Abdominal pain in children
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief:
Synonyms and keywords: Abdominal pain in kids
Overview
Abdominal pain in children is a common presenting symptom in pediatrics primary care. There's multiple causes of abdominal pain that require different types of investigations and treatment options.
Historical Perspective
- Celiac disease was first discovered by Dutch pediatricians, in late 1940s[1].
- In late 1980s, the first classification and diagnostic criteria for functional gastrointestinal disorders was developed by a group of international experts were recruited by Professor Aldo Torsoli from Italy to develop Working Teams for the International Gastroenterology meeting in Rome 1988 to the goal was to answer difficult questions using a consensus methodology through the Delphi approach about a group of gastrointestinal disorders that had little scientific-based evidence to understand etiology pathophysiology and treatment at the time[2].
- In May of 2016, after Rome III had been in effect for a decade, Rome IV was released[3]. It is a result of collective work by committees that included more than 100 leading functional GI experts[3].
Classification
- Abdominal pain in children may be classified according to age into two groups:[4]
- Other method for classification of abdominal pain can be according to the duration of the pain[5]:
- Acute Abdominal pain(less than 1 week).
- Chronic Abdominal pain(more than 1 week).
Pathophysiology
- The pathogenesis of abdominal pain is related to either insult to intra-abdominal structures or extra-abdominal structure. Also it can be due to injury to somatic structures that's overlay the abdominal wall [6].
- On Summary the pathophysiology of abdominal pain maybe due to :
- Visceral Pain:
- Result when there's a damage to nerve within the abdomen.[6]
- Due to the fact that visceral nerve fibers that responsible for pain sensation are non-myelinated, the visceral pain is Vague, dull, poorly localized and slow on onset.[6]
- Different types of stimuli including chemical, osmotic and even normal peristalsis can stimulate these fibers.[6]
- Visceral pain is always sensed when the threshold of intensity or duration is reached.[6]
- Mild stimuli may result in sensing non-painful or vaguely un-comfortable sensation, in contrast to powerful stimulation to visceral nerve fibers which causes pain.[6]
- Example for pain caused due to over-sensation of visceral nerve fibers is functional abdominal pain.[6]
- Somatic Pain:
- Due to insult to somatic structures(parietal peritoneum, fascia, muscles, and skin of the abdominal wall).[6].
- Somatic nerve fibers are myelinated that can rapidly transmit well localized painful stimuli[6].
- Visceral pain can progress to somatic pain when the insult from intra-abdominal structures progress to affect the somatic structures(for example parietal peritoneum)as happens in acute appendicitis which start as visceral pain after that it progress to somatic pain.[6].
- Referred Pain:
- Pain sensation that referred from other site on the body.[6].
- This occur due to stimulation of spinal cord somatic sensory cell bodies which activated by stimuli from visceral afferent fibers, which located on the same level on the spinal cord[6].
- Visceral Pain:
Causes
There is a wide range of causes for pediatric abdominal pain which maybe due to a disease in variety of systems. In general, differentiating between acute and chronic pain in children is not easy, Despite it's being benign conditions in most children presenting with abdominal pain but some serious conditions may be the cause of the abdominal pain. On the table below there's some systems and related diseases that can cause abdominal pain in children:[7]
| System | Disesease |
|---|---|
| Gastrointestinal | Appendicitis[8], Gastrointestinal reflux disease[9], constipation [9],irritable bowel syndrome[10], celiac disease [11],Meckel's diverticulum[12], Intussusception[13], Volvulus[14].functional dyspepsia (FD)[15], abdominal migraine (AM)[15], functional abdominal pain (FAP) and functional abdominal pain syndrome (FAPS)[15] |
| Genitourinary | Nephrolithiasis[16] , urinary tract infection[17]. |
| Infections | viral (mesenteric adenitis)[18], gastroenteritis[19],Multisystem Inflammatory Syndrome in Children (MIS-C) caused by covid-19[20] |
| Gynecologic | Dysmenorrhea.[21] |
| Psychology | Anxiety [22] |
| Others | Toxins (lead poising)[23] , Sickle cell disease[24]. |
Differentiational Diagnosis of Abdominal Pain Children
For further information about the differential diagnosis, click abdominal pain differential diagnosis.
Epidemiology and Demographics
- The pooled prevalence of abdominal pain in children is approximately 13.5% per 196,472 individuals worldwide.[15]
- Abdominal pain is about 5% of presented cases in pediatrics, surgery is required only in 7% of cases, and non-specific diagnosis in up to 15%[25].
- In 2001,the incidence of nonspecific abdominal pain was estimated to be 25% cases per 1,000 individuals in Netherland.[26]
- Incidence of appendicitis is 11/10,000 population per year[27]
- At least,20% of children present with abdominal pain,5% of them need hospitalization[28].
Age
- Age can help in differentiating causes of abdominal pain:[29]:
- Neonates and infants:
- Most common presentation in this age group is due to congenital anomalies and prematurity. For example Necrotizing enterocolitis and Meckel's diverticulum, Hirschsprung's disease, volvulus, stenosis or congenial atresia causing intestinal obstruction. Also intussusception can cause abdominal pain in this age group[30].
- School-age children:
- Most common causes of abdominal pain in this age group are idiopathic constipation and infectious causes. other causes may include functional abdominal pain and abdominal migraine.[30]
- Adolescents:
- In female adolescents causes related to menstruation, ovarian torsion and pregnancy might be the underlying cause of the pain[30].
- In male adolescents testicular torsion should be considered[30].
- Other causes to consider in both genders that's cause abdominal pain in this age group include irritable bowel syndrome, sexually transmitted diseases and inflammatory bowel disease[30].
- Neonates and infants:
Gender
- Females are more commonly affected with abdominal pain than males.[31]
- Appendicitis male to female ratio is (1.4:1) with life time risk of 8.6% in males and 6.7% in females[27]
Race
- There is no racial predilection for abdominal pain in children
Risk Factors
- Common risk factors in the development of abdominal pain in children:
- Anxiety , preceding emotional or physical trauma and prior gastrointestinal infection are risk factors for functional abdominal [32]
- Some environmental factors along with specific genetic predisposition are linked to crohn's disease.[33]
Natural History, Complications and Prognosis
- Abdominal pain is a common presenting symptom in pediatrics primary care. Most of times it's due to benign causes without risk for complications, but severe abdominal pain maybe an alarming sign for abdominal pathology that requires surgical intervention[34]
- Early clinical features of acute appendicitis include pain that's start in the middle of the abdomen and radiate to the right iliac fossa, followed y fever and vomiting[35].
- Prognosis of infantile colic is generally good,One self-reporting parent questionnaire on crying patterns found that 29% of infants aged 1 to 3 months cried for more than 3 hours a day, but the estimated prevalence of the age of 4 to 6 months found to be between 7% to 11%[36].
Diagnosis
Diagnostic Criteria
- The diagnosis of appendicitis is made with Pediatrics Appendicitis score[37] :
| Variable | Score |
|---|---|
| Pain migrating to right lower quadrant | 1 |
| Anorexia | 1 |
| Nausea/vomiting | 1 |
| Fever>38 | 1 |
| Right Iliac Fossa Pain | 2 |
| Pain with Cough/Percussion/Hopping | 2 |
| White Blood Cell Count>10,000 cells/ml | 1 |
| Neutrophils count>7,500 | 1 |
| Total score | 10 |
- If the score is 5 or less: Appendicitis is less likely or excluded, If the score is more than 5: Appendicitis is high likely to be the diagnosis[38].
- The diagnosis of Functional abdominal pain is established by using New Rome IV Criteria[39]:
- All aspects of criteria must be reached for at least two month before the diagnosis, and the criteria must be fulfilled for at least four time per month[40].
- New Rome IV Criteria include all of the following [40]:
- Abdominal pain that may occur in episodic or continuous manner, pain that not occur only during physiological events like eating[40].
- Not fulfill the criteria of any other functional GI disorders, like irritable bowel syndrome and abdominal migraine[40].
- Abdominal pain that can not fully explained after full assessment[40].
Symptoms
- First, Red flag symptoms must be excluded:
- Symptoms associated with abdominal pain may vary according to the cause[42]:
| Disease | Associated Sympyoms |
|---|---|
| Colic | Irritability, paroxysmal crying[43] |
| Appendicitis | Vomiting,fever, localized right lower quadrant tenderness[44]. |
| Irritable bowel syndrome | Diarrhea, Constipation[45]. |
| Hepatitis | jaundice[46] |
| Henchon-schonlein purpura | Skin Rash[47] |
| Urolithiasis | Hematuria[48] |
| Pyelonephritis | Dysuria, fever, urinary frequency, vomiting.[49] |
Physical Examination
- First, check vital signs, growth parameters and if there is evidence of failure to thrive. [41].
- Inspect abdominal wall contour, protrusions, or skin abnormalities.[41]
- Palpate superficially while looking to patient's face.[25]
- Deep palpation for masses, kidney, spleen and liver[25].
- Percussion and auscultation[41].
- Digital rectal examinations and genital examinations[42]
Laboratory Findings
- Initial laboratory tests according to symptoms include:
- Complete blood count, Urine analysis, Stool analysis.[50]
- Liver enzyme, pancreatic enzymes if liver and pancreas diseases in suspected[30].
- Electrolyte (Sodium and serum bicarbonate levels) and creatinine, and glucose levels are useful in assessment of dehydration in patient with gastroenteritis[51]
Electrocardiogram
There are no ECG findings associated with abdominal pain in children.
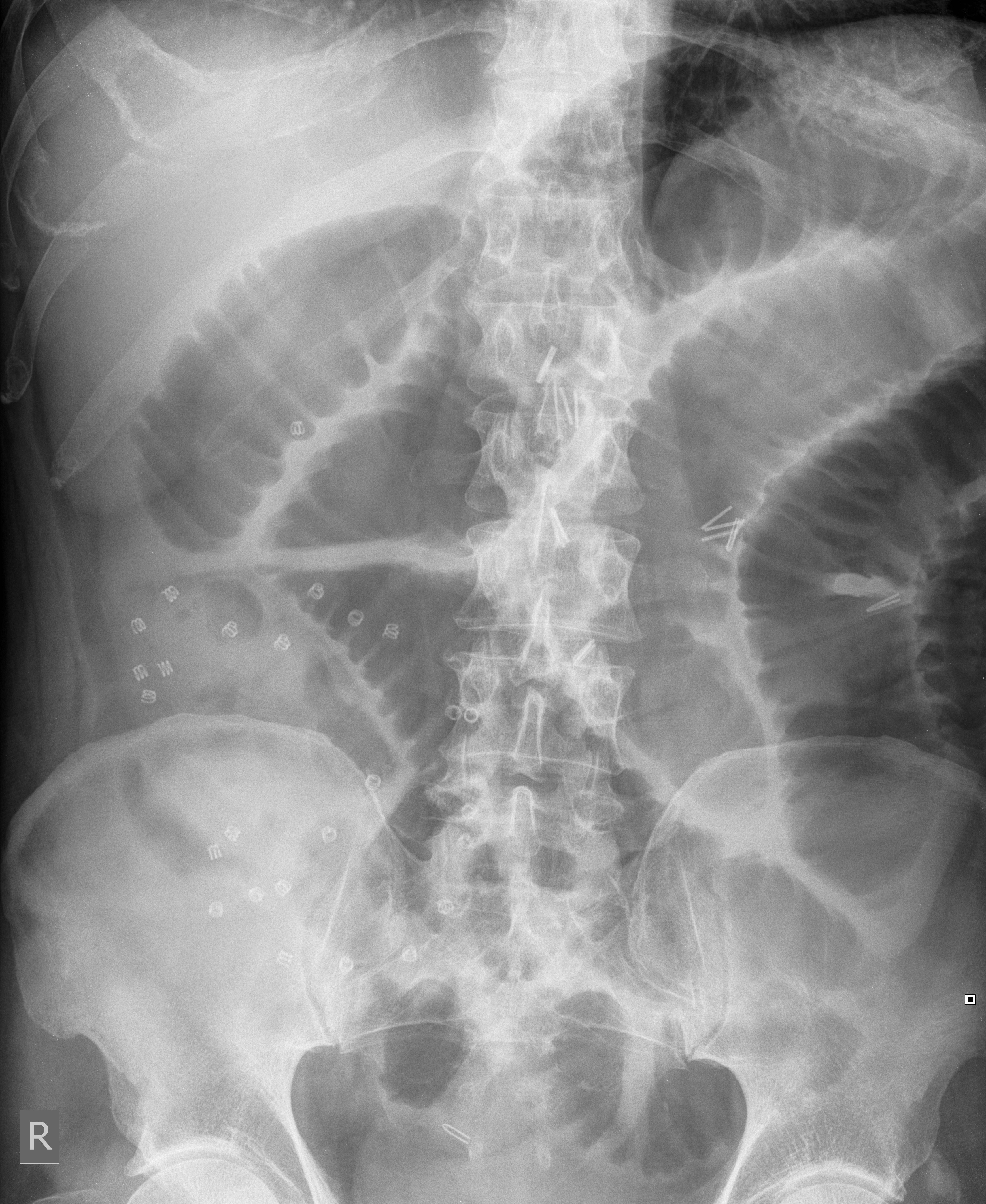
X-ray
- Plain abdominal pain X-ray may show evidence of bowel obstruction, free air and kidney stone[6].

Ultrasound
- Ultrasound may be helpful in the diagnosis of appendicitis [30].
- Findings on an ultrasound suggestive of appendicitis include:
- aperistaltic, non-compressible, width(>6 mm outer diameter), when compressed it's appears round[52].

- Ultrasound may be useful in diagnosing urinary tract (including kidneys) anatomical abnormalities, including nephrolithiasis and associated complications such as hydronephrosis [30].
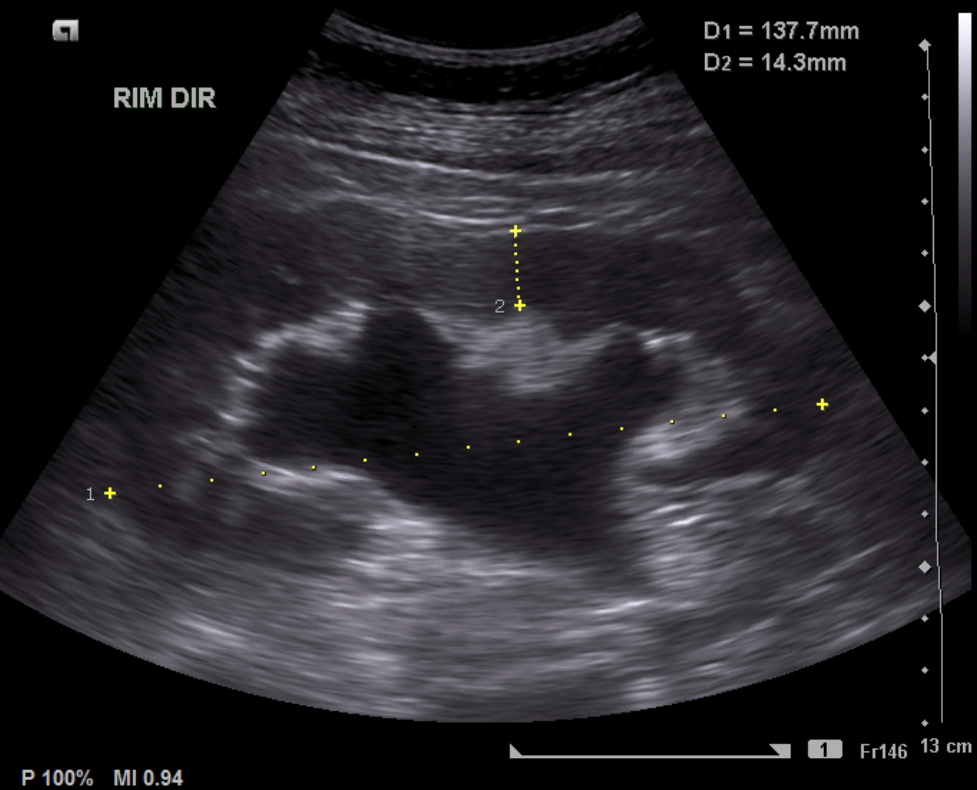
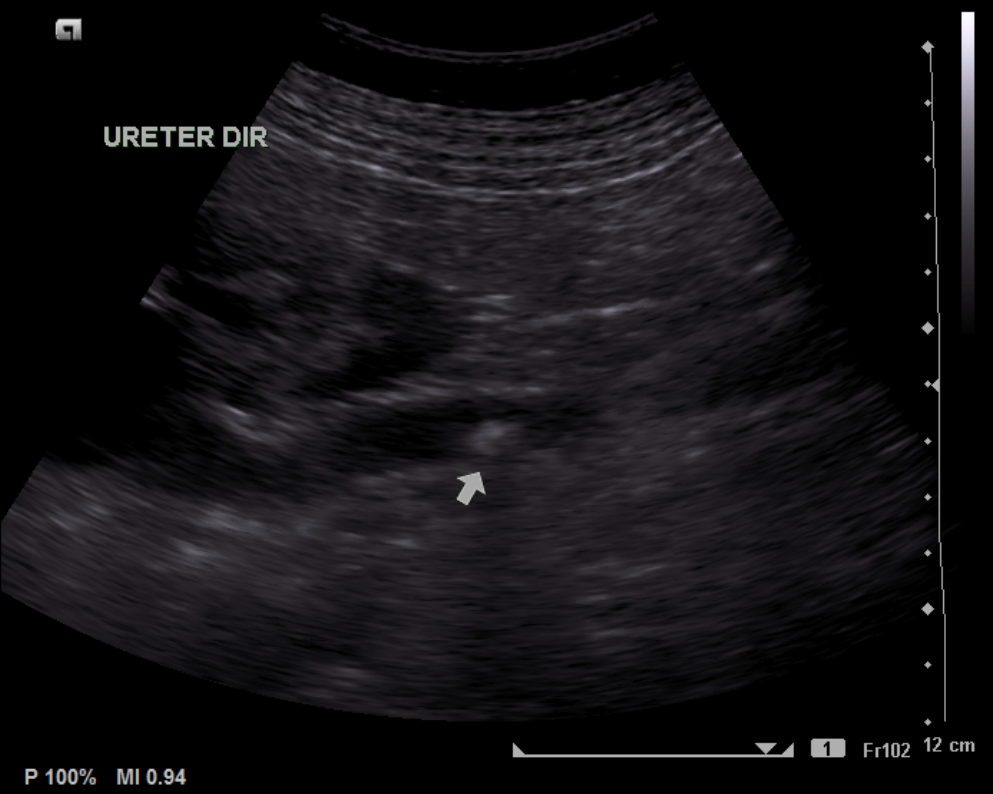
- Ultrasound is used in diagnosis of intussusception , classic finding on ultrasound[53]:
- Target sign
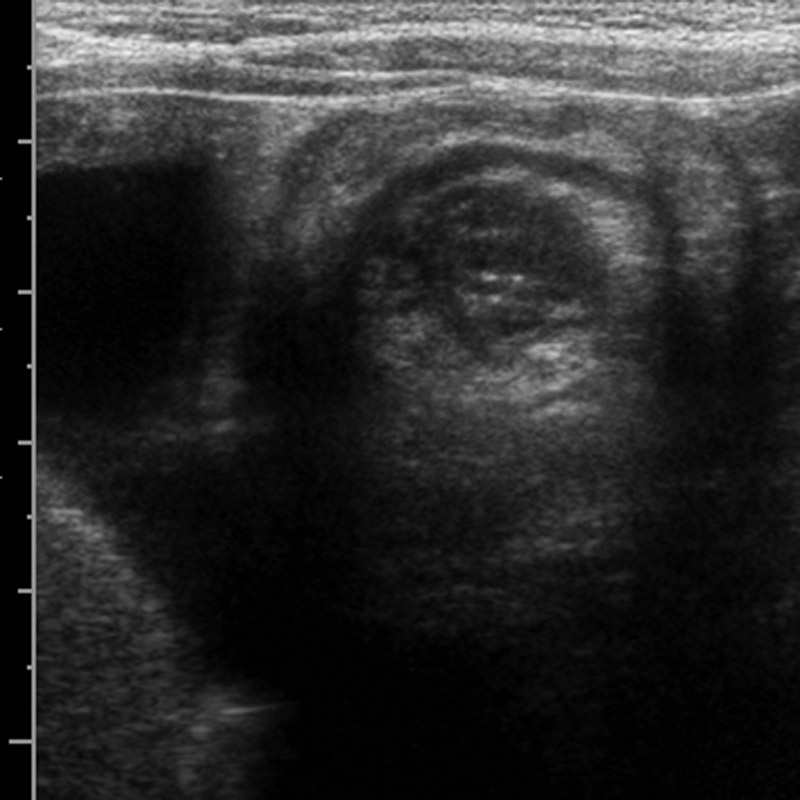
Case courtesy of Assoc Prof Frank Gaillard, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/6502">rID: 6502</a - Pseudokidney sign
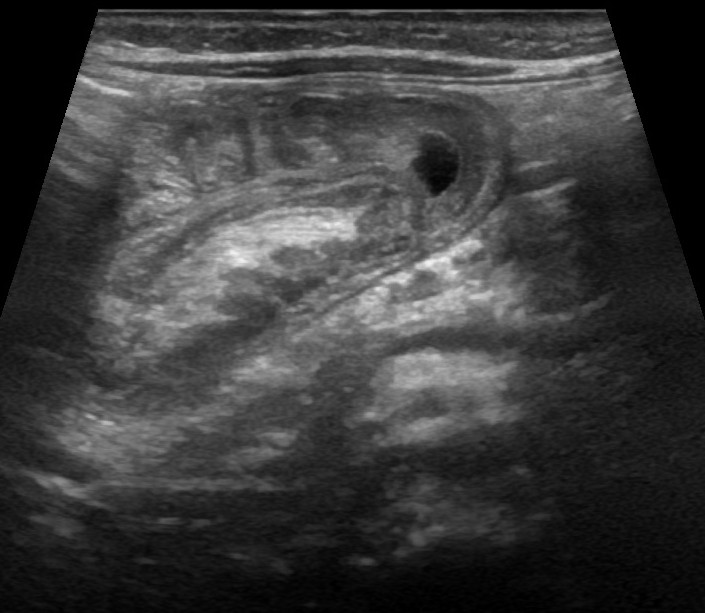
Case courtesy of Dr Tee Yu Jin, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/70238">rID: 70238</a>
- Target sign
CT scan
- Abdominal CT scan may be helpful in the diagnosis of acute appendicitis[30]. Findings on CT scan suggestive of acute appendicitis include:
- Dilation of appendix (>6 mm diameter)[52]
- Enhancement of appendiceal wall and wall thickness (>3mm diameter) [52]
- Cecal apex thickness[52].
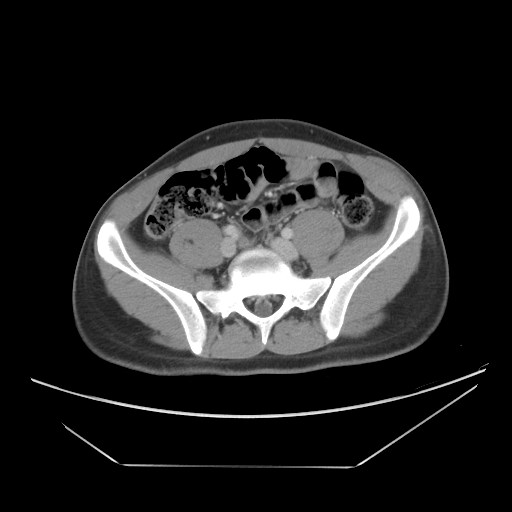
Case courtesy of Dr Naim Qaqish, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/72705">rID: 72705</a>
MRI
- Abdominal MRI may be helpful in the diagnosis of appendicitis, with sensitivity of 96% and specificity of 96%[54] .Finding on MRI has many similar findings to CT scan[54].
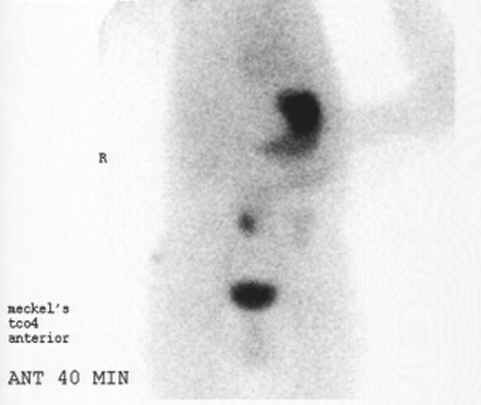
Other Imaging Findings
- Technetium-99m pertechnetate scan may be helpful in the diagnosis of suspected Meckel's diverticulum[30]. Identification of an ectopic gastric mucosa diagnostic of Meckel's diverticulum [30].
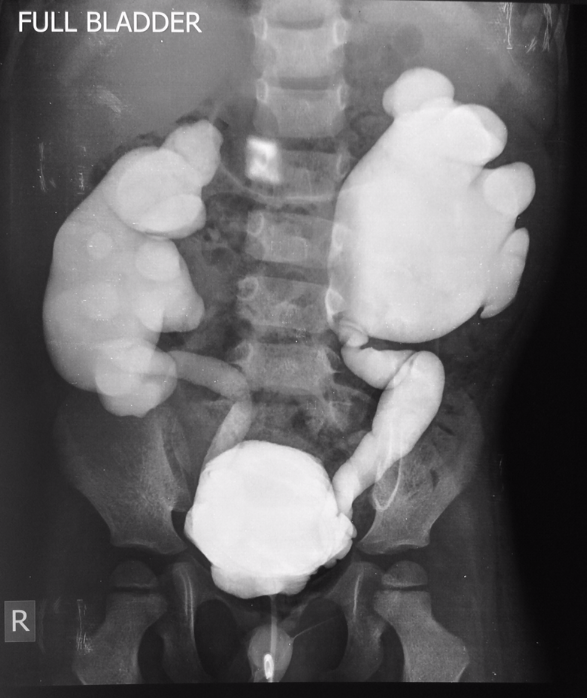
Other Diagnostic Studies
- High-grade vesicoureteral reflux or obstructive uropathy can be diagnosed using voiding cystourethrogram (VCUG)[30].
Treatment
Medical Therapy
- The mainstay of therapy for acute gastroenteritis depends on the degree of dehydration ranging from simple oral rehydration at home to hospital admission[55].
- In functional abdominal pain if bloating is predominate symptom, dietary measures may be effective for example, a low-FODMAP diet to exclude foods with certain types of carbohydrates including wheat, various fruits, lactose, fructose, and some artificial sweeteners[40]. If constipation is a predominate symptoms, incorporating non-stimulant laxatives such as PEG-3350 or increased fiber diets can be helpful[40]. Pharmacological treatment with drugs like selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants (TCAs) are often used to treat functional abdominal pain[40].
Surgery
- Surgery is the mainstay of therapy for appendicitis, which can be done either laparoscopically or open[52] .
Prevention
- Effective measures for the primary prevention of acute gastroenteritis include handwashing, breastfeeding, and rotavirus vaccination[51].
References
- ↑ "CELIAC DISEASE".
- ↑ "What Is New in Rome IV".
- ↑ 3.0 3.1 "Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice - PubMed".
- ↑ Short AR (1935). "ABDOMINAL PAIN IN CHILDREN". Br Med J. 1 (3883): 1157–9. doi:10.1136/bmj.1.3883.1157. PMC 2460552. PMID 20779127.
- ↑ Eizenga W, Gieteling MJ, Berger M, Geijer RM (2013). "[Summary of the NHG guideline 'Abdominal pain in children', the 100th NHG guideline]". Ned Tijdschr Geneeskd. 157 (15): A6191. PMID 23575296.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 "Abdominal pain in children".
- ↑ "Evaluation of abdominal pain in children - Etiology | BMJ Best Practice US".
- ↑ Marzuillo P, Germani C, Krauss BS, Barbi E (May 2015). "Appendicitis in children less than five years old: A challenge for the general practitioner". World J Clin Pediatr. 4 (2): 19–24. doi:10.5409/wjcp.v4.i2.19. PMC 4438437. PMID 26015876.
- ↑ 9.0 9.1 Moir CR (October 1996). "Abdominal pain in infants and children". Mayo Clin Proc. 71 (10): 984–9, quiz 989. doi:10.1016/S0025-6196(11)63773-7. PMID 8820774.
- ↑ Devanarayana NM, Rajindrajith S (June 2018). "Irritable bowel syndrome in children: Current knowledge, challenges and opportunities". World J Gastroenterol. 24 (21): 2211–2235. doi:10.3748/wjg.v24.i21.2211. PMC 5989237. PMID 29881232.
- ↑ Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean L, Mirzaa G, Amemiya A, Taylor AK, Lebwohl B, Snyder CL, Green P. PMID 20301720. Vancouver style error: initials (help); Missing or empty
|title=(help) - ↑ Keese D, Rolle U, Gfroerer S, Fiegel H (2019). "Symptomatic Meckel's Diverticulum in Pediatric Patients-Case Reports and Systematic Review of the Literature". Front Pediatr. 7: 267. doi:10.3389/fped.2019.00267. PMC 6606722 Check
|pmc=value (help). PMID 31294008. - ↑ Simon NM, Joseph J, Philip RR, Sukumaran TU, Philip R (January 2019). "Intussusception: Single Center Experience of 10 Years". Indian Pediatr. 56 (1): 29–32. PMID 30806357.
- ↑ Le CK, Nahirniak P, Anand S, Cooper W. PMID 28722866. Missing or empty
|title=(help) - ↑ 15.0 15.1 15.2 15.3 "Epidemiology of Pediatric Functional Abdominal Pain Disorders: A Meta-Analysis".
- ↑ "Nephrolithiasis - PubMed".
- ↑ Simões E Silva AC, Oliveira EA, Mak RH (2020). "Urinary tract infection in pediatrics: an overview". J Pediatr (Rio J). 96 Suppl 1: 65–79. doi:10.1016/j.jped.2019.10.006. PMID 31783012. Vancouver style error: missing comma (help)
- ↑ "Correction". Am Fam Physician. 99 (12): 732. June 2019. PMID 31194486.
- ↑ Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, Gupta A (August 2020). "Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation". Paediatr Respir Rev. doi:10.1016/j.prrv.2020.08.001. PMC 7417920 Check
|pmc=value (help). PMID 32891582 Check|pmid=value (help). - ↑ Gieteling MJ, Lisman-van Leeuwen Y, van der Wouden JC, Schellevis FG, Berger MY (2011). "Childhood nonspecific abdominal pain in family practice: incidence, associated factors, and management". Ann Fam Med. 9 (4): 337–43. doi:10.1370/afm.1268. PMC 3133581. PMID 21747105.
- ↑ Ramchandani PG, Hotopf M, Sandhu B, Stein A (July 2005). "The epidemiology of recurrent abdominal pain from 2 to 6 years of age: results of a large, population-based study". Pediatrics. 116 (1): 46–50. doi:10.1542/peds.2004-1854. PMID 15995029.
- ↑ "Lead Poisoning in Children - American Family Physician".
- ↑ "Sickle Cell Disease - PubMed".
- ↑ 25.0 25.1 25.2 "Abdo pain in children".
- ↑ "Childhood Nonspecific Abdominal Pain in Family Practice: Incidence, Associated Factors, and Management | Annals of Family Medicine".
- ↑ 27.0 27.1 "Abdominal Pain in Children By Prof. Dr. Sushmita Bhatnagar".
- ↑ "Approach to abdominal pain".
- ↑ "Acute Abdominal Pain in Children - American Family Physician".
- ↑ 30.00 30.01 30.02 30.03 30.04 30.05 30.06 30.07 30.08 30.09 30.10 30.11 "Assessment of abdominal pain in children - Diagnosis Approach | BMJ Best Practice".
- ↑ BEACH Program, AIHW General Practice Statistics and Classification Unit (2004). "Presentations of abdominal pain in Australian general practice". Aust Fam Physician. 33 (12): 968–9. PMID 15630915.
- ↑ "Recurrent abdominal pain in pediatrics".
- ↑ Veauthier B, Hornecker JR (December 2018). "Crohn's Disease: Diagnosis and Management". Am Fam Physician. 98 (11): 661–669. PMID 30485038.
- ↑ "www.longdom.org" (PDF).
- ↑ "www.ncbi.nlm.nih.gov" (PDF).
- ↑ "Colic in infants".
- ↑ "Pediatric abdominal pain".
- ↑ "Pediatric appendicitis score: A retrospective analysis".
- ↑ "Functional Disorders: Children and Adolescents - PubMed".
- ↑ 40.0 40.1 40.2 40.3 40.4 40.5 40.6 40.7 "Functional Abdominal Pain In Children - StatPearls - NCBI Bookshelf".
- ↑ 41.0 41.1 41.2 41.3 41.4 41.5 41.6 41.7 "Approach to pediatric abdominal pain".
- ↑ 42.0 42.1 "Abdominal pain in pediatrics".
- ↑ "Abdominal pain in pediatrics".
- ↑ "Abdominal Pain in Children By Prof. Dr. Sushmita Bhatnagar".
- ↑ "Abdominal pain in children".
- ↑ "Abdominal pain in pediatrics".
- ↑ "Abdominal pain in pediatrics".
- ↑ "Abdominal pain in children".
- ↑ "Abdominal pain in children".
- ↑ "Recurrent abdominal pain in children".
- ↑ 51.0 51.1 "Gastroenteritis in Children - American Family Physician".
- ↑ 52.0 52.1 52.2 52.3 52.4 "Appendicitis | Radiology Reference Article | Radiopaedia.org".
- ↑ "Intussusception | Radiology Reference Article | Radiopaedia.org".
- ↑ 54.0 54.1 "Appendicitis (summary) | Radiology Reference Article | Radiopaedia.org".
- ↑ "Acute gastroenteritis in children".