Pineocytoma
|
WikiDoc Resources for Pineocytoma |
|
Articles |
|---|
|
Most recent articles on Pineocytoma Most cited articles on Pineocytoma |
|
Media |
|
Powerpoint slides on Pineocytoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pineocytoma at Clinical Trials.gov Clinical Trials on Pineocytoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pineocytoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pineocytoma Discussion groups on Pineocytoma Patient Handouts on Pineocytoma Directions to Hospitals Treating Pineocytoma Risk calculators and risk factors for Pineocytoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pineocytoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Sujit Routray, M.D. [2] Aditya Ganti M.B.B.S. [3]
Synonyms and keywords: Pineocytomas; Pinealocytoma; Pinealocytomas; PC; Pineal gland tumor; Brain tumor
Overview
Pineocytoma is a benign, slowly growing pineal parenchymal tumor. The pineal gland, in the brain secretes melatonin which regulates sleep cycle . Pineocytomas most often occur in adults as a solid mass, although they may appear to have fluid-filled (cystic) spaces on images of the brain. Signs and symptoms of pineocytomas include headaches, nausea, vision abnormalities, and Parinaud syndrome. Pineocytomas are usually slow-growing and rarely spread to other parts of the body. Treatment includes surgery to remove the pineocytoma; most of these tumors do not regrow (recur) after surgery.[1]
Classification
The 2007 WHO classification of central nervous system tumors divides pineal gland tumors into four groups:
- Pineocytoma (grade I)
- Pineal parenchymal tumors of intermediate differentiation (grade II or III)
- Papillary tumor of the pineal region (grade II or III)
- Pineoblastoma (grade IV)
According to the WHO classification of tumors of the central nervous system, pineocytoma is classified into a WHO grade I tumor.[2]
Pathophysiology
Pathogenesis
- Due to the pineal gland's location, any tumor or cyst formation would lead to the compression of the aqueduct of Sylvius.
- The aqueduct of Sylvius allows the cerebrospinal fluid to circulate out.
- When there is a blockage in aqueduct of Sylvius by an abnormal pineal gland, the passage of the duct is blocked, and CSF pressure builds up, leading to hydrocephalus.
- Increase in intracranial pressure can even be life-threatening, prompting emergency treatment.
- The hydrocephalus can be relieved by the placement of a VP shunt or ventriculostomy.
- Vision changes would also occur due to an involvement of the tectal region.
- The tectal region helps dictate eye movements.
- Fault in the tectal region causes double vision, an issue with focusing on objects, and eye movement impairment.
- The pineal gland can cause Parinaud syndrome due to the increasing size of the gland compressing the pretectal area and superior colliculi of the midbrain.
- Parinaud syndrome prevents a person from moving his or her eyes up and down.
- The thalamus can be affected, and if so, there can be disturbances on that side of the body which would result in weakness and loss of sensation.
- The tumor's effect on the hypothalamus will lead to weight gain, disruption of sleep, disruption of temperature control, and water regulation.
- Cerebellar involvement would result in motor impairment.
- If the tumor of the pineal gland is present in childhood, then endocrine dysfunctions can also result such as precocious pseudopuberty, diabetes insipidus, and a slowed growth rate.
Gross Pathology
On gross pathology, pineocytoma is characterized by solid, sometimes with focal areas of cystic change, gray, well-circumscribed mass with or without hemorrhage.[3][4]
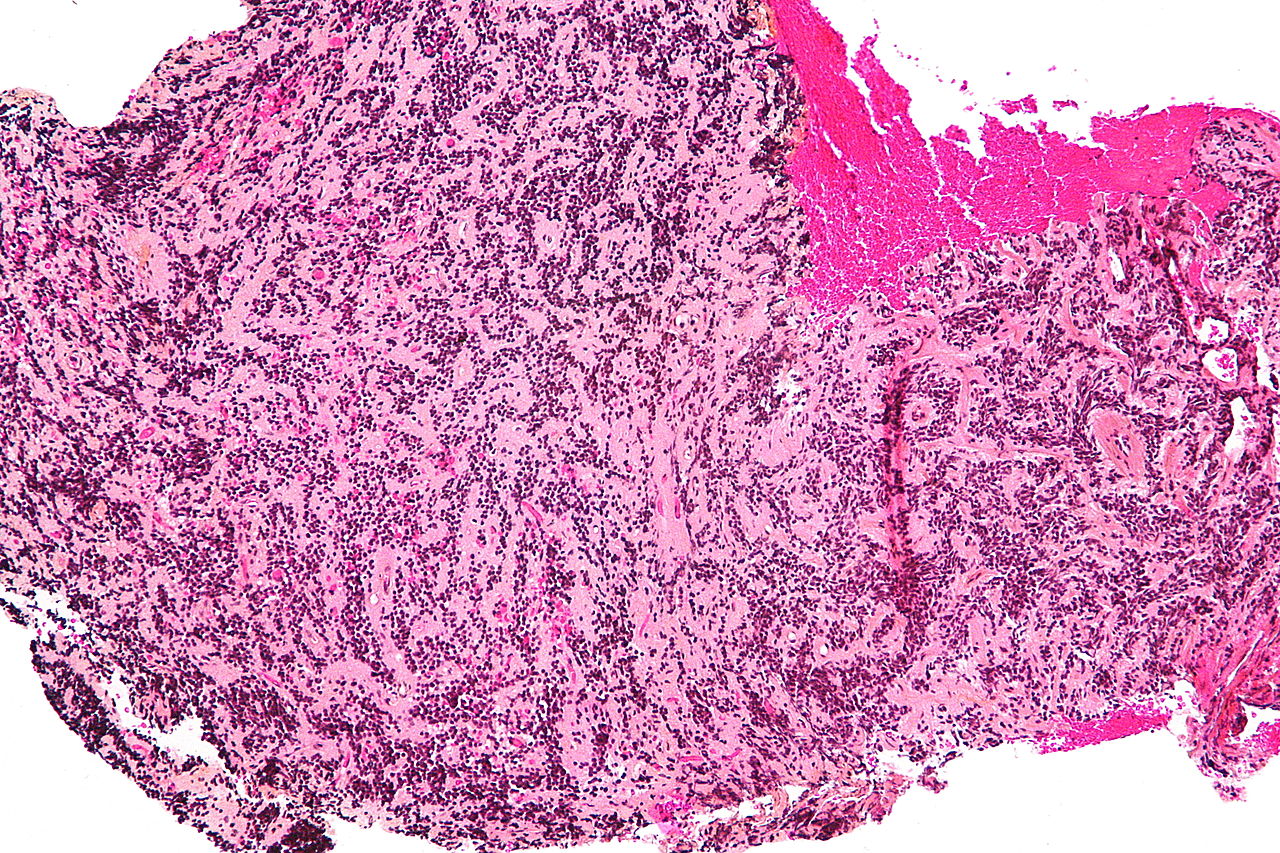
Microscopic Pathology
On microscopic histopathological analysis, pineocytoma is characterized by:[5]
- Cytologically benign cells (uniform size of nuclei, regular nuclear membrane, light chromatin)
- Pineocytomatous/neurocytic rosette, which is an irregular circular/flower-like arrangement of cells with a large meshwork of fibers (neuropil) at the center.
Immunohistochemistry
Pineocytoma is demonstrated by positivity to tumor markers such as:[7][8][9][10]
Differentiating Pineocytoma from other Diseases
Pineocytoma must be differentiated from:[11]
- Pineal parenchymal tumor with intermediate differentiation
- Papillary tumor of the pineal region
- Pineoblastoma
- Pineal germinoma
- Pineal embryonal carcinoma
- Pineal choriocarcinoma
- Pineal yolk sac carcinoma (endodermal sinus tumor)
- Pineal teratoma
- Pineal cyst
- Astrocytoma of the pineal gland
- Meningioma near pineal gland
- Pineal metastasis
- Cavernoma in pineal region
- Aneurysm in pineal region
For differentiating pineal gland tumors from other cranial tumors click here
For differentiating among different types of pineal gland tumors click here
Epidemiology
Prevalence
- Pineocytoma constitutes approximately 45% of the pineal parenchymal tumors.[10][12]
- Pineocytoma constitutes approximately 0.4 - 1% of the intracranial neoplasms.[13]
Age
- Pineocytoma is a rare disease that tends to affect all age groups, most commonly in the second decade of life.[12]
Natural History, Complication and Prognosis
Natural History
If left untreated, patients with pineocytoma may progress to develop seizures, obstructive hydrocephalus, local recurrence, and CSF metastasis.[14][15]
Complications
Common complications of pineocytoma include:[15][10]
- Obstructive hydrocephalus
- Local recurrence
- CSF metastasis
- Distant metastasis (most commonly, lung)
Prognosis
- Prognosis is generally excellent, and the 5-year survival rate of patients with pineocytoma is approximately 86%.[15]
- Pineocytoma has the most favorable prognosis among all the pineal gland tumors.[16]
- Clark et al. after performing a systematic review of the literature reported that the 1- and 5-year progression free survival (PFS) rates for patients that underwent resection versus the biopsy group were 97% and 90%, and 89% and 75% respectively. The 1- and 5-year PFS rates for the gross total resection group versus the group undergoing subtotal resection combined with radiation therapy were 100% and 94%, and 100% and 84% respectively.[17]
Diagnosis
History
When evaluating a patient for pineocytoma, you should take a detailed history of the presenting symptom (onset, duration, and progression), other associated symptoms, and a thorough family and past medical history review.
Symptoms
- The clinical presentation of pineocytoma is mainly from the obstructive hydrocephalus secondary to compression of the tectum of the midbrain and obstruction of the aqueduct.[14]
- Pineal tumors cause neurologic dysfunction by direct invasion, compression, or obstruction of cerebrospinal fluid (CSF) flow.
- The rate of tumor growth determines the rapidity of symptom onset and is an important prognostic factor.
- Pineal gland tumors share some common clinical and radiographic features based upon their anatomic location. Symptoms of pineocytoma include:
- Hydrocephalus is common, manifested by headaches, lethargy, and signs of increased intracranial pressure.
- Progressive local tumor growth may result in cranial neuropathies or hypothalamic dysfunction.
| Symtpoms | Signs |
|---|---|
| Headaches | Papilledema |
| Vision abnormalities | Ataxia |
| Nausea and vomiting | Loss of upward gaze |
| Impaired ambulation | Tremor |
| Altered pupillary reflexes | |
| Hyperactive deep tendon reflexes |
Staging
The staging work-up for pineal tumors include
- Contrast-enhanced MRI of the brain and the entire spine.
- The cerebrospinal fluid (CSF) for cytological examination.
Physical Examination
Compression of the superior colliculi can lead to a characteristic gaze palsy, known as Parinaud syndrome. Common physical examination findings of pineocytoma include:[14]
HEENT
- Bulging soft spots (fontanelles)
- Eyes that are constantly looking down (sunsetting sign)
- Deficiency in upward-gaze
- Pupillary light-near dissociation (pupils respond to near stimuli but not light)
- Convergence-retraction nystagmus
Neurological
Laboratory Diagnosis
There are no specific laboratory findings for pineocytoma. However, the following findings are of significant
- Both serum and CSF should be assayed for alpha-fetoprotein and beta human chorionic gonadotropin (beta-hCG) to help diagnose a germ cell tumor.
- Immunohistochemistry may be of value in detecting these markers or placental alkaline phosphatase.
CT
- Head CT scan may be diagnostic of pineocytoma.
- Findings on CT scan suggestive of pineocytoma include a mass of intermediate density similar to the adjacent brain with peripheral calcifications.[18]

MRI
- Brain MRI may be diagnostic of pineocytoma.
- Features on MRI suggestive of pineocytoma include:[18]
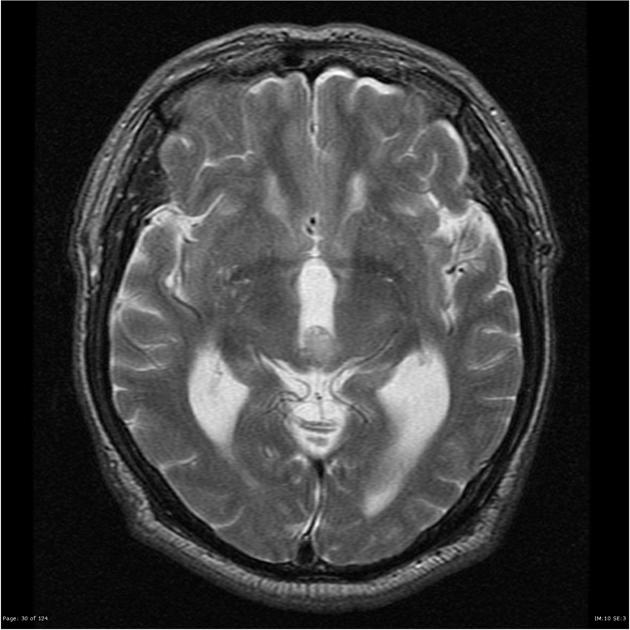
| MRI component | Findings |
|---|---|
|
T1 |
|
|
T2 |
|
|
T1 with gadolinium contrast |
|
Other Diagnostic Studies
Stereotactic biopsy
- A direct, visually guided biopsy of the pineal gland mass with open or neuroendoscopic surgery has been preferred due to concerns about injury to the deep cerebral veins.
- An open procedure also allows CSF to be obtained for
- Tumor marker studies
- Permits direct visualization of the third ventricle for staging purposes
- Sllows a third ventriculostomy to be performed for CSF diversion if needed.
- The diagnostic yield of stereotactic biopsy ranges from 94 to 100 percent.
- If the biopsy is nondiagnostic, equivocal, or suggests a benign tumor such as mature teratoma or meningioma, surgery is recommended to establish a definitive diagnosis or to identify focal areas of malignant disease
Treatment
- The mainstay of therapy for pineocytoma is surgery (gross total or subtotal resection).[15][16][17]
- The treatment of PPTs must be guided by the histologic sub type can be assessed by tissue diagnosis
- Empiric therapy is recommended in nongerminomatous GCT in a patient with characteristic neuroimaging studies and elevated serum or CSF levels of the tumor markers alpha-fetoprotein and/or the beta subunit of human chorionic gonadotropin.
- Empiric therapy for patient with germinoma can be initiated based upon the imaging presence of “bi focal” tumors, CSF beta-hCG <50 mIU/mL, and no elevation of alpha-fetoprotein.
| Management Options of Penial Gland tumors | |
|---|---|
| CSF diversion |
|
| Surgical resection |
|
| Radiation |
|
| Stereotactic radiosurgery |
|
| Chemotherapy as part of multimodality therapy |
|
- Successful treatment of pineocytomas requires surgery with or without RT, while the best results with pineoblastomas are seen with multimodality approaches that include chemotherapy.
- The main goal of open surgery on pineocytoma is the complete tumor removal with minimal morbidity, whenever possible. However, even if gross total excision cannot be achieved, establishment of an accurate diagnosis, maximal cytoreduction, and restoration of the CSF pathway may be achieved.
- Radiotherapy administration to subtotally resected tumor is not associated with an increase in either tumor control or survival.[17]
- Stereotactically guided iodine-125 seed implantation has been proposed as a potential alternative to microsurgery in de novo diagnosed pineocytomas, since it was proven efficient and safe.
- Patients with pineocytoma will develop hydrocephalus in majority of the cases and they will require CSF diversion. Ventriculo-peritoneal (V-P) shunt placement is a viable option with low morbidity and mortality rate. However, shunt malfunction in this population is as high as 20%. In addition, tumor metastasis through a CSF shunt has been reported. Endoscopic third ventriculostomy (ETVC) is an alternative option, which also permits a biopsy of the tumor in the same procedure. Ahn et al. reported that the biopsy samples, obtained in the lateral ventricle or pineal region, were more favorable towards a successful diagnosis than those in the thalamus or tectal region. Neuroendoscopic biopsy procedures have been proven safe with low complication rates.[17]
References
- ↑ Pineocytoma. Wikipedia 2015. https://en.wikipedia.org/wiki/Pineocytoma. Accessed on November 18, 2015
- ↑ General feature of pineocytoma. Libre pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineocytoma. Accessed on November 18, 2015
- ↑ Pathology and radiographic features of pineocytoma. Dr Bruno Di Muzio and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineocytoma. Accessed on November 18, 2015
- ↑ Gross description of pineocytoma. Pathology Outlines 2015. http://pathologyoutlines.com/topic/cnstumorpineocytoma.html. Accessed on November 20, 2015
- ↑ Microscopic features of pineocytoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineocytoma. Accessed on November 18, 2015
- ↑ Microscopic images of pineocytoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineocytoma. Accessed on November 18, 2015
- ↑ Microscopic description of pineocytoma causing hydrocephalus. Dr Frank Gaillard. Radiopaedia 2015. http://radiopaedia.org/cases/pineocytoma-causing-hydrocephalus. Accessed on November 20, 2015
- ↑ Histology of pineocytoma. Dr Frank Gaillard. Radiopaedia 2015. http://radiopaedia.org/cases/pineocytoma-with-astrocytic-differentiation-1. Accessed on November 20, 2015
- ↑ IHC features of pineocytoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineocytoma. Accessed on November 20, 2015
- ↑ 10.0 10.1 10.2 Hirato, Junko; Nakazato, Yoichi (2001). Journal of Neuro-Oncology. 54 (3): 239–249. doi:10.1023/A:1012721723387. ISSN 0167-594X. Missing or empty
|title=(help) - ↑ Differential diagnosis of pineal region mass. Dr Henry Knipe and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineal-region-mass. Accessed on November 20, 2015
- ↑ 12.0 12.1 Epidemiology of pineocytoma. Dr Bruno Di Muzio and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineocytoma. Accessed on November 20, 2015
- ↑ Clark, Aaron J.; Sughrue, Michael E.; Aranda, Derick; Parsa, Andrew T. (2011). "Contemporary Management of Pineocytoma". Neurosurgery Clinics of North America. 22 (3): 403–407. doi:10.1016/j.nec.2011.05.004. ISSN 1042-3680.
- ↑ 14.0 14.1 14.2 Clinical presentation of pineocytoma. Dr Bruno Di Muzio and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineocytoma. Accessed on November 20, 2015
- ↑ 15.0 15.1 15.2 15.3 Treatment and prognosis of pineocytoma. Dr Bruno Di Muzio and Dr Frank Gaillard et al. Radiopaedia 2015.http://radiopaedia.org/articles/pineocytoma. Accessed on November 20, 2015
- ↑ 16.0 16.1 Deshmukh, Vivek R.; Smith, Kris A.; Rekate, Harold L.; Coons, Stephen; Spetzler, Robert F. (2004). "Diagnosis and Management of Pineocytomas". Neurosurgery. 55 (2): 349–357. doi:10.1227/01.NEU.0000129479.70696.D2. ISSN 0148-396X.
- ↑ 17.0 17.1 17.2 17.3 Alexiou, George A (2012). "Management of pineal region tumours in children". Journal of Solid Tumors. 2 (2). doi:10.5430/jst.v2n2p15. ISSN 1925-4075.
- ↑ 18.0 18.1 Radiographic features of pineocytoma. Dr Bruno Di Muzio and Dr Frank Gaillard et al. Radiopeadia 2015. http://radiopaedia.org/articles/pineocytoma. Accessed on November 20, 2015
- ↑ Image courtesy of Dr. Frank Gaillard. Radiopaedia (original file here). Creative Commons BY-SA-NC