitative [[PCR]] (RQ-PCR) for BCR-ABL</small> | |||
| | |||
* <small>[[Granulocytic]] [[dysplasia]] is minimal/absent</small> | |||
* <small>May present with [[blast]] crisis</small> | |||
* <small>Absolute [[leukocytosis]]</small> <small>(median of 100,000/µL)</small> | |||
* <small>Classic [[myelocyte]] bulge</small> | |||
* <small>[[thrombocytopenia]] indicates advanced stage</small> | |||
|- | |||
| colspan="2" |[[Chronic neutrophilic leukemia]] ([[CNL]])<ref name="pmid29440636">{{cite journal |vauthors=Szuber N, Tefferi A |title=Chronic neutrophilic leukemia: new science and new diagnostic criteria |journal=Blood Cancer J |volume=8 |issue=2 |pages=19 |date=February 2018 |pmid=29440636 |pmc=5811432 |doi=10.1038/s41408-018-0049-8 |url=}}</ref><ref name="pmid28028025">{{cite journal |vauthors=Maxson JE, Tyner JW |title=Genomics of chronic neutrophilic leukemia |journal=Blood |volume=129 |issue=6 |pages=715–722 |date=February 2017 |pmid=28028025 |pmc=5301820 |doi=10.1182/blood-2016-10-695981 |url=}}</ref><ref name="pmid26366092">{{cite journal |vauthors=Menezes J, Cigudosa JC |title=Chronic neutrophilic leukemia: a clinical perspective |journal=Onco Targets Ther |volume=8 |issue= |pages=2383–90 |date=2015 |pmid=26366092 |pmc=4562747 |doi=10.2147/OTT.S49688 |url=}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional symptoms</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Heptomegaly]]</small> | |||
* <small>[[Purpura]]</small> | |||
* <small>[[Anemia]] related</small> | |||
|↑ | |||
|<small>Minimal</small> | |||
| + | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[LDH]]</small> | |||
* <small>↑ [[B12]] levels</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Uniforme and intense hypercellularity with minimal to none [[fibrosis]]</small> | |||
* <small>[[Neutrophil]] toxic granulations and [[Dohle bodies]]</small> | |||
| | |||
* <small>[[FISH]]</small> | |||
* <small>Imaging for [[hepatosplenomegaly]]</small> | |||
| | |||
* <small>Associationed with [[polycythemia vera]] and [[plasma cell disorders]]</small> | |||
* <small>[[Leukocytosis]] with<br>[[chronic]] [[neutrophilia]]</small> | |||
|- | |||
| colspan="2" |[[Polycythemia vera]]<br>([[PV]])<ref name="pmid29194068">{{cite journal |vauthors=Vannucchi AM, Guglielmelli P, Tefferi A |title=Polycythemia vera and essential thrombocythemia: algorithmic approach |journal=Curr. Opin. Hematol. |volume=25 |issue=2 |pages=112–119 |date=March 2018 |pmid=29194068 |doi=10.1097/MOH.0000000000000402 |url=}}</ref><ref name="pmid30252337">{{cite journal |vauthors=Pillai AA, Babiker HM |title= |journal= |volume= |issue= |pages= |date= |pmid=30252337 |doi= |url=}}</ref><ref name="pmid30281843">{{cite journal |vauthors=Tefferi A, Barbui T |title=Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management |journal=Am. J. Hematol. |volume=94 |issue=1 |pages=133–143 |date=January 2019 |pmid=30281843 |doi=10.1002/ajh.25303 |url=}}</ref><ref name="pmid28028026">{{cite journal |vauthors=Rumi E, Cazzola M |title=Diagnosis, risk stratification, and response evaluation in classical myeloproliferative neoplasms |journal=Blood |volume=129 |issue=6 |pages=680–692 |date=February 2017 |pmid=28028026 |pmc=5335805 |doi=10.1182/blood-2016-10-695957 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Thromboembolism]]<br>and [[bleeding]]</small> | |||
* <small>[[Pruritus]] after<br>a warm bath</small> | |||
* <small>[[PUD]] related</small> | |||
| | |||
* <small>Facial ruddiness</small> | |||
* <small>Related to underlying cause</small> | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Renal]] [[bruit]]</small> | |||
|<small>NL or ↑</small> | |||
|<small>None</small> | |||
| - | |||
|<small>↑ or ↓</small> | |||
|<small>NL or ↑</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↓ Serum [[ferritin]]</small> | |||
* <small>↓ [[Folate]] levels</small> | |||
* <small>↑↑ [[B12]] levels</small> | |||
|<small>↑↑</small> | |||
|<small>NL</small> | |||
| | |||
* <small>Hypercellularity for age with tri-lineage growth</small> | |||
* <small>[[Myelofibrosis]] (in up to 20% of patients)</small> | |||
| | |||
* <small>[[Radioisotope]] studies</small> | |||
* <small>[[Serum]] [[EPO]] levels</small> | |||
* <small>[[LFTs]]</small> | |||
* <small>[[RFTs]]</small> | |||
* <small>[[Imaging]] studies</small> | |||
| | |||
* <small>May transform into [[myelofibrosis]] or [[leukemia]]</small> | |||
|- | |||
| colspan="2" |[[Primary myelofibrosis]] ([[PMF]])<ref name="pmid26891375">{{cite journal |vauthors=Cervantes F, Correa JG, Hernandez-Boluda JC |title=Alleviating anemia and thrombocytopenia in myelofibrosis patients |journal=Expert Rev Hematol |volume=9 |issue=5 |pages=489–96 |date=May 2016 |pmid=26891375 |doi=10.1586/17474086.2016.1154452 |url=}}</ref><ref>{{cite book | last = Hoffman | first = Ronald | title = Hematology : basic principles and practice | publisher = Elsevier | location = Philadelphia, PA | year = 2018 | isbn = 9780323357623 }}</ref><ref name="pmid16919893">{{cite journal |vauthors=Michiels JJ, Bernema Z, Van Bockstaele D, De Raeve H, Schroyens W |title=Current diagnostic criteria for the chronic myeloproliferative disorders (MPD) essential thrombocythemia (ET), polycythemia vera (PV) and chronic idiopathic myelofibrosis (CIMF) |journal=Pathol. Biol. |volume=55 |issue=2 |pages=92–104 |date=March 2007 |pmid=16919893 |doi=10.1016/j.patbio.2006.06.002 |url=}}</ref><ref>{{cite book | last = Hoffman | first = Ronald | title = Hematology : basic principles and practice | publisher = Elsevier | location = Philadelphia, PA | year = 2018 | isbn = 9780323357623 }}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
* <small>[[Abdominal]] [[Pain]]</small> | |||
| | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
* <small>[[Petechiae]] & [[ecchymoses]]</small> | |||
* <small>Abdominal distension</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
|↓ | |||
|<small>[[Erythroblasts]]</small> | |||
| - | |||
|<small>Absent</small> | |||
|<small>NL</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[LAP]]</small> | |||
* <small>↑ [[LAD]]</small> | |||
* ↑ <small>[[Uric acid]]</small> | |||
* <small>↑ [[B12]] levels</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Variable with [[fibrosis]] or hypercellularity</small> | |||
| | |||
* <small>JAK2 mutation</small> | |||
* <small>[[CALR]] [[mutation]]</small> | |||
* <small>[[MPL]] [[mutation]]</small> | |||
| | |||
* <small>[[Bone marrow]] aspiration shows a dry tap</small> | |||
* <small>Variable with [[leukocytosis]] or [[leukopenia]]</small> | |||
|- | |||
| colspan="2" |[[Essential thrombocythemia]] ([[ET]])<ref name="pmidhttp://dx.doi.org/10.1182/blood-2007-04-083501">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=http://dx.doi.org/10.1182/blood-2007-04-083501 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref>{{Cite journal | |||
| author = [[Daniel A. Arber]], [[Attilio Orazi]], [[Robert Hasserjian]], [[Jurgen Thiele]], [[Michael J. Borowitz]], [[Michelle M. Le Beau]], [[Clara D. Bloomfield]], [[Mario Cazzola]] & [[James W. Vardiman]] | |||
| title = The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia | |||
| journal = [[Blood]] | |||
| volume = 127 | |||
| issue = 20 | |||
| pages = 2391–2405 | |||
| year = 2016 | |||
| month = May | |||
| doi = 10.1182/blood-2016-03-643544 | |||
| pmid = 27069254 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[A. Tefferi]], [[R. Fonseca]], [[D. L. Pereira]] & [[H. C. Hoagland]] | |||
| title = A long-term retrospective study of young women with essential thrombocythemia | |||
| journal = [[Mayo Clinic proceedings]] | |||
| volume = 76 | |||
| issue = 1 | |||
| pages = 22–28 | |||
| year = 2001 | |||
| month = January | |||
| doi = 10.4065/76.1.22 | |||
| pmid = 11155408 | |||
}}</ref> | |||
| | |||
* <small>Headache</small> | |||
* <small>[[Dizziness]]</small> | |||
* <small>[[Visual]] disturbances</small> | |||
* <small>[[Priapism]]</small> | |||
* <small>Acute [[chest pain]]</small> | |||
| | |||
* <small>[[Splenomegaly]]</small> | |||
* <small>[[Skin]] [[bruises]]</small> | |||
| | |||
<small>NL or ↑</small> | |||
| | |||
<small>None</small> | |||
| - | |||
| | |||
<small>↓ or absent</small> | |||
| | |||
<small>NL</small> | |||
| | |||
<small>NL</small> | |||
| | |||
* <small>N/A</small> | |||
| | |||
[[Anemia|<small>↓</small>]] | |||
| | |||
<small>↑↑</small> | |||
| | |||
* <small>Normal/Hypercellular</small> | |||
| | |||
* <small>[[JAK2]] [[mutation]]</small> | |||
* <small>[[CALR]] [[mutation]]</small> | |||
* <small>[[MPL]] [[mutation]]</small> | |||
| | |||
* <small>[[Thrombosis]]</small> | |||
* <small>[[Hemorrhage]]</small> | |||
* <small>[[Pregnancy]] loss</small> | |||
|- | |||
| colspan="2" |[[Chronic eosinophilic leukemia]],<br>not otherwise specified<br>(NOS)<ref name="pmid27512192">{{cite journal |vauthors=Vidyadharan S, Joseph B, Nair SP |title=Chronic Eosinophilic Leukemia Presenting Predominantly with Cutaneous Manifestations |journal=Indian J Dermatol |volume=61 |issue=4 |pages=437–9 |date=2016 |pmid=27512192 |pmc=4966405 |doi=10.4103/0019-5154.185716 |url=}}</ref><ref name="pmid29892549">{{cite journal |vauthors=Hofmans M, Delie A, Vandepoele K, Van Roy N, Van der Meulen J, Philippé J, Moors I |title=A case of chronic eosinophilic leukemia with secondary transformation to acute myeloid leukemia |journal=Leuk Res Rep |volume=9 |issue= |pages=45–47 |date=2018 |pmid=29892549 |pmc=5993353 |doi=10.1016/j.lrr.2018.04.001 |url=}}</ref><ref name="pmid23662039">{{cite journal |vauthors=Yamada Y, Rothenberg ME, Cancelas JA |title=Current concepts on the pathogenesis of the hypereosinophilic syndrome/chronic eosinophilic leukemia |journal=Transl Oncogenomics |volume=1 |issue= |pages=53–63 |date=2006 |pmid=23662039 |pmc=3642145 |doi= |url=}}</ref><ref name="pmid27722133">{{cite journal |vauthors=Kim TH, Gu HJ, Lee WI, Lee J, Yoon HJ, Park TS |title=Chronic eosinophilic leukemia with FIP1L1-PDGFRA rearrangement |journal=Blood Res |volume=51 |issue=3 |pages=204–206 |date=September 2016 |pmid=27722133 |doi=10.5045/br.2016.51.3.204 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Rash]]</small> | |||
* <small>[[Rhinitis]]</small> | |||
* <small>[[Gastritis]]</small> | |||
* <small>[[Thromboembolism]]<br>related</small> | |||
| | |||
* <small>[[Hypertension]]</small> | |||
* <small>[[Eczema]], [[mucosal]] [[ulcers]], [[erythema]]</small> | |||
* <small>[[Angioedema]]</small> | |||
* <small>[[Ataxia]]</small> | |||
* <small>[[Anemia]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>Present</small> | |||
| + | |||
|<small>↑</small> | |||
|<small>↑↑</small> | |||
|<small>↑</small> | |||
| | |||
* <small>↑ [[B12]] levels</small> | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercelluar with ↑ [[eosinophilic]] precursors, ↑ [[eosinophils]], and atypical [[mononuclear cells]]</small> | |||
| | |||
* <small>[[FISH]]</small> | |||
* <small>Cytogenetic analysis of purified [[eosinophils]] and [[X-chromosome]] inactivation analysis</small> | |||
| | |||
* <small>[[Heart failure]]</small> <small>[[Lung fibrosis]]</small> | |||
* <small>[[Encephalopathy]]</small> | |||
* <small>[[Erythema annulare centrifugam]]</small> | |||
|- | |||
| colspan="2" |[[Myeloproliferative neoplasm|MPN]],<br>unclassifiable | |||
|<small> | |||
*Similar to other<br>[[Myeloproliferative neoplasm|myeloproliferative neoplasms]]</small> | |||
|<small> | |||
*Similar to other<br>[[Myeloproliferative neoplasm|myeloproliferative neoplasms]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>Variable</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>May resemble other<br>[[myeloproliferative neoplasms]]</small> | |||
|<small>↓</small> | |||
|<small>↑</small> | |||
| | |||
* <small>↑ [[megakaryocyte]] proliferation with variable hypercellularity in [[granulocytic]] or [[erythrocytic]] cell lines</small> | |||
| | |||
* <small>N/A</small> | |||
|<small> | |||
*Similar to other [[myeloprolifeartive neoplasms]] but do not fulfil the criteria to be classified to a specific type</small> | |||
|- | |||
| colspan="2" |[[Mastocytosis]]<ref name="pmid24262698">{{cite journal |vauthors=Carter MC, Metcalfe DD, Komarow HD |title=Mastocytosis |journal=Immunol Allergy Clin North Am |volume=34 |issue=1 |pages=181–96 |date=February 2014 |pmid=24262698 |pmc=3863935 |doi=10.1016/j.iac.2013.09.001 |url=}}</ref><ref name="pmid29494109">{{cite journal |vauthors=Macri A, Cook C |title= |journal= |volume= |issue= |pages= |date= |pmid=29494109 |doi= |url=}}</ref><ref name="pmid25031064">{{cite journal |vauthors=Lladó AC, Mihon CE, Silva M, Galzerano A |title=Systemic mastocytosis - a diagnostic challenge |journal=Rev Bras Hematol Hemoter |volume=36 |issue=3 |pages=226–9 |date=2014 |pmid=25031064 |pmc=4109736 |doi=10.1016/j.bjhh.2014.03.003 |url=}}</ref><ref name="pmid28031180">{{cite journal |vauthors=Valent P, Akin C, Metcalfe DD |title=Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts |journal=Blood |volume=129 |issue=11 |pages=1420–1427 |date=March 2017 |pmid=28031180 |pmc=5356454 |doi=10.1182/blood-2016-09-731893 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Pruritus]] & [[Flushing]]</small> | |||
* <small>[[Urticaria]] & [[Blisters]]</small> | |||
* <small>[[Hypotension]] & [[PUD]]</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Bronchoconstriction]]</small> | |||
| | |||
* <small>[[Mastocytosis exanthema]]</small> | |||
* <small>[[Blistering]]</small> | |||
* <small>[[Swelling]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Fibrosis]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>None</small> | |||
| - | |||
|<small>NL</small> | |||
|<small>[[Eosinophilia|↑]]</small> | |||
|<small>NL</small> | |||
| | |||
* <small>↑ [[Alkaline phosphatase]]</small> | |||
* <small>↑ [[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>↓ or ↑</small> | |||
| | |||
* <small>Multifocal dense infiltrates of [[mast cells]] with atypical [[morphology]] in >25 %</small> | |||
| | |||
* <small>Cytogenetic analysis for [[c-KIT]] [[receptor]] [[mutations]]</small> | |||
* <small>[[Serum]] [[tryptase]] levels</small> | |||
* <small>24-hour urine test for N-methyl [[histamine]] and 11-beta-[[prostaglandine]]</small> | |||
| | |||
* <small>Skin most commonly involved</small> | |||
* <small>Susceptibility to [[anaphylaxix]]</small> | |||
* <small>[[Osteoporosis]]</small> | |||
|- | |||
| colspan="2" |[[Myeloid]]/[[lymphoid]] [[neoplasms]]<br>with [[eosinophilia]] and rearrangement<br>of [[PDGFR|PDGFRA]], [[PDGFRB]], or [[FGFR1]],<br>or with [[PCM1]]-[[JAK2]]<ref name="KumarChen2015">{{cite journal|last1=Kumar|first1=Kirthi R.|last2=Chen|first2=Weina|last3=Koduru|first3=Prasad R.|last4=Luu|first4=Hung S.|title=Myeloid and Lymphoid Neoplasm With Abnormalities of FGFR1 Presenting With Trilineage Blasts and RUNX1 Rearrangement|journal=American Journal of Clinical Pathology|volume=143|issue=5|year=2015|pages=738–748|issn=1943-7722|doi=10.1309/AJCPUD6W1JLQQMNA}}</ref><ref>{{Cite journal | |||
| author = [[Paolo Strati]], [[Guilin Tang]], [[Dzifa Y. Duose]], [[Saradhi Mallampati]], [[Rajyalakshmi Luthra]], [[Keyur P. Patel]], [[Mohammad Hussaini]], [[Abu-Sayeef Mirza]], [[Rami S. Komrokji]], [[Stephen Oh]], [[John Mascarenhas]], [[Vesna Najfeld]], [[Vivek Subbiah]], [[Hagop Kantarjian]], [[Guillermo Garcia-Manero]], [[Srdan Verstovsek]] & [[Naval Daver]] | |||
| title = Myeloid/lymphoid neoplasms with FGFR1 rearrangement | |||
| journal = [[Leukemia & lymphoma]] | |||
| volume = 59 | |||
| issue = 7 | |||
| pages = 1672–1676 | |||
| year = 2018 | |||
| month = July | |||
| doi = 10.1080/10428194.2017.1397663 | |||
| pmid = 29119847 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Ximena Montenegro-Garreaud]], [[Roberto N. Miranda]], [[Alexandra Reynolds]], [[Guilin Tang]], [[Sa A. Wang]], [[Mariko Yabe]], [[Wei Wang]], [[Lianghua Fang]], [[Carlos E. Bueso-Ramos]], [[Pei Lin]], [[L. Jeffrey Medeiros]] & [[Xinyan Lu]] | |||
| title = Myeloproliferative neoplasms with t(8;22)(p11.2;q11.2)/BCR-FGFR1: a meta-analysis of 20 cases shows cytogenetic progression with B-lymphoid blast phase | |||
| journal = [[Human pathology]] | |||
| volume = 65 | |||
| pages = 147–156 | |||
| year = 2017 | |||
| month = July | |||
| doi = 10.1016/j.humpath.2017.05.008 | |||
| pmid = 28551329 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Paola Villafuerte-Gutierrez]], [[Montserrat Lopez Rubio]], [[Pilar Herrera]] & [[Eva Arranz]] | |||
| title = A Case of Myeloproliferative Neoplasm with BCR-FGFR1 Rearrangement: Favorable Outcome after Haploidentical Allogeneic Transplantation | |||
| journal = [[Case reports in hematology]] | |||
| volume = 2018 | |||
| pages = 5724960 | |||
| year = 2018 | |||
| month = | |||
| doi = 10.1155/2018/5724960 | |||
| pmid = 30647980 | |||
}}</ref> | |||
| | |||
* <small>Asymptomatic</small> | |||
* <small>Constitutional</small> | |||
* <small>[[Rash]]</small> | |||
* <small>[[Cough]] & breathlessness</small> | |||
* <small>[[Peripheral neuropathy]]/<br>[[encephalopathy]]</small> | |||
| | |||
* <small>[[Fever]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
| ↑ | |||
| <small>NL</small> | |||
| - | |||
| <small>NL</small> | |||
| <small>[[Eosinophilia|↑]]</small> | |||
|<small>[[Monocytosis|↑]]</small> | |||
| | |||
* <small>None</small> | |||
| <small>NL</small> | |||
| <small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Myeloid]] expansion with [[eosinophilia]]</small> | |||
| | |||
* <small>[[FISH]] shows t(8;13) and t(8;22)</small> | |||
| | |||
* <small>May present or evolve into [[acute myeloid]] or [[lymphoblastic leukemia]]</small> | |||
* <small>[[Leukocytosis]] (30 - 59 × 10<sup>9</sup>/L</small> | |||
|- | |||
| colspan="2" |B-lymphoblastic leukemia/lymphoma<ref name="pmid30107017">{{cite journal |vauthors=Kamiya-Matsuoka C, Garciarena P, Amin HM, Tremont-Lukats IW, de Groot JF |title=B lymphoblastic leukemia/lymphoma presenting as seventh cranial nerve palsy |journal=Neurol Clin Pract |volume=3 |issue=6 |pages=532–534 |date=December 2013 |pmid=30107017 |pmc=6082360 |doi=10.1212/CPJ.0b013e3182a78ef0 |url=}}</ref><ref name="pmid29029550">{{cite journal |vauthors=Zhang X, Rastogi P, Shah B, Zhang L |title=B lymphoblastic leukemia/lymphoma: new insights into genetics, molecular aberrations, subclassification and targeted therapy |journal=Oncotarget |volume=8 |issue=39 |pages=66728–66741 |date=September 2017 |pmid=29029550 |pmc=5630450 |doi=10.18632/oncotarget.19271 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
* <small>[[Bone pain]]</small> | |||
| | |||
* <small>[[Pallor]]</small> | |||
* <small>[[Petechiae]]</small> | |||
* <small>[[Organomegaly]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
|<small>NL or ↑</small> | |||
|<small>>25%</small> | |||
|<small>N/A</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>[[Auer rod|Auer bodies]]</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercellular with [[blast]] infilteration</small><small>with or without [[myelodysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>May present as [[Extramedullary myeloid tumor|extramedullary]] disease ([[Extramedullary Myeloid Cell Tumor|Myeloid sarcoma]])</small> | |||
|- | |||
| colspan="2" |[[Myelodysplastic syndrome|Myelodysplastic syndromes]]<br>([[MDS]])<ref name="pmid24300826">{{cite journal |vauthors=Germing U, Kobbe G, Haas R, Gattermann N |title=Myelodysplastic syndromes: diagnosis, prognosis, and treatment |journal=Dtsch Arztebl Int |volume=110 |issue=46 |pages=783–90 |date=November 2013 |pmid=24300826 |pmc=3855821 |doi=10.3238/arztebl.2013.0783 |url=}}</ref><ref name="pmid26769228">{{cite journal |vauthors=Gangat N, Patnaik MM, Tefferi A |title=Myelodysplastic syndromes: Contemporary review and how we treat |journal=Am. J. Hematol. |volume=91 |issue=1 |pages=76–89 |date=January 2016 |pmid=26769228 |doi=10.1002/ajh.24253 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infection]]</small> | |||
| | |||
* <small>[[Pallor]]</small> | |||
* <small>[[Petechiae]]</small> | |||
* <small>[[Organomegaly]]</small> | |||
|[[Leukopenia|<small>↓</small>]] | |||
|<small>Variable</small> | |||
| - | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Macro-ovalocytes</small> | |||
* <small>Basophilic stippling</small> | |||
* [[Howell-Jolly body|<small>Howell-Jolly body</small>]] | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercellular</small><small>/ normocellular [[bone marrow]] with [[Dysplastic change|dysplastic]] changes</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>[[Leukemia]] transformation</small> | |||
* <small>Acquired pseudo-Pelger-Huët anomaly</small> | |||
|- | |||
| colspan="2" |[[Acute myeloid leukemia]] ([[AML]])<br>and related [[neoplasms]]<ref name="pmid3864727">{{cite journal |vauthors=Islam A, Catovsky D, Goldman JM, Galton DA |title=Bone marrow biopsy changes in acute myeloid leukaemia. I: Observations before chemotherapy |journal=Histopathology |volume=9 |issue=9 |pages=939–57 |date=September 1985 |pmid=3864727 |doi= |url=}}</ref><ref name="pmid17587881">{{cite journal |vauthors=Orazi A |title=Histopathology in the diagnosis and classification of acute myeloid leukemia, myelodysplastic syndromes, and myelodysplastic/myeloproliferative diseases |journal=Pathobiology |volume=74 |issue=2 |pages=97–114 |date=2007 |pmid=17587881 |doi=10.1159/000101709 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* [[Bleeding|<small>Bleeding</small>]] | |||
* [[Bone pain|<small>Bone pain</small>]] | |||
* [[Joint pain|<small>Joint pain</small>]] | |||
* [[Infections|<small>Infections</small>]] | |||
| | |||
* <small>[[Infection]] related</small> | |||
* [[Pallor|<small>Pallor</small>]] | |||
* [[Chloroma|<small>Leukemia cutis</small>]] | |||
* <small>[[Bruising]] & [[Petechia|petechiae]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* [[Hepatomegaly|<small>Hepatosplenomegaly</small>]] | |||
|<small>NL or ↑</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* <small>↑ [[Potassium]]</small> | |||
* <small>↑ [[Uric acid]]</small> | |||
* <small>↑ [[Phosphorus]]</small> | |||
* <small>↓ [[Calcium]]</small> | |||
* <small>↑ [[LDH]]</small> | |||
|[[Anemia|<small>↓</small>]] | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Increased immature[[myeloid]] [[cells]]</small> | |||
<small>with [[Dysplastic change|dysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>Common in [[Down syndrome]]</small> | |||
|- | |||
| colspan="2" |[[Blastic plasmacytoid dendritic cell neoplasm|Blastic plasmacytoid<br>dendritic cell neoplasm]]<ref>{{Cite journal | |||
| author = [[F. Julia]], [[T. Petrella]], [[M. Beylot-Barry]], [[M. Bagot]], [[D. Lipsker]], [[L. Machet]], [[P. Joly]], [[O. Dereure]], [[M. Wetterwald]], [[M. d'Incan]], [[F. Grange]], [[J. Cornillon]], [[G. Tertian]], [[E. Maubec]], [[P. Saiag]], [[S. Barete]], [[I. Templier]], [[F. Aubin]] & [[S. Dalle]] | |||
| title = Blastic plasmacytoid dendritic cell neoplasm: clinical features in 90 patients | |||
| journal = [[The British journal of dermatology]] | |||
| volume = 169 | |||
| issue = 3 | |||
| pages = 579–586 | |||
| year = 2013 | |||
| month = September | |||
| doi = 10.1111/bjd.12412 | |||
| pmid = 23646868 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Livio Pagano]], [[Caterina Giovanna Valentini]], [[Alessandro Pulsoni]], [[Simona Fisogni]], [[Paola Carluccio]], [[Francesco Mannelli]], [[Monia Lunghi]], [[Gianmatteo Pica]], [[Francesco Onida]], [[Chiara Cattaneo]], [[Pier Paolo Piccaluga]], [[Eros Di Bona]], [[Elisabetta Todisco]], [[Pellegrino Musto]], [[Antonio Spadea]], [[Alfonso D'Arco]], [[Stefano Pileri]], [[Giuseppe Leone]], [[Sergio Amadori]] & [[Fabio Facchetti]] | |||
| title = Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study | |||
| journal = [[Haematologica]] | |||
| volume = 98 | |||
| issue = 2 | |||
| pages = 239–246 | |||
| year = 2013 | |||
| month = February | |||
| doi = 10.3324/haematol.2012.072645 | |||
| pmid = 23065521 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Joseph D. Khoury]] | |||
| title = Blastic Plasmacytoid Dendritic Cell Neoplasm | |||
| journal = [[Current hematologic malignancy reports]] | |||
| volume = 13 | |||
| issue = 6 | |||
| pages = 477–483 | |||
| year = 2018 | |||
| month = December | |||
| doi = 10.1007/s11899-018-0489-z | |||
| pmid = 30350260 | |||
}}</ref><ref>{{Cite journal | |||
| author = [[Shinichiro Sukegawa]], [[Mamiko Sakata-Yanagimoto]], [[Ryota Matsuoka]], [[Haruka Momose]], [[Yusuke Kiyoki]], [[Masayuki Noguchi]], [[Naoya Nakamura]], [[Rei Watanabe]], [[Manabu Fujimoto]], [[Yasuhisa Yokoyama]], [[Hidekazu Nishikii]], [[Takayasu Kato]], [[Manabu Kusakabe]], [[Naoki Kurita]], [[Naoshi Obara]], [[Yuichi Hasegawa]] & [[Shigeru Chiba]] | |||
| title = [Blastic plasmacytoid dendritic cell neoplasm accompanied by chronic myelomonocytic leukemia successfully treated with azacitidine] | |||
| journal = <nowiki>[[[Rinsho ketsueki] The Japanese journal of clinical hematology]]</nowiki> | |||
| volume = 59 | |||
| issue = 12 | |||
| pages = 2567–2573 | |||
| year = 2018 | |||
| month = | |||
| doi = 10.11406/rinketsu.59.2567 | |||
| pmid = 30626790 | |||
}}</ref> | |||
| | |||
* <small>[[Cutaneous]] symptoms (brown/purple nodular lesions) on [[face]], [[scalp]], [[lower limb]] & [[trunk]]</small> | |||
| | |||
* <small>Brown/violaceous [[bruise]] like lesions</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Splenomegaly]]</small> | |||
| <small>NL</small> | |||
| <small>↑</small> | |||
| | |||
|<small>NL</small> | |||
| <small>NL</small> | |||
| <small>NL</small> | |||
| | |||
* <small>[[Neutropenia]]</small> | |||
| [[Anemia|<small>↓</small>]] | |||
| <small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Malignant|Malignant cells]]</small> | |||
| | |||
* <small>[[Immunohistochemistry]] or [[flow cytometry]] for [[CD4]] & [[CD56]]</small> | |||
| | |||
* <small>TdT expression positive</small> | |||
* <small>May develop [[chronic myelomonocytic leukemia]] (CMML)</small> | |||
|- | |||
| rowspan="4" |[[Myelodysplastic]]<br>/[[Myeloproliferative neoplasm|myeloproliferative<br>neoplasms]] (MDS/MPN) | |||
|<small>[[Chronic myelomonocytic leukemia]] (CMML)</small><ref name="pmid27185207">{{cite journal |vauthors=Patnaik MM, Tefferi A |title=Chronic myelomonocytic leukemia: 2016 update on diagnosis, risk stratification, and management |journal=Am. J. Hematol. |volume=91 |issue=6 |pages=631–42 |date=June 2016 |pmid=27185207 |doi=10.1002/ajh.24396 |url=}}</ref> | |||
: <ref name="pmid22615103">{{cite journal |vauthors=Parikh SA, Tefferi A |title=Chronic myelomonocytic leukemia: 2012 update on diagnosis, risk stratification, and management |journal=Am. J. Hematol. |volume=87 |issue=6 |pages=610–9 |date=June 2012 |pmid=22615103 |doi=10.1002/ajh.23203 |url=}}</ref><ref name="pmid25869097">{{cite journal |vauthors=Benton CB, Nazha A, Pemmaraju N, Garcia-Manero G |title=Chronic myelomonocytic leukemia: Forefront of the field in 2015 |journal=Crit. Rev. Oncol. Hematol. |volume=95 |issue=2 |pages=222–42 |date=August 2015 |pmid=25869097 |pmc=4859155 |doi=10.1016/j.critrevonc.2015.03.002 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Infections]]</small> | |||
* <small>[[Bone]] [[pain]]</small> | |||
* <small>[[Leukemia Cutis]]</small> | |||
| | |||
* <small>[[Organomegaly]]</small> | |||
* <small>[[Bruising]]</small> | |||
|↑ | |||
| <small>< 20%</small> | |||
| | |||
|<small>NL</small> | |||
|<small>[[Eosinophilia|↑]]</small> | |||
|↑↑ | |||
| | |||
* <small>↑ [[LDH]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>[[Myelodysplastic]] and [[myeloproliferative]] feature</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Overlapping of both, [[MDS]] and [[MPN]]</small> | |||
* <small>Absolute [[monocytosis]] > 1 × 10<sup>9</sup>/L (defining feature)</small> | |||
* <small>MD-CMML:</small><small>[[WBC]] ≤ 13 × 10<sup>9</sup>/L (FAB)</small> | |||
* <small> MP-CMML:</small><small>[[WBC]] > 13 × 10<sup>9</sup>/L</small> <small>(FAB)</small> | |||
|- | |||
|<small>[[Atypical chronic myeloid leukemia]] (aCML), [[BCR/ABL|BCR-ABL]]1-</small><ref name="pmid26637732">{{cite journal |vauthors=Dao KH, Tyner JW |title=What's different about atypical CML and chronic neutrophilic leukemia? |journal=Hematology Am Soc Hematol Educ Program |volume=2015 |issue= |pages=264–71 |date=2015 |pmid=26637732 |pmc=5266507 |doi=10.1182/asheducation-2015.1.264 |url=}}</ref><ref name="pmid22289493">{{cite journal |vauthors=Muramatsu H, Makishima H, Maciejewski JP |title=Chronic myelomonocytic leukemia and atypical chronic myeloid leukemia: novel pathogenetic lesions |journal=Semin. Oncol. |volume=39 |issue=1 |pages=67–73 |date=February 2012 |pmid=22289493 |pmc=3523950 |doi=10.1053/j.seminoncol.2011.11.004 |url=}}</ref> | |||
|<small> | |||
*Asymptomatic</small> | |||
* Constitutional | |||
* [[Hyperviscosity|Hyperviscosity]] and/or [[anemia]] related | |||
* [[Bleeding|Bleeding]] | |||
* [[Infection|Infection]] | |||
|<small> | |||
* [[Splenomegaly]]</small> (46–76%) | |||
* [[Purpura]] | |||
* [[Anemia]] related | |||
* [[Priapism]] | |||
|↑ | |||
|<small><20%</small> | |||
| + | |||
|<small><2% of WBCs</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
| | |||
* <small>N/A</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Granulocytic [[hyperplasia]] with prominent [[dysplasia]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Granulocytic [[dysplasia]] is prominent</small> | |||
* <small>Absence of ''[[BCR/ABL|BCR-ABL]]'' or ''PDGFRA'', [[PDGFRB|''PDGFRB'',]] or ''[[FGFR1]]'' rearrangements</small> | |||
* <small>[[WBC]] > 13 × 10<sup>9</sup>/L</small> | |||
|- | |||
|<small>[[Juvenile myelomonocytic leukemia (patient information)|Juvenile myelomonocytic leukemia (]]JMML)</small><ref name="pmid9226148">{{cite journal |vauthors=Aricò M, Biondi A, Pui CH |title=Juvenile myelomonocytic leukemia |journal=Blood |volume=90 |issue=2 |pages=479–88 |date=July 1997 |pmid=9226148 |doi= |url=}}</ref><ref name="pmid80255132">{{cite journal |vauthors=Hasle H |title=Myelodysplastic syndromes in childhood--classification, epidemiology, and treatment |journal=Leuk. Lymphoma |volume=13 |issue=1-2 |pages=11–26 |date=March 1994 |pmid=8025513 |doi=10.3109/10428199409051647 |url=}}</ref> | |||
| | |||
* <small>[[Infections]]</small> | |||
* <small>[[Anemia]] related</small> | |||
| | |||
* <small>[[Hepatosplenomegaly]]</small> | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Rash]]</small> | |||
|<small>[[Leukocytosis|↑]]</small> | |||
|<small>↑</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
|<small>[[Monocytosis|↑]]</small> | |||
| | |||
* <small>↓ [[Serum]] [[Iron]]</small> | |||
* <small>↑ [[Vitamin B12|B12]] levels</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytopenia|↓]]</small> | |||
| | |||
* <small>Hypercelluar with ↑ [[myeloid cells]] in stages of maturation</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Polyclonal [[hypergammaglobulinemia]]</small> | |||
|- | |||
|<small>[[MDS]]/[[MPN]] with ring sideroblasts and [[thrombocytosis]] (MDS/MPN-RS-T)</small><ref name="pmid28188970">{{cite journal |vauthors=Patnaik MM, Tefferi A |title=Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis (RARS-T): 2017 update on diagnosis, risk-stratification, and management |journal=Am. J. Hematol. |volume=92 |issue=3 |pages=297–310 |date=March 2017 |pmid=28188970 |doi=10.1002/ajh.24637 |url=}}</ref><ref name="pmid30186759">{{cite journal |vauthors=Alshaban A, Padilla O, Philipovskiy A, Corral J, McAlice M, Gaur S |title=Lenalidomide induced durable remission in a patient with MDS/MPN-with ring sideroblasts and thrombocytosis with associated 5q- syndrome |journal=Leuk Res Rep |volume=10 |issue= |pages=37–40 |date=2018 |pmid=30186759 |doi=10.1016/j.lrr.2018.08.001 |url=}}</ref><ref name="pmid30524760">{{cite journal |vauthors=Bouchla A, Papageorgiou SG, Tsakiraki Z, Glezou E, Pavlidis G, Stavroulaki G, Bazani E, Foukas P, Pappa V |title=Plasmablastic Lymphoma in an Immunocompetent Patient with MDS/MPN with Ring Sideroblasts and Thrombocytosis-A Case Report |journal=Case Rep Hematol |volume=2018 |issue= |pages=2525070 |date=2018 |pmid=30524760 |pmc=6247723 |doi=10.1155/2018/2525070 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] related</small> | |||
* <small>[[Thrombosis]]</small> | |||
| | |||
* <small>Variable</small> | |||
|<small>NL or ↑</small> | |||
|<small>NL</small> | |||
| - | |||
|<small>NL</small> | |||
|<small>N/A</small> | |||
|<small>N/A</small> | |||
| | |||
* ↑ <small>[[Serum]] [[Iron]]</small> | |||
|<small>[[Anemia|↓]]</small> | |||
|<small>[[Thrombocytosis|↑]]</small> | |||
| | |||
* <small>Hypercellularity with [[dyserythropoiesis]] and increased [[megakaryocytes]]</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Large atypical [[megakaryocytes]]</small> | |||
* <small>Ringed [[sideroblasts]]</small> | |||
* <small>[[SF3B1]] [[mutation]]</small> | |||
|- | |||
| rowspan="3" |T-lymphoblastic leukemia/<br>lymphoma | |||
* | |||
* | |||
|<small>T-lymphoblastic leukemia/<br>lymphoma</small><ref name="pmid26276771">{{cite journal |vauthors=You MJ, Medeiros LJ, Hsi ED |title=T-lymphoblastic leukemia/lymphoma |journal=Am. J. Clin. Pathol. |volume=144 |issue=3 |pages=411–22 |date=September 2015 |pmid=26276771 |doi=10.1309/AJCPMF03LVSBLHPJ |url=}}</ref><ref name="pmid19284608">{{cite journal |vauthors=Patel KJ, Latif SU, de Calaca WM |title=An unusual presentation of precursor T cell lymphoblastic leukemia/lymphoma with cholestatic jaundice: case report |journal=J Hematol Oncol |volume=2 |issue= |pages=12 |date=March 2009 |pmid=19284608 |pmc=2663564 |doi=10.1186/1756-8722-2-12 |url=}}</ref><ref name="pmid24822133">{{cite journal |vauthors=Elreda L, Sandhu M, Sun X, Bekele W, Cohen AJ, Shah M |title=T-cell lymphoblastic leukemia/lymphoma: relapse 16 years after first remission |journal=Case Rep Hematol |volume=2014 |issue= |pages=359158 |date=2014 |pmid=24822133 |pmc=4005062 |doi=10.1155/2014/359158 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>>25% [[Blast|blasts]] ([[Leukemia]])</small> | |||
<small><25% [[Blast|blasts]] ([[Lymphoma]])</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
* <small>Positive for TdT</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Hypercelluarity with increased [[T cells]] precursors</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small><small>[[Flow cytometry]]</small> | |||
* <small>[[FISH]]</small> | |||
| | |||
* <small>May involve [[brain]], [[skin]], and [[testes]].</small> | |||
|- | |||
|<small>Provisional entity: Natural killer (NK) cell lymphoblastic leukemia/lymph</small><ref name="pmid28868017">{{cite journal |vauthors=Sedick Q, Alotaibi S, Alshieban S, Naheet KB, Elyamany G |title=Natural Killer Cell Lymphoblastic Leukaemia/Lymphoma: Case Report and Review of the Recent Literature |journal=Case Rep Oncol |volume=10 |issue=2 |pages=588–595 |date=2017 |pmid=28868017 |doi=10.1159/000477843 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>N/A</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[FISH]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Similar to [[T-cell]] lymphoblastic [[leukemia]] but may have more aggressive clinical course.</small> | |||
* <small>[[Diagnosis]] is usually based on presence of [[CD56]] expression, and [[T-cell]]-associated markers such as [[CD2]] and [[CD7]].</small> | |||
* <small>[[B cell|B-cell]] markers are absent.</small> | |||
|- | |||
|<small>Provisional entity: Early T-cell precursor lymphoblastic leukemia</small><ref name="pmid26747249">{{cite journal |vauthors=Jain N, Lamb AV, O'Brien S, Ravandi F, Konopleva M, Jabbour E, Zuo Z, Jorgensen J, Lin P, Pierce S, Thomas D, Rytting M, Borthakur G, Kadia T, Cortes J, Kantarjian HM, Khoury JD |title=Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype |journal=Blood |volume=127 |issue=15 |pages=1863–9 |date=April 2016 |pmid=26747249 |pmc=4915808 |doi=10.1182/blood-2015-08-661702 |url=}}</ref><ref name="pmid23695450">{{cite journal |vauthors=Haydu JE, Ferrando AA |title=Early T-cell precursor acute lymphoblastic leukaemia |journal=Curr. Opin. Hematol. |volume=20 |issue=4 |pages=369–73 |date=July 2013 |pmid=23695450 |pmc=3886681 |doi=10.1097/MOH.0b013e3283623c61 |url=}}</ref> | |||
| | |||
* <small>Constitutional</small> | |||
* <small>[[Anemia]] Related</small> | |||
* <small>[[Bleeding]]</small> | |||
* <small>[[Superior vena cava syndrome]]</small> | |||
| | |||
* <small>[[Lymphadenopathy]]</small> | |||
* <small>[[Mediastinal mass]]</small> | |||
* <small>[[Pleural effusions]]</small> | |||
* <small>[[Trachea|Tracheal]] obstruction</small> | |||
* <small>[[Pericardial effusions]]</small> | |||
|<small>↑</small> | |||
|<small>↑</small> | |||
|± | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
|<small>↑ or ↓</small> | |||
| | |||
* ↑ <small>[[LDH]]</small> | |||
|<small>↓</small> | |||
|<small>↓</small> | |||
| | |||
* <small>Hypercelluarity with increased [[T cells]] precursors</small> | |||
| | |||
* <small>[[Cytogenetic analysis]]</small> | |||
* <small>[[FISH]]</small> | |||
* <small>[[Flow cytometry]]</small> | |||
| | |||
* <small>Similar to [[T cell|T-cell]] lymphoblastic [[leukemia]] but is more aggressive clinically and cell are characterized by [[Flow cytometry|cytometry]] as [[CD1a]]<sup>−</sup>, [[CD8]]<sup>−</sup>, [[CD5]]<sup>−</sup> (dim), and positivity for 1 or more stem cell or [[myeloid]] [[antigens]].</small> | |||
* <small>[[Gene expression]] indicates more immature [[cells]] as compared to other subtypes of [[T cell|T-cell]] [[neoplasms]].</small> | |||
|} | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* The prevalence of blastic | * The prevalence of blastic natural killer cell lymphoma is unknown as it is an extremely rare disorder.<ref name="pmid25568744">{{cite journal| author=Saeed H, Awasthi M, Al-Qaisi A, Massarweh S| title=Blastic plasmacytoid dendritic cell neoplasm with extensive cutaneous and central nervous system involvement. | journal=Rare Tumors | year= 2014 | volume= 6 | issue= 4 | pages= 5474 | pmid=25568744 | doi=10.4081/rt.2014.5474 | pmc=PMC4274438 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25568744 }} </ref> | ||
===Age=== | ===Age=== | ||
*Blastic | *Blastic natural killer cell lymphoma is more commonly observed amongmiddle-aged or elderly patients. The mean age at diagnosis is 66 years.<ref name="HouJaworski2015">{{cite journal|last1=Hou|first1=Steve|last2=Jaworski|first2=Joseph|last3=Swami|first3=Vanlila|last4=Heintzelman|first4=Rebecca|last5=Cusack|first5=Carrie|last6=Chung|first6=Christina|last7=Peck|first7=Jeremy|last8=Fanelli|first8=Matthew|last9=Styler|first9=Michael|last10=Rizk|first10=Sanaa|title=Blastic plasmacytoid dendritic cell neoplasm with absolute monocytosis at presentation|journal=Pathology and Laboratory Medicine International|year=2015|pages=7|issn=1179-2698|doi=10.2147/PLMI.S71492}}</ref> | ||
===Gender=== | ===Gender=== | ||
*Males are more commonly affected with blastic | *Males are more commonly affected with blastic natural killer cell lymphoma than females. | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The majority of patients with | *The majority of patients with blastic natural killer cell lymphoma have an aggressive clinical course. | ||
*Prognosis is generally poor, and the | *[[Prognosis]] is generally poor, and the median survival rate is 15 months.<ref name="pmid15981806">{{cite journal| author=Petrella T, Bagot M, Willemze R, Beylot-Barry M, Vergier B, Delaunay M et al.| title=Blastic NK-cell lymphomas (agranular CD4+CD56+ hematodermic neoplasms): a review. | journal=Am J Clin Pathol | year= 2005 | volume= 123 | issue= 5 | pages= 662-75 | pmid=15981806 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15981806 }} </ref> | ||
==Diagnosis== | ==Diagnosis== | ||
=== Symptoms === | === Symptoms === | ||
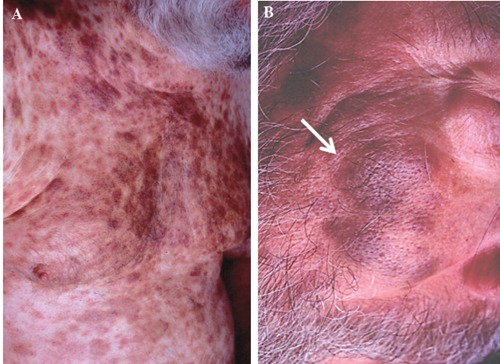
*Symptoms of blastic | *Symptoms of blastic natural killer cell lymphoma may include: | ||
:*Nodules, plaques and patches of variable sizes on skin | :*Nodules, plaques and patches of variable sizes on [[skin]] | ||
=== Physical Examination === | === Physical Examination === | ||
*Physical examination may be remarkable for: | *Physical examination may be remarkable for: | ||
:*Nodules, plaques and patches of variable sizes on skin | :*Nodules, plaques and patches of variable sizes on [[skin]] | ||
[[File:Rt-2014-4-5474-g001.jpg|thumb|center|500px|A plaque-like pigmented bruised rash over the patient’s trunk (A) and face (B)<ref name="pmid25568744">{{cite journal| author=Saeed H, Awasthi M, Al-Qaisi A, Massarweh S| title=Blastic plasmacytoid dendritic cell neoplasm with extensive cutaneous and central nervous system involvement. | journal=Rare Tumors | year= 2014 | volume= 6 | issue= 4 | pages= 5474 | pmid=25568744 | doi=10.4081/rt.2014.5474 | pmc=PMC4274438 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25568744 }} </ref>]] | [[File:Rt-2014-4-5474-g001.jpg|thumb|center|500px|A plaque-like pigmented bruised rash over the patient’s trunk (A) and face (B)<ref name="pmid25568744">{{cite journal| author=Saeed H, Awasthi M, Al-Qaisi A, Massarweh S| title=Blastic plasmacytoid dendritic cell neoplasm with extensive cutaneous and central nervous system involvement. | journal=Rare Tumors | year= 2014 | volume= 6 | issue= 4 | pages= 5474 | pmid=25568744 | doi=10.4081/rt.2014.5474 | pmc=PMC4274438 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25568744 }} </ref>]] | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*There are no specific laboratory findings associated with blastic | *There are no specific laboratory findings associated with blastic natural killer cell lymphoma. | ||
===Imaging Findings=== | ===Imaging Findings=== | ||
*There are no imaging study findings associated with blastic | *There are no imaging study findings associated with blastic natural killer cell lymphoma | ||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*Blastic | *Blastic natural killer cell lymphoma may also be diagnosed using [[immunochemistry]]. | ||
* Immunohistochemical staining is positive for r CD4 and CD56, with variable positivity for CD43, TdT, and CD68. | |||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*The mainstay of therapy for blastic NK cell lymphoma is chemotherapy with CHOP or COP-like regimens. | *The mainstay of therapy for blastic NK cell lymphoma is chemotherapy with CHOP or COP-like regimens. | ||
*[[Immunomodulation]] or immunotherapy with IL-3 or with antiCD123 antibody is also being considered for chemotherapy-resistant patients. | |||
=== Prevention === | === Prevention === | ||
*There are no primary preventive measures available for blastic | *There are no primary preventive measures available for blastic natural killer cell lymphoma. | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 63: | Line 854: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Hematology]] | |||
[[Category:Immunology]] | |||
Latest revision as of 18:35, 8 May 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Agranular CD4+CD56+ hematodermic neoplasm; CD4+CD56+ hematodermic neoplasm; HDT; Blastic plasmacytoid dendritic cell neoplasm; BPDCN; Blastic natural killer cell lymphoma
Overview
Blastic natural killer cell lymphoma was first discovered by Adachi, an American hematologist, in 1994 following an unusual presentation of cutaneous lymphoma that express CD4 and CD56 antigens but no other T cell and B cell antigens. The deletion in 5q has been associated with the development of blastic natural killer cell lymphoma. Blastic natural killer cell lymphoma must be differentiated from other malignancies such as acute myeloid leukemia, human T-cell lymphotropic virus 1 associated adult T-cell leukemia/lymphoma, cutaneous NK/T-cell lymphoma, primary and secondary cutaneous pleomorphic T-cell lymphomas, undifferentiated carcinoma, and malignant melanoma. Blastic NK cell lymphoma is more commonly observed among middle-aged or elderly patients. The mean age at diagnosis is 66 years.[1]Males are more commonly affected with blastic natural killer cell lymphoma than females. Prognosis is generally poor, and the median survival rate is 15 months. Symptoms of blastic natural killer cell lymphoma may include nodules, plaques and patches of variable sizes on skin. Immunohistochemical staining is positive for r CD4 and CD56, with variable positivity for CD43, TdT, and CD68. The mainstay of therapy for blastic natural killer cell lymphoma is chemotherapy with CHOP or COP-like regimens.
Historical Perspective
- Blastic natural killer cell lymphoma was first discovered by Adachi, an American hematologist, in 1994 following an unusual presentation of cutaneous lymphoma that express CD4 and CD56 antigens but no other T cell and B cell antigens.[2]
- Chaperot et al demonstrated that predendritic cells (plasmacytoid monocytes) and CD4/CD56 leukemic cells are similar in the production of alpha-interferon in response to influenza virus stimulation, which on maturation with interleukin 3 (IL-3) become powerful inducers for CD4 proliferation and Th-2 polarization. .[3]
- Petrella and Karube demonstrated that CD123, which is a marker of predendritic cells, are expressed on the tumor cells in blastic natural killer cell lymphoma and proposed an oncogenic transformation of NCAM-expressing plasmacytoid monocyte-like cells as cell of origin in CD4/CD56 blastic natural killer cell lymphoma.[4][5]
Pathophysiology
- Blastic natural killer cell lymphoma is a type of lymphoma. It does not appear to be associated with Epstein Barr virus (EBV) .[6]
- Blastic natural killer cell lymphoma is derived from plasmacytoid type 2 dendritic cell precursors. These dendritic cell precursors are possibly related to a common myeloid/NK-cell precursor cell.[7]
- Blastic natural killer cell lymphoma is currently classified by World Health Organization (WHO) Classification of Tumors of Hematopoietic and Lymphoid Tissues as an aggressive neoplasm derived from the precursors of plasmacytoid dendritic cells and categorically placed under the heading “Acute myeloid leukemia (AML) and related precursor neoplasms.”
- The deletion in 5q has been associated with the development of blastic natural killer cell lymphoma.
- Other genetic abnormalities associated with blastic natural killer cell lymphoma are deletion of 12p, abnormalities of chromosome 13, deletion of 6q, and loss of chromosomes 15 and 9.
- On hematoxylin and eosin (H&E) staining, fine chromatin and scanty cytoplasm resembling lymphoblasts, or in some cases, myeloblasts, and may on occasion exhibit sub-membranous cytoplasmic vacuolations surrounding the nucleus are characteristic findings of blastic natural killer cell lymphoma.
- Tumor cells are invariably CD4+ and CD56+, and usually HLA-DR and CD45RA are positive as well.
- CD2 and CD34 are usually negative; and expression of TdT, CD7 and cytoplasmic CD3 is variable.[8]
-
Hematoxylin & Eosin stain of skin lesion biopsy. Low power view of leukemic infiltrate corresponding to the raised plaque (A, black arrows) and high power view of the malignant cells in the skin infiltrate
-
Large malignant-appearing cells, with agranular cytoplasm, cleaved nuclei and prominent neocleoli on peripheral blood smear using Wright stain (A) and similar blast cells present in cerebrospinal fluid
Differentiating Blastic NK cell Lymphoma from other Diseases
ABBREVIATIONS
N/A: Not available, NL: Normal, FISH: Fluorescence in situ hybridization, PCR: Polymerase chain reaction, LDH: Lactate dehydrogenase, PUD: Peptic ulcer disease, EPO: Erythropoietin, LFTs: Liver function tests, RFTs: Renal function tests, LAP: Leukocyte alkaline phosphatase, LAD: Leukocyte alkaline dehydrgenase, WBCs: White blood cells.
| Myeloproliferative neoplasms (MPN) | Clinical manifestations | Diagnosis | Other features | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | CBC & Peripheral smear | Bone marrow biopsy | Other investigations | |||||||||||
| WBCs | Hb | Plat- elets | |||||||||||||
| Leuko-cytes | Blasts | Left shift |
Baso- phils |
Eosino- phils |
Mono- cytes |
Others | |||||||||
| Chronic myeloid leukemia (CML), BCR-ABL1+[9][10] |
|
|
↑ | <2% | + | ↑ | ↑ | ↑ | N/A | ↓ | NL |
|
|
| |
| Chronic neutrophilic leukemia (CNL)[11][12][13] |
|
↑ | Minimal | + | NL | NL | NL | ↓ | ↓ |
|
|
| |||
| Polycythemia vera (PV)[14][15][16][17] |
|
|
NL or ↑ | None | - | ↑ or ↓ | NL or ↑ | NL | ↑↑ | NL |
|
| |||
| Primary myelofibrosis (PMF)[18][19][20][21] |
|
↓ | Erythroblasts | - | Absent | NL | NL | ↓ | ↓ |
|
| ||||
| Essential thrombocythemia (ET)[22][23][24] |
|
NL or ↑ |
None |
- |
↓ or absent |
NL |
NL |
|
↑↑ |
|
|||||
| Chronic eosinophilic leukemia, not otherwise specified (NOS)[25][26][27][28] |
|
↑ | Present | + | ↑ | ↑↑ | ↑ | ↓ | ↓ |
|
|
||||
| MPN, unclassifiable |
|
|
↑ | Variable | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↑ |
|
|
| |
| Mastocytosis[29][30][31][32] |
|
↑ | None | - | NL | ↑ | NL | ↓ | ↓ or ↑ |
|
| ||||
| Myeloid/lymphoid neoplasms with eosinophilia and rearrangement of PDGFRA, PDGFRB, or FGFR1, or with PCM1-JAK2[33][34][35][36] |
|
↑ | NL | - | NL | ↑ | ↑ |
|
NL | ↓ |
|
|
| ||
| B-lymphoblastic leukemia/lymphoma[37][38] | NL or ↑ | >25% | N/A | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ | ↓ | ↓ |
|
| |||||
| Myelodysplastic syndromes (MDS)[39][40] |
↓ | Variable | - | ↓ | ↓ | ↓ |
|
↓ | ↓ |
|
| ||||
| Acute myeloid leukemia (AML) and related neoplasms[41][42] |
|
|
NL or ↑ | ↑ | N/A | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
with dysplasia |
| ||
| Blastic plasmacytoid dendritic cell neoplasm[43][44][45][46] |
|
|
NL | ↑ | NL | NL | NL | ↓ | ↓ |
|
| ||||
| Myelodysplastic /myeloproliferative neoplasms (MDS/MPN) |
Chronic myelomonocytic leukemia (CMML)[47] |
|
↑ | < 20% | NL | ↑ | ↑↑ |
|
↓ | ↓ |
|
| |||
| Atypical chronic myeloid leukemia (aCML), BCR-ABL1-[50][51] |
|
|
↑ | <20% | + | <2% of WBCs | N/A | N/A |
|
↓ | ↓ |
|
|||
| Juvenile myelomonocytic leukemia (JMML)[52][53] |
|
↑ | ↑ | N/A | N/A | N/A | ↑ | ↓ | ↓ |
|
| ||||
| MDS/MPN with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T)[54][55][56] |
|
|
NL or ↑ | NL | - | NL | N/A | N/A | ↓ | ↑ |
|
| |||
| T-lymphoblastic leukemia/ lymphoma |
T-lymphoblastic leukemia/ lymphoma[57][58][59] |
|
↑ | >25% blasts (Leukemia) | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
|||
| Provisional entity: Natural killer (NK) cell lymphoblastic leukemia/lymph[60] |
|
↑ | ↑ | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
||||
| Provisional entity: Early T-cell precursor lymphoblastic leukemia[61][62] |
|
↑ | ↑ | ± | ↑ or ↓ | ↑ or ↓ | ↑ or ↓ |
|
↓ | ↓ |
|
||||
Epidemiology and Demographics
- The prevalence of blastic natural killer cell lymphoma is unknown as it is an extremely rare disorder.[63]
Age
- Blastic natural killer cell lymphoma is more commonly observed amongmiddle-aged or elderly patients. The mean age at diagnosis is 66 years.[1]
Gender
- Males are more commonly affected with blastic natural killer cell lymphoma than females.
Natural History, Complications and Prognosis
- The majority of patients with blastic natural killer cell lymphoma have an aggressive clinical course.
- Prognosis is generally poor, and the median survival rate is 15 months.[8]
Diagnosis
Symptoms
- Symptoms of blastic natural killer cell lymphoma may include:
- Nodules, plaques and patches of variable sizes on skin
Physical Examination
- Physical examination may be remarkable for:
- Nodules, plaques and patches of variable sizes on skin
Laboratory Findings
- There are no specific laboratory findings associated with blastic natural killer cell lymphoma.
Imaging Findings
- There are no imaging study findings associated with blastic natural killer cell lymphoma
Other Diagnostic Studies
- Blastic natural killer cell lymphoma may also be diagnosed using immunochemistry.
- Immunohistochemical staining is positive for r CD4 and CD56, with variable positivity for CD43, TdT, and CD68.
Treatment
Medical Therapy
- The mainstay of therapy for blastic NK cell lymphoma is chemotherapy with CHOP or COP-like regimens.
- Immunomodulation or immunotherapy with IL-3 or with antiCD123 antibody is also being considered for chemotherapy-resistant patients.
Prevention
- There are no primary preventive measures available for blastic natural killer cell lymphoma.
References
- ↑ 1.0 1.1 Hou, Steve; Jaworski, Joseph; Swami, Vanlila; Heintzelman, Rebecca; Cusack, Carrie; Chung, Christina; Peck, Jeremy; Fanelli, Matthew; Styler, Michael; Rizk, Sanaa (2015). "Blastic plasmacytoid dendritic cell neoplasm with absolute monocytosis at presentation". Pathology and Laboratory Medicine International: 7. doi:10.2147/PLMI.S71492. ISSN 1179-2698.
- ↑ Adachi M, Maeda K, Takekawa M, Hinoda Y, Imai K, Sugiyama S; et al. (1994). "High expression of CD56 (N-CAM) in a patient with cutaneous CD4-positive lymphoma". Am J Hematol. 47 (4): 278–82. PMID 7526680.
- ↑ Chaperot L, Bendriss N, Manches O, Gressin R, Maynadie M, Trimoreau F; et al. (2001). "Identification of a leukemic counterpart of the plasmacytoid dendritic cells". Blood. 97 (10): 3210–7. PMID 11342451.
- ↑ Petrella T, Meijer CJ, Dalac S, Willemze R, Maynadié M, Machet L; et al. (2004). "TCL1 and CLA expression in agranular CD4/CD56 hematodermic neoplasms (blastic NK-cell lymphomas) and leukemia cutis". Am J Clin Pathol. 122 (2): 307–13. doi:10.1309/0QPP-AVTU-PCV9-UCLV. PMID 15323148.
- ↑ Karube K, Ohshima K, Tsuchiya T, Yamaguchi T, Suefuji H, Suzumiya J; et al. (2003). "Non-B, non-T neoplasms with lymphoblast morphology: further clarification and classification". Am J Surg Pathol. 27 (10): 1366–74. PMID 14508398.
- ↑ Chan JK, Sin VC, Wong KF; et al. (1997). "Nonnasal lymphoma expressing the natural killer cell marker CD56: a clinicopathologic study of 49 cases of an uncommon aggressive neoplasm". Blood. 89 (12): 4501–13. PMID 9192774. Unknown parameter
|month=ignored (help) - ↑ Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH; et al. (2005). "WHO-EORTC classification for cutaneous lymphomas". Blood. 105 (10): 3768–85. doi:10.1182/blood-2004-09-3502. PMID 15692063.
- ↑ 8.0 8.1 Petrella T, Bagot M, Willemze R, Beylot-Barry M, Vergier B, Delaunay M; et al. (2005). "Blastic NK-cell lymphomas (agranular CD4+CD56+ hematodermic neoplasms): a review". Am J Clin Pathol. 123 (5): 662–75. PMID 15981806.
- ↑ Savage DG, Szydlo RM, Goldman JM (January 1997). "Clinical features at diagnosis in 430 patients with chronic myeloid leukaemia seen at a referral centre over a 16-year period". Br. J. Haematol. 96 (1): 111–6. PMID 9012696.
- ↑ Thompson PA, Kantarjian HM, Cortes JE (October 2015). "Diagnosis and Treatment of Chronic Myeloid Leukemia in 2015". Mayo Clin. Proc. 90 (10): 1440–54. doi:10.1016/j.mayocp.2015.08.010. PMC 5656269. PMID 26434969.
- ↑ Szuber N, Tefferi A (February 2018). "Chronic neutrophilic leukemia: new science and new diagnostic criteria". Blood Cancer J. 8 (2): 19. doi:10.1038/s41408-018-0049-8. PMC 5811432. PMID 29440636.
- ↑ Maxson JE, Tyner JW (February 2017). "Genomics of chronic neutrophilic leukemia". Blood. 129 (6): 715–722. doi:10.1182/blood-2016-10-695981. PMC 5301820. PMID 28028025.
- ↑ Menezes J, Cigudosa JC (2015). "Chronic neutrophilic leukemia: a clinical perspective". Onco Targets Ther. 8: 2383–90. doi:10.2147/OTT.S49688. PMC 4562747. PMID 26366092.
- ↑ Vannucchi AM, Guglielmelli P, Tefferi A (March 2018). "Polycythemia vera and essential thrombocythemia: algorithmic approach". Curr. Opin. Hematol. 25 (2): 112–119. doi:10.1097/MOH.0000000000000402. PMID 29194068.
- ↑ Pillai AA, Babiker HM. PMID 30252337. Missing or empty
|title=(help) - ↑ Tefferi A, Barbui T (January 2019). "Polycythemia vera and essential thrombocythemia: 2019 update on diagnosis, risk-stratification and management". Am. J. Hematol. 94 (1): 133–143. doi:10.1002/ajh.25303. PMID 30281843.
- ↑ Rumi E, Cazzola M (February 2017). "Diagnosis, risk stratification, and response evaluation in classical myeloproliferative neoplasms". Blood. 129 (6): 680–692. doi:10.1182/blood-2016-10-695957. PMC 5335805. PMID 28028026.
- ↑ Cervantes F, Correa JG, Hernandez-Boluda JC (May 2016). "Alleviating anemia and thrombocytopenia in myelofibrosis patients". Expert Rev Hematol. 9 (5): 489–96. doi:10.1586/17474086.2016.1154452. PMID 26891375.
- ↑ Hoffman, Ronald (2018). Hematology : basic principles and practice. Philadelphia, PA: Elsevier. ISBN 9780323357623.
- ↑ Michiels JJ, Bernema Z, Van Bockstaele D, De Raeve H, Schroyens W (March 2007). "Current diagnostic criteria for the chronic myeloproliferative disorders (MPD) essential thrombocythemia (ET), polycythemia vera (PV) and chronic idiopathic myelofibrosis (CIMF)". Pathol. Biol. 55 (2): 92–104. doi:10.1016/j.patbio.2006.06.002. PMID 16919893.
- ↑ Hoffman, Ronald (2018). Hematology : basic principles and practice. Philadelphia, PA: Elsevier. ISBN 9780323357623.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID http://dx.doi.org/10.1182/blood-2007-04-083501 Check
|pmid=value (help). - ↑ Daniel A. Arber, Attilio Orazi, Robert Hasserjian, Jurgen Thiele, Michael J. Borowitz, Michelle M. Le Beau, Clara D. Bloomfield, Mario Cazzola & James W. Vardiman (2016). "The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia". Blood. 127 (20): 2391–2405. doi:10.1182/blood-2016-03-643544. PMID 27069254. Unknown parameter
|month=ignored (help) - ↑ A. Tefferi, R. Fonseca, D. L. Pereira & H. C. Hoagland (2001). "A long-term retrospective study of young women with essential thrombocythemia". Mayo Clinic proceedings. 76 (1): 22–28. doi:10.4065/76.1.22. PMID 11155408. Unknown parameter
|month=ignored (help) - ↑ Vidyadharan S, Joseph B, Nair SP (2016). "Chronic Eosinophilic Leukemia Presenting Predominantly with Cutaneous Manifestations". Indian J Dermatol. 61 (4): 437–9. doi:10.4103/0019-5154.185716. PMC 4966405. PMID 27512192.
- ↑ Hofmans M, Delie A, Vandepoele K, Van Roy N, Van der Meulen J, Philippé J, Moors I (2018). "A case of chronic eosinophilic leukemia with secondary transformation to acute myeloid leukemia". Leuk Res Rep. 9: 45–47. doi:10.1016/j.lrr.2018.04.001. PMC 5993353. PMID 29892549.
- ↑ Yamada Y, Rothenberg ME, Cancelas JA (2006). "Current concepts on the pathogenesis of the hypereosinophilic syndrome/chronic eosinophilic leukemia". Transl Oncogenomics. 1: 53–63. PMC 3642145. PMID 23662039.
- ↑ Kim TH, Gu HJ, Lee WI, Lee J, Yoon HJ, Park TS (September 2016). "Chronic eosinophilic leukemia with FIP1L1-PDGFRA rearrangement". Blood Res. 51 (3): 204–206. doi:10.5045/br.2016.51.3.204. PMID 27722133.
- ↑ Carter MC, Metcalfe DD, Komarow HD (February 2014). "Mastocytosis". Immunol Allergy Clin North Am. 34 (1): 181–96. doi:10.1016/j.iac.2013.09.001. PMC 3863935. PMID 24262698.
- ↑ Macri A, Cook C. PMID 29494109. Missing or empty
|title=(help) - ↑ Lladó AC, Mihon CE, Silva M, Galzerano A (2014). "Systemic mastocytosis - a diagnostic challenge". Rev Bras Hematol Hemoter. 36 (3): 226–9. doi:10.1016/j.bjhh.2014.03.003. PMC 4109736. PMID 25031064.
- ↑ Valent P, Akin C, Metcalfe DD (March 2017). "Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts". Blood. 129 (11): 1420–1427. doi:10.1182/blood-2016-09-731893. PMC 5356454. PMID 28031180.
- ↑ Kumar, Kirthi R.; Chen, Weina; Koduru, Prasad R.; Luu, Hung S. (2015). "Myeloid and Lymphoid Neoplasm With Abnormalities of FGFR1 Presenting With Trilineage Blasts and RUNX1 Rearrangement". American Journal of Clinical Pathology. 143 (5): 738–748. doi:10.1309/AJCPUD6W1JLQQMNA. ISSN 1943-7722.
- ↑ Paolo Strati, Guilin Tang, Dzifa Y. Duose, Saradhi Mallampati, Rajyalakshmi Luthra, Keyur P. Patel, Mohammad Hussaini, Abu-Sayeef Mirza, Rami S. Komrokji, Stephen Oh, John Mascarenhas, Vesna Najfeld, Vivek Subbiah, Hagop Kantarjian, Guillermo Garcia-Manero, Srdan Verstovsek & Naval Daver (2018). "Myeloid/lymphoid neoplasms with FGFR1 rearrangement". Leukemia & lymphoma. 59 (7): 1672–1676. doi:10.1080/10428194.2017.1397663. PMID 29119847. Unknown parameter
|month=ignored (help) - ↑ Ximena Montenegro-Garreaud, Roberto N. Miranda, Alexandra Reynolds, Guilin Tang, Sa A. Wang, Mariko Yabe, Wei Wang, Lianghua Fang, Carlos E. Bueso-Ramos, Pei Lin, L. Jeffrey Medeiros & Xinyan Lu (2017). "Myeloproliferative neoplasms with t(8;22)(p11.2;q11.2)/BCR-FGFR1: a meta-analysis of 20 cases shows cytogenetic progression with B-lymphoid blast phase". Human pathology. 65: 147–156. doi:10.1016/j.humpath.2017.05.008. PMID 28551329. Unknown parameter
|month=ignored (help) - ↑ Paola Villafuerte-Gutierrez, Montserrat Lopez Rubio, Pilar Herrera & Eva Arranz (2018). "A Case of Myeloproliferative Neoplasm with BCR-FGFR1 Rearrangement: Favorable Outcome after Haploidentical Allogeneic Transplantation". Case reports in hematology. 2018: 5724960. doi:10.1155/2018/5724960. PMID 30647980.
- ↑ Kamiya-Matsuoka C, Garciarena P, Amin HM, Tremont-Lukats IW, de Groot JF (December 2013). "B lymphoblastic leukemia/lymphoma presenting as seventh cranial nerve palsy". Neurol Clin Pract. 3 (6): 532–534. doi:10.1212/CPJ.0b013e3182a78ef0. PMC 6082360. PMID 30107017.
- ↑ Zhang X, Rastogi P, Shah B, Zhang L (September 2017). "B lymphoblastic leukemia/lymphoma: new insights into genetics, molecular aberrations, subclassification and targeted therapy". Oncotarget. 8 (39): 66728–66741. doi:10.18632/oncotarget.19271. PMC 5630450. PMID 29029550.
- ↑ Germing U, Kobbe G, Haas R, Gattermann N (November 2013). "Myelodysplastic syndromes: diagnosis, prognosis, and treatment". Dtsch Arztebl Int. 110 (46): 783–90. doi:10.3238/arztebl.2013.0783. PMC 3855821. PMID 24300826.
- ↑ Gangat N, Patnaik MM, Tefferi A (January 2016). "Myelodysplastic syndromes: Contemporary review and how we treat". Am. J. Hematol. 91 (1): 76–89. doi:10.1002/ajh.24253. PMID 26769228.
- ↑ Islam A, Catovsky D, Goldman JM, Galton DA (September 1985). "Bone marrow biopsy changes in acute myeloid leukaemia. I: Observations before chemotherapy". Histopathology. 9 (9): 939–57. PMID 3864727.
- ↑ Orazi A (2007). "Histopathology in the diagnosis and classification of acute myeloid leukemia, myelodysplastic syndromes, and myelodysplastic/myeloproliferative diseases". Pathobiology. 74 (2): 97–114. doi:10.1159/000101709. PMID 17587881.
- ↑ F. Julia, T. Petrella, M. Beylot-Barry, M. Bagot, D. Lipsker, L. Machet, P. Joly, O. Dereure, M. Wetterwald, M. d'Incan, F. Grange, J. Cornillon, G. Tertian, E. Maubec, P. Saiag, S. Barete, I. Templier, F. Aubin & S. Dalle (2013). "Blastic plasmacytoid dendritic cell neoplasm: clinical features in 90 patients". The British journal of dermatology. 169 (3): 579–586. doi:10.1111/bjd.12412. PMID 23646868. Unknown parameter
|month=ignored (help) - ↑ Livio Pagano, Caterina Giovanna Valentini, Alessandro Pulsoni, Simona Fisogni, Paola Carluccio, Francesco Mannelli, Monia Lunghi, Gianmatteo Pica, Francesco Onida, Chiara Cattaneo, Pier Paolo Piccaluga, Eros Di Bona, Elisabetta Todisco, Pellegrino Musto, Antonio Spadea, Alfonso D'Arco, Stefano Pileri, Giuseppe Leone, Sergio Amadori & Fabio Facchetti (2013). "Blastic plasmacytoid dendritic cell neoplasm with leukemic presentation: an Italian multicenter study". Haematologica. 98 (2): 239–246. doi:10.3324/haematol.2012.072645. PMID 23065521. Unknown parameter
|month=ignored (help) - ↑ Joseph D. Khoury (2018). "Blastic Plasmacytoid Dendritic Cell Neoplasm". Current hematologic malignancy reports. 13 (6): 477–483. doi:10.1007/s11899-018-0489-z. PMID 30350260. Unknown parameter
|month=ignored (help) - ↑ Shinichiro Sukegawa, Mamiko Sakata-Yanagimoto, Ryota Matsuoka, Haruka Momose, Yusuke Kiyoki, Masayuki Noguchi, Naoya Nakamura, Rei Watanabe, Manabu Fujimoto, Yasuhisa Yokoyama, Hidekazu Nishikii, Takayasu Kato, Manabu Kusakabe, Naoki Kurita, Naoshi Obara, Yuichi Hasegawa & Shigeru Chiba (2018). "[Blastic plasmacytoid dendritic cell neoplasm accompanied by chronic myelomonocytic leukemia successfully treated with azacitidine]". [[[Rinsho ketsueki] The Japanese journal of clinical hematology]]. 59 (12): 2567–2573. doi:10.11406/rinketsu.59.2567. PMID 30626790.
- ↑ Patnaik MM, Tefferi A (June 2016). "Chronic myelomonocytic leukemia: 2016 update on diagnosis, risk stratification, and management". Am. J. Hematol. 91 (6): 631–42. doi:10.1002/ajh.24396. PMID 27185207.
- ↑ Parikh SA, Tefferi A (June 2012). "Chronic myelomonocytic leukemia: 2012 update on diagnosis, risk stratification, and management". Am. J. Hematol. 87 (6): 610–9. doi:10.1002/ajh.23203. PMID 22615103.
- ↑ Benton CB, Nazha A, Pemmaraju N, Garcia-Manero G (August 2015). "Chronic myelomonocytic leukemia: Forefront of the field in 2015". Crit. Rev. Oncol. Hematol. 95 (2): 222–42. doi:10.1016/j.critrevonc.2015.03.002. PMC 4859155. PMID 25869097.
- ↑ Dao KH, Tyner JW (2015). "What's different about atypical CML and chronic neutrophilic leukemia?". Hematology Am Soc Hematol Educ Program. 2015: 264–71. doi:10.1182/asheducation-2015.1.264. PMC 5266507. PMID 26637732.
- ↑ Muramatsu H, Makishima H, Maciejewski JP (February 2012). "Chronic myelomonocytic leukemia and atypical chronic myeloid leukemia: novel pathogenetic lesions". Semin. Oncol. 39 (1): 67–73. doi:10.1053/j.seminoncol.2011.11.004. PMC 3523950. PMID 22289493.
- ↑ Aricò M, Biondi A, Pui CH (July 1997). "Juvenile myelomonocytic leukemia". Blood. 90 (2): 479–88. PMID 9226148.
- ↑ Hasle H (March 1994). "Myelodysplastic syndromes in childhood--classification, epidemiology, and treatment". Leuk. Lymphoma. 13 (1–2): 11–26. doi:10.3109/10428199409051647. PMID 8025513.
- ↑ Patnaik MM, Tefferi A (March 2017). "Refractory anemia with ring sideroblasts (RARS) and RARS with thrombocytosis (RARS-T): 2017 update on diagnosis, risk-stratification, and management". Am. J. Hematol. 92 (3): 297–310. doi:10.1002/ajh.24637. PMID 28188970.
- ↑ Alshaban A, Padilla O, Philipovskiy A, Corral J, McAlice M, Gaur S (2018). "Lenalidomide induced durable remission in a patient with MDS/MPN-with ring sideroblasts and thrombocytosis with associated 5q- syndrome". Leuk Res Rep. 10: 37–40. doi:10.1016/j.lrr.2018.08.001. PMID 30186759.
- ↑ Bouchla A, Papageorgiou SG, Tsakiraki Z, Glezou E, Pavlidis G, Stavroulaki G, Bazani E, Foukas P, Pappa V (2018). "Plasmablastic Lymphoma in an Immunocompetent Patient with MDS/MPN with Ring Sideroblasts and Thrombocytosis-A Case Report". Case Rep Hematol. 2018: 2525070. doi:10.1155/2018/2525070. PMC 6247723. PMID 30524760.
- ↑ You MJ, Medeiros LJ, Hsi ED (September 2015). "T-lymphoblastic leukemia/lymphoma". Am. J. Clin. Pathol. 144 (3): 411–22. doi:10.1309/AJCPMF03LVSBLHPJ. PMID 26276771.
- ↑ Patel KJ, Latif SU, de Calaca WM (March 2009). "An unusual presentation of precursor T cell lymphoblastic leukemia/lymphoma with cholestatic jaundice: case report". J Hematol Oncol. 2: 12. doi:10.1186/1756-8722-2-12. PMC 2663564. PMID 19284608.
- ↑ Elreda L, Sandhu M, Sun X, Bekele W, Cohen AJ, Shah M (2014). "T-cell lymphoblastic leukemia/lymphoma: relapse 16 years after first remission". Case Rep Hematol. 2014: 359158. doi:10.1155/2014/359158. PMC 4005062. PMID 24822133.
- ↑ Sedick Q, Alotaibi S, Alshieban S, Naheet KB, Elyamany G (2017). "Natural Killer Cell Lymphoblastic Leukaemia/Lymphoma: Case Report and Review of the Recent Literature". Case Rep Oncol. 10 (2): 588–595. doi:10.1159/000477843. PMID 28868017.
- ↑ Jain N, Lamb AV, O'Brien S, Ravandi F, Konopleva M, Jabbour E, Zuo Z, Jorgensen J, Lin P, Pierce S, Thomas D, Rytting M, Borthakur G, Kadia T, Cortes J, Kantarjian HM, Khoury JD (April 2016). "Early T-cell precursor acute lymphoblastic leukemia/lymphoma (ETP-ALL/LBL) in adolescents and adults: a high-risk subtype". Blood. 127 (15): 1863–9. doi:10.1182/blood-2015-08-661702. PMC 4915808. PMID 26747249.
- ↑ Haydu JE, Ferrando AA (July 2013). "Early T-cell precursor acute lymphoblastic leukaemia". Curr. Opin. Hematol. 20 (4): 369–73. doi:10.1097/MOH.0b013e3283623c61. PMC 3886681. PMID 23695450.
- ↑ 63.0 63.1 Saeed H, Awasthi M, Al-Qaisi A, Massarweh S (2014). "Blastic plasmacytoid dendritic cell neoplasm with extensive cutaneous and central nervous system involvement". Rare Tumors. 6 (4): 5474. doi:10.4081/rt.2014.5474. PMC 4274438. PMID 25568744.