ST elevation myocardial infarction case study five
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction case study five On the Web |
|
ST elevation myocardial infarction case study five in the news |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction case study five |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Case 5: Mural Thrombus
Clinical Summary
A 67-year-old female was transferred to the hospital from a nursing home in a comatose state.
Physical findings on examination were compatible with brain stem infarction.
On the fourth hospital day, an electrocardiogram revealed changes compatible with anterior myocardial infarction.
The patient remained comatose with quadriplegia and died on the 16th day of hospital stay.
Autopsy Findings
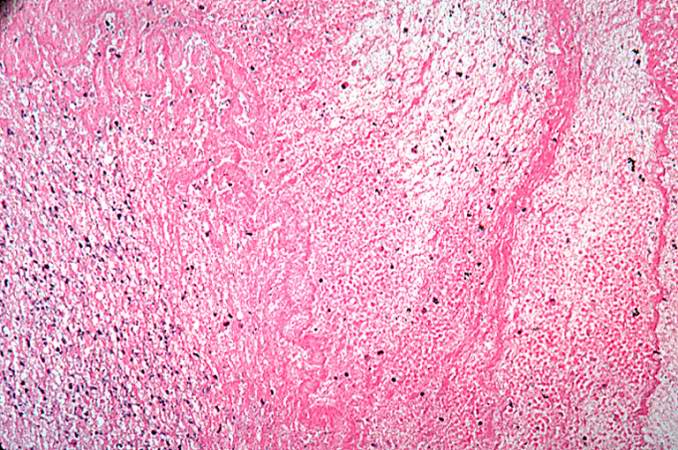
Examination of the brain revealed extensive infarction involving the midbrain and cerebellum with complete occlusion of the upper one-half of the basilar artery; there was also extensive coronary artery atherosclerosis.
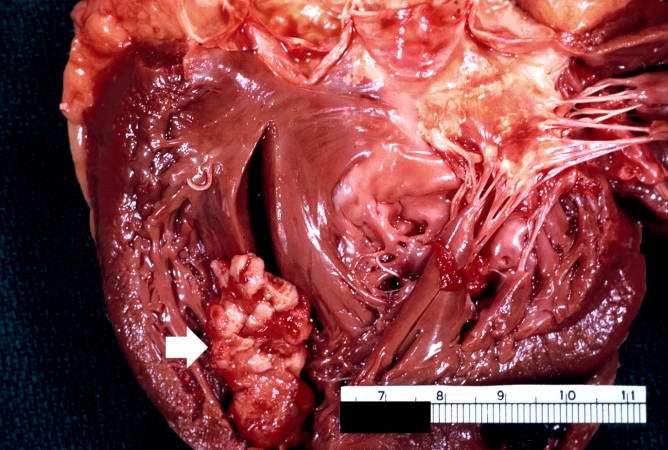
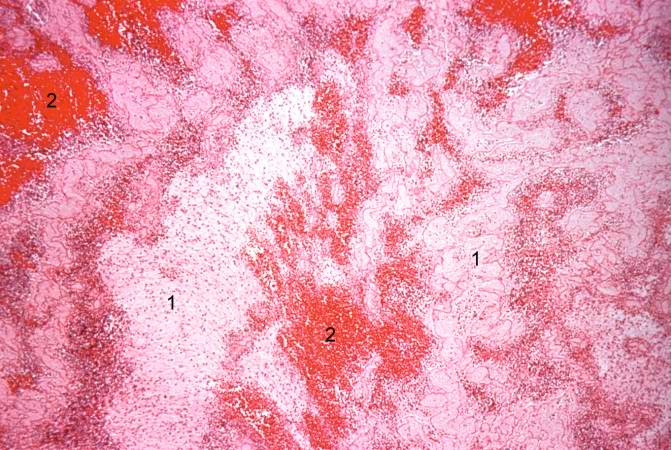
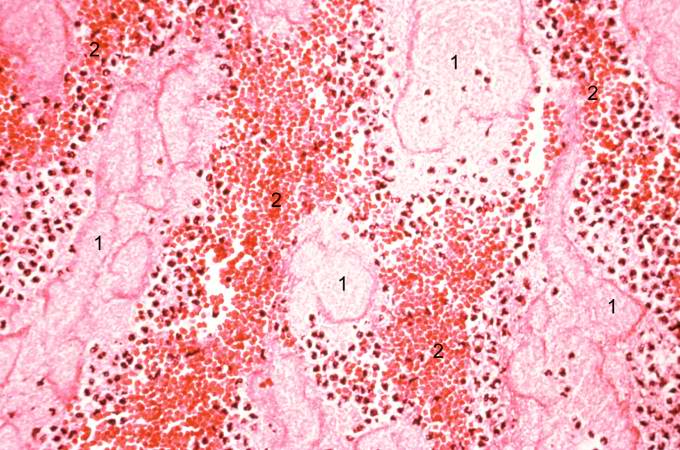
A large aneurysm of the left ventricle was present; this was filled with mural thrombus.
Extensive infarction of the lateral and posterior portions of the left ventricular wall toward the base of the heart was also found.
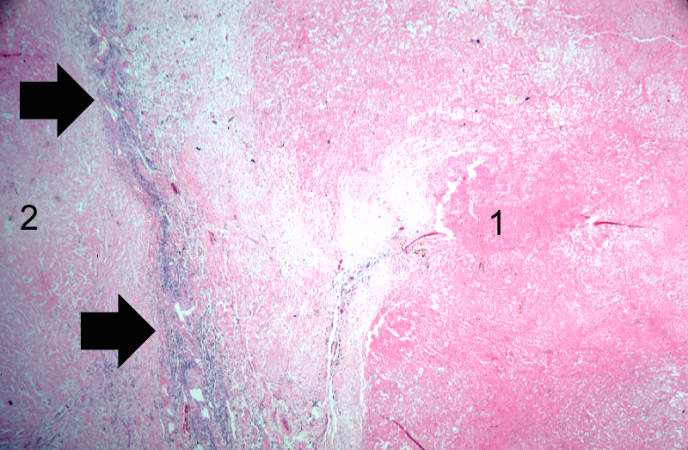
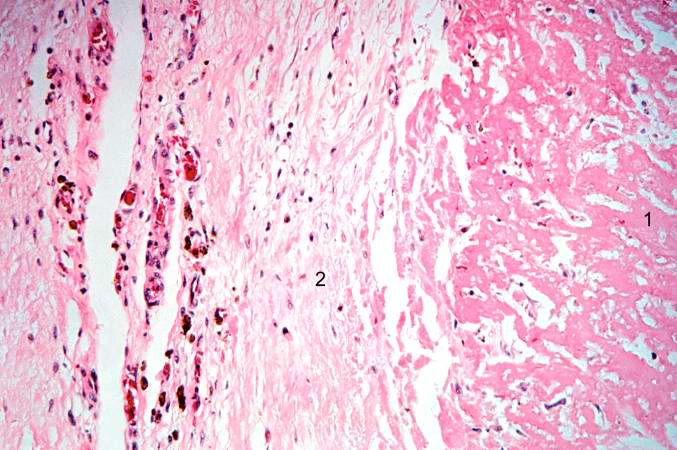
Histopathological Findings