Phenobarbital (injection)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Phenobarbital (injection) is an anticonvulsant that is FDA approved for the treatment of preanesthetic, sedative, hypnotic. Common adverse reactions include somnolence, syncope, megaloblastic anemia, liver damage,hypersensitivity and angioedema.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Parenteral
Sedative
- Sedation is obtainable within an hour, and in adequate dosage, the duration of action is more than six hours. Included in the more common conditions in which the sedative action of this class of drugs is desired are anxiety-tension states, hyperthyroidism, essential hypertension, nausea and vomiting of functional origin, motion sickness, acute labyrinthitis, pylorospasm in infants, chorea and cardiac failure.
- Phenobarbital is also a useful adjunct in treatment of hemorrhage from the respiratory or gastrointestinal tract. Phenobarbital controls anxiety, decreases muscular activity and lessens nervous excitability in hyperthyroid patients. However, thyrotoxic individuals occasionally react poorly to barbiturates.
- Hypnotic, for the short-term treatment of insomnia, since it appears to lose its effectiveness for sleep induction and sleep maintenance after 2 weeks.
Preanesthetic
- Long-term anticonvulsant, (phenobarbital, mephobarbital and metharbital) for the treatment of generalized tonic-clonic and cortical focal seizures. And, in the emergency control of certain acute convulsive episodes, e.g., those associated with status epilepticus, cholera, eclampsia, cerebral hemorrhage, meningitis,tetanus, and toxic reactions to strychnine or local anesthetics.
- Phenobarbital sodium may be administered intramuscularly or intravenously as an anticonvulsant for emergency use. When administered intravenously, it may require 15 or more minutes before reaching peak concentrations in the brain. Therefore, injecting phenobarbital sodium until the convulsions stop may cause the brain level to exceed that required to control the convulsions and lead to severe barbiturate-induced depression.
- Phenobarbital is indicated in pediatric patients as an anticonvulsant and as a sedative, including its preoperative and postoperative use.
Adult Dosage
(intended as a guide)
- Daytime Sedation
- 30 to 120 mg daily in 2 to 3 divided doses IM or IV
- Bedtime Hypnosis: 100 to 320 mg IM or IV
- Preoperative Sedation: IM only — 100 to 200 mg 60 to 90 minutes before surgery
- Acute Convulsions: 20 to 320 mg IM or IV, repeated in 6 hours as necessary
- Parenteral routes should be used only when oral administration is impossible or impractical.
- Intramuscular injection of the sodium salts of barbiturates should be made deeply into a large muscle and a volume of 5 mL should not be exceeded at any one site because of possible tissue irritation.
- Injection into or near peripheral nerves may result in permanent neurological deficit. After intramuscular injection of a hypnotic dose, the patient’s vital signs should be monitored.
- Subcutaneous administration is not recommended.
Intravenous Administration
- Intravenous injection is restricted to conditions in which other routes are not feasible, either because the patient is unconscious (as in cerebral hemorrhage, eclampsia or status epilepticus), or because the patient resists (as in delirium) or because prompt action is imperative. Slow IV injection is essential, and patients should be carefully observed during administration. This requires that blood pressure, respiration and cardiac function be maintained, vital signs be recorded and equipment for resuscitation and artificial ventilation be available.
- The rate of intravenous injection for adults should not exceed 60 mg/min for phenobarbital sodium.
- When given intravenously, do not use small veins, such as those on the dorsum of the hand or wrist. Preference should be given to a larger vein to minimize the risk of irritation with the possibility of resultant thrombosis. Avoid administration into varicose veins because circulation there is retarded. Inadvertent injection into or adjacent to an artery has resulted in gangrene requiring amputation of an extremity or a portion thereof. Careful technique, including aspiration, is necessary to avoid inadvertent intraarterial injection.
- Treatment of Adverse Effects Due to Inadvertent Error in Administration
- Extravasation into subcutaneous tissues causes tissue irritation. This may vary from slight tenderness and redness to necrosis.
- Recommended treatment includes the application of moist heat and the injection of 0.5% procaine solution into the affected area.
- Intraarterial injection of any barbiturate must be avoided. The accidental intraarterial injection of a small amount of the solution may cause spasm and severe pain along the course of the artery.
- The injection should be terminated if the patient complains of pain or if other indications of accidental intraarterial injection occur, such as a white hand with cyanosed skin or patches of discolored skin and delayed onset of hypnosis.
- The consequences of intraarterial injection of phenobarbital can vary from transient pain to gangrene. It is not possible to formulate strict rules for management of such accidents. The following procedures have been suggested: 1) release of the tourniquet or restrictive garments to permit dilution of injected drug, 2) relief of arterial spasm by injecting 10 mL of a 1% procaine solution into the artery and, if considered necessary, brachial plexus block, 3) prevention of thrombosis by early anticoagulant therapy and 4) supportive treatment.
Anticonvulsant Use
- A therapeutic anticonvulsant level of phenobarbital in the serum is 10 to 25 µg/mL. To achieve the blood levels considered therapeutic in children, higher per-kilogram dosages are generally necessary for phenobarbital and most other anticonvulsants. In children and infants, phenobarbital at loading doses of 15 to 20 mg/kg produces blood levels of about 20 µg/mL shortly after administration.
- In status epilepticus, it is imperative to achieve therapeutic blood levels of a barbiturate (or other anticonvulsants) as rapidly as possible. When administered intravenously, phenobarbital sodium may require 15 minutes or more to attain peak concentrations in the brain. If phenobarbital sodium is injected continuously until the convulsions stop, the brain concentration will continue to rise and can eventually exceed that required to control the seizures.
- Because a barbiturate-induced depression may occur along with a postictal depression once the seizures are controlled, it is important, therefore, to use the minimal amount required and to wait for the anticonvulsant effect to develop before administering a second dose.
- Phenobarbital has been used in the treatment and prophylaxis of febrile seizures. However, it has not been established that prevention of febrile seizures influences the subsequent development of epilepsy.
Special Patient Population
- Dosage should be reduced in the elderly or debilitated because these patients may be more sensitive to barbiturates. Dosage should be reduced for patients with impaired renal function or hepatic disease.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- This drug has not been found by the US Food and Drug Administration (FDA) to be safe and effective, and the drug product labeling has not been approved by the FDA
discontinuation dosing, decrease the daily phenobarbital dosage by 10%, if tolerated, and monitor carefully
- Average dose, 100 to 320 mg slow IV or IM; larger doses may be required in patients with status epilepticus; MAX, 600 mg/24 hr
- Insomnia, Short-term management
- Average dose, 100 to 320 mg slow IV or IM; repeat if necessary up to a total MAX dose of 600 mg/24 hr.
- Sedation, To relieve anxiety, tension or apprehension: average dose, 100 to 320 mg slow IV or IM; repeat if necessary up to a MAX dose of 600 mg/24 hrs.
- Seizure, Emergency control of acute convulsions: average dose, 100 to 320 mg slow IV or IM; larger doses may be required in patients with status epilepticus; MAX, 600 mg/24 hr.
- Status epilepticus, For emergency use: average dose, 100 to 320 mg slow IV or IM; larger doses may be required in patients with status epilepticus; MAX, 600 mg/24 hr.
Non–Guideline-Supported Use
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Pediatric Dosage
- Recommended by the American Academy of Pediatrics (intended as a guide)
- Preoperative Sedation: 1 to 3 mg/kg IM or IV
- Anticonvulsion: 4 to 6 mg/kg/day for 7 to 10 days to blood level of 10 to 15 mcg/mL or 10 to 15 mg/kg/day IM or IV
- Status Epilepticus: 15 to 20 mg/kg over 10 to 15 minutes IV
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- Status epilepticus, For emergency use: loading dose, 20 mg/kg IV infused no faster than 60 to 100 mg/min, followed by a maintenance dose of 5 mg/kg IV given at 12 and 24 hours after the loading dose was used in a clinical trial (n=60).[1]
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Phenobarbital in pediatric patients.
Contraindications
- Barbiturates are contraindicated in patients with known barbiturate sensitivity. Barbiturates are also contraindicated in patients with a history of manifest or latent porphyria, marked impairment of liver functions or with severe respiratory distress where dyspnea or obstruction is evident. Large doses are contraindicated in nephritic subjects.
- Barbiturates should not be administered to persons with known previous addiction to the sedative-hypnotic group since ordinary doses may be ineffectual and may contribute to further addiction.
- Intraarterial administration is contraindicated. Its consequences vary from transient pain to gangrene. Subcutaneous administration produces tissue irritation, ranging from tenderness and redness to necrosis and is not recommended.
Warnings
- Phenobarbital Sodium Injection contains the preservative benzyl alcohol and is not recommended for use in neonates. There have been reports of fatal ‘gasping syndrome’ in neonates (children less than one month of age) following the administration of intravenous solutions containing the preservative benzyl alcohol.
- Symptoms include a striking onset of gasping respiration, hypotension, bradycardia, and cardiovascular collapse.
Habit Forming
- Barbiturates may be habit forming. Tolerance and psychological and physical dependence may occur with continued use.
- Patients who are psychologically dependent on barbiturates may increase the dosage or decrease the dosage interval without consulting a physician and may subsequently develop a physical dependence on barbiturates.
- To minimize the possibility of overdosage or the development of dependence, the prescribing and dispensing of sedative-hypnotic barbiturates should be limited to the amount required for the interval until the next appointment.
- Abrupt cessation after prolonged use in the dependent person may result in withdrawal symptoms, including delirium, convulsions and possibly death. Barbiturates should be withdrawn gradually from any patient known to be taking excessive dosage over long periods of time.
Dermatologic Reactions
- Exfoliative dermatitis and Stevens-Johnson syndrome, possibly fatal, are rare hypersensitivity reactions to phenobarbital. Physicians should be alert to signs which may precede the onset of barbiturate-induced cutaneous lesions, and the drug should be discontinued whenever dermatological reactions occur.
Intravenous Administration
- Too rapid administration may cause severe respiratory depression, apnea, laryngospasm, hypertension or vasodilation with fall in blood pressure.
- When administered intravenously, it may require 15 or more minutes before reaching peak concentrations in the brain. Therefore, injecting phenobarbital sodium until the convulsions stop may cause brain levels to exceed that required to control the convulsions and lead to severe barbiturate-induced depression.
Acute or Chronic Pain
- Caution should be exercised when barbiturates are administered to patients with acute or chronic pain, because paradoxical excitement could be induced or important symptoms could be masked. However, the use of barbiturates as sedatives in the postoperative surgical period and as adjuncts to cancer chemotherapy is well established.
Use in Pregnancy
- Barbiturates can cause fetal harm when administered to a pregnant woman. Retrospective, case-controlled studies have suggested a connection between the maternal consumption of barbiturates and a higher than expected incidence of fetal abnormalities. Phenobarbital may cause major fetal malformations.
- Following oral or parenteral administration, barbiturates readily cross the placental barrier and are distributed throughout fetal tissues with highest concentrations found in the placenta, fetal liver and brain. Fetal blood levels approach maternal blood levels following parenteral administration.
- Withdrawal symptoms occur in infants born to mothers who receive barbiturates throughout the last trimester of pregnancy.
- Phenobarbital should be used during pregnancy only whenclearly indicated. If phenobarbital is used during pregnancy or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential hazard to the fetus.
Use in Children
- Phenobarbital has been reported to be associated with cognitive defects in children taking it for complicated febrile seizures.
Synergistic Effects
- The concomitant use of alcohol or other CNS depressants may produce additive CNS depressant effects.
Adverse Reactions
Clinical Trials Experience
There is limited information regarding Phenobarbital (injection) Clinical Trials Experience in the drug label.
Postmarketing Experience
- The following adverse reactions and their incidence were compiled from surveillance of thousands of hospitalized patients. Because such patients may be less aware of certain of the milder adverse effects of barbiturates, the incidence of these reactions may be somewhat higher in fully ambulatory patients.
Nervous System
- Somnolence, agitation, confusion, hyperkinesia, ataxia, CNS depression, nightmares, nervousness, psychiatric disturbance, hallucinations, insomnia, anxiety, dizziness, thinking abnormality
Respiratory System
- Hypoventilation, apnea
Cardiovascular System
- Bradycardia, hypotension, syncope
Digestive System
Dermatologic Reactions
Other Reported Reactions
- Headache; injection site reactions; hypersensitivity reactions, including but not limited to angioedema and skin rashes; fever; liver damage and megaloblastic anemia following chronic phenobarbital use.
Drug Interactions
There is limited information regarding Phenobarbital (injection) Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Phenobarbital (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Phenobarbital (injection) during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Phenobarbital (injection) with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Phenobarbital (injection) with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Phenobarbital (injection) with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Phenobarbital (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Phenobarbital (injection) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Phenobarbital (injection) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Phenobarbital (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Phenobarbital (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Phenobarbital (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Monitoring
- Monitoring of vital signs and fluid balance.
IV Compatibility
There is limited information regarding IV Compatibility of Phenobarbital (injection) in the drug label.
Overdosage
- The toxic dose of barbiturates varies considerably. Barbiturate intoxication may be confused with alcoholism, bromide intoxication and various neurological disorders.
- For sedation, therapeutic blood levels of phenobarbital range from 5-40 µg/mL; the lethal blood level is greater than 80 µg/mL and usually ranges from 100-200 µg/mL.
- Acute overdosage with barbiturates is manifested by CNS and respiratory depression which may progress to Cheyne-Stokes respiration, areflexia, constriction of the pupils to a slight degree (though in severe poisoning, they may show paralytic dilation),oliguria, tachycardia, hypotension, lowered body temperature and coma. Typical shock syndrome (apnea, circulatory collapse, respiratory arrest and death) may occur.
- In extreme overdose, all electrical activity in the brain may cease, in which case a “flat” EEG normally equated with clinical death cannot be accepted. This effect is fully reversible unless hypoxic damage occurs. Consideration should be given to the possibility of barbiturate intoxication even in situations that appear to involve trauma.
- Complications such as pneumonia, pulmonary edema, cardiac arrhythmias, congestive heart failure and renal failure may occur. Uremia may increase CNS sensitivity to barbiturates if renal function is impaired. Differential diagnosis should include hypoglycemia, head trauma, cerebrovascular accidents, convulsive states and diabetic coma. To obtain up-to-date information about the treatment of overdosage, a good resource is your certified Regional Poison Control Center. Telephone numbers of certified poison control centers are listed in the Physicians’ Desk Reference (PDR). In managing overdosage, consider the possibility of multiple drug overdose, interaction among drugs and the unusual drug kinetics in your patient.
- Treatment of overdosage is mainly supportive and consists of the following:
- Maintenance of an adequate airway, with assisted respiration and oxygen administration as necessary.
- Monitoring of vital signs and fluid balance.
- Fluid therapy and other standard treatment for shock, if needed.
- If renal function is normal, forced diuresis may aid in the elimination of the barbiturate. Alkalinization of the urine increases renal excretion of phenobarbital.
- Although not recommended as a routine procedure, hemodialysis may be used in severe barbiturate intoxication or if the patient is anuric or in shock. Hemoperfusion through an anion-exchange resin or activated charcoal has been successful. Peritoneal dialysis is significantly less effective in removing barbiturates.
- Patient should be rolled from side to side every 30 minutes.
- Antibiotics should be given if pneumonia is suspected.
- Appropriate nursing care to prevent hypostatic pneumonia, decubiti, aspiration and other complications of patients with altered states of consciousness.
- The use of analeptic agents is not recommended.
Pharmacology
| |
| |
Phenobarbital (injection)
| |
| Systematic (IUPAC) name | |
| 5-ethyl-5-phenylpyrimidine-2,4,6(1H,3H,5H)-trione | |
| Identifiers | |
| CAS number | |
| ATC code | N05 N03AA02 (WHO) |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 232.235 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | >95% |
| Protein binding | 20 to 45% |
| Metabolism | Hepatic (mostly CYP2C19) |
| Half life | 53 to 118 hours |
| Excretion | Renal and fecal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status | |
| Dependence Liability | High |
| Routes | Oral, rectal, parenteral (intramuscular and intravenous) |
Mechanism of Action
There is limited information regarding Phenobarbital (injection) Mechanism of Action in the drug label.
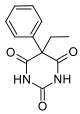
Structure
- The barbiturates are nonselective central nervous system (CNS) depressants which are primarily used as sedative hypnotics and also anticonvulsants in subhypnotic doses. The barbiturates and their sodium salts are subject to control under the Federal Controlled Substances Act (CIV).
- Barbiturates are substituted pyrimidine derivatives in which the basic structure common to these drugs is barbituric acid, a substance which has no central nervous system activity. CNS activity is obtained by substituting alkyl, alkenyl or aryl groups on the pyrimidine ring.
- Phenobarbital Sodium Injection, USP is a sterile solution for intramuscular or slow intravenous administration as a long-acting barbiturate. Each mL contains phenobarbital sodium either 65 mg or 130 mg, alcohol 0.1 mL, propylene glycol 0.678 mL and benzyl alcohol 0.015 mL in Water for Injection; hydrochloric acid added, if needed, for pH adjustment. The pH range is 9.2-10.2.
- Chemically, phenobarbital sodium is 2,4,6(1H,3H,5H)-Pyrimidinetrione,5-ethyl-5-phenyl-, monosodium salt and has the following structural formula:
Pharmacodynamics
- Barbiturates are capable of producing all levels of CNS mood alteration from excitation to mild sedation, to hypnosis and deep coma. Overdosage can produce death. In high enough therapeutic doses, barbiturates induce anesthesia.
- Barbiturates depress the sensory cortex, decrease motor activity, alter cerebellar function and produce drowsiness, sedation and hypnosis.
- Barbiturate-induced sleep differs from physiological sleep. Sleep laboratory studies have demonstrated that barbiturates reduce the amount of time spent in the rapid eye movement (REM) phase of sleep or dreaming stage. Also, Stages III and IV sleep are decreased. Following abrupt cessation of barbiturates used regularly, patients may experience markedly increased dreaming, nightmares and/or insomnia. Therefore, withdrawal of a single therapeutic dose over 5 or 6 days has been recommended to lessen the REM rebound and disturbed sleep which contribute to drug withdrawal syndrome (for example, decrease the dose from 3 to 2 doses a day for 1 week).
- In studies, secobarbital sodium and pentobarbital sodium have been found to lose most of their effectiveness for both inducing and maintaining sleep by the end of 2 weeks of continued drug administration even with the use of multiple doses. As with secobarbital sodium and pentobarbital sodium, other barbiturates might be expected to lose their effectiveness for inducing and maintaining sleep after about 2 weeks. The short-, intermediate- and, to a lesser degree, long-acting barbiturates have been widely prescribed for treating insomnia. Although the clinical literature abounds with claims that the short-acting barbiturates are superior for producing sleep while the intermediate-acting compounds are more effective in maintaining sleep, controlled studies have failed to demonstrate these differential effects. Therefore, as sleep medications, the barbiturates are of limited value beyond short-term use.
- Barbiturates have little analgesic action at subanesthetic doses. Rather, in subanesthetic doses these drugs may increase the reaction to painful stimuli. All barbiturates exhibit anticonvulsant activity in anesthetic doses.
- Barbiturates are respiratory depressants by virtue of their direct effect on the medullary respiratory center. They diminish and, in high doses, may abolish the sensitivity of the respiratory center to its normal stimulus, carbon dioxide. The degree of respiratory depression is dependent upon dose. With hypnotic doses, respiratory depression produced by barbiturates is similar to that which occurs during physiologic sleep with slight decrease in blood pressure and heart rate.
- Ordinary hypnotic doses of barbiturates have no significant effect on the cardiovascular system. The barbiturates tend to decrease the tonus of the gastrointestinal musculature. They have no direct injurious effect on the normal kidney. Severe oliguria or anuria may occur in acute barbiturate poisoning, largely as a result of the marked hypotension.
- Hypnotic doses tend to reduce slightly the metabolic rate in man. Body temperature is reduced slightly, owing to lessened activity and to depression of the central temperature-regulatory mechanisms.
- While anesthetic doses of all barbiturates exert an anticonvulsant effect, phenobarbital has a selective anticonvulsant activity independent of the degree of sedation produced. Phenobarbital limits the spread of seizures and raises the seizure threshold in grand mal (generalized tonic-clonic) epilepsy.
- Studies in laboratory animals have shown that barbiturates cause reduction in the tone and contractility of the uterus, ureters and urinary bladder. However, concentrations of the drugs required to produce this effect in humans are not reached with sedative-hypnotic doses.
- Barbiturates do not impair normal hepatic function, but have been shown to induce liver microsomal enzymes, thus increasing and/or altering the metabolism of barbiturates and other drugs.
- Following IV administration, the onset of action is 5 minutes for phenobarbital sodium. For IM administration, the onset of action is slightly slower. Maximal CNS depression may not occur until 15 minutes or more after IV administration.
- Duration of action, which is related to the rate at which the barbiturates are redistributed throughout the body, varies among persons and in the same person from time to time.
- No studies have demonstrated that the different routes of administration are equivalent with respect to bioavailability.
- Barbiturates are weak acids that are absorbed and rapidly distributed to all tissues and fluids with high concentrations in the brain, liver and kidneys. Lipid solubility of the barbiturates is the dominant factor in their distribution within the body. The more lipid soluble the barbiturate, the more rapidly it penetrates all tissues of the body. Barbiturates are bound to plasma and tissue proteins to a varying degree with the degree of binding increasing directly as a function of lipid solubility.
- Phenobarbital has the lowest lipid solubility, lowest plasma binding, lowest brain protein binding, the longest delay in onset of activity and the longest duration of action. Its diffusion across the blood-brain barrier and its distribution into other tissues occurs more slowly than with other short-acting barbiturates. Fifteen minutes or more may be required for maximal central depression following intravenous administration of phenobarbital. However, with time, phenobarbital distributes into all tissues and fluids. Barbiturates are known to cross the placenta. Phenobarbital is 20-45% protein bound. In adults, the plasma half-life of phenobarbital is 53 to 118 hours (mean 79 hours) and in children/newborns, the plasma half-life is 60 to 180 hours (mean 110 hours).
- Barbiturates are metabolized primarily by the hepatic microsomal enzyme system, and the metabolic products are excreted in the urine and, less commonly, in the feces. Approximately 25 to 50 percent of a dose of phenobarbital is eliminated unchanged in the urine, whereas the amount of other barbiturates excreted unchanged in the urine is negligible. Urinary pH and rate of urine flow affect the renal circulation of unchanged phenobarbital, a greater quantity being eliminated in alkaline urine and at increased flow rates. The excretion of unmetabolized barbiturate is one feature that distinguishes the long-acting category from those belonging to other categories which are almost entirely metabolized. The inactive metabolites of the barbiturates are excreted as conjugates of glucuronic acid.
Pharmacokinetics
Phenobarbital has an oral bioavailability of about 90%. Peak plasma concentrations are reached eight to 12 hours after oral administration. It is one of the longest-acting barbiturates available – it remains in the body for a very long time (half-life of two to seven days) and has very low protein binding (20 to 45%). * Phenobarbital is metabolized by the liver, mainly through hydroxylation and glucuronidation, and induces many isozymes of the cytochrome P450 system. Cytochrome P450 2B6 (CYP2B6) is specifically induced by phenobarbital via the CAR/RXR nuclear receptor heterodimer. It is excreted primarily by the kidneys.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Phenobarbital (injection) in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Phenobarbital (injection) in the drug label.
How Supplied
- Phenobarbital Sodium Injection, USP is available in the following:
- 65 mg/mL, 1 mL vials packaged in 25s (NDC 0641-0476-25)
- 130 mg/mL, 1 mL vials packaged in 25s (NDC 0641-0477-25)
Storage
- Store at 20°-25°C (68°-77°F), excursions permitted to 15°-30°C (59°-86°F).
- Do not use if solution is discolored or contains a precipitate.
Images
Drug Images
{{#ask: Page Name::Phenobarbital (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel







{{#ask: Label Page::Phenobarbital (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Phenobarbital (injection) in the drug label.
Precautions with Alcohol
- Alcohol-Phenobarbital (injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- PHENOBARBITAL SODIUM®[2]
Look-Alike Drug Names
There is limited information regarding Phenobarbital (injection) Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Malamiri RA, Ghaempanah M, Khosroshahi N, Nikkhah A, Bavarian B, Ashrafi MR (2012). "Efficacy and safety of intravenous sodium valproate versus phenobarbital in controlling convulsive status epilepticus and acute prolonged convulsive seizures in children: a randomised trial". Eur J Paediatr Neurol. 16 (5): 536–41. doi:10.1016/j.ejpn.2012.01.012. PMID 22326977 PMID: 22326977 Check
|pmid=value (help). - ↑ "PHENOBARBITAL SODIUM- phenobarbital sodium injection".
