Pneumoconiosis pathophysiology
|
Pneumoconiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pneumoconiosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Pneumoconiosis pathophysiology |
|
Risk calculators and risk factors for Pneumoconiosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Karol Gema Hernández, M.D. [2], Dushka Riaz, MD
Overview
Pneumoconiosis is an interstitial lung disease caused by the accumulation of different dust particles in the alveolar space. As the particles accumulate, the body's elimination mechanisms begin to fail, resulting in activation of chemotactic factors that exacerbate the inflammatory response, and subsequently leading to fibrosis. [1]
Pathophysiology
Pathogenesis
The pathogenesis of pneumoconiosis starts with the inhalation of mineral, metallic or dust particles. The most common particles that cause pneumoconiosis are:
- Silica (quartz, cristobalite, coesite or tridymite silica polymorphs)
- Structural differences between the polymorphs of silica, are important because of the different degrees of biological reactivity they present, making some of them more toxic than others. The biological reactivity makes quartz more toxic, followed by tridymite, cristobalite, coesite, and finally stishovite. [3] [4] [5]
Other dust particles may also lead to pneumoconiosis, such as hydrated magnesium silicate, hydrous aluminum silicate, bauxite, cobalt, beryllium and iron. [6] [7]
Biological Reactivity of Different Dust Particles
Each dust particle has a different degree of biological reactivity. The dust particles ultimately cause inflammation, fibrosis and finally, irreversible lung disease. [1] This variability is due to properties in the surface of the particles. In the case of silica, there are two theories explaining their biological reactivity. One of them is that silica is a hydrogen donor, whereas biological macromolecules are hydrogen acceptors, creating strong hydrogen bonds that contribute to the damage. The other theory is that at a pH of 7.0 [3], silica is negatively charged, and therefore attracting alveolar macrophages, and activating the generation of reactive oxygen species and cytokines.
Shown below is a table summarizing the dust exposure associated with pneumoconiosis.
| Disease | Dust |
|---|---|
| Coal workers’ pneumoconiosis | Coal dust |
| Silicosis | Silica |
| Asbestosis | Asbestos |
| Talcosis | Hydrated aluminium silicate |
| Kaolin- induced pneumoconiosis | Hydrous aluminum silicate |
| Mixed dust pneumoconiosis | Coal dust, smoke from fires, and silicates |
| Aluminum- induced pneumoconiosis | Bauxite (Al2O3) |
| Berylliosis | Beryllium |
| Silicosiderosis | Silica and iron |
| Hard- metal disease (giant cell pneumonitis) | Cobalt |
When particles reach the distal lung, the mucociliary and lymphatic system take care of their elimination. Dust fibers must be less than 3 μm in diameter in order to penetrate the distal lung. Fibers greater than 5 μm are phagocytosed incompletely and retained in tissues. When particles increase in number, macrophages are activated to engulf those particles. Reticulin is then secreted by fibroblasts to entrap macrophages, as an attempt to control the excess of dust particles. [8]
The physiology of macrophage activation is subject to several theories. The macrophages are mainly derived from peripheral blood monocytes and, from local replication. The recruitment of monocytes from peripheral blood occurs in response to several chemotactic factors. Boitelle et al [9] suggest that one of the most potent chemotactic factors for peripheral blood monocytes is monocyte chemoattractant protein- 1 (MCP- 1), suggesting its role in chronic macrophage inflammation. TNFα activates MCP- 1 expression. MCP-1 is a 76 amino acid peptide that activates monocytes, and also increases its cytostatic activity and the expression of monocyte adhesion molecules such as CD11c/CD18 and CD11b/CD18.
As exposure continues, the elimination system begins to fail, leading to release of reactive oxygen species. These in turn exacerbates the inflammatory response, with the release of more cytokines, such as TNF and interleukins, which subsequently lead to fibrogenesis.
The determinants for the rate of disease progression are the accumulative dose; that is based in duration and intensity of exposure, the fiber type and individual susceptibility.
The underlying pathogenic mechanisms that lead to pulmonary fibrosis in pneumoconiosis remain unclear. Some studies in bronchoalveolar lavage made by Vanhée et al [10] suggest a potential protective effect of TGF- β on the development of pulmonary fibrosis. The alveolar macrophages in coal miners with massive fibrosis, secreted two main profibrotic factors; platelet-derived growth factor (PDGF) and insulin-like growth factor- 1 (IGF-1), whereas, the patients with simple pneumoconiosis secreted transforming- growth factor- β (TGF- β). This suggested a potential protective effect of TGF- β against the development of pulmonary fibrosis.
The risk for pneumoconiosis among constructions workers is evident, but Tjoe et al concluded there is not a clear-cut relationship between exposure and body’s response. This is complex due to the heterogeneity in exposure levels, as well as dust composition and the possible modification of toxicity by other factors present in dust.[11]
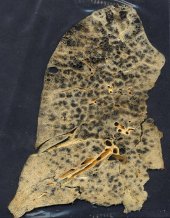
Shown below is an image depicting a lung affected with pneumoconiosis.
Genetics
Pneumoconiosis is caused by environmental exposure. However, acute and more severe forms of the disease do develop in more genetically susceptible people. For example, a study found polymorphism in IL‐1RA (+ 2018) may increase the risk for the development of silicosis. [12]
Associated Conditions
Conditions associated with pneumoconiosis include: [13]
- Asbestosis can cause malignant mesothelioma and bronchogenic carcinoma.
- Silicosis can exacerbate carcinoma and tuberculosis.
- Coal worker's pneumoconiosis can increase the risk of tuberculosis.
Gross Pathology
On gross pathology, pleural plaques are characteristic findings of asbestosis as well as diffuse interstitial pulmonary fibrosis in reticular formation. Coal worker's pneumoconiosis and silicosis both show small interstitial nodules in the upper lung. All pneumoconiosis will present with chronic fibrosis. Silicosis may include eggshell dystrophic calcification. [14]
Microscopic Pathology
On microscopic histopathological analysis, anthrocytes, or dust-laden macrophages are characteristic findings of coal worker's pneumoconiosis. Onion skin lesions with concentrically arranged fibers and a central acellular area are typical of silicosis. In asbestosis, asbestosis bodies appear. Finally, ferruginous bodies are typical for inhalation of inorganic dust with deposition of ferrous materials. [14] [13] [15]
References
- ↑ 1.0 1.1 Farzaneh MR, Jamshidiha F, Kowsarian S (2010). "Inhalational lung disease". Int J Occup Environ Med. 1 (1): 11–20. PMID 23022777.
- ↑ Yang M, Wang D, Gan S, Fan L, Cheng M, Yu L; et al. (2020). "Increasing incidence of asbestosis worldwide, 1990-2017: results from the Global Burden of Disease study 2017". Thorax. 75 (9): 798–800. doi:10.1136/thoraxjnl-2020-214822. PMID 32467338 Check
|pmid=value (help). - ↑ 3.0 3.1 Castranova V, Vallyathan V (2000). "Silicosis and coal workers' pneumoconiosis". Environ Health Perspect. 108 Suppl 4: 675–84. PMC 1637684. PMID 10931786.
- ↑ Lapp NL (1981). "Lung disease secondary to inhalation of nonfibrous minerals". Clin Chest Med. 2 (2): 219–33. PMID 6273058.
- ↑ Merget R, Bauer T, Küpper HU, Philippou S, Bauer HD, Breitstadt R; et al. (2002). "Health hazards due to the inhalation of amorphous silica". Arch Toxicol. 75 (11–12): 625–34. doi:10.1007/s002040100266. PMID 11876495.
- ↑ Cullinan P, Reid P (2013). "Pneumoconiosis". Prim Care Respir J. 22 (2): 249–52. doi:10.4104/pcrj.2013.00055. PMC 6442808. PMID 23708110.
- ↑ "StatPearls". 2021. PMID 32310362 Check
|pmid=value (help). - ↑ Li J, Yao W, Hou JY, Zhang L, Bao L, Chen HT; et al. (2018). "The Role of Fibrocyte in the Pathogenesis of Silicosis". Biomed Environ Sci. 31 (4): 311–316. doi:10.3967/bes2018.040. PMID 29773095.
- ↑ Boitelle A, Gosset P, Copin MC, Vanhee D, Marquette CH, Wallaert B; et al. (1997). "MCP-1 secretion in lung from nonsmoking patients with coal worker's pneumoconiosis". Eur Respir J. 10 (3): 557–62. PMID 9072984.
- ↑ Vanhée D, Gosset P, Boitelle A, Wallaert B, Tonnel AB (1995). "Cytokines and cytokine network in silicosis and coal workers' pneumoconiosis". Eur Respir J. 8 (5): 834–42. PMID 7656959.
- ↑ Tjoe E, Borm P, Hohr D and Heederik D (2002)."Pneumoconiosis and Exposure to Quartz-containing Dust in the Construction Industry". British Occupational Hygiene Society. Vol. 46, Supplement 1, pp. 71–75.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID <286: https://doi.org/10.1002/1097-0274(200103)39:3<286: Check
|pmid=value (help). - ↑ 13.0 13.1 Fujimura N (2000). "Pathology and pathophysiology of pneumoconiosis". Curr Opin Pulm Med. 6 (2): 140–4. doi:10.1097/00063198-200003000-00010. PMID 10741774.
- ↑ 14.0 14.1 Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS (2006). "Pneumoconiosis: comparison of imaging and pathologic findings". Radiographics. 26 (1): 59–77. doi:10.1148/rg.261055070. PMID 16418244.
- ↑ Cohen RA, Petsonk EL, Rose C, Young B, Regier M, Najmuddin A; et al. (2016). "Lung Pathology in U.S. Coal Workers with Rapidly Progressive Pneumoconiosis Implicates Silica and Silicates". Am J Respir Crit Care Med. 193 (6): 673–80. doi:10.1164/rccm.201505-1014OC. PMC 4824937. PMID 26513613.