Palpitations resident survival guide: Difference between revisions
Sergekorjian (talk | contribs) |
Sergekorjian (talk | contribs) (→Do's) |
||
| (50 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
<div style="width: 80%;"> | <div style="width: 80%;"> | ||
{| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0"; | {| class="infobox" style="margin: 0 0 0 0; border: 0; float: right; width: 100px; background: #A8A8A8; position: fixed; top: 250px; right: 21px; border-radius: 0 0 10px 10px;" cellpadding="0" cellspacing="0" ; | ||
|- | |- | ||
! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align=center| {{fontcolor|#2B3B44|Palpitations Resident Survival Guide Microchapters}} | ! style="padding: 0 5px; font-size: 85%; background: #A8A8A8" align="center" | {{fontcolor|#2B3B44|Palpitations Resident Survival Guide Microchapters}} | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Overview|Overview]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Overview|Overview]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Causes|Causes]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Causes|Causes]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#FIRE: Focused Initial Rapid Evaluation|FIRE]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Complete Diagnostic Approach|Diagnosis]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Complete Diagnostic Approach|Diagnosis]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Treatment|Treatment]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Treatment|Treatment]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#Do's|Do's]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#Do's|Do's]] | ||
|- | |- | ||
! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align=left | [[Palpitations resident survival guide#EKG gallery|Gallery]] | ! style="font-size: 80%; padding: 0 5px; background: #DCDCDC" align="left" | [[Palpitations resident survival guide#EKG gallery|Gallery]] | ||
|} | |} | ||
| Line 81: | Line 81: | ||
❑ [[Hypotension]] or shock <br>(suggestive of [[VT]])<br> | ❑ [[Hypotension]] or shock <br>(suggestive of [[VT]])<br> | ||
❑ [[Chest pain]] <br>(suggestive of [[ischemia]], complete AV block)<br> | ❑ [[Chest pain]] <br>(suggestive of [[ischemia]], complete AV block)<br> | ||
❑ [[Shortness of breath]] <br>(suggestive of cardiac tamponade, complete AV block)</div>}} | ❑ [[Shortness of breath]] <br>(suggestive of PE, cardiac tamponade, complete AV block)</div>}} | ||
{{familytree | | | | | | | | | | |,|-|-|^|-|-|.| | |}} | {{familytree | | | | | | | | | | |,|-|-|^|-|-|.| | |}} | ||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | W01 | | | | W02 | |W01={{fontcolor|#F8F8FF|'''Yes'''}}|W02=<div style="text-align: center; background: #FFFFFF; height: 25px; line-height: 25px;">'''No'''</div>}} | {{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | W01 | | | | W02 | |W01={{fontcolor|#F8F8FF|'''Yes'''}}|W02=<div style="text-align: center; background: #FFFFFF; height: 25px; line-height: 25px;">'''No'''</div>}} | ||
| Line 97: | Line 97: | ||
❑ Consider CTA if patient has a Wells score >4}} </div>|boxstyle= background: #FA8072}} | ❑ Consider CTA if patient has a Wells score >4}} </div>|boxstyle= background: #FA8072}} | ||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | |!| | | | | | | | | | |}} | {{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | |!| | | | | | | | | | |}} | ||
{{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | F01 | | | | | | | | | |F01=<div style="float: center; width: 14em; padding:1em; color: #FFFFFF;"><center>Does the patient have any [[EKG|<span style="color:white;">ECG</span>]] | {{familytree |boxstyle= padding: 0; background: #FA8072; text-align: center;| | | | | | | | | | F01 | | | | | | | | | |F01=<div style="float: center; width: 14em; padding:1em; color: #FFFFFF;"><center>Does the patient have any characteristic signs and symptoms or any [[EKG|<span style="color:white;">ECG</span>]] / lab abnormalities?</center></div>}} | ||
{{familytree | | | | | | |,|-|-|-|^ | {{familytree | | | | | | |,|-|-|-|^|-|-|-|-|-|-|-|-|-|-|.|}} | ||
{{familytree | | | | | | C01 | {{familytree | | | | | | C01 | | | | | | | | | | | | | C02 |C01={{fontcolor|#F8F8FF|'''Yes'''}}|C02={{fontcolor|#F8F8FF|'''No'''}}|boxstyle= background-color: #FA8072}} | ||
{{familytree | | | | | | |! | {{familytree | | | | | | |!| | | | | | | | | | | | | | |!| | }} | ||
{{familytree | | |,|-|-|-|+ | {{familytree | | |,|-|-|-|+|-|-|-|v|-|-|-|v|-|-|-|.| | L01 | |L01=<div style="float: center; width: 14em; padding:1em; color: #FFFFFF;"><center>'''❑ Continue supportive care<br>❑ Place patient on cardiac monitor <br>❑ Re-evaluate if status worsens'''</center></div>|boxstyle= background-color: #FA8072}} | ||
{{familytree | | H01 | | H02 | | H03 | | H04 | | H05 | | | {{familytree | | H01 | | H02 | | H03 | | H04 | | H05 | | | | | |H01=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Tachyarrhythmia'''</center></div> | ||
{{familytree | | | ---- | ||
{{familytree |I01| |I02| | | | | | | <div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Abnormal rhythm w/ a ventricular rate of ≥100/min<br><br><br></div> | ||
|H02=<div style="float: center; padding:1em; color: #FFFFFF; width:8em;"><center>'''Ischemia'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ ST-segment deviation<br>❑ Elevated cardiac biomarkers</div> | |||
|H03=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Cardiac Tamponade'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Elevated JVP<br>❑ Pulsus paradoxus<br>❑ Low-voltage QRS complexes<br>❑ Electrical alternans<br> | |||
❑ PR segment depression</div> | |||
|H04=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Thyroid Storm'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Suppressed TSH<br>❑ Elevated free T3/T4<br><br><br><br></div> | |||
|H05=<div style="float: center; padding:1em; color: #FFFFFF;"><center>'''Pulmonary Embolism'''</center></div> | |||
---- | |||
<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;">❑ Tachypnea<br>❑ Wells Score >4<br>❑ Positive chest CTA<br><br></div> | |||
|boxstyle= background-color: #FA8072}} | |||
{{familytree | | |!| | | |!| | | |!| | | |!| | | |!| | | | | | | |}} | |||
{{familytree | | I01 | | I02 | | I03 | | I04 | | I05 | | | | | | |I01=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Narrow_complex_tachycardia_resident_survival_guide#Treatment|<span style="color:white;">Supraventricular / Narrow-Complex Tachyarrhythmia Treatment Algorithm</span>]] | |||
*[[Wide_complex_tachycardia_resident_survival_guide#Treatment|<span style="color:white;">Ventricular / Wide-Complex Tachyarrhythmia Treatment Algorithm</span>]]</div> | |||
|I02=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Unstable_angina/_NSTEMI_resident_survival_guide|<span style="color:white;">UA / NSTEMI Treatment Algorithm</span>]] | |||
*[[STEMI_resident_survival_guide#FIRE:_Focused_Initial_Rapid_Evaluation|<span style="color:white;">STEMI Treatment Algorithm</span>]]<br><br><br><br><br><br></div> | |||
|I03=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Cardiac_tamponade_resident_survival_guide#Treatment|<span style="color:white;">Cardiac Tamponade Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|I04=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Hyperthroidism_resident_survival_guide#Treatment|<span style="color:white;">Thyroid Storm Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|I05=<div style="float: left; padding:1em; color: #FFFFFF; text-align: left;"> | |||
*[[Pulmonary_embolism_resident_survival_guide#Treatment|<span style="color:white;">Pulmonary Embolism Treatment Algorithm</span>]]<br><br><br><br><br><br><br><br><br><br><br><br></div> | |||
|boxstyle= background-color: #FA8072}} | |||
{{familytree/end}} | {{familytree/end}} | ||
| Line 123: | Line 156: | ||
: ❑ Pulsation [[palpitations]] <br> | : ❑ Pulsation [[palpitations]] <br> | ||
: ❑ [[Anxiety|Anxiety-related]] palpitations<br> | : ❑ [[Anxiety|Anxiety-related]] palpitations<br> | ||
❑ '''Onset''' | ❑ '''Onset'''<br> | ||
: ❑ Sudden <br> | : ❑ Sudden <br> | ||
: ❑ Gradual<br> | : ❑ Gradual<br> | ||
❑ '''Duration''' | ❑ '''Duration'''<br> | ||
: ❑ Brief<br> | : ❑ Brief<br> | ||
: ❑ Persistent<br> | : ❑ Persistent<br> | ||
❑ '''Frequency''' | ❑ '''Frequency'''<br> | ||
❑ '''Termination | : ❑ Daily | ||
❑ '''Associated | : ❑ Weekly | ||
❑ Sudden changes of posture (suggestive of [[Orthostatic hypotension|intolerance to orthostasis]] or [[AVNRT]])<br> | : ❑ Monthly<br> | ||
❑ [[Syncope]]<br> | ❑ '''Termination'''<br> | ||
❑ [[Angina]], [[dyspnea]], [[fatigue]], [[vertigo]], [[dizziness]]<br> | : ❑ Successful with [[vagal maneuvers]] (suggestive of [[SVT]])<br> | ||
❑ [[Polyuria]] (suggestive of [[AF]])<br> | ❑ '''Associated with'''<br> | ||
❑ Rapid regular pulse in the [[neck]]<br> | : ❑ Sudden changes of posture (suggestive of [[Orthostatic hypotension|intolerance to orthostasis]] or [[AVNRT]])<br> | ||
: ❑ [[Syncope]]<br> | |||
: ❑ [[Angina]], [[dyspnea]], [[fatigue]], [[vertigo]], [[dizziness]]<br> | |||
: ❑ [[Polyuria]] (suggestive of [[AF]])<br> | |||
: ❑ Rapid regular pulse in the [[neck]]<br> | |||
</div>}} | </div>}} | ||
{{familytree | | | | | | | |!| | | | | | | |}} | {{familytree | | | | | | | |!| | | | | | | |}} | ||
{{familytree | | | | | | | B01 | | | | | |B01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Inquire about drugs that can cause palpitations:'''<br> | {{familytree | | | | | | | B01 | | | | | |B01=<div style="float: left; text-align: left; width: 24em; padding:1em;">'''Inquire about drugs that can cause palpitations:'''<br> | ||
❑ [[Sympathomimetic|Sympathomimetic agents]] <br> | ❑ [[Sympathomimetic|Sympathomimetic agents]] <br> | ||
❑ | ❑ Inhaled beta-agonists <br> | ||
❑ [[Vasodilator|Vasodilators]]<br> | ❑ [[Vasodilator|Vasodilators]]<br> | ||
❑ [[Anticholinergic|Anticholinergic agents]]<br> | ❑ [[Anticholinergic|Anticholinergic agents]]<br> | ||
❑ | ❑ [[Beta-blocker]] withdrawal<br> | ||
❑ Recreational drugs<br> | ❑ Recreational drugs<br> | ||
: ❑ [[Alcohol]]<br> | : ❑ [[Alcohol]]<br> | ||
| Line 160: | Line 197: | ||
❑ Previous episodes of palpitations<br> | ❑ Previous episodes of palpitations<br> | ||
: ❑ First episode | : ❑ First episode | ||
: ❑ Number of episodes<br> | : ❑ Number of episodes<br> | ||
: ❑ Time since last episode<br> | : ❑ Time since last episode<br> | ||
| Line 196: | Line 231: | ||
❑ [[Temperature]]<br> | ❑ [[Temperature]]<br> | ||
: ❑ [[Fever]] (suggestive of [[infection]])<br> | : ❑ [[Fever]] (suggestive of [[infection]])<br> | ||
❑ [[ | ❑ [[Tachypnea]] (non-specific)<br> | ||
'''Eyes'''<br> | '''Eyes'''<br> | ||
❑ [[Exophthalmos]] (suggestive of [[Graves disease]])<br> | ❑ [[Exophthalmos]] (suggestive of [[Graves disease]])<br> | ||
| Line 224: | Line 259: | ||
: ❑ Determine if the rhythm is regular or irregular | : ❑ Determine if the rhythm is regular or irregular | ||
: ❑ Assess the [[p wave]] and [[QRS]] morphology | : ❑ Assess the [[p wave]] and [[QRS]] morphology | ||
: ❑ Rate over 100 bpm, QRS <120 ms (suggestive of [[Narrow complex tachycardia resident survival guide|narrow complex tachycardia]]) | : ❑ Rate over 100 bpm, QRS < 120 ms (suggestive of [[Narrow complex tachycardia resident survival guide|narrow complex tachycardia]]) | ||
: ❑ Search for short [[PR intervals]] and [[delta waves]] (suggestive of [[WPW]]) | : ❑ Search for short [[PR intervals]] and [[delta waves]] (suggestive of [[WPW]]) | ||
: ❑ Irregular rhythm, change in [[p wave]] morphology (suggestive of [[AF]]) | : ❑ Irregular rhythm, change in [[p wave]] morphology (suggestive of [[AF]]) | ||
: ❑ Regular rhythm, saw-tooth appearance (suggestive of [[atrial flutter]]) | : ❑ Regular rhythm, saw-tooth appearance (suggestive of [[atrial flutter]]) | ||
: ❑ Rate over 100 bpm, [[QRS]] >120 ms (suggestive of [[Wide complex tachycardia resident survival guide|wide complex tachycardia]]) | : ❑ Rate over 100 bpm, [[QRS]] > 120 ms (suggestive of [[Wide complex tachycardia resident survival guide|wide complex tachycardia]]) | ||
: ❑ Search for deep septal [[Q waves]] in [[Introduction to ECG#Leads|I]], [[Introduction to ECG#Leads|V4]] to [[Introduction to ECG#Leads|V6]] and signs of [[left ventricular hypertrophy]] (suggestive of [[hypertrophic obstructive cardiomyopathy]]) | : ❑ Search for deep septal [[Q waves]] in [[Introduction to ECG#Leads|I]], [[Introduction to ECG#Leads|V4]] to [[Introduction to ECG#Leads|V6]] and signs of [[left ventricular hypertrophy]] (suggestive of [[hypertrophic obstructive cardiomyopathy]]) | ||
: ❑ Normal [[EKG]] (suggestive of [[anxiety]] or [[panic attack]]) | : ❑ Normal [[EKG]] (suggestive of [[anxiety]] or [[panic attack]]) | ||
❑ [[CBC]] (to rule out [[anemia]] or [[infection]])<br> | ❑ [[CBC]] (to rule out [[anemia]] or [[infection]])<br> | ||
❑ [[Electrolyte disturbances|Electrolytes]] (to rule out | ❑ [[Electrolyte disturbances|Electrolytes]] (to rule out potassium and magnesium imbalances)<br> | ||
❑ [[TSH]] (to rule out [[hyperthyroidism]])<br> | ❑ [[TSH]] (to rule out [[hyperthyroidism]])<br> | ||
❑ [[Blood sugar|Glucose level]] (to rule out [[hypoglycemia]])<br> | ❑ [[Blood sugar|Glucose level]] (to rule out [[hypoglycemia]])<br> | ||
| Line 240: | Line 275: | ||
❑ [[TTE]] (to rule out [[structural heart disease]])<br> | ❑ [[TTE]] (to rule out [[structural heart disease]])<br> | ||
</div>}} | </div>}} | ||
{{familytree | | | | | | |!| | | | | | | |}} | {{familytree | | | | | | |!| | | | | | | |}} | ||
{{familytree | | | | | | W01 | | | | | | | |W01= <div style="float: left; text-align: left; width: 24em; padding:1em;">'''Consider hospitalization'''<br> | {{familytree | | | | | | W01 | | | | | | | |W01= <div style="float: left; text-align: left; width: 24em; padding:1em;">'''Consider hospitalization'''<br> | ||
| Line 257: | Line 291: | ||
❑ [[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|Wolff-Parkinson-White syndrome]]<br> | ❑ [[Wolff-Parkinson-White syndrome resident survival guide#Complete Diagnostic Approach|Wolff-Parkinson-White syndrome]]<br> | ||
</div>|S02=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Myocardial ischemia'''<br> | </div>|S02=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Myocardial ischemia'''<br> | ||
❑ | ❑ [[Acute coronary syndrome]]<br> | ||
: ❑ [[STEMI resident survival guide#Diagnosis|STEMI]]<br> | : ❑ [[STEMI resident survival guide#Diagnosis|STEMI]]<br> | ||
: ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|NSTEMI]]<br> | : ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|NSTEMI]]<br> | ||
: ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|Unstable angina]]<br> | : ❑ [[Unstable angina/ NSTEMI resident survival guide#Diagnostic approach|Unstable angina]]<br> | ||
</div>|S03=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Other EKG findings'''</div>|S04=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Does the patient have history | </div>|S03=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Other EKG findings'''</div>|S04=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''Does the patient have a history of [[psychiatric disorder]]s?'''</div>}} | ||
{{familytree | | | | | | |,|-|^|-|.| | | |,|-|^|-|.| | |}} | {{familytree | | | | | | |,|-|^|-|.| | | |,|-|^|-|.| | |}} | ||
{{familytree | | | | | | R01 | | R02 | | R03 | | R04 | | |R01=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''EKG findings suggestive of pericarditis'''<br> | {{familytree | | | | | | R01 | | R02 | | R03 | | R04 | | |R01=<div style="float: left; text-align: left; width: 14em; padding:1em;">'''EKG findings suggestive of pericarditis'''<br> | ||
| Line 268: | Line 302: | ||
❑ [[PR segment depression]]<br> | ❑ [[PR segment depression]]<br> | ||
❑ [[Low QRS voltage]] (in large [[Pericardial effusion]] and [[Constrictive pericarditis]])<br> | ❑ [[Low QRS voltage]] (in large [[Pericardial effusion]] and [[Constrictive pericarditis]])<br> | ||
</div>|R02=''' | </div>|R02='''Non-specific EKG findings'''|R03='''Yes'''|R04='''No'''}} | ||
{{familytree | | | | | | | | | | | |!| | | |!| | | |!| | }} | {{familytree | | | | | | | | | | | |!| | | |!| | | |!| | }} | ||
{{familytree | | | | | | | | | | | T01 | | T02 | | T03 | | |T01='''Order a TTE'''|T02=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | {{familytree | | | | | | | | | | | T01 | | T02 | | T03 | | |T01='''Order a TTE'''|T02=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | ||
Consider the following if all diagnostic tests are normal:<br> | |||
❑ [[Anxiety]]<br> | ❑ [[Anxiety]]<br> | ||
| Line 276: | Line 311: | ||
❑ [[Depression]]<br> | ❑ [[Depression]]<br> | ||
❑ [[Somatization]]<br> | ❑ [[Somatization]]<br> | ||
</div>|T03=<div style="float: left; text-align: left; width: 12em; padding:1em;">''' | </div>|T03=<div style="float: left; text-align: left; width: 12em; padding:1em;">'''Is the patient taking any substances/drugs that can cause palpitations?'''</div>}} | ||
{{familytree | | | | | | | | | | | |!| | | | |,|-|-|^|-|-|.| | |}} | {{familytree | | | | | | | | | | | |!| | | | |,|-|-|^|-|-|.| | |}} | ||
{{familytree | | | | | | | | | | | Q01 | | | Z01 | | | | Z02 | | | | |Q01=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | {{familytree | | | | | | | | | | | Q01 | | | Z01 | | | | Z02 | | | | |Q01=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | ||
| Line 290: | Line 325: | ||
{{familytree | | | | | | | | | | | | | | | | I03 | | | | I04 | | | |I03=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | {{familytree | | | | | | | | | | | | | | | | I03 | | | | I04 | | | |I03=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | ||
<span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | <span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | ||
❑ [[Acute alcohol intoxication|Alcohol]]<br> | ❑ [[Acute alcohol intoxication|Alcohol]]<br> | ||
❑ [[Caffeine#Overuse|Caffeine]]<br> | ❑ [[Caffeine#Overuse|Caffeine]]<br> | ||
| Line 297: | Line 331: | ||
: ❑ [[Vasodilator|Vasodilators]]<br> | : ❑ [[Vasodilator|Vasodilators]]<br> | ||
: ❑ [[Anticholinergic#Effects|Anticholinergic agents]]<br> | : ❑ [[Anticholinergic#Effects|Anticholinergic agents]]<br> | ||
: ❑ | : ❑ [[Beta-blocker]] withdrawal<br> | ||
: ❑ [[Beta-agonists]]<br> | : ❑ [[Beta-agonists]]<br> | ||
: ❑ [[Digoxin#Wanrings|Digitalis]]<br> | : ❑ [[Digoxin#Wanrings|Digitalis]]<br> | ||
| Line 306: | Line 340: | ||
: ❑ [[Amphetamines]] | : ❑ [[Amphetamines]] | ||
❑ [[Nicotine]] | ❑ [[Nicotine]] | ||
</div>|I04=<div style="float: left; text-align: left; width: 12em; padding:1em;" | </div>|I04=<div style="float: left; text-align: left; width: 12em; padding:1em;"> | ||
<span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | <span style="font-size:85%">Click in each link for the specific diagnostic approach and management</span><br> | ||
❑ [[Anemia]]<br> | ❑ [[Anemia]]<br> | ||
❑ [[Electrolyte disturbances]]<br> | ❑ [[Electrolyte disturbances]]<br> | ||
| Line 321: | Line 354: | ||
==Treatment== | ==Treatment== | ||
The management of palpitations | The management of palpitations should be directed towards the underlying cause. If the etiology can be determined and low risk, potentially curative treatments are available these should be the first choice of management. For benign arrhythmias, such as extrasystole, lifestyle changes may be sufficient to prevent future episodes. For patients in whom no clear disease has been established, patients should be advised to avoid possible triggers of palpitations such as caffeine, alcohol, nicotine, recreational drugs.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Zimetbaum-1998">{{Cite journal | last1 = Zimetbaum | first1 = P. | last2 = Josephson | first2 = ME. | title = Evaluation of patients with palpitations. | journal = N Engl J Med | volume = 338 | issue = 19 | pages = 1369-73 | month = May | year = 1998 | doi = 10.1056/NEJM199805073381907 | PMID = 9571258 }}</ref><ref name="har">{{Cite web | last = | first = | title = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | url = http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf | publisher = | date = | accessdate = 16 April 2014 }}</ref><ref name="Abbott-2005">{{Cite journal | last1 = Abbott | first1 = AV. | title = Diagnostic approach to palpitations. | journal = Am Fam Physician | volume = 71 | issue = 4 | pages = 743-50 | month = Feb | year = 2005 | doi = | PMID = 15742913 }}</ref><ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | ||
<span style="font-size:85%">'''Abbreviations:''' '''NSTEMI:''' [[Non ST elevation myocardial infarction]]; '''STEMI:''' [[ST elevation myocardial infarction]]</span> | <span style="font-size:85%">'''Abbreviations:''' '''NSTEMI:''' [[Non ST elevation myocardial infarction]]; '''STEMI:''' [[ST elevation myocardial infarction]]</span> | ||
| Line 327: | Line 360: | ||
{{familytree | | | | | | | | A01 | | | | | | | | | | |A01='''Determine the cause of the palpitations'''}} | {{familytree | | | | | | | | A01 | | | | | | | | | | |A01='''Determine the cause of the palpitations'''}} | ||
{{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | | | | | | }} | {{familytree | | | | |,|-|-|-|^|-|-|-|-|.| | | | | | | | }} | ||
{{familytree | | | B01 | | | | | | | | B02 | | | | | | |B01=<div style="float: left; text-align: left; width: 08em; padding:1em;">'''Cardiac cause'''</div>|B02=''' | {{familytree | | | B01 | | | | | | | | B02 | | | | | | |B01=<div style="float: left; text-align: left; width: 08em; padding:1em;">'''Cardiac cause'''</div>|B02='''Non-cardiac cause'''}} | ||
{{familytree | |,|-|^|-|.| | | |,|-|-|-|+|-|-|-|.| | | |}} | {{familytree | |,|-|^|-|.| | | |,|-|-|-|+|-|-|-|.| | | |}} | ||
{{familytree | C01 | | C02 | | C03 | | C04 | | C05 | | | |C01=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Arrhythmia'''<br> | {{familytree | C01 | | C02 | | C03 | | C04 | | C05 | | | |C01=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Arrhythmia'''<br> | ||
| Line 351: | Line 384: | ||
: [[Aortic stenosis resident survival guide#treatment|Aortic stenosis]]<br> | : [[Aortic stenosis resident survival guide#treatment|Aortic stenosis]]<br> | ||
: [[Aortic regurgitation resident survival guide#Treatment|Aortic regurgitation]]<br> | : [[Aortic regurgitation resident survival guide#Treatment|Aortic regurgitation]]<br> | ||
</div>|C03=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Psychiatric | </div>|C03=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Psychiatric disorder'''<br> | ||
[[Anxiety]]<br> | [[Anxiety]]<br> | ||
[[Panic attack]]<br> | [[Panic attack]]<br> | ||
[[Depression]]<br> | [[Depression]]<br> | ||
[[Somatization]]<br> | [[Somatization]]<br> | ||
</div>|C04=<div style="float: left; text-align: left; width: 16em; padding:1em;">''' | </div>|C04=<div style="float: left; text-align: left; width: 16em; padding:1em;">'''Substance/drug intake'''<br> | ||
❑ [[Alcohol]]<br> | ❑ [[Alcohol]]<br> | ||
❑ [[Caffeine]]<br> | ❑ [[Caffeine]]<br> | ||
| Line 363: | Line 396: | ||
: ❑ [[Vasodilators]]<br> | : ❑ [[Vasodilators]]<br> | ||
: ❑ [[Anticholinergic|Anticholinergic agents]]<br> | : ❑ [[Anticholinergic|Anticholinergic agents]]<br> | ||
: ❑ | : ❑ [[Beta-blocker]] withdrawal<br> | ||
: ❑ [[Beta-agonists]]<br> | : ❑ [[Beta-agonists]]<br> | ||
: ❑ [[Digitalis]]<br> | : ❑ [[Digitalis]]<br> | ||
| Line 395: | Line 428: | ||
==Do's== | ==Do's== | ||
* If possible, perform physical exam and [[EKG]] when the patient is symptomatic.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | * If possible, perform a physical exam and an [[EKG|ECG]] when the patient is symptomatic.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* | * If a patient is asymptomatic, search for signs of [[structural heart disease]] such as [[murmurs]], displaced [[apex beat]] or [[S3]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an ambulatory [[EKG]] in patients with recurrent episodes of [[palpitations]] | * Perform an ambulatory [[EKG|ECG]] in patients with recurrent episodes of [[palpitations]] of undetermined etiology.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[Electrophysiology|EPS]] | * Perform an electrophysiologic study ([[Electrophysiology|EPS]]) for patients with inconclusive ambulatory [[EKG|ECG]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[Electrophysiology|EPS]], with [[Catheter ablation|ablation therapy]] if necessary, in patients severe [[heart disease]], when [[palpitations]] preceded [[syncope]] and when the patient | * Perform an [[Electrophysiology|EPS]], with [[Catheter ablation|ablation therapy]] if necessary, in patients with severe [[heart disease]], particularly when [[palpitations]] preceded [[syncope]] and when the patient required cardio-respiratory resuscitation maneuvers.<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref><ref name="Thavendiranathan-2009">{{Cite journal | last1 = Thavendiranathan | first1 = P. | last2 = Bagai | first2 = A. | last3 = Khoo | first3 = C. | last4 = Dorian | first4 = P. | last5 = Choudhry | first5 = NK. | title = Does this patient with palpitations have a cardiac arrhythmia? | journal = JAMA | volume = 302 | issue = 19 | pages = 2135-43 | month = Nov | year = 2009 | doi = 10.1001/jama.2009.1673 | PMID = 19920238 }}</ref> | ||
* | * Advise life-style changes that may lower the possibility of future episodes, such as exercise, lower [[alcohol]] and [[caffeine]] intake, and [[Smoking|smoking cessation]].<ref name="pmid21697315">{{cite journal| author=Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L et al.| title=Management of patients with palpitations: a position paper from the European Heart Rhythm Association. | journal=Europace | year= 2011 | volume= 13 | issue= 7 | pages= 920-34 | pmid=21697315 | doi=10.1093/europace/eur130 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21697315 }} </ref> | ||
* Perform an [[exercise stress test]] in patients with exercise induced [[palpitations]].<ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | * Perform an [[exercise stress test]] in patients with exercise induced [[palpitations]].<ref name="turner">{{Cite web | last = | first = | title = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | url = http://www.turner-white.com/pdf/hp_jan03_methods.pdf | publisher = | date = | accessdate = 25 April 2014 }}</ref><br> | ||
| Line 408: | Line 441: | ||
{| style="cellpadding=0; cellspacing= 0; width: 800px;" | {| style="cellpadding=0; cellspacing= 0; width: 800px;" | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Type of [[Arrhythmia]]'''||style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''[[EKG]]''' (lead II) ||style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align=center | '''Clues''' | | style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''Type of [[Arrhythmia]]'''|| style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''[[EKG]]''' (lead II) || style="padding: 0 5px; font-size: 100%; background: #F5F5F5;" align="center" | '''Clues''' | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left| '''[[Sinus tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:Sinus tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': gradual<br> '''Rhythm''': regular<br> '''Rate''': >220 minus the age of the patient <br> '''Response to adenosine''': transient decrease of the rate | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" | '''[[Sinus tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:Sinus tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': gradual<br> '''Rhythm''': regular<br> '''Rate''': >220 minus the age of the patient <br> '''Response to adenosine''': transient decrease of the rate | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Atrial fibrillation]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:atrial fibrillation.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': irregular <br> '''Rate''':100-180 bpm <br> '''Response to adenosine''': transient decrease of the ventricular rate | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Atrial fibrillation]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:atrial fibrillation.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': irregular <br> '''Rate''':100-180 bpm <br> '''Response to adenosine''': transient decrease of the ventricular rate | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Atrial flutter]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:atrial flutter.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': >150 bpm <br> '''Response to adenosine''': transient decrease of the rate <br> Presence of saw-tooth appearance | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Atrial flutter]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:atrial flutter.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': >150 bpm <br> '''Response to adenosine''': transient decrease of the rate <br> Presence of saw-tooth appearance | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[AVNRT]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:AVNRT.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[AVNRT]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:AVNRT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[AVRT]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:AVRT.png|300px|link=Narrow complex tachycardia resident survival guide]]||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left| '''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[AVRT]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:AVRT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" | '''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm <br> '''Response to adenosine''': termination of the arrhythmia | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Focal atrial tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:focal atrial tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Focal atrial tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:focal atrial tachycardia.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': abrupt <br> '''Rhythm''': regular<br> '''Rate''': 150-250 bpm | ||
|- | |- | ||
|style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Junctional tachycardia|Nonparoxysmal junctional tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:JTS.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Rhythm''': regular <br> Retrograde P wave<br> Most commonly due to ischemia or digitalis toxicity | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Junctional tachycardia|Nonparoxysmal junctional tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:JTS.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Rhythm''': regular <br> Retrograde P wave<br> Most commonly due to ischemia or digitalis toxicity | ||
|- | |- | ||
| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''[[Multifocal atrial tachycardia]]'''||style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|[[Image:MAT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align=left|'''Onset and termination''': gradual<br> '''Rhythm''': irregular<br> '''Rate''': 100-150 bpm <br> '''Response to adenosine''': no effect<br>3 different [[P wave]] morphologies | | style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''[[Multifocal atrial tachycardia]]'''|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |[[Image:MAT.png|300px|link=Narrow complex tachycardia resident survival guide]]|| style="padding: 0 5px; font-size: 90%; background: #DCDCDC;" align="left" |'''Onset and termination''': gradual<br> '''Rhythm''': irregular<br> '''Rate''': 100-150 bpm <br> '''Response to adenosine''': no effect<br>3 different [[P wave]] morphologies | ||
|- | |- | ||
|} | |} | ||
===Wide complex tachycardia=== | ===Wide complex tachycardia=== | ||
| Line 440: | Line 472: | ||
!p-wave | !p-wave | ||
!Effect of adenosine | !Effect of adenosine | ||
|- | |- | ||
| colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Wide complex (QRS > 0.12)''' | | colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Wide complex (QRS > 0.12)''' | ||
|- | |- | ||
| Line 496: | Line 528: | ||
| [[AV-dissociation]] | | [[AV-dissociation]] | ||
| no rate reduction | | no rate reduction | ||
|- | |- | ||
|colspan="8"|* Bundle-branch re-entrant tachycardia is extremely rare | | colspan="8" |* Bundle-branch re-entrant tachycardia is extremely rare | ||
|} | |} | ||
Latest revision as of 16:20, 4 May 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D.
| Palpitations Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Gallery |
Overview
Causes
Life-Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common causes
- Cardiac causes
- Arrhythmic
- Non-arrhythmic
- Valvular disease
- Pericarditis
- Structural heart disease
- Malfunctioning pacemaker
- Psychiatric causes
- Substance - drug causes
- Systemic causes
Click here for a complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[1][2]
Boxes in the red signify that an urgent management is needed.
Abbreviations: EKG: Electrocardiogram; IV: Intravenous; NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Does the patient have any of the following findings that require urgent management? ❑ Syncope (suggestive of PE, cardiac tamponade, complete AV block) | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Stabilize the patient ❑ Consider intubation if the patient's airway is compromised, has a Glasgow coma scale (GCS < 8) or profound hemodynamic instability ❑ Administer oxygen and maintain a saturation >90% ❑ 12 lead ECG | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Place patient on cardiac monitor ❑ Re-evaluate if status worsens | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Abnormal rhythm w/ a ventricular rate of ≥100/min | ❑ ST-segment deviation ❑ Elevated cardiac biomarkers | ❑ Elevated JVP ❑ Pulsus paradoxus ❑ Low-voltage QRS complexes ❑ Electrical alternans ❑ PR segment depression | ❑ Suppressed TSH ❑ Elevated free T3/T4 | ❑ Tachypnea ❑ Wells Score >4 ❑ Positive chest CTA | |||||||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1][3][4][5][6][7]
Abbreviations: AF: Atrial fibrillation; AVRT: AV reentry tachycardia; AVNRT: AV nodal reentry tachycardia; BP: Blood pressure; CBC: Complete blood count; EKG: Electrocardiogram; EPS: Electrophysiological study SVT: Supraventricular tachycardia TSH: Thyroid stimulating hormone; TTE: Transthoracic echocardiography; VT: Ventricular tachycardia; WPW: Wolff-Parkinson-White syndrome
Characterize the symptoms: ❑ Character of palpitations
❑ Onset
❑ Duration
❑ Frequency
❑ Termination
❑ Associated with | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Inquire about drugs that can cause palpitations: ❑ Sympathomimetic agents ❑ Weight reduction drugs | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed past medical history: ❑ Previous episodes of palpitations
❑ Cardiac arrhythmia ❑ History of panic attacks | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vitals
❑ Tachypnea (non-specific) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order labs and tests: ❑ EKG
❑ CBC (to rule out anemia or infection) Order imaging studies | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Recurrent episodes when no ambulatory EKG devices are available | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have clinical or EKG findings suggestive of a cardiac cause of the palpitations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Other EKG findings | Does the patient have a history of psychiatric disorders? | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
EKG findings suggestive of pericarditis Pericarditis | Non-specific EKG findings | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order a TTE | Consider the following if all diagnostic tests are normal: ❑ Anxiety | Is the patient taking any substances/drugs that can cause palpitations? | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Click in each link for the specific diagnostic approach and management
❑ Recreational drugs
❑ Nicotine | Click in each link for the specific diagnostic approach and management | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
The management of palpitations should be directed towards the underlying cause. If the etiology can be determined and low risk, potentially curative treatments are available these should be the first choice of management. For benign arrhythmias, such as extrasystole, lifestyle changes may be sufficient to prevent future episodes. For patients in whom no clear disease has been established, patients should be advised to avoid possible triggers of palpitations such as caffeine, alcohol, nicotine, recreational drugs.[1][3][4][5][7]
Abbreviations: NSTEMI: Non ST elevation myocardial infarction; STEMI: ST elevation myocardial infarction
| Determine the cause of the palpitations | |||||||||||||||||||||||||||||||||||||||||||
Cardiac cause | Non-cardiac cause | ||||||||||||||||||||||||||||||||||||||||||
Psychiatric disorder | Substance/drug intake ❑ Alcohol
❑ Recreational drugs
❑ Nicotine | ||||||||||||||||||||||||||||||||||||||||||
Consider hospitalization ❑ Implantations or replacement of pacemakers for bradyarrhythmias | |||||||||||||||||||||||||||||||||||||||||||
Do's
- If possible, perform a physical exam and an ECG when the patient is symptomatic.[1]
- If a patient is asymptomatic, search for signs of structural heart disease such as murmurs, displaced apex beat or S3.[1]
- Perform an ambulatory ECG in patients with recurrent episodes of palpitations of undetermined etiology.[1]
- Perform an electrophysiologic study (EPS) for patients with inconclusive ambulatory ECG.[1]
- Perform an EPS, with ablation therapy if necessary, in patients with severe heart disease, particularly when palpitations preceded syncope and when the patient required cardio-respiratory resuscitation maneuvers.[1][6]
- Advise life-style changes that may lower the possibility of future episodes, such as exercise, lower alcohol and caffeine intake, and smoking cessation.[1]
- Perform an exercise stress test in patients with exercise induced palpitations.[7]
EKG gallery
Narrow complex tachycardia
| Type of Arrhythmia | EKG (lead II) | Clues |
| Sinus tachycardia |  |
Onset and termination: gradual Rhythm: regular Rate: >220 minus the age of the patient Response to adenosine: transient decrease of the rate |
| Atrial fibrillation | 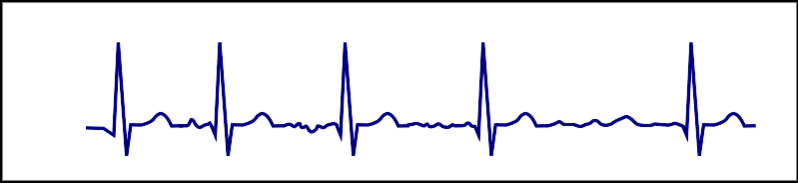 |
Onset and termination: abrupt Rhythm: irregular Rate:100-180 bpm Response to adenosine: transient decrease of the ventricular rate |
| Atrial flutter | 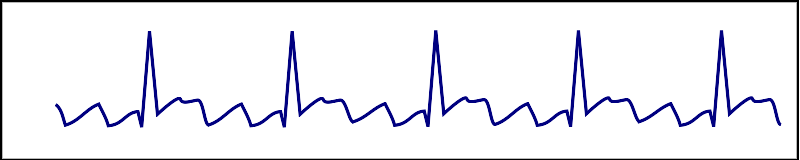 |
Onset and termination: abrupt Rhythm: regular Rate: >150 bpm Response to adenosine: transient decrease of the rate Presence of saw-tooth appearance |
| AVNRT | 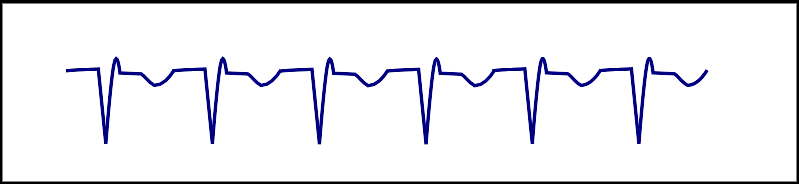 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| AVRT |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| Focal atrial tachycardia | 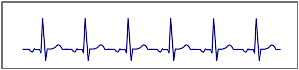 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm |
| Nonparoxysmal junctional tachycardia |  |
Rhythm: regular Retrograde P wave Most commonly due to ischemia or digitalis toxicity |
| Multifocal atrial tachycardia | 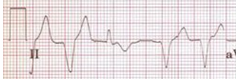 |
Onset and termination: gradual Rhythm: irregular Rate: 100-150 bpm Response to adenosine: no effect 3 different P wave morphologies |
Wide complex tachycardia
| Example | Regularity | Atrial frequency | Ventricular frequency | Origin (SVT/VT) | p-wave | Effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Wide complex (QRS > 0.12) | |||||||
| Ventricular Tachycardia | regular (mostly) | 60-100 bpm | 110-250 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Ventricular Fibrillation | irregular | 60-100 bpm | 400-600 bpm | ventricle (VT) | AV-dissociation | none | |
| Ventricular Flutter | regular | 60-100 bpm | 150-300 bpm | ventricle (VT) | AV-dissociation | none | |
| Accelerated Idioventricular Rhythm | regular (mostly) | 60-100 bpm | 50-110 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | |
| Torsade de Pointes | regular | 150-300 bpm | ventricle (VT) | AV-dissociation | no rate reduction (sometimes accelerates) | ||
| Bundle-branch re-entrant Tachycardia* | regular | 60-100 bpm | 150-300 bpm | ventricles (VT) | AV-dissociation | no rate reduction | |
| * Bundle-branch re-entrant tachycardia is extremely rare | |||||||
STEMI
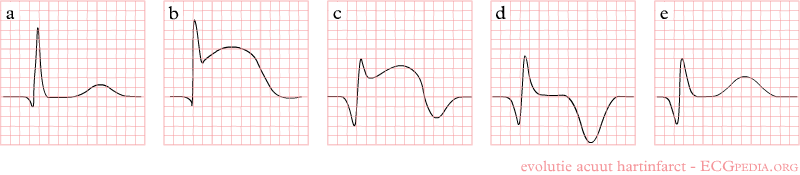
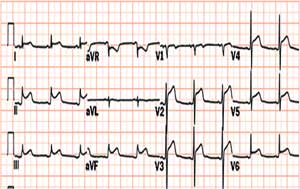
Shown below is an EKG demonstrating the evolution of an infarct on the EKG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave suggest STEMI.
NSTEMI
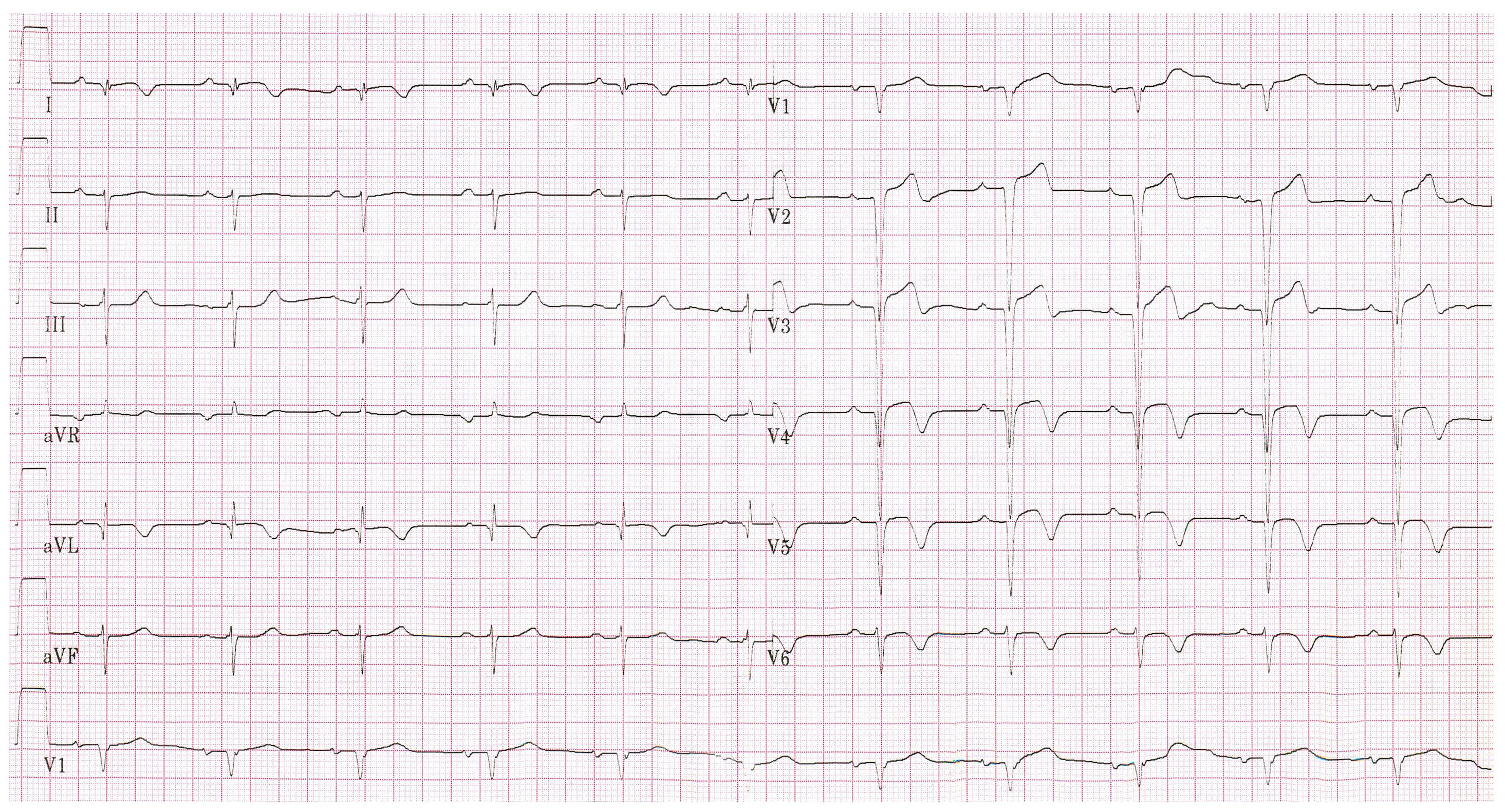
Shown below is an EKG showing an ST depression in V2, V3, V4 and V6.
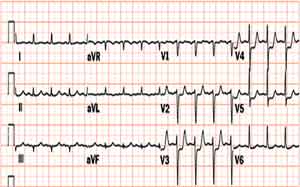
Shown below is an EKG showing an inversion in the T wave at leads V4, V5 and V6.
Pericarditis
Shown below is an EKG with ST elevation in lead I, II, V2, V3, V4, V5 and V6.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L; et al. (2011). "Management of patients with palpitations: a position paper from the European Heart Rhythm Association". Europace. 13 (7): 920–34. doi:10.1093/europace/eur130. PMID 21697315.
- ↑ "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ 3.0 3.1 Zimetbaum, P.; Josephson, ME. (1998). "Evaluation of patients with palpitations". N Engl J Med. 338 (19): 1369–73. doi:10.1056/NEJM199805073381907. PMID 9571258. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 "http://scholar.harvard.edu/files/barkoudah/files/management_of_palpitations.pdf" (PDF). Retrieved 16 April 2014. External link in
|title=(help) - ↑ 5.0 5.1 Abbott, AV. (2005). "Diagnostic approach to palpitations". Am Fam Physician. 71 (4): 743–50. PMID 15742913. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Thavendiranathan, P.; Bagai, A.; Khoo, C.; Dorian, P.; Choudhry, NK. (2009). "Does this patient with palpitations have a cardiac arrhythmia?". JAMA. 302 (19): 2135–43. doi:10.1001/jama.2009.1673. PMID 19920238. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 7.2 "http://www.turner-white.com/pdf/hp_jan03_methods.pdf" (PDF). Retrieved 25 April 2014. External link in
|title=(help)