ST elevation myocardial infarction case study four
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction case study four On the Web |
|
ST elevation myocardial infarction case study four in the news |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction case study four |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
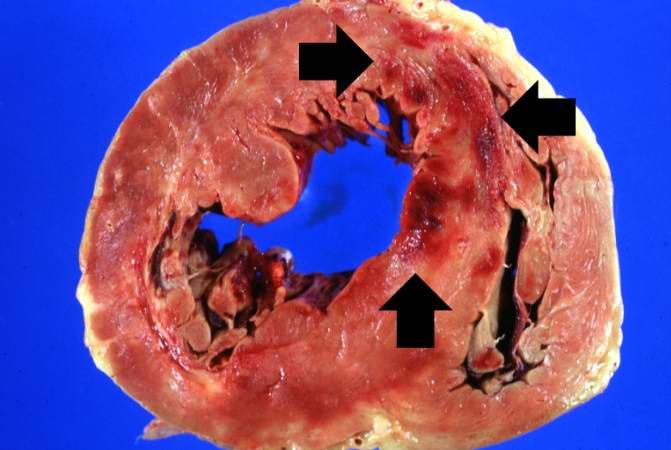
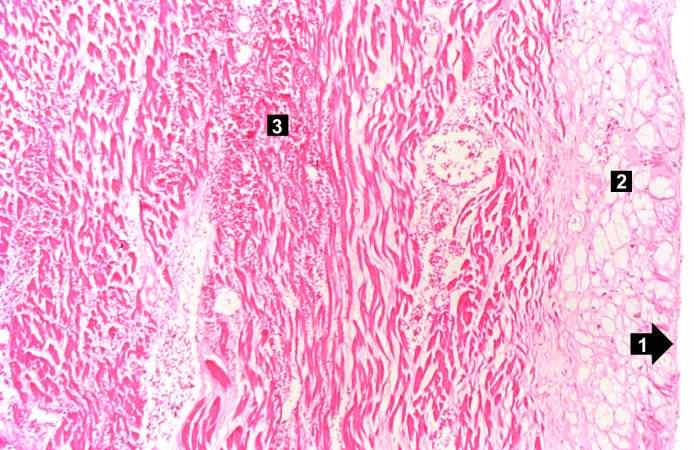
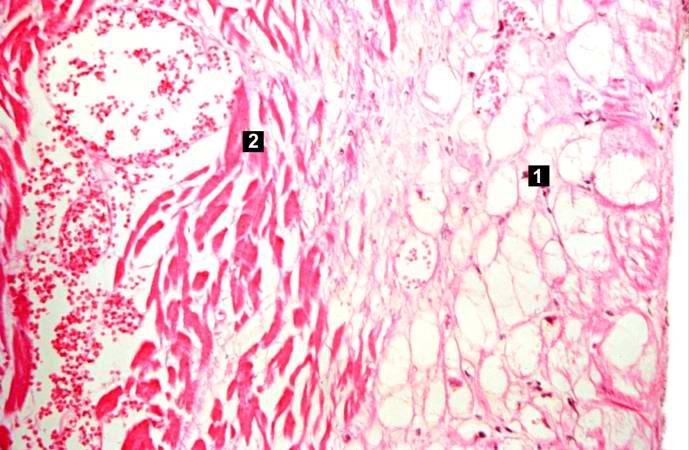
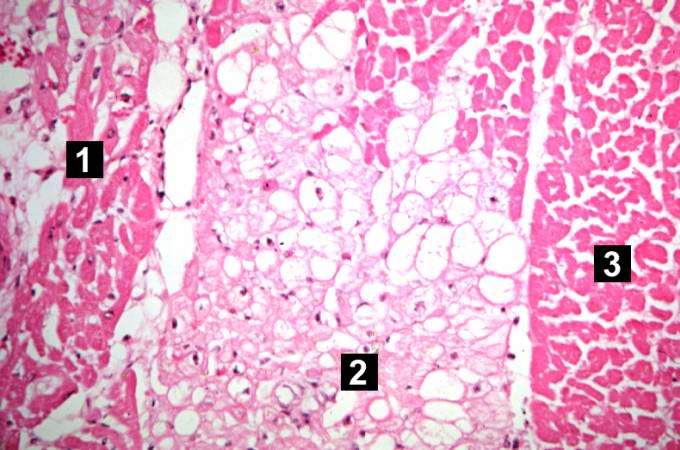
Case 4: Coagulative Necrosis
Clinical Summary
This was a 57-year-old male whose hospital course following abdominal surgery was characterized by progressive deterioration and hypotension.
Four days post-operatively, the patient sustained an anterior myocardial infarction and died the next day.
Autopsy Findings
The patient's heart weighed 410 grams.
Examination of the coronary arteries revealed marked atherosclerotic narrowing of all three vessels with focal occlusion by a thrombus of the left anterior descending artery.
Fresh necrosis of the anterior wall of the left ventricle and anterior portion of the septum was present, extending from the endocardium to the inner half of the ventricular wall.
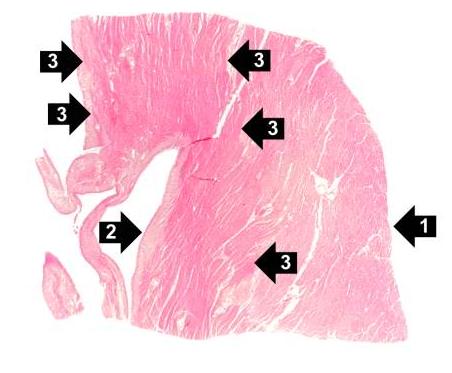
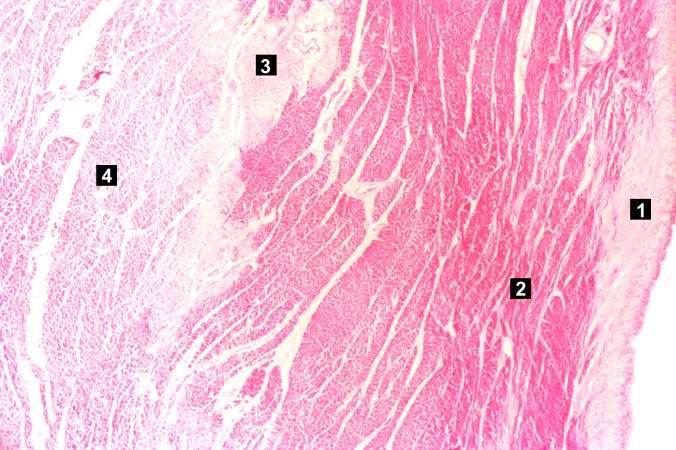
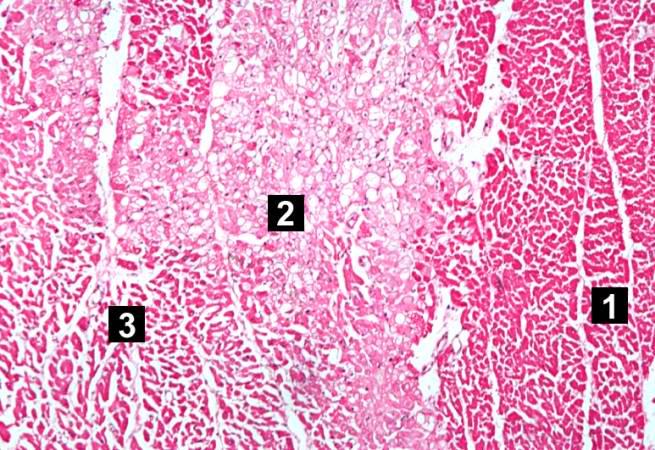
Histopathological Findings