Skin cancer: Difference between revisions
Sara Mohsin (talk | contribs) |
Sara Mohsin (talk | contribs) No edit summary |
||
| (17 intermediate revisions by 2 users not shown) | |||
| Line 15: | Line 15: | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
{{CMG}} {{AE}}{{S.M.}} | {{CMG}} {{AE}} {{S.M.}} | ||
==Overview== | ==Overview== | ||
[[Skin]] [[cancer]] is the [[malignant]] [[growth]] on the [[skin]] which is the most common type of [[malignancy]] in [[Caucasian honey bee|Caucasians]]. [[Skin]] [[Cancer (disease)|cancer]] [[Generality|generally]] [[Development (biology)|develops]] in the [[Epidermis (skin)|epidermis]] (the outermost layer of [[skin]]), so a [[tumor]] is usually [[ClearNET|clearly]] [[Visible spectrum|visible]]. This [[MakeBot|makes]] most [[skin]] [[cancers]] [[Detectable warning|detectable]] in the early stages. | [[Skin]] [[cancer]] is the [[malignant]] [[growth]] on the [[skin]] which is the most common type of [[malignancy]] in [[Caucasian honey bee|Caucasians]]. [[Skin]] [[Cancer (disease)|cancer]] [[Generality|generally]] [[Development (biology)|develops]] in the [[Epidermis (skin)|epidermis]] (the outermost layer of [[skin]]), so a [[tumor]] is usually [[ClearNET|clearly]] [[Visible spectrum|visible]]. This [[MakeBot|makes]] most [[skin]] [[cancers]] [[Detectable warning|detectable]] in the early stages. [[Skin]] [[Cancer (disease)|cancer]] is broadly [[Classification|classified]] into [[melanoma]] and non-[[melanoma]] [[skin]] [[cancer]] (NMSC) with most common NMSC types to be [[Squamous cell carcinoma of the skin|squamous cell carcinoma]] and [[basal cell carcinoma]]. Most common [[Causes|cause]] of [[skin]] [[cancer]] is [[DNA mutations]] [[Causes|caused]] by [[UV radiation|UV irradiation]] over a proplonged [[period]] of [[Time-series|time]] especially in fair-[[Skin|skinned]] [[Individual growth|individuals]]. [[Skin]] [[Cancers|cancer]] is the fastest [[Growth|growing]] type of [[Cancer (disease)|cancer]] in the [[United States]]. [[Skin]] [[Cancer (disease)|cancer]] [[Representative agent|represents]] the most commonly [[Diagnose|diagnosed]] [[malignancy]], [[Surpass|surpassing]] [[Lung cancer|lung]], [[Breast cancer|breast]], [[Colorectal cancer|colorectal]] and [[prostate cancer]]. More than 1 million Americans were [[Estimate|estimated]] to be [[Diagnose|diagnosed]] with [[skin]] [[Cancer (disease)|cancer]] in 2007. [[Skin]] [[cancer]] can be [[Treatments|treated]] by [[surgery]], or other non-[[Surgery|surgical]] options such as [[cryotherapy]], [[electrotherapy]], [[curettage]], [[photodynamic therapy]], [[chemical peel]], [[chemotherapy]], [[radiation therapy]], [[targeted therapy]] and [[biological therapy]]. [[Cancers]] [[Causes|caused]] by [[Ultraviolet|UV]] [[Exposure (photography)|exposure]] may be [[Prevention (medical)|prevented]] by [[Avoidance reaction|avoiding]] [[Exposure (photography)|exposure]] to [[sunlight]] or other [[Ultraviolet|UV]] [[Source document|sources]], [[Wear red day|wearing]] [[Sun exposure|sun]]-[[Protective group|protective]] clothes, and [[Usage analysis|using]] a [[broad-spectrum]] [[sunscreen]]. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*In 1928, [[sunscreens]] were first [[Introduction|introduced]] in [[United States]] after which they [[Gain|gained]] tremendous commercial success<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * In 1928, [[sunscreens]] were first [[Introduction|introduced]] in [[United States]] after which they [[Gain|gained]] tremendous commercial success<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | ||
*In 1978, [[US FDA]] first adopted the [[efficacy]] of [[Protecting group|protection]] by [[sunscreens]] as [[Indication (medicine)|indicated]] by the [[sun protection factor]] ([[SPF]])<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * In 1978, [[US FDA]] first adopted the [[efficacy]] of [[Protecting group|protection]] by [[sunscreens]] as [[Indication (medicine)|indicated]] by the [[sun protection factor]] ([[SPF]])<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | ||
*In 1988, Bestor first identified [[DNA methyltransferase]] 1 ([[DNMT1]]), which is the primary [[Target cell|target]] of [[UV radiation|UV radiations]] in [[carcinogenic]] [[Process (anatomy)|process]] of [[skin]] [[cancer]]<ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref> | * In 1988, Bestor first identified [[DNA methyltransferase]] 1 ([[DNMT1]]), which is the primary [[Target cell|target]] of [[UV radiation|UV radiations]] in [[carcinogenic]] [[Process (anatomy)|process]] of [[skin]] [[cancer]]<ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref> | ||
*From 1992 to 1994, free [[American Academy of Dermatology|American Academy of Dermatology's]] National [[Skin]] [[Cancer (disease)|Cancer]] Early [[Detection theory|Detection]] and [[Screening (medicine)|Screening]] Program was launched which provided broad [[skin]] [[Cancer (disease)|cancer]] [[Education|educational]] [[Information science|information]] to general [[Public health|public]] and enabled almost 750,000 free [[Expert Patient Programme|expert]] [[skin]] [[Cancer (disease)|cancer]] [[Examination|examinations]] which mostly found out thin, [[Localized disease|localized]] stage 1 [[melanomas]] with high [[Project Halo|projected]] [[Five year survival rate|5-year survival rate]]<ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA">{{cite web |url=https://www.massgeneral.org/cancer/services/treatmentprograms.aspx?id=1196&utm_source=google&utm_medium=cpc&utm_campaign=cancerppc&utm_content=Skin_Cancer_Tests&utm_term=%2Bskin%20%2Bcancer%20%2Bscreening&gclid=Cj0KCQjwyLDpBRCxARIsAEENsrLfUiAniaSP1Yn6UijTzqDMp0KFhlTv2Eikg5a9TyVSGnWkmoiA3bsaAqNfEALw_wcB |title=Skin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA |format= |work= |accessdate=}}</ref><ref name="pmid8647990">{{cite journal| author=Koh HK, Norton LA, Geller AC, Sun T, Rigel DS, Miller DR et al.| title=Evaluation of the American Academy of Dermatology's National Skin Cancer Early Detection and Screening Program. | journal=J Am Acad Dermatol | year= 1996 | volume= 34 | issue= 6 | pages= 971-8 | pmid=8647990 | doi=10.1016/s0190-9622(96)90274-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8647990 }} </ref> | * From 1992 to 1994, free [[American Academy of Dermatology|American Academy of Dermatology's]] National [[Skin]] [[Cancer (disease)|Cancer]] Early [[Detection theory|Detection]] and [[Screening (medicine)|Screening]] Program was launched which provided broad [[skin]] [[Cancer (disease)|cancer]] [[Education|educational]] [[Information science|information]] to general [[Public health|public]] and enabled almost 750,000 free [[Expert Patient Programme|expert]] [[skin]] [[Cancer (disease)|cancer]] [[Examination|examinations]] which mostly found out thin, [[Localized disease|localized]] stage 1 [[melanomas]] with high [[Project Halo|projected]] [[Five year survival rate|5-year survival rate]]<ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA">{{cite web |url=https://www.massgeneral.org/cancer/services/treatmentprograms.aspx?id=1196&utm_source=google&utm_medium=cpc&utm_campaign=cancerppc&utm_content=Skin_Cancer_Tests&utm_term=%2Bskin%20%2Bcancer%20%2Bscreening&gclid=Cj0KCQjwyLDpBRCxARIsAEENsrLfUiAniaSP1Yn6UijTzqDMp0KFhlTv2Eikg5a9TyVSGnWkmoiA3bsaAqNfEALw_wcB |title=Skin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA |format= |work= |accessdate=}}</ref><ref name="pmid8647990">{{cite journal| author=Koh HK, Norton LA, Geller AC, Sun T, Rigel DS, Miller DR et al.| title=Evaluation of the American Academy of Dermatology's National Skin Cancer Early Detection and Screening Program. | journal=J Am Acad Dermatol | year= 1996 | volume= 34 | issue= 6 | pages= 971-8 | pmid=8647990 | doi=10.1016/s0190-9622(96)90274-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8647990 }} </ref> | ||
*From 2001 to 2005, [[American Academy of Dermatology]] National [[Melanoma]]/[[Skin]] [[Cancer (disease)|Cancer]] [[Screening (medicine)|Screening]] Program was launched which led to the conclusion that HARMM [[criteria]] can be [[Usage analysis|used]] to identify the higher-[[RiskMetrics|risk]] [[Subgroup analysis|subgroup]] of [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]] [[Population (statistics)|population]] via [[Assessment and Plan|assessment]] of multiple [[risk factors]] for [[MM]] , which will not only [[Reduced|reduce]] the [[Cost-effectiveness|cost]] but will also increase the [[Yield (chemistry)|yields]] for suspected [[MM]] in [[Future interests (actuarial science)|future]] [[mass]] [[Screening (medicine)|screening]] [[Initiation (chemistry)|initiatives]]<ref name="pmid17490783">{{cite journal| author=Goldberg MS, Doucette JT, Lim HW, Spencer J, Carucci JA, Rigel DS| title=Risk factors for presumptive melanoma in skin cancer screening: American Academy of Dermatology National Melanoma/Skin Cancer Screening Program experience 2001-2005. | journal=J Am Acad Dermatol | year= 2007 | volume= 57 | issue= 1 | pages= 60-6 | pmid=17490783 | doi=10.1016/j.jaad.2007.02.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17490783 }} </ref> | * From 2001 to 2005, [[American Academy of Dermatology]] National [[Melanoma]]/[[Skin]] [[Cancer (disease)|Cancer]] [[Screening (medicine)|Screening]] Program was launched which led to the conclusion that HARMM [[criteria]] can be [[Usage analysis|used]] to identify the higher-[[RiskMetrics|risk]] [[Subgroup analysis|subgroup]] of [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]] [[Population (statistics)|population]] via [[Assessment and Plan|assessment]] of multiple [[risk factors]] for [[MM]] , which will not only [[Reduced|reduce]] the [[Cost-effectiveness|cost]] but will also increase the [[Yield (chemistry)|yields]] for suspected [[MM]] in [[Future interests (actuarial science)|future]] [[mass]] [[Screening (medicine)|screening]] [[Initiation (chemistry)|initiatives]]<ref name="pmid17490783">{{cite journal| author=Goldberg MS, Doucette JT, Lim HW, Spencer J, Carucci JA, Rigel DS| title=Risk factors for presumptive melanoma in skin cancer screening: American Academy of Dermatology National Melanoma/Skin Cancer Screening Program experience 2001-2005. | journal=J Am Acad Dermatol | year= 2007 | volume= 57 | issue= 1 | pages= 60-6 | pmid=17490783 | doi=10.1016/j.jaad.2007.02.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17490783 }} </ref> | ||
*In 2007, more than 1 million Americans were [[Estimate|estimated]] to be [[Diagnose|diagnosed]] with [[skin]] [[cancer]] | * In 2007, more than 1 million Americans were [[Estimate|estimated]] to be [[Diagnose|diagnosed]] with [[skin]] [[cancer]] | ||
*In 2014, 6500 [[new]] [[Case-based reasoning|cases]] of [[melanoma]] and 76,100 [[Case-based reasoning|cases]] of NMSC were [[Estimate|estimated]] to have occurred in [[Canada Health Act|Canada]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * In 2014, 6500 [[new]] [[Case-based reasoning|cases]] of [[melanoma]] and 76,100 [[Case-based reasoning|cases]] of NMSC were [[Estimate|estimated]] to have occurred in [[Canada Health Act|Canada]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | ||
*In 2016, the [[Estimate|estimated]] [[number]] of [[new]] [[Case-based reasoning|cases]] of [[skin]] [[melanoma]] was 76,380 which is 4.5% of all [[new]] [[Cancer (disease)|cancer]] [[Case-based reasoning|cases]] | * In 2016, the [[Estimate|estimated]] [[number]] of [[new]] [[Case-based reasoning|cases]] of [[skin]] [[melanoma]] was 76,380 which is 4.5% of all [[new]] [[Cancer (disease)|cancer]] [[Case-based reasoning|cases]] | ||
*In 2016, a National [[Consensus (medical)|Consensus]] on [[Sun exposure|Sun]] [[Safety climate|Safety]] [[Message-passing method|Messages]] was [[Development (biology)|developed]] in [[Canada Health Act|Canada]] in order to [[Promoter|promote]] the [[Uniformity of Content|uniformity]] of [[Public health informatics|public health messages]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * In 2016, a National [[Consensus (medical)|Consensus]] on [[Sun exposure|Sun]] [[Safety climate|Safety]] [[Message-passing method|Messages]] was [[Development (biology)|developed]] in [[Canada Health Act|Canada]] in order to [[Promoter|promote]] the [[Uniformity of Content|uniformity]] of [[Public health informatics|public health messages]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | ||
*From 1946 to December 2018, a [[SearchBox|search]] for [[Study design|studies]] [[Related phenomena|related]] to [[Protecting group|protection]] by [[sunscreen]] was [[Performance status|performed]] in [[MEDLINE]] | * From 1946 to December 2018, a [[SearchBox|search]] for [[Study design|studies]] [[Related phenomena|related]] to [[Protecting group|protection]] by [[sunscreen]] was [[Performance status|performed]] in [[MEDLINE]] | ||
==Classification== | ==Classification== | ||
*[[Skin]] [[Cancer (disease)|cancer]] is broadly divided into [[Melanoma, Malignant|melanoma]] and non[[melanoma]] types as shown in the following table:<ref name="urlNonmelanoma skin cancer - Symptoms and causes - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/nonmelanoma-skin-cancer/symptoms-causes/syc-20355397 |title=Nonmelanoma skin cancer - Symptoms and causes - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="pmid26612377">{{cite journal| author=Linares MA, Zakaria A, Nizran P| title=Skin Cancer. | journal=Prim Care | year= 2015 | volume= 42 | issue= 4 | pages= 645-59 | pmid=26612377 | doi=10.1016/j.pop.2015.07.006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26612377 }} </ref><ref name="pmid15080294">{{cite journal| author=Lee PK| title=Common skin cancers. | journal=Minn Med | year= 2004 | volume= 87 | issue= 3 | pages= 44-7 | pmid=15080294 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15080294 }} </ref><ref name="pmid29261131">{{cite journal| author=Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C| title=Histology of Non-Melanoma Skin Cancers: An Update. | journal=Biomedicines | year= 2017 | volume= 5 | issue= 4 | pages= | pmid=29261131 | doi=10.3390/biomedicines5040071 | pmc=5744095 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29261131 }} </ref><ref name="pmid25663185">{{cite journal| author=Majores M, Bierhoff E| title=[Actinic keratosis, Bowen's disease, keratoacanthoma and squamous cell carcinoma of the skin]. | journal=Pathologe | year= 2015 | volume= 36 | issue= 1 | pages= 16-29 | pmid=25663185 | doi=10.1007/s00292-014-2063-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25663185 }} </ref><ref name="pmid31112591">{{cite journal| author=Hosny KM, Kassem MA, Foaud MM| title=Classification of skin lesions using transfer learning and augmentation with Alex-net. | journal=PLoS One | year= 2019 | volume= 14 | issue= 5 | pages= e0217293 | pmid=31112591 | doi=10.1371/journal.pone.0217293 | pmc=6529006 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31112591 }} </ref><ref name="pmid30458354">{{cite journal| author=Mahbod A, Schaefer G, Ellinger I, Ecker R, Pitiot A, Wang C| title=Fusing fine-tuned deep features for skin lesion classification. | journal=Comput Med Imaging Graph | year= 2019 | volume= 71 | issue= | pages= 19-29 | pmid=30458354 | doi=10.1016/j.compmedimag.2018.10.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30458354 }} </ref><ref name="pmid30103029">{{cite journal| author=Harangi B| title=Skin lesion classification with ensembles of deep convolutional neural networks. | journal=J Biomed Inform | year= 2018 | volume= 86 | issue= | pages= 25-32 | pmid=30103029 | doi=10.1016/j.jbi.2018.08.006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30103029 }} </ref><ref name="pmid29428356">{{cite journal| author=Han SS, Kim MS, Lim W, Park GH, Park I, Chang SE| title=Classification of the Clinical Images for Benign and Malignant Cutaneous Tumors Using a Deep Learning Algorithm. | journal=J Invest Dermatol | year= 2018 | volume= 138 | issue= 7 | pages= 1529-1538 | pmid=29428356 | doi=10.1016/j.jid.2018.01.028 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29428356 }} </ref><ref name="pmid28117445">{{cite journal| author=Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM et al.| title=Dermatologist-level classification of skin cancer with deep neural networks. | journal=Nature | year= 2017 | volume= 542 | issue= 7639 | pages= 115-118 | pmid=28117445 | doi=10.1038/nature21056 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28117445 }} </ref> | * [[Skin]] [[Cancer (disease)|cancer]] is broadly divided into [[Melanoma, Malignant|melanoma]] and non[[melanoma]] types as shown in the following table:<ref name="urlNonmelanoma skin cancer - Symptoms and causes - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/nonmelanoma-skin-cancer/symptoms-causes/syc-20355397 |title=Nonmelanoma skin cancer - Symptoms and causes - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="pmid26612377">{{cite journal| author=Linares MA, Zakaria A, Nizran P| title=Skin Cancer. | journal=Prim Care | year= 2015 | volume= 42 | issue= 4 | pages= 645-59 | pmid=26612377 | doi=10.1016/j.pop.2015.07.006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26612377 }} </ref><ref name="pmid15080294">{{cite journal| author=Lee PK| title=Common skin cancers. | journal=Minn Med | year= 2004 | volume= 87 | issue= 3 | pages= 44-7 | pmid=15080294 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15080294 }} </ref><ref name="pmid29261131">{{cite journal| author=Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C| title=Histology of Non-Melanoma Skin Cancers: An Update. | journal=Biomedicines | year= 2017 | volume= 5 | issue= 4 | pages= | pmid=29261131 | doi=10.3390/biomedicines5040071 | pmc=5744095 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29261131 }} </ref><ref name="pmid25663185">{{cite journal| author=Majores M, Bierhoff E| title=[Actinic keratosis, Bowen's disease, keratoacanthoma and squamous cell carcinoma of the skin]. | journal=Pathologe | year= 2015 | volume= 36 | issue= 1 | pages= 16-29 | pmid=25663185 | doi=10.1007/s00292-014-2063-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25663185 }} </ref><ref name="pmid31112591">{{cite journal| author=Hosny KM, Kassem MA, Foaud MM| title=Classification of skin lesions using transfer learning and augmentation with Alex-net. | journal=PLoS One | year= 2019 | volume= 14 | issue= 5 | pages= e0217293 | pmid=31112591 | doi=10.1371/journal.pone.0217293 | pmc=6529006 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31112591 }} </ref><ref name="pmid30458354">{{cite journal| author=Mahbod A, Schaefer G, Ellinger I, Ecker R, Pitiot A, Wang C| title=Fusing fine-tuned deep features for skin lesion classification. | journal=Comput Med Imaging Graph | year= 2019 | volume= 71 | issue= | pages= 19-29 | pmid=30458354 | doi=10.1016/j.compmedimag.2018.10.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30458354 }} </ref><ref name="pmid30103029">{{cite journal| author=Harangi B| title=Skin lesion classification with ensembles of deep convolutional neural networks. | journal=J Biomed Inform | year= 2018 | volume= 86 | issue= | pages= 25-32 | pmid=30103029 | doi=10.1016/j.jbi.2018.08.006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30103029 }} </ref><ref name="pmid29428356">{{cite journal| author=Han SS, Kim MS, Lim W, Park GH, Park I, Chang SE| title=Classification of the Clinical Images for Benign and Malignant Cutaneous Tumors Using a Deep Learning Algorithm. | journal=J Invest Dermatol | year= 2018 | volume= 138 | issue= 7 | pages= 1529-1538 | pmid=29428356 | doi=10.1016/j.jid.2018.01.028 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29428356 }} </ref><ref name="pmid28117445">{{cite journal| author=Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM et al.| title=Dermatologist-level classification of skin cancer with deep neural networks. | journal=Nature | year= 2017 | volume= 542 | issue= 7639 | pages= 115-118 | pmid=28117445 | doi=10.1038/nature21056 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28117445 }} </ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Classification of skin cancer | |+Classification of skin cancer | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Skin cancer type}} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Skin cancer type}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 500px;" | {{fontcolor|#FFF|Characteristics}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF|}} | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Malignant melanoma]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Malignant melanoma]] | ||
| | | | ||
* Can occur anywhere in the [[Human body|body]] involving either even normal [[skin]] or any existing [[mole]] becoming [[cancerous]] later on | * Can occur anywhere in the [[Human body|body]] involving either even normal [[skin]] or any existing [[mole]] becoming [[cancerous]] later on | ||
*[[Signs]] suspicious for [[melanoma]] include: | * [[Signs]] suspicious for [[melanoma]] include: | ||
**[[Mole]] [[Change detection|changing]] in [[Size consistency|size]], [[color]], [[Feeling|feel]] or [[bleeding]] | ** [[Mole]] [[Change detection|changing]] in [[Size consistency|size]], [[color]], [[Feeling|feel]] or [[bleeding]] | ||
**[[Large-print|Large]] [[Brown|brownish]] [[spot]] having [[Dark matter|darker]] [[Speckle pattern|speckles]] | ** [[Large-print|Large]] [[Brown|brownish]] [[spot]] having [[Dark matter|darker]] [[Speckle pattern|speckles]] | ||
**[[Itchy]] or [[Burn|burning]] [[painful]] [[lesion]] | ** [[Itchy]] or [[Burn|burning]] [[painful]] [[lesion]] | ||
**[[Dark matter|Darker]] [[lesions]] involving [[fingertips]], [[toes]], [[Palms of the hands|palms]], [[soles]], or [[mucous membrane]] [[Line|lining]] of [[nose]], [[mouth]], [[anus]] or [[vagina]] | ** [[Dark matter|Darker]] [[lesions]] involving [[fingertips]], [[toes]], [[Palms of the hands|palms]], [[soles]], or [[mucous membrane]] [[Line|lining]] of [[nose]], [[mouth]], [[anus]] or [[vagina]] | ||
**Small [[lesion]] having [[Irregular lesion|irregular]] [[Borderline|borders]] & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or blue-black | ** Small [[lesion]] having [[Irregular lesion|irregular]] [[Borderline|borders]] & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or blue-black | ||
*Most [[Dangerous goods|dangerous]] type of [[skin]] [[Cancer (disease)|cancer]] | * Most [[Dangerous goods|dangerous]] type of [[skin]] [[Cancer (disease)|cancer]] | ||
* [[Fatal]] if not [[Treatments|treated]] early | * [[Fatal]] if not [[Treatments|treated]] early | ||
* Comprises only a small portion of all [[skin]] [[cancers]] | * Comprises only a small portion of all [[skin]] [[cancers]] | ||
| Line 59: | Line 59: | ||
| | | | ||
* Mostly occurs on the [[Sun exposure|sun-exposed]] [[Area|areas]] such as: | * Mostly occurs on the [[Sun exposure|sun-exposed]] [[Area|areas]] such as: | ||
**[[Face]] | ** [[Face]] | ||
**[[Neck]] | ** [[Neck]] | ||
* May [[Appearance|appear]] as any of the following: | * May [[Appearance|appear]] as any of the following: | ||
**[[Waxy flexibility|Waxy]] or a [[Pearl powder|pearly]] [[Bumps on skin|bump]] | ** [[Waxy flexibility|Waxy]] or a [[Pearl powder|pearly]] [[Bumps on skin|bump]] | ||
**[[Brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flats|flat]] [[lesion]] | ** [[Brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flats|flat]] [[lesion]] | ||
**[[Scab|Scabbing]] or a [[bleeding]] [[sore]] ([[Healing|heals]] and returns) | ** [[Scab|Scabbing]] or a [[bleeding]] [[sore]] ([[Healing|heals]] and returns) | ||
| rowspan="3" |Most common types | | rowspan="3" |Most common types | ||
|- | |- | ||
| Line 70: | Line 70: | ||
| | | | ||
* Mostly involves [[Sun exposure|sun-exposed]] [[skin]] [[Area|areas]] such as: | * Mostly involves [[Sun exposure|sun-exposed]] [[skin]] [[Area|areas]] such as: | ||
**[[Face]] | ** [[Face]] | ||
**[[Ears]] | ** [[Ears]] | ||
**[[Hands]] | ** [[Hands]] | ||
*Unexposed [[Area|areas]] to [[Sun exposure|sun]] are also involved in [[Dark matter|darker]]-[[Skin|skinned]] [[Individual growth|individuals]] | * Unexposed [[Area|areas]] to [[Sun exposure|sun]] are also involved in [[Dark matter|darker]]-[[Skin|skinned]] [[Individual growth|individuals]] | ||
*May [[Appearance|appear]] as any of the following: | * May [[Appearance|appear]] as any of the following: | ||
**[[Red-Al|Red]], [[Firming agent|firm]] [[nodule]] | ** [[Red-Al|Red]], [[Firming agent|firm]] [[nodule]] | ||
**[[Flats|Flat]] [[lesion]] having a crusted, [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | ** [[Flats|Flat]] [[lesion]] having a crusted, [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | ||
*[[Local]] [[Disfigurement|disfiguration]] | * [[Local]] [[Disfigurement|disfiguration]] | ||
* Unlikely to [[metastasize]] | * Unlikely to [[metastasize]] | ||
|- | |- | ||
| Line 94: | Line 94: | ||
| | | | ||
* Also known as: | * Also known as: | ||
**[[Bowen's carcinoma]] | ** [[Bowen's carcinoma]] | ||
**[[Squamous cell carcinoma in situ of skin]] | ** [[Squamous cell carcinoma in situ of skin]] | ||
**[[Intraepidermal carcinoma skin]] | ** [[Intraepidermal carcinoma skin]] | ||
* Considered as a [[Slow|slowly]] [[Growth|growing]], very early stage of [[squamous cell carcinoma of skin]] | * Considered as a [[Slow|slowly]] [[Growth|growing]], very early stage of [[squamous cell carcinoma of skin]] | ||
*[[Appearance|Appears]] as [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | * [[Appearance|Appears]] as [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | ||
* Has 3 to 5% [[RiskMetrics|risk]] of [[Development|developing]] into [[invasive]] [[squamous cell carcinoma]] | * Has 3 to 5% [[RiskMetrics|risk]] of [[Development|developing]] into [[invasive]] [[squamous cell carcinoma]] | ||
* Most commonly occurs in [[elderly]] with multiple [[comorbidities]] | * Most commonly occurs in [[elderly]] with multiple [[comorbidities]] | ||
| Line 107: | Line 107: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Keratoacanthoma]]'''<ref name="urlKeratoacanthoma - StatPearls - NCBI Bookshelf">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK499931/ |title=Keratoacanthoma - StatPearls - NCBI Bookshelf |format= |work= |accessdate=}}</ref><ref name="pmid30771415">{{cite journal| author=Gibbons M, Ernst A, Patel A, Armbrecht E, Behshad R| title=Keratoacanthomas: A review of excised specimens. | journal=J Am Acad Dermatol | year= 2019 | volume= 80 | issue= 6 | pages= 1794-1796 | pmid=30771415 | doi=10.1016/j.jaad.2019.02.011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30771415 }} </ref><ref name="pmid30429717">{{cite journal| author=Jankowska-Konsur A, Kopeć-Pytlarz K, Woźniak Z, Hryncewicz-Gwóźdź A, Maj J| title=Multiple disseminated keratoacanthoma-like nodules: a rare form of distant metastases to the skin. | journal=Postepy Dermatol Alergol | year= 2018 | volume= 35 | issue= 5 | pages= 535-537 | pmid=30429717 | doi=10.5114/ada.2018.77245 | pmc=6232540 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30429717 }} </ref><ref name="pmid20952995">{{cite journal| author=Rastogi S, Kumar P, Swarup K, Mohan L, Mukhija RD| title=Keratoacanthoma centrifugum marginatum. | journal=Indian J Dermatol Venereol Leprol | year= 1995 | volume= 61 | issue= 5 | pages= 297-8 | pmid=20952995 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20952995 }} </ref><ref name="pmid12055541">{{cite journal| author=Cherif F, Mebazaa A, Kort R, Makni N, Haouet S, Mokni M et al.| title=[Multiple keratoacanthoma centrifugum marginatum]. | journal=Ann Dermatol Venereol | year= 2002 | volume= 129 | issue= 4 Pt 1 | pages= 413-5 | pmid=12055541 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12055541 }} </ref><ref name="pmid9615129">{{cite journal| author=Lo Schiavo A, Pinto F, Degener AM, Bucci M, Ruocco V| title=[Keratoacanthoma centrifugum marginatum. Possible etiological role of papillomavirus and therapeutic response to etretinate]. | journal=Ann Dermatol Venereol | year= 1996 | volume= 123 | issue= 10 | pages= 660-3 | pmid=9615129 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9615129 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Keratoacanthoma]]'''<ref name="urlKeratoacanthoma - StatPearls - NCBI Bookshelf">{{cite web |url=https://www.ncbi.nlm.nih.gov/books/NBK499931/ |title=Keratoacanthoma - StatPearls - NCBI Bookshelf |format= |work= |accessdate=}}</ref><ref name="pmid30771415">{{cite journal| author=Gibbons M, Ernst A, Patel A, Armbrecht E, Behshad R| title=Keratoacanthomas: A review of excised specimens. | journal=J Am Acad Dermatol | year= 2019 | volume= 80 | issue= 6 | pages= 1794-1796 | pmid=30771415 | doi=10.1016/j.jaad.2019.02.011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30771415 }} </ref><ref name="pmid30429717">{{cite journal| author=Jankowska-Konsur A, Kopeć-Pytlarz K, Woźniak Z, Hryncewicz-Gwóźdź A, Maj J| title=Multiple disseminated keratoacanthoma-like nodules: a rare form of distant metastases to the skin. | journal=Postepy Dermatol Alergol | year= 2018 | volume= 35 | issue= 5 | pages= 535-537 | pmid=30429717 | doi=10.5114/ada.2018.77245 | pmc=6232540 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30429717 }} </ref><ref name="pmid20952995">{{cite journal| author=Rastogi S, Kumar P, Swarup K, Mohan L, Mukhija RD| title=Keratoacanthoma centrifugum marginatum. | journal=Indian J Dermatol Venereol Leprol | year= 1995 | volume= 61 | issue= 5 | pages= 297-8 | pmid=20952995 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20952995 }} </ref><ref name="pmid12055541">{{cite journal| author=Cherif F, Mebazaa A, Kort R, Makni N, Haouet S, Mokni M et al.| title=[Multiple keratoacanthoma centrifugum marginatum]. | journal=Ann Dermatol Venereol | year= 2002 | volume= 129 | issue= 4 Pt 1 | pages= 413-5 | pmid=12055541 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12055541 }} </ref><ref name="pmid9615129">{{cite journal| author=Lo Schiavo A, Pinto F, Degener AM, Bucci M, Ruocco V| title=[Keratoacanthoma centrifugum marginatum. Possible etiological role of papillomavirus and therapeutic response to etretinate]. | journal=Ann Dermatol Venereol | year= 1996 | volume= 123 | issue= 10 | pages= 660-3 | pmid=9615129 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9615129 }} </ref> | ||
| | | | ||
*[[Benign]] [[epithelial]] [[tumor]] | * [[Benign]] [[epithelial]] [[tumor]] | ||
* Considered as to be a variant of [[Squamous cell carcinoma of the skin|SCC]] | * Considered as to be a variant of [[Squamous cell carcinoma of the skin|SCC]] | ||
*[[Eruption|Erupts]] with an initial rapid [[growth]] (like a little [[volcano]]) on [[Sun exposure|sun]]-damaged [[skin]] and resolves on its own later on after [[Fewmets|few]] months | * [[Eruption|Erupts]] with an initial rapid [[growth]] (like a little [[volcano]]) on [[Sun exposure|sun]]-damaged [[skin]] and resolves on its own later on after [[Fewmets|few]] months | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Dermatofibrosarcoma protuberans]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Dermatofibrosarcoma protuberans]] | ||
| | | | ||
*[[Association (statistics)|Associated]] with t(17,22)(q21;q13) | * [[Association (statistics)|Associated]] with t(17,22)(q21;q13) | ||
* Begins as a minor [[Firming agent|firm]] [[area]] of [[skin]] resembling a [[bruise]], [[birthmark]], or [[pimple]] | * Begins as a minor [[Firming agent|firm]] [[area]] of [[skin]] resembling a [[bruise]], [[birthmark]], or [[pimple]] | ||
* May [[Appearance|appear]] as a raised [[Nodule (medicine)|nodule]] with [[Bleeding (Excessive)|bleeding]] | * May [[Appearance|appear]] as a raised [[Nodule (medicine)|nodule]] with [[Bleeding (Excessive)|bleeding]] | ||
| Line 123: | Line 123: | ||
| | | | ||
* Most commonly involves: | * Most commonly involves: | ||
**[[Head]] | ** [[Head]] | ||
**[[Neck]] | ** [[Neck]] | ||
**[[Trunk]] | ** [[Trunk]] | ||
*[[Appearance|Appear]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] | * [[Appearance|Appear]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Kaposi's sarcoma]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Kaposi's sarcoma]] | ||
| Line 134: | Line 134: | ||
* Involves [[Individual growth|individuals]]: | * Involves [[Individual growth|individuals]]: | ||
** Having [[Weak interaction|weak]] [[immune system]] such as: | ** Having [[Weak interaction|weak]] [[immune system]] such as: | ||
***[[AIDS]] [[patients]] | *** [[AIDS]] [[patients]] | ||
***[[Patients]] on [[immunosuppressant therapy]] (after an [[organ transplant]]) | *** [[Patients]] on [[immunosuppressant therapy]] (after an [[organ transplant]]) | ||
**[[Young adult|Young]] African [[men]] | ** [[Young adult|Young]] African [[men]] | ||
** Eastern European jewish or Italian [[Old age|older]] [[men]] | ** Eastern European jewish or Italian [[Old age|older]] [[men]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Angiosarcoma]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Angiosarcoma]] | ||
| | | | ||
*[[Association (statistics)|Associated]] with [[PTPRB]]/[[Phospholipase C|PLCG1]] [[genes]] [[mutation]] | * [[Association (statistics)|Associated]] with [[PTPRB]]/[[Phospholipase C|PLCG1]] [[genes]] [[mutation]] | ||
*Involves: | * Involves: | ||
**[[Head]] | ** [[Head]] | ||
**[[Neck]] | ** [[Neck]] | ||
**[[Kidney]] | ** [[Kidney]] | ||
**[[Liver]] | ** [[Liver]] | ||
**[[Lung]] | ** [[Lung]] | ||
**[[Breast]] ([[radiation]]-[[Induced activity|induced]] [[angiosarcoma]]) | ** [[Breast]] ([[radiation]]-[[Induced activity|induced]] [[angiosarcoma]]) | ||
*Common [[clinical]] manifestations include: | * Common [[clinical]] manifestations include: | ||
**Gradually enlarging, painless [[mass]] (most common) | ** Gradually enlarging, painless [[mass]] (most common) | ||
**[[Skin]] [[Thickener|thickening]], [[erythema]], or [[skin discoloration]] (primary [[cutaneous]]) | ** [[Skin]] [[Thickener|thickening]], [[erythema]], or [[skin discoloration]] (primary [[cutaneous]]) | ||
**[[Lymphedema]] ([[secondary]] [[angiosarcoma]]) | ** [[Lymphedema]] ([[secondary]] [[angiosarcoma]]) | ||
**[[Pain]], [[edema]] or other [[symptoms]] due to [[Compression garment|compression]] of adjacent [[Neurovascular bundle|neurovascular]] [[Structure factor|structures]] | ** [[Pain]], [[edema]] or other [[symptoms]] due to [[Compression garment|compression]] of adjacent [[Neurovascular bundle|neurovascular]] [[Structure factor|structures]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Cutaneous B cell lymphoma]]<ref name="urlCutaneous T-cell lymphoma - Symptoms and causes - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/cutaneous-t-cell-lymphoma/symptoms-causes/syc-20351056 |title=Cutaneous T-cell lymphoma - Symptoms and causes - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="urlCutaneous B-Cell Lymphoma - Lymphoma Research Foundation">{{cite web |url=https://www.lymphoma.org/aboutlymphoma/nhl/cbcl/ |title=Cutaneous B-Cell Lymphoma - Lymphoma Research Foundation |format= |work= |accessdate=}}</ref> | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Cutaneous B cell lymphoma]]<ref name="urlCutaneous T-cell lymphoma - Symptoms and causes - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/cutaneous-t-cell-lymphoma/symptoms-causes/syc-20351056 |title=Cutaneous T-cell lymphoma - Symptoms and causes - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="urlCutaneous B-Cell Lymphoma - Lymphoma Research Foundation">{{cite web |url=https://www.lymphoma.org/aboutlymphoma/nhl/cbcl/ |title=Cutaneous B-Cell Lymphoma - Lymphoma Research Foundation |format= |work= |accessdate=}}</ref> | ||
| Line 161: | Line 161: | ||
** [[Nodules]] | ** [[Nodules]] | ||
*Involves: | * Involves: | ||
**[[Head]] | ** [[Head]] | ||
**[[Neck]] | ** [[Neck]] | ||
**[[Torso]] of the [[Human body|body]] | ** [[Torso]] of the [[Human body|body]] | ||
*[[Cutaneous B cell lymphoma]] is [[Classification|classified]] into following types: | * [[Cutaneous B cell lymphoma]] is [[Classification|classified]] into following types: | ||
**Primary [[Cutaneous B cell lymphoma|cutaneous]] [[Marginal zone lymphoma|marginal zone]] [[B-cell lymphoma]] | ** Primary [[Cutaneous B cell lymphoma|cutaneous]] [[Marginal zone lymphoma|marginal zone]] [[B-cell lymphoma]] | ||
**Primary [[Cutaneous B cell lymphoma|cutaneous]] [[follicle]] center [[lymphoma]] | ** Primary [[Cutaneous B cell lymphoma|cutaneous]] [[follicle]] center [[lymphoma]] | ||
**Primary [[Cutaneous B cell lymphoma|cutaneous]] [[Diffuse Large B-Cell Lymphoma|diffuse large B-cell lymphoma]] ([[Leg (anatomy)|leg]] type) | ** Primary [[Cutaneous B cell lymphoma|cutaneous]] [[Diffuse Large B-Cell Lymphoma|diffuse large B-cell lymphoma]] ([[Leg (anatomy)|leg]] type) | ||
**[[Intravascular large B-cell lymphoma|Intravascular diffuse large B-cell lymphoma]] | ** [[Intravascular large B-cell lymphoma|Intravascular diffuse large B-cell lymphoma]] | ||
** [[Plasmacytoma]] | ** [[Plasmacytoma]] | ||
** [[Plasmacytosis]] | ** [[Plasmacytosis]] | ||
| Line 177: | Line 177: | ||
* Raised or [[Scale (social sciences)|scaly]], [[itchy]], round [[skin]] [[Patching|patches]] | * Raised or [[Scale (social sciences)|scaly]], [[itchy]], round [[skin]] [[Patching|patches]] | ||
*[[Skin]] [[Patching|patches]] [[lighter]] in [[color]] than the surrounding [[skin]] | * [[Skin]] [[Patching|patches]] [[lighter]] in [[color]] than the surrounding [[skin]] | ||
*[[Lumpyskin disease|Lumps on skin]] ([[Ulcerated lesion|ulcerate]] or break open) | * [[Lumpyskin disease|Lumps on skin]] ([[Ulcerated lesion|ulcerate]] or break open) | ||
*[[Hair loss]] | * [[Hair loss]] | ||
*[[Enlarged lymph nodes]] | * [[Enlarged lymph nodes]] | ||
* Intensely [[Itchy skin|itchy]], [[rash]]-like [[skin]] [[Redness of the skin|redness]] over whole [[Human body|body]] | * Intensely [[Itchy skin|itchy]], [[rash]]-like [[skin]] [[Redness of the skin|redness]] over whole [[Human body|body]] | ||
*[[Skin]] [[Thickener|thickening]] in [[Palms of the hands|palms]] & [[Sole (foot)|soles]] | * [[Skin]] [[Thickener|thickening]] in [[Palms of the hands|palms]] & [[Sole (foot)|soles]] | ||
It is further [[Classification|classified]] into: | It is further [[Classification|classified]] into: | ||
| Line 197: | Line 197: | ||
==Pathophysiology== | ==Pathophysiology== | ||
*[[Skin]] [[Cancer (medicine)|cancer]] is most closely [[Association (statistics)|associated]] with [[chronic inflammation]] of the [[skin]] | * [[Skin]] [[Cancer (medicine)|cancer]] is most closely [[Association (statistics)|associated]] with [[chronic inflammation]] of the [[skin]] | ||
===Normal skin function=== | ===Normal skin function=== | ||
*[[Skin]] is the [[Large-print|largest]] [[Organ (biology)|organ]] of [[Human body|body]] with following [[Function (biology)|functions]]: | * [[Skin]] is the [[Large-print|largest]] [[Organ (biology)|organ]] of [[Human body|body]] with following [[Function (biology)|functions]]: | ||
**As a [[Physical activity|physical]] [[Barrier (pharmaceutical)|barrier]], it provides [[Protecting group|protection]] against: | ** As a [[Physical activity|physical]] [[Barrier (pharmaceutical)|barrier]], it provides [[Protecting group|protection]] against: | ||
***[[Sunlight]] | *** [[Sunlight]] | ||
***[[Heat]] | *** [[Heat]] | ||
***[[Infection]] | *** [[Infection]] | ||
***[[Injury]] | *** [[Injury]] | ||
**[[Control|Controls]] the [[body temperature]] (provides [[Insulator|insulation]] to the [[internal]] [[Human body|body]] [[organs]]) | ** [[Control|Controls]] the [[body temperature]] (provides [[Insulator|insulation]] to the [[internal]] [[Human body|body]] [[organs]]) | ||
**It stores: | ** It stores: | ||
***[[Water]] | *** [[Water]] | ||
***[[Vitamin D]] | *** [[Vitamin D]] | ||
***[[Fat]] | *** [[Fat]] | ||
===Normal skin anatomy=== | ===Normal skin anatomy=== | ||
*The two [[Main effect|main]] layers of [[skin]] include: | * The two [[Main effect|main]] layers of [[skin]] include: | ||
**Outer layer of [[Epidermis (skin)|epidermis]] ([[skin]] [[Cancer (disease)|cancer]] starts in this layer), which has following three different kinds of [[Cells (biology)|cells]]: | ** Outer layer of [[Epidermis (skin)|epidermis]] ([[skin]] [[Cancer (disease)|cancer]] starts in this layer), which has following three different kinds of [[Cells (biology)|cells]]: | ||
***[[Top7|Top]] layer of [[Epidermis (skin)|epidermis]] is made up of thin, [[Flat affect|flat]] '''[[Squamous cell|squamous cells]]''' | *** [[Top7|Top]] layer of [[Epidermis (skin)|epidermis]] is made up of thin, [[Flat affect|flat]] '''[[Squamous cell|squamous cells]]''' | ||
***[[Round face|Round]] [[Basal cell|'''basal cells''']] are [[Presenting symptom|present]] below the layer of [[Squamous cell|squamous cells]] | *** [[Round face|Round]] [[Basal cell|'''basal cells''']] are [[Presenting symptom|present]] below the layer of [[Squamous cell|squamous cells]] | ||
***Lower [[epidermal]] layer has [[melanin]] [[Product (biology)|producing]] [[Cells (biology)|cells]] ([[melanocytes]]) which on increased [[sun exposure]] [[lead]] to more [[pigment]] [[Product (biology)|production]] [[Causality|causing]] [[skin]] [[Dark matter|darkening]] | *** Lower [[epidermal]] layer has [[melanin]] [[Product (biology)|producing]] [[Cells (biology)|cells]] ([[melanocytes]]) which on increased [[sun exposure]] [[lead]] to more [[pigment]] [[Product (biology)|production]] [[Causality|causing]] [[skin]] [[Dark matter|darkening]] | ||
**[[Inner coat|Inner]] layer of [[dermis]] | ** [[Inner coat|Inner]] layer of [[dermis]] | ||
{| | {| | ||
| Line 234: | Line 234: | ||
[[UVA]] & [[UVB radiation|UVB]] have both been implicated in [[Causality|causing]] [[DNA damage]] [[Result|resulting]] in [[Cancer (medicine)|cancer]] by any of the following [[Mechanisms of action|mechanisms]]:<ref name="pmid31237383">{{cite journal| author=Yang Y, Yin R, Wu R, Ramirez CN, Sargsyan D, Li S et al.| title=DNA methylome and transcriptome alterations and cancer prevention by triterpenoid ursolic acid in UVB-induced skin tumor in mice. | journal=Mol Carcinog | year= 2019 | volume= | issue= | pages= | pmid=31237383 | doi=10.1002/mc.23046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237383 }} </ref><ref name="pmid30771437">{{cite journal| author=Yang Y, Wu R, Sargsyan D, Yin R, Kuo HC, Yang I et al.| title=UVB drives different stages of epigenome alterations during progression of skin cancer. | journal=Cancer Lett | year= 2019 | volume= 449 | issue= | pages= 20-30 | pmid=30771437 | doi=10.1016/j.canlet.2019.02.010 | pmc=6411449 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30771437 }} </ref><ref name="pmid25093921">{{cite journal| author=Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y et al.| title=Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models. | journal=Life Sci | year= 2014 | volume= 113 | issue= 1-2 | pages= 45-54 | pmid=25093921 | doi=10.1016/j.lfs.2014.07.031 | pmc=5897904 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25093921 }} </ref><ref name="pmid29466247">{{cite journal| author=Yi Y, Xie H, Xiao X, Wang B, Du R, Liu Y et al.| title=Ultraviolet A irradiation induces senescence in human dermal fibroblasts by down-regulating DNMT1 via ZEB1. | journal=Aging (Albany NY) | year= 2018 | volume= 10 | issue= 2 | pages= 212-228 | pmid=29466247 | doi=10.18632/aging.101383 | pmc=5842848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29466247 }} </ref><ref name="pmid28627622">{{cite journal| author=Zhang C, Yuchi H, Sun L, Zhou X, Lin J| title=Human amnion-derived mesenchymal stem cells protect against UVA irradiation-induced human dermal fibroblast senescence, in vitro. | journal=Mol Med Rep | year= 2017 | volume= 16 | issue= 2 | pages= 2016-2022 | pmid=28627622 | doi=10.3892/mmr.2017.6795 | pmc=5561982 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28627622 }} </ref><ref name="pmid26126510">{{cite journal| author=Zhang C, Wen C, Lin J, Shen G| title=Protective effect of pyrroloquinoline quinine on ultraviolet A irradiation-induced human dermal fibroblast senescence in vitro proceeds via the anti-apoptotic sirtuin 1/nuclear factor-derived erythroid 2-related factor 2/heme oxygenase 1 pathway. | journal=Mol Med Rep | year= 2015 | volume= 12 | issue= 3 | pages= 4382-4388 | pmid=26126510 | doi=10.3892/mmr.2015.3990 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26126510 }} </ref><ref name="pmid28106292">{{cite journal| author=Youn HJ, Kim KB, Han HS, An IS, Ahn KJ| title=23-Hydroxytormentic acid protects human dermal fibroblasts by attenuating UVA-induced oxidative stress. | journal=Photodermatol Photoimmunol Photomed | year= 2017 | volume= 33 | issue= 2 | pages= 92-100 | pmid=28106292 | doi=10.1111/phpp.12294 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28106292 }} </ref><ref name="pmid28142143">{{cite journal| author=Yang S, Zhou B, Xu W, Xue F, Nisar MF, Bian C et al.| title=Nrf2- and Bach1 May Play a Role in the Modulation of Ultraviolet A-Induced Oxidative Stress by Acetyl-11-Keto-β-Boswellic Acid in Skin Keratinocytes. | journal=Skin Pharmacol Physiol | year= 2017 | volume= 30 | issue= 1 | pages= 13-23 | pmid=28142143 | doi=10.1159/000452744 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28142143 }} </ref><ref name="pmid22386815">{{cite journal| author=Hseu YC, Chou CW, Senthil Kumar KJ, Fu KT, Wang HM, Hsu LS et al.| title=Ellagic acid protects human keratinocyte (HaCaT) cells against UVA-induced oxidative stress and apoptosis through the upregulation of the HO-1 and Nrf-2 antioxidant genes. | journal=Food Chem Toxicol | year= 2012 | volume= 50 | issue= 5 | pages= 1245-55 | pmid=22386815 | doi=10.1016/j.fct.2012.02.020 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22386815 }} </ref><ref name="pmid26021820">{{cite journal| author=Hseu YC, Lo HW, Korivi M, Tsai YC, Tang MJ, Yang HL| title=Dermato-protective properties of ergothioneine through induction of Nrf2/ARE-mediated antioxidant genes in UVA-irradiated Human keratinocytes. | journal=Free Radic Biol Med | year= 2015 | volume= 86 | issue= | pages= 102-17 | pmid=26021820 | doi=10.1016/j.freeradbiomed.2015.05.026 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26021820 }} </ref><ref name="pmid30597920">{{cite journal| author=Zhao P, Alam MB, Lee SH| title=Protection of UVB-Induced Photoaging by Fuzhuan-Brick Tea Aqueous Extract via MAPKs/Nrf2-Mediated Down-Regulation of MMP-1. | journal=Nutrients | year= 2018 | volume= 11 | issue= 1 | pages= | pmid=30597920 | doi=10.3390/nu11010060 | pmc=6357030 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30597920 }} </ref><ref name="pmid27641753">{{cite journal| author=Sun Z, Park SY, Hwang E, Zhang M, Seo SA, Lin P et al.| title=Thymus vulgaris alleviates UVB irradiation induced skin damage via inhibition of MAPK/AP-1 and activation of Nrf2-ARE antioxidant system. | journal=J Cell Mol Med | year= 2017 | volume= 21 | issue= 2 | pages= 336-348 | pmid=27641753 | doi=10.1111/jcmm.12968 | pmc=5264136 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27641753 }} </ref><ref name="pmid29748977">{{cite journal| author=Sun Z, Du J, Hwang E, Yi TH| title=Paeonol extracted from Paeonia suffruticosa Andr. ameliorated UVB-induced skin photoaging via DLD/Nrf2/ARE and MAPK/AP-1 pathway. | journal=Phytother Res | year= 2018 | volume= 32 | issue= 9 | pages= 1741-1749 | pmid=29748977 | doi=10.1002/ptr.6100 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29748977 }} </ref><ref name="pmid31237025">{{cite journal| author=Al-Matouq J, Holmes TR, Hansen LA| title=CDC25B and CDC25C overexpression in nonmelanoma skin cancer suppresses cell death. | journal=Mol Carcinog | year= 2019 | volume= | issue= | pages= | pmid=31237025 | doi=10.1002/mc.23075 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237025 }} </ref><ref name="pmid31237010">{{cite journal| author=Sehati N, Sadeghie N, Mansoori B, Mohammadi A, Shanehbandi D, Baradaran B| title=MicroRNA-330 inhibits growth and migration of melanoma A375 cells: In vitro study. | journal=J Cell Biochem | year= 2019 | volume= | issue= | pages= | pmid=31237010 | doi=10.1002/jcb.29211 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237010 }} </ref><ref name="pmid30286469">{{cite journal| author=Xiong Y, Liu L, Qiu Y, Liu L| title=MicroRNA-29a Inhibits Growth, Migration and Invasion of Melanoma A375 Cells in Vitro by Directly Targeting BMI1. | journal=Cell Physiol Biochem | year= 2018 | volume= 50 | issue= 1 | pages= 385-397 | pmid=30286469 | doi=10.1159/000494015 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30286469 }} </ref><ref name="pmid27533779">{{cite journal| author=Mao XH, Chen M, Wang Y, Cui PG, Liu SB, Xu ZY| title=MicroRNA-21 regulates the ERK/NF-κB signaling pathway to affect the proliferation, migration, and apoptosis of human melanoma A375 cells by targeting SPRY1, PDCD4, and PTEN. | journal=Mol Carcinog | year= 2017 | volume= 56 | issue= 3 | pages= 886-894 | pmid=27533779 | doi=10.1002/mc.22542 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27533779 }} </ref><ref name="pmid30545089">{{cite journal| author=Orioli D, Dellambra E| title=Epigenetic Regulation of Skin Cells in Natural Aging and Premature Aging Diseases. | journal=Cells | year= 2018 | volume= 7 | issue= 12 | pages= | pmid=30545089 | doi=10.3390/cells7120268 | pmc=6315602 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30545089 }} </ref> | [[UVA]] & [[UVB radiation|UVB]] have both been implicated in [[Causality|causing]] [[DNA damage]] [[Result|resulting]] in [[Cancer (medicine)|cancer]] by any of the following [[Mechanisms of action|mechanisms]]:<ref name="pmid31237383">{{cite journal| author=Yang Y, Yin R, Wu R, Ramirez CN, Sargsyan D, Li S et al.| title=DNA methylome and transcriptome alterations and cancer prevention by triterpenoid ursolic acid in UVB-induced skin tumor in mice. | journal=Mol Carcinog | year= 2019 | volume= | issue= | pages= | pmid=31237383 | doi=10.1002/mc.23046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237383 }} </ref><ref name="pmid30771437">{{cite journal| author=Yang Y, Wu R, Sargsyan D, Yin R, Kuo HC, Yang I et al.| title=UVB drives different stages of epigenome alterations during progression of skin cancer. | journal=Cancer Lett | year= 2019 | volume= 449 | issue= | pages= 20-30 | pmid=30771437 | doi=10.1016/j.canlet.2019.02.010 | pmc=6411449 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30771437 }} </ref><ref name="pmid25093921">{{cite journal| author=Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y et al.| title=Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models. | journal=Life Sci | year= 2014 | volume= 113 | issue= 1-2 | pages= 45-54 | pmid=25093921 | doi=10.1016/j.lfs.2014.07.031 | pmc=5897904 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25093921 }} </ref><ref name="pmid29466247">{{cite journal| author=Yi Y, Xie H, Xiao X, Wang B, Du R, Liu Y et al.| title=Ultraviolet A irradiation induces senescence in human dermal fibroblasts by down-regulating DNMT1 via ZEB1. | journal=Aging (Albany NY) | year= 2018 | volume= 10 | issue= 2 | pages= 212-228 | pmid=29466247 | doi=10.18632/aging.101383 | pmc=5842848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29466247 }} </ref><ref name="pmid28627622">{{cite journal| author=Zhang C, Yuchi H, Sun L, Zhou X, Lin J| title=Human amnion-derived mesenchymal stem cells protect against UVA irradiation-induced human dermal fibroblast senescence, in vitro. | journal=Mol Med Rep | year= 2017 | volume= 16 | issue= 2 | pages= 2016-2022 | pmid=28627622 | doi=10.3892/mmr.2017.6795 | pmc=5561982 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28627622 }} </ref><ref name="pmid26126510">{{cite journal| author=Zhang C, Wen C, Lin J, Shen G| title=Protective effect of pyrroloquinoline quinine on ultraviolet A irradiation-induced human dermal fibroblast senescence in vitro proceeds via the anti-apoptotic sirtuin 1/nuclear factor-derived erythroid 2-related factor 2/heme oxygenase 1 pathway. | journal=Mol Med Rep | year= 2015 | volume= 12 | issue= 3 | pages= 4382-4388 | pmid=26126510 | doi=10.3892/mmr.2015.3990 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26126510 }} </ref><ref name="pmid28106292">{{cite journal| author=Youn HJ, Kim KB, Han HS, An IS, Ahn KJ| title=23-Hydroxytormentic acid protects human dermal fibroblasts by attenuating UVA-induced oxidative stress. | journal=Photodermatol Photoimmunol Photomed | year= 2017 | volume= 33 | issue= 2 | pages= 92-100 | pmid=28106292 | doi=10.1111/phpp.12294 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28106292 }} </ref><ref name="pmid28142143">{{cite journal| author=Yang S, Zhou B, Xu W, Xue F, Nisar MF, Bian C et al.| title=Nrf2- and Bach1 May Play a Role in the Modulation of Ultraviolet A-Induced Oxidative Stress by Acetyl-11-Keto-β-Boswellic Acid in Skin Keratinocytes. | journal=Skin Pharmacol Physiol | year= 2017 | volume= 30 | issue= 1 | pages= 13-23 | pmid=28142143 | doi=10.1159/000452744 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28142143 }} </ref><ref name="pmid22386815">{{cite journal| author=Hseu YC, Chou CW, Senthil Kumar KJ, Fu KT, Wang HM, Hsu LS et al.| title=Ellagic acid protects human keratinocyte (HaCaT) cells against UVA-induced oxidative stress and apoptosis through the upregulation of the HO-1 and Nrf-2 antioxidant genes. | journal=Food Chem Toxicol | year= 2012 | volume= 50 | issue= 5 | pages= 1245-55 | pmid=22386815 | doi=10.1016/j.fct.2012.02.020 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22386815 }} </ref><ref name="pmid26021820">{{cite journal| author=Hseu YC, Lo HW, Korivi M, Tsai YC, Tang MJ, Yang HL| title=Dermato-protective properties of ergothioneine through induction of Nrf2/ARE-mediated antioxidant genes in UVA-irradiated Human keratinocytes. | journal=Free Radic Biol Med | year= 2015 | volume= 86 | issue= | pages= 102-17 | pmid=26021820 | doi=10.1016/j.freeradbiomed.2015.05.026 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26021820 }} </ref><ref name="pmid30597920">{{cite journal| author=Zhao P, Alam MB, Lee SH| title=Protection of UVB-Induced Photoaging by Fuzhuan-Brick Tea Aqueous Extract via MAPKs/Nrf2-Mediated Down-Regulation of MMP-1. | journal=Nutrients | year= 2018 | volume= 11 | issue= 1 | pages= | pmid=30597920 | doi=10.3390/nu11010060 | pmc=6357030 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30597920 }} </ref><ref name="pmid27641753">{{cite journal| author=Sun Z, Park SY, Hwang E, Zhang M, Seo SA, Lin P et al.| title=Thymus vulgaris alleviates UVB irradiation induced skin damage via inhibition of MAPK/AP-1 and activation of Nrf2-ARE antioxidant system. | journal=J Cell Mol Med | year= 2017 | volume= 21 | issue= 2 | pages= 336-348 | pmid=27641753 | doi=10.1111/jcmm.12968 | pmc=5264136 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27641753 }} </ref><ref name="pmid29748977">{{cite journal| author=Sun Z, Du J, Hwang E, Yi TH| title=Paeonol extracted from Paeonia suffruticosa Andr. ameliorated UVB-induced skin photoaging via DLD/Nrf2/ARE and MAPK/AP-1 pathway. | journal=Phytother Res | year= 2018 | volume= 32 | issue= 9 | pages= 1741-1749 | pmid=29748977 | doi=10.1002/ptr.6100 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29748977 }} </ref><ref name="pmid31237025">{{cite journal| author=Al-Matouq J, Holmes TR, Hansen LA| title=CDC25B and CDC25C overexpression in nonmelanoma skin cancer suppresses cell death. | journal=Mol Carcinog | year= 2019 | volume= | issue= | pages= | pmid=31237025 | doi=10.1002/mc.23075 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237025 }} </ref><ref name="pmid31237010">{{cite journal| author=Sehati N, Sadeghie N, Mansoori B, Mohammadi A, Shanehbandi D, Baradaran B| title=MicroRNA-330 inhibits growth and migration of melanoma A375 cells: In vitro study. | journal=J Cell Biochem | year= 2019 | volume= | issue= | pages= | pmid=31237010 | doi=10.1002/jcb.29211 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31237010 }} </ref><ref name="pmid30286469">{{cite journal| author=Xiong Y, Liu L, Qiu Y, Liu L| title=MicroRNA-29a Inhibits Growth, Migration and Invasion of Melanoma A375 Cells in Vitro by Directly Targeting BMI1. | journal=Cell Physiol Biochem | year= 2018 | volume= 50 | issue= 1 | pages= 385-397 | pmid=30286469 | doi=10.1159/000494015 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30286469 }} </ref><ref name="pmid27533779">{{cite journal| author=Mao XH, Chen M, Wang Y, Cui PG, Liu SB, Xu ZY| title=MicroRNA-21 regulates the ERK/NF-κB signaling pathway to affect the proliferation, migration, and apoptosis of human melanoma A375 cells by targeting SPRY1, PDCD4, and PTEN. | journal=Mol Carcinog | year= 2017 | volume= 56 | issue= 3 | pages= 886-894 | pmid=27533779 | doi=10.1002/mc.22542 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27533779 }} </ref><ref name="pmid30545089">{{cite journal| author=Orioli D, Dellambra E| title=Epigenetic Regulation of Skin Cells in Natural Aging and Premature Aging Diseases. | journal=Cells | year= 2018 | volume= 7 | issue= 12 | pages= | pmid=30545089 | doi=10.3390/cells7120268 | pmc=6315602 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30545089 }} </ref> | ||
*[[UV radiation]] [[Induced activity|induces]] [[Histone 3' UTR stem-loop|histone]] 3 [[methylation]] [[Change detection|changes]] in the [[gene]] [[promoters]] of [[MMP1|matrix metalloproteinase 1]] and [[MMP3]] in primary [[human]] [[dermal]] [[fibroblasts]] [[Lead|leading]] to the increased [[Expression (genetics)|expression]] of [[MMP1]] and [[MMP3]]<ref name="pmid25707437">{{cite journal| author=Gesumaria L, Matsui MS, Kluz T, Costa M| title=Solar-simulated ultraviolet radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinases 1 and 3 in primary human dermal fibroblasts. | journal=Exp Dermatol | year= 2015 | volume= 24 | issue= 5 | pages= 384-5 | pmid=25707437 | doi=10.1111/exd.12675 | pmc=4471858 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25707437 }} </ref> | * [[UV radiation]] [[Induced activity|induces]] [[Histone 3' UTR stem-loop|histone]] 3 [[methylation]] [[Change detection|changes]] in the [[gene]] [[promoters]] of [[MMP1|matrix metalloproteinase 1]] and [[MMP3]] in primary [[human]] [[dermal]] [[fibroblasts]] [[Lead|leading]] to the increased [[Expression (genetics)|expression]] of [[MMP1]] and [[MMP3]]<ref name="pmid25707437">{{cite journal| author=Gesumaria L, Matsui MS, Kluz T, Costa M| title=Solar-simulated ultraviolet radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinases 1 and 3 in primary human dermal fibroblasts. | journal=Exp Dermatol | year= 2015 | volume= 24 | issue= 5 | pages= 384-5 | pmid=25707437 | doi=10.1111/exd.12675 | pmc=4471858 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25707437 }} </ref> | ||
*[[UVB radiation|UVB irradiation]] [[Lead|leads]] to [[DNA]] [[CpG site|CpG]] [[methylation]] and [[Transcriptomics|transcriptomic]] [[Change detection|changes]] in following [[genes]] & [[Cancer (medicine)|cancer]] [[Related phenomena|related]] pathways at the different stages of [[carcinogenesis]]: | * [[UVB radiation|UVB irradiation]] [[Lead|leads]] to [[DNA]] [[CpG site|CpG]] [[methylation]] and [[Transcriptomics|transcriptomic]] [[Change detection|changes]] in following [[genes]] & [[Cancer (medicine)|cancer]] [[Related phenomena|related]] pathways at the different stages of [[carcinogenesis]]: | ||
**[[PTEN (gene)|PTEN]] | ** [[PTEN (gene)|PTEN]] | ||
**[[p53]] | ** [[p53]] | ||
**Nrf2 | ** Nrf2 | ||
**[[p21]](Waf1/Cip1) | ** [[p21]](Waf1/Cip1) | ||
**[[Inflammatory]] [[Signaling pathway|signaling]] | ** [[Inflammatory]] [[Signaling pathway|signaling]] | ||
**Enf2 | ** Enf2 | ||
**Mgst2 | ** Mgst2 | ||
**Vegfa | ** Vegfa | ||
**Cdk4 | ** Cdk4 | ||
*[[UVA radiation|UVA irradiation]] [[causes]] an increase in [[intracellular]] [[reactive oxygen species]] ([[ROS1|ROS]]), [[PGE2|prostaglandin E2]] ([[PGE2]]), and [[Prostaglandin E2 receptor|PGE2 receptors]], which [[Lead|leads]] to decreased [[expression]] of [[transcription factor]] [[zinc finger]] [[E-box]] [[binding]] [[homeobox]] 1([[ZEB1]]) which [[Binding|binds]] to [[DNA methyltransferase]] 1 ([[DNMT1]]) [[promoter]] and regulates its [[Transcription (genetics)|transcription]], thus [[Lead|leading]] to [[senescence]] of [[DNMT1]] in [[human]] [[dermal]] [[fibroblasts]] ([[HDFP|HDFs]]). This [[causes]] low [[methylation]] [[Leveling effect|level]] of [[senescence]] related [[proteins]] [[P53 (protein)|p53]] thus, increasing its [[Expression (genetics)|expression]], eventually [[Result|resulting]] in [[cellular]] [[senescence]]<ref name="pmid29466247">{{cite journal| author=Yi Y, Xie H, Xiao X, Wang B, Du R, Liu Y et al.| title=Ultraviolet A irradiation induces senescence in human dermal fibroblasts by down-regulating DNMT1 via ZEB1. | journal=Aging (Albany NY) | year= 2018 | volume= 10 | issue= 2 | pages= 212-228 | pmid=29466247 | doi=10.18632/aging.101383 | pmc=5842848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29466247 }} </ref><ref name="pmid23820721">{{cite journal| author=Gilchrest BA| title=Photoaging. | journal=J Invest Dermatol | year= 2013 | volume= 133 | issue= E1 | pages= E2-6 | pmid=23820721 | doi=10.1038/skinbio.2013.176 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23820721 }} </ref><ref name="pmid25351668">{{cite journal| author=Poon F, Kang S, Chien AL| title=Mechanisms and treatments of photoaging. | journal=Photodermatol Photoimmunol Photomed | year= 2015 | volume= 31 | issue= 2 | pages= 65-74 | pmid=25351668 | doi=10.1111/phpp.12145 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25351668 }} </ref><ref name="pmid23463292">{{cite journal| author=Xie H, Liu F, Liu L, Dan J, Luo Y, Yi Y et al.| title=Protective role of AQP3 in UVA-induced NHSFs apoptosis via Bcl2 up-regulation. | journal=Arch Dermatol Res | year= 2013 | volume= 305 | issue= 5 | pages= 397-406 | pmid=23463292 | doi=10.1007/s00403-013-1324-y | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23463292 }} </ref><ref name="pmid25234829">{{cite journal| author=Battie C, Jitsukawa S, Bernerd F, Del Bino S, Marionnet C, Verschoore M| title=New insights in photoaging, UVA induced damage and skin types. | journal=Exp Dermatol | year= 2014 | volume= 23 Suppl 1 | issue= | pages= 7-12 | pmid=25234829 | doi=10.1111/exd.12388 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25234829 }} </ref><ref name="pmid22265401">{{cite journal| author=Rando TA, Chang HY| title=Aging, rejuvenation, and epigenetic reprogramming: resetting the aging clock. | journal=Cell | year= 2012 | volume= 148 | issue= 1-2 | pages= 46-57 | pmid=22265401 | doi=10.1016/j.cell.2012.01.003 | pmc=3336960 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22265401 }} </ref><ref name="pmid27004597">{{cite journal| author=Bormann F, Rodríguez-Paredes M, Hagemann S, Manchanda H, Kristof B, Gutekunst J et al.| title=Reduced DNA methylation patterning and transcriptional connectivity define human skin aging. | journal=Aging Cell | year= 2016 | volume= 15 | issue= 3 | pages= 563-71 | pmid=27004597 | doi=10.1111/acel.12470 | pmc=4854925 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27004597 }} </ref><ref name="pmid25707437">{{cite journal| author=Gesumaria L, Matsui MS, Kluz T, Costa M| title=Solar-simulated ultraviolet radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinases 1 and 3 in primary human dermal fibroblasts. | journal=Exp Dermatol | year= 2015 | volume= 24 | issue= 5 | pages= 384-5 | pmid=25707437 | doi=10.1111/exd.12675 | pmc=4471858 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25707437 }} </ref><ref name="pmid19076306">{{cite journal| author=Pollack BP, Sapkota B, Boss JM| title=Ultraviolet radiation-induced transcription is associated with gene-specific histone acetylation. | journal=Photochem Photobiol | year= 2009 | volume= 85 | issue= 3 | pages= 652-62 | pmid=19076306 | doi=10.1111/j.1751-1097.2008.00485.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19076306 }} </ref><ref name="pmid16514663">{{cite journal| author=Zheng QH, Ma LW, Zhu WG, Zhang ZY, Tong TJ| title=p21Waf1/Cip1 plays a critical role in modulating senescence through changes of DNA methylation. | journal=J Cell Biochem | year= 2006 | volume= 98 | issue= 5 | pages= 1230-48 | pmid=16514663 | doi=10.1002/jcb.20838 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16514663 }} </ref><ref name="pmid21572997">{{cite journal| author=So AY, Jung JW, Lee S, Kim HS, Kang KS| title=DNA methyltransferase controls stem cell aging by regulating BMI1 and EZH2 through microRNAs. | journal=PLoS One | year= 2011 | volume= 6 | issue= 5 | pages= e19503 | pmid=21572997 | doi=10.1371/journal.pone.0019503 | pmc=3091856 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21572997 }} </ref><ref name="pmid21507356">{{cite journal| author=Kinney SR, Pradhan S| title=Regulation of expression and activity of DNA (cytosine-5) methyltransferases in mammalian cells. | journal=Prog Mol Biol Transl Sci | year= 2011 | volume= 101 | issue= | pages= 311-33 | pmid=21507356 | doi=10.1016/B978-0-12-387685-0.00009-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21507356 }} </ref><ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref><ref name="pmid18311151">{{cite journal| author=Benetti R, Gonzalo S, Jaco I, Muñoz P, Gonzalez S, Schoeftner S et al.| title=A mammalian microRNA cluster controls DNA methylation and telomere recombination via Rbl2-dependent regulation of DNA methyltransferases. | journal=Nat Struct Mol Biol | year= 2008 | volume= 15 | issue= 3 | pages= 268-79 | pmid=18311151 | doi=10.1038/nsmb.1399 | pmc=2990406 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18311151 }} </ref><ref name="pmid22894906">{{cite journal| author=Kar S, Deb M, Sengupta D, Shilpi A, Parbin S, Torrisani J et al.| title=An insight into the various regulatory mechanisms modulating human DNA methyltransferase 1 stability and function. | journal=Epigenetics | year= 2012 | volume= 7 | issue= 9 | pages= 994-1007 | pmid=22894906 | doi=10.4161/epi.21568 | pmc=3515020 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22894906 }} </ref><ref name="pmid27482540">{{cite journal| author=Pal S, Tyler JK| title=Epigenetics and aging. | journal=Sci Adv | year= 2016 | volume= 2 | issue= 7 | pages= e1600584 | pmid=27482540 | doi=10.1126/sciadv.1600584 | pmc=4966880 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27482540 }} </ref><ref name="pmid27019618">{{cite journal| author=Sierra MI, Fernández AF, Fraga MF| title=Epigenetics of Aging. | journal=Curr Genomics | year= 2015 | volume= 16 | issue= 6 | pages= 435-40 | pmid=27019618 | doi=10.2174/1389202916666150817203459 | pmc=4765531 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27019618 }} </ref><ref name="pmid25637097">{{cite journal| author=Jung M, Pfeifer GP| title=Aging and DNA methylation. | journal=BMC Biol | year= 2015 | volume= 13 | issue= | pages= 7 | pmid=25637097 | doi=10.1186/s12915-015-0118-4 | pmc=4311512 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25637097 }} </ref><ref name="pmid25093921">{{cite journal| author=Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y et al.| title=Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models. | journal=Life Sci | year= 2014 | volume= 113 | issue= 1-2 | pages= 45-54 | pmid=25093921 | doi=10.1016/j.lfs.2014.07.031 | pmc=5897904 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25093921 }} </ref><ref name="pmid21186298">{{cite journal| author=Nandakumar V, Vaid M, Tollefsbol TO, Katiyar SK| title=Aberrant DNA hypermethylation patterns lead to transcriptional silencing of tumor suppressor genes in UVB-exposed skin and UVB-induced skin tumors of mice. | journal=Carcinogenesis | year= 2011 | volume= 32 | issue= 4 | pages= 597-604 | pmid=21186298 | doi=10.1093/carcin/bgq282 | pmc=3066413 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21186298 }} </ref><ref name="pmid23814491">{{cite journal| author=Prasad R, Katiyar SK| title=Prostaglandin E2 Promotes UV radiation-induced immune suppression through DNA hypermethylation. | journal=Neoplasia | year= 2013 | volume= 15 | issue= 7 | pages= 795-804 | pmid=23814491 | doi=10.1593/neo.13424 | pmc=3689242 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23814491 }} </ref><ref name="pmid23746838">{{cite journal| author=López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G| title=The hallmarks of aging. | journal=Cell | year= 2013 | volume= 153 | issue= 6 | pages= 1194-217 | pmid=23746838 | doi=10.1016/j.cell.2013.05.039 | pmc=3836174 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23746838 }} </ref><ref name="pmid12743038">{{cite journal| author=Postigo AA| title=Opposing functions of ZEB proteins in the regulation of the TGFbeta/BMP signaling pathway. | journal=EMBO J | year= 2003 | volume= 22 | issue= 10 | pages= 2443-52 | pmid=12743038 | doi=10.1093/emboj/cdg225 | pmc=155983 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12743038 }} </ref><ref name="pmid12743039">{{cite journal| author=Postigo AA, Depp JL, Taylor JJ, Kroll KL| title=Regulation of Smad signaling through a differential recruitment of coactivators and corepressors by ZEB proteins. | journal=EMBO J | year= 2003 | volume= 22 | issue= 10 | pages= 2453-62 | pmid=12743039 | doi=10.1093/emboj/cdg226 | pmc=155984 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12743039 }} </ref><ref name="pmid23098078">{{cite journal| author=Johnson AA, Akman K, Calimport SR, Wuttke D, Stolzing A, de Magalhães JP| title=The role of DNA methylation in aging, rejuvenation, and age-related disease. | journal=Rejuvenation Res | year= 2012 | volume= 15 | issue= 5 | pages= 483-94 | pmid=23098078 | doi=10.1089/rej.2012.1324 | pmc=3482848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23098078 }} </ref><ref name="pmid29685765">{{cite journal| author=Kim HY, Lee DH, Shin MH, Shin HS, Kim MK, Chung JH| title=UV-induced DNA methyltransferase 1 promotes hypermethylation of tissue inhibitor of metalloproteinase 2 in the human skin. | journal=J Dermatol Sci | year= 2018 | volume= 91 | issue= 1 | pages= 19-27 | pmid=29685765 | doi=10.1016/j.jdermsci.2018.03.009 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29685765 }} </ref> | * [[UVA radiation|UVA irradiation]] [[causes]] an increase in [[intracellular]] [[reactive oxygen species]] ([[ROS1|ROS]]), [[PGE2|prostaglandin E2]] ([[PGE2]]), and [[Prostaglandin E2 receptor|PGE2 receptors]], which [[Lead|leads]] to decreased [[expression]] of [[transcription factor]] [[zinc finger]] [[E-box]] [[binding]] [[homeobox]] 1([[ZEB1]]) which [[Binding|binds]] to [[DNA methyltransferase]] 1 ([[DNMT1]]) [[promoter]] and regulates its [[Transcription (genetics)|transcription]], thus [[Lead|leading]] to [[senescence]] of [[DNMT1]] in [[human]] [[dermal]] [[fibroblasts]] ([[HDFP|HDFs]]). This [[causes]] low [[methylation]] [[Leveling effect|level]] of [[senescence]] related [[proteins]] [[P53 (protein)|p53]] thus, increasing its [[Expression (genetics)|expression]], eventually [[Result|resulting]] in [[cellular]] [[senescence]]<ref name="pmid29466247">{{cite journal| author=Yi Y, Xie H, Xiao X, Wang B, Du R, Liu Y et al.| title=Ultraviolet A irradiation induces senescence in human dermal fibroblasts by down-regulating DNMT1 via ZEB1. | journal=Aging (Albany NY) | year= 2018 | volume= 10 | issue= 2 | pages= 212-228 | pmid=29466247 | doi=10.18632/aging.101383 | pmc=5842848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29466247 }} </ref><ref name="pmid23820721">{{cite journal| author=Gilchrest BA| title=Photoaging. | journal=J Invest Dermatol | year= 2013 | volume= 133 | issue= E1 | pages= E2-6 | pmid=23820721 | doi=10.1038/skinbio.2013.176 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23820721 }} </ref><ref name="pmid25351668">{{cite journal| author=Poon F, Kang S, Chien AL| title=Mechanisms and treatments of photoaging. | journal=Photodermatol Photoimmunol Photomed | year= 2015 | volume= 31 | issue= 2 | pages= 65-74 | pmid=25351668 | doi=10.1111/phpp.12145 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25351668 }} </ref><ref name="pmid23463292">{{cite journal| author=Xie H, Liu F, Liu L, Dan J, Luo Y, Yi Y et al.| title=Protective role of AQP3 in UVA-induced NHSFs apoptosis via Bcl2 up-regulation. | journal=Arch Dermatol Res | year= 2013 | volume= 305 | issue= 5 | pages= 397-406 | pmid=23463292 | doi=10.1007/s00403-013-1324-y | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23463292 }} </ref><ref name="pmid25234829">{{cite journal| author=Battie C, Jitsukawa S, Bernerd F, Del Bino S, Marionnet C, Verschoore M| title=New insights in photoaging, UVA induced damage and skin types. | journal=Exp Dermatol | year= 2014 | volume= 23 Suppl 1 | issue= | pages= 7-12 | pmid=25234829 | doi=10.1111/exd.12388 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25234829 }} </ref><ref name="pmid22265401">{{cite journal| author=Rando TA, Chang HY| title=Aging, rejuvenation, and epigenetic reprogramming: resetting the aging clock. | journal=Cell | year= 2012 | volume= 148 | issue= 1-2 | pages= 46-57 | pmid=22265401 | doi=10.1016/j.cell.2012.01.003 | pmc=3336960 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22265401 }} </ref><ref name="pmid27004597">{{cite journal| author=Bormann F, Rodríguez-Paredes M, Hagemann S, Manchanda H, Kristof B, Gutekunst J et al.| title=Reduced DNA methylation patterning and transcriptional connectivity define human skin aging. | journal=Aging Cell | year= 2016 | volume= 15 | issue= 3 | pages= 563-71 | pmid=27004597 | doi=10.1111/acel.12470 | pmc=4854925 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27004597 }} </ref><ref name="pmid25707437">{{cite journal| author=Gesumaria L, Matsui MS, Kluz T, Costa M| title=Solar-simulated ultraviolet radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinases 1 and 3 in primary human dermal fibroblasts. | journal=Exp Dermatol | year= 2015 | volume= 24 | issue= 5 | pages= 384-5 | pmid=25707437 | doi=10.1111/exd.12675 | pmc=4471858 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25707437 }} </ref><ref name="pmid19076306">{{cite journal| author=Pollack BP, Sapkota B, Boss JM| title=Ultraviolet radiation-induced transcription is associated with gene-specific histone acetylation. | journal=Photochem Photobiol | year= 2009 | volume= 85 | issue= 3 | pages= 652-62 | pmid=19076306 | doi=10.1111/j.1751-1097.2008.00485.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19076306 }} </ref><ref name="pmid16514663">{{cite journal| author=Zheng QH, Ma LW, Zhu WG, Zhang ZY, Tong TJ| title=p21Waf1/Cip1 plays a critical role in modulating senescence through changes of DNA methylation. | journal=J Cell Biochem | year= 2006 | volume= 98 | issue= 5 | pages= 1230-48 | pmid=16514663 | doi=10.1002/jcb.20838 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16514663 }} </ref><ref name="pmid21572997">{{cite journal| author=So AY, Jung JW, Lee S, Kim HS, Kang KS| title=DNA methyltransferase controls stem cell aging by regulating BMI1 and EZH2 through microRNAs. | journal=PLoS One | year= 2011 | volume= 6 | issue= 5 | pages= e19503 | pmid=21572997 | doi=10.1371/journal.pone.0019503 | pmc=3091856 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21572997 }} </ref><ref name="pmid21507356">{{cite journal| author=Kinney SR, Pradhan S| title=Regulation of expression and activity of DNA (cytosine-5) methyltransferases in mammalian cells. | journal=Prog Mol Biol Transl Sci | year= 2011 | volume= 101 | issue= | pages= 311-33 | pmid=21507356 | doi=10.1016/B978-0-12-387685-0.00009-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21507356 }} </ref><ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref><ref name="pmid18311151">{{cite journal| author=Benetti R, Gonzalo S, Jaco I, Muñoz P, Gonzalez S, Schoeftner S et al.| title=A mammalian microRNA cluster controls DNA methylation and telomere recombination via Rbl2-dependent regulation of DNA methyltransferases. | journal=Nat Struct Mol Biol | year= 2008 | volume= 15 | issue= 3 | pages= 268-79 | pmid=18311151 | doi=10.1038/nsmb.1399 | pmc=2990406 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18311151 }} </ref><ref name="pmid22894906">{{cite journal| author=Kar S, Deb M, Sengupta D, Shilpi A, Parbin S, Torrisani J et al.| title=An insight into the various regulatory mechanisms modulating human DNA methyltransferase 1 stability and function. | journal=Epigenetics | year= 2012 | volume= 7 | issue= 9 | pages= 994-1007 | pmid=22894906 | doi=10.4161/epi.21568 | pmc=3515020 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22894906 }} </ref><ref name="pmid27482540">{{cite journal| author=Pal S, Tyler JK| title=Epigenetics and aging. | journal=Sci Adv | year= 2016 | volume= 2 | issue= 7 | pages= e1600584 | pmid=27482540 | doi=10.1126/sciadv.1600584 | pmc=4966880 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27482540 }} </ref><ref name="pmid27019618">{{cite journal| author=Sierra MI, Fernández AF, Fraga MF| title=Epigenetics of Aging. | journal=Curr Genomics | year= 2015 | volume= 16 | issue= 6 | pages= 435-40 | pmid=27019618 | doi=10.2174/1389202916666150817203459 | pmc=4765531 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27019618 }} </ref><ref name="pmid25637097">{{cite journal| author=Jung M, Pfeifer GP| title=Aging and DNA methylation. | journal=BMC Biol | year= 2015 | volume= 13 | issue= | pages= 7 | pmid=25637097 | doi=10.1186/s12915-015-0118-4 | pmc=4311512 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25637097 }} </ref><ref name="pmid25093921">{{cite journal| author=Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y et al.| title=Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models. | journal=Life Sci | year= 2014 | volume= 113 | issue= 1-2 | pages= 45-54 | pmid=25093921 | doi=10.1016/j.lfs.2014.07.031 | pmc=5897904 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25093921 }} </ref><ref name="pmid21186298">{{cite journal| author=Nandakumar V, Vaid M, Tollefsbol TO, Katiyar SK| title=Aberrant DNA hypermethylation patterns lead to transcriptional silencing of tumor suppressor genes in UVB-exposed skin and UVB-induced skin tumors of mice. | journal=Carcinogenesis | year= 2011 | volume= 32 | issue= 4 | pages= 597-604 | pmid=21186298 | doi=10.1093/carcin/bgq282 | pmc=3066413 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21186298 }} </ref><ref name="pmid23814491">{{cite journal| author=Prasad R, Katiyar SK| title=Prostaglandin E2 Promotes UV radiation-induced immune suppression through DNA hypermethylation. | journal=Neoplasia | year= 2013 | volume= 15 | issue= 7 | pages= 795-804 | pmid=23814491 | doi=10.1593/neo.13424 | pmc=3689242 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23814491 }} </ref><ref name="pmid23746838">{{cite journal| author=López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G| title=The hallmarks of aging. | journal=Cell | year= 2013 | volume= 153 | issue= 6 | pages= 1194-217 | pmid=23746838 | doi=10.1016/j.cell.2013.05.039 | pmc=3836174 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23746838 }} </ref><ref name="pmid12743038">{{cite journal| author=Postigo AA| title=Opposing functions of ZEB proteins in the regulation of the TGFbeta/BMP signaling pathway. | journal=EMBO J | year= 2003 | volume= 22 | issue= 10 | pages= 2443-52 | pmid=12743038 | doi=10.1093/emboj/cdg225 | pmc=155983 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12743038 }} </ref><ref name="pmid12743039">{{cite journal| author=Postigo AA, Depp JL, Taylor JJ, Kroll KL| title=Regulation of Smad signaling through a differential recruitment of coactivators and corepressors by ZEB proteins. | journal=EMBO J | year= 2003 | volume= 22 | issue= 10 | pages= 2453-62 | pmid=12743039 | doi=10.1093/emboj/cdg226 | pmc=155984 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12743039 }} </ref><ref name="pmid23098078">{{cite journal| author=Johnson AA, Akman K, Calimport SR, Wuttke D, Stolzing A, de Magalhães JP| title=The role of DNA methylation in aging, rejuvenation, and age-related disease. | journal=Rejuvenation Res | year= 2012 | volume= 15 | issue= 5 | pages= 483-94 | pmid=23098078 | doi=10.1089/rej.2012.1324 | pmc=3482848 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23098078 }} </ref><ref name="pmid29685765">{{cite journal| author=Kim HY, Lee DH, Shin MH, Shin HS, Kim MK, Chung JH| title=UV-induced DNA methyltransferase 1 promotes hypermethylation of tissue inhibitor of metalloproteinase 2 in the human skin. | journal=J Dermatol Sci | year= 2018 | volume= 91 | issue= 1 | pages= 19-27 | pmid=29685765 | doi=10.1016/j.jdermsci.2018.03.009 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29685765 }} </ref> | ||
{{Family tree/start}} | {{Family tree/start}} | ||
{{Family tree | | | | A01 | | | |A01= [[UVA]] exposure to the [[sun]]-exposed [[skin]]}} | {{Family tree | | | | A01 | | | |A01= [[UVA]] exposure to the [[sun]]-exposed [[skin]]}} | ||
| Line 260: | Line 260: | ||
{{Family tree | | | | |!| | | | | }} | {{Family tree | | | | |!| | | | | }} | ||
{{Family tree | | | | G01 | | | |G01= This leads to: | {{Family tree | | | | G01 | | | |G01= This leads to: | ||
*Low [[methylation]] level of [[senescence]] related [[proteins]] [[p53]], thus, increased [[expression]] | * Low [[methylation]] level of [[senescence]] related [[proteins]] [[p53]], thus, increased [[expression]] | ||
*Hypermethylation of [[tissue]] [[inhibitor]] of [[metalloproteinase]] 2 ([[TIMP2]])}} | * Hypermethylation of [[tissue]] [[inhibitor]] of [[metalloproteinase]] 2 ([[TIMP2]])}} | ||
{{Family tree | | | | |!| | | | | }} | {{Family tree | | | | |!| | | | | }} | ||
{{Family tree | | | | H01 | | | |H01= [[Cellular]] [[senescence]]}} | {{Family tree | | | | H01 | | | |H01= [[Cellular]] [[senescence]]}} | ||
{{Family tree/end}} | {{Family tree/end}} | ||
*[[UV radiation]] [[Lead|leads]] to [[overexpression]] of [[COX-2]] whose end [[Product (chemistry)|product]] is [[PGE2|prostaglandin E2]], involved in [[skin]] [[carcinogenesis]]<ref name="pmid18194346">{{cite journal| author=Rundhaug JE, Fischer SM| title=Cyclo-oxygenase-2 plays a critical role in UV-induced skin carcinogenesis. | journal=Photochem Photobiol | year= 2008 | volume= 84 | issue= 2 | pages= 322-9 | pmid=18194346 | doi=10.1111/j.1751-1097.2007.00261.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18194346 }} </ref><ref name="pmid12126310">{{cite journal| author=An KP, Athar M, Tang X, Katiyar SK, Russo J, Beech J et al.| title=Cyclooxygenase-2 expression in murine and human nonmelanoma skin cancers: implications for therapeutic approaches. | journal=Photochem Photobiol | year= 2002 | volume= 76 | issue= 1 | pages= 73-80 | pmid=12126310 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12126310 }} </ref><ref name="pmid12086405">{{cite journal| author=Fischer SM| title=Is cyclooxygenase-2 important in skin carcinogenesis? | journal=J Environ Pathol Toxicol Oncol | year= 2002 | volume= 21 | issue= 2 | pages= 183-91 | pmid=12086405 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12086405 }} </ref><ref name="pmid10828079">{{cite journal| author=Maldve RE, Kim Y, Muga SJ, Fischer SM| title=Prostaglandin E(2) regulation of cyclooxygenase expression in keratinocytes is mediated via cyclic nucleotide-linked prostaglandin receptors. | journal=J Lipid Res | year= 2000 | volume= 41 | issue= 6 | pages= 873-81 | pmid=10828079 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10828079 }} </ref> | * [[UV radiation]] [[Lead|leads]] to [[overexpression]] of [[COX-2]] whose end [[Product (chemistry)|product]] is [[PGE2|prostaglandin E2]], involved in [[skin]] [[carcinogenesis]]<ref name="pmid18194346">{{cite journal| author=Rundhaug JE, Fischer SM| title=Cyclo-oxygenase-2 plays a critical role in UV-induced skin carcinogenesis. | journal=Photochem Photobiol | year= 2008 | volume= 84 | issue= 2 | pages= 322-9 | pmid=18194346 | doi=10.1111/j.1751-1097.2007.00261.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18194346 }} </ref><ref name="pmid12126310">{{cite journal| author=An KP, Athar M, Tang X, Katiyar SK, Russo J, Beech J et al.| title=Cyclooxygenase-2 expression in murine and human nonmelanoma skin cancers: implications for therapeutic approaches. | journal=Photochem Photobiol | year= 2002 | volume= 76 | issue= 1 | pages= 73-80 | pmid=12126310 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12126310 }} </ref><ref name="pmid12086405">{{cite journal| author=Fischer SM| title=Is cyclooxygenase-2 important in skin carcinogenesis? | journal=J Environ Pathol Toxicol Oncol | year= 2002 | volume= 21 | issue= 2 | pages= 183-91 | pmid=12086405 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12086405 }} </ref><ref name="pmid10828079">{{cite journal| author=Maldve RE, Kim Y, Muga SJ, Fischer SM| title=Prostaglandin E(2) regulation of cyclooxygenase expression in keratinocytes is mediated via cyclic nucleotide-linked prostaglandin receptors. | journal=J Lipid Res | year= 2000 | volume= 41 | issue= 6 | pages= 873-81 | pmid=10828079 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10828079 }} </ref> | ||
*[[Overexpression]] of MiR-211, MiR-217 and miR-377 is [[Association (statistics)|associated]] with [[Suppression (eye)|suppression]] of [[DNMT1|DNMT-1]] [[Mediated transport|mediated]] [[methylation]] of [[P16 (gene)|p16]] and [[PRb protein|pRb]], thus, [[Induced activity|inducing]] [[senescence]] in [[human]] [[skin]] [[fibroblasts]]<ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref><ref name="pmid27237979">{{cite journal| author=Yu H, Yang W| title=MiR-211 is epigenetically regulated by DNMT1 mediated methylation and inhibits EMT of melanoma cells by targeting RAB22A. | journal=Biochem Biophys Res Commun | year= 2016 | volume= 476 | issue= 4 | pages= 400-405 | pmid=27237979 | doi=10.1016/j.bbrc.2016.05.133 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27237979 }} </ref><ref name="pmid24784027">{{cite journal| author=Mancini M, Lena AM, Saintigny G, Mahé C, Di Daniele N, Melino G et al.| title=MicroRNAs in human skin ageing. | journal=Ageing Res Rev | year= 2014 | volume= 17 | issue= | pages= 9-15 | pmid=24784027 | doi=10.1016/j.arr.2014.04.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24784027 }} </ref> | * [[Overexpression]] of MiR-211, MiR-217 and miR-377 is [[Association (statistics)|associated]] with [[Suppression (eye)|suppression]] of [[DNMT1|DNMT-1]] [[Mediated transport|mediated]] [[methylation]] of [[P16 (gene)|p16]] and [[PRb protein|pRb]], thus, [[Induced activity|inducing]] [[senescence]] in [[human]] [[skin]] [[fibroblasts]]<ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref><ref name="pmid27237979">{{cite journal| author=Yu H, Yang W| title=MiR-211 is epigenetically regulated by DNMT1 mediated methylation and inhibits EMT of melanoma cells by targeting RAB22A. | journal=Biochem Biophys Res Commun | year= 2016 | volume= 476 | issue= 4 | pages= 400-405 | pmid=27237979 | doi=10.1016/j.bbrc.2016.05.133 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27237979 }} </ref><ref name="pmid24784027">{{cite journal| author=Mancini M, Lena AM, Saintigny G, Mahé C, Di Daniele N, Melino G et al.| title=MicroRNAs in human skin ageing. | journal=Ageing Res Rev | year= 2014 | volume= 17 | issue= | pages= 9-15 | pmid=24784027 | doi=10.1016/j.arr.2014.04.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24784027 }} </ref> | ||
*MicroRNA-152 and -181a modulate the [[Leveling effect|levels]] of [[Cell adhesion molecule|adhesion proteins]] and [[Extracellular matrix protein|extra-cellular matrix components]], such as [[Integrin|integrin α5]] and [[Collagen XVII|collagen XVI]] hence, in this way [[lead]] to [[senescence]] of [[human]] [[dermal]] [[fibroblasts]]<ref name="pmid23238588">{{cite journal| author=Mancini M, Saintigny G, Mahé C, Annicchiarico-Petruzzelli M, Melino G, Candi E| title=MicroRNA-152 and -181a participate in human dermal fibroblasts senescence acting on cell adhesion and remodeling of the extra-cellular matrix. | journal=Aging (Albany NY) | year= 2012 | volume= 4 | issue= 11 | pages= 843-53 | pmid=23238588 | doi=10.18632/aging.100508 | pmc=3560438 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23238588 }} </ref> | * MicroRNA-152 and -181a modulate the [[Leveling effect|levels]] of [[Cell adhesion molecule|adhesion proteins]] and [[Extracellular matrix protein|extra-cellular matrix components]], such as [[Integrin|integrin α5]] and [[Collagen XVII|collagen XVI]] hence, in this way [[lead]] to [[senescence]] of [[human]] [[dermal]] [[fibroblasts]]<ref name="pmid23238588">{{cite journal| author=Mancini M, Saintigny G, Mahé C, Annicchiarico-Petruzzelli M, Melino G, Candi E| title=MicroRNA-152 and -181a participate in human dermal fibroblasts senescence acting on cell adhesion and remodeling of the extra-cellular matrix. | journal=Aging (Albany NY) | year= 2012 | volume= 4 | issue= 11 | pages= 843-53 | pmid=23238588 | doi=10.18632/aging.100508 | pmc=3560438 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23238588 }} </ref> | ||
*Decreased [[Expression (genetics)|expression]] of [[UHRF1]] ([[ubiquitin]]-like with [[PHD finger protein 7|PHD]] and [[Ring finger|ring finger domains]] 1) is the [[Main effect|main]] initial [[Event (probability theory)|event]] in [[Suppression (eye)|suppressing]] [[DNMT1]]-[[Mediated transport|mediated]] [[DNA methylation]] which increases [[WNT5A]] [[Expression (genetics)|expression]] [[Result|resulting]] in [[consequent]] [[Induction (biology)|induction]] of [[senescence]]<ref name="pmid28100769">{{cite journal| author=Jung HJ, Byun HO, Jee BA, Min S, Jeoun UW, Lee YK et al.| title=The Ubiquitin-like with PHD and Ring Finger Domains 1 (UHRF1)/DNA Methyltransferase 1 (DNMT1) Axis Is a Primary Regulator of Cell Senescence. | journal=J Biol Chem | year= 2017 | volume= 292 | issue= 9 | pages= 3729-3739 | pmid=28100769 | doi=10.1074/jbc.M116.750539 | pmc=5339756 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28100769 }} </ref><ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref> | * Decreased [[Expression (genetics)|expression]] of [[UHRF1]] ([[ubiquitin]]-like with [[PHD finger protein 7|PHD]] and [[Ring finger|ring finger domains]] 1) is the [[Main effect|main]] initial [[Event (probability theory)|event]] in [[Suppression (eye)|suppressing]] [[DNMT1]]-[[Mediated transport|mediated]] [[DNA methylation]] which increases [[WNT5A]] [[Expression (genetics)|expression]] [[Result|resulting]] in [[consequent]] [[Induction (biology)|induction]] of [[senescence]]<ref name="pmid28100769">{{cite journal| author=Jung HJ, Byun HO, Jee BA, Min S, Jeoun UW, Lee YK et al.| title=The Ubiquitin-like with PHD and Ring Finger Domains 1 (UHRF1)/DNA Methyltransferase 1 (DNMT1) Axis Is a Primary Regulator of Cell Senescence. | journal=J Biol Chem | year= 2017 | volume= 292 | issue= 9 | pages= 3729-3739 | pmid=28100769 | doi=10.1074/jbc.M116.750539 | pmc=5339756 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28100769 }} </ref><ref name="pmid28277545">{{cite journal| author=Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY et al.| title=miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1. | journal=Cell Death Dis | year= 2017 | volume= 8 | issue= 3 | pages= e2663 | pmid=28277545 | doi=10.1038/cddis.2017.75 | pmc=5386568 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28277545 }} </ref> | ||
*MicroRNA‐21 is involved in [[Regulation of gene expression|regulation]] of [[Extracellular signal-regulated kinases|ERK]]/[[NF-κB|NF‐κB]] [[signaling pathway]] which [[Affect|affects]] the [[proliferation]], migration, and [[apoptosis]] of [[human]] [[melanoma]] A375 [[Cells (biology)|cells]] by [[Targeted therapy|targeting]] [[SPRY1]], [[PDCD4]], and [[PTEN (gene)|PTEN]] | * MicroRNA‐21 is involved in [[Regulation of gene expression|regulation]] of [[Extracellular signal-regulated kinases|ERK]]/[[NF-κB|NF‐κB]] [[signaling pathway]] which [[Affect|affects]] the [[proliferation]], migration, and [[apoptosis]] of [[human]] [[melanoma]] A375 [[Cells (biology)|cells]] by [[Targeted therapy|targeting]] [[SPRY1]], [[PDCD4]], and [[PTEN (gene)|PTEN]] | ||
{| class="wikitable" | |||
|+Main effects of UV radiation on normal-appearing human skin | |||
! colspan="2" style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Acute}} | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Chronic}} | |||
|- | |||
!style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Molecular/cellular}} | |||
! colspan="2" style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Clinical}} | |||
|- | |||
| | |||
* [[DNA]] photodamage (and its repair)/[[mutation]] ([[Cytosine|C]]/[[Thymine|T]], [[Cytosine|CC]]/[[Thymine|TT]]) | |||
* [[Reactive oxygen species]] | |||
* [[Gene]] and [[protein expression]] | |||
* [[Apoptosis]] | |||
* [[Melanogenesis]] | |||
* [[Langerhans cell]] depletion | |||
* [[Nitric oxide]] [[Release factor|release]] ([[UVA]]) | |||
* [[Vitamin-D]] [[photosynthesis]] | |||
| | |||
* [[Erythema]] | |||
* Tanning | |||
* [[Enhancer|Enhancement]] of [[innate immunity]] | |||
* [[Suppression (eye)|Suppression]] of [[acquired immunity]] | |||
* [[Reduction]] of [[blood pressure]] via [[nitric oxide]] | |||
| | |||
* [[Skin cancer]] | |||
* Photoaging | |||
|} | |||
===Gross Pathology=== | ===Gross Pathology=== | ||
*[[Macroscopic|Macroscopically]], the [[tumor]] is often [[Elevate (organization)|elevated]], fungating, or may be [[Ulcerated lesion|ulcerated]] with [[Irregular lesion|irregular]] [[Borderline|borders]] | * [[Macroscopic|Macroscopically]], the [[tumor]] is often [[Elevate (organization)|elevated]], fungating, or may be [[Ulcerated lesion|ulcerated]] with [[Irregular lesion|irregular]] [[Borderline|borders]] | ||
*[[Malignant melanoma]] [[Appearance|appears]] as a small [[lesion]] having [[Irregular lesion|irregular]] borders & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or [[blue]]-[[black]] | * [[Malignant melanoma]] [[Appearance|appears]] as a small [[lesion]] having [[Irregular lesion|irregular]] borders & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or [[blue]]-[[black]] | ||
*[[Basal cell carcinoma]] [[Appearance|appears]] as a [[Waxy flexibility|waxy]] or a [[Pearly gates|pearly]] [[Bumps on skin|bump]], or a [[brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flat affect|flat]] [[lesion]], or a [[Scab|scabbing]] or a [[bleeding]] [[sore]] that [[Healing|heals]] and returns | * [[Basal cell carcinoma]] [[Appearance|appears]] as a [[Waxy flexibility|waxy]] or a [[Pearly gates|pearly]] [[Bumps on skin|bump]], or a [[brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flat affect|flat]] [[lesion]], or a [[Scab|scabbing]] or a [[bleeding]] [[sore]] that [[Healing|heals]] and returns | ||
*[[Squamous cell carcinoma of the skin|Squamous cell carcinoma]] [[Appearance|appears]] as a [[Red-Al|red]], [[Firming agent|firm]] [[Nodule (medicine)|nodule]] or a [[Flat affect|flat]] [[lesion]] having a [[Crustacean|crusted]], [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | * [[Squamous cell carcinoma of the skin|Squamous cell carcinoma]] [[Appearance|appears]] as a [[Red-Al|red]], [[Firming agent|firm]] [[Nodule (medicine)|nodule]] or a [[Flat affect|flat]] [[lesion]] having a [[Crustacean|crusted]], [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | ||
*[[Bowen's disease]] [[Appearance|appears]] as a [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | * [[Bowen's disease]] [[Appearance|appears]] as a [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | ||
*[[Merkel cell carcinoma]] [[Appearance|appears]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] | * [[Merkel cell carcinoma]] [[Appearance|appears]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] | ||
*[[Kaposi's sarcoma]] [[Appearance|appears]] as [[Purple haze|purple]] or [[Red-Al|red]] [[Patching|patches]] on [[skin]] or [[mucous membrane]] | * [[Kaposi's sarcoma]] [[Appearance|appears]] as [[Purple haze|purple]] or [[Red-Al|red]] [[Patching|patches]] on [[skin]] or [[mucous membrane]] | ||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
*[[Microscopic|Microscopically]], [[Tumor cell|tumor cells]] [[Destroying angel|destroy]] the [[basement membrane]] and [[Formal charge|form]] sheets or [[Compact tissue|compact]] [[Mass|masses]] which [[Invasive (medical)|invade]] the subjacent [[connective tissue]] ([[dermis]])<ref name="pmid29261131">{{cite journal| author=Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C| title=Histology of Non-Melanoma Skin Cancers: An Update. | journal=Biomedicines | year= 2017 | volume= 5 | issue= 4 | pages= | pmid=29261131 | doi=10.3390/biomedicines5040071 | pmc=5744095 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29261131 }} </ref> | * [[Microscopic|Microscopically]], [[Tumor cell|tumor cells]] [[Destroying angel|destroy]] the [[basement membrane]] and [[Formal charge|form]] sheets or [[Compact tissue|compact]] [[Mass|masses]] which [[Invasive (medical)|invade]] the subjacent [[connective tissue]] ([[dermis]])<ref name="pmid29261131">{{cite journal| author=Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C| title=Histology of Non-Melanoma Skin Cancers: An Update. | journal=Biomedicines | year= 2017 | volume= 5 | issue= 4 | pages= | pmid=29261131 | doi=10.3390/biomedicines5040071 | pmc=5744095 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29261131 }} </ref> | ||
*In well-[[Differentiate|differentiated]] [[carcinomas]], [[Tumor cell|tumor cells]] are [[pleomorphic]]/atypical, but resembling [[normal]] [[keratinocytes]] from [[Prickle (protein)|prickle]] layer ([[Large-print|large]], polygonal, with abundant [[eosinophilic]] ([[Pinks|pink]]) [[cytoplasm]] and [[central]] [[Cell nucleus|nucleus]]) | * In well-[[Differentiate|differentiated]] [[carcinomas]], [[Tumor cell|tumor cells]] are [[pleomorphic]]/atypical, but resembling [[normal]] [[keratinocytes]] from [[Prickle (protein)|prickle]] layer ([[Large-print|large]], polygonal, with abundant [[eosinophilic]] ([[Pinks|pink]]) [[cytoplasm]] and [[central]] [[Cell nucleus|nucleus]]) | ||
*Their disposal tends to be [[Similarity matrix|similar]] to that of [[normal]] [[Epidermis (skin)|epidermis]]: immature/[[Basal cell|basal cells]] at the [[periphery]], becoming more mature to the centre of the [[tumor]] [[Mass|masses]] | * Their disposal tends to be [[Similarity matrix|similar]] to that of [[normal]] [[Epidermis (skin)|epidermis]]: immature/[[Basal cell|basal cells]] at the [[periphery]], becoming more mature to the centre of the [[tumor]] [[Mass|masses]] | ||
*[[Tumor cell|Tumor cells]] [[Transformation|transform]] into [[keratinized]] [[Squamous cell|squamous cells]] and [[Formal charge|form]] [[Round face|round]] [[nodules]] with [[concentric]], laminated layers, called "[[Cell (biology)|cell]] nests" or "[[epithelial]]/[[keratinous]] pearls" | * [[Tumor cell|Tumor cells]] [[Transformation|transform]] into [[keratinized]] [[Squamous cell|squamous cells]] and [[Formal charge|form]] [[Round face|round]] [[nodules]] with [[concentric]], laminated layers, called "[[Cell (biology)|cell]] nests" or "[[epithelial]]/[[keratinous]] pearls" | ||
*The surrounding [[stroma]] is [[reduced]] and contains [[inflammatory]] [[Infiltration (medical)|infiltrate]] ([[lymphocytes]]) | * The surrounding [[stroma]] is [[reduced]] and contains [[inflammatory]] [[Infiltration (medical)|infiltrate]] ([[lymphocytes]]) | ||
*Poorly [[Differentiate|differentiated]] [[Squamous cell carcinoma of the skin|squamous carcinomas]] contain more [[pleomorphic]] [[Cells (biology)|cells]] and no [[keratinization]] | * Poorly [[Differentiate|differentiated]] [[Squamous cell carcinoma of the skin|squamous carcinomas]] contain more [[pleomorphic]] [[Cells (biology)|cells]] and no [[keratinization]] | ||
==Causes== | ==Causes== | ||
*[[Skin]] [[cancer]] occurs due to [[mutations]] in [[DNA]] of [[skin]] [[cells]] [[Causality|causing]] them to [[grow]] out of [[control]] [[Lead|leading]] to [[formation]] of a [[mass]] of [[cancer]] [[cells]] | * [[Skin]] [[cancer]] occurs due to [[mutations]] in [[DNA]] of [[skin]] [[cells]] [[Causality|causing]] them to [[grow]] out of [[control]] [[Lead|leading]] to [[formation]] of a [[mass]] of [[cancer]] [[cells]] | ||
==Epidemiology & Demographics== | ==Epidemiology & Demographics== | ||
*[[Skin]] [[cancer]] is a common [[condition]] because of the increased [[Exposure (photography)|exposure]] to [[UV radiation]] ([[Causes|caused]] by increasing [[Popular errors|popularity]] of [[sun tanning]]/[[Sun exposure|sun]] [[Bath salts|bathing]])<ref name="pmid14674897">{{cite journal| author=Katalinic A, Kunze U, Schäfer T| title=Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer). | journal=Br J Dermatol | year= 2003 | volume= 149 | issue= 6 | pages= 1200-6 | pmid=14674897 | doi=10.1111/j.1365-2133.2003.05554.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14674897 }} </ref><ref name="pmid26213814">{{cite journal| author=Rudolph C, Schnoor M, Eisemann N, Katalinic A| title=Incidence trends of nonmelanoma skin cancer in Germany from 1998 to 2010. | journal=J Dtsch Dermatol Ges | year= 2015 | volume= 13 | issue= 8 | pages= 788-97 | pmid=26213814 | doi=10.1111/ddg.12690 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26213814 }} </ref><ref name="pmid19438088">{{cite journal| author=Bulliard JL, Panizzon RG, Levi F| title=[Epidemiology of epithelial skin cancers]. | journal=Rev Med Suisse | year= 2009 | volume= 5 | issue= 200 | pages= 882, 884-8 | pmid=19438088 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19438088 }} </ref><ref name="pmid2233471">{{cite journal| author=Stenbeck KD, Balanda KP, Williams MJ, Ring IT, MacLennan R, Chick JE et al.| title=Patterns of treated non-melanoma skin cancer in Queensland--the region with the highest incidence rates in the world. | journal=Med J Aust | year= 1990 | volume= 153 | issue= 9 | pages= 511-5 | pmid=2233471 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2233471 }} </ref><ref name="pmid2786135">{{cite journal| author=Marks R, Jolley D, Dorevitch AP, Selwood TS| title=The incidence of non-melanocytic skin cancers in an Australian population: results of a five-year prospective study. | journal=Med J Aust | year= 1989 | volume= 150 | issue= 9 | pages= 475-8 | pmid=2786135 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2786135 }} </ref><ref name="pmid6957767">{{cite journal| author=Freeman NR, Fairbrother GE, Rose RJ| title=Survey of skin cancer incidence in the Hamilton area. | journal=N Z Med J | year= 1982 | volume= 95 | issue= 713 | pages= 529-33 | pmid=6957767 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6957767 }} </ref> | * [[Skin]] [[cancer]] is a common [[condition]] because of the increased [[Exposure (photography)|exposure]] to [[UV radiation]] ([[Causes|caused]] by increasing [[Popular errors|popularity]] of [[sun tanning]]/[[Sun exposure|sun]] [[Bath salts|bathing]])<ref name="pmid14674897">{{cite journal| author=Katalinic A, Kunze U, Schäfer T| title=Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer). | journal=Br J Dermatol | year= 2003 | volume= 149 | issue= 6 | pages= 1200-6 | pmid=14674897 | doi=10.1111/j.1365-2133.2003.05554.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14674897 }} </ref><ref name="pmid26213814">{{cite journal| author=Rudolph C, Schnoor M, Eisemann N, Katalinic A| title=Incidence trends of nonmelanoma skin cancer in Germany from 1998 to 2010. | journal=J Dtsch Dermatol Ges | year= 2015 | volume= 13 | issue= 8 | pages= 788-97 | pmid=26213814 | doi=10.1111/ddg.12690 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26213814 }} </ref><ref name="pmid19438088">{{cite journal| author=Bulliard JL, Panizzon RG, Levi F| title=[Epidemiology of epithelial skin cancers]. | journal=Rev Med Suisse | year= 2009 | volume= 5 | issue= 200 | pages= 882, 884-8 | pmid=19438088 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19438088 }} </ref><ref name="pmid2233471">{{cite journal| author=Stenbeck KD, Balanda KP, Williams MJ, Ring IT, MacLennan R, Chick JE et al.| title=Patterns of treated non-melanoma skin cancer in Queensland--the region with the highest incidence rates in the world. | journal=Med J Aust | year= 1990 | volume= 153 | issue= 9 | pages= 511-5 | pmid=2233471 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2233471 }} </ref><ref name="pmid2786135">{{cite journal| author=Marks R, Jolley D, Dorevitch AP, Selwood TS| title=The incidence of non-melanocytic skin cancers in an Australian population: results of a five-year prospective study. | journal=Med J Aust | year= 1989 | volume= 150 | issue= 9 | pages= 475-8 | pmid=2786135 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2786135 }} </ref><ref name="pmid6957767">{{cite journal| author=Freeman NR, Fairbrother GE, Rose RJ| title=Survey of skin cancer incidence in the Hamilton area. | journal=N Z Med J | year= 1982 | volume= 95 | issue= 713 | pages= 529-33 | pmid=6957767 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6957767 }} </ref> | ||
*It is the most common malignancy in Caucasian population<ref name="pmid26902923">{{cite journal| author=Whiteman DC, Green AC, Olsen CM| title=The Growing Burden of Invasive Melanoma: Projections of Incidence Rates and Numbers of New Cases in Six Susceptible Populations through 2031. | journal=J Invest Dermatol | year= 2016 | volume= 136 | issue= 6 | pages= 1161-1171 | pmid=26902923 | doi=10.1016/j.jid.2016.01.035 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26902923 }} </ref><ref name="pmid15519506">{{cite journal| author=de Vries E, Coebergh JW| title=Cutaneous malignant melanoma in Europe. | journal=Eur J Cancer | year= 2004 | volume= 40 | issue= 16 | pages= 2355-66 | pmid=15519506 | doi=10.1016/j.ejca.2004.06.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15519506 }} </ref><ref name="pmid16650166">{{cite journal| author=Lasithiotakis K, Krüger-Krasagakis S, Manousaki A, Ioannidou D, Panagiotides I, Tosca A| title=The incidence of cutaneous melanoma on Crete, Greece. | journal=Int J Dermatol | year= 2006 | volume= 45 | issue= 4 | pages= 397-401 | pmid=16650166 | doi=10.1111/j.1365-4632.2006.02492.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16650166 }} </ref><ref name="pmid12102157">{{cite journal| author=Månsson-Brahme E, Johansson H, Larsson O, Rutqvist LE, Ringborg U| title=Trends in incidence of cutaneous malignant melanoma in a Swedish population 1976-1994. | journal=Acta Oncol | year= 2002 | volume= 41 | issue= 2 | pages= 138-46 | pmid=12102157 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12102157 }} </ref><ref name="pmid16477634">{{cite journal| author=Stang A, Pukkala E, Sankila R, Söderman B, Hakulinen T| title=Time trend analysis of the skin melanoma incidence of Finland from 1953 through 2003 including 16,414 cases. | journal=Int J Cancer | year= 2006 | volume= 119 | issue= 2 | pages= 380-4 | pmid=16477634 | doi=10.1002/ijc.21836 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16477634 }} </ref><ref name="pmid15926213">{{cite journal| author=Ulmer MJ, Tonita JM, Hull PR| title=Trends in invasive cutaneous melanoma in Saskatchewan 1970-1999. | journal=J Cutan Med Surg | year= 2003 | volume= 7 | issue= 6 | pages= 433-42 | pmid=15926213 | doi=10.1177/120347540300700601 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15926213 }} </ref><ref name="pmid10086448">{{cite journal| author=Dennis LK| title=Analysis of the melanoma epidemic, both apparent and real: data from the 1973 through 1994 surveillance, epidemiology, and end results program registry. | journal=Arch Dermatol | year= 1999 | volume= 135 | issue= 3 | pages= 275-80 | pmid=10086448 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10086448 }} </ref><ref name="pmid12365954">{{cite journal| author=Geller AC, Miller DR, Annas GD, Demierre MF, Gilchrest BA, Koh HK| title=Melanoma incidence and mortality among US whites, 1969-1999. | journal=JAMA | year= 2002 | volume= 288 | issue= 14 | pages= 1719-20 | pmid=12365954 | doi=10.1001/jama.288.14.1719 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12365954 }} </ref><ref name="pmid9922010">{{cite journal| author=Hall HI, Miller DR, Rogers JD, Bewerse B| title=Update on the incidence and mortality from melanoma in the United States. | journal=J Am Acad Dermatol | year= 1999 | volume= 40 | issue= 1 | pages= 35-42 | pmid=9922010 | doi=10.1016/s0190-9622(99)70562-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9922010 }} </ref><ref name="pmid25716064">{{cite journal| author=Perera E, Gnaneswaran N, Staines C, Win AK, Sinclair R| title=Incidence and prevalence of non-melanoma skin cancer in Australia: A systematic review. | journal=Australas J Dermatol | year= 2015 | volume= 56 | issue= 4 | pages= 258-67 | pmid=25716064 | doi=10.1111/ajd.12282 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25716064 }} </ref> | * It is the most common malignancy in Caucasian population<ref name="pmid26902923">{{cite journal| author=Whiteman DC, Green AC, Olsen CM| title=The Growing Burden of Invasive Melanoma: Projections of Incidence Rates and Numbers of New Cases in Six Susceptible Populations through 2031. | journal=J Invest Dermatol | year= 2016 | volume= 136 | issue= 6 | pages= 1161-1171 | pmid=26902923 | doi=10.1016/j.jid.2016.01.035 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26902923 }} </ref><ref name="pmid15519506">{{cite journal| author=de Vries E, Coebergh JW| title=Cutaneous malignant melanoma in Europe. | journal=Eur J Cancer | year= 2004 | volume= 40 | issue= 16 | pages= 2355-66 | pmid=15519506 | doi=10.1016/j.ejca.2004.06.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15519506 }} </ref><ref name="pmid16650166">{{cite journal| author=Lasithiotakis K, Krüger-Krasagakis S, Manousaki A, Ioannidou D, Panagiotides I, Tosca A| title=The incidence of cutaneous melanoma on Crete, Greece. | journal=Int J Dermatol | year= 2006 | volume= 45 | issue= 4 | pages= 397-401 | pmid=16650166 | doi=10.1111/j.1365-4632.2006.02492.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16650166 }} </ref><ref name="pmid12102157">{{cite journal| author=Månsson-Brahme E, Johansson H, Larsson O, Rutqvist LE, Ringborg U| title=Trends in incidence of cutaneous malignant melanoma in a Swedish population 1976-1994. | journal=Acta Oncol | year= 2002 | volume= 41 | issue= 2 | pages= 138-46 | pmid=12102157 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12102157 }} </ref><ref name="pmid16477634">{{cite journal| author=Stang A, Pukkala E, Sankila R, Söderman B, Hakulinen T| title=Time trend analysis of the skin melanoma incidence of Finland from 1953 through 2003 including 16,414 cases. | journal=Int J Cancer | year= 2006 | volume= 119 | issue= 2 | pages= 380-4 | pmid=16477634 | doi=10.1002/ijc.21836 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16477634 }} </ref><ref name="pmid15926213">{{cite journal| author=Ulmer MJ, Tonita JM, Hull PR| title=Trends in invasive cutaneous melanoma in Saskatchewan 1970-1999. | journal=J Cutan Med Surg | year= 2003 | volume= 7 | issue= 6 | pages= 433-42 | pmid=15926213 | doi=10.1177/120347540300700601 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15926213 }} </ref><ref name="pmid10086448">{{cite journal| author=Dennis LK| title=Analysis of the melanoma epidemic, both apparent and real: data from the 1973 through 1994 surveillance, epidemiology, and end results program registry. | journal=Arch Dermatol | year= 1999 | volume= 135 | issue= 3 | pages= 275-80 | pmid=10086448 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10086448 }} </ref><ref name="pmid12365954">{{cite journal| author=Geller AC, Miller DR, Annas GD, Demierre MF, Gilchrest BA, Koh HK| title=Melanoma incidence and mortality among US whites, 1969-1999. | journal=JAMA | year= 2002 | volume= 288 | issue= 14 | pages= 1719-20 | pmid=12365954 | doi=10.1001/jama.288.14.1719 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12365954 }} </ref><ref name="pmid9922010">{{cite journal| author=Hall HI, Miller DR, Rogers JD, Bewerse B| title=Update on the incidence and mortality from melanoma in the United States. | journal=J Am Acad Dermatol | year= 1999 | volume= 40 | issue= 1 | pages= 35-42 | pmid=9922010 | doi=10.1016/s0190-9622(99)70562-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9922010 }} </ref><ref name="pmid25716064">{{cite journal| author=Perera E, Gnaneswaran N, Staines C, Win AK, Sinclair R| title=Incidence and prevalence of non-melanoma skin cancer in Australia: A systematic review. | journal=Australas J Dermatol | year= 2015 | volume= 56 | issue= 4 | pages= 258-67 | pmid=25716064 | doi=10.1111/ajd.12282 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25716064 }} </ref> | ||
*[[Individual growth|Individuals]] with [[lighter]]-[[skin]] are more [[Vulnerable populations|vulnerable]] to [[Get involved|get]] it | * [[Individual growth|Individuals]] with [[lighter]]-[[skin]] are more [[Vulnerable populations|vulnerable]] to [[Get involved|get]] it | ||
* One out of every three [[new]] [[cancers]] arises from [[skin]] in [[United States]]<ref name="urlCommon Cancer Types - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/common-cancers?redirect=true |title=Common Cancer Types - National Cancer Institute |format= |work= |accessdate=}}</ref> | * One out of every three [[new]] [[cancers]] arises from [[skin]] in [[United States]]<ref name="urlCommon Cancer Types - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/common-cancers?redirect=true |title=Common Cancer Types - National Cancer Institute |format= |work= |accessdate=}}</ref> | ||
*[[Incidence (epidemiology)|Incidence]] of both [[malignant melanoma]] ([[MM]]) and non-[[melanoma]] [[skin]] [[Cancer (disease)|cancer]] (NMSC) is increasing with [[MM]] having an annual increase of 0.6% in [[Individual growth|individuals]] >50 [[Year|years]]<ref name="urlCancer Facts & Figures 2016 | American Cancer Society">{{cite web |url=https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2016.html |title=Cancer Facts & Figures 2016 | American Cancer Society |format= |work= |accessdate=}}</ref><ref name="pmid16081427">{{cite journal| author=Welch HG, Woloshin S, Schwartz LM| title=Skin biopsy rates and incidence of melanoma: population based ecological study. | journal=BMJ | year= 2005 | volume= 331 | issue= 7515 | pages= 481 | pmid=16081427 | doi=10.1136/bmj.38516.649537.E0 | pmc=1199022 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16081427 }} </ref> | * [[Incidence (epidemiology)|Incidence]] of both [[malignant melanoma]] ([[MM]]) and non-[[melanoma]] [[skin]] [[Cancer (disease)|cancer]] (NMSC) is increasing with [[MM]] having an annual increase of 0.6% in [[Individual growth|individuals]] >50 [[Year|years]]<ref name="urlCancer Facts & Figures 2016 | American Cancer Society">{{cite web |url=https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2016.html |title=Cancer Facts & Figures 2016 | American Cancer Society |format= |work= |accessdate=}}</ref><ref name="pmid16081427">{{cite journal| author=Welch HG, Woloshin S, Schwartz LM| title=Skin biopsy rates and incidence of melanoma: population based ecological study. | journal=BMJ | year= 2005 | volume= 331 | issue= 7515 | pages= 481 | pmid=16081427 | doi=10.1136/bmj.38516.649537.E0 | pmc=1199022 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16081427 }} </ref> | ||
*In 2014, 6500 [[new]] [[Case-based reasoning|cases]] of [[melanoma]] and 76,100 [[Case-based reasoning|cases]] of NMSC were [[Estimate|estimated]] to have occurred in [[Canada Health Act|Canada]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * In 2014, 6500 [[new]] [[Case-based reasoning|cases]] of [[melanoma]] and 76,100 [[Case-based reasoning|cases]] of NMSC were [[Estimate|estimated]] to have occurred in [[Canada Health Act|Canada]]<ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence |journal=Journal of Cutaneous Medicine and Surgery|volume=23|issue=4|year=2019|pages=357–369|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | ||
*In 2016, the [[Estimate|estimated]] [[number]] of [[new]] [[Case-based reasoning|cases]] of [[skin]] [[melanoma]] was 76,380 which is 4.5% of all [[new]] [[Cancer (disease)|cancer]] [[Case-based reasoning|cases]]<ref name="urlMelanoma of the Skin - Cancer Stat Facts">{{cite web |url=https://seer.cancer.gov/statfacts/html/melan.html |title=Melanoma of the Skin - Cancer Stat Facts |format= |work= |accessdate=}}</ref> | * In 2016, the [[Estimate|estimated]] [[number]] of [[new]] [[Case-based reasoning|cases]] of [[skin]] [[melanoma]] was 76,380 which is 4.5% of all [[new]] [[Cancer (disease)|cancer]] [[Case-based reasoning|cases]]<ref name="urlMelanoma of the Skin - Cancer Stat Facts">{{cite web |url=https://seer.cancer.gov/statfacts/html/melan.html |title=Melanoma of the Skin - Cancer Stat Facts |format= |work= |accessdate=}}</ref> | ||
*Annual [[Incidence (epidemiology)|incidence]] of [[melanoma]] [[in situ]] is 9.5% according to some [[Recent changes|recent]] [[Epidemiological study|epidemiological studies]]<ref name="urlMelanoma of the Skin - Cancer Stat Facts">{{cite web |url=https://seer.cancer.gov/statfacts/html/melan.html |title=Melanoma of the Skin - Cancer Stat Facts |format= |work= |accessdate=}}</ref> | * Annual [[Incidence (epidemiology)|incidence]] of [[melanoma]] [[in situ]] is 9.5% according to some [[Recent changes|recent]] [[Epidemiological study|epidemiological studies]]<ref name="urlMelanoma of the Skin - Cancer Stat Facts">{{cite web |url=https://seer.cancer.gov/statfacts/html/melan.html |title=Melanoma of the Skin - Cancer Stat Facts |format= |work= |accessdate=}}</ref> | ||
*National [[Cancer (medicine)|Cancer]] Registries has reported an underestimation of the [[Incidence (epidemiology)|incidence]] of [[melanoma]] in certain countries, hence, its [[Incidence (epidemiology)|incidence]] may even be [[Higher Power|higher]] than actually [[Document classification|documented]] [[Dependent variable|depending]] upon [[Population (statistics)|population]]-[[Base|based]] varying [[risk factors]] and discrepancies in national [[Registration Successful|registration]] [[systems]]<ref name="pmid26802530">{{cite journal| author=Monshi B, Vujic M, Kivaranovic D, Sesti A, Oberaigner W, Vujic I et al.| title=The burden of malignant melanoma--lessons to be learned from Austria. | journal=Eur J Cancer | year= 2016 | volume= 56 | issue= | pages= 45-53 | pmid=26802530 | doi=10.1016/j.ejca.2015.11.026 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26802530 }} </ref> | * National [[Cancer (medicine)|Cancer]] Registries has reported an underestimation of the [[Incidence (epidemiology)|incidence]] of [[melanoma]] in certain countries, hence, its [[Incidence (epidemiology)|incidence]] may even be [[Higher Power|higher]] than actually [[Document classification|documented]] [[Dependent variable|depending]] upon [[Population (statistics)|population]]-[[Base|based]] varying [[risk factors]] and discrepancies in national [[Registration Successful|registration]] [[systems]]<ref name="pmid26802530">{{cite journal| author=Monshi B, Vujic M, Kivaranovic D, Sesti A, Oberaigner W, Vujic I et al.| title=The burden of malignant melanoma--lessons to be learned from Austria. | journal=Eur J Cancer | year= 2016 | volume= 56 | issue= | pages= 45-53 | pmid=26802530 | doi=10.1016/j.ejca.2015.11.026 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26802530 }} </ref> | ||
==Risk factors== | ==Risk factors== | ||
| Line 311: | Line 339: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Excess risk|Excessive]] [[sun exposure]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Excess risk|Excessive]] [[sun exposure]] | ||
| | | | ||
*[[Sun exposure|Sun]] [[Bath salts|bathing]] | * [[Sun exposure|Sun]] [[Bath salts|bathing]] | ||
*Especially early in [[life]] can lead to [[skin]] damage and even [[sunburn]] if [[skin]] isn't [[Protected health information|protected]] by: | * Especially early in [[life]] can lead to [[skin]] damage and even [[sunburn]] if [[skin]] isn't [[Protected health information|protected]] by: | ||
**Clothing | ** Clothing | ||
**[[Sunscreen]] | ** [[Sunscreen]] | ||
* [[Sun exposure]] between 10AM and 4PM is considered to be most harmful | * [[Sun exposure]] between 10AM and 4PM is considered to be most harmful | ||
|- | |- | ||
| Line 320: | Line 348: | ||
|[[Tanning activator|Tanning]] is the [[Response element|response]] of [[skin]] to [[Excess risk|excessive]] [[UV radiation|UV radiations]]: | |[[Tanning activator|Tanning]] is the [[Response element|response]] of [[skin]] to [[Excess risk|excessive]] [[UV radiation|UV radiations]]: | ||
*[[Tanning booths|Tanning salons]] | * [[Tanning booths|Tanning salons]] | ||
*Tanning lamps | * Tanning lamps | ||
*Tanning beds | * Tanning beds | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Fair use|Fair]] [[skin]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Fair use|Fair]] [[skin]] | ||
| | | | ||
* Less [[melanin]] [[pigment]] in the [[skin]] means less [[Protecting group|protection]] from damaging [[UV radiation]] | * Less [[melanin]] [[pigment]] in the [[skin]] means less [[Protecting group|protection]] from damaging [[UV radiation]] | ||
*Having a [[Fair use|fair]] [[complexion]] includes the following: | * Having a [[Fair use|fair]] [[complexion]] includes the following: | ||
**[[Fair use|Fair]] [[skin]] that [[burns]] and [[freckles]] easily, does not [[Tanning oil|tan]], or [[Tanning oil|tans]] poorly | ** [[Fair use|Fair]] [[skin]] that [[burns]] and [[freckles]] easily, does not [[Tanning oil|tan]], or [[Tanning oil|tans]] poorly | ||
**Blond or [[Red-Al|red]] [[hair]] | ** Blond or [[Red-Al|red]] [[hair]] | ||
**[[Green S|Green]], [[blue]], or other [[light]]-[[Color|colored]] [[eyes]] | ** [[Green S|Green]], [[blue]], or other [[light]]-[[Color|colored]] [[eyes]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Genetic predisposition]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Genetic predisposition]] | ||
| | | | ||
* '''[[Congenital]] [[Melanocytic naevi|Melanocytic Nevi]] [[Syndrome]]''' is [[Characterization (mathematics)|characterized]] by: | * '''[[Congenital]] [[Melanocytic naevi|Melanocytic Nevi]] [[Syndrome]]''' is [[Characterization (mathematics)|characterized]] by: | ||
**[[Presenting symptom|Presence]] of varying [[Size consistency|sized]] "[[nevi]]" or [[moles]] | ** [[Presenting symptom|Presence]] of varying [[Size consistency|sized]] "[[nevi]]" or [[moles]] | ||
** [[Appearance|Appear]] at or within 6 months of [[birth]] | ** [[Appearance|Appear]] at or within 6 months of [[birth]] | ||
** [[Nevi]] larger than 20 mm (3/4") in [[Size consistency|size]] are at higher [[RiskMetrics|risk]] for becoming [[cancerous]] | ** [[Nevi]] larger than 20 mm (3/4") in [[Size consistency|size]] are at higher [[RiskMetrics|risk]] for becoming [[cancerous]] | ||
| Line 360: | Line 388: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Moles]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Moles]] | ||
| | | | ||
*Having large number of [[moles]] increases the chances of having [[skin]] [[cancer]] in future | * Having large number of [[moles]] increases the chances of having [[skin]] [[cancer]] in future | ||
*'''[[Dysplastic nevi]]''' which are multiple [[abnormal]] [[Irregular lesion|irregular]] [[moles]], have increased tendency to become [[cancerous]] | *'''[[Dysplastic nevi]]''' which are multiple [[abnormal]] [[Irregular lesion|irregular]] [[moles]], have increased tendency to become [[cancerous]] | ||
|- | |- | ||
| Line 382: | Line 410: | ||
| | | | ||
* There's an increased [[RiskMetrics|risk]] for [[development]] of [[skin]] [[Cancer (disease)|cancer]] (especially [[basal cell carcinoma]]) in [[Individual growth|individuals]] with a prior [[History and Physical examination|history]] of [[radiation therapy]] for [[skin]] [[conditions]] such as: | * There's an increased [[RiskMetrics|risk]] for [[development]] of [[skin]] [[Cancer (disease)|cancer]] (especially [[basal cell carcinoma]]) in [[Individual growth|individuals]] with a prior [[History and Physical examination|history]] of [[radiation therapy]] for [[skin]] [[conditions]] such as: | ||
**[[Acne]] | ** [[Acne]] | ||
** [[Eczema]] | ** [[Eczema]] | ||
|- | |- | ||
| Line 404: | Line 432: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Beta-1|Beta]]-[[Human Papilloma Virus]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Beta-1|Beta]]-[[Human Papilloma Virus]] | ||
| | | | ||
*[[HPV infection]] is [[Association (statistics)|associated]] with increased [[RiskMetrics|risk]] of [[BCC]] | * [[HPV infection]] is [[Association (statistics)|associated]] with increased [[RiskMetrics|risk]] of [[BCC]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Male]] [[Gender-based medicine|gender]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Male]] [[Gender-based medicine|gender]] | ||
| Line 412: | Line 440: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Prolonged [[skin]] [[inflammation]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Prolonged [[skin]] [[inflammation]] | ||
| | | | ||
*Having a [[skin]] [[inflammation]] that has lasted for prolonged [[periods]] of [[Time constant|time]] also [[Predisposition|predisposes]] to the [[Development (biology)|development]] of [[skin]] [[Cancer (medicine)|cancer]] | * Having a [[skin]] [[inflammation]] that has lasted for prolonged [[periods]] of [[Time constant|time]] also [[Predisposition|predisposes]] to the [[Development (biology)|development]] of [[skin]] [[Cancer (medicine)|cancer]] | ||
|} | |} | ||
| Line 418: | Line 446: | ||
According to different [[Study design|studies]] going on for so many [[Year|years]], following [[data]] is available regarding the different [[Method of Levels|methods]]/tools and their [[Effective method|effectiveness]] for [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]]: | According to different [[Study design|studies]] going on for so many [[Year|years]], following [[data]] is available regarding the different [[Method of Levels|methods]]/tools and their [[Effective method|effectiveness]] for [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]]: | ||
*From 1992 to 1994, free [[American Academy of Dermatology|American Academy of Dermatology's]] National [[Skin]] [[Cancer (disease)|Cancer]] Early [[Detection theory|Detection]] and [[Screening (medicine)|Screening]] Program was launched which provided broad [[skin]] [[Cancer (disease)|cancer]] [[Education|educational]] [[Information science|information]] to general [[Public health|public]] and enabled almost 750,000 free [[Expert Patient Programme|expert]] [[skin]] [[Cancer (disease)|cancer]] [[Examination|examinations]] which mostly found out thin, [[Localized disease|localized]] stage 1 [[melanomas]] with high [[Project Halo|projected]] [[Five year survival rate|5-year survival rate]]<ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA" /><ref name="pmid8647990" /> | * From 1992 to 1994, free [[American Academy of Dermatology|American Academy of Dermatology's]] National [[Skin]] [[Cancer (disease)|Cancer]] Early [[Detection theory|Detection]] and [[Screening (medicine)|Screening]] Program was launched which provided broad [[skin]] [[Cancer (disease)|cancer]] [[Education|educational]] [[Information science|information]] to general [[Public health|public]] and enabled almost 750,000 free [[Expert Patient Programme|expert]] [[skin]] [[Cancer (disease)|cancer]] [[Examination|examinations]] which mostly found out thin, [[Localized disease|localized]] stage 1 [[melanomas]] with high [[Project Halo|projected]] [[Five year survival rate|5-year survival rate]]<ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA" /><ref name="pmid8647990" /> | ||
*From 2001 to 2005, [[American Academy of Dermatology]] National [[Melanoma]]/[[Skin]] [[Cancer (disease)|Cancer]] [[Screening (medicine)|Screening]] Program was launched which led to the conclusion that HARMM [[criteria]] can be [[Usage analysis|used]] to identify the higher-[[RiskMetrics|risk]] [[Subgroup analysis|subgroup]] of [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]] [[Population (statistics)|population]] via [[Assessment and Plan|assessment]] of multiple [[risk factors]] for [[MM]] , which will not only [[Reduced|reduce]] the [[Cost-effectiveness|cost]] but will also increase the [[Yield (chemistry)|yields]] for suspected [[MM]] in [[Future interests (actuarial science)|future]] [[mass]] [[Screening (medicine)|screening]] [[Initiation (chemistry)|initiatives]]<ref name="pmid17490783" /> | * From 2001 to 2005, [[American Academy of Dermatology]] National [[Melanoma]]/[[Skin]] [[Cancer (disease)|Cancer]] [[Screening (medicine)|Screening]] Program was launched which led to the conclusion that HARMM [[criteria]] can be [[Usage analysis|used]] to identify the higher-[[RiskMetrics|risk]] [[Subgroup analysis|subgroup]] of [[skin]] [[Cancer (disease)|cancer]] [[Screening (medicine)|screening]] [[Population (statistics)|population]] via [[Assessment and Plan|assessment]] of multiple [[risk factors]] for [[MM]] , which will not only [[Reduced|reduce]] the [[Cost-effectiveness|cost]] but will also increase the [[Yield (chemistry)|yields]] for suspected [[MM]] in [[Future interests (actuarial science)|future]] [[mass]] [[Screening (medicine)|screening]] [[Initiation (chemistry)|initiatives]]<ref name="pmid17490783" /> | ||
*[[Melanoma]] [[Genetics]] Program identifies the [[genetic]] [[causes]] of [[skin]] [[Cancer (disease)|cancer]], and also provides [[genetic counseling]] to the [[Individual growth|individuals]] having a [[strong]] [[family history]] of [[melanoma]]<ref name="pmid19739523">{{cite journal| author=Gauwerky K, Ruzicka T, Berking C| title=[Skin cancer screening at the family doctor's office]. | journal=MMW Fortschr Med | year= 2009 | volume= 151 | issue= 25 | pages= 38-42; quiz 43 | pmid=19739523 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19739523 }} </ref><ref name="pmid24908774">{{cite journal| author=Treiber N, Huber MA, Scharffetter-Kochanek K, Schneider LA| title=[Early detection of skin cancer]. | journal=MMW Fortschr Med | year= 2014 | volume= 156 | issue= 4 | pages= 37-40 | pmid=24908774 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24908774 }} </ref><ref name="pmid15884241">{{cite journal| author=Mierzwa T, Zegarski W, Placek W, Zegarska B| title=[Skin cancer screening program in the population of Bydgoszcz]. | journal=Wiad Lek | year= 2004 | volume= 57 Suppl 1 | issue= | pages= 211-4 | pmid=15884241 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15884241 }} </ref><ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA" /><ref name="pmid31106016">{{cite journal| author=Bajaj S, Wolner ZJ, Dusza SW, Braun RP, Marghoob AA, DeFazio J| title=Total Body Skin Examination Practices: A Survey Study Amongst Dermatologists at High-Risk Skin Cancer Clinics. | journal=Dermatol Pract Concept | year= 2019 | volume= 9 | issue= 2 | pages= 132-138 | pmid=31106016 | doi=10.5826/dpc.0902a09 | pmc=6502292 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31106016 }} </ref><ref name="pmid21757257">{{cite journal| author=Argenziano G, Zalaudek I, Hofmann-Wellenhof R, Bakos RM, Bergman W, Blum A et al.| title=Total body skin examination for skin cancer screening in patients with focused symptoms. | journal=J Am Acad Dermatol | year= 2012 | volume= 66 | issue= 2 | pages= 212-9 | pmid=21757257 | doi=10.1016/j.jaad.2010.12.039 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21757257 }} </ref><ref name="urlSkin Cancer Screening: MedlinePlus Lab Test Information">{{cite web |url=https://medlineplus.gov/lab-tests/skin-cancer-screening/ |title=Skin Cancer Screening: MedlinePlus Lab Test Information |format= |work= |accessdate=}}</ref> | * [[Melanoma]] [[Genetics]] Program identifies the [[genetic]] [[causes]] of [[skin]] [[Cancer (disease)|cancer]], and also provides [[genetic counseling]] to the [[Individual growth|individuals]] having a [[strong]] [[family history]] of [[melanoma]]<ref name="pmid19739523">{{cite journal| author=Gauwerky K, Ruzicka T, Berking C| title=[Skin cancer screening at the family doctor's office]. | journal=MMW Fortschr Med | year= 2009 | volume= 151 | issue= 25 | pages= 38-42; quiz 43 | pmid=19739523 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19739523 }} </ref><ref name="pmid24908774">{{cite journal| author=Treiber N, Huber MA, Scharffetter-Kochanek K, Schneider LA| title=[Early detection of skin cancer]. | journal=MMW Fortschr Med | year= 2014 | volume= 156 | issue= 4 | pages= 37-40 | pmid=24908774 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24908774 }} </ref><ref name="pmid15884241">{{cite journal| author=Mierzwa T, Zegarski W, Placek W, Zegarska B| title=[Skin cancer screening program in the population of Bydgoszcz]. | journal=Wiad Lek | year= 2004 | volume= 57 Suppl 1 | issue= | pages= 211-4 | pmid=15884241 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15884241 }} </ref><ref name="urlSkin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA" /><ref name="pmid31106016">{{cite journal| author=Bajaj S, Wolner ZJ, Dusza SW, Braun RP, Marghoob AA, DeFazio J| title=Total Body Skin Examination Practices: A Survey Study Amongst Dermatologists at High-Risk Skin Cancer Clinics. | journal=Dermatol Pract Concept | year= 2019 | volume= 9 | issue= 2 | pages= 132-138 | pmid=31106016 | doi=10.5826/dpc.0902a09 | pmc=6502292 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31106016 }} </ref><ref name="pmid21757257">{{cite journal| author=Argenziano G, Zalaudek I, Hofmann-Wellenhof R, Bakos RM, Bergman W, Blum A et al.| title=Total body skin examination for skin cancer screening in patients with focused symptoms. | journal=J Am Acad Dermatol | year= 2012 | volume= 66 | issue= 2 | pages= 212-9 | pmid=21757257 | doi=10.1016/j.jaad.2010.12.039 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21757257 }} </ref><ref name="urlSkin Cancer Screening: MedlinePlus Lab Test Information">{{cite web |url=https://medlineplus.gov/lab-tests/skin-cancer-screening/ |title=Skin Cancer Screening: MedlinePlus Lab Test Information |format= |work= |accessdate=}}</ref> | ||
*[[Dermoscopy]] [[Usage analysis|usage]] [[Improving agent|improves]] the [[Ability grouping|ability]] of [[Primary care physician|primary care physicians]] to [[triage]] [[lesions]] which are [[Suggestion|suggestive]] of [[skin]] [[Cancer (disease)|cancer]] and saves from [[Unnecessary Fuss|unnecessary]] [[Expert Patient Programme|expert]] [[Consultation|consultations]]<ref name="pmid16622262">{{cite journal| author=Argenziano G, Puig S, Zalaudek I, Sera F, Corona R, Alsina M et al.| title=Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. | journal=J Clin Oncol | year= 2006 | volume= 24 | issue= 12 | pages= 1877-82 | pmid=16622262 | doi=10.1200/JCO.2005.05.0864 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16622262 }} </ref> | * [[Dermoscopy]] [[Usage analysis|usage]] [[Improving agent|improves]] the [[Ability grouping|ability]] of [[Primary care physician|primary care physicians]] to [[triage]] [[lesions]] which are [[Suggestion|suggestive]] of [[skin]] [[Cancer (disease)|cancer]] and saves from [[Unnecessary Fuss|unnecessary]] [[Expert Patient Programme|expert]] [[Consultation|consultations]]<ref name="pmid16622262">{{cite journal| author=Argenziano G, Puig S, Zalaudek I, Sera F, Corona R, Alsina M et al.| title=Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. | journal=J Clin Oncol | year= 2006 | volume= 24 | issue= 12 | pages= 1877-82 | pmid=16622262 | doi=10.1200/JCO.2005.05.0864 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16622262 }} </ref> | ||
*[[Combination therapy|Combination]] of [[dermoscopy]] and short-term [[Sequential analysis|sequential]] [[Digital dictation|digital]] [[dermoscopy]] [[imaging]] (SDDI) in a [[Primary care provider|primary care setting]] doubles the [[Sensitivity (tests)|sensitivity]] for [[melanoma]] [[diagnosis]] and also [[Lead|leads]] to >50% [[chance]] of [[reduction]] in [[excision]] or [[Reference|referral]] of [[benign]] [[pigmented lesions]]<ref name="pmid19747359">{{cite journal| author=Menzies SW, Emery J, Staples M, Davies S, McAvoy B, Fletcher J et al.| title=Impact of dermoscopy and short-term sequential digital dermoscopy imaging for the management of pigmented lesions in primary care: a sequential intervention trial. | journal=Br J Dermatol | year= 2009 | volume= 161 | issue= 6 | pages= 1270-7 | pmid=19747359 | doi=10.1111/j.1365-2133.2009.09374.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19747359 }} </ref><ref name="pmid19832836">{{cite journal| author=van der Rhee JI, Bergman W, Kukutsch NA| title=The impact of dermoscopy on the management of pigmented lesions in everyday clinical practice of general dermatologists: a prospective study. | journal=Br J Dermatol | year= 2010 | volume= 162 | issue= 3 | pages= 563-7 | pmid=19832836 | doi=10.1111/j.1365-2133.2009.09551.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19832836 }} </ref><ref name="pmid30521682">{{cite journal| author=Dinnes J, Deeks JJ, Chuchu N, Ferrante di Ruffano L, Matin RN, Thomson DR et al.| title=Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD011902 | pmid=30521682 | doi=10.1002/14651858.CD011902.pub2 | pmc=6517096 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521682 }} </ref><ref name="pmid30521691">{{cite journal| author=Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C et al.| title=Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013186 | pmid=30521691 | doi=10.1002/14651858.CD013186 | pmc=6517147 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521691 }} </ref><ref name="pmid30521690">{{cite journal| author=Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C et al.| title=Optical coherence tomography for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013189 | pmid=30521690 | doi=10.1002/14651858.CD013189 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521690 }} </ref> | * [[Combination therapy|Combination]] of [[dermoscopy]] and short-term [[Sequential analysis|sequential]] [[Digital dictation|digital]] [[dermoscopy]] [[imaging]] (SDDI) in a [[Primary care provider|primary care setting]] doubles the [[Sensitivity (tests)|sensitivity]] for [[melanoma]] [[diagnosis]] and also [[Lead|leads]] to >50% [[chance]] of [[reduction]] in [[excision]] or [[Reference|referral]] of [[benign]] [[pigmented lesions]]<ref name="pmid19747359">{{cite journal| author=Menzies SW, Emery J, Staples M, Davies S, McAvoy B, Fletcher J et al.| title=Impact of dermoscopy and short-term sequential digital dermoscopy imaging for the management of pigmented lesions in primary care: a sequential intervention trial. | journal=Br J Dermatol | year= 2009 | volume= 161 | issue= 6 | pages= 1270-7 | pmid=19747359 | doi=10.1111/j.1365-2133.2009.09374.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19747359 }} </ref><ref name="pmid19832836">{{cite journal| author=van der Rhee JI, Bergman W, Kukutsch NA| title=The impact of dermoscopy on the management of pigmented lesions in everyday clinical practice of general dermatologists: a prospective study. | journal=Br J Dermatol | year= 2010 | volume= 162 | issue= 3 | pages= 563-7 | pmid=19832836 | doi=10.1111/j.1365-2133.2009.09551.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19832836 }} </ref><ref name="pmid30521682">{{cite journal| author=Dinnes J, Deeks JJ, Chuchu N, Ferrante di Ruffano L, Matin RN, Thomson DR et al.| title=Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD011902 | pmid=30521682 | doi=10.1002/14651858.CD011902.pub2 | pmc=6517096 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521682 }} </ref><ref name="pmid30521691">{{cite journal| author=Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C et al.| title=Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013186 | pmid=30521691 | doi=10.1002/14651858.CD013186 | pmc=6517147 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521691 }} </ref><ref name="pmid30521690">{{cite journal| author=Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C et al.| title=Optical coherence tomography for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013189 | pmid=30521690 | doi=10.1002/14651858.CD013189 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521690 }} </ref> | ||
==Diagnosis== | ==Diagnosis== | ||
| Line 429: | Line 457: | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
====Common sites of involvement==== | ====Common sites of involvement==== | ||
*Primarily involves the [[Sun exposure|sun-exposed]] [[Area|areas]] of [[skin]] such as: | * Primarily involves the [[Sun exposure|sun-exposed]] [[Area|areas]] of [[skin]] such as: | ||
**[[Scalp]] | ** [[Scalp]] | ||
**[[Face]] | ** [[Face]] | ||
**[[Lips]] | ** [[Lips]] | ||
**[[Ears]] | ** [[Ears]] | ||
**[[Neck]] | ** [[Neck]] | ||
**[[Chest]] | ** [[Chest]] | ||
**[[Arm|Arms]] | ** [[Arm|Arms]] | ||
**[[Hands]] | ** [[Hands]] | ||
**[[Legs]] (especially in [[Womens Pack|women]]) | ** [[Legs]] (especially in [[Womens Pack|women]]) | ||
**[[Eyelids]] ([[sebaceous gland carcinoma]]) | ** [[Eyelids]] ([[sebaceous gland carcinoma]]) | ||
*Can also involve the [[skin]] [[Area|areas]] very [[Rare|rarely]] [[Sun exposure|exposed to sun]] such as: | * Can also involve the [[skin]] [[Area|areas]] very [[Rare|rarely]] [[Sun exposure|exposed to sun]] such as: | ||
**Underneath [[fingernails]] or [[toenails]] | ** Underneath [[fingernails]] or [[toenails]] | ||
**[[Palms of the hands|Palm of the hand]] | ** [[Palms of the hands|Palm of the hand]] | ||
**[[Sole of the foot]] | ** [[Sole of the foot]] | ||
**[[Genital area|Genital region]] | ** [[Genital area|Genital region]] | ||
====Common symptoms==== | ====Common symptoms==== | ||
*There are a variety of different [[skin]] [[Cancer (medicine)|cancer]] [[symptoms]] including [[crabs]] or [[Change detection|changes]] in the [[skin]] that do not [[Healing|heal]], [[ulcers]] in the [[skin]], discoloration, and [[Change detection|changes]] in existing [[moles]] | * There are a variety of different [[skin]] [[Cancer (medicine)|cancer]] [[symptoms]] including [[crabs]] or [[Change detection|changes]] in the [[skin]] that do not [[Healing|heal]], [[ulcers]] in the [[skin]], discoloration, and [[Change detection|changes]] in existing [[moles]] | ||
* [[Malignant melanoma|'''Malignant melanoma''']] [[Appearance|appears]] as a small [[lesion]] having [[Irregular lesion|irregular]] borders & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or [[blue]]-[[black]] | * [[Malignant melanoma|'''Malignant melanoma''']] [[Appearance|appears]] as a small [[lesion]] having [[Irregular lesion|irregular]] borders & [[Portion control (dieting)|portions]] with multiple [[Color|colors]] such as [[White (mutation)|white]], [[Pinks|pink]], [[Red-Al|red]], [[blue]] or [[blue]]-[[black]] | ||
* [[Basal cell carcinoma|'''Basal cell carcinoma''']] [[Appearance|appears]] as a [[Waxy flexibility|waxy]] or a [[Pearly gates|pearly]] [[Bumps on skin|bump]], or a [[brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flat affect|flat]] [[lesion]], or a [[Scab|scabbing]] or a [[bleeding]] [[sore]] that [[Healing|heals]] and returns | * [[Basal cell carcinoma|'''Basal cell carcinoma''']] [[Appearance|appears]] as a [[Waxy flexibility|waxy]] or a [[Pearly gates|pearly]] [[Bumps on skin|bump]], or a [[brown]] [[scar]]-like or [[flesh]]-[[Color|colored]] [[Flat affect|flat]] [[lesion]], or a [[Scab|scabbing]] or a [[bleeding]] [[sore]] that [[Healing|heals]] and returns | ||
*[[Squamous cell carcinoma of the skin|'''Squamous cell carcinoma''']] [[Appearance|appears]] as a [[Red-Al|red]], [[Firming agent|firm]] [[Nodule (medicine)|nodule]] or a [[Flat affect|flat]] [[lesion]] having a [[Crustacean|crusted]], [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | * [[Squamous cell carcinoma of the skin|'''Squamous cell carcinoma''']] [[Appearance|appears]] as a [[Red-Al|red]], [[Firming agent|firm]] [[Nodule (medicine)|nodule]] or a [[Flat affect|flat]] [[lesion]] having a [[Crustacean|crusted]], [[Scale (zoology)|scaly]] [[Surface anatomy|surface]] | ||
* [[Actinic keratosis|'''Actinic keratosis''']] [[Appearance|appears]] as either a [[Rough (facility)|rough]], [[Pinks|pink]], [[Red-Al|red]] or [[brown]], [[Scale (social sciences)|scaly]], [[Flat affect|flat]] or raised [[Patched|patch]] on the [[skin]] or as peeling or [[Cracking (chemistry)|cracking]] of [[lower lip]] not [[Cure|cured]] by [[lip balm]] or [[petroleum jelly]] and most commonly involves [[face]] and [[Top7|top]] of the [[hands]] | * [[Actinic keratosis|'''Actinic keratosis''']] [[Appearance|appears]] as either a [[Rough (facility)|rough]], [[Pinks|pink]], [[Red-Al|red]] or [[brown]], [[Scale (social sciences)|scaly]], [[Flat affect|flat]] or raised [[Patched|patch]] on the [[skin]] or as peeling or [[Cracking (chemistry)|cracking]] of [[lower lip]] not [[Cure|cured]] by [[lip balm]] or [[petroleum jelly]] and most commonly involves [[face]] and [[Top7|top]] of the [[hands]] | ||
* [[Bowen's disease|'''Bowen's disease''']] [[Appearance|appears]] as a [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | * [[Bowen's disease|'''Bowen's disease''']] [[Appearance|appears]] as a [[Red-Al|red]] or [[brown]] [[Scale (social sciences)|scaly]] [[Patched|patch]]/[[plaque]] on the [[Sun exposure|sun]]-damaged [[skin]] | ||
*'''[[Keratoacanthoma]]''' [[Eruption|erupts]] with an initial rapid [[growth]] (like a little [[volcano]]) on [[Sun exposure|sun]]-damaged [[skin]] and resolves on its own later on after [[Fewmets|few]] months | *'''[[Keratoacanthoma]]''' [[Eruption|erupts]] with an initial rapid [[growth]] (like a little [[volcano]]) on [[Sun exposure|sun]]-damaged [[skin]] and resolves on its own later on after [[Fewmets|few]] months | ||
* [[Dermatofibrosarcoma protuberans|'''Dermatofibrosarcoma protuberans''']] begins as a minor [[Firming agent|firm]] [[area]] of [[skin]] resembling a [[bruise]], [[birthmark]], or [[pimple]] | * [[Dermatofibrosarcoma protuberans|'''Dermatofibrosarcoma protuberans''']] begins as a minor [[Firming agent|firm]] [[area]] of [[skin]] resembling a [[bruise]], [[birthmark]], or [[pimple]] | ||
*[[Merkel cell carcinoma|'''Merkel cell carcinoma''']] [[Appearance|appears]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] and mostly involves [[Head (anatomy)|head]], [[neck]] and [[trunk]] | * [[Merkel cell carcinoma|'''Merkel cell carcinoma''']] [[Appearance|appears]] as shiny, [[Firming agent|firm]] [[nodules]] just beneath or on the [[skin]] & in [[hair follicles]] and mostly involves [[Head (anatomy)|head]], [[neck]] and [[trunk]] | ||
* [[Kaposi's sarcoma|'''Kaposi's sarcoma''']] [[Appearance|appears]] as [[Purple haze|purple]] or [[Red-Al|red]] [[Patching|patches]] on [[skin]] or [[mucous membrane]] | * [[Kaposi's sarcoma|'''Kaposi's sarcoma''']] [[Appearance|appears]] as [[Purple haze|purple]] or [[Red-Al|red]] [[Patching|patches]] on [[skin]] or [[mucous membrane]] | ||
* [[Angiosarcoma|'''Angiosarcoma's''']] most common manifestation is a gradually enlarging, painless [[mass]], with other symptoms including [[skin]] [[Thickener|thickening]], [[erythema]], or [[skin discoloration]] (primary [[cutaneous]]),[[lymphedema]] ([[secondary]] [[angiosarcoma]]), [[pain]], [[edema]] or other [[symptoms]] due to [[Compression garment|compression]]<nowiki/>of adjacent [[Neurovascular bundle|neurovascular]] [[Structure factor|structures]] | * [[Angiosarcoma|'''Angiosarcoma's''']] most common manifestation is a gradually enlarging, painless [[mass]], with other symptoms including [[skin]] [[Thickener|thickening]], [[erythema]], or [[skin discoloration]] (primary [[cutaneous]]),[[lymphedema]] ([[secondary]] [[angiosarcoma]]), [[pain]], [[edema]] or other [[symptoms]] due to [[Compression garment|compression]]<nowiki/>of adjacent [[Neurovascular bundle|neurovascular]] [[Structure factor|structures]] | ||
| Line 465: | Line 493: | ||
* On [[physical examination]], [[basal cell carcinoma]] usually [[Lookahead|looks]] like a raised, smooth, [[Pearly gates|pearly]] [[Bumps on skin|bump]] on the [[Sun exposure|sun-exposed]] [[skin]] of the [[head]], [[neck]] or [[shoulders]]<ref name="pmid13677122">{{cite journal| author=Godsell G| title=Recognising the signs of skin cancer. | journal=Nurs Times | year= 2003 | volume= 99 | issue= 31 | pages= 44-5 | pmid=13677122 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13677122 }} </ref> | * On [[physical examination]], [[basal cell carcinoma]] usually [[Lookahead|looks]] like a raised, smooth, [[Pearly gates|pearly]] [[Bumps on skin|bump]] on the [[Sun exposure|sun-exposed]] [[skin]] of the [[head]], [[neck]] or [[shoulders]]<ref name="pmid13677122">{{cite journal| author=Godsell G| title=Recognising the signs of skin cancer. | journal=Nurs Times | year= 2003 | volume= 99 | issue= 31 | pages= 44-5 | pmid=13677122 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=13677122 }} </ref> | ||
* Small [[blood vessels]], [[Crustacean|crusting]] and [[bleeding]] in the center of [[tumor]] can be seen sometimes, hence, often mistaken as a non-[[healing]] [[sore]] | * Small [[blood vessels]], [[Crustacean|crusting]] and [[bleeding]] in the center of [[tumor]] can be seen sometimes, hence, often mistaken as a non-[[healing]] [[sore]] | ||
*[[Squamous cell carcinoma of the skin|Squamous cell carcinoma]] commonly [[Appearance|appears]] as a [[Red-Al|red]], [[Scaling skin|scaling]], [[Thickener|thickened]] [[Patching|patch]] on [[Sun exposure|sun-exposed]] [[skin]] with/without [[ulceration]] or [[bleeding]], and can [[Development (biology)|develop]] into a [[Large-print|large]] [[mass]] if left untreated | * [[Squamous cell carcinoma of the skin|Squamous cell carcinoma]] commonly [[Appearance|appears]] as a [[Red-Al|red]], [[Scaling skin|scaling]], [[Thickener|thickened]] [[Patching|patch]] on [[Sun exposure|sun-exposed]] [[skin]] with/without [[ulceration]] or [[bleeding]], and can [[Development (biology)|develop]] into a [[Large-print|large]] [[mass]] if left untreated | ||
* Most [[melanomas]] [[Appearance|appear]] as [[brown]] to [[black]] [[Lookahead|looking]] [[lesions]] | * Most [[melanomas]] [[Appearance|appear]] as [[brown]] to [[black]] [[Lookahead|looking]] [[lesions]] | ||
*[[Signs]] [[Indication (medicine)|indicating]] a [[malignant melanoma]] include [[Change detection|change]] in [[Size consistency|size]], [[Shape parameter|shape]], [[color]] or [[elevation]] of a [[mole]] | * [[Signs]] [[Indication (medicine)|indicating]] a [[malignant melanoma]] include [[Change detection|change]] in [[Size consistency|size]], [[Shape parameter|shape]], [[color]] or [[elevation]] of a [[mole]] | ||
*[[Appearance]] of a [[new]] [[mole]] during [[Adult|adulthood]], or [[new]] [[pain]], [[itching]], [[ulceration]] or [[bleeding]] of an [[Existential therapy|existing]] [[mole]] should always be [[Check|checked]] as it is suspicious for [[melanoma]] | * [[Appearance]] of a [[new]] [[mole]] during [[Adult|adulthood]], or [[new]] [[pain]], [[itching]], [[ulceration]] or [[bleeding]] of an [[Existential therapy|existing]] [[mole]] should always be [[Check|checked]] as it is suspicious for [[melanoma]] | ||
===Laboratory Tests=== | ===Laboratory Tests=== | ||
*[[Dermoscopy]] [[Usage analysis|usage]] [[Improving agent|improves]] the [[Ability grouping|ability]] of [[Primary care physician|primary care physicians]] to [[triage]] [[lesions]] which are [[Suggestion|suggestive]] of [[skin]] [[Cancer (disease)|cancer]] and saves from [[Unnecessary Fuss|unnecessary]] [[Expert Patient Programme|expert]] [[Consultation|consultations]]<ref name="pmid16622262">{{cite journal| author=Argenziano G, Puig S, Zalaudek I, Sera F, Corona R, Alsina M et al.| title=Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. | journal=J Clin Oncol | year= 2006 | volume= 24 | issue= 12 | pages= 1877-82 | pmid=16622262 | doi=10.1200/JCO.2005.05.0864 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16622262 }} </ref> | * [[Dermoscopy]] [[Usage analysis|usage]] [[Improving agent|improves]] the [[Ability grouping|ability]] of [[Primary care physician|primary care physicians]] to [[triage]] [[lesions]] which are [[Suggestion|suggestive]] of [[skin]] [[Cancer (disease)|cancer]] and saves from [[Unnecessary Fuss|unnecessary]] [[Expert Patient Programme|expert]] [[Consultation|consultations]]<ref name="pmid16622262">{{cite journal| author=Argenziano G, Puig S, Zalaudek I, Sera F, Corona R, Alsina M et al.| title=Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. | journal=J Clin Oncol | year= 2006 | volume= 24 | issue= 12 | pages= 1877-82 | pmid=16622262 | doi=10.1200/JCO.2005.05.0864 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16622262 }} </ref> | ||
*[[Combination therapy|Combination]] of [[dermoscopy]] and short-term [[Sequential analysis|sequential]] [[Digital dictation|digital]] [[dermoscopy]] [[imaging]] (SDDI) in a [[Primary care provider|primary care setting]] doubles the [[Sensitivity (tests)|sensitivity]] for [[melanoma]] [[diagnosis]] and also [[Lead|leads]] to >50% [[chance]] of [[reduction]] in [[excision]] or [[Reference|referral]] of [[benign]] [[pigmented lesions]]<ref name="pmid19747359">{{cite journal| author=Menzies SW, Emery J, Staples M, Davies S, McAvoy B, Fletcher J et al.| title=Impact of dermoscopy and short-term sequential digital dermoscopy imaging for the management of pigmented lesions in primary care: a sequential intervention trial. | journal=Br J Dermatol | year= 2009 | volume= 161 | issue= 6 | pages= 1270-7 | pmid=19747359 | doi=10.1111/j.1365-2133.2009.09374.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19747359 }} </ref><ref name="pmid19832836">{{cite journal| author=van der Rhee JI, Bergman W, Kukutsch NA| title=The impact of dermoscopy on the management of pigmented lesions in everyday clinical practice of general dermatologists: a prospective study. | journal=Br J Dermatol | year= 2010 | volume= 162 | issue= 3 | pages= 563-7 | pmid=19832836 | doi=10.1111/j.1365-2133.2009.09551.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19832836 }} </ref><ref name="pmid30521682">{{cite journal| author=Dinnes J, Deeks JJ, Chuchu N, Ferrante di Ruffano L, Matin RN, Thomson DR et al.| title=Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD011902 | pmid=30521682 | doi=10.1002/14651858.CD011902.pub2 | pmc=6517096 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521682 }} </ref><ref name="pmid30521691">{{cite journal| author=Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C et al.| title=Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013186 | pmid=30521691 | doi=10.1002/14651858.CD013186 | pmc=6517147 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521691 }} </ref><ref name="pmid30521690">{{cite journal| author=Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C et al.| title=Optical coherence tomography for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013189 | pmid=30521690 | doi=10.1002/14651858.CD013189 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521690 }} </ref> | * [[Combination therapy|Combination]] of [[dermoscopy]] and short-term [[Sequential analysis|sequential]] [[Digital dictation|digital]] [[dermoscopy]] [[imaging]] (SDDI) in a [[Primary care provider|primary care setting]] doubles the [[Sensitivity (tests)|sensitivity]] for [[melanoma]] [[diagnosis]] and also [[Lead|leads]] to >50% [[chance]] of [[reduction]] in [[excision]] or [[Reference|referral]] of [[benign]] [[pigmented lesions]]<ref name="pmid19747359">{{cite journal| author=Menzies SW, Emery J, Staples M, Davies S, McAvoy B, Fletcher J et al.| title=Impact of dermoscopy and short-term sequential digital dermoscopy imaging for the management of pigmented lesions in primary care: a sequential intervention trial. | journal=Br J Dermatol | year= 2009 | volume= 161 | issue= 6 | pages= 1270-7 | pmid=19747359 | doi=10.1111/j.1365-2133.2009.09374.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19747359 }} </ref><ref name="pmid19832836">{{cite journal| author=van der Rhee JI, Bergman W, Kukutsch NA| title=The impact of dermoscopy on the management of pigmented lesions in everyday clinical practice of general dermatologists: a prospective study. | journal=Br J Dermatol | year= 2010 | volume= 162 | issue= 3 | pages= 563-7 | pmid=19832836 | doi=10.1111/j.1365-2133.2009.09551.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19832836 }} </ref><ref name="pmid30521682">{{cite journal| author=Dinnes J, Deeks JJ, Chuchu N, Ferrante di Ruffano L, Matin RN, Thomson DR et al.| title=Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD011902 | pmid=30521682 | doi=10.1002/14651858.CD011902.pub2 | pmc=6517096 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521682 }} </ref><ref name="pmid30521691">{{cite journal| author=Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C et al.| title=Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013186 | pmid=30521691 | doi=10.1002/14651858.CD013186 | pmc=6517147 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521691 }} </ref><ref name="pmid30521690">{{cite journal| author=Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C et al.| title=Optical coherence tomography for diagnosing skin cancer in adults. | journal=Cochrane Database Syst Rev | year= 2018 | volume= 12 | issue= | pages= CD013189 | pmid=30521690 | doi=10.1002/14651858.CD013189 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30521690 }} </ref> | ||
===Biopsy=== | ===Biopsy=== | ||
*[[Skin biopsy]] (i.e. removal of a [[Sample (statistics)|sample]] of suspicious [[skin]] for [[testing]]) is an essential component of [[skin]] [[Cancer (medicine)|cancer]] [[diagnosis]] and by [[histopathological]] [[Laboratory|lab]] [[analysis]], can determine whether it is a [[skin]] [[Cancer (medicine)|cancer]] or not, and if so, what type of [[skin]] [[Cancer (medicine)|cancer]] it is | * [[Skin biopsy]] (i.e. removal of a [[Sample (statistics)|sample]] of suspicious [[skin]] for [[testing]]) is an essential component of [[skin]] [[Cancer (medicine)|cancer]] [[diagnosis]] and by [[histopathological]] [[Laboratory|lab]] [[analysis]], can determine whether it is a [[skin]] [[Cancer (medicine)|cancer]] or not, and if so, what type of [[skin]] [[Cancer (medicine)|cancer]] it is | ||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
* In case of a [[metastatic]] stage IV [[skin]] [[Cancer (disease)|cancer]] such as a large [[SCC]], [[melanoma]], & [[merkel cell carcinoma]], [[lymph nodes]] become involved, which requires further [[testing]] such as: | * In case of a [[metastatic]] stage IV [[skin]] [[Cancer (disease)|cancer]] such as a large [[SCC]], [[melanoma]], & [[merkel cell carcinoma]], [[lymph nodes]] become involved, which requires further [[testing]] such as: | ||
**[[Sentinel lymph node]] [[biopsy]] | ** [[Sentinel lymph node]] [[biopsy]] | ||
** [[Imaging studies|Imaging tests]] for [[lymph node]] involvement such as [[Chest X-ray]], [[Computed tomography|CT]], [[Magnetic resonance imaging|MRI]], [[PET scan]] or [[ultrasound]] [[Dependent variable|depending]] on the site involved | ** [[Imaging studies|Imaging tests]] for [[lymph node]] involvement such as [[Chest X-ray]], [[Computed tomography|CT]], [[Magnetic resonance imaging|MRI]], [[PET scan]] or [[ultrasound]] [[Dependent variable|depending]] on the site involved | ||
*[[Eye examination]] with [[dilated pupil]] to look for [[retina]] and [[optic nerve]] involvement in [[Case fatality|case]] of [[metastasis]] | * [[Eye examination]] with [[dilated pupil]] to look for [[retina]] and [[optic nerve]] involvement in [[Case fatality|case]] of [[metastasis]] | ||
==Treatment== | ==Treatment== | ||
*[[Treatments|Treatment]] of [[skin]] [[Cancer (disease)|cancer]] [[Variable|varies]] [[Dependent variable|depending]] upon the [[Size consistency|size]], type, [[Depth of field|depth]], [[Location parameter|location]], stage of the [[tumor]], involved [[Human body|body]] part, and [[Patient|patient’s]] [[Generalization|general]] [[health]] | * [[Treatments|Treatment]] of [[skin]] [[Cancer (disease)|cancer]] [[Variable|varies]] [[Dependent variable|depending]] upon the [[Size consistency|size]], type, [[Depth of field|depth]], [[Location parameter|location]], stage of the [[tumor]], involved [[Human body|body]] part, and [[Patient|patient’s]] [[Generalization|general]] [[health]] | ||
*Small [[lesions]] [[Limiting factor|limited]] only to the [[skin]] [[Surface anatomy|surface]] can easily be [[Cure|cured]] by [[Simple cell|simple]] initial [[skin biopsy]] and may not require any further [[Treatments|treatment]] whereas [[Large-print|large]] [[lesions]] with [[metastasis]] require further [[Treatments|treatment]] options as shown in the table below:<ref name="urlSkin cancer - Diagnosis and treatment - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/skin-cancer/diagnosis-treatment/drc-20377608 |title=Skin cancer - Diagnosis and treatment - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="urlSkin Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/skin/patient/skin-treatment-pdq |title=Skin Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute |format= |work= |accessdate=}}</ref> | * Small [[lesions]] [[Limiting factor|limited]] only to the [[skin]] [[Surface anatomy|surface]] can easily be [[Cure|cured]] by [[Simple cell|simple]] initial [[skin biopsy]] and may not require any further [[Treatments|treatment]] whereas [[Large-print|large]] [[lesions]] with [[metastasis]] require further [[Treatments|treatment]] options as shown in the table below:<ref name="urlSkin cancer - Diagnosis and treatment - Mayo Clinic">{{cite web |url=https://www.mayoclinic.org/diseases-conditions/skin-cancer/diagnosis-treatment/drc-20377608 |title=Skin cancer - Diagnosis and treatment - Mayo Clinic |format= |work= |accessdate=}}</ref><ref name="urlSkin Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute">{{cite web |url=https://www.cancer.gov/types/skin/patient/skin-treatment-pdq |title=Skin Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute |format= |work= |accessdate=}}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 495: | Line 523: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Cryosurgery]]/[[Freezing]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Cryosurgery]]/[[Freezing]]''' | ||
| | | | ||
*[[Cancer cells]] are destroyed by [[freezing]] them with [[liquid nitrogen]] | * [[Cancer cells]] are destroyed by [[freezing]] them with [[liquid nitrogen]] | ||
* Later on, the [[Dead space|dead]] [[Tissue (biology)|tissue]] sloughs off on thawing | * Later on, the [[Dead space|dead]] [[Tissue (biology)|tissue]] sloughs off on thawing | ||
| rowspan="6" | | | rowspan="6" | | ||
| Line 504: | Line 532: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Electrotherapy]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Electrotherapy]]''' | ||
| | | | ||
*[[Electromagnetic therapy]] [[Usage analysis|uses]] [[electrical stimulation]] to [[Killer cell|kill]] [[cancer cells]] | * [[Electromagnetic therapy]] [[Usage analysis|uses]] [[electrical stimulation]] to [[Killer cell|kill]] [[cancer cells]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Curettage]] & electrodesiccation or [[cryotherapy]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Curettage]] & electrodesiccation or [[cryotherapy]]''' | ||
| Line 514: | Line 542: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Photodynamic therapy]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Photodynamic therapy]]''' | ||
| | | | ||
*[[Usage analysis|Uses]] [[Combination therapy|combination]] of [[laser]] [[light]] and [[drugs]] [[MakeBot|making]] [[cancer cells]] [[Sensitive Skin|sensitive]] to [[light]] to destroy [[skin]] [[cancer cells]] | * [[Usage analysis|Uses]] [[Combination therapy|combination]] of [[laser]] [[light]] and [[drugs]] [[MakeBot|making]] [[cancer cells]] [[Sensitive Skin|sensitive]] to [[light]] to destroy [[skin]] [[cancer cells]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Chemical peel]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Chemical peel]] | ||
| | | | ||
*[[Chemical]] [[solution]] is put on the [[skin]] to dissolve the [[Top7|top]] layers of [[cancerous]] [[Skin cell|skin cells]] | * [[Chemical]] [[solution]] is put on the [[skin]] to dissolve the [[Top7|top]] layers of [[cancerous]] [[Skin cell|skin cells]] | ||
*[[Usage analysis|Used]] to [[Treatments|treat]] [[actinic keratosis]] | * [[Usage analysis|Used]] to [[Treatments|treat]] [[actinic keratosis]] | ||
* Also known as: | * Also known as: | ||
** Chemabrasion | ** Chemabrasion | ||
| Line 526: | Line 554: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other [[drug therapy]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |Other [[drug therapy]] | ||
| | | | ||
*[[Retinoids]] are [[Usage analysis|used]] to [[Treatments|treat]] [[squamous cell carcinoma of skin]] | * [[Retinoids]] are [[Usage analysis|used]] to [[Treatments|treat]] [[squamous cell carcinoma of skin]] | ||
*[[Topical]] [[drugs]] [[Usage analysis|used]] to [[Treatments|treat]] [[actinic keratosis]] include: | * [[Topical]] [[drugs]] [[Usage analysis|used]] to [[Treatments|treat]] [[actinic keratosis]] include: | ||
**[[Diclofenac]] | ** [[Diclofenac]] | ||
**[[Ingenol mebutate|Ingenol]] | ** [[Ingenol mebutate|Ingenol]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Simple [[Excisional biopsy|excisional]] [[surgery]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Simple [[Excisional biopsy|excisional]] [[surgery]]''' | ||
| Line 541: | Line 569: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Mohs micrographic surgery]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Mohs micrographic surgery]]''' | ||
| | | | ||
*[[Usage analysis|Uses]] [[Special function|special]] [[training]] & technique involving the [[skin]] removal, layer by layer with subsequent [[examination]] of each layer under [[microscope]], until no [[abnormal]] [[Cells (biology)|cells]] are remaining | * [[Usage analysis|Uses]] [[Special function|special]] [[training]] & technique involving the [[skin]] removal, layer by layer with subsequent [[examination]] of each layer under [[microscope]], until no [[abnormal]] [[Cells (biology)|cells]] are remaining | ||
*[[Least squares|Least]] [[Amount of substance|amount]] of the surrounding [[healthy]] [[Tissue (biology)|tissue]] is removed | * [[Least squares|Least]] [[Amount of substance|amount]] of the surrounding [[healthy]] [[Tissue (biology)|tissue]] is removed | ||
*[[Edge detection|Edges]] are immediately [[Check|checked]] to [[See Clearly Method|see]] if [[tumor]] is found | * [[Edge detection|Edges]] are immediately [[Check|checked]] to [[See Clearly Method|see]] if [[tumor]] is found | ||
* Provides [[Best practice|best]] [[Cosmetics|cosmetically]] favorable [[Result|results]] especially on the [[skin]] [[Area|areas]] with [[Limiting factor|limited]] [[Excess risk|excess]] [[skin]] such as [[face]] | * Provides [[Best practice|best]] [[Cosmetics|cosmetically]] favorable [[Result|results]] especially on the [[skin]] [[Area|areas]] with [[Limiting factor|limited]] [[Excess risk|excess]] [[skin]] such as [[face]] | ||
*[[Cure]] [[rates]] are [[Equivalent (chemistry)|equivalent]] to [[Wide and fast|wide]] [[excision]] | * [[Cure]] [[rates]] are [[Equivalent (chemistry)|equivalent]] to [[Wide and fast|wide]] [[excision]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Shaved ice|Shave]] [[excision]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Shaved ice|Shave]] [[excision]]''' | ||
| | | | ||
*[[Abnormal]] [[area]] is [[Shaved ice|shaved]] off the [[skin]] [[Surface anatomy|surface]] [[Usage analysis|using]] a small blade | * [[Abnormal]] [[area]] is [[Shaved ice|shaved]] off the [[skin]] [[Surface anatomy|surface]] [[Usage analysis|using]] a small blade | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Laser surgery]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Laser surgery]] | ||
| Line 557: | Line 585: | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Dermabrasion]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Dermabrasion]] | ||
| | | | ||
*[[Top7|Top]] layer of [[skin]] is removed [[Usage analysis|using]] a [[rotating]] [[Wheelbench|wheel]] or small [[Particle amplitude|particles]] to rub away [[Skin cell|skin cells]] | * [[Top7|Top]] layer of [[skin]] is removed [[Usage analysis|using]] a [[rotating]] [[Wheelbench|wheel]] or small [[Particle amplitude|particles]] to rub away [[Skin cell|skin cells]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Chemotherapy]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Chemotherapy]]''' | ||
|<br /> | |<br /> | ||
*[[Topical]] [[Chemotherapy agent|chemotherapy]] including [[Cream (pharmaceutical)|creams]] or [[Lotion|lotions]] containing [[anticancer agents]] can be [[Applicability Domain|applied]] [[Directly observed treatment|directly]] to the [[skin]] in [[Case fatality|case]] of [[cancers]] [[Limiting factor|limited]] to the [[Top7|top]] layer of [[skin]] | * [[Topical]] [[Chemotherapy agent|chemotherapy]] including [[Cream (pharmaceutical)|creams]] or [[Lotion|lotions]] containing [[anticancer agents]] can be [[Applicability Domain|applied]] [[Directly observed treatment|directly]] to the [[skin]] in [[Case fatality|case]] of [[cancers]] [[Limiting factor|limited]] to the [[Top7|top]] layer of [[skin]] | ||
*[[Systemic]] [[chemotherapy]] can be [[Usage analysis|used]] to [[Treatments|treat]] [[skin]] [[cancers]] with [[metastasis]] to other parts of the [[Human body|body]] | * [[Systemic]] [[chemotherapy]] can be [[Usage analysis|used]] to [[Treatments|treat]] [[skin]] [[cancers]] with [[metastasis]] to other parts of the [[Human body|body]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Radiation therapy]]''' | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Radiation therapy]]''' | ||
| | | | ||
* High-[[Power (communication)|powered]] [[Energy (biology)|energy]] [[Beamline|beams]] such as [[X-rays]] are [[Usage analysis|used]] to [[Killer cell|kill]] [[cancer cells]] | * High-[[Power (communication)|powered]] [[Energy (biology)|energy]] [[Beamline|beams]] such as [[X-rays]] are [[Usage analysis|used]] to [[Killer cell|kill]] [[cancer cells]] | ||
*[[Usage analysis|Used]] when [[Cancer (disease)|cancer]] can't be completely removed via [[surgery]] | * [[Usage analysis|Used]] when [[Cancer (disease)|cancer]] can't be completely removed via [[surgery]] | ||
*Two types of [[radiation therapy]] can be [[Usage analysis|used]]: | * Two types of [[radiation therapy]] can be [[Usage analysis|used]]: | ||
**[[External beam radiation therapy|External radiation therapy]] (a [[Machine perception|machine]] outside the [[Human body|body]] is [[Usage analysis|used]] to send [[radiation]] towards the [[Cancer (disease)|cancer]]) | ** [[External beam radiation therapy|External radiation therapy]] (a [[Machine perception|machine]] outside the [[Human body|body]] is [[Usage analysis|used]] to send [[radiation]] towards the [[Cancer (disease)|cancer]]) | ||
**[[Internal]] [[radiation therapy]] ([[radioactive]] [[substance]] is [[Usage analysis|used]] which is [[Sealed source radiotherapy|sealed]] in [[Needle|needles]], [[Seed|seeds]], [[Wire|wires]], or [[catheters]] which are [[Place cell|placed]] [[Directly observed treatment|directly]] into or near the [[Cancer (disease)|cancer]]) | ** [[Internal]] [[radiation therapy]] ([[radioactive]] [[substance]] is [[Usage analysis|used]] which is [[Sealed source radiotherapy|sealed]] in [[Needle|needles]], [[Seed|seeds]], [[Wire|wires]], or [[catheters]] which are [[Place cell|placed]] [[Directly observed treatment|directly]] into or near the [[Cancer (disease)|cancer]]) | ||
|- | |- | ||
|style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Targeted therapy]] | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Targeted therapy]] | ||
| | | | ||
*[[Targeted therapy]] [[Usage analysis|uses]] [[signal transduction inhibitor]] to [[Treatments|treat]] [[basal cell carcinoma]], which includes: | * [[Targeted therapy]] [[Usage analysis|uses]] [[signal transduction inhibitor]] to [[Treatments|treat]] [[basal cell carcinoma]], which includes: | ||
**[[Vismodegib]] | ** [[Vismodegib]] | ||
**[[Sonidegib]] | ** [[Sonidegib]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Biological therapy]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Biological therapy]]''' | ||
| | | | ||
* Also known as: | * Also known as: | ||
**[[Biotherapy]] | ** [[Biotherapy]] | ||
**[[Immunotherapy]] | ** [[Immunotherapy]] | ||
*[[Immunotherapy]] [[Usage analysis|uses]] [[Human body|body's]] own [[immune system]] to [[Killer cell|kill]] [[cancer cells]] | * [[Immunotherapy]] [[Usage analysis|uses]] [[Human body|body's]] own [[immune system]] to [[Killer cell|kill]] [[cancer cells]] | ||
*Commonly [[Usage analysis|used]] [[Immunotherapy|immunotherapeutic]] [[Agent Blue|agents]] include: | * Commonly [[Usage analysis|used]] [[Immunotherapy|immunotherapeutic]] [[Agent Blue|agents]] include: | ||
**[[Injection (medicine)|Injectable]] [[interferon]] ([[SCC]]) | ** [[Injection (medicine)|Injectable]] [[interferon]] ([[SCC]]) | ||
**[[Topical application|Topical]] [[imiquimod]] ([[Basal cell carcinoma|BCC]]) | ** [[Topical application|Topical]] [[imiquimod]] ([[Basal cell carcinoma|BCC]]) | ||
| | | | ||
*[[Done]] when [[surgery]] or [[radiation therapy]] has [[Failure|failed]] to [[cure]] [[skin]] [[cancer]] | * [[Done]] when [[surgery]] or [[radiation therapy]] has [[Failure|failed]] to [[cure]] [[skin]] [[cancer]] | ||
|} | |} | ||
| Line 601: | Line 629: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Avoidance reaction|Avoiding]] [[Sunburn|sunburns]] and [[Suntanning|suntans]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Avoidance reaction|Avoiding]] [[Sunburn|sunburns]] and [[Suntanning|suntans]] | ||
| | | | ||
*[[Avoidance response|Avoid]] [[sun exposure]]: | * [[Avoidance response|Avoid]] [[sun exposure]]: | ||
** During the middle of the [[Day spa|day]], usually from 10 AM to 4 PM, especially in North America | ** During the middle of the [[Day spa|day]], usually from 10 AM to 4 PM, especially in North America | ||
** Even during [[Cloud|cloudy]] [[Day spa|days]] or winters | ** Even during [[Cloud|cloudy]] [[Day spa|days]] or winters | ||
| Line 610: | Line 638: | ||
* Tightly woven, [[Dark matter|dark]] clothing | * Tightly woven, [[Dark matter|dark]] clothing | ||
* Shirts with long sleeves | * Shirts with long sleeves | ||
*[[Broad Institute|Broad]]-brimmed hats | * [[Broad Institute|Broad]]-brimmed hats | ||
* Pants that [[Full service|fully]] [[Cover test|cover]] the [[legs]] ([[Avoidance response|avoid]] shorts) | * Pants that [[Full service|fully]] [[Cover test|cover]] the [[legs]] ([[Avoidance response|avoid]] shorts) | ||
* Photoprotective clothing | * Photoprotective clothing | ||
*[[Sunglasses]] (the ones which [[Block design|block]] both types of [[UV radiation]] i.e. [[UVA radiation|UVA]] & [[UVB radiation|UVB]]) | * [[Sunglasses]] (the ones which [[Block design|block]] both types of [[UV radiation]] i.e. [[UVA radiation|UVA]] & [[UVB radiation|UVB]]) | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wear red day|Wearing]] [[SPF]] [[sunscreen]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Wear red day|Wearing]] [[SPF]] [[sunscreen]] | ||
| | | | ||
*[[Wear red day|Wear]] a [[sunscreen]] generously [[year]]-round, even during winters & cloudy days | * [[Wear red day|Wear]] a [[sunscreen]] generously [[year]]-round, even during winters & cloudy days | ||
* It should be at least [[SPF]] 30 | * It should be at least [[SPF]] 30 | ||
* It should be [[broad-spectrum]] [[Blocking (statistics)|blocking]] both [[UVA radiation|UVA]] and [[UVB radiation|UVB rays]] | * It should be [[broad-spectrum]] [[Blocking (statistics)|blocking]] both [[UVA radiation|UVA]] and [[UVB radiation|UVB rays]] | ||
*[[Cover test|Cover]] all the [[Exposure effect|exposed]] [[Area|areas]] including the [[back]] of [[hands]], [[neck]], [[lips]], tip of [[ears]] | * [[Cover test|Cover]] all the [[Exposure effect|exposed]] [[Area|areas]] including the [[back]] of [[hands]], [[neck]], [[lips]], tip of [[ears]] | ||
* Reapply it every 2 hours & more often after [[swimming]] or if [[Perspiration|perspiring]] a lot | * Reapply it every 2 hours & more often after [[swimming]] or if [[Perspiration|perspiring]] a lot | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Avoidance response|Avoiding]] [[Tanning booths|tanning beds]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Avoidance response|Avoiding]] [[Tanning booths|tanning beds]]''' | ||
| | | | ||
*[[Tanning booths|Tanning beds]] [[Usage analysis|use]] the [[Light|lights]] that emit [[Ultraviolet|UV]] [[Ray (optics)|rays]] which can increase the [[RiskMetrics|risk]] for [[skin]] [[cancer]] | * [[Tanning booths|Tanning beds]] [[Usage analysis|use]] the [[Light|lights]] that emit [[Ultraviolet|UV]] [[Ray (optics)|rays]] which can increase the [[RiskMetrics|risk]] for [[skin]] [[cancer]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Being aware of [[Sun exposure|sun]]-[[Sensitization|sensitizing]] [[medications]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Being aware of [[Sun exposure|sun]]-[[Sensitization|sensitizing]] [[medications]]''' | ||
| | | | ||
*[[Over-the-counter drugs]] and common [[prescriptions]] including [[antibiotics]] may have tendency to increase the [[sensitivity]] of [[skin]] | * [[Over-the-counter drugs]] and common [[prescriptions]] including [[antibiotics]] may have tendency to increase the [[sensitivity]] of [[skin]] | ||
* Always [[Ask a question|ask]] the [[Doctor of Medicine|doctor]] or [[pharmacist]] about the [[Possibility theory|possible]] [[side effects]] of any [[medications]] before taking them | * Always [[Ask a question|ask]] the [[Doctor of Medicine|doctor]] or [[pharmacist]] about the [[Possibility theory|possible]] [[side effects]] of any [[medications]] before taking them | ||
| Line 637: | Line 665: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Check|Checking]] [[skin]] regularly and [[Reporting disease cases|reporting]] any [[new]] or unusual [[skin changes]] to the [[Doctor of Medicine|doctor]]''' | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Check|Checking]] [[skin]] regularly and [[Reporting disease cases|reporting]] any [[new]] or unusual [[skin changes]] to the [[Doctor of Medicine|doctor]]''' | ||
| | | | ||
*[[Examination|Examine]] the [[skin]] often for any [[new]] [[skin]] [[Growth|growths]] or [[Change detection|changes]] in [[Existential therapy|existing]] [[moles]], [[Bumps on skin|bumps]], [[birthmarks]], & [[freckles]] | * [[Examination|Examine]] the [[skin]] often for any [[new]] [[skin]] [[Growth|growths]] or [[Change detection|changes]] in [[Existential therapy|existing]] [[moles]], [[Bumps on skin|bumps]], [[birthmarks]], & [[freckles]] | ||
*[[Check]] [[face]], [[ears]], [[neck]], and [[scalp]] by [[Usage analysis|using]] the [[mirror]] | * [[Check]] [[face]], [[ears]], [[neck]], and [[scalp]] by [[Usage analysis|using]] the [[mirror]] | ||
*[[Examination|Examine]] the [[chest]], [[trunk]], [[Top7|top]] & [[Arm pit|underside of arms]] and [[hands]] | * [[Examination|Examine]] the [[chest]], [[trunk]], [[Top7|top]] & [[Arm pit|underside of arms]] and [[hands]] | ||
*[[Examination|Examine]] both the [[Frontal|front]] and [[back]] of [[legs]], and [[feet]], including [[soles]] and spaces between the [[toes]] | * [[Examination|Examine]] both the [[Frontal|front]] and [[back]] of [[legs]], and [[feet]], including [[soles]] and spaces between the [[toes]] | ||
*Also [[check]] the [[genital area]] and [[area]] between the [[buttocks]] | * Also [[check]] the [[genital area]] and [[area]] between the [[buttocks]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Watching pages|Watching]] [[dysplastic nevi]] ([[Abnormality (behavior)|abnormal]] [[Irregular lesion|irregular]] multiple [[moles]]) regularly | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Watching pages|Watching]] [[dysplastic nevi]] ([[Abnormality (behavior)|abnormal]] [[Irregular lesion|irregular]] multiple [[moles]]) regularly | ||
| Line 649: | Line 677: | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Reducing equivalent|Reducing]] the [[Exposure effect|exposure]] to [[Ultraviolet radiation|ultraviolet (UV) radiation]], especially during the early [[Year|years]] of [[life]] | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Reducing equivalent|Reducing]] the [[Exposure effect|exposure]] to [[Ultraviolet radiation|ultraviolet (UV) radiation]], especially during the early [[Year|years]] of [[life]] | ||
| | | | ||
*[[Prior probability|Prior]] [[History and Physical examination|history]] of [[radiation exposure]] (both [[Ultraviolet|UV]] or artifical [[radiation therapy]] for [[acne]] or [[eczema]]) [[Lead|leads]] to increased [[chance]] for [[development]] of [[basal cell carcinoma]] | * [[Prior probability|Prior]] [[History and Physical examination|history]] of [[radiation exposure]] (both [[Ultraviolet|UV]] or artifical [[radiation therapy]] for [[acne]] or [[eczema]]) [[Lead|leads]] to increased [[chance]] for [[development]] of [[basal cell carcinoma]] | ||
|} | |} | ||
===Effectiveness of sunscreen in prevention of skin cancer=== | ===Effectiveness of sunscreen in prevention of skin cancer=== | ||
Multiple studies have been carried out to find out the effectiveness of sunscreen in protection against skin cancer<ref name="pmid28038885">{{cite journal| author=Young AR, Claveau J, Rossi AB| title=Ultraviolet radiation and the skin: Photobiology and sunscreen photoprotection. | journal=J Am Acad Dermatol | year= 2017 | volume= 76 | issue= 3S1 | pages= S100-S109 | pmid=28038885 | doi=10.1016/j.jaad.2016.09.038 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28038885 }} </ref><ref name="pmid22913442">{{cite journal| author=Burnett ME, Hu JY, Wang SQ| title=Sunscreens: obtaining adequate photoprotection. | journal=Dermatol Ther | year= 2012 | volume= 25 | issue= 3 | pages= 244-51 | pmid=22913442 | doi=10.1111/j.1529-8019.2012.01503.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22913442 }} </ref><ref name="pmid18806906">{{cite journal| author=Bissonnette R| title=Update on sunscreens. | journal=Skin Therapy Lett | year= 2008 | volume= 13 | issue= 6 | pages= 5-7 | pmid=18806906 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18806906 }} </ref><ref name="pmid20532468">{{cite journal| author=Medeiros VL, Lim HW| title=Sunscreens in the management of photodermatoses. | journal=Skin Therapy Lett | year= 2010 | volume= 15 | issue= 6 | pages= 1-3 | pmid=20532468 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20532468 }} </ref><ref name="pmid23464719">{{cite journal| author=Diaz JH, Nesbitt LT| title=Sun exposure behavior and protection: recommendations for travelers. | journal=J Travel Med | year= 2013 | volume= 20 | issue= 2 | pages= 108-18 | pmid=23464719 | doi=10.1111/j.1708-8305.2012.00667.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23464719 }} </ref><ref name="pmid29161214">{{cite journal| author=Andersen PA, Buller DB, Walkosz BJ, Scott MD, Beck L, Liu X et al.| title=A Randomized Trial of an Advanced Sun Safety Intervention for Vacationers at 41 North American Resorts. | journal=J Health Commun | year= 2017 | volume= 22 | issue= 12 | pages= 951-963 | pmid=29161214 | doi=10.1080/10810730.2017.1382615 | pmc=6309206 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29161214 }} </ref><ref name="pmid28189810">{{cite journal| author=Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR| title=Effect of an intervention on observed sun protection by vacationers in a randomized controlled trial at North American resorts. | journal=Prev Med | year= 2017 | volume= 99 | issue= | pages= 29-36 | pmid=28189810 | doi=10.1016/j.ypmed.2017.01.014 | pmc=5432386 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28189810 }} </ref><ref name="pmid26593781">{{cite journal| author=Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR| title=Rationale, design, samples, and baseline sun protection in a randomized trial on a skin cancer prevention intervention in resort environments. | journal=Contemp Clin Trials | year= 2016 | volume= 46 | issue= | pages= 67-76 | pmid=26593781 | doi=10.1016/j.cct.2015.11.015 | pmc=4714565 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26593781 }} </ref><ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence|journal=Journal of Cutaneous Medicine and Surgery|year=2019|pages=120347541985661|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | * Multiple [[Study design|studies]] have been [[Carrying capacity|carried]] out to find out the [[Effective method|effectiveness]] of [[sunscreen]] in [[Protecting group|protection]] against [[skin cancer]] | ||
* '''International [[standard]] [[quantity]] of [[sunscreen]]''' application [[Usage analysis|used]] to determine [[SPF]] is '''2 mg/cm''' but mostly [[People's Solidarity|people]] apply only 0.5 to 1.5 mg/cm2 of [[sunscreen]] and don't reapply [[sunscreens]] after [[sweating]] excessively or [[swimming]]<ref name="pmid11712033">{{cite journal| author=Diffey BL| title=When should sunscreen be reapplied? | journal=J Am Acad Dermatol | year= 2001 | volume= 45 | issue= 6 | pages= 882-5 | pmid=11712033 | doi=10.1067/mjd.2001.117385 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11712033 }} </ref><ref name="urlSunscreens in the Management of Photodermatoses">{{cite web |url=https://www.skintherapyletter.com/sunscreen/photodermatoses/ |title=Sunscreens in the Management of Photodermatoses |format= |work= |accessdate=}}</ref><ref name="urlUpdate on Sunscreens">{{cite web |url=https://www.skintherapyletter.com/sunscreen/advances-update/ |title=Update on Sunscreens |format= |work= |accessdate=}}</ref><ref name="pmid28038885">{{cite journal| author=Young AR, Claveau J, Rossi AB| title=Ultraviolet radiation and the skin: Photobiology and sunscreen photoprotection. | journal=J Am Acad Dermatol | year= 2017 | volume= 76 | issue= 3S1 | pages= S100-S109 | pmid=28038885 | doi=10.1016/j.jaad.2016.09.038 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28038885 }} </ref><ref name="pmid22913442">{{cite journal| author=Burnett ME, Hu JY, Wang SQ| title=Sunscreens: obtaining adequate photoprotection. | journal=Dermatol Ther | year= 2012 | volume= 25 | issue= 3 | pages= 244-51 | pmid=22913442 | doi=10.1111/j.1529-8019.2012.01503.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22913442 }} </ref><ref name="pmid18806906">{{cite journal| author=Bissonnette R| title=Update on sunscreens. | journal=Skin Therapy Lett | year= 2008 | volume= 13 | issue= 6 | pages= 5-7 | pmid=18806906 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18806906 }} </ref><ref name="pmid20532468">{{cite journal| author=Medeiros VL, Lim HW| title=Sunscreens in the management of photodermatoses. | journal=Skin Therapy Lett | year= 2010 | volume= 15 | issue= 6 | pages= 1-3 | pmid=20532468 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20532468 }} </ref><ref name="pmid23464719">{{cite journal| author=Diaz JH, Nesbitt LT| title=Sun exposure behavior and protection: recommendations for travelers. | journal=J Travel Med | year= 2013 | volume= 20 | issue= 2 | pages= 108-18 | pmid=23464719 | doi=10.1111/j.1708-8305.2012.00667.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23464719 }} </ref><ref name="pmid29161214">{{cite journal| author=Andersen PA, Buller DB, Walkosz BJ, Scott MD, Beck L, Liu X et al.| title=A Randomized Trial of an Advanced Sun Safety Intervention for Vacationers at 41 North American Resorts. | journal=J Health Commun | year= 2017 | volume= 22 | issue= 12 | pages= 951-963 | pmid=29161214 | doi=10.1080/10810730.2017.1382615 | pmc=6309206 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29161214 }} </ref><ref name="pmid28189810">{{cite journal| author=Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR| title=Effect of an intervention on observed sun protection by vacationers in a randomized controlled trial at North American resorts. | journal=Prev Med | year= 2017 | volume= 99 | issue= | pages= 29-36 | pmid=28189810 | doi=10.1016/j.ypmed.2017.01.014 | pmc=5432386 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28189810 }} </ref><ref name="pmid26593781">{{cite journal| author=Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR| title=Rationale, design, samples, and baseline sun protection in a randomized trial on a skin cancer prevention intervention in resort environments. | journal=Contemp Clin Trials | year= 2016 | volume= 46 | issue= | pages= 67-76 | pmid=26593781 | doi=10.1016/j.cct.2015.11.015 | pmc=4714565 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26593781 }} </ref><ref name="LiColantonio2019">{{cite journal|last1=Li|first1=Heidi|last2=Colantonio|first2=Sophia|last3=Dawson|first3=Andrea|last4=Lin|first4=Xing|last5=Beecker|first5=Jennifer|title=Sunscreen Application, Safety, and Sun Protection: The Evidence|journal=Journal of Cutaneous Medicine and Surgery|year=2019|pages=120347541985661|issn=1203-4754|doi=10.1177/1203475419856611}}</ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
|+Different sunscreen | |+Different sunscreen recommendations and recommendations' grading according to Canadian Task Force on Preventive Health Care (CTFPHC) GRADE System | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Sunscreen property}} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Sunscreen property}} | ||
! style="background: #4479BA; width: | ! style="background: #4479BA; width: 500px;" | {{fontcolor|#FFF|Recommendation}} | ||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF| | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Grade of Recommendations}} | ||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[SPF]] ([[Sun Protection Factor]]) | |||
| | |||
* An [[Idealization|ideal]] [[sunscreen]] should have the following properties: | |||
** [[Broad-spectrum]] | |||
** Both [[UVA radiation|UVA]] & [[UVB radiation|UVB]] [[Filter (chemistry)|filters]] | |||
** Atleast [[SPF]] 30 | |||
| rowspan="8" | | |||
* '''[[Strong|Strongly]] recommended''' | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Water]] [[resistance]] | |||
| | |||
* [[Sunscreen]] providing [[water]]-[[resistance]] for 40-80 [[Minute|minutes]] must be worn in following [[conditions]]: | |||
** [[Water]] [[Immersion Therapy|immersion]] | |||
** Excessive [[sweating]] | |||
** Contact with sand | |||
** Physical contact [[Causes|causing]] increased [[skin]] [[friction]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Organic Chemistry|Organic]] vs [[inorganic]] [[sunscreens]] | |||
| | |||
* Whether the components of [[sunscreen]] are [[Organic Chemistry|organic]] or [[inorganic]], the recommended [[sunscreen]] must be [[broad spectrum]] with both [[UVA radiation|UVA]] & [[UVB radiation|UVB]] [[Filter (chemistry)|filters]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Lip]] [[Protecting group|protection]] | |||
| | |||
* Whole [[lip]] should be generously covered by high-[[SPF]] (>/= 30) and reapplication of [[lip]] [[sunscreen]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Sunscreen]] application | |||
| | |||
* [[Sunscreen]] is recommended to be applied according to the following [[Guideline (medical)|guidelines]]: | |||
** Should be applied liberally (approximately 45 ml) to all the [[Exposure (photography)|exposed]] [[Area|areas]] | |||
** [[Strong]] reapplication within a [[period]] of 8 hours is [[Mandatory labelling|mandatory]] only after [[Activities of daily living|activities]] that may remove the [[sunscreen]] layer such as [[sweating]], [[swimming]], or [[friction]] | |||
** Should be applied before any [[sun exposure]] and at least 20 [[Minute|minutes]] before the [[water]] [[Activities of daily living|activities]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Patient education]] on [[sunscreen]] | |||
| | |||
* [[Patients]] should be [[Education|educated]] about the [[Mean|meaning]] of [[SPF]] and its [[Effective method|effectiveness]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Sunscreen]] [[Safety film|safety]] | |||
| | |||
* [[Sunscreens]] have a favorable [[RiskMetrics|risk]]-benefit profile, hence, are considered to be safe overall | |||
* There is still a [[RiskMetrics|risk]] of following [[Fewmets|few]] [[complications]] due to [[sunscreen]] application in some [[People's Solidarity|people]]: | |||
** [[Photoallergy]] (most common, but quite [[rare]]) | |||
** [[Reproductive]] [[toxicity]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Sunscreen]] benefits | |||
| | |||
* [[Prevention (medical)|Prevents]] photoaging | |||
* [[Prevention (medical)|Prevents]] [[melanoma]] and non–[[melanoma]] [[skin cancer]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Sunscreen]] [[Vehicle extrication|vehicle]] | |||
| | |||
* Highest [[SPF]] and [[water]] [[resistance]] properties of [[sunscreen]] can be obtained by [[Usage analysis|using]] a '''[[water]]-in-[[oil]] [[emulsion]]''' [[formulation]] for [[sunscreens]] | |||
| rowspan="2" | | |||
* '''Weakly recommended''' | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |[[Expiration|Expiry]] date | |||
| | |||
* Avoid [[Usage analysis|using]] [[sunscreens]] past their manufacturer-[[Specific activity|specified]] [[Expiration|expiry]] date/recommended [[period]] after opening | |||
* [[Sunscreens]] should be [[Storage (memory)|stored]] at [[normal]] [[room temperature]] in order to ensure their proper [[stability]] | |||
|} | |||
{| class="wikitable" | |||
|+US FDA monograph list of active ingredients of sunscreen | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Type of filter}} | |||
! colspan="2" style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|Name of UV filter}} | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Concentration in percentage}} | |||
|- | |||
| rowspan="9" style="padding: 5px 5px; background: #DCDCDC; font-weight: bold"|'''[[Organic Chemistry|Organic]] [[UVB radiation|UVB]] [[Filter (chemistry)|Filters]]''' | |||
| rowspan="2" |'''Cinnamates''' | |||
|Octinoxate ([[octyl methoxycinnamate]], Parsol MCX) | |||
|7.5% | |||
|- | |||
|[[Cinoxate]] | |||
|3% | |||
|- | |||
| rowspan="2" |'''[[PABA|PABA derivatives]]''' | |||
|15% [[Para-aminobenzoic acid]] ([[PABA]]) | |||
|15% | |||
|- | |||
|[[Padimate O]] (octyl dimethyl [[PABA]]) | |||
|8% | |||
|- | |||
| rowspan="3" |'''[[Salicylates]]''' | |||
|Octisalate ([[octyl salicylate]]) | |||
|5% | |||
|- | |||
|[[Homosalate]] | |||
|15% | |||
|- | |||
|[[Trolamine salicylate]] | |||
|12% | |||
|- | |||
| rowspan="2" |'''Others''' | |||
|[[Octocrylene]] | |||
|10% | |||
|- | |||
|Ensulizole ([[phenylbenzimidazole sulfonic acid]]) | |||
|4% | |||
|- | |||
| rowspan="5" style="padding: 5px 5px; background: #DCDCDC; font-weight: bold"|'''[[Organic Chemistry|Organic]] [[UVA radiation|UVA]] [[Filter (chemistry)|Filters]]''' | |||
| rowspan="3" |'''[[Benzophenone|Benzophenones]]''' | |||
|[[Oxybenzone]] ([[benzophenone]]-3) | |||
|6% | |||
|- | |||
|Sulisobenzone ([[benzophenone]]-4) | |||
|10% | |||
|- | |||
|[[Dioxybenzone]] ([[benzophenone]]-8) | |||
|3% | |||
|- | |||
| rowspan="2" |'''Others''' | |||
|[[Butyl]] methoxydibenzoylmethane ([[avobenzone]], Parsol 1789) | |||
|3% | |||
|- | |||
|Meradimate (menthyl anthranilate) | |||
|5% | |||
|- | |||
| rowspan="2" style="padding: 5px 5px; background: #DCDCDC; font-weight: bold"|'''[[Inorganic]] [[Filter (chemistry)|Filters]]''' | |||
| colspan="2" |'''[[Titanium dioxide]]''' | |||
|25% | |||
|- | |||
| colspan="2" |'''[[Zinc oxide]]''' | |||
|25% | |||
|} | |||
{| class="wikitable" | |||
|+Measurement of UV protection afforded by sunscreens and clothing | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Measurement system}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''SPF (Sun protection factor)'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''UVA‐PF (UVA‐protection factor''')}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''UPF (Ultraviolet protection factor)'''}} | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''Definition''' | ||
| | | | ||
* [[Minimum|Minimal]] [[erythema]] [[dose]] ([[MED]]) of [[UVB radiation]] [[Causes|causing]] [[erythema]] after [[Applicability Domain|applying]] 2 mg/cm2 of [[sunscreen]] to [[skin]] [[Division (biology)|divided]] by the [[dose]] [[Product (biology)|producing]] 1 [[MED]] on unprotected [[skin]] | |||
| | | | ||
* The [[Dose (biochemistry)|dose]] of [[UVA radiation|UVA]] [[Causes|causing]] [[observable]] [[pigment]] [[Dark matter|darkening]] ([[Minimum|minimal]] [[pigment]] [[dose]] [MPD]) after applying 2 mg/cm2 of [[sunscreen]] to [[skin]] divided by the [[dose]] [[Product (biology)|producing]] 1 MPD on unprotected [[skin]] | |||
| | |||
* The [[Ability grouping|ability]] of fabrics to [[Prevention (medical)|prevent]] [[UV radiation]] [[Transmission (medicine)|transmission]] via [[absorption]] and/or [[Reflection (physics)|reflection]] and highly [[Dependent variable|dependent]] on fabric type, [[color]], [[porosity]], thickness, [[weight]], and other factors | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Development|Developed]] for''' | ||
| | |||
* [[Sunscreens]] | |||
| | | | ||
* [[Sunscreens]] | |||
| | | | ||
* Clothing | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[GlobalCures|Global]] [[Acceptor|acceptance]]''' | ||
| | |||
* International | |||
| | | | ||
* [[United States]] only | |||
| | | | ||
* International | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Ultraviolet|UV]] [[wavelengths]] [[Protected health information|protected]]''' | ||
| | | | ||
* [[UVB radiation|UVB]] | |||
| | | | ||
* [[UVA radiation|UVA]] | |||
| | |||
* [[UVA radiation|UVA]], [[UVB radiation|UVB]] | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''[[Example 1|Examples]]''' | ||
| | | | ||
* [[SPF]] 2 [[Protecting group|protects]] against 50% of [[UVB radiation|UVB]] | |||
* [[SPF]] 8 [[Protecting group|protects]] against 88% of [[UVB radiation|UVB]] | |||
* [[SPF]] 15 [[Protecting group|protects]] against 93% of [[UVB radiation|UVB]] | |||
* [[SPF]] 30 [[Protecting group|protects]] against 97% of [[UVB radiation|UVB]] | |||
* [[SPF]] 50 [[Protecting group|protects]] against 98% of [[UVB radiation|UVB]] | |||
| | | | ||
* [[UVA radiation|UVA]]‐PF1 [[Protecting group|protects]] against 20–39% of [[UVA radiation|UVA]] | |||
* [[UVA radiation|UVA]]‐PF2 [[Protecting group|protects]] against 40–69% of [[UVA radiation|UVA]] | |||
* [[UVA radiation|UVA]]‐PF3 [[Protecting group|protects]] against 70–95% of [[UVA radiation|UVA]] | |||
* [[UVA radiation|UVA]]‐PF4 [[Protecting group|protects]] against >95% of [[UVA radiation|UVA]] | |||
| | |||
* [[UPF1|UPF]] cotton 5–10 | |||
* [[UPF1|UPF]] denim 1700 | |||
|} | |||
{| class="wikitable" | |||
|+Knowing individual skin type and using the right sunscreen accordingly | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|'''Skin type by the Fitzpatrick Scale'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''Skin color'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''Skin tone or other common descriptors'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''Sun exposure effects'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|'''Recommended sunscreen SPF'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|''' 1 MED- Minimal erythemal dose (as SED- standard erythemal dose)'''}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|''' Susceptibility to skin cancer'''}} | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''I''' | ||
| | | | ||
* [[Pale skin|Pale]] white | |||
| | | | ||
* [[Paleness|Pale]] or [[albino]], [[freckles]] common ([[Celtic (water)|Celtic]]) | |||
| | |||
* Always [[burns]] (very readily) | |||
* Never tans | |||
| rowspan="2" |30+ | |||
| | |||
* 2-3 | |||
| | |||
* Very high | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''II''' | ||
| | |||
* White | |||
| | |||
* [[Light]] or fair (European) | |||
| | | | ||
* Always [[burns]] (readily) | |||
* Rarely tans | |||
| | | | ||
* 3-4 | |||
| | |||
* Very high | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''III''' | ||
| | | | ||
* White | |||
| | | | ||
* [[Light]]‐intermediate (Dark European) | |||
| | |||
* Sometimes [[burns]] (moderately) | |||
* Sometimes tans | |||
| rowspan="4" |15+ | |||
| | |||
* 4-5 | |||
| | |||
* High | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''IV''' | ||
| | | | ||
* [[Light]] brown | |||
| | | | ||
* [[Olive]] with/without [[brown]] tint (Mediterranean) | |||
| | |||
* Tans easily | |||
*[[Burns]] less (occasionally) | |||
| | |||
* 5-6 | |||
| | |||
* Moderate | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''V''' | ||
| | | | ||
* Dark [[brown]] | |||
| | | | ||
* [[Brown]] | |||
| | |||
* Tans easily and substantially | |||
* Rarely [[burns]] | |||
| | |||
* 8-12 | |||
| | |||
* Low | |||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | | style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" |'''VI''' | ||
| | |||
* [[Black]] | |||
| | |||
* [[Black]] | |||
| | |||
* Tans readily and profusely | |||
* Does not [[burn]] | |||
| | | | ||
* 16-24 | |||
| | | | ||
* Low | |||
|} | |} | ||
===Skin Cancer Prevention Facial-Aging Mobile App=== | ===Skin Cancer Prevention by using Facial-Aging Mobile App=== | ||
app<ref name="pmid29523502">{{cite journal| author=Brinker TJ, Heckl M, Gatzka M, Heppt MV, Resende Rodrigues H, Schneider S et al.| title=A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study. | journal=JMIR Mhealth Uhealth | year= 2018 | volume= 6 | issue= 3 | pages= e60 | pmid=29523502 | doi=10.2196/mhealth.9794 | pmc=5866300 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29523502 }} </ref><ref name="pmid28887295">{{cite journal| author=Brinker TJ, Brieske CM, Schaefer CM, Buslaff F, Gatzka M, Petri MP et al.| title=Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study. | journal=J Med Internet Res | year= 2017 | volume= 19 | issue= 9 | pages= e319 | pmid=28887295 | doi=10.2196/jmir.8661 | pmc=5610355 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28887295 }} </ref><ref name="pmid28747297">{{cite journal| author=Brinker TJ, Schadendorf D, Klode J, Cosgarea I, Rösch A, Jansen P et al.| title=Photoaging Mobile Apps as a Novel Opportunity for Melanoma Prevention: Pilot Study. | journal=JMIR Mhealth Uhealth | year= 2017 | volume= 5 | issue= 7 | pages= e101 | pmid=28747297 | doi=10.2196/mhealth.8231 | pmc=5550737 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28747297 }} </ref> | * [[Study design|Studies]] show that photoaging mobile app [[Usage analysis|usage]] by different [[Adolescent|adolescents]] actually [[Motivation|motivates]] them to [[Avoidance response|avoid]] the [[Ultraviolet|UV]] [[Exposure (photography)|exposure]] after [[Lookahead|looking]] at their 3D selfie<ref name="pmid29523502">{{cite journal| author=Brinker TJ, Heckl M, Gatzka M, Heppt MV, Resende Rodrigues H, Schneider S et al.| title=A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study. | journal=JMIR Mhealth Uhealth | year= 2018 | volume= 6 | issue= 3 | pages= e60 | pmid=29523502 | doi=10.2196/mhealth.9794 | pmc=5866300 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29523502 }} </ref><ref name="pmid28887295">{{cite journal| author=Brinker TJ, Brieske CM, Schaefer CM, Buslaff F, Gatzka M, Petri MP et al.| title=Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study. | journal=J Med Internet Res | year= 2017 | volume= 19 | issue= 9 | pages= e319 | pmid=28887295 | doi=10.2196/jmir.8661 | pmc=5610355 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28887295 }} </ref><ref name="pmid28747297">{{cite journal| author=Brinker TJ, Schadendorf D, Klode J, Cosgarea I, Rösch A, Jansen P et al.| title=Photoaging Mobile Apps as a Novel Opportunity for Melanoma Prevention: Pilot Study. | journal=JMIR Mhealth Uhealth | year= 2017 | volume= 5 | issue= 7 | pages= e101 | pmid=28747297 | doi=10.2196/mhealth.8231 | pmc=5550737 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28747297 }} </ref> | ||
* One of the [[Study design|studies]] [[Motivation|motivated]]:<ref name="urlJMU - A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study | Brinker | JMIR mHealth and uHealth">{{cite web |url=https://mhealth.jmir.org/2018/3/e60/ |title=JMU - A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study | Brinker | JMIR mHealth and uHealth |format= |work= |accessdate=}}</ref> | |||
** 90.5% [[People's Solidarity|people]] to avoid using a [[Tanning booth|tanning bed]] | |||
** 90.2% [[People's Solidarity|people]] to improve their [[Sun protection factor|sun protection]] | |||
* Another [[Study design|study]] showed the positive [[Effective method|effectiveness]] of photoaging mobile app in [[Change detection|changing]] [[behavioral]] [[Prediction|predictors]] in [[Adolescent|adolescents]] with fair [[skin]] (i.e. [[Fitzpatrick scale|Fitzpatrick]] [[skin]] types 1-2)<ref name="BrinkerBrieske2017">{{cite journal|last1=Brinker|first1=Titus Josef|last2=Brieske|first2=Christian Martin|last3=Schaefer|first3=Christoph Matthias|last4=Buslaff|first4=Fabian|last5=Gatzka|first5=Martina|last6=Petri|first6=Maximilian Philip|last7=Sondermann|first7=Wiebke|last8=Schadendorf|first8=Dirk|last9=Stoffels|first9=Ingo|last10=Klode|first10=Joachim|title=Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study|journal=Journal of Medical Internet Research|volume=19|issue=9|year=2017|pages=e319|issn=1438-8871|doi=10.2196/jmir.8661}}</ref><ref name="BrinkerSchadendorf2017">{{cite journal|last1=Brinker|first1=Titus Josef|last2=Schadendorf|first2=Dirk|last3=Klode|first3=Joachim|last4=Cosgarea|first4=Ioana|last5=Rösch|first5=Alexander|last6=Jansen|first6=Philipp|last7=Stoffels|first7=Ingo|last8=Izar|first8=Benjamin|title=Photoaging Mobile Apps as a Novel Opportunity for Melanoma Prevention: Pilot Study|journal=JMIR mHealth and uHealth|volume=5|issue=7|year=2017|pages=e101|issn=2291-5222|doi=10.2196/mhealth.8231}}</ref> | |||
==Related Chapters== | ==Related Chapters== | ||
Latest revision as of 20:50, 19 August 2020
|
Skin cancer Microchapters |
| Skin cancer | |
| ICD-10 | C43-C44 |
|---|---|
| ICD-9 | 172, 173 |
| ICD-O: | 8010-8720 |
| MeSH | D012878 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4] Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[5]
Overview
Skin cancer is the malignant growth on the skin which is the most common type of malignancy in Caucasians. Skin cancer generally develops in the epidermis (the outermost layer of skin), so a tumor is usually clearly visible. This makes most skin cancers detectable in the early stages. Skin cancer is broadly classified into melanoma and non-melanoma skin cancer (NMSC) with most common NMSC types to be squamous cell carcinoma and basal cell carcinoma. Most common cause of skin cancer is DNA mutations caused by UV irradiation over a proplonged period of time especially in fair-skinned individuals. Skin cancer is the fastest growing type of cancer in the United States. Skin cancer represents the most commonly diagnosed malignancy, surpassing lung, breast, colorectal and prostate cancer. More than 1 million Americans were estimated to be diagnosed with skin cancer in 2007. Skin cancer can be treated by surgery, or other non-surgical options such as cryotherapy, electrotherapy, curettage, photodynamic therapy, chemical peel, chemotherapy, radiation therapy, targeted therapy and biological therapy. Cancers caused by UV exposure may be prevented by avoiding exposure to sunlight or other UV sources, wearing sun-protective clothes, and using a broad-spectrum sunscreen.
Historical Perspective
- In 1928, sunscreens were first introduced in United States after which they gained tremendous commercial success[1]
- In 1978, US FDA first adopted the efficacy of protection by sunscreens as indicated by the sun protection factor (SPF)[1]
- In 1988, Bestor first identified DNA methyltransferase 1 (DNMT1), which is the primary target of UV radiations in carcinogenic process of skin cancer[2]
- From 1992 to 1994, free American Academy of Dermatology's National Skin Cancer Early Detection and Screening Program was launched which provided broad skin cancer educational information to general public and enabled almost 750,000 free expert skin cancer examinations which mostly found out thin, localized stage 1 melanomas with high projected 5-year survival rate[3][4]
- From 2001 to 2005, American Academy of Dermatology National Melanoma/Skin Cancer Screening Program was launched which led to the conclusion that HARMM criteria can be used to identify the higher-risk subgroup of skin cancer screening population via assessment of multiple risk factors for MM , which will not only reduce the cost but will also increase the yields for suspected MM in future mass screening initiatives[5]
- In 2007, more than 1 million Americans were estimated to be diagnosed with skin cancer
- In 2014, 6500 new cases of melanoma and 76,100 cases of NMSC were estimated to have occurred in Canada[1]
- In 2016, the estimated number of new cases of skin melanoma was 76,380 which is 4.5% of all new cancer cases
- In 2016, a National Consensus on Sun Safety Messages was developed in Canada in order to promote the uniformity of public health messages[1]
- From 1946 to December 2018, a search for studies related to protection by sunscreen was performed in MEDLINE
Classification
- Skin cancer is broadly divided into melanoma and nonmelanoma types as shown in the following table:[6][7][8][9][10][11][12][13][14][15]
Pathophysiology
- Skin cancer is most closely associated with chronic inflammation of the skin
Normal skin function
Normal skin anatomy
- The two main layers of skin include:
- Outer layer of epidermis (skin cancer starts in this layer), which has following three different kinds of cells:
- Top layer of epidermis is made up of thin, flat squamous cells
- Round basal cells are present below the layer of squamous cells
- Lower epidermal layer has melanin producing cells (melanocytes) which on increased sun exposure lead to more pigment production causing skin darkening
- Inner layer of dermis
- Outer layer of epidermis (skin cancer starts in this layer), which has following three different kinds of cells:
 |
 |
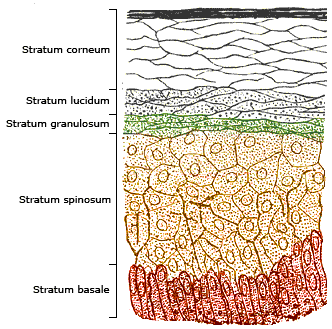 |
Epigenetics
UVA & UVB have both been implicated in causing DNA damage resulting in cancer by any of the following mechanisms:[25][26][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42]
- UV radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinase 1 and MMP3 in primary human dermal fibroblasts leading to the increased expression of MMP1 and MMP3[43]
- UVB irradiation leads to DNA CpG methylation and transcriptomic changes in following genes & cancer related pathways at the different stages of carcinogenesis:
- PTEN
- p53
- Nrf2
- p21(Waf1/Cip1)
- Inflammatory signaling
- Enf2
- Mgst2
- Vegfa
- Cdk4
- UVA irradiation causes an increase in intracellular reactive oxygen species (ROS), prostaglandin E2 (PGE2), and PGE2 receptors, which leads to decreased expression of transcription factor zinc finger E-box binding homeobox 1(ZEB1) which binds to DNA methyltransferase 1 (DNMT1) promoter and regulates its transcription, thus leading to senescence of DNMT1 in human dermal fibroblasts (HDFs). This causes low methylation level of senescence related proteins p53 thus, increasing its expression, eventually resulting in cellular senescence[28][44][45][46][47][48][49][43][50][51][52][53][2][54][55][56][57][58][27][59][60][61][62][63][64][65]
| UVA exposure to the sun-exposed skin | |||||||||||||||||||
| Suppression of the contact hypersensitivity (CHS) response | |||||||||||||||||||
| Increased intracellular ROS, PGE2, and PGE2 receptors in human dermal fibroblasts | |||||||||||||||||||
| Decreased expression of transcription factor zinc finger E-box binding homeobox 1(ZEB1) | |||||||||||||||||||
| Decreased binding of ZEB1 to DNA methyltransferase 1 (DNMT1) promoter | |||||||||||||||||||
| Senescence of DNMT1 (gene silencer) | |||||||||||||||||||
This leads to:
| |||||||||||||||||||
| Cellular senescence | |||||||||||||||||||
- UV radiation leads to overexpression of COX-2 whose end product is prostaglandin E2, involved in skin carcinogenesis[66][67][68][69]
- Overexpression of MiR-211, MiR-217 and miR-377 is associated with suppression of DNMT-1 mediated methylation of p16 and pRb, thus, inducing senescence in human skin fibroblasts[2][70][71]
- MicroRNA-152 and -181a modulate the levels of adhesion proteins and extra-cellular matrix components, such as integrin α5 and collagen XVI hence, in this way lead to senescence of human dermal fibroblasts[72]
- Decreased expression of UHRF1 (ubiquitin-like with PHD and ring finger domains 1) is the main initial event in suppressing DNMT1-mediated DNA methylation which increases WNT5A expression resulting in consequent induction of senescence[73][2]
- MicroRNA‐21 is involved in regulation of ERK/NF‐κB signaling pathway which affects the proliferation, migration, and apoptosis of human melanoma A375 cells by targeting SPRY1, PDCD4, and PTEN
| Acute | Chronic | |
|---|---|---|
| Molecular/cellular | Clinical | |
|
|
|
Gross Pathology
- Macroscopically, the tumor is often elevated, fungating, or may be ulcerated with irregular borders
- Malignant melanoma appears as a small lesion having irregular borders & portions with multiple colors such as white, pink, red, blue or blue-black
- Basal cell carcinoma appears as a waxy or a pearly bump, or a brown scar-like or flesh-colored flat lesion, or a scabbing or a bleeding sore that heals and returns
- Squamous cell carcinoma appears as a red, firm nodule or a flat lesion having a crusted, scaly surface
- Bowen's disease appears as a red or brown scaly patch/plaque on the sun-damaged skin
- Merkel cell carcinoma appears as shiny, firm nodules just beneath or on the skin & in hair follicles
- Kaposi's sarcoma appears as purple or red patches on skin or mucous membrane
Microscopic Pathology
- Microscopically, tumor cells destroy the basement membrane and form sheets or compact masses which invade the subjacent connective tissue (dermis)[9]
- In well-differentiated carcinomas, tumor cells are pleomorphic/atypical, but resembling normal keratinocytes from prickle layer (large, polygonal, with abundant eosinophilic (pink) cytoplasm and central nucleus)
- Their disposal tends to be similar to that of normal epidermis: immature/basal cells at the periphery, becoming more mature to the centre of the tumor masses
- Tumor cells transform into keratinized squamous cells and form round nodules with concentric, laminated layers, called "cell nests" or "epithelial/keratinous pearls"
- The surrounding stroma is reduced and contains inflammatory infiltrate (lymphocytes)
- Poorly differentiated squamous carcinomas contain more pleomorphic cells and no keratinization
Causes
- Skin cancer occurs due to mutations in DNA of skin cells causing them to grow out of control leading to formation of a mass of cancer cells
Epidemiology & Demographics
- Skin cancer is a common condition because of the increased exposure to UV radiation (caused by increasing popularity of sun tanning/sun bathing)[74][75][76][77][78][79]
- It is the most common malignancy in Caucasian population[80][81][82][83][84][85][86][87][88][89]
- Individuals with lighter-skin are more vulnerable to get it
- One out of every three new cancers arises from skin in United States[90]
- Incidence of both malignant melanoma (MM) and non-melanoma skin cancer (NMSC) is increasing with MM having an annual increase of 0.6% in individuals >50 years[91][92]
- In 2014, 6500 new cases of melanoma and 76,100 cases of NMSC were estimated to have occurred in Canada[1]
- In 2016, the estimated number of new cases of skin melanoma was 76,380 which is 4.5% of all new cancer cases[93]
- Annual incidence of melanoma in situ is 9.5% according to some recent epidemiological studies[93]
- National Cancer Registries has reported an underestimation of the incidence of melanoma in certain countries, hence, its incidence may even be higher than actually documented depending upon population-based varying risk factors and discrepancies in national registration systems[94]
Risk factors
Common risk factors for skin cancer include:[95][96][7]
Screening
According to different studies going on for so many years, following data is available regarding the different methods/tools and their effectiveness for skin cancer screening:
- From 1992 to 1994, free American Academy of Dermatology's National Skin Cancer Early Detection and Screening Program was launched which provided broad skin cancer educational information to general public and enabled almost 750,000 free expert skin cancer examinations which mostly found out thin, localized stage 1 melanomas with high projected 5-year survival rate[3][4]
- From 2001 to 2005, American Academy of Dermatology National Melanoma/Skin Cancer Screening Program was launched which led to the conclusion that HARMM criteria can be used to identify the higher-risk subgroup of skin cancer screening population via assessment of multiple risk factors for MM , which will not only reduce the cost but will also increase the yields for suspected MM in future mass screening initiatives[5]
- Melanoma Genetics Program identifies the genetic causes of skin cancer, and also provides genetic counseling to the individuals having a strong family history of melanoma[102][103][104][3][105][106][107]
- Dermoscopy usage improves the ability of primary care physicians to triage lesions which are suggestive of skin cancer and saves from unnecessary expert consultations[108]
- Combination of dermoscopy and short-term sequential digital dermoscopy imaging (SDDI) in a primary care setting doubles the sensitivity for melanoma diagnosis and also leads to >50% chance of reduction in excision or referral of benign pigmented lesions[109][110][111][112][113]
Diagnosis
The two sentinel features of skin cancer diagnosis are skin examination and subsequent biopsy of the suspected skin lesion. Common history, symptoms, physical examination findings and diagnostic tests are mentioned below:
History and Symptoms
Common sites of involvement
- Primarily involves the sun-exposed areas of skin such as:
- Can also involve the skin areas very rarely exposed to sun such as:
- Underneath fingernails or toenails
- Palm of the hand
- Sole of the foot
- Genital region
Common symptoms
- There are a variety of different skin cancer symptoms including crabs or changes in the skin that do not heal, ulcers in the skin, discoloration, and changes in existing moles
- Malignant melanoma appears as a small lesion having irregular borders & portions with multiple colors such as white, pink, red, blue or blue-black
- Basal cell carcinoma appears as a waxy or a pearly bump, or a brown scar-like or flesh-colored flat lesion, or a scabbing or a bleeding sore that heals and returns
- Squamous cell carcinoma appears as a red, firm nodule or a flat lesion having a crusted, scaly surface
- Actinic keratosis appears as either a rough, pink, red or brown, scaly, flat or raised patch on the skin or as peeling or cracking of lower lip not cured by lip balm or petroleum jelly and most commonly involves face and top of the hands
- Bowen's disease appears as a red or brown scaly patch/plaque on the sun-damaged skin
- Keratoacanthoma erupts with an initial rapid growth (like a little volcano) on sun-damaged skin and resolves on its own later on after few months
- Dermatofibrosarcoma protuberans begins as a minor firm area of skin resembling a bruise, birthmark, or pimple
- Merkel cell carcinoma appears as shiny, firm nodules just beneath or on the skin & in hair follicles and mostly involves head, neck and trunk
- Kaposi's sarcoma appears as purple or red patches on skin or mucous membrane
- Angiosarcoma's most common manifestation is a gradually enlarging, painless mass, with other symptoms including skin thickening, erythema, or skin discoloration (primary cutaneous),lymphedema (secondary angiosarcoma), pain, edema or other symptoms due to compressionof adjacent neurovascular structures
- Cutaneous B cell lymphoma appears as red-brown bumpy rash or nodules involving head, neck or torso of the body
- Cutaneous T-cell lymphoma has multiple manifestations including raised or scaly, itchy, round skin patches, skin patches lighter in color than the surrounding skin, lumps on skin (ulcerate or break open), hair loss, enlarged lymph nodes, intensely itchy, rash-like skin redness over whole body, and skin thickening in palms & soles
Physical Examination
- On physical examination, basal cell carcinoma usually looks like a raised, smooth, pearly bump on the sun-exposed skin of the head, neck or shoulders[114]
- Small blood vessels, crusting and bleeding in the center of tumor can be seen sometimes, hence, often mistaken as a non-healing sore
- Squamous cell carcinoma commonly appears as a red, scaling, thickened patch on sun-exposed skin with/without ulceration or bleeding, and can develop into a large mass if left untreated
- Most melanomas appear as brown to black looking lesions
- Signs indicating a malignant melanoma include change in size, shape, color or elevation of a mole
- Appearance of a new mole during adulthood, or new pain, itching, ulceration or bleeding of an existing mole should always be checked as it is suspicious for melanoma
Laboratory Tests
- Dermoscopy usage improves the ability of primary care physicians to triage lesions which are suggestive of skin cancer and saves from unnecessary expert consultations[108]
- Combination of dermoscopy and short-term sequential digital dermoscopy imaging (SDDI) in a primary care setting doubles the sensitivity for melanoma diagnosis and also leads to >50% chance of reduction in excision or referral of benign pigmented lesions[109][110][111][112][113]
Biopsy
- Skin biopsy (i.e. removal of a sample of suspicious skin for testing) is an essential component of skin cancer diagnosis and by histopathological lab analysis, can determine whether it is a skin cancer or not, and if so, what type of skin cancer it is
Other Diagnostic Studies
- In case of a metastatic stage IV skin cancer such as a large SCC, melanoma, & merkel cell carcinoma, lymph nodes become involved, which requires further testing such as:
- Sentinel lymph node biopsy
- Imaging tests for lymph node involvement such as Chest X-ray, CT, MRI, PET scan or ultrasound depending on the site involved
- Eye examination with dilated pupil to look for retina and optic nerve involvement in case of metastasis
Treatment
- Treatment of skin cancer varies depending upon the size, type, depth, location, stage of the tumor, involved body part, and patient’s general health
- Small lesions limited only to the skin surface can easily be cured by simple initial skin biopsy and may not require any further treatment whereas large lesions with metastasis require further treatment options as shown in the table below:[115][116]
Prevention
Although the possibility of skin cancer can't be eliminated completely, but the risk for developing skin cancer can be significantly reduced by acting on the following preventive measures in the first place to decrease the excessive exposure to UV rays:[96][117]
| Preventive method | Details |
|---|---|
| Avoiding sunburns and suntans | |
| Wearing protective clothing | Wear the following while being in the outdoor environment: |
| Wearing SPF sunscreen | |
| Avoiding tanning beds | |
| Being aware of sun-sensitizing medications |
|
| Checking skin regularly and reporting any new or unusual skin changes to the doctor |
|
| Watching dysplastic nevi (abnormal irregular multiple moles) regularly |
|
| Reducing the exposure to ultraviolet (UV) radiation, especially during the early years of life |
|
Effectiveness of sunscreen in prevention of skin cancer
- Multiple studies have been carried out to find out the effectiveness of sunscreen in protection against skin cancer
- International standard quantity of sunscreen application used to determine SPF is 2 mg/cm but mostly people apply only 0.5 to 1.5 mg/cm2 of sunscreen and don't reapply sunscreens after sweating excessively or swimming[118][119][120][121][122][123][124][125][126][127][128][1]
| Sunscreen property | Recommendation | Grade of Recommendations |
|---|---|---|
| SPF (Sun Protection Factor) |
| |
| Water resistance | ||
| Organic vs inorganic sunscreens | ||
| Lip protection | ||
| Sunscreen application |
| |
| Patient education on sunscreen |
| |
| Sunscreen safety |
| |
| Sunscreen benefits |
| |
| Sunscreen vehicle |
|
|
| Expiry date |
|
| Type of filter | Name of UV filter | Concentration in percentage | |
|---|---|---|---|
| Organic UVB Filters | Cinnamates | Octinoxate (octyl methoxycinnamate, Parsol MCX) | 7.5% |
| Cinoxate | 3% | ||
| PABA derivatives | 15% Para-aminobenzoic acid (PABA) | 15% | |
| Padimate O (octyl dimethyl PABA) | 8% | ||
| Salicylates | Octisalate (octyl salicylate) | 5% | |
| Homosalate | 15% | ||
| Trolamine salicylate | 12% | ||
| Others | Octocrylene | 10% | |
| Ensulizole (phenylbenzimidazole sulfonic acid) | 4% | ||
| Organic UVA Filters | Benzophenones | Oxybenzone (benzophenone-3) | 6% |
| Sulisobenzone (benzophenone-4) | 10% | ||
| Dioxybenzone (benzophenone-8) | 3% | ||
| Others | Butyl methoxydibenzoylmethane (avobenzone, Parsol 1789) | 3% | |
| Meradimate (menthyl anthranilate) | 5% | ||
| Inorganic Filters | Titanium dioxide | 25% | |
| Zinc oxide | 25% | ||
| Measurement system | SPF (Sun protection factor) | UVA‐PF (UVA‐protection factor) | UPF (Ultraviolet protection factor) |
|---|---|---|---|
| Definition |
| ||
| Developed for |
| ||
| Global acceptance |
|
|
|
| UV wavelengths protected | |||
| Examples |
| Skin type by the Fitzpatrick Scale | Skin color | Skin tone or other common descriptors | Sun exposure effects | Recommended sunscreen SPF | 1 MED- Minimal erythemal dose (as SED- standard erythemal dose) | Susceptibility to skin cancer |
|---|---|---|---|---|---|---|
| I |
|
|
30+ |
|
| |
| II |
|
|
|
|
| |
| III |
|
|
|
15+ |
|
|
| IV |
|
|
|
| ||
| V |
|
|
|
| ||
| VI |
|
|
|
Skin Cancer Prevention by using Facial-Aging Mobile App
- Studies show that photoaging mobile app usage by different adolescents actually motivates them to avoid the UV exposure after looking at their 3D selfie[129][130][131]
- One of the studies motivated:[132]
- 90.5% people to avoid using a tanning bed
- 90.2% people to improve their sun protection
- Another study showed the positive effectiveness of photoaging mobile app in changing behavioral predictors in adolescents with fair skin (i.e. Fitzpatrick skin types 1-2)[133][134]
Related Chapters
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Li, Heidi; Colantonio, Sophia; Dawson, Andrea; Lin, Xing; Beecker, Jennifer (2019). "Sunscreen Application, Safety, and Sun Protection: The Evidence". Journal of Cutaneous Medicine and Surgery. 23 (4): 357–369. doi:10.1177/1203475419856611. ISSN 1203-4754.
- ↑ 2.0 2.1 2.2 2.3 Xie HF, Liu YZ, Du R, Wang B, Chen MT, Zhang YY; et al. (2017). "miR-377 induces senescence in human skin fibroblasts by targeting DNA methyltransferase 1". Cell Death Dis. 8 (3): e2663. doi:10.1038/cddis.2017.75. PMC 5386568. PMID 28277545.
- ↑ 3.0 3.1 3.2 "Skin Cancer (Melanoma) Treatment Program - Massachusetts General Hospital, Boston, MA".
- ↑ 4.0 4.1 Koh HK, Norton LA, Geller AC, Sun T, Rigel DS, Miller DR; et al. (1996). "Evaluation of the American Academy of Dermatology's National Skin Cancer Early Detection and Screening Program". J Am Acad Dermatol. 34 (6): 971–8. doi:10.1016/s0190-9622(96)90274-1. PMID 8647990.
- ↑ 5.0 5.1 Goldberg MS, Doucette JT, Lim HW, Spencer J, Carucci JA, Rigel DS (2007). "Risk factors for presumptive melanoma in skin cancer screening: American Academy of Dermatology National Melanoma/Skin Cancer Screening Program experience 2001-2005". J Am Acad Dermatol. 57 (1): 60–6. doi:10.1016/j.jaad.2007.02.010. PMID 17490783.
- ↑ "Nonmelanoma skin cancer - Symptoms and causes - Mayo Clinic".
- ↑ 7.0 7.1 Linares MA, Zakaria A, Nizran P (2015). "Skin Cancer". Prim Care. 42 (4): 645–59. doi:10.1016/j.pop.2015.07.006. PMID 26612377.
- ↑ Lee PK (2004). "Common skin cancers". Minn Med. 87 (3): 44–7. PMID 15080294.
- ↑ 9.0 9.1 Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C (2017). "Histology of Non-Melanoma Skin Cancers: An Update". Biomedicines. 5 (4). doi:10.3390/biomedicines5040071. PMC 5744095. PMID 29261131.
- ↑ Majores M, Bierhoff E (2015). "[Actinic keratosis, Bowen's disease, keratoacanthoma and squamous cell carcinoma of the skin]". Pathologe. 36 (1): 16–29. doi:10.1007/s00292-014-2063-3. PMID 25663185.
- ↑ Hosny KM, Kassem MA, Foaud MM (2019). "Classification of skin lesions using transfer learning and augmentation with Alex-net". PLoS One. 14 (5): e0217293. doi:10.1371/journal.pone.0217293. PMC 6529006 Check
|pmc=value (help). PMID 31112591. - ↑ Mahbod A, Schaefer G, Ellinger I, Ecker R, Pitiot A, Wang C (2019). "Fusing fine-tuned deep features for skin lesion classification". Comput Med Imaging Graph. 71: 19–29. doi:10.1016/j.compmedimag.2018.10.007. PMID 30458354.
- ↑ Harangi B (2018). "Skin lesion classification with ensembles of deep convolutional neural networks". J Biomed Inform. 86: 25–32. doi:10.1016/j.jbi.2018.08.006. PMID 30103029.
- ↑ Han SS, Kim MS, Lim W, Park GH, Park I, Chang SE (2018). "Classification of the Clinical Images for Benign and Malignant Cutaneous Tumors Using a Deep Learning Algorithm". J Invest Dermatol. 138 (7): 1529–1538. doi:10.1016/j.jid.2018.01.028. PMID 29428356.
- ↑ Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM; et al. (2017). "Dermatologist-level classification of skin cancer with deep neural networks". Nature. 542 (7639): 115–118. doi:10.1038/nature21056. PMID 28117445.
- ↑ Neubert T, Lehmann P (2008). "Bowen's disease - a review of newer treatment options". Ther Clin Risk Manag. 4 (5): 1085–95. PMC 2621408. PMID 19209288.
- ↑ "Keratoacanthoma - StatPearls - NCBI Bookshelf".
- ↑ Gibbons M, Ernst A, Patel A, Armbrecht E, Behshad R (2019). "Keratoacanthomas: A review of excised specimens". J Am Acad Dermatol. 80 (6): 1794–1796. doi:10.1016/j.jaad.2019.02.011. PMID 30771415.
- ↑ Jankowska-Konsur A, Kopeć-Pytlarz K, Woźniak Z, Hryncewicz-Gwóźdź A, Maj J (2018). "Multiple disseminated keratoacanthoma-like nodules: a rare form of distant metastases to the skin". Postepy Dermatol Alergol. 35 (5): 535–537. doi:10.5114/ada.2018.77245. PMC 6232540. PMID 30429717.
- ↑ Rastogi S, Kumar P, Swarup K, Mohan L, Mukhija RD (1995). "Keratoacanthoma centrifugum marginatum". Indian J Dermatol Venereol Leprol. 61 (5): 297–8. PMID 20952995.
- ↑ Cherif F, Mebazaa A, Kort R, Makni N, Haouet S, Mokni M; et al. (2002). "[Multiple keratoacanthoma centrifugum marginatum]". Ann Dermatol Venereol. 129 (4 Pt 1): 413–5. PMID 12055541.
- ↑ Lo Schiavo A, Pinto F, Degener AM, Bucci M, Ruocco V (1996). "[Keratoacanthoma centrifugum marginatum. Possible etiological role of papillomavirus and therapeutic response to etretinate]". Ann Dermatol Venereol. 123 (10): 660–3. PMID 9615129.
- ↑ 23.0 23.1 "Cutaneous T-cell lymphoma - Symptoms and causes - Mayo Clinic".
- ↑ "Cutaneous B-Cell Lymphoma - Lymphoma Research Foundation".
- ↑ Yang Y, Yin R, Wu R, Ramirez CN, Sargsyan D, Li S; et al. (2019). "DNA methylome and transcriptome alterations and cancer prevention by triterpenoid ursolic acid in UVB-induced skin tumor in mice". Mol Carcinog. doi:10.1002/mc.23046. PMID 31237383.
- ↑ Yang Y, Wu R, Sargsyan D, Yin R, Kuo HC, Yang I; et al. (2019). "UVB drives different stages of epigenome alterations during progression of skin cancer". Cancer Lett. 449: 20–30. doi:10.1016/j.canlet.2019.02.010. PMC 6411449. PMID 30771437.
- ↑ 27.0 27.1 Yang AY, Lee JH, Shu L, Zhang C, Su ZY, Lu Y; et al. (2014). "Genome-wide analysis of DNA methylation in UVB- and DMBA/TPA-induced mouse skin cancer models". Life Sci. 113 (1–2): 45–54. doi:10.1016/j.lfs.2014.07.031. PMC 5897904. PMID 25093921.
- ↑ 28.0 28.1 Yi Y, Xie H, Xiao X, Wang B, Du R, Liu Y; et al. (2018). "Ultraviolet A irradiation induces senescence in human dermal fibroblasts by down-regulating DNMT1 via ZEB1". Aging (Albany NY). 10 (2): 212–228. doi:10.18632/aging.101383. PMC 5842848. PMID 29466247.
- ↑ Zhang C, Yuchi H, Sun L, Zhou X, Lin J (2017). "Human amnion-derived mesenchymal stem cells protect against UVA irradiation-induced human dermal fibroblast senescence, in vitro". Mol Med Rep. 16 (2): 2016–2022. doi:10.3892/mmr.2017.6795. PMC 5561982. PMID 28627622.
- ↑ Zhang C, Wen C, Lin J, Shen G (2015). "Protective effect of pyrroloquinoline quinine on ultraviolet A irradiation-induced human dermal fibroblast senescence in vitro proceeds via the anti-apoptotic sirtuin 1/nuclear factor-derived erythroid 2-related factor 2/heme oxygenase 1 pathway". Mol Med Rep. 12 (3): 4382–4388. doi:10.3892/mmr.2015.3990. PMID 26126510.
- ↑ Youn HJ, Kim KB, Han HS, An IS, Ahn KJ (2017). "23-Hydroxytormentic acid protects human dermal fibroblasts by attenuating UVA-induced oxidative stress". Photodermatol Photoimmunol Photomed. 33 (2): 92–100. doi:10.1111/phpp.12294. PMID 28106292.
- ↑ Yang S, Zhou B, Xu W, Xue F, Nisar MF, Bian C; et al. (2017). "Nrf2- and Bach1 May Play a Role in the Modulation of Ultraviolet A-Induced Oxidative Stress by Acetyl-11-Keto-β-Boswellic Acid in Skin Keratinocytes". Skin Pharmacol Physiol. 30 (1): 13–23. doi:10.1159/000452744. PMID 28142143.
- ↑ Hseu YC, Chou CW, Senthil Kumar KJ, Fu KT, Wang HM, Hsu LS; et al. (2012). "Ellagic acid protects human keratinocyte (HaCaT) cells against UVA-induced oxidative stress and apoptosis through the upregulation of the HO-1 and Nrf-2 antioxidant genes". Food Chem Toxicol. 50 (5): 1245–55. doi:10.1016/j.fct.2012.02.020. PMID 22386815.
- ↑ Hseu YC, Lo HW, Korivi M, Tsai YC, Tang MJ, Yang HL (2015). "Dermato-protective properties of ergothioneine through induction of Nrf2/ARE-mediated antioxidant genes in UVA-irradiated Human keratinocytes". Free Radic Biol Med. 86: 102–17. doi:10.1016/j.freeradbiomed.2015.05.026. PMID 26021820.
- ↑ Zhao P, Alam MB, Lee SH (2018). "Protection of UVB-Induced Photoaging by Fuzhuan-Brick Tea Aqueous Extract via MAPKs/Nrf2-Mediated Down-Regulation of MMP-1". Nutrients. 11 (1). doi:10.3390/nu11010060. PMC 6357030. PMID 30597920.
- ↑ Sun Z, Park SY, Hwang E, Zhang M, Seo SA, Lin P; et al. (2017). "Thymus vulgaris alleviates UVB irradiation induced skin damage via inhibition of MAPK/AP-1 and activation of Nrf2-ARE antioxidant system". J Cell Mol Med. 21 (2): 336–348. doi:10.1111/jcmm.12968. PMC 5264136. PMID 27641753.
- ↑ Sun Z, Du J, Hwang E, Yi TH (2018). "Paeonol extracted from Paeonia suffruticosa Andr. ameliorated UVB-induced skin photoaging via DLD/Nrf2/ARE and MAPK/AP-1 pathway". Phytother Res. 32 (9): 1741–1749. doi:10.1002/ptr.6100. PMID 29748977.
- ↑ Al-Matouq J, Holmes TR, Hansen LA (2019). "CDC25B and CDC25C overexpression in nonmelanoma skin cancer suppresses cell death". Mol Carcinog. doi:10.1002/mc.23075. PMID 31237025.
- ↑ Sehati N, Sadeghie N, Mansoori B, Mohammadi A, Shanehbandi D, Baradaran B (2019). "MicroRNA-330 inhibits growth and migration of melanoma A375 cells: In vitro study". J Cell Biochem. doi:10.1002/jcb.29211. PMID 31237010.
- ↑ Xiong Y, Liu L, Qiu Y, Liu L (2018). "MicroRNA-29a Inhibits Growth, Migration and Invasion of Melanoma A375 Cells in Vitro by Directly Targeting BMI1". Cell Physiol Biochem. 50 (1): 385–397. doi:10.1159/000494015. PMID 30286469.
- ↑ Mao XH, Chen M, Wang Y, Cui PG, Liu SB, Xu ZY (2017). "MicroRNA-21 regulates the ERK/NF-κB signaling pathway to affect the proliferation, migration, and apoptosis of human melanoma A375 cells by targeting SPRY1, PDCD4, and PTEN". Mol Carcinog. 56 (3): 886–894. doi:10.1002/mc.22542. PMID 27533779.
- ↑ Orioli D, Dellambra E (2018). "Epigenetic Regulation of Skin Cells in Natural Aging and Premature Aging Diseases". Cells. 7 (12). doi:10.3390/cells7120268. PMC 6315602. PMID 30545089.
- ↑ 43.0 43.1 Gesumaria L, Matsui MS, Kluz T, Costa M (2015). "Solar-simulated ultraviolet radiation induces histone 3 methylation changes in the gene promoters of matrix metalloproteinases 1 and 3 in primary human dermal fibroblasts". Exp Dermatol. 24 (5): 384–5. doi:10.1111/exd.12675. PMC 4471858. PMID 25707437.
- ↑ Gilchrest BA (2013). "Photoaging". J Invest Dermatol. 133 (E1): E2–6. doi:10.1038/skinbio.2013.176. PMID 23820721.
- ↑ Poon F, Kang S, Chien AL (2015). "Mechanisms and treatments of photoaging". Photodermatol Photoimmunol Photomed. 31 (2): 65–74. doi:10.1111/phpp.12145. PMID 25351668.
- ↑ Xie H, Liu F, Liu L, Dan J, Luo Y, Yi Y; et al. (2013). "Protective role of AQP3 in UVA-induced NHSFs apoptosis via Bcl2 up-regulation". Arch Dermatol Res. 305 (5): 397–406. doi:10.1007/s00403-013-1324-y. PMID 23463292.
- ↑ Battie C, Jitsukawa S, Bernerd F, Del Bino S, Marionnet C, Verschoore M (2014). "New insights in photoaging, UVA induced damage and skin types". Exp Dermatol. 23 Suppl 1: 7–12. doi:10.1111/exd.12388. PMID 25234829.
- ↑ Rando TA, Chang HY (2012). "Aging, rejuvenation, and epigenetic reprogramming: resetting the aging clock". Cell. 148 (1–2): 46–57. doi:10.1016/j.cell.2012.01.003. PMC 3336960. PMID 22265401.
- ↑ Bormann F, Rodríguez-Paredes M, Hagemann S, Manchanda H, Kristof B, Gutekunst J; et al. (2016). "Reduced DNA methylation patterning and transcriptional connectivity define human skin aging". Aging Cell. 15 (3): 563–71. doi:10.1111/acel.12470. PMC 4854925. PMID 27004597.
- ↑ Pollack BP, Sapkota B, Boss JM (2009). "Ultraviolet radiation-induced transcription is associated with gene-specific histone acetylation". Photochem Photobiol. 85 (3): 652–62. doi:10.1111/j.1751-1097.2008.00485.x. PMID 19076306.
- ↑ Zheng QH, Ma LW, Zhu WG, Zhang ZY, Tong TJ (2006). "p21Waf1/Cip1 plays a critical role in modulating senescence through changes of DNA methylation". J Cell Biochem. 98 (5): 1230–48. doi:10.1002/jcb.20838. PMID 16514663.
- ↑ So AY, Jung JW, Lee S, Kim HS, Kang KS (2011). "DNA methyltransferase controls stem cell aging by regulating BMI1 and EZH2 through microRNAs". PLoS One. 6 (5): e19503. doi:10.1371/journal.pone.0019503. PMC 3091856. PMID 21572997.
- ↑ Kinney SR, Pradhan S (2011). "Regulation of expression and activity of DNA (cytosine-5) methyltransferases in mammalian cells". Prog Mol Biol Transl Sci. 101: 311–33. doi:10.1016/B978-0-12-387685-0.00009-3. PMID 21507356.
- ↑ Benetti R, Gonzalo S, Jaco I, Muñoz P, Gonzalez S, Schoeftner S; et al. (2008). "A mammalian microRNA cluster controls DNA methylation and telomere recombination via Rbl2-dependent regulation of DNA methyltransferases". Nat Struct Mol Biol. 15 (3): 268–79. doi:10.1038/nsmb.1399. PMC 2990406. PMID 18311151.
- ↑ Kar S, Deb M, Sengupta D, Shilpi A, Parbin S, Torrisani J; et al. (2012). "An insight into the various regulatory mechanisms modulating human DNA methyltransferase 1 stability and function". Epigenetics. 7 (9): 994–1007. doi:10.4161/epi.21568. PMC 3515020. PMID 22894906.
- ↑ Pal S, Tyler JK (2016). "Epigenetics and aging". Sci Adv. 2 (7): e1600584. doi:10.1126/sciadv.1600584. PMC 4966880. PMID 27482540.
- ↑ Sierra MI, Fernández AF, Fraga MF (2015). "Epigenetics of Aging". Curr Genomics. 16 (6): 435–40. doi:10.2174/1389202916666150817203459. PMC 4765531. PMID 27019618.
- ↑ Jung M, Pfeifer GP (2015). "Aging and DNA methylation". BMC Biol. 13: 7. doi:10.1186/s12915-015-0118-4. PMC 4311512. PMID 25637097.
- ↑ Nandakumar V, Vaid M, Tollefsbol TO, Katiyar SK (2011). "Aberrant DNA hypermethylation patterns lead to transcriptional silencing of tumor suppressor genes in UVB-exposed skin and UVB-induced skin tumors of mice". Carcinogenesis. 32 (4): 597–604. doi:10.1093/carcin/bgq282. PMC 3066413. PMID 21186298.
- ↑ Prasad R, Katiyar SK (2013). "Prostaglandin E2 Promotes UV radiation-induced immune suppression through DNA hypermethylation". Neoplasia. 15 (7): 795–804. doi:10.1593/neo.13424. PMC 3689242. PMID 23814491.
- ↑ López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013). "The hallmarks of aging". Cell. 153 (6): 1194–217. doi:10.1016/j.cell.2013.05.039. PMC 3836174. PMID 23746838.
- ↑ Postigo AA (2003). "Opposing functions of ZEB proteins in the regulation of the TGFbeta/BMP signaling pathway". EMBO J. 22 (10): 2443–52. doi:10.1093/emboj/cdg225. PMC 155983. PMID 12743038.
- ↑ Postigo AA, Depp JL, Taylor JJ, Kroll KL (2003). "Regulation of Smad signaling through a differential recruitment of coactivators and corepressors by ZEB proteins". EMBO J. 22 (10): 2453–62. doi:10.1093/emboj/cdg226. PMC 155984. PMID 12743039.
- ↑ Johnson AA, Akman K, Calimport SR, Wuttke D, Stolzing A, de Magalhães JP (2012). "The role of DNA methylation in aging, rejuvenation, and age-related disease". Rejuvenation Res. 15 (5): 483–94. doi:10.1089/rej.2012.1324. PMC 3482848. PMID 23098078.
- ↑ Kim HY, Lee DH, Shin MH, Shin HS, Kim MK, Chung JH (2018). "UV-induced DNA methyltransferase 1 promotes hypermethylation of tissue inhibitor of metalloproteinase 2 in the human skin". J Dermatol Sci. 91 (1): 19–27. doi:10.1016/j.jdermsci.2018.03.009. PMID 29685765.
- ↑ Rundhaug JE, Fischer SM (2008). "Cyclo-oxygenase-2 plays a critical role in UV-induced skin carcinogenesis". Photochem Photobiol. 84 (2): 322–9. doi:10.1111/j.1751-1097.2007.00261.x. PMID 18194346.
- ↑ An KP, Athar M, Tang X, Katiyar SK, Russo J, Beech J; et al. (2002). "Cyclooxygenase-2 expression in murine and human nonmelanoma skin cancers: implications for therapeutic approaches". Photochem Photobiol. 76 (1): 73–80. PMID 12126310.
- ↑ Fischer SM (2002). "Is cyclooxygenase-2 important in skin carcinogenesis?". J Environ Pathol Toxicol Oncol. 21 (2): 183–91. PMID 12086405.
- ↑ Maldve RE, Kim Y, Muga SJ, Fischer SM (2000). "Prostaglandin E(2) regulation of cyclooxygenase expression in keratinocytes is mediated via cyclic nucleotide-linked prostaglandin receptors". J Lipid Res. 41 (6): 873–81. PMID 10828079.
- ↑ Yu H, Yang W (2016). "MiR-211 is epigenetically regulated by DNMT1 mediated methylation and inhibits EMT of melanoma cells by targeting RAB22A". Biochem Biophys Res Commun. 476 (4): 400–405. doi:10.1016/j.bbrc.2016.05.133. PMID 27237979.
- ↑ Mancini M, Lena AM, Saintigny G, Mahé C, Di Daniele N, Melino G; et al. (2014). "MicroRNAs in human skin ageing". Ageing Res Rev. 17: 9–15. doi:10.1016/j.arr.2014.04.003. PMID 24784027.
- ↑ Mancini M, Saintigny G, Mahé C, Annicchiarico-Petruzzelli M, Melino G, Candi E (2012). "MicroRNA-152 and -181a participate in human dermal fibroblasts senescence acting on cell adhesion and remodeling of the extra-cellular matrix". Aging (Albany NY). 4 (11): 843–53. doi:10.18632/aging.100508. PMC 3560438. PMID 23238588.
- ↑ Jung HJ, Byun HO, Jee BA, Min S, Jeoun UW, Lee YK; et al. (2017). "The Ubiquitin-like with PHD and Ring Finger Domains 1 (UHRF1)/DNA Methyltransferase 1 (DNMT1) Axis Is a Primary Regulator of Cell Senescence". J Biol Chem. 292 (9): 3729–3739. doi:10.1074/jbc.M116.750539. PMC 5339756. PMID 28100769.
- ↑ Katalinic A, Kunze U, Schäfer T (2003). "Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer)". Br J Dermatol. 149 (6): 1200–6. doi:10.1111/j.1365-2133.2003.05554.x. PMID 14674897.
- ↑ Rudolph C, Schnoor M, Eisemann N, Katalinic A (2015). "Incidence trends of nonmelanoma skin cancer in Germany from 1998 to 2010". J Dtsch Dermatol Ges. 13 (8): 788–97. doi:10.1111/ddg.12690. PMID 26213814.
- ↑ Bulliard JL, Panizzon RG, Levi F (2009). "[Epidemiology of epithelial skin cancers]". Rev Med Suisse. 5 (200): 882, 884–8. PMID 19438088.
- ↑ Stenbeck KD, Balanda KP, Williams MJ, Ring IT, MacLennan R, Chick JE; et al. (1990). "Patterns of treated non-melanoma skin cancer in Queensland--the region with the highest incidence rates in the world". Med J Aust. 153 (9): 511–5. PMID 2233471.
- ↑ Marks R, Jolley D, Dorevitch AP, Selwood TS (1989). "The incidence of non-melanocytic skin cancers in an Australian population: results of a five-year prospective study". Med J Aust. 150 (9): 475–8. PMID 2786135.
- ↑ Freeman NR, Fairbrother GE, Rose RJ (1982). "Survey of skin cancer incidence in the Hamilton area". N Z Med J. 95 (713): 529–33. PMID 6957767.
- ↑ Whiteman DC, Green AC, Olsen CM (2016). "The Growing Burden of Invasive Melanoma: Projections of Incidence Rates and Numbers of New Cases in Six Susceptible Populations through 2031". J Invest Dermatol. 136 (6): 1161–1171. doi:10.1016/j.jid.2016.01.035. PMID 26902923.
- ↑ de Vries E, Coebergh JW (2004). "Cutaneous malignant melanoma in Europe". Eur J Cancer. 40 (16): 2355–66. doi:10.1016/j.ejca.2004.06.003. PMID 15519506.
- ↑ Lasithiotakis K, Krüger-Krasagakis S, Manousaki A, Ioannidou D, Panagiotides I, Tosca A (2006). "The incidence of cutaneous melanoma on Crete, Greece". Int J Dermatol. 45 (4): 397–401. doi:10.1111/j.1365-4632.2006.02492.x. PMID 16650166.
- ↑ Månsson-Brahme E, Johansson H, Larsson O, Rutqvist LE, Ringborg U (2002). "Trends in incidence of cutaneous malignant melanoma in a Swedish population 1976-1994". Acta Oncol. 41 (2): 138–46. PMID 12102157.
- ↑ Stang A, Pukkala E, Sankila R, Söderman B, Hakulinen T (2006). "Time trend analysis of the skin melanoma incidence of Finland from 1953 through 2003 including 16,414 cases". Int J Cancer. 119 (2): 380–4. doi:10.1002/ijc.21836. PMID 16477634.
- ↑ Ulmer MJ, Tonita JM, Hull PR (2003). "Trends in invasive cutaneous melanoma in Saskatchewan 1970-1999". J Cutan Med Surg. 7 (6): 433–42. doi:10.1177/120347540300700601. PMID 15926213.
- ↑ Dennis LK (1999). "Analysis of the melanoma epidemic, both apparent and real: data from the 1973 through 1994 surveillance, epidemiology, and end results program registry". Arch Dermatol. 135 (3): 275–80. PMID 10086448.
- ↑ Geller AC, Miller DR, Annas GD, Demierre MF, Gilchrest BA, Koh HK (2002). "Melanoma incidence and mortality among US whites, 1969-1999". JAMA. 288 (14): 1719–20. doi:10.1001/jama.288.14.1719. PMID 12365954.
- ↑ Hall HI, Miller DR, Rogers JD, Bewerse B (1999). "Update on the incidence and mortality from melanoma in the United States". J Am Acad Dermatol. 40 (1): 35–42. doi:10.1016/s0190-9622(99)70562-1. PMID 9922010.
- ↑ Perera E, Gnaneswaran N, Staines C, Win AK, Sinclair R (2015). "Incidence and prevalence of non-melanoma skin cancer in Australia: A systematic review". Australas J Dermatol. 56 (4): 258–67. doi:10.1111/ajd.12282. PMID 25716064.
- ↑ "Common Cancer Types - National Cancer Institute".
- ↑ "Cancer Facts & Figures 2016 | American Cancer Society".
- ↑ Welch HG, Woloshin S, Schwartz LM (2005). "Skin biopsy rates and incidence of melanoma: population based ecological study". BMJ. 331 (7515): 481. doi:10.1136/bmj.38516.649537.E0. PMC 1199022. PMID 16081427.
- ↑ 93.0 93.1 "Melanoma of the Skin - Cancer Stat Facts".
- ↑ Monshi B, Vujic M, Kivaranovic D, Sesti A, Oberaigner W, Vujic I; et al. (2016). "The burden of malignant melanoma--lessons to be learned from Austria". Eur J Cancer. 56: 45–53. doi:10.1016/j.ejca.2015.11.026. PMID 26802530.
- ↑ Ishdorj G, Beiggi S, Nugent Z, Streu E, Banerji V, Dhaliwal D; et al. (2019). "Risk factors for skin cancer and solid tumors in newly diagnosed patients with chronic lymphocytic leukemia and the impact of skin surveillance on survival". Leuk Lymphoma: 1–10. doi:10.1080/10428194.2019.1620941. PMID 31237469.
- ↑ 96.0 96.1 "Skin cancer - Symptoms and causes - Mayo Clinic".
- ↑ Duarte AF, Sousa-Pinto B, Haneke E, Correia O (2018). "Risk factors for development of new skin neoplasms in patients with past history of skin cancer: A survival analysis". Sci Rep. 8 (1): 15744. doi:10.1038/s41598-018-33763-7. PMC 6200724. PMID 30356134.
- ↑ van der Leest RJT, Hollestein LM, Liu L, Nijsten T, de Vries E (2018). "Risks of different skin tumour combinations after a first melanoma, squamous cell carcinoma and basal cell carcinoma in Dutch population-based cohorts: 1989-2009". J Eur Acad Dermatol Venereol. 32 (3): 382–389. doi:10.1111/jdv.14587. PMID 28898461.
- ↑ Milán T, Pukkala E, Verkasalo PK, Kaprio J, Jansén CT, Koskenvuo M; et al. (2000). "Subsequent primary cancers after basal-cell carcinoma: A nationwide study in Finland from 1953 to 1995". Int J Cancer. 87 (2): 283–8. PMID 10861488.
- ↑ Levi F, La Vecchia C, Te VC, Randimbison L, Erler G (1998). "Incidence of invasive cancers following basal cell skin cancer". Am J Epidemiol. 147 (8): 722–6. doi:10.1093/oxfordjournals.aje.a009516. PMID 9554413.
- ↑ Levi F, Randimbison L, Maspoli M, Te VC, La Vecchia C (2006). "High incidence of second basal cell skin cancers". Int J Cancer. 119 (6): 1505–7. doi:10.1002/ijc.22000. PMID 16642479.
- ↑ Gauwerky K, Ruzicka T, Berking C (2009). "[Skin cancer screening at the family doctor's office]". MMW Fortschr Med. 151 (25): 38–42, quiz 43. PMID 19739523.
- ↑ Treiber N, Huber MA, Scharffetter-Kochanek K, Schneider LA (2014). "[Early detection of skin cancer]". MMW Fortschr Med. 156 (4): 37–40. PMID 24908774.
- ↑ Mierzwa T, Zegarski W, Placek W, Zegarska B (2004). "[Skin cancer screening program in the population of Bydgoszcz]". Wiad Lek. 57 Suppl 1: 211–4. PMID 15884241.
- ↑ Bajaj S, Wolner ZJ, Dusza SW, Braun RP, Marghoob AA, DeFazio J (2019). "Total Body Skin Examination Practices: A Survey Study Amongst Dermatologists at High-Risk Skin Cancer Clinics". Dermatol Pract Concept. 9 (2): 132–138. doi:10.5826/dpc.0902a09. PMC 6502292 Check
|pmc=value (help). PMID 31106016. - ↑ Argenziano G, Zalaudek I, Hofmann-Wellenhof R, Bakos RM, Bergman W, Blum A; et al. (2012). "Total body skin examination for skin cancer screening in patients with focused symptoms". J Am Acad Dermatol. 66 (2): 212–9. doi:10.1016/j.jaad.2010.12.039. PMID 21757257.
- ↑ "Skin Cancer Screening: MedlinePlus Lab Test Information".
- ↑ 108.0 108.1 Argenziano G, Puig S, Zalaudek I, Sera F, Corona R, Alsina M; et al. (2006). "Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer". J Clin Oncol. 24 (12): 1877–82. doi:10.1200/JCO.2005.05.0864. PMID 16622262.
- ↑ 109.0 109.1 Menzies SW, Emery J, Staples M, Davies S, McAvoy B, Fletcher J; et al. (2009). "Impact of dermoscopy and short-term sequential digital dermoscopy imaging for the management of pigmented lesions in primary care: a sequential intervention trial". Br J Dermatol. 161 (6): 1270–7. doi:10.1111/j.1365-2133.2009.09374.x. PMID 19747359.
- ↑ 110.0 110.1 van der Rhee JI, Bergman W, Kukutsch NA (2010). "The impact of dermoscopy on the management of pigmented lesions in everyday clinical practice of general dermatologists: a prospective study". Br J Dermatol. 162 (3): 563–7. doi:10.1111/j.1365-2133.2009.09551.x. PMID 19832836.
- ↑ 111.0 111.1 Dinnes J, Deeks JJ, Chuchu N, Ferrante di Ruffano L, Matin RN, Thomson DR; et al. (2018). "Dermoscopy, with and without visual inspection, for diagnosing melanoma in adults". Cochrane Database Syst Rev. 12: CD011902. doi:10.1002/14651858.CD011902.pub2. PMC 6517096 Check
|pmc=value (help). PMID 30521682. - ↑ 112.0 112.1 Ferrante di Ruffano L, Takwoingi Y, Dinnes J, Chuchu N, Bayliss SE, Davenport C; et al. (2018). "Computer-assisted diagnosis techniques (dermoscopy and spectroscopy-based) for diagnosing skin cancer in adults". Cochrane Database Syst Rev. 12: CD013186. doi:10.1002/14651858.CD013186. PMC 6517147 Check
|pmc=value (help). PMID 30521691. - ↑ 113.0 113.1 Ferrante di Ruffano L, Dinnes J, Deeks JJ, Chuchu N, Bayliss SE, Davenport C; et al. (2018). "Optical coherence tomography for diagnosing skin cancer in adults". Cochrane Database Syst Rev. 12: CD013189. doi:10.1002/14651858.CD013189. PMID 30521690.
- ↑ Godsell G (2003). "Recognising the signs of skin cancer". Nurs Times. 99 (31): 44–5. PMID 13677122.
- ↑ "Skin cancer - Diagnosis and treatment - Mayo Clinic".
- ↑ "Skin Cancer Treatment (PDQ®)–Patient Version - National Cancer Institute".
- ↑ "Skin Cancer Prevention and Early Detection".
- ↑ Diffey BL (2001). "When should sunscreen be reapplied?". J Am Acad Dermatol. 45 (6): 882–5. doi:10.1067/mjd.2001.117385. PMID 11712033.
- ↑ "Sunscreens in the Management of Photodermatoses".
- ↑ "Update on Sunscreens".
- ↑ Young AR, Claveau J, Rossi AB (2017). "Ultraviolet radiation and the skin: Photobiology and sunscreen photoprotection". J Am Acad Dermatol. 76 (3S1): S100–S109. doi:10.1016/j.jaad.2016.09.038. PMID 28038885.
- ↑ Burnett ME, Hu JY, Wang SQ (2012). "Sunscreens: obtaining adequate photoprotection". Dermatol Ther. 25 (3): 244–51. doi:10.1111/j.1529-8019.2012.01503.x. PMID 22913442.
- ↑ Bissonnette R (2008). "Update on sunscreens". Skin Therapy Lett. 13 (6): 5–7. PMID 18806906.
- ↑ Medeiros VL, Lim HW (2010). "Sunscreens in the management of photodermatoses". Skin Therapy Lett. 15 (6): 1–3. PMID 20532468.
- ↑ Diaz JH, Nesbitt LT (2013). "Sun exposure behavior and protection: recommendations for travelers". J Travel Med. 20 (2): 108–18. doi:10.1111/j.1708-8305.2012.00667.x. PMID 23464719.
- ↑ Andersen PA, Buller DB, Walkosz BJ, Scott MD, Beck L, Liu X; et al. (2017). "A Randomized Trial of an Advanced Sun Safety Intervention for Vacationers at 41 North American Resorts". J Health Commun. 22 (12): 951–963. doi:10.1080/10810730.2017.1382615. PMC 6309206. PMID 29161214.
- ↑ Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR (2017). "Effect of an intervention on observed sun protection by vacationers in a randomized controlled trial at North American resorts". Prev Med. 99: 29–36. doi:10.1016/j.ypmed.2017.01.014. PMC 5432386. PMID 28189810.
- ↑ Buller DB, Andersen PA, Walkosz BJ, Scott MD, Beck L, Cutter GR (2016). "Rationale, design, samples, and baseline sun protection in a randomized trial on a skin cancer prevention intervention in resort environments". Contemp Clin Trials. 46: 67–76. doi:10.1016/j.cct.2015.11.015. PMC 4714565. PMID 26593781.
- ↑ Brinker TJ, Heckl M, Gatzka M, Heppt MV, Resende Rodrigues H, Schneider S; et al. (2018). "A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study". JMIR Mhealth Uhealth. 6 (3): e60. doi:10.2196/mhealth.9794. PMC 5866300. PMID 29523502.
- ↑ Brinker TJ, Brieske CM, Schaefer CM, Buslaff F, Gatzka M, Petri MP; et al. (2017). "Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study". J Med Internet Res. 19 (9): e319. doi:10.2196/jmir.8661. PMC 5610355. PMID 28887295.
- ↑ Brinker TJ, Schadendorf D, Klode J, Cosgarea I, Rösch A, Jansen P; et al. (2017). "Photoaging Mobile Apps as a Novel Opportunity for Melanoma Prevention: Pilot Study". JMIR Mhealth Uhealth. 5 (7): e101. doi:10.2196/mhealth.8231. PMC 5550737. PMID 28747297.
- ↑ "JMU - A Skin Cancer Prevention Facial-Aging Mobile App for Secondary Schools in Brazil: Appearance-Focused Interventional Study | Brinker | JMIR mHealth and uHealth".
- ↑ Brinker, Titus Josef; Brieske, Christian Martin; Schaefer, Christoph Matthias; Buslaff, Fabian; Gatzka, Martina; Petri, Maximilian Philip; Sondermann, Wiebke; Schadendorf, Dirk; Stoffels, Ingo; Klode, Joachim (2017). "Photoaging Mobile Apps in School-Based Melanoma Prevention: Pilot Study". Journal of Medical Internet Research. 19 (9): e319. doi:10.2196/jmir.8661. ISSN 1438-8871.
- ↑ Brinker, Titus Josef; Schadendorf, Dirk; Klode, Joachim; Cosgarea, Ioana; Rösch, Alexander; Jansen, Philipp; Stoffels, Ingo; Izar, Benjamin (2017). "Photoaging Mobile Apps as a Novel Opportunity for Melanoma Prevention: Pilot Study". JMIR mHealth and uHealth. 5 (7): e101. doi:10.2196/mhealth.8231. ISSN 2291-5222.